Abstract
Healthcare is experiencing a rapid transformation largely due to the challenges posed by rising costs, inequalities in health provision, pandemics, aging populations and the rise in non-communicable diseases. Design is now playing an important role in addressing these challenges, by applying a user centred approach to transform healthcare along with the development of new products, services systems and spaces. This special issue first describes current advances within healthcare and the role of design in the future of health care. It then introduces three papers that address design for health and wellbeing. The first paper describes design probes to configure sensory conditions to reduce pain in hospitals. The second paper, explores the use of participatory design in the co-designing of resources for knowledge-based self-reflection for people living with Parkinson’s disease to enable independent living. The third paper describes a multidisciplinary research project concerned with the development and prototyping of a training tool for neurosurgery. This special issue highlights the varied benefits that design can bring to create better experiences for all stakeholder within the healthcare model. It advocates for Design to continue to be a major part of this transformation in healthcare.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
With ageing populations, more people living with chronic conditions, Covid 19, further threats from pandemics and stretched funding, there are huge global challenges for our future healthcare. Healthcare transformation requires a shared vision between various stakeholders to create patient-centered models [6]. Design has become the focus in solving challenges in health care, and is leading to the development of new products, services systems and spaces. These can range from medical devices for surgery, wearable, smartphone and sensor based products to monitor health, digital and visual tools to support patients, systems that can be navigated smoothly, spaces that create an improved experience to virtual visits with clinicians and online pharmacies. Design is about improving people’s lives. Design influences behaviour to adopt positive health care choices. It seeks to understand and incorporate all viewpoints to arrive at solutions to complex challenges.
1 Innovation in Health and Wellbeing
Healthcare has traditionally focused on diagnosis and treatment. The focus is shifting from health care to health and well-being and from treatment to prevention. There will be a greater emphasises on the promotion of healthy lifestyles, fitness, and wellbeing, prevention and early diagnosis [32]. Meskó [22] argues that the digital revolution will create an equal partnership between patients and their healthcare providers. By being able to monitor their own health at home, patients will feel empowered to take responsibility and decision making around their health. Care models will need to change the focus from acute to preventative care and well-being, empower consumers and patients to manage their own health, move towards holistic and personalized medical care and broaden the definition of health to include mental and spiritual health [12].
The severity and impact of Covid 19 has been a catalyst to prompt governments and health care providers, to respond innovatively and there is now an opportunity for design to play its part in addressing some of these challenges [12]. Future care solutions will include telehealth, remote patient monitoring, and technology enabled ways of diagnosing, monitoring, and treating patients [31]. Consumers have increasingly been placed at the centre of healthcare decision making and expect on-demand, and connected clinician-patient interactions [4]. They are more informed and showing a greater interest in managing their own health and are driving the demand for innovation in health-related products, services, and tools to track their health [12].
These innovative design solutions create an opportunity for “connected health,” where individuals can collect data, remotely from a healthcare setting and then report this information to clinicians. The benefits are that the distributed gathering and monitoring of patient-generated health data (PGHD) can free up health care centres [20]. Wearable technologies such as heart rate sensors, exercise trackers and oximeters are also seeing a surge in growth. Wearable devices can provide up-to-date monitoring of high-risk patients preventing the occurrence of a major health event [29]. The wearable medical device market is expected to reach more than US$ 27 million by 2023, from just under US$ 8 million in 2017 [28]. New digital tools will continue to facilitate remote monitoring and adherence to medications allowing users to remain at home [5]. While most of these, measure vital signs, future avenues of development are in cognitive and mental health and ingestible sensors to communicate with other wearable devices to monitor the body’s internals [29].
The impact of Covid 19 has also accelerated how readily consumers have adapted to digital technologies [12]. Consumers are also engaging in virtual consultations and ordering prescriptions online. Virtual visits rose from 15% in 2019 to 28% in April 2020 [13]. Video calls, phone calls, texts, and emails became an essential component in care delivery due to the pandemic to enable clinicians and patients to stay connected. Similarly, telehealth, tele-pharmacy, and virtual-hospital-at-home programs are on the rise [21]. While virtual visits are desirable for consumers, when surveyed many found it limited the quality of the interaction with the clinician pointing to the need for training tools in building virtual relationships for clinicians [12].
The need for upskilling and training of health care staff is increasing to provide clinicians with the training tools to practice at the heights of their profession [12]. This means that along with the design of medical devices, designers may also be involved in the development and advancement of simulated systems and environments for training. The overall philosophy of simulation is to develop skills for professionals and increased patient safety. The human factors aspects and training needs required for the safe and effective use of medical devices can be elucidated within the simulation environment [25]. Moreover, simulation has the potential to recreate scenarios that are rarely experienced and test professionals in challenging situations. Where there is limited access to clinical settings or limited exposure to patients who are experiencing low-frequency and high-risk situations, students might not receive the experience necessary to become confident and competent [1]. Simulation also aims to reduce both lead times and costs in the production of existing medical devices [10].
Furthermore, augmented reality (AR) and Virtual Reality (VR) are being applied to personalize medicine and create behavioural change [12]. For example, VR technology is being used to treat pain, as well as conditions ranging from anxiety and post-traumatic stress disorder and stroke to the training of surgeons and other clinicians [28]. Possible future uses of VR and AR are in training tools for medical students, calming environments for patients and the application of gamification to support patients in rehabilitation [16]. Artificial intelligence (AI) has also radically transformed health care by personalising medicine. Robots to assist nurses such as ‘Moxi’, Chatbots and virtual health assistants are examples of AI-based technology. AI is also being applied in precision medicine, medical imaging, drug discovery, and genomics. For example, AI can analyse multiple pathology images of different cancers to provide an accurate diagnoses and specify the best anti-cancer drug combinations to create personalised care. The AI market for health care is expected to exceed US$34 billion by 2025 (https://www.businesswire.com/news/home/20180827005149/en/) (ibid).
3D printing has revolutionised advances in health care. Current uses, include patient-specific implants, cutting guides, prosthesis and anatomical models [9]. The advantages of 3D printing is that it allows for instant bespoke rapid fix solutions to clinical problems, such as [23] where 3D printing was used to create a bespoke repair of a Percutaneous Endoscopic Gastrostomy (PEG) tube in a patient unfit for surgical replacement. Other examples are one off braces or dental implants. 3D printed medical devices can now be built to the exact specifications of a patient and patient-specific dimensions have shown greater acceptance by the body, with increased comfort and performance outcomes [11]. The capabilities of 3D printing is likely to be increased and emerging areas are in drug manufacturing and stem cell development to create organic substances such as skin and organoids [29].
Point of care testing (POCT) and diagnostics is another emerging area. Traditional models involve the transfer of a sample for testing to a lab and waiting several days for results. POCT facilitates testing the patient at multiple locations with on the spot results. The technology leverages biosensors and labs-on a-chip to integrate multiple laboratory functions into a single compact circuit that can perform diagnostics on very small samples [29].
2 The Role of Design in the Future of Health Care
Whilst we are witnessing an increasing interest in the role of design, set within the context of health there is a long history of the utilisation of design in the development of medical devices. The global market for medical devices was US$425.5 Billion in 2018 and expected to rise to US$612.7 Billion by 2025 (Insights). In building on this role, clinicians are now calling for design to help with every aspect of the healthcare system from designing medical devices to tackling pandemics, the layout of operating theatres and medical charts [14]. Designers can provide essential skill sets to healthcare. Park [24] lists five unique skills that designers can bring to healthcare; (1) problem solving and the ability to deal with ambiguity to structure problems, (2) an ability to communicate which is essential to understand the needs of others and to communicate solutions, (3) empathy and the skills to step into the shoes of those who may be anxious or suffering from chronic illness, (4) an ability to co-create with users and stakeholders and know when and where to involve them in the process and (5) creativity in challenging conventional solutions with blue sky ideas. While design alone is not the solution to all of healthcare’s challenges, applying the methods of design can help make the delivery of healthcare more efficient and empathetic.
The shift in outlook towards viewing healthcare as a point of treatment for the physically unwell to the inclusion of the holistic wellbeing of the mind, body and spirit will demand a redesign of services that include the needs of consumers [12]. Fry [15] advocate that co-creation and multidisciplinary teams are essential in the redesign of healthcare services and that healthcare providers would benefit from using an iterative, user-centered and holistic approach that considers the patient experience. They state that a service design process through co-creation can challenge the hierarchy and silo-mentality that is ingrained in many healthcare organisations. This includes virtual visits, remote monitoring, prescription delivery, digital diagnostics and decision support [8].
Addressing some of the inequalities and inefficiencies of health care may also be achieved by questioning the norm of specific locations such as hospitals and GP clinics as entry points to health care. Opportunities exist for designers to consider alternative entry points. This may be achieved by targeting communities to address the drivers of health and connecting communities to a variety of health and educational services [5]. For example a more distributed healthcare service could include free-standing emergency care clinics [27].
While the future of Design within health care is promising, there are many challenges to implementing solutions. Bhavani et al. [6] state that there is a lack of evidence of whether many innovative solutions that have been implemented within healthcare actually improve outcomes and the quality of care. In response to this, the American College of Cardiology (ACC) convened a Healthcare Innovation Summit to understand the needs of various stakeholders across healthcare, including patient advocacy groups, clinicians, researchers, entrepreneurs, and industry groups. The outcome of the summit was a health policy statement that intends to guide healthcare policies, programs and innovations. The objectives are to promote patient-centric innovations that have measures and evidence of their impact on health, access, equity, costs, and outcomes (ibid). As part of a multidisciplinary team designers have a duty of care to ensure that solutions are serving the needs of the people they wish to address.
3 In This Special Issue
This special issue comprises three papers that address design for health and wellbeing. The first paper, ‘Pain[off]: using Design Probes to configure sensory conditions to reduce pain in hospitals’, describes how in healthcare, the contexts in which patients and caregivers find themselves in, is often complex regarding activities taking place, number and roles of people involved, number and types of objects in the environment, as well as in types of interactions. Gambera, Riccò and Duarte proposed to address a prevalent issue in these scenarios: body pain and ways to soothe it. Contrary to what is usually found in the literature on pain management, they did so through a designerly approach which embraced the challenge of considering synaesthesis rather than individual senses alone. The authors created a probe in the form of a room in which participants who were familiar with Design methods could manipulate a number of sensory stimuli until they reached the combination that felt the best to them in order to relieve pain. The authors discuss the challenges of this designerly approach, lessons learned and future work with users who are representative of a population affected by pain issues.
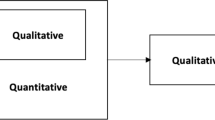
The second paper, ‘Co-designing resources for knowledge-based self-reflection for people living with Parkinson’s disease to better enable independent living’ explores the use of participatory design in the Co-designing of resources for knowledge-based self-reflection for people living with Parkinson’s disease to better enable independent living. Participatory designs are widely regarded as a positive way to develop and implement organizational interventions, as well as to develop products and solutions, entailing the engagement of different stakeholders and communication among them, in several activity sectors [2, 7, 26]. Healthcare is a complex and dynamic setting, where professionals and patients interact in different pathways, not always in a coordinated and complementary way. In participatory change processes, handling the interests of different stakeholders is one of the main challenges. Another one is being able to implement adequate tools regarding a holistic approach (Ibid). The paper presents an empirical study focused on Parkinson’s disease, using a participatory design approach. Based on the identification of the different stakeholders needs and the problems users faced in using the services, facilitating mutual learning between participants and generating solutions. The reflexive processes lead to the integration of solutions in a final outcome: the Home Based Care Pathway. The project outcome evidences the benefits of participatory design in healthcare. It contributes to empowering patients and understanding the patients' journey to understand their needs. Finally, it shows how participatory design enhances professionals and patients to address and solve common problems.
The third paper, ‘Neurosurgery Training Tool. Design as facilitator between disciplines for the improvement of medical devices’ describes a multidisciplinary research project concerned with the development of a prototype training system that simulates the spinal column. The iterative development of applied design research utilises state of the art 3D printing, moulding and casting processes to simulate different material qualities of human bone and tissue. The paper highlights the increasing logistical and ethical problem of using cadavers and body parts to support learning and training of surgical techniques and the increasing need and advantages of simulated approaches. The paper argues for Design to be placed at the centre of a multi-disciplinary research environment combining both medical and technological disciplines where the adoption of User/Human-Centred Design methods can be useful in integrating information from different disciplinary perspectives. The case study also demonstrates the value of Design in creating physical tools acting as a common language to aid communication between stakeholders involved and impacted by the research. With increasing intolerance of error and the ever-increasing cost of ‘medical procedures’ the creation of simulated systems for testing and training are likely to be an increasing focus of research.
References
Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, Macaulay C, Mancini ME, Morimoto T, Soper N (2010) Training and simulation for patient safety. BMJ Qual Saf 19:i34–i43
Ajslev JZ, Wåhlin-Jacobsen CD, Brandt M, Møller JL, Andersen LL (2020) Losing face from engagement–an overlooked risk in the implementation of participatory organisational health and safety initiatives in the construction industry. Constr Manag Econ 38:824–839
Bank W (2019) Current health expenditure. Available: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS
Barton JL, Kunneman M, Hargraves I, Leblanc A, Brito JP, Scholl I, Montori VM (2020) Envisioning shared decision making: a reflection for the next decade. SAGE Publications, Los Angeles, CA
Betts D, Korenda L, Giuliani S (2020) Are consumers already living the future of health? Key trends in agency, virtual health, remote monitoring, and data-sharing
Bhavnani SP, Parakh K, Atreja A, Druz R, Graham GN, Hayek SS, Krumholz HM, Maddox TM, Majmudar MD, Rumsfeld JS (2017) 2017 Roadmap for innovation—ACC health policy statement on healthcare transformation in the era of digital health, big data, and precision health: a report of the American College of Cardiology task force on health policy statements and systems of care. J Am Coll Cardiol 70:2696–2718
Burgess-Limerick R (2018) Participatory ergonomics: evidence and implementation lessons. Appl Ergon 68:289–293
Burill SB, Kroll D, Wheeler A, Sowar T, James (2020) Implications of the COVID-19 crisis for the health care ecosystem - gearing up for the next normal. Available: https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-implications-of-the-covid-19-crisis-for-the-health-care-ecosystem.pdf
Chae MP, Rozen WM, McMenamin PG, Findlay MW, Spychal RT, Hunter-Smith DJ (2015) Emerging applications of bedside 3D printing in plastic surgery. Front Surg 2:25
Ciurana J (2014) Designing, prototyping and manufacturing medical devices: an overview. Int J Comput Integr Manuf 27:901–918
Clinic C (2018) Cleveland clinic unveils top 10 medical innovations for 2019. Newsroom [Online]. Available: https://newsroom.clevelandclinic.org/2018/10/24/cleveland-clinic-unveils-top-10-medical-innovations-for-2019/
Deloitte (2021) Global health care outlook—accelerating industry change
Deloitte (2021) Global health care outlook laying a foundation for the future
Fairs M (2020). Lack of design input in healthcare is putting both patients and doctors at risk, says physician. Available: https://www.dezeen.com/2020/04/21/design-input-healthcare-risk/. Accessed 30 April 2020
Fry KR (2019) Why hospitals need service design. In: Service design and service thinking in healthcare and hospital management. Springer
Futurist TM (2020) 5 ways medical virtual reality is already changing healthcare. Available: https://medicalfuturist.com/5-ways-medical-vr-is-changing-healthcare/
Insights FB Medical device market size, share and industry analysis by type. Medical device/Medical device markets [Online]. Available: https://www.fortunebusinessinsights.com/industry-reports/medical-devices-market-100085. Accessed 18 April 2021
Jakovljevic M, Jakab M, Gerdtham U, McDaid D, Ogura S, Varavikova E, Merrick J, Adany R, Okunade A, Getzen TE (2019) Comparative financing analysis and political economy of noncommunicable diseases. J Med Econ 22:722–727
Jakovljevic M, Timofeyev Y, Ranabhat CL, Fernandes PO, Teixeira JP, Rancic N, Reshetnikov V (2020) Real GDP growth rates and healthcare spending–comparison between the G7 and the EM7 countries. Glob Health 16:1–13
Lavallee DC, Lee JR, Austin E, Bloch R, Lawrence SO, Mccall D, Munson SA, Nery-Hurwit MB Amtmann D (2020) mHealth and patient generated health data: stakeholder perspectives on opportunities and barriers for transforming healthcare. Mhealth 6
Mehendale RRJ (2020) Welcome to the virtual age: industrial 5.0 is changing the future of work. Deloitte Health Forward blog [Online]
Meskó B (2014) The guide to the future of medicine: technology and the human touch. Webicina Kft
O’Sullivan KJ, O’Sullivan AG, Power N, Gillick J, Dunne CP, O’Sullivan L, Linnane B (2018) Use of 3D printing to create a bespoke repair of a Percutaneous Endoscopic Gastrostomy (PEG) tube in patient unfit for surgical replacement. BMJ Innov 4:29–31
Park T (2020) Why healthcare needs designers. The health Care Blog [Online]. Available from: https://thehealthcareblog.com/blog/2020/01/28/why-healthcare-needs-designers/. Accessed 30 Mar 2021
Power D, O'Donovan K, Deasy C, Henn P (2020) Simulation test: can medical devices pass? BMJ Simul Technol Enhanced Learn 6
Punnett L, Nobrega S, Zhang Y, Rice S, Gore R, Kurowski A (2020) Safety and Health through Integrated, Facilitated Teams (SHIFT): stepped-wedge protocol for prospective, mixed-methods evaluation of the Healthy Workplace Participatory Program. BMC Public Health 20:1–14
Ratanjee V (2020) Five forces that will reshape the future of healthcare. Workplace [Online]
Reddy M (2021) Digital transformation in healthcare in 2021: 7 key trends. Available: https://www.digitalauthority.me/resources/state-of-digital-transformation-healthcare/
School of Business TGWU (2019) Which innovations are revolutionizing healthcare today? Online Healthcare MBA [Online]. Available from: https://healthcaremba.gwu.edu/blog/which-innovations-are-revolutionizing-healthcare-today/
Tavakoli M, Carriere J, Torabi A (2020) Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: An analysis of the state of the art and future vision. Adv Intell Syst 2:2000071
Taylor K, Bhatti S, Ferris K (2020) The future unmasked: Life sciences and health care predictions 2025
Taylor K, Properzi F, Bhatti S, Ferris K (2020) Digital transformation, shaping the future of European healthcare
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Kiernan, L., de Barros, A.C., Cotrim, T., Chamberlain, P. (2022). The Future of Design for Health and Wellbeing. In: Duarte, E., Rosa, C. (eds) Developments in Design Research and Practice. Senses 2019. Springer Series in Design and Innovation , vol 17. Springer, Cham. https://doi.org/10.1007/978-3-030-86596-2_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-86596-2_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-86595-5
Online ISBN: 978-3-030-86596-2
eBook Packages: EngineeringEngineering (R0)