Abstract
Acute lymphoblastic leukemia (ALL) in infants younger than 1 year of age is an aggressive, high-risk subtype of childhood ALL. Rearrangement of the KMT2A gene (KMT2A-r) on chromosome band 11q23 is a defining cytogenetic feature that occurs in approximately 80% of infants with ALL and is associated with poor prognosis for long-term remission and survival. Infant ALL with KMT2A-r is characteristically poorly responsive to chemotherapy and hematopoietic stem cell transplantation. New strategies, such as molecularly targeted therapies and immunotherapies, are in development and show promise in preclinical models and early phase studies. In this chapter, we discuss the unique biological features of ALL in infants, provide a historical overview of the clinical trials and outcomes for infants with ALL, and offer insight into the novel treatment approaches in development.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Infant acute lymphoblastic leukemia (ALL), defined as ALL diagnosed prior to the first birthday, is a rare, aggressive cancer with a poor prognosis. In the United States, the incidence of ALL in infants is 1.9 cases per 100,000 or about 80 to 100 infants diagnosed each year [1]. Infant ALL is slightly more common among females compared to males (F:M ratio 1.4:1), and approximately 20% of cases are diagnosed in the first 3 months of life [1,2,3,4]. Infant ALL is a high-risk subtype of childhood ALL, associated with an event-free survival (EFS) of 45% [2,3,4,5,6]. Whereas many subsets of children with ALL have seen improvements over time, overall survival for infants with ALL has remained poor (Fig. 6.1) [7]. Additional unfavorable prognostic features in infants include very young age (age less than 3 or 6 months at diagnosis has each been used in clinical trials to define higher-risk cohorts), hyperleukocytosis with white blood cell (WBC) count greater than 300,000/μL at diagnosis, poor response to prednisone during the first week of induction therapy, presence of KMT2A (formerly MLL) gene rearrangement (KMT2A-r), and persistence of minimal residual disease (MRD) in the bone marrow following induction chemotherapy [2,3,4,5,6, 8,9,10,11,12]. Of these factors, the principal defining biological feature is presence of KMT2A-r. The EFS of infants with KMT2A-r ALL is significantly inferior compared to infants without KMT2A-r (36–66% vs. 74–93%) [2,3,4,5,6, 13]. Treatments with very intensive chemotherapy, with or without allogeneic hematopoietic stem cell transplantation (HSCT), have been unsuccessful in improving the poor outcomes of infants with KMT2A-r ALL, and modern clinical trials are focused on delivering novel targeted therapies in an effort to improve outcome for these high-risk infants.
In this chapter, we examine the unique biological features of infant ALL that make it challenging to cure with current available therapies. We review the design and outcomes of prior clinical trials and discuss treatment strategies that are currently in development.
Biological Features
In the late 1980s/early 1990s, scientists identified abnormalities of chromosome band 11q23 as key recurring cytogenetic features in hematological malignancies, including ALL and acute myeloid leukemia (AML) [14]. Alterations of 11q23 were associated with secondary leukemias in patients whose previous therapy included topoisomerase II inhibitors, as well as in infants less than 1 year of age with acute leukemia [15, 16]. Chromosomal translocations at this locus were found to disrupt the human trithorax gene (HRX) and resulted in expression of a chimeric protein containing the DNA binding domain of HRX fused to various translocation protein partners [17]. A subsequent review of 96 infants with ALL treated on Pediatric Oncology Group (POG) protocols demonstrated that 81% had molecular evidence of a HRX (subsequently renamed MLL or KMT2A) rearrangement [18]. These cases were associated with younger age at diagnosis, higher WBC count at diagnosis, and poor prognosis.
Extensive characterization of infant ALL has demonstrated KMT2A-r as a clear oncogenic driver. While 94 distinct direct translocation partner genes have been identified, the vast majority of infant ALL cases are characterized by KMT2A-r involving the AFF1 (49%), MLLT1 (22%), MLLT3 (16%), and MLLT10 (6%) genes [19]. Most of these rearrangements occur between exon 9 and intron 11 in the major breakpoint cluster region of the KMT2A gene and result in a fusion transcript which encodes for the N-terminus of the MLL protein (MLL-N), fused in frame with its translocation partner. The MLL-N contains key functional domains including a domain for binding Menin, AT-hook motifs (DNA-binding domains), two speckled nuclear localization domains, and two repression domains [20]. The wild-type MLL protein is proteolytically cleaved into the N-terminal fragment and the C-terminal fragment, which then associate within a multiprotein complex that regulates chromatin modification and gene expression, specifically in genes involved in embryogenesis, hematopoiesis, and stem cell function [20].
Early studies exploring the mechanisms of leukemic transformation in infant ALL have postulated that the KMT2A translocation is the sentinel event in KMT2A-r infant leukemia and is sufficient to act as the sole driver for leukemic transformation. KMT2A-r infant ALL has a nearly 100% concordance rate in monozygotic twins with evidence of a shared molecularly identical clone confirming an in utero origin [21]. The short latency of KMT2A-r leukemia, occurring within the first year of life for infants and within 2 years for those that develop therapy-related secondary KMT2A-r leukemia , also suggests the translocation event may be sufficient for leukemic transformation. Our understanding of the molecular drivers of leukemogenesis has been advanced by recent insights revealed through the application of next-generation sequencing. Infant ALL with KMT2A-r is notable for an extremely low frequency of somatic mutations (1.3 non-silent mutations per case in the dominant clone) [22,23,24]. The most frequent co-occurring mutations can be found within the tyrosine kinase-PI3K-RAS signaling pathways [22, 24]. RAS family mutations are often subclonal and demonstrate a heterogeneous pattern of clonal evolution [25]. RAS pathway mutations have been associated with a high WBC at diagnosis and glucocorticoid resistance and confer a proliferative advantage [25]. Additionally, while activating mutations in FLT3 are not commonly seen, expression profiling has demonstrated significant upregulation of FLT3 gene expression in KMT2A-r infant ALL, with high-level gene expression of the wild-type protein associated with phosphorylation and activation of the protein [20]. Furthermore, abnormal DNA methylation is a striking feature of infant ALL blasts with KMT2A-r and provides a potential target for epigenetic therapies [26,27,28,29,30].
Leukemias with KMT2A-r are notable for their high-level expression of HOX cluster genes and the HOX cofactor MEIS1 [31, 32]. These genes are normally expressed in hematopoietic stem cells and progenitors, with decreasing expression as cells differentiate [33]. Recruitment of the MLL fusion protein (MLL-FP) to loci of target genes is facilitated by the interaction with the polymerase-associated factor complex (PAFc) and the trimolecular complex comprising MLL, Menin, and the chromatin-binding protein lens epithelium-derived growth factor (LEDGF), which have been found to be critical for MLL-FP-mediated leukemic transformation [34]. The MLL-FP recruits components of the super elongation complex (SEC), which includes MLL fusion partners (AFF1, AFF4, AF9, and ENL); the elongation factors ELL2, ELL3, EAF1, and EAF2; and the positive transcription elongation factor b (P-TEFb), which promotes transcriptional elongation through phosphorylation of RNA polymerase II. The AF9 and ENL fusion partners also form components of the DotCom complex, which includes AF10 and AF17, and the H3K79 methyltransferase, DOT1L. Recruitment of DOT1L to target genes by corresponding MLL-FPs can further promote transcriptional activation, with increased levels of H3K79 methylation found at MLL-FP targeted genomic loci such as HOXA9 and MEIS1 (Fig. 6.2) [35, 36]. Importantly, constitutive expression of HOXA9 ex vivo results in immortalization of hematopoietic progenitors [37]. Similarly, constitutive activation leads to stem cell-like properties found in KMT2A-r leukemias and is required for their survival.
MLL complex proteins during normal and malignant hematopoiesis. MLL interacts with a variety of protein complexes in hematopoietic stem and progenitor cells to promote transcription of critical target genes like HOXA9 and MEIS1. The PAF complex (PAFc) associates with RNA polymerase II (Pol II) and recruits the RAD6/BRE1 E2/E3 ubiquitin ligase, which promotes mono-ubiquitination of histone H2B (Ub). H2B mono-ubiquitination is a histone mark associated with transcriptional activation. PAFc, along with Menin/LEDGF, recruits the MLL complex to target genes which delivers H3K4 (Me) methyltransferase activity and promotes gene transcription. MLL associates with the HAT MOF, which promotes further gene transcription through histone H4K16 acetylation (Ac). During hematopoietic differentiation, MLL is not recruited to target genes in part due to decreased transcription of PAFc. Insufficient recruitment of MLL leads to decreased expression of target genes. Chromosomal translocations involving KMT2A (MLL) generate MLL fusion proteins that can recruit transcriptional activation complexes dependent on the fusion partner. These complexes involve the recruitment of pTEFb, which is required to phosphorylate the RNA Pol II C-terminal domain, which promotes transcriptional elongation. The H3K79 methyltransferase DOT1l is also recruited to some MLL fusion proteins, which can further promote transcriptional activation. (Image and edited caption reprinted with permission [36])
Given the relatively simple genetic background of KMT2A-r leukemia, it has been an attractive model to explore mechanisms of leukemogenesis. Mouse models have demonstrated that differences in KMT2A fusion partner, cell of origin, timing of expression, and the microenvironment can influence the resulting immunophenotype (B-ALL, AML, T-ALL, or mixed phenotype acute leukemia) and latency of leukemia development [38]. Early models of KMT2A-MLLT3-driven leukemia demonstrated a strong bias toward myeloid disease. In these models, expression of the fusion transcript in primitive long-term hematopoietic stem cells resulted in shorter latency and more resistance to chemotherapy than those derived from differentiated granulocyte-macrophage progenitors [39]. This suggests that the chemotherapy-resistant disease seen in infant ALL may be related to a more primitive cell of origin. Subsequent studies expressing the KMT2A-MLLT3 fusion in fetal liver cells revealed the potential for lymphoid leukemia, and newer models using genetic engineering to express the KMT2A-MLLT3 or KMT2A-MLLT1 oncogenes from the endogenous KMT2A locus in cord blood-derived CD34+ cells led to ALL, AML, and mixed lineage leukemias (KMT2A-MLLT3) and ALL (KMT2A-MLLT1) in xenografts, demonstrating the potential plasticity of these leukemias based on cell of origin and the microenvironment [40, 41]. While KMT2A-AFF1-driven leukemia models have proven more challenging to develop, a recent model using a human/murine cDNA hybrid fusion transcript for KMT2A-Aff1 resulted in a pro-B ALL that more accurately recapitulates the immunophenotype and molecular features of human KMT2A-AFF1 ALL [42]. Additionally, a recently identified CD10-negative Pre-Pro-B-cell progenitor found in fetal liver and fetal bone marrow may serve as a potential cell of origin and provide additional insight into the unique biology found in infant leukemia [43].
Treatment
Treatment for infants with ALL has evolved significantly over time [44]. Infants were initially treated by individual study groups on childhood ALL protocols. The unfavorable prognosis carried by infants diagnosed at less than 1 year of age led to risk adaptation within childhood ALL studies, with stratification of infants to high-risk regimens. Combined analysis of infants enrolled on successive childhood ALL protocols led to the identification of several independent risk factors associated with an inferior outcome, including presence of KMT2A-r, hyperleukocytosis at presentation, absence of CD10 antigen, age less than 6 months at diagnosis, and poor response to initial prednisone therapy [9, 45, 46]. Outcomes of infants treated on childhood ALL protocols remained poor, and the number of infants recruited by each individual study group was limited. This limitation was pivotal in stimulating the development of infant-specific ALL protocols facilitated by collaboration of study groups. The outcomes for infant-specific ALL studies are summarized in Table 6.1.
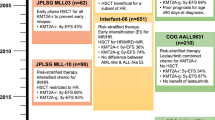
The first US-based infant-specific ALL trials were conducted by the Children’s Cancer Group (CCG-107 and CCG-1883) and the Pediatric Oncology Group (POG 8493 and POG 9107). Compared to infants treated on childhood ALL protocols, these studies introduced the concept of delivering intensified therapy to infants, demonstrating a progressive, modest improvement in survival; however outcomes remained poor with marrow relapse being the primary cause of treatment failure [12, 47, 48]. The CCG studies successfully replaced cranial radiotherapy with intrathecal and high-dose systemic therapy as an effective strategy for central nervous system (CNS) prophylaxis, whereas the POG studies were able to demonstrate low rates of isolated CNS relapse with triple intrathecal therapy. The subsequent parallel POG 9407 (cohorts 1 and 2) and CCG-1953 protocols implemented further early treatment intensification, which led to a reduction in relapse rate; however this was countered by excessive treatment-related morbidity and mortality [48,49,50,51]. When CCG and POG merged to form the Children’s Oncology Group (COG), amendments were made to P9407, and cohort 3 received a short infusion of daunorubicin rather than continuous infusion and prednisone rather than dexamethasone [51]. Despite a reduction in the rate of early deaths compared to preceding cohorts, cohort 3 experienced a high rate of relapse, resulting in relatively unchanged outcomes. Independent factors associated with an inferior outcome included age ≤90 days at diagnosis, hyperleukocytosis at presentation, and presence of KMT2A-r [4]. The successor COG study, AALL0631, also required an initial amendment to reduce the intensity of induction therapy due to excessive toxicity [52]. COG AALL0631 was pivotal in being the first study to demonstrate the safety and feasibility of adding a novel targeted therapy to post-induction chemotherapy for infants with KMT2A-r ALL. Although addition of the FLT3 inhibitor, lestaurtinib, did not improve overall outcomes, benefit was shown for a subset of patients who achieved potent pharmacodynamic inhibition of FLT3 and whose leukemia cells were sensitive to ex vivo FLT3 inhibition, highlighting the need for identification and selection of infants with ALL that may be sensitive to novel agents in future studies [5, 53]. This study also demonstrated that flow cytometry-based MRD, detected at a level of ≥0.01% in the bone marrow, is a powerful predictor of EFS for infants with KMT2A-r ALL [8]. The COG AALL15P1 pilot study has recently completed accrual and aims to test the tolerability and biologic activity of adding 5-day cycles of azacitidine, a demethylating agent, prior to each block of chemotherapy following induction (NCT02828358). St Jude Children’s Research Hospital is also conducting a pilot trial, testing the safety of bortezomib, a proteasome inhibitor, and vorinostat, a histone deacetylase inhibitor, on a chemotherapy backbone (NCT02553460).
The first infant-specific studies conducted by the United Kingdom Childhood Leukemia Working Party, Infant 87 and Infant 92, drew similar conclusions to the early CCG and POG studies, identifying significant treatment-related toxicity and high relapse rates despite delivering increased therapeutic intensity [54, 55]. The Interfant Study Group subsequently formed in 1999 and currently comprises of over 20 international and national study groups. The first trial of the Interfant Study Group, Interfant-99, employed a hybrid treatment schedule, composed of elements used in the treatment of both ALL and AML. No additional benefit was seen for infants who were randomized to a late intensification course [3]. This study was notably the first in infants to identify the prognostic impact of detectable MRD in the bone marrow following induction and consolidation [11]. A significantly higher relapse rate was identified for congenital ALL, defined as diagnosis in the first month of life [10]. The outcome for infants who relapsed on Interfant-99 was dismal with 3-year overall survival of 20.9% for all patients and 24.9% for those treated with curative intent [56]. The subsequent study, Interfant-06, showed no benefit of early post-induction intensification with myeloid compared to lymphoid-based chemotherapy for KMT2A-r infant ALL and no improvement in overall outcome compared to Interfant-99 [2]. Both studies affirmed the presence of KMT2A-r, age less than 6 months at diagnosis, and poor response to initial prednisone therapy as independent adverse prognostic factors for outcome, with hyperleukocytosis at presentation also identified as an adverse prognostic factor on Interfant-06 [2, 3]. The Interfant Study Group has recently completed accrual for a pilot study testing the feasibility, safety, and efficacy of adding one post-induction course of the monoclonal antibody blinatumomab, a bi-specific T-cell engager, to the standard Interfant-06 chemotherapy backbone for infants with KMT2A-r ALL (EudraCT 2016-004674-17).
In Japan, allogeneic HSCT has historically been the standard approach for treating infants with KMT2A-r ALL. Two consecutive protocols, MLL96 and MLL98, scheduled HSCT following induction and three courses of post-remission intensification. These studies identified a high proportion of relapses between first complete remission and HSCT, indicating the need for more effective post-remission therapy [57]. Infants with relapsed/refractory disease fared poorly with 5-year overall survival of 25.6%, with failure to achieve remission after salvage therapy independently identified as a poor prognostic factor [58]. The MLL03 study conducted by the Japanese Pediatric Leukemia/Lymphoma Study Group (JPLSG) built on findings of the preceding studies with the aim of early phase HSCT, within 4 months of initial induction. Although this strategy was able to effectively prevent early relapse and enabled patients to receive HSCT, there was a low overall complete remission rate and a substantial number of infants relapsed following HSCT, highlighting the limited efficacy of HSCT for treatment of infants with KMT2A-r ALL [6]. As such, the subsequent JPLSG MLL-10 study risk stratified infants to spare HSCT in non-high-risk patients and introduced early intensification of therapy with the inclusion of high-dose cytarabine within an early consolidation phase following induction, leading to significantly improved outcomes. Clearance of MRD at the end of the early consolidation phase was confirmed as an independent prognostic factor for favorable outcome [13].
The indications for use of allogeneic HSCT for treatment of infants with ALL remain unresolved. Findings are limited by the absence of a randomized study comparing HSCT to chemotherapy alone, and analysis of prior studies is subject to selection bias of higher-risk infants for HSCT. All study groups have demonstrated that infants without KMT2A-r have acceptable outcomes using an intensive chemotherapy approach without requiring HSCT [2,3,4, 13, 49, 57]. For KMT2A-r infants, the COG demonstrated no difference in outcome between those that received HSCT compared to those that received chemotherapy alone [59]. The Interfant-99 study was able to demonstrate benefit for HSCT; however this was restricted to a high-risk subgroup of KMT2A-r infants who were less than 6 months of age at diagnosis and either had a poor prednisone response or hyperleukocytosis at diagnosis [60]. The JPLSG MLL-10 study achieved good outcomes by limiting HSCT to high-risk KMT2A-r infants who were less than 6 months of age at diagnosis or had CNS involvement [13]. Given these findings, HSCT is reserved for a high-risk subset of infants with KMT2A-r ALL on Interfant and JPLSG studies and is omitted from COG protocols. Given the emergence of novel therapies and increasing recognition of late effects in survivors of infant leukemia following HSCT, this treatment modality is likely to be utilized even less frequently in the future [57, 61].
Future Directions
Novel strategies are desperately needed for the treatment of infant ALL with KMT2A-r. Preclinical models have generated evidence for several potential drug targets, including inhibition of DOT1L, FLT3, DNA methyltransferase, histone deacetylase, BCL-2, and the Menin-MLL interaction. Molecularly targeted therapy with DOT1L inhibition did not produce the desired results in a clinical trial of relapsed KMT2A-r leukemia in adults, but different DOT1L inhibitors remain under investigation in preclinical studies [62, 63]. As discussed, FLT3 inhibition may have failed to improve overall outcomes in COG AALL0631, but could be beneficial for a select cohort of infants with KMT2A-r ALL whose leukemic blasts display in vitro sensitivity to FLT3 inhibition [5, 53]. A small molecule inhibitor of the Menin-MLL interaction has entered a first-in-human trial (NCT04065399) after showing marked activity in KMT2A-r preclinical models, including infant ALL, and may be feasible to investigate in infants in the near future [64]. Currently, the COG is developing a phase 2 trial of venetoclax, a BCL-2 inhibitor, in combination with chemotherapy for the treatment of infants with KMT2A-r ALL. BCL-2 inhibition has shown activity against KMT2A-r ALL in preclinical models, and venetoclax has been identified as a promising therapeutic agent for KMT2A-r infant ALL [65,66,67].
Immunotherapy is likely to form an important component of future clinical trials for infant ALL. Immunotherapy has led to remarkable improvements in outcomes in the treatment of relapsed childhood ALL, but its applicability to infant ALL remains unclear [68,69,70,71]. Chimeric antigen receptor T-cell (CAR T-cell) therapy, either autologous or off-the-shelf, is available to infants at relapse in some countries, although the efficacy of CAR T-cell therapy in infants is not yet known [72, 73]. CAR T-cell therapy is an attractive alternative to upfront chemotherapy for infants with ALL, but is not without potential challenges. These challenges may include inability to harvest sufficient T-cells, exhaustion of T-cells following chemotherapy, and the potential for lineage switch to myeloid leukemia at relapse [74]. The results of early CAR T-cell studies in infants with relapsed or refractory ALL and the results of the Interfant Study Group’s pilot blinatumomab trial in upfront therapy will be very informative to the development of future treatment approaches. Further investigation of anti-CD22 therapy with inotuzumab ozogamicin may also be warranted, following promising findings from a retrospective study in a small cohort of infants and young children with relapsed or refractory ALL [75].
Conclusion
Infant ALL remains a high-risk subtype of childhood ALL, with no major advances in therapy nor improvements in outcome over several decades. This can be attributed, at least in part, to the characteristic chemotherapy refractory nature of KMT2A-r infant ALL. A number of novel treatment strategies have shown strong preclinical evidence of efficacy. Any therapy that successfully targets KMT2A-r has the potential to result in a major breakthrough for this disease. The international infant ALL research community is actively collaborating to discover molecular targets, test agents in preclinical models, and implement clinical trials, with the primary aim to prioritize improvements in outcome for infants with ALL.
References
Howlander N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al., editors. SEER Cancer Statistics Review, 1975–2016. Bethesda: National Cancer Institute. https://seer.cancer.gov/csr/1975_2016 based on November 2018 SEER data submission, posted to the SEER web site, April 2019.
Pieters R, De Lorenzo P, Ancliffe P, Aversa LA, Brethon B, Biondi A, et al. Outcome of infants younger than 1 year with acute lymphoblastic leukemia treated with the Interfant-06 protocol: results from an international phase III randomized study. J Clin Oncol. 2019;37(25):2246–56.
Pieters R, Schrappe M, De Lorenzo P, Hann I, De Rossi G, Felice M, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet. 2007;370(9583):240–50.
Dreyer ZE, Hilden JM, Jones TL, Devidas M, Winick NJ, Willman CL, et al. Intensified chemotherapy without SCT in infant ALL: results from COG P9407 (cohort 3). Pediatr Blood Cancer. 2015;62(3):419–26.
Brown P, Kairalla J, Wang C, Dreyer Z, Salzer W, Sorenson M, et al. Addition of FLT3 inhibitor lestaurtinib to post-induction chemotherapy does not improve outcomes in MLL-rearranged infant acute lymphoblastic leukemia (ALL): AALL0631, a Children’s Oncology Group study. Pediatr Blood Cancer. 2016;63(S3):S5–S321.
Koh K, Tomizawa D, Moriya Saito A, Watanabe T, Miyamura T, Hirayama M, et al. Early use of allogeneic hematopoietic stem cell transplantation for infants with MLL gene-rearrangement-positive acute lymphoblastic leukemia. Leukemia. 2015;29(2):290–6.
Raetz E, Lu X, Devidas M, Loh M, Winick N, Carroll W, et al. Continued improvements in overall survival (OS) in children with newly diagnosed acute lymphoblastic leukemia (ALL): a Children’s Oncology Group (COG) report. Pediatr Blood Cancer. 2018;65(S1):e27057.
Brown P, Kairalla J, Hilden J, Dreyer Z, Carroll A, Heerema NA, et al. Minimal residual disease (MRD) predicts outcomes in KMT2A-rearranged but not KMT2A-wild type infant acute lymphoblastic leukemia (ALL): AALL0631, a Children’s Oncology Group study. Pediatr Blood Cancer. 2019;66(S4):e27989.
Dordelmann M, Reiter A, Borkhardt A, Ludwig WD, Gotz N, Viehmann S, et al. Prednisone response is the strongest predictor of treatment outcome in infant acute lymphoblastic leukemia. Blood. 1999;94(4):1209–17.
van der Linden MH, Valsecchi MG, De Lorenzo P, Moricke A, Janka G, Leblanc TM, et al. Outcome of congenital acute lymphoblastic leukemia treated on the Interfant-99 protocol. Blood. 2009;114(18):3764–8.
Van der Velden VH, Corral L, Valsecchi MG, Jansen MW, De Lorenzo P, Cazzaniga G, et al. Prognostic significance of minimal residual disease in infants with acute lymphoblastic leukemia treated within the Interfant-99 protocol. Leukemia. 2009;23(6):1073–9.
Reaman GH, Sposto R, Sensel MG, Lange BJ, Feusner JH, Heerema NA, et al. Treatment outcome and prognostic factors for infants with acute lymphoblastic leukemia treated on two consecutive trials of the Children’s Cancer Group. J Clin Oncol. 1999;17(2):445–55.
Tomizawa D, Miyamura T, Imamura T, Watanabe T, Moriya Saito A, Ogawa A, et al. A risk-stratified therapy for infants with acute lymphoblastic leukemia: a report from the JPLSG MLL-10 trial. Blood. 2020;136(16):1813–23.
Heim S, Mitelman F. Cancer Cytogenetics. Alan R Liss; New York 1987.
Kaneko Y, Shikano T, Maseki N, Sakurai M, Sakurai M, Takeda T, et al. Clinical characteristics of infant acute leukemia with or without 11q23 translocations. Leukemia. 1988;2(10):672–6.
Pui CH, Ribeiro RC, Hancock ML, Rivera GK, Evans WE, Raimondi SC, et al. Acute myeloid leukemia in children treated with epipodophyllotoxins for acute lymphoblastic leukemia. N Engl J Med. 1991;325(24):1682–7.
Tkachuk DC, Kohler S, Cleary ML. Involvement of a homolog of Drosophila trithorax by 11q23 chromosomal translocations in acute leukemias. Cell. 1992;71(4):691–700.
Rubnitz JE, Link MP, Shuster JJ, Carroll AJ, Hakami N, Frankel LS, et al. Frequency and prognostic significance of HRX rearrangements in infant acute lymphoblastic leukemia: a Pediatric Oncology Group study. Blood. 1994;84(2):570–3.
Meyer C, Burmeister T, Groger D, Tsaur G, Fechina L, Renneville A, et al. The MLL recombinome of acute leukemias in 2017. Leukemia. 2018;32(2):273–84.
Winters AC, Bernt KM. MLL-rearranged leukemias - an update on science and clinical approaches. Front Pediatr. 2017;5:4.
Greaves MF, Maia AT, Wiemels JL, Ford AM. Leukemia in twins: lessons in natural history. Blood. 2003;102(7):2321–33.
Andersson AK, Ma J, Wang J, Chen X, Gedman AL, Dang J, et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat Genet. 2015;47(4):330–7.
Kostadinov R, Farooqi M, Yoo B, Farrow E, Kelley S, Gibson M, et al. Landscape of somatic mutations and gene expression changes in relapsed infant MLL-rearranged acute lymphoblastic leukemia. Blood. 2016;128(22):1735.
Agraz-Doblas A, Bueno C, Bashford-Rogers R, Roy A, Schneider P, Bardini M, et al. Unraveling the cellular origin and clinical prognostic markers of infant B-cell acute lymphoblastic leukemia using genome-wide analysis. Haematologica. 2019;104(6):1176–88.
Mansur MB, Ford AM, Emerenciano M. The role of RAS mutations in MLL-rearranged leukaemia: a path to intervention? Biochim Biophys Acta Rev Cancer. 2017;1868(2):521–6.
Schafer E, Irizarry R, Negi S, McIntyre E, Small D, Figueroa ME, et al. Promoter hypermethylation in MLL-r infant acute lymphoblastic leukemia: biology and therapeutic targeting. Blood. 2010;115(23):4798–809.
Stumpel DJ, Schneider P, van Roon EH, Boer JM, de Lorenzo P, Valsecchi MG, et al. Specific promoter methylation identifies different subgroups of MLL-rearranged infant acute lymphoblastic leukemia, influences clinical outcome, and provides therapeutic options. Blood. 2009;114(27):5490–8.
Stumpel DJ, Schneider P, van Roon EH, Pieters R, Stam RW. Absence of global hypomethylation in promoter hypermethylated Mixed Lineage Leukaemia-rearranged infant acute lymphoblastic leukaemia. Eur J Cancer. 2013;49(1):175–84.
Stumpel DJ, Schotte D, Lange-Turenhout EA, Schneider P, Seslija L, de Menezes RX, et al. Hypermethylation of specific microRNA genes in MLL-rearranged infant acute lymphoblastic leukemia: major matters at a micro scale. Leukemia. 2011;25(3):429–39.
Bergmann AK, Castellano G, Alten J, Ammerpohl O, Kolarova J, Nordlund J, et al. DNA methylation profiling of pediatric B-cell lymphoblastic leukemia with KMT2A rearrangement identifies hypomethylation at enhancer sites. Pediatr Blood Cancer. 2017;64(3):e26251.
Yokoyama A. Transcriptional activation by MLL fusion proteins in leukemogenesis. Exp Hematol. 2017;46:21–30.
Armstrong SA, Golub TR, Korsmeyer SJ. MLL-rearranged leukemias: insights from gene expression profiling. Semin Hematol. 2003;40(4):268–73.
Collins CT, Hess JL. Deregulation of the HOXA9/MEIS1 axis in acute leukemia. Curr Opin Hematol. 2016;23(4):354–61.
Chan AKN, Chen CW. Rewiring the epigenetic networks in MLL-rearranged leukemias: epigenetic dysregulation and pharmacological interventions. Front Cell Dev Biol. 2019;7:81.
Ballabio E, Milne TA. Epigenetic control of gene expression in leukemogenesis: cooperation between wild type MLL and MLL fusion proteins. Mol Cell Oncol. 2014;1(2):e955330.
Muntean AG, Hess JL. The pathogenesis of mixed lineage leukemia. Annu Rev Pathol. 2012;7:283–301.
Schnabel CA, Jacobs Y, Cleary ML. HoxA9-mediated immortalization of myeloid progenitors requires functional interactions with TALE cofactors Pbx and Meis. Oncogene. 2000;19(5):608–16.
Milne TA. Mouse models of MLL leukemia: recapitulating the human disease. Blood. 2017;129(16):2217–23.
Stavropoulou V, Kaspar S, Brault L, Sanders MA, Juge S, Morettini S, et al. MLL-AF9 expression in hematopoietic stem cells drives a highly invasive AML expressing EMT-related genes linked to poor outcome. Cancer Cell. 2016;30(1):43–58.
Chen W, O’Sullivan MG, Hudson W, Kersey J. Modeling human infant MLL leukemia in mice: leukemia from fetal liver differs from that originating in postnatal marrow. Blood. 2011;117(12):3474–5.
Buechele C, Breese EH, Schneidawind D, Lin CH, Jeong J, Duque-Afonso J, et al. MLL leukemia induction by genome editing of human CD34+ hematopoietic cells. Blood. 2015;126(14):1683–94.
Lin S, Luo RT, Ptasinska A, Kerry J, Assi SA, Wunderlich M, et al. Instructive role of MLL-fusion proteins revealed by a model of t(4;11) pro-B acute lymphoblastic leukemia. Cancer Cell. 2016;30(5):737–49.
O’Byrne S, Elliott N, Rice S, Buck G, Fordham N, Garnett C, et al. Discovery of a CD10-negative B-progenitor in human fetal life identifies unique ontogeny-related developmental programs. Blood. 2019;134(13):1059–71.
Kotecha RS, Gottardo NG, Kees UR, Cole CH. The evolution of clinical trials for infant acute lymphoblastic leukemia. Blood Cancer J. 2014;4:e200.
Pui CH, Behm FG, Downing JR, Hancock ML, Shurtleff SA, Ribeiro RC, et al. 11q23/MLL rearrangement confers a poor prognosis in infants with acute lymphoblastic leukemia. J Clin Oncol. 1994;12(5):909–15.
Silverman LB, McLean TW, Gelber RD, Donnelly MJ, Gilliland DG, Tarbell NJ, et al. Intensified therapy for infants with acute lymphoblastic leukemia: results from the Dana-Farber Cancer Institute Consortium. Cancer. 1997;80(12):2285–95.
Salzer WL, Devidas M, Carroll WL, Winick N, Pullen J, Hunger SP, et al. Long-term results of the Pediatric Oncology Group studies for childhood acute lymphoblastic leukemia 1984-2001: a report from the Children’s Oncology Group. Leukemia. 2010;24(2):355–70.
Gaynon PS, Angiolillo AL, Carroll WL, Nachman JB, Trigg ME, Sather HN, et al. Long-term results of the Children’s Cancer Group studies for childhood acute lymphoblastic leukemia 1983-2002: a Children’s Oncology Group Report. Leukemia. 2010;24(2):285–97.
Hilden JM, Dinndorf PA, Meerbaum SO, Sather H, Villaluna D, Heerema NA, et al. Analysis of prognostic factors of acute lymphoblastic leukemia in infants: report on CCG 1953 from the Children’s Oncology Group. Blood. 2006;108(2):441–51.
Salzer W, Dinndorf P, Dreyer Z, Hilden J, Reaman GH. Analysis of infectious complications in infants with acute lymphoblastic leukemia treated on the Children’s Cancer Group protocol 1953: a report from the Children’s Oncology Group. J Pediatr Hematol Oncol. 2009;31(6):398–405.
Salzer WL, Jones TL, Devidas M, Hilden JM, Winick N, Hunger S, et al. Modifications to induction therapy decrease risk of early death in infants with acute lymphoblastic leukemia treated on Children’s Oncology Group P9407. Pediatr Blood Cancer. 2012;59(5):834–9.
Salzer WL, Jones TL, Devidas M, Dreyer ZE, Gore L, Winick NJ, et al. Decreased induction morbidity and mortality following modification to induction therapy in infants with acute lymphoblastic leukemia enrolled on AALL0631: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2015;62(3):414–8.
Brown PA, Kairalla J, Hilden JM, Dreyer ZE, Carroll AJ, Heerema NA, et al. FLT3 inhibitor correlative laboratory assays impact outcomes in KMT2A-rearranged infant acute lymphoblastic leukemia (ALL) patients treated with lestaurtinib: AALL0631, a Children’s Oncology Group study. Blood. 2019;134(Supplement_1):1293.
Chessells JM, Eden OB, Bailey CC, Lilleyman JS, Richards SM. Acute lymphoblastic leukaemia in infancy: experience in MRC UKALL trials. Report from the Medical Research Council Working Party on Childhood Leukaemia. Leukemia. 1994;8(8):1275–9.
Chessells JM, Harrison CJ, Watson SL, Vora AJ, Richards SM, Medical Research Council Working Party on Childhood Leukaemia. Treatment of infants with lymphoblastic leukaemia: results of the UK Infant Protocols 1987-1999. Br J Haematol. 2002;117(2):306–14.
Driessen EM, de Lorenzo P, Campbell M, Felice M, Ferster A, Hann I, et al. Outcome of relapsed infant acute lymphoblastic leukemia treated on the Interfant-99 protocol. Leukemia. 2016;30(5):1184–7.
Tomizawa D, Koh K, Sato T, Kinukawa N, Morimoto A, Isoyama K, et al. Outcome of risk-based therapy for infant acute lymphoblastic leukemia with or without an MLL gene rearrangement, with emphasis on late effects: a final report of two consecutive studies, MLL96 and MLL98, of the Japan Infant Leukemia Study Group. Leukemia. 2007;21(11):2258–63.
Tomizawa D, Koh K, Hirayama M, Miyamura T, Hatanaka M, Saikawa Y, et al. Outcome of recurrent or refractory acute lymphoblastic leukemia in infants with MLL gene rearrangements: a report from the Japan Infant Leukemia Study Group. Pediatr Blood Cancer. 2009;52(7):808–13.
Dreyer ZE, Dinndorf PA, Camitta B, Sather H, La MK, Devidas M, et al. Analysis of the role of hematopoietic stem-cell transplantation in infants with acute lymphoblastic leukemia in first remission and MLL gene rearrangements: a report from the Children’s Oncology Group. J Clin Oncol. 2011;29(2):214–22.
Mann G, Attarbaschi A, Schrappe M, De Lorenzo P, Peters C, Hann I, et al. Improved outcome with hematopoietic stem cell transplantation in a poor prognostic subgroup of infants with mixed-lineage-leukemia (MLL)-rearranged acute lymphoblastic leukemia: results from the Interfant-99 study. Blood. 2010;116(15):2644–50.
Aoki Y, Hayakawa A, Koike K, Tauchi H, Ishii E, Koh K, et al. Late effects in survivors of infant acute lymphoblastic leukemia from the 3 consecutive Japanese nationwide clinical trials. Blood. 2019;134(Supplement_1):4559.
Daigle SR, Olhava EJ, Therkelsen CA, Basavapathruni A, Jin L, Boriack-Sjodin PA, et al. Potent inhibition of DOT1L as treatment of MLL-fusion leukemia. Blood. 2013;122(6):1017–25.
Stein EM, Garcia-Manero G, Rizzieri DA, Tibes R, Berdeja JG, Savona MR, et al. The DOT1L inhibitor pinometostat reduces H3K79 methylation and has modest clinical activity in adult acute leukemia. Blood. 2018;131(24):2661–9.
Krivtsov AV, Evans K, Gadrey JY, Eschle BK, Hatton C, Uckelmann HJ, et al. A Menin-MLL inhibitor induces specific chromatin changes and eradicates disease in models of MLL-rearranged leukemia. Cancer Cell. 2019;36(6):660–73.e11.
Urtishak KA, Edwards AY, Wang LS, Hudome A, Robinson BW, Barrett JS, et al. Potent obatoclax cytotoxicity and activation of triple death mode killing across infant acute lymphoblastic leukemia. Blood. 2013;121(14):2689–703.
Suryani S, Carol H, Chonghaile TN, Frismantas V, Sarmah C, High L, et al. Cell and molecular determinants of in vivo efficacy of the BH3 mimetic ABT-263 against pediatric acute lymphoblastic leukemia xenografts. Clin Cancer Res. 2014;20(17):4520–31.
Khaw SL, Suryani S, Evans K, Richmond J, Robbins A, Kurmasheva RT, et al. Venetoclax responses of pediatric ALL xenografts reveal sensitivity of MLL-rearranged leukemia. Blood. 2016;128(10):1382–95.
Locatelli F, Zugmaier G, Rizzari C, Morris JD, Gruhn B, Klingebiel T, et al. Effect of blinatumomab vs chemotherapy on event-free survival among children with high-risk first relapse B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(9):843–54.
Brown PA, Ji L, Xu X, Devidas M, Hogan LE, Borowitz MJ, et al. Effect of postreinduction therapy consolidation with blinatumomab vs chemotherapy on disease-free survival in children, adolescents and young adults with first relapse of B-cell acute lymphoblastic leukemia: a randomized clinical trial. JAMA. 2021;325(9):833–42.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439–48.
Clesham K, Rao V, Bartram J, Ancliff P, Ghorashian S, O’Connor D, et al. Blinatumomab for infant acute lymphoblastic leukemia. Blood. 2020;135(17):1501–4.
Qasim W, Zhan H, Samarasinghe S, Adams S, Amrolia P, Stafford S, et al. Molecular remission of infant B-ALL after infusion of universal TALEN gene-edited CAR T cells. Sci Transl Med. 2017;9(374):eaaj2013.
Annesley C, Summers C, Pulsipher MA, Wayne AS, Rivers J, Lamble AJ, et al. Clinical experience of CAR T cell immunotherapy for relapsed and refractory infant ALL demonstrates feasibility and favorable responses. Blood. 2019;134(Supplement_1):3869.
Gardner R, Wu D, Cherian S, Fang M, Hanafi LA, Finney O, et al. Acquisition of a CD19-negative myeloid phenotype allows immune escape of MLL-rearranged B-ALL from CD19 CAR-T-cell therapy. Blood. 2016;127(20):2406–10.
Brivio E, Chantrain CF, Gruber TA, Thano A, Rialland F, Contet A, et al. Inotuzumab ozogamicin in infants and young children with relapsed or refractory acute lymphoblastic leukaemia: a case series. Br J Haematol. 2021;193(6):1172–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Breese, E.H., Kotecha, R.S., Guest, E.M. (2022). Acute Lymphoblastic Leukemia in Infants: A Distinctive, High-Risk Subtype of Childhood Acute Lymphoblastic Leukemia. In: Litzow, M.R., Raetz, E.A. (eds) Clinical Management of Acute Lymphoblastic Leukemia. Springer, Cham. https://doi.org/10.1007/978-3-030-85147-7_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-85147-7_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-85146-0
Online ISBN: 978-3-030-85147-7
eBook Packages: MedicineMedicine (R0)