Abstract
Acute lymphoblastic leukemia (ALL) in infants (<1 year old) accounts for less than 5% of childhood ALL, but demonstrate as very aggressive form of ALL with KMT2A gene rearrangement (MLL-r ALL) in 70–80% of the patients. Outcome of infants with MLL-r ALL is poor with <50% event-free survival rate even with intensive chemotherapy with or without hematopoietic stem cell transplantation. Introduction of novel therapies through international collaboration is necessary for further improvement in outcome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
ALL in infants younger than 1-year old accounts for less than 5% of childhood ALL and is positioned as a special entity both biologically and clinically. Among this age group, acute leukemia, neuroblastoma, and brain tumors occur with similar frequency, in contrast to the children over 1-year old in which acute leukemia predominates. As for acute leukemia, frequency of ALL and AML is almost equal in infants. In addition, there is a female predominance in infant ALL and most present with B-lineage phenotype.
Infant ALL comprises two distinct subtypes; ALL with rearrangements of histone lysine methyltransferase 2A gene (KMT2A, also known as mixed lineage leukemia [MLL] gene) which accounts for 70–80% of infant ALL, and ALL with germline KMT2A gene. KMT2A gene rearrangement occurs as a result of balanced chromosomal translocations involving 11q23 locus, which results in fusion of the N terminus of the KMT2A gene with the C terminus of a partner gene. Among the 94 known KMT2A partner genes nowadays, AFF1 (known as AF4) comprises approximately 50% of the infant ALL cases followed by MLLT1 (ENL) and MLLT2 (AF9) [1].
Infants with KMT2A-rearranged ALL (MLL-r ALL) usually present with high leukocyte count (WBC) and frequent involvement of extramedullary sites, such as central nervous system (CNS) and/or skin (leukemia cutis). Additionally, majority of MLL-r ALL has an immature CD10-negative B-cell precursor phenotype and is frequently associated with co-expression of myeloid-specific antigens, suggesting that infant MLL-r ALL originates from very immature lymphoid progenitors [2]. In fact, MLL-r leukemia in infants could present as an acute leukemia with ambiguous lineage (mixed phenotype acute leukemia [MPAL] or acute undifferentiated leukemia [AUL]) [3]. Also “lineage switch” from ALL to AML (usually, acute monocytic leukemia) is occasionally observed [4].
Prognosis of infants with MLL-r ALL is extremely poor with <50% event-free survival (EFS) rate in published clinical trials worldwide (Table 9.1) [5]. On the other hand, EFS rate of infants with germline KMT2A (MLL-g) ALL is >70%, relatively similar to that of older children with ALL [6, 7].
2 Risk Stratifications in Infant ALL
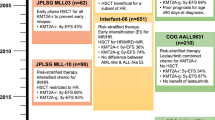
There are three major cooperative study groups worldwide conducting infant ALL-specific clinical trials: Interfant (mainly based on European countries), Children’s Oncology Group (COG, mainly based on North America), and the Japan Children’s Cancer Group (JCCG). The Japanese infant ALL trials were formerly conducted by the Japanese Infant Leukemia Cooperative Study Group (JILSG, 1995–2002) and the Japanese Pediatric Leukemia/Lymphoma Study Group (JPLSG, 2003–2013). Risk stratifications used in the recently completed clinical trials conducted by each study group is shown in Table 9.2.
As KMT2A gene status is the most significant prognostic factor in infant ALL, all three groups consider MLL-g ALL as low-risk (LR) group and MLL-r ALL as either high-risk (HR) or intermediate-risk (IR) group. Among the infants with MLL-r ALL, young age at diagnosis is most predictive of relapse, although cutoff age used is somewhat different. High WBC at diagnosis and CNS disease at diagnosis is also prognostic, but are strongly associated with young age.
In vivo treatment response at the early phase of the treatment, such as “prednisolone response” evaluating residual leukemic blasts in peripheral blood following 7 days of prednisolone monotherapy with single intrathecal methotrexate injection, is widely used for risk stratification in pediatric ALL protocols [8]. Nearly 30% of the infants with ALL fall into prednisolone poor responders (≥1000 blasts/μL), while it is less than 10% in older children with B-lineage ALL. In recent years, measurement of minimal (or measurable) residual disease (MRD) using flow cytometry detecting aberrant combinations of leukemic cell-surface antigen or PCR amplification targeting leukemic clone-specific rearrangement of immunoglobulin (Ig) or T-cell receptor (TCR) genes has become a main stratification tool in pediatric ALL protocols. These techniques can detect submicroscopic levels of residual leukemia with sensitivity of 0.01% in flow-MRD and 0.01–0.001% in PCR-MRD. MRD is highly predictive of relapse risk also in infant ALL, therefore, should be used in future risk stratifications. However, there are several cautions especially when using Ig/TCR PCR-MRD in infant MLL-r ALL. It has been reported that only half of the Ig/TCR targets in infant ALL cases reached a quantitative range of at least 10−4 and that approximately 10% of infant ALL samples resulted in underestimation of actual MRD load [9]. This phenomenon is due to less frequency of Ig/TCR rearrangements and oligoclonality of infant MLL-r ALL cells. In that sense, use of KMT2A breakpoint as a PCR target might be preferable because it should be present in total leukemic clone [10].
3 Treatment of Infant MLL-r ALL
3.1 Chemotherapy
Based on in vitro drug sensitivity experiments of infant ALL cells showing high sensitivity to cytarabine while showing high resistance against major key ALL drugs, prednisolone and asparaginase, a “hybrid chemotherapy” incorporating AML-oriented drugs (e.g., cytarabine, anthracyclines, etoposide) to ALL chemotherapy backbone is generally used to treat infants with ALL [11]. Currently, all the major study groups adopt an identical induction therapy based on Interfant-99, adding cytarabine to typical 4-drug pediatric ALL induction, which enables more than 90% of the patients to obtain complete remission [5].
A problem of infant ALL chemotherapy lies on post-induction phase, because nearly half of the patients in remission eventually relapse in relatively early phase of the treatment (usually, 4–5 months after achieving remission). A failure of improving the outcome of infants with ALL by intensifying delayed intensification phase with “VIMARAM (combination of high-dose cytarabine, high-dose methotrexate and others)” in the Interfant-99 study led the Interfant group to intensify early intensification phase with two courses of AML-oriented chemotherapy (ADE [cytarabine, daunomycin and etoposide] followed by MAE [cytarabine, mitoxantrone, and etoposide]) comparing with single course of ALL-oriented chemotherapy “IB (cyclophosphamide, 6-mercaputopurine and cytarabine)” in the Interfant-06 study, but again it showed no improvement in survival rate [5, 12]. So far, it is unlikely that further improvement could be achieved by intensifying post-induction chemotherapy using conventional drugs.
Another issue on chemotherapy for infant ALL is that most of the drugs currently used lack pharmacokinetic (PK) data on this age group [13]. PK in infants is influenced by many age-specific factors: higher percentage of total and extracellular body water content than older children or adults, higher unbound active fraction of drugs because of lower affinity of drugs to serum protein, lower P450 enzyme activity, lower tubular and glomerular function, and lower bodyweight to body surface area ratio. Currently, each cooperative study group is adjusting the dose according to age of the patients based on anecdotal evidence as shown in Table 9.3.
3.2 Hematopoietic Stem Cell Transplantation
There is a controversy over the role of allogeneic hematopoietic stem cell transplantation (HSCT) as a curative option for infants with ALL. A retrospective analysis of children and young adults with MLL-r ALL treated by 11 cooperative groups and single institutions in the United States and Europe demonstrated worse disease-free survival (DFS) and overall survival (OS) in infants with t(4;11) ALL who underwent any HSCT compared to those who underwent chemotherapy alone [14]. Combined analysis of the studies Children’s Cancer Group (CCG) 1953 and Pediatric Oncology Group (POG) 9407 showed a 5-year EFS rate of 48.8% in infants who received HSCT vs. 48.7% in infants who received chemotherapy alone (P = 0.60) [15]. Given these negative results on benefit of HSCT, the recent COG infant ALL studies have entirely eliminated an indication of HSCT for infants with ALL in first remission. On the other hand, analysis of the Interfant-99 study demonstrated a benefit of HSCT in a high-risk subset of infants with ALL in terms of DFS (59.0% versus 22.7%, P = 0.01) and OS (66.0% versus 19.3%, P = 0.001) rates, therefore, indication of HSCT is restricted but allocated to infants with HR group or with high MRD before re-induction phase in the Intrerfant-06 study [16]. The Japanese infant ALL studies in the late 1990s (MLL96 and MLL98 by JILSG) have shown the potential benefit of HSCT in an early phase before a relapse occurs [17, 18]. To prospectively evaluate this hypothesis, JPLSG MLL03 study was conducted, but nearly 50% of the infants who underwent HSCT still relapsed and ended up with 4-year EFS of 43.2% [19]. In the recently completed MLL-10 study (umin.ac.jp, UMIN000004801), HSCT was restricted to the HR cases only.
A retrospective study on 132 infants with MLL-r ALL using nationwide registry data in Japan has demonstrated no difference in relapse, non-relapse mortality and OS regarding donor type (related versus unrelated versus cord blood), and conditioning (busulfan [BU]-based vs. total body irradiation [TBI]-based myeloablative regimen) [20]. Currently, unrelated cord blood transplantation using BU-based myeloablative conditioning (e.g., BU, etoposide and cyclophosphamide) is a preferred method for transplanting infants with MLL-r ALL because of donor availability and risk of late effects associated with TBI. However, cautions are needed because BU-based conditioning is associated with risk of sinusoidal obstruction syndrome and/or pulmonary artery hypertension and with HSCT-related late effects as well [21].
3.3 Novel Therapies
It is obvious that further improvement in the outcome of infant ALL is unlikely to be achieved without novel therapeutic approach. Additionally, international collaboration is important given the rarity of the disease. Development of several novel therapies with effort on international collaboration among the Interfant, COG, and JCCG is currently underway.
3.3.1 Nucleoside Analogues
Infant MLL-r ALL cells are highly sensitive to purine nucleoside analog. Clofarabine is a second-generation purine nucleoside analog and showed highest in vitro activity among all the nucleoside analogs as well as synergistic cytotoxicity in combination with cytarabine. Additionally, clofarabine induces demethylation of the promoter region of a tumor suppressor gene FHIT (fragile histidine triad) which is often hyper-methylated in infant MLL-r ALL [22]. Efficacy and safety of clofarabine/cytarabine combination is currently tested in the JCCG infant ALL trial MLL-17 (jrct.niph.go.jp, jRCTs041190043).
3.3.2 FLT3 Inhibitors
Gene-expression profile studies have shown a unique pattern of infant MLL-r ALL. One of the highly expressed is fms-related tyrosine kinase 3 (FLT3) gene and was associated with poor prognosis [23, 24]. COG has evaluated the role of FLT3 inhibitor lestaurtinib for infants with newly diagnosed MLL-r ALL in combination with post-induction chemotherapy in the AALL0631 trial, but could not show any improvement in the outcome. Midostaurin, a multi-kinase inhibitor including FLT3, was tested against 13 children with relapsed or refractory MLL-r ALL in a European phase 1/2 single-agent study, but the response rate was modest [25].
3.3.3 Epigenetic Agents
Recent genomic studies have revealed that infant MLL-r leukemia cells are characterized by aberrant methylated genomic state with very few cooperating gene alterations [26]. Its leukemogenesis is driven by leukemia-specific histone modifications such as H3K79 dimethylation induced via DOT1L recruitment by KMT2A fusion proteins, which leads to site-specific hyper-methylation and to aberrant transcription of leukemogenic genes [27]. Thus, epigenetic modifiers such as hypomethylating agents (e.g., azacytidine, decitabine) and/or histone deacetylase inhibitors (e.g., vorinostat, panobinostat) are attractive targeting agents for infant MLL-r ALL. Pilot studies testing azacytidine-combined chemotherapy are ongoing in the United States (COG AALL15P1; clinicaltrials.gov, NCT02828358) and in Japan (AZA-MLL-P16; jrct.niph.go.jp, jRCTs031180063). In the early clinical trial, testing single-agent DOT1L inhibitor pinometostat for adults and children with MLL-r leukemia, clinical activity was unfortunately modest [28].
3.3.4 BCL-2 Inhibitors
BCL-2 family proteins regulate the intrinsic apoptosis pathway by integrating diverse prosurvival or proapoptotic intracellular signals. Recent studies revealed that KMT2A rearrangement directly induces BCL-2 overexpression in ALL cells by promoting DOT1L-mediated H3K79 methylation at the BCL2 locus [29]. BCL-2 inhibitor venetoclax has shown potent in vitro and in vivo single-agent activity against MLL-r ALL and synergized with standard ALL induction chemotherapy in a xenograft model [30].
3.3.5 Immunotherapies
Immunotherapies targeting CD19 and/or CD22 are emerging as attractive therapeutic options for high-risk B-lineage ALL [31,32,33]. A pilot study of blinatumomab, a CD19/CD3 bi-specific T-cell engager (BiTE), combined with the Interfant chemotherapy backbone is currently underway (clinicaltrialsregister.eu, 2016-004674-17). Inotuzumab ozogamicin, a CD22-targeting immunoconjugate of calicheamicin, is also drawing attention as a promising agent for B-lineage ALL, but low levels of CD22 expression in MLL-r ALL might be a limitation for its use in infants. Ultimately, chimeric antigen receptor (CAR) T-cell therapy is expected as a curative option. However, generating autologous CAR-T cells is not easy in heavily pre-treated infants because of the low number of host T-cells. Recently, two successful infant cases with relapsed MLL-r ALL, who received third-party CD19 CAR-T cells, were reported. This “off-the-shelf” allogeneic CAR-T was manufactured by disrupting TCR alpha and CD52 to avoid rejection and graft-versus-host disease (GVHD) by a gene-editing technique [34]. In the future, identification of more potent target will be important for immunotherapy in infant MLL-r ALL, because CD19 is not uniformly expressed in their leukemic cells and both CD19-negative relapse and lineage switch to CD19-negative myeloid leukemia are reported as a result of immune escape [35, 36].
4 Treatment of Infant MLL-g ALL
Unlike infants with MLL-r ALL, majority of infants with MLL-g ALL could be cured with combination of conventional chemotherapy. However, it is unclear whether they could be treated with the identical chemotherapy regimen as for older childhood counterparts or requires infant-specific chemotherapy regimen. Clinically, infants with MLL-g ALL are diagnosed at older age (majority are over 6 months old) and with lower WBC and demonstrates with higher percentage of good prednisolone response compared to infants with MLL-r ALL. The reported EFS rate is 67–95.5% [6, 7]. Biologically, frequency of favorable cytogenetics such as ETV6-RUNX1 or high hyperdiploidy is much less and have fewer genetic alterations compared to older children with ALL. Reports by the Interfant group showed high expression levels of MEIS-1 and were associated with unfavorable prognosis [37]. So far, infants with MLL-g ALL should be treated with chemotherapy specifically designed for infant ALL.
5 Treatment of Relapsed Infant ALL
Report on relapsed infant ALL is very few, and there is no standardized approach for these patients. Outcome of infants with relapsed ALL is very poor with approximately 20% OS rate. However, irrespective of previous history of HSCT, the study from Japan showed 50% chance of survival if a remission was achieved [38]. Interestingly, data from the Interfant group demonstrates that outcome of patients with MLL-g ALL is also dismal once they relapse [39]. Given the dismal outcome of relapsed patients, novel therapeutic options should be offered if available.
6 Acute and Late Toxicities on Infant ALL Treatment
Given the vulnerability of infants to cytotoxic agents, toxicity management is extremely important. Particularly during the remission induction phase, infants are at high risk of tumor lysis syndrome and intracranial hemorrhage because of the high leukemic burden in MLL-r ALL, together with a risk of severe infection [40]. To prevent sever tumor lysis syndrome, use of rasburicase is mandatory, and exchange transfusion should be considered for patients presenting with very high WBC (e.g., ≥500 K/μL).
Infants are also at high risk of developing late toxicities especially for those who underwent HSCT. Various late effects are observed among the infant ALL survivors with HSCT history such as chronic GVHD, hypothyroidism, skin abnormalities, ophthalmologic complications, pulmonary complications, dental abnormalities, and neurocognitive problems. In particular, growth retardation is very common [41, 42]. Generally, severe late effects are not commonly observed among the survivors who underwent chemotherapy only. But recently, there has been a series of case reports on fatal secondary T-cell immunodeficiency soon after the completion of COG AALL0631 chemotherapy [43]. It is not clear whether this phenomenon is derived from age-related, therapy-related, or disease-related factors, but close monitoring on immune function should be considered for follow-up of infant ALL patients.
References
Meyer C, Burmeister T, Gröger D, Tsaur G, Fechina L, Renneville A, et al. The MLL recombinome of acute leukemias in 2017. Leukemia. 2017;92:3793.
Tomizawa D. Recent progress in the treatment of infant acute lymphoblastic leukemia. Pediatr Int. 2015;57(5):811–9.
Alexander TB, Gu Z, Iacobucci I, Dickerson K, Choi JK, Xu B, et al. The genetic basis and cell of origin of mixed phenotype acute leukaemia. Nature. 2018;562(7727):373–9.
Sakaki H, Kanegane H, Nomura K, Goi K, Sugita K, Miura M, et al. Early lineage switch in an infant acute lymphoblastic leukemia. Int J Hematol. 2009;90(5):653–5.
Pieters R, Schrappe M, de Lorenzo P, Hann I, De Rossi G, Felice M, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet. 2007;370(9583):240–50.
Nagayama J, Tomizawa D, Koh K, Nagatoshi Y, Hotta N, Kishimoto T, et al. Infants with acute lymphoblastic leukemia and a germline MLL gene are highly curable with use of chemotherapy alone: results from the Japan Infant Leukemia Study Group. Blood. 2006;107(12):4663–5.
Moorman AV, Pieters R, Dreyer ZE, Heerema NA, Carroll AJ, Hunger SP, et al. Cytogenetics and outcome of infants with acute lymphoblastic leukemia and absence of MLL rearrangements. Leukemia. 2014;28(2):428–30.
Dördelmann M, Reiter A, Borkhardt A, Ludwig WD, Götz N, Viehmann S, et al. Prednisone response is the strongest predictor of treatment outcome in infant acute lymphoblastic leukemia. Blood. 1999;94(4):1209–17.
Van der Velden VHJ, Corral L, Valsecchi MG, Jansen MWJC, Cazzaniga G, Schrappe M, et al. Prognostic significance of minimal residual disease in infants with acute lymphoblastic leukemia treated within the Interfant-99 protocol. Leukemia. 2009;23(6):1073–9.
Jansen MWJC, Corral L, Van der Velden VHJ, Panzer-Grümayer R, Schrappe M, Schrauder A, et al. Immunobiological diversity in infant acute lymphoblastic leukemia is related to the occurrence and type of MLL gene rearrangement. Leukemia. 2007;21(4):633–41.
Pieters R, Boer den ML, Durian M, Janka G, Schmiegelow K, Kaspers GJL, et al. Relation between age, immunophenotype and in vitro drug resistance in 395 children with acute lymphoblastic leukemia–implications for treatment of infants. Leukemia. 1998;12(9):1344–8.
Pieters R, de Lorenzo P, Ancliffe P, Aversa LA, Brethon B, Biondi A, et al. Outcome of infants younger than 1 year with acute lymphoblastic leukemia treated with the interfant-06 protocol; results from an International Phase III Randomised Study. J Clin Oncol. 2019;37(25):2246–56.
Balis FM, Womer RB, Berg S, Winick N, Adamson PC, Fox E, et al. Dosing anticancer drugs in infants: Current approach and recommendations from the Children“s Oncology Group”s Chemotherapy Standardization Task Force. Pediatr Blood Cancer. 2017;14(9):e26636.
Pui C-H, Gaynon PS, Boyett JM, Chessells JM, Baruchel A, Kamps W, et al. Outcome of treatment in childhood acute lymphoblastic leukaemia with rearrangements of the 11q23 chromosomal region. Lancet. 2002;359(9321):1909–15.
Dreyer ZE, Dinndorf PA, Camitta B, Sather H, La MK, Devidas M, et al. Analysis of the role of hematopoietic stem-cell transplantation in infants with acute lymphoblastic leukemia in first remission and MLL gene rearrangements: a report from the Children's Oncology Group. J Clin Oncol. 2011;29(2):214–22.
Mann G, Attarbaschi A, Schrappe M, de Lorenzo P, Peters C, Hann I, et al. Improved outcome with hematopoietic stem cell transplantation in a poor prognostic subgroup of infants with mixed-lineage-leukemia (MLL)-rearranged acute lymphoblastic leukemia: results from the Interfant-99 Study. Blood. 2010;116(15):2644–50.
Isoyama K, Eguchi M, Hibi S, Kinukawa N, Ohkawa H, Kawasaki H, et al. Risk-directed treatment of infant acute lymphoblastic leukaemia based on early assessment of MLL gene status: results of the Japan Infant Leukaemia Study (MLL96). Br J Haematol. 2002;118(4):999–1010.
Kosaka Y, Koh K, Kinukawa N, Wakazono Y, Isoyama K, Oda T, et al. Infant acute lymphoblastic leukemia with MLL gene rearrangements: outcome following intensive chemotherapy and hematopoietic stem cell transplantation. Blood. 2004;104(12):3527–34.
Koh K, Tomizawa D, Moriya Saito A, Watanabe T, Miyamura T, Hirayama M, et al. Early use of allogeneic hematopoietic stem cell transplantation for infants with MLL gene-rearrangement-positive acute lymphoblastic leukemia. Leukemia. 2015;29(2):290–6.
Kato M, Hasegawa D, Koh K, Kato K, Takita J, Inagaki J, et al. Allogeneic haematopoietic stem cell transplantation for infant acute lymphoblastic leukaemia with KMT2A (MLL) rearrangements: a retrospective study from the paediatric acute lymphoblastic leukaemia working group of the Japan Society for Haematopoietic Cell Transplantation. Br J Haematol. 2015;168(4):564–70.
Kawashima N, Ikoma M, Sekiya Y, Narita A, Yoshida N, Matsumoto K, et al. Successful treatment of pulmonary hypertension with beraprost and sildenafil after cord blood transplantation for infantile leukemia. Int J Hematol. 2013;97(1):147–50.
Stumpel DJPM, Schneider P, Pieters R, Stam RW. The potential of clofarabine in MLL-rearranged infant acute lymphoblastic leukaemia. Eur J Cancer. 2015;51(14):2008–21.
Armstrong SA, Staunton JE, Silverman LB, Pieters R, Boer Den ML, Minden MD, et al. MLL translocations specify a distinct gene expression profile that distinguishes a unique leukemia. Nat Genet. 2002;30(1):41–7.
Stam RW, Schneider P, de Lorenzo P, Valsecchi MG, Boer Den ML, Pieters R. Prognostic significance of high-level FLT3 expression in MLL-rearranged infant acute lymphoblastic leukemia. Blood. 2007;110(7):2774–5.
Zwaan CM, Söderhäll S, Brethon B, Luciani M, Rizzari C, Stam RW, et al. A phase 1/2, open-label, dose-escalation study of midostaurin in children with relapsed or refractory acute leukaemia. Br J Haematol. 2018;4:263.
Andersson AK, Ma J, Wang J, Chen X, Gedman AL, Dang J, et al. The landscape of somatic mutations in infant MLL-rearranged acute lymphoblastic leukemias. Nat Genet. 2015;47(4):330–7.
Krivtsov AV, Armstrong SA. MLL translocations, histone modifications and leukaemia stem-cell development. Nat Rev Cancer. 2007;7(11):823–33.
Stein EM, Garcia-Manero G, Rizzieri DA, Tibes R, Berdeja JG, Savona MR, et al. The DOT1L inhibitor pinometostat reduces H3K79 methylation and has modest clinical activity in adult acute leukemia. Blood. 2018;131(24):2661–9.
Benito JM, Godfrey L, Kojima K, Hogdal L, Wunderlich M, Geng H, et al. MLL-rearranged acute lymphoblastic leukemias activate BCL-2 through H3K79 methylation and are sensitive to the BCL-2-specific antagonist ABT-199. Cell Rep. 2015;13(12):2715–27.
Khaw SL, Suryani S, Evans K, Richmond J, Robbins A, Kurmasheva RT, et al. Venetoclax responses of pediatric ALL xenografts reveal sensitivity of MLL-rearranged leukemia. Blood. 2016;128(10):1382–95.
Stackelberg von A, Locatelli F, Zugmaier G, Handgretinger R, Trippett TM, Rizzari C, et al. Phase I/Phase II study of blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. J Clin Oncol. 2016;34(36):4381–9.
Bhojwani D, Sposto R, Shah NN, Rodriguez V, Yuan C, Stetler-Stevenson M, et al. Inotuzumab ozogamicin in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. Leukemia. 2018;14:e205.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439–48.
Qasim W, Zhan H, Samarasinghe S, Adams S, Amrolia P, Stafford S, et al. Molecular remission of infant B-ALL after infusion of universal TALEN gene-edited CAR T cells. Sci Transl Med. 2017;9(374):eaaj2013.
Gardner R, Wu D, Cherian S, Fang M, Hanafi L-A, Finney O, et al. Acquisition of a CD19-negative myeloid phenotype allows immune escape of MLL-rearranged B-ALL from CD19 CAR-T-cell therapy. Blood. 2016;127(20):2406–10.
Zoghbi A, Stadt Zur U, Winkler B, Müller I, Escherich G. Lineage switch under blinatumomab treatment of relapsed common acute lymphoblastic leukemia without MLL rearrangement. Pediatr Blood Cancer. 2017;95(6):e26594.
van der Linden MH, Boer JM, Schneider P, Willekes M, Seslija L, de Lorenzo P, et al. Clinical and molecular genetic characterization of wild-type MLL infant acute lymphoblastic leukemia identifies few recurrent abnormalities. Haematologica. 2016;101(3):e95–9.
Tomizawa D, Koh K, Hirayama M, Miyamura T, Hatanaka M, Saikawa Y, et al. Outcome of recurrent or refractory acute lymphoblastic leukemia in infants with MLL gene rearrangements: A report from the Japan Infant Leukemia Study Group. Pediatr Blood Cancer. 2009;52(7):808–13.
Driessen EMC, de Lorenzo P, Campbell M, Felice M, Ferster A, Hann I, et al. Outcome of relapsed infant acute lymphoblastic leukemia treated on the interfant-99 protocol. Leukemia. 2016;30(5):1184–7.
Salzer WL, Jones TL, Devidas M, Hilden JM, Winick N, Hunger S, et al. Modifications to induction therapy decrease risk of early death in infants with acute lymphoblastic leukemia treated on Children’s Oncology Group P9407. Pediatr Blood Cancer. 2012;59(5):834–9.
Tomizawa D, Koh K, Sato T, Kinukawa N, Isoyama K, Kosaka Y, et al. Outcome of risk-based therapy for infant acute lymphoblastic leukemia with or without an MLL gene rearrangement, with emphasis on late effects: a final report of two consecutive studies, MLL96 and MLL98, of the Japan Infant Leukemia Study Group. Leukemia. 2007;21(11):2258–63.
Gandemer V, Bonneau J, Oudin C, Berbis J, Bertrand Y, Tabone M-D, et al. Late effects in survivors of infantile acute leukemia: a study of the L.E.A program. Blood Cancer J. 2017;7(1):e518.
Geerlinks AV, Issekutz T, Wahlstrom JT, Sullivan KE, Cowan MJ, Dvorak CC, et al. Severe, persistent, and fatal T-cell immunodeficiency following therapy for infantile leukemia. Pediatr Blood Cancer. 2016;63(11):2046–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Tomizawa, D. (2020). Infant ALL. In: Kato, M. (eds) Pediatric Acute Lymphoblastic Leukemia. Springer, Singapore. https://doi.org/10.1007/978-981-15-0548-5_9
Download citation
DOI: https://doi.org/10.1007/978-981-15-0548-5_9
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-0547-8
Online ISBN: 978-981-15-0548-5
eBook Packages: MedicineMedicine (R0)