Abstract
In most cases, acromegaly is caused by a GH-secreting pituitary somatotroph cell adenoma. Excess GH secretion subsequently increases IGF-1 levels. The clinical presentation, severity, and prognosis of the disease have been associated to distinctive tumor behavior and pathology characteristics. Some patients may harbor small localized microadenomas, whereas others have invasive macroadenomas causing compression of the optic chiasm, the latter with lower remission rates. Diverse clinical profiles are seen between patients with densely and sparsely granulated adenomas, those with and without p21-mediated cell-cycle arrest, and the degree of type 2 somatostatin receptor (SSTR2) expression on the tumor. Currently, the first-line therapy is transsphenoidal surgery in most patients followed by the somatostatin receptor ligands octreotide LAR and lanreotide autogel (directed mainly to SSTR2) or the multi-receptor SSTR ligand pasireotide LAR. Cabergoline, a dopamine D2 receptor agonist, and pegvisomant, a GH receptor antagonist, are second-line medical choices for disease control. Oral octreotide has been recently approved. Combination therapy is also increasingly employed. Stereotactic radiotherapy is indicated when patients remain active. In this chapter we will review three cases of acromegaly in patients with different clinical presentations, tumor aggressiveness, and outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Objectives-
To highlight the diverse clinical presentation and tumor behavior in patients with acromegaly.
-
To review the potential pitfalls in the diagnosis of acromegaly.
-
To learn the screening methods and follow-up of the potential comorbidities of acromegaly.
-
To review available treatment options and medical treatment response according to different clinical settings.
Overview
Acromegaly is a chronic and debilitating disorder characterized by abnormal somatic growth as a consequence of increased growth hormone (GH) levels, secreted by a somatotroph cell pituitary adenoma [1]. Research to uncover the pathophysiological mechanisms underlying somatotroph tumor cell proliferation and GH synthesis and release has shown different tumor behavior, disease activity, and response to treatment [2].
Somatotroph adenomas have been classified depending on their granulation density, hormone content, and cytogenesis [3]. Densely granulated (type 1) GH cell adenomas can be identified either by electronic microscopy or a perinuclear pattern of low-molecular-weight cytokeratin staining (CAM 5.2 or CK18). These tumors hold abundant large GH-containing secretory granules, meaning a decreased rate of GH secretion, which is reflected as a milder clinical and biochemical disease activity. In contrast, sparsely granulated adenomas show higher cell proliferation and invasiveness and cause greater disease activity, commonly unresponsive to multiple therapeutic modalities [2]. The mechanisms explaining such different tumor behavior, the current and novel therapeutic approaches, and related comorbidities of acromegaly are summarized in this chapter with the description of three clinical representative cases.
Case Presentation
Case 1
An 84-year-old woman diagnosed with acromegaly at the age of 64 presented for fatigue, muscle weakness, and weight gain. At the time of diagnosis, her symptoms were headache, prognathism, and acral growth. She received medical care after 7 years of symptoms onset. GH and insulin-like growth factor type 1 (IGF-1) levels were found increased, and a right-side, hypointense, pituitary microadenoma of 7 mm was present (Table 2.1 and Fig. 2.1). She refused neurosurgery and, therefore, was treated medically with once monthly octreotide LAR 20 mg and primary stereotactic radiosurgery with Gamma Knife. GH and IGF1 levels were normalized after treatment and remained under medical control for the following 20 years. Therapy was withdrawn after 2, 5, and 10 years to evaluate if in remission, however, increased GH levels were identified after oral glucose tolerance testing (OGTT), confirming persistent disease activity. Octreotide LAR 20 mg every 28 days was resumed, but developed symptoms of GH deficiency are confirmed by low IGF-1 levels. The medication was adjusted to every 45 and then every 60 days with resolution of symptoms. Seven years later, the patient died at 91 years due to a stage IV bladder adenocarcinoma.
Case 2
A 27-year-old man has an 8-year long evolution of acral growth, frontal bossing, nose widening, and prognathism. He also complained of arthralgia in hands and knees and increasing shoe size. Physical examination was positive for skin tags, goiter, and obesity. GH and IGF-1 levels were increased at diagnosis (Table 2.1), and pituitary MRI showed a non-invasive, intrasellar, macroadenoma (Fig. 2.1). Transsphenoidal surgery (TSS) was performed with no complications; however, the patient had persistent disease activity, and lineal accelerator (LiNAC) stereotactic fractionated radiotherapy was used for the residual tumor. Lanreotide autogel 120 mg every 28 days and cabergoline 2 mg per week were also added with good tolerance and response. Such therapy persisted until last follow-up.
Case 3
A more symptomatic 37-year-old man has a 4-year history of headache and temporal visual field impairment (manifested by multiple involuntary collisions with furniture and doors with his shoulders, arms, and knees). Physical examination was relevant for a typical acromegalic facies with macroglossia (Fig. 2.1), with significant growth of the soft tissue on his hands and feet, hypertension, tachypnea, tachycardia, and peripheral edema. The patient was hospitalized for urgent treatment and diagnosis. GH and IGF1 confirmed of acromegaly (Table 2.1). Also, prolactin was moderately high, explained by compression of the pituitary stalk. An invasive macroadenoma was found on MRI (Fig. 2.1). The patient also had hyperglycemia (285 mg/dl) corrected with an insulin analog therapy. TSS was scheduled, and primary medical treatment with lanreotide autogel 120 mg and cabergoline 1 mg per week was started to improve the patient’s condition. Cabergoline was planned to be titrated to 2 mg per week gradually; however, the patient developed acute heart failure and cardiogenic shock and unfortunately died the night before surgery.
How Does the Clinical Presentation of Acromegaly Relate to Tumor Behavior?
Every organ can be affected by the excessive systemic effect of GH and IGF1 in acromegaly, from local tumor effects (headache and visual field defects) to acral enlargement and musculoskeletal, skin, gastrointestinal, cardiovascular, endocrine, pulmonary systems morbidity [1]. However, a better understanding of acromegaly clinical presentation is emerging from recent studies [2, 4, 5]. Men are significantly younger than women at diagnosis by about 4.5 years [6]. Microadenomas in acromegaly are usually densely granulated tumors with lower disease activity and complications and more easily controlled with current therapy than sparsely granulated macroadenomas. Patients with microadenomas are usually less symptomatic and may have long-term remission without needing therapy (case 1). Despite no treatment, some patients with >65 years harbor small adenomas, with low invasion rates and a high probability of surgical remission (73%) [7]. Therefore, age is not a good predictor of remission [8]. On the other hand, invasive macroadenomas cause more symptomatology, requiring prompted evaluation and therapy. Despite earlier evaluation and treatment, remission is difficult, and multiple therapeutic modalities are commonly required [2].
Which Mechanisms Determine the Diverse Tumor Aggressiveness and Disease Activity Among These Patients?
Pituitary somatotroph cell adenomas exhibit a heterogeneous behavior ranging from small and difficult-to-detect tumors, with limited biochemical activity (case 1), to large, invasive, and highly active adenomas (case 3). Although some of the molecular mechanisms are shared by the different pituitary tumor lineages, somatotroph cell adenomas develop on a specific background of chromosomal instability with overexpression of the pituitary tumor-transforming gene protein (PTTG), which is a securin molecule that regulates chromatid segregation [9]. Then, cell cycle disruption leads to tumor growth without malignant transformation in most of all somatotroph cell adenomas, thanks to the senescence pathway [9,10,11]. PTTG overexpression leads to p53 pathway induction, increasing expression of cyclin-dependent kinase (CDKs) inhibitors such as p21, p57, and p16, which leads to irreversible cell cycle arrest [11, 12]. GH-secreting carcinomas are extremely rare cases in which p21 expression is lost [11]. When SSTR2 expression is low, it also correlates with decreased somatostatin-mediated inhibition of cell proliferation, leading to tumor growth, aggressive tumor behavior, and impaired response to treatment [13, 14]. GH secretion is lower in densely granulated cells (likely to be senescent) than in sparsely granulated somatotroph cells (likely to have higher proliferation rate) [15]. In summary, patients with densely granulated tumors are likely to show microadenomas with lower biochemical activity, higher p21 and SSTR2 expression, and more feasible to reach surgical remission or control with medical therapy. In contrast, sparsely granulated tumors are highly active and invasive and have lower p21 and SSTR2 expression and higher probability to persist with active disease despite multimodal treatment [2]. This somatotroph adenoma subtype requires close clinical surveillance and an individualized therapeutic approach.
Which Are the Pitfalls in the Diagnostic Workup of Acromegaly?
The diagnosis of acromegaly may be challenging in patients with very mild or recent-onset disease in which clinical features may not be as evident as in more active disease, which may be not related with disease duration in all cases. On the other hand, certain acromegalic features may be present in certain ethnic groups in which “acromegaloidism,” or pseudoacromegaly, is more prevalent. Pseudoacromegaly is a differential diagnosis of acromegaly and is defined in patients who have an acromegalic facies as a consequence of physiologic or pathological causes, other than increased GH or IGF-1 levels [16].
An important pitfall is the biochemically discordant acromegaly at diagnosis, previously called “micromegaly” or “small acromegaly,” and has been found not to differ from acromegaly. Between 2.4% and 13.7% of patients with acromegaly will have this biochemical discordance at diagnosis, with elevated IGF-1 levels and normal GH-nadir levels after an OGTT [17].
Pitfalls can also be found in laboratory assays. It is important for the clinician to know the details of GH and IGF-1 measurements when interpreting results. As GH has many isoforms, it is crucial to know whether the assay measures the most common variant (22 kD) GH (monoclonal) or other isoforms (polyclonal) and if it is a sensitive assay or ultra-sensitive assay [18]. In the interpretation of the OGTT, GH-nadir <1 μg/L is appropriate for sensitive assays, while 0.4 μg/L is for ultra-sensitive ones [19]. Random GH measurement is not recommended for initial diagnosis, since it is extremely variable, due to its pulsatile nature [20]. Changes in the levels of the GH-binding protein may also affect the measurement of GH [21].
Although IGF-1 is a molecule much more stable than GH, IGF-1 assays have a considerable (~ 20%) intraindividual variation to be taken into account for interpretation [19,20,21]. IGF-1 has six binding proteins (IGFBP), mainly IGFBP-3. For this reason, an IGF-1/IGFBP-3 ratio is considered as a surrogate marker of free IGF-1, which may be used when the biochemical result is discordant to the clinical picture [21].
GH and IGF-1 are the assessments of choice for diagnosis and follow-up. When further confirmation at diagnosis is necessary, an OGTT using the immunodiagnostic systems (IDS-iSYS) chemiluminescence GH assay may be required [5]. IGF-1 measurement should be adjusted for body mass index (BMI), age, and gender. Also, estrogen-containing oral contraceptives may be considered for test interpretation and to avoid false-positive results [22]. IGF-binding protein 3 (IGFBP3) and acid-labile subunit are not routinely necessary. To evaluate remission, IGF-1 should be measured at least 6 weeks post-operatively, and if they are mildly elevated, they may yet normalize by 3–6 months [5].
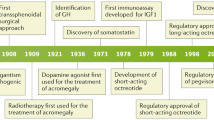
Which Therapeutic Options Are Currently Available for Acromegaly?
First-line therapy for acromegaly is pituitary adenoma resection through TSS. However, depending on country practices, some patients are treated with SRLs for tumor volume reduction before surgery, particularly those with invasive tumors without optic chiasm compression. Surgical and pharmacological outcomes in acromegaly are highly dependent on tumor size and invasiveness. Patients with microadenomas (case 1) achieve higher remission rates than non-invasive macroadenomas (case 2), and both show better outcomes than invasive macroadenomas (case 3) [23]. Somatostatin receptor ligands, octreotide LAR and lanreotide acting as SSTR2 agonists and the multiligand pasireotide LAR directed to SSTR5 > SSTR2 > SSTR3 > SSTR1 [24], have shown >20% tumor volume reduction [25, 26]. If the disease does not reach remission, combination therapy with the D2 dopamine receptor agonist cabergoline [27] and/or the GH receptor antagonist pegvisomant has shown improved efficacy than monotherapy [28,29,30]. One study found low-dose octreotide LAR (10 mg) or lanreotide (60 mg) combined with once weekly pegvisomant (40–160 mg/week) was a cost-effective option, showing a 96% biochemical control rate [31]. Stereotactic radiotherapy or radiosurgery has also demonstrated good efficacy and safety as an adjuvant therapy in patients with persistent disease and tumor residual [32, 33]. Medical therapy should be continued until reaching remission after a complete radiotherapy effect. Oral octreotide capsules (40–80 mg/day) have been recently approved by the US Food and Drug Administration for long-term maintenance treatment after proving non-inferiority in patients with adequate response and tolerance to first-generation SSTR agonist therapy (octreotide or lanreotide) [5, 34,35,36]. Potential therapies in the near future include octreotide fluid crystal (CAM2029) [37] and blocking GH receptor through antisense oligonucleotide therapy (ATL1103) [38].
These novel strategies aim to improve acromegaly disease control which is crucial to prevent excess mortality [39]. Before 2008, studies reporting higher mortality in acromegaly than general population were more commonly published (n = 17) [40]. Recent studies show normalization of mortality risk over time in disease-controlled patients when compared with the general population (SMR 1.3, 95% CI 0.9–1.8) [40, 41]. Extended dosing intervals may be an effective weaning therapy in patients under good biochemical control with SRLs and suspected remission [42].
How Should Patient Comorbidities Be Screened, Treated, and Followed?
Excess mortality in patients with acromegaly is mainly related to cardiovascular and cerebrovascular disease [41]. Comorbidities leading to this excess mortality risk are secondary diabetes mellitus, hypertension, and obstructive sleep apnea (OSA). Some patients will also develop acromegalic cardiopathy and valvular disease, leading to heart failure (case 3).
Blood pressure should be assessed every visit, while screening glucose abnormalities and electrocardiogram may be performed every 6 months to 1 year. If an impaired fasting glucose is found, an OGTT and glycated hemoglobin (HbA1c) may be performed and followed every 6 months.
OSA screening with validated scales as the Epworth sleepiness scale may be a practical option, but none of the known OSA scales has been validated as screening tools for acromegaly, and a sleep study (polysomnography) is still the study of choice for ruling out OSA at diagnosis [5]. A recent meta-analysis found significant improvement after surgical or medical treatment of acromegaly [43] and 69% OSA cure rate with disease control [44].
A clear role for echocardiography (ECHO) in acromegaly is yet to be defined [45, 46]. The Acromegaly Consensus Group suggests a baseline ECHO for screening valve disease or acromegalic cardiopathy, and repeat it yearly thereafter as needed [45].
Malignancy as an effect of chronically increased GH and IGF-1 is also a potential risk but has a lower effect on mortality. Currently, controlled acromegaly patients will have similar or longer life expectancy, increasing the chance for comorbidities that lead to death like in case 1. The most common malignancies associated with acromegaly are colorectal and thyroid cancer [46, 47]. Physical examination of the thyroid and a screening colonoscopy are therefore important. Benign neoplasms are more frequent than malignant. Therefore, follow-up colonoscopy or thyroid ultrasound is indicated similar to patients without acromegaly. If the disease remains active, surveillance can be performed more frequently individualizing each case [45].
Acromegaly has shown lower femoral neck bone mineral density (BMD) and higher risk of vertebral fractures (VF) related with lower trabecular bone score (TBS). A baseline dual-energy X-ray absorptiometry (DEXA) is therefore recommended [48]. Although acromegaly patients may have normal BMD by DEXA, they may still have fragility fractures because of lower TBS. BMD does not correlate with fracture risk as disease control does. A proactive evaluation of VF risk, with a morphometric approach, is therefore recommended [42].
Pituitary function might be followed in an individualized fashion and is frequently assessed every 6 to 12 months. Evaluation of quality of life scores with approved questionnaires may be performed annually [49].
Conclusions
Disease control is the strongest predictor of favorable outcomes in acromegaly. Somatotroph adenoma subtypes are likely to be related to the patient’s clinical manifestations of the disease. Aggressive subtypes are less likely to reach remission or biochemical control. When disease control is achieved (cases 1 and 2), comorbidities such as DM, OSA, hypertension, cardiopathy, and valvular disease are likely to be prevented, disappear, or have better response to treatment. This in turn decreases the risk of cardiovascular events, which are the most common cause of morbidity and mortality in acromegalic patients. However, chronic somatic and visceral changes are unlikely to be reversed; therefore, early diagnosis and treatment are quite important to reduce the likelihood of developing respiratory and cardiovascular complications which may lead to death (case 3). As novel treatment options continue to emerge, it is likely to achieve better outcomes for patients with acromegaly.
Lessons Learned
-
Diagnosis of acromegaly may be challenging in patients with mild symptoms, due to several pitfalls found in the interpretation GH or IGF-1 assays or discordant results at diagnosis.
-
The first-line treatment for acromegaly is transsphenoidal surgery; however, some patients with severe disease and comorbidities may benefit from primary medical therapy. Some studies report improvement in surgical remission after pretreatment, but data are conflicting.
-
Surgical and pharmacological outcomes in acromegaly are highly dependent on tumor size and invasiveness.
-
Treatment responsiveness in acromegaly may vary depending on the structural and functional characteristics of the somatotroph cell adenoma subtype.
-
As emerging medications for treating acromegaly are being approved, it is likely to achieve disease control with subsequent reduction of morbidity and mortality.
Multiple-Choice Question
-
1.
Which of the following factors are associated with somatotroph cell adenoma aggressiveness?
-
(a)
Number of mitosis
-
(b)
p21 expression
-
(c)
Granulation
-
(d)
(a) and (b)
-
(e)
(b) and (c)
-
(a)
-
Answer (e) = PTTG overexpression leads to p53 pathway induction, increasing expression of cyclin-dependent kinase (CDKs) inhibitors such as p21, which leads to irreversible cell cycle arrest and cell senescence [11, 12]. Somatotroph cell adenomas with high p21 levels are less invasive microadenomas with better disease control and prognosis. Also, GH secretion is lower in densely granulated cells (likely to be senescent) than that in sparsely granulated somatotroph cells (likely to have higher proliferation rate) with better disease control and outcomes [15]. Since usual are benign tumors, number of mitosis is low and not related with aggressiveness.
-
2.
Which of the following statements is correct regarding somatostatin receptor ligands (SRLs)?
-
(a)
Longer periods of SRL injection are not recommended despite good disease control.
-
(b)
Parenteral octreotide (IM, SC) is the only FDA-authorized route of administration in acromegaly.
-
(c)
SRLs should not be combined with other FDA-approved therapies for active acromegaly.
-
(d)
Expression of SSTR2 at somatotroph cells has a good correlation with SRL responsiveness.
-
(e)
None of the SRLs has shown tumor volume reduction >20% when used before surgery.
-
(a)
-
Answer (d) = When SSTR2 expression is low, it also correlates with decreased somatostatin-mediated inhibition of cell proliferation, leading to tumor growth, aggressive tumor behavior, and impaired response to treatment [13, 14]. Extended dosing intervals may be an effective weaning therapy in patients under good biochemical control with SRLs and suspected remission [42]. Since there are novel treatment options with different mechanisms of action, combination therapy is increasingly employed [42]. All SRLs have shown tumor volume reduction [42].
-
3.
Which factors are highly associated with surgical and pharmacological outcomes in acromegaly?
-
(a)
Age and gender
-
(b)
Neurosurgeon experience and access to stereotactic radiotherapy
-
(c)
Tumor size and invasiveness
-
(d)
Disease duration before diagnosis
-
(e)
IGFBP3 and acid-labile subunit serum levels at diagnosis
-
(a)
-
Answer (c) = Despite no treatment, some patients with >65 years harbor small adenomas, with low invasion rates and a high probability of surgical remission (73%) [7]. Therefore, age is not a good predictor of remission [8]. First-line therapy for acromegaly is pituitary adenoma resection through TSS. However, if cavernous sinus invasion is positive, neurosurgery is more difficult with lower successful rates, and it is not related with neurosurgeon experience. Therefore, surgical and pharmacological outcomes in acromegaly are highly dependent on tumor size and invasiveness. Disease duration depends on clinical and biochemical activity [2].
-
4.
How should the patient risk of comorbidities be followed?
-
(a)
Colonoscopy every year or every 5 years in patients in remission
-
(b)
Fine-needle thyroid aspiration every year when thyroid nodules are palpable
-
(c)
Echocardiography only when symptomatology is present
-
(d)
Proactive evaluation of VF with a morphometric approach
-
(e)
Acromegaly Quality of Life Questionnaire (AcroQoL) every 6 months
-
(a)
-
Answer (d) = Acromegaly has shown lower femoral neck bone mineral density (BMD) and higher risk of vertebral fractures (VF) related with lower trabecular bone score (TBS). A baseline dual-energy X-ray absorptiometry (DEXA) is therefore recommended [48]. Otherwise, follow-up colonoscopy or thyroid ultrasound is indicated similar to patients without acromegaly. If the disease remains active, surveillance can be performed more frequently individualizing each case [45]. A clear role for echocardiography in acromegaly is yet to be defined [45, 46]. Evaluation of quality of life scores with approved questionnaires (AcroQoL) may be performed annually [49].
References
Melmed S. Medical progress: acromegaly. N Engl J Med. 2006;355:2558–73.
Cuevas-Ramos D, Carmichel JD, Cooper O, et al. A structural and functional acromegaly classification. J Clin Endocrinol Metab. 2015;100:122–31.
Melmed S, Braunstein GD, Horvath E, Ezrin C, Kovacs K. Pathophysiology of acromegaly. Endocr Rev. 1983;4(3):271–90.
Lopes MBS. The 2017 World Health Organization classification of tumors of the pituitary gland: a summary. Acta Neuropathol. 2017;134(4):521–35.
Fleseriu M, Biller BMK, Freda P, et al. A pituitary society update to acromegaly management guidelines. Pituitary. 2020; https://doi.org/10.1007/s11102-020-01091-7.
Lenders NF, McCormack AI, KKY H. Management of endocrine disease: does gender matter in the management of acromegaly? Eur J Endocrinol. 2020;182(5):R67–82.
Spina A, Losa M, Mortini P. Pituitary adenomas in elderly patients: clinical and surgical outcome analysis in a large series. Endocrine. 2019;65(3):637–45.
Jane JA Jr, Starke RM, Elzoghby MA, Reames DL, Payne SC, Thorner MO, et al. Endoscopic transsphenoidal surgery for acromegaly: remission using modern criteria, complications, and predictors of outcome. J Clin Endocrinol Metab. 2011;96(9):2732–40.
Melmed S. Pathogenesis of pituitary tumors. Nat Rev Endocrinol. 2011;7:257–66.
Melmed S. Acromegaly pathogenesis and treatment. J Clin Invest. 2009;119:3189–202.
Chesnokova V, Zonis S, Kovacs K, et al. p21(Cip1) restrains pituitary pituitary tumor growth. Proc Natl Acad Sci U S A. 2008;105:17498–503.
Kuilman T, Michaloglou C, Vredeveld LC, et al. Oncogene-induced senescence relayed by an interleukin-dependent inflammatory network. Cell. 2008;133:1019–31.
Brzana J, Yedinak CG, Gultekin SH, Delashaw JB, Fleseriu M. Growth hormone granulation pattern and somatostatin receptor subtype 2A correlate with postoperative somatostatin receptor ligand response in acromegaly: a large single center experience. Pituitary. 2013;16:490–8.
Cuevas-Ramos D, Fleseriu M. Somatostatin receptor ligands and resistance to treatment in pituitary adenomas. J Mol Endocrinol. 2014;52:R223–40.
Larkin S, Reddy R, Karavitaki N, Cudlip S, Wass J, Ansorge O. Granulation pattern, but not GSP or GHR mutation, is associated with clinical characteristics in somatostatin-naive patients with somatotroph adenomas. Eur J Endocrinol. 2013;168:491–9.
Marques P, Korbonits M. Pseudoacromegaly. Front Neuroendocrinol. 2019;52:113–43.
Oliveira-Machado E, Taboada GF, Vieira-Nieto L, et al. Prevalence of discordant GH and IGF-I levels in acromegalics at diagnosis, after surgical treatment and during treatment with octreotide LAR. Growth Hormon IGF Res. 2008;18(5):389–93.
Mercado M, Espinosa-de-los-Monteros AL, Sosa E, et al. Clinical-biochemical correlations in acromegaly at diagnosis and the real prevalence of biochemically discordant disease. Horm Res. 2004;62(6):293–9.
Bidlingmaier M, Strasburger CJ. What endocrinologists should know about growth hormone measurements. Endocrinol Metab Clin N Am. 2007;36(1):101–8.
Junnila RK, Strasburger CJ, Bidlingmaier M. Pitfalls of insulin-like growth factor-I and growth hormone assays. Endocrinol Metab Clin N Am. 2015;44(1):27–34.
Frystyk J, Freda P, Clemmons DR. The current status of IGF-I assays – a 2009 update. Growth Hormon IGF Res. 2010;20(1):8–18.
Schilbach K, Gar C, Lechner A, Nicolay SS, Schwerdt L, Haenelt M, et al. Determinants of the growth hormone nadir during oral glucose tolerance test in adults. Eur J Endocrinol. 2019;181(1):55–67.
Mercado M, Abreu C, Vergara-López A, González-Virla B, Espinosa-de-Los-Monteros AL, Sosa-Eroza E, Cadena-Obando D, Cuevas-Ramos D, Portocarrero-Ortiz LA, Pérez-Reyes SP, Mercado-Cherem A, Ibarra-Salce R, Talavera JO. Surgical and pharmacological outcomes in acromegaly: real-life data from the mexican acromegaly registry. J Clin Endocrinol Metab. 2020;105(12):dgaa664.
Cuevas-Ramos D, Fleseriu M. Pasireotide: a novel treatment for patients with acromegaly. Drug Des Devel Ther. 2016;10:227–39.
Caron PJ, Bevan JS, Petersenn S, Flanagan D, Tabarin A, Prevost G, et al. Tumor shrinkage with lanreotide autogel 120 mg as primary therapy in acromegaly: results of a prospective multicenter clinical trial. J Clin Endocrinol Metab. 2014;99(4):1282–90.
Gadelha MR, Bronstein MD, Brue T, Coculescu M, Fleseriu M, Guitelman M, et al. Pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controlled acromegaly (PAOLA): a randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2014;2(11):875–84.
Sandret L, Maison P, Chanson P. Place of cabergoline in acromegaly: a meta-analysis. J Clin Endocrinol Metab. 2011;96(5):1327–35.
Buchfelder M, van der Lely AJ, Biller BMK, Webb SM, Brue T, Strasburger CJ, et al. Long-term treatment with pegvisomant: observations from 2090 acromegaly patients in ACROSTUDY. Eur J Endocrinol. 2018;179(6):419–27.
Leonart LP, Tonin FS, Ferreira VL, Fernandez-Llimos F, Pontarolo R. Effectiveness and safety of pegvisomant: a systematic review and meta-analysis of observational longitudinal studies. Endocrine. 2019;63(1):18–26.
Tritos NA, Mattsson AF, Vila G, Biller BMK, Klibanski A, Valluri S, et al. All-cause mortality in patients with acromegaly treated with pegvisomant: an ACROSTUDY analysis. Eur J Endocrinol. 2020;182(3):285–92.
Bonert V, Mirocha J, Carmichael J, Yuen KCJ, Araki T. Melmed S (2020) cost-effectiveness and efficacy of a novel combination regimen in acromegaly: a prospective, randomized trial. J Clin Endocrinol Metab. 2020;105(9):3236–45.
Graffeo CS, Donegan D, Erickson D, Brown PD, Perry A, Link MJ, et al. The impact of insulin-like growth factor index and biologically effective dose on outcomes after stereotactic radiosurgery for acromegaly: cohort study. Neurosurgery. 2020;87(3):538–46.
Knappe UJ, Petroff D, Quinkler M, Schmid SM, Schofl C, Schopohl J, et al. Fractionated radiotherapy and radiosurgery in acromegaly: analysis of 352 patients from the German acromegaly registry. Eur J Endocrinol. 2020;182(3):275–84.
Samson SL, Nachtigall LB, Fleseriu M, Gordon MB, Bolanowski M, Labadzhyan A, et al. Maintenance of acromegaly control in patients switching from injectable somatostatin receptor ligands to oral octreotide therapy. J Clin Endocrinol Metab. 2020; https://doi.org/10.1210/clinem/dgaa526.
Samson SL, Nachtigall LB, Fleseriu M, Gordon MB, Ludlam WH, Patou G, et al. Results from the phase 3, randomized, double-blind, placebo-controlled CHIASMA OPTIMAL study of oral octreotide capsules in adult patients with acromegaly. J Endocr Soc. 2020; https://doi.org/10.1210/jendso/bvaa046.211.
Melmed S, et al. Safety and efficacy of oral octreotide in acromegaly: results of a multicenter phase III trial. J Clin Endocrinol Metab. 2015;100:1699–708.
Roberts J, Linden M, Cervin C, Tiberg F. Randomized study demonstrating that octreotide fluid crystal provides sustained octreotide bioavailability and similar IGF1 suppression to octreotide LAR (sandostatin LAR) in healthy volunteers. [abstract OR17-6], Presented at the Endocrine Society’s 96th Annual Meeting and Exposition. 2014.
Trainer PJ, et al. A Phase 2 study of antisense oligonucleotide therapy directed at the GH receptor demonstrates lowering of serum IGF-I in patients with acromegaly. [abstract OR09-1], Presented at the Endocrine Society’s 97th Annual Meeting and Exposition. 2015.
Holdaway IM, Rajasoorya RC. Factors influencing mortality in acromegaly. J Clin Endocrinol Metab. 2004;89(2):667–74.
Bolfi F, Neves AF, Boguszewski CL, Nunes-Nogueira VS. Mortality in acromegaly decreased in the last decade: a systematic review and meta-analysis. Eur J Endocrinol. 2018;179(1):59–71.
Esposito D, Ragnarsson O, Granfeldt D, Marlow T, Johannsson G, Olsson DS. Decreasing mortality and changes in treatment patterns in patients with acromegaly from a nationwide study. Eur J Endocrinol. 2018;178(5):459–69.
Melmed S, Bronstein MD, Chanson P, Klibanski A, Casanueva FF, Wass JAH, et al. A consensus statement on acromegaly therapeutic outcomes. Nat Rev Endocrinol. 2018;14(9):552–61.
Parolin M, Dassie F, Allesio L, et al. Obstructive sleep apnea in acromegaly and the effect of treatment: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2020;105(3):dgz116.
Wolters TLC, Roerink SHP, Drenthen LCA, et al. The course of obstructive sleep apnea syndrome in patients with acromegaly during treatment. J Clin Endocrinol Metab. 2020;105(1):dgz050.
Melmed S, Casanueva FF, Klibanski A, et al. A consensus on the diagnosis and treatment of acromegaly. Pituitary. 2013;3:294–302.
Gadelha MR, Kasuki L, Lim DST, Fleseriu M. Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr Rev. 2019;40(1):268–332.
Lai NB, Garg D, Heaney AP, Bergsneider M, Leung AM. No benefit of dedicated thyroid nodule screening in patients with acromegaly. Endocr Pract. 2020;26(1):16–21.
Giustina A. Acromegaly and vertebral fractures: facts and questions. Trends Endocrinol Metab. 2020;31(4):274–5.
Melmed S, Casanueva FF, Klinanski A. A consensus on the diagnosis and treatment of acromegaly complications. Pituitary. 2013;16(3):294–302.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hinojosa-Amaya, J.M., Cuevas-Ramos, D. (2022). Pituitary Tumor Behavior and Disease Severity in Patients with Acromegaly. In: Davies, T.F. (eds) A Case-Based Guide to Clinical Endocrinology. Springer, Cham. https://doi.org/10.1007/978-3-030-84367-0_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-84367-0_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-84366-3
Online ISBN: 978-3-030-84367-0
eBook Packages: MedicineMedicine (R0)