Abstract
Purpose
The increased life expectancy in the general population is causing rapid growth of the number of elderly patients. Pituitary adenomas (PAs) are one of those tumors whose incidence increases with age. Pituitary surgery in elderly has usually been considered riskier than in the younger population. The aim of this study was to evaluate the surgical outcome of a large series of patients who underwent transsphenoidal surgery for PAs.
Methods
We retrospectively reviewed a series of patients who underwent transsphenoidal surgery for PAs in our institution. Inclusion criteria were: 65 years of age or more, and no previous pituitary surgery. Surgical outcomes of patients aged <70 years (group 1) was compared to those aged 70 years or more (group 2) at the time of surgery.
Results
A total of 336 patients met the inclusion criteria. Clinically, 230 (68.5%) patients had a non-functioning PAs. Among the remaining 106 patients with a hormone-secreting PA, 57 (53.8%) had acromegaly, 39 (36.8%) Cushing’s disease, 5 patients (4.7%) had a prolactinoma, and 5 a thyrotropin-secreting PA (4.7%). Mortality rate was 1.5%. Groups 1 and 2 showed no significantly different surgery-related complication, visual recovery, radical surgery, and remission rates.
Conclusions
Surgical management of PAs in the elderly has been considered riskier than in the younger population. Our results demonstrated that transsphenoidal surgery is a safe and effective treatment for PAs. No statistically significant differences in terms of outcome were found in two group ages, showing that, when clinically indicated, transsphenoidal surgery can be performed even in very old subjects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The increased life expectancy in the general population is causing rapid growth of the number of elderly patients and associated diseases [1,2,3,4]. Pituitary adenomas (PAs) are one of the central nervous system tumors whose incidence increases with age [5]. Moreover, the improvement and widespread availability of diagnostic tools have considerably increased diagnosis of such tumors in the elderly [3, 6,7,8,9,10,11,12]. Notwithstanding, the real incidence of PAs in elderly patients is probably underestimated because some endocrinological and neurological manifestations related to PAs could be misinterpreted as age-related disturbances [3, 12].
Pituitary surgery in elderly patients has usually been considered riskier when compared to younger patients [3, 13,14,15].
The aim of this retrospective study was to evaluate the surgical outcome in a large series of elderly patients undergoing transsphenoidal surgery (TSS) for PAs at our institution.
Material and methods
Patients’ selection
The medical records of all consecutive patients undergoing surgery for PA between 1990 and 2015 at our institution were reviewed. Inclusion criteria were: patients aged 65 years or more at the time of TSS surgery. The only exclusion criterion was a previous pituitary surgery.
Age at surgery, sex, symptoms at presentation, hormonal data, previous treatments, neuroimaging features, surgical results, perioperative complications, the occurrence of recurrence, further treatments, and follow-up data were prospectively collected and retrospectively analyzed.
Patients were further divided into two cohorts based on the median of the population’s age distribution: group 1 included patients aged <70 years at the time of surgery, whereas those aged 70 years or more were classified as group 2.
Standard informed consent was obtained from each patient undergoing pituitary surgery.
Preoperative evaluation
All patients underwent baseline hormonal, neuroophthalmologic, and neuroradiological evaluation before surgery, as previously described [16]. Secondary hypothyroidism was diagnosed in the presence of low free T4 with normal or low thyroid-stimulating hormone (TSH) level. Secondary hypoadrenalism was diagnosed in patients with low morning cortisol level and/or clinical symptoms of cortisol deficiency that improved with glucocorticoid replacement therapy. Hypogonadotropic hypogonadism was diagnosed in women with gonadotropin levels low or inappropriately normal for menopausal status and in males with subnormal testosterone (T) levels. Hyperprolactinemia was defined when prolactin (PRL) levels were higher than 20 µg/L in women and 15 µg/L in men in the absence of dopaminergic therapy. Visual field defect was detected by standard automated perimetry techniques.
The anesthesiologic risk was assessed according to the American Society of Anesthesiologist (ASA) risk score [17, 18].
All patients underwent a T1- and T2-weighted with gadolinium enhancement magnetic resonance imaging (MRI). Cavernous sinus invasion (CSI) was defined according to grade 3 and 4 of Knosp’s classification [19].
All patients underwent TSS, according to the previously reported technique, performed by the senior author (P.M.).
Postoperative evaluation
In patients with hormone-secreting PA (HSPA), the already described criteria of cure were adopted [20], whereas in non-functioning PAs (NFPAs), a successful surgical outcome was considered when postoperative MRI showed no adenomatous tissue.
Recurrence of disease was defined in HSPAs when hormonal hypersecretion ensued after at least 6 months of hormonal remission, while in NFPAs recurrence was defined as either appearance of new adenomatous tissue after apparent radical removal or growth of a residual tumor [16, 20].
Follow-up information was collected during outpatients’ controls.
Statistical analysis
Continuous variables were reported as the mean ± standard deviation (SD) and compared with the unpaired Student’s t test and one-way analysis of variance for repeated measures as appropriate. Categorical variables were compared with the χ2 test with Yates’ correction or Fisher’s exact test, as appropriate. Multiple logistic regression analysis with the resulting odds ratio (OR) used to determine which variables independently predicted surgical outcome and 95% confidence interval (CI) were generated for the association between baseline characteristics and analyzed variables. Kaplan–Meier analysis was performed to evaluate recurrence-free survival. Patients were censored at the date of the last follow-up. A probability value <0.05 was considered to indicate statistical significance and all reported probability values are two tailed. All calculations were performed using the statistical package IBM SPSS Statistics for Mac, version 22.0.0 (IBM Corp., Armonk, NY, USA).
Results
Patients’ characteristics
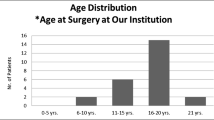
From 1990 to 2015, a total of 2655 patients underwent TSS as the first surgical procedure for PA in our institution. Elderly patients meeting the inclusion criteria were 336 (12.7%). In this group, the mean age at surgery was 70.2 ± 4.4 years (median 69 years; range 65–85 years). There were 198 (58.9%) male and 138 (41.1%) female patients for a male-to-female ratio of 1.43. According to the clinical diagnosis, 230 patients (68.5%) had NFPA, whereas the remaining 106 patients (31.5%) had an HSPA. Among HSPAs, 57 patients (53.8%) had acromegaly, 39 patients had Cushing’s disease (36.8%), 5 patients had prolactinoma (4.7%), and 5 patients had a TSH-secreting PA (4.7%).
Two hundred ninety-eight patients (88.7%) had a macroadenoma, while the remaining 38 patients (11.3%) had a microadenoma. Mean maximum tumor diameter, available in 319 patients (94.9%), was 25.0 ± 11.2 mm (median 25; range 2–80 mm). Invasion of the cavernous sinus was detected in 103 cases (30.8%) and extension into the sphenoid sinus was found in 50 patients (14.9%). Twenty-one cases presented with tumor apoplexy (6.3%).
Sixty-nine patients were classified as ASA I (20.8%), 182 as ASA II (54.8%), 79 as ASA III (23.8%), and only 2 patients as ASA IV (0.6%).
Preoperative visual function, formally assessed in 327 cases, was normal in 172 patients (52.6%), while a visual defect was found in the remaining 155 patients (47.4%): 91 patients (58.7%) had a compromised visual acuity in one or both eyes and 64 patients (41.3%) had a visual field defect only.
Hypogonadism was present in 207 of 315 patients (63.7%) with available data, hypothyroidism was present in 89 of 311 patients (28.6%), and hypoadrenalism was detected in 70 of 284 patients (24.6%).
Clinical characteristics of the patients according to age at surgery are summarized in Table 1. Compared to patients in group 1, older patients (group 2) had a significantly higher probability to have a diagnosis of NFPA and a larger PA (Table 1). CSI tended to be more frequent in group 2 patients and visual deficit at presentation was much more prevalent in group 2 than in group 1 patients (Table 1).
Surgical complications
Five patients, aged 68, 71, 72, 75, and 80 years, respectively, died in the perioperative period, accounting for an overall mortality rate of 1.5%. Two patients died of postoperative intracranial hemorrhage for residual tumors in case of giant invasive PAs, one of meningitis due to CSF leak, one of massive pulmonary embolism, and one patient with Cushing’s disease of peritonitis due to a colonic diverticulum perforation.
Table 2 summarizes the surgical and endocrinological complications.
Twenty-seven patients (8.0%) experienced a major complication of surgery. The frequency of surgical complications was similar in group 1 and group 2 patients (7.1 and 9.1%, respectively; p = 0.55). Minor complications of surgery were recorded in 16 patients (4.8%) and were equally distributed among group 1 and group 2 patients (4.4 and 5.2%, respectively; p = 0.80).
Diabetes insipidus of more than 2 months of duration and requiring treatment with desmopressin was uncommon in our series, occurring in only nine cases (2.7%). Transient postoperative hyponatremia was recorded in 18 patients (5.4%) and was classified as severe (serum sodium level below 125 mmol/L) in nine cases (2.7%). Transient hyponatremia developed in 3.8% of group 1 patients and in 7.1% of group 2 patients (p = 0.23).
New cases of pituitary deficiency were analyzed for each pituitary axis separately.
New onset hypogonadism developed in 14 of 113 (12.4%) patients with normal gonadal function before surgery and available hormonal evaluation after surgery. Similarly, new onset hypothyroidism developed in 5 of 214 (2.7%) patients and hypoadrenalism developed in 16 of 213 (7.5%) patients. Mean hospital stay was 10.5 ± 4.8 days (median 9; range 5–37 days).
Early surgical outcome
Data on visual function after surgery were available in 308 cases (91.7%). No patients with normal visual function experienced visual worsening. Among 136 patients with abnormal visual function before surgery, 33 (24.3%) had complete normalization of the visual field defect, while 83 patients (61.0%) experienced some kind of amelioration, for an overall improvement rate of 85.3%. The visual field defect remained unchanged in 17 cases (12.5%) and worsened in the remaining three patients (2.2%). The probability of partial or complete visual recovery in group 1 (87.9%) and group 2 patients (83.3%) was similar.
Normalization of hormone hypersecretion was achieved in 67.6% of the 105 cases with an HSPA (one patient with Cushing’s disease could not be assessed because of perioperative death). The rate of remission was similar in group 1 and group 2 patients (70.0 vs. 62.9%, respectively; p = 0.61). According to tumor type, the remission rate was 73.7% in acromegaly, 65.8% in Cushing’s disease, 20.0% in prolactinoma, and 60.0% in TSH-secreting pituitary adenoma.
After exclusion of 11 patients with no available postoperative MRI, the frequency of radical tumor removal in patients with NFPA was 58.9% and was similar in group 1 and group 2 patients (63.3 and 54.5%, respectively; p = 0.24).
When combining all types of pituitary adenoma, a successful surgical outcome was achieved in 200 of 324 patients with available information (61.7%). Again, no significant difference was noted between group 1 (65.9%) and group 2 patients (56.6%; p = 0.11)
Long-term outcome
Follow-up data were available for 323 patients (96.1%). The mean follow-up was 58.5 months (median 40; range 6–254 months). Forty-three patients (13.3%) underwent adjuvant postoperative radiation therapy (RT) because of a residual tumor, while 11 patients continued or commenced medical therapy for PRL- and growth hormone-secreting pituitary adenomas.
Thirty-one patients (9.4%) experienced tumor recurrence after surgery alone or surgery plus RT. Recurrences occurred after a mean time of 46.2 months (median 29 months; range 6–211 months). Further treatments for patients with tumor recurrence included RT alone in 21 cases (67.7%) and a second surgical procedure in 5 cases (16.1%). The remaining five patients (16.1%) were still on follow-up monitoring.
At last follow-up (mean 58.5 months; median 40 months; range 6–254 months), 270 patients (83.6%) were still alive, while 53 patients (16.4%) had died.
Discussion
Life expectancy in the general population has rapidly increased in the past decades and this trend is still rising [1,2,3,4]. It has been estimated that globally, from 2010 to 2015, people aged more than 60 years have annually increased at a rate of 3.7% and this rate is predicted at 2.9% every year until 2050 [1, 21].
In recent population-based studies, the highest frequency of PAs is between the ages of 40 and 60 years [6]. The incidence of PAs depends on tumor type, sex, and race. For instance, prolactinomas tend to manifest earlier than NFPAs [5, 9], while the incidence of prolactinomas tend to decrease with increasing age [5, 22]. Interestingly, Kuratsu and Ushio [10], in a study about intracranial tumor in elderly, found an age-adjusted incidence of 2.36 cases/100.000 persons/year for people aged 70 years or more, whereas it was 1.91 in patients aged <70 years.
Clinical presentation of PAs in the elderly differs from that in younger patients. For example, in elderly patients with prolactinomas, symptoms of hypogonadism are often overlooked and only large tumors are diagnosed because of mass effect symptoms, such as visual deficits [3, 12]. Moreover, visual disturbances in elderly patients can be confused with other age-related pathologies, such as cataract, macular degeneration, and vascular ocular diseases [3, 12, 23]. Hypopituitarism in elderly patients may also be misdiagnosed because of overlapping symptoms with the aging process as well as the misleading interpretation of hormonal values [12]. Hypersecreting syndromes, such as acromegaly and Cushing’s disease, are diagnosed because of typical physical changes, but in elderly patients such symptoms are mild, while other findings, such as hypertension, glucose intolerance, asthenia, and mood depression may not be correctly interpreted because of the high prevalence of these symptoms in elderly subjects [3, 12, 14, 24].
Aging is characterized by a series of co-morbidities and a generally more complex medical setting, which may negatively affect any type of treatment, especially surgical therapy [12, 14, 25]. Pituitary surgery is riskier in elderly patients [3, 13,14,15]. Anesthesia itself can potentially be hazardous because elderly patients may be less tolerant to anesthetic drugs and may be prone to more complications than younger patients [14]. In this study as well as in other series, elderly patients received the same preoperative and postoperative care of younger patients [11, 12, 14, 23, 26,27,28,29]. In our series, the proportion of patients with an ASA score >1 is similar to that reported in the literature. We did not find any correlation between the ASA score and the complication rate. This is probably due to the limits of this score for surgical procedures of short duration, such as TSS in the hands of our senior surgeon [30]. In a previous paper from our group, giant tumors and age >65 years were related to higher medical morbidity [31]. Similarly, surgical morbidity was increased in giant PAs, in NFPAs, and in older patients [20]. These data suggested that surgical management of elderly harboring PAs might be critical.
To the best of our knowledge, this is the largest surgical series of PAs in elderly patients published to date. Some studies deal with NFPAs only, whereas other series included also other sellar tumor types (Table 3) [1,2,3,4, 11, 12, 14, 23, 24, 26, 27, 29, 32,33,34,35,36,37,38,39,40,41,42,43,44].
In our series, most of the tumors were NFPAs (68.5%) and macroadenomas (88.7%), as reported in the literature. As mentioned above, HSPAs are uncommon in elderly patients and the most frequent symptom is visual disturbance [1, 3, 4, 11, 12, 14, 23, 24, 26,27,28,29, 31, 32, 34, 37, 38, 40,41,42,43, 45, 46].
The overall complication rate in our study was 9.8% and it is consistent with those reported in the literature [1,2,3,4, 11, 12, 14, 23, 24, 26, 27, 29, 32,33,34,35,36,37,38,39,40,41,42,43,44]. However, a direct comparison between our study and published series must be interpreted with caution because of varying selection criteria and different categorization of complications. Only five studies compared complication rates between different age groups [1, 4, 11, 42, 43]. Wilson et al. [43] found a statistically significant higher risk of cranial complications in patients aged 70 years or more than in those aged between 60 and 69 years, while Gondim et al. [1] found a statistically significant lower complication rate in patients younger than 60 years than in older patients. On the contrary, Robenshtok et al. [4], Zhan et al. [42], and Liu et al. [11] did not find any significant difference. In our study, no statistical difference was detected in the complication rate between the two subgroups of elderly patients.
Hyponatremia (4.8%) and permanent DI (2.7%) rates were lower than those reported in the literature. Among selected surgical complications, hemorrhage (3.9%) and CSF leak (4.5%) were similar to the rates recorded in younger patients in our center. The mortality rate in this series was 1.2% (n = 4), a slightly lower frequency than that reported in the literature, which ranges between 1.8 and 4.0%.
Hypopituitarism was a common symptom at presentation in this study as well as in most published series, especially those including NFPAs only [26]. Hypopituitarism may improve after surgical removal of the pituitary tumor. However, elderly patients have a relatively low rate of pituitary recovery [4, 11, 26, 27]. Age and the preoperative hormonal status play a crucial role for the recovery of pituitary function after surgery in patients with NFPA [47]. Preservation of pituitary function may be one of the factors to consider in choosing the optimal therapeutic strategy even in elderly patients [12, 26, 27, 47]. In our series, surgery caused pituitary deficits in a minority of patients, which was counterbalanced by improvement of preoperative deficits in other patients.
Visual disturbance improved in 80.6%, while 2.9% of patients experienced worsening of vision after surgery. The best results were obtained in patients with less severe visual defects, in keeping with previous data from our group [48].
The effect of age on visual recovery after TSS has not been entirely defined. In previously published series, resolution of visual defects has been reported in 11.5% to 100% of patients, while visual worsening has been reported between 1.9 and 20% [1, 2, 4, 11, 14, 23, 24, 26,27,28,29, 32, 34,35,36,37,38,39, 41,42,43, 49]. Robenshtok et al. [4] found less visual recovery in older patients, while other comparative series did not find any significant correlation with age [1, 11, 42]. We explored whether within elderly patients there was a difference in visual outcome after surgery. Even though older patients (group 2) had a worse preoperative visual status than group 1 patients, the chance of visual improvement was similar in the two groups. It is important to point out that serious visual defects can dramatically worse quality of life and patient independence in daily activities [50].
In PAs management, aggressive surgical resection of invasive tumors may increase the potential risk of complications without increasing clinical benefits. Partial surgical debulking is a reasonable option in invasive tumors because adjuvant RT or Gamma Knife radiosurgery represent an effective option to prevent tumor regrowth [51,52,53,54,55]. Goal of surgical treatment is primarily to relief visual and hormonal symptoms and to avoid further damages [3, 6, 16, 30, 31, 48, 51,52,53,54,55,56].
The reported rate of tumor recurrence, regardless of age, ranged from 16 to 80% depending on the degree of resection [54, 57,58,59]. In this series, 65 patients (19.3%) received postoperative adjuvant RT for residual or recurrent tumors. As underlined by Grossmann and co-workers [45], center and surgeon’s experience play an important role in elderly patient’s outcome. Considering the higher risk of perioperative complications in the elderly, it is likely that referral to high volume centers may minimize the risk of surgical management [14, 16].
The retrospective type represents one of the main limitations of this study, together with the related need to refer to a previous classification. Future studies should investigate the role of the recent classification of PAs also in this particular subset of patients.
Conclusion
With the extension of life expectancy, the number of elderly patients harboring PAs is increasing. The surgical management of PAs in these patients has been considered riskier than in the younger population. However, our results show that TSS in elderly patients is a safe and effective treatment for PAs. Moreover, we did not find any significant differences between patients aged <70 years and older ones, underscoring the notion that, when clinically indicated, TSS can be performed even in very old subjects.
References
J.A. Gondim, J.P. Almeida, L.A. de Albuquerque, E. Gomes, M. Schops, J.I. Mota, Endoscopic endonasal transsphenoidal surgery in elderly patients with pituitary adenomas. J. Neurosurg. 123(1), 31–38 (2015). https://doi.org/10.3171/2014.10.JNS14372
M. Kurosaki, W. Saeger, D.K. Ludecke, Pituitary tumors in the elderly. Pathol. Res Pract. 197(7), 493–497 (2001). https://doi.org/10.1078/0344-0338-00117
M. Losa, Pituitary tumors in the elderly. Eur. J. Endocrinol. 140(5), 378–380 (1999)
E. Robenshtok, C.A. Benbassat, D. Hirsch, G. Tzvetov, Z.R. Cohen, H.M. Iraqi, A. Gorshtein, Y. Toledano, I. Shimon, Clinical course and outcome of nonfunctioning pituitary adenomas in the elderly compared with younger age groups. Endocr. Pract. 20(2), 159–164 (2014). https://doi.org/10.4158/EP13182.OR
B.D. McDowell, R.B. Wallace, R.M. Carnahan, E.A. Chrischilles, C.F. Lynch, J.A. Schlechte, Demographic differences in incidence for pituitary adenoma. Pituitary 14(1), 23–30 (2011). https://doi.org/10.1007/s11102-010-0253-4
E.D. Aflorei, M. Korbonits, Epidemiology and etiopathogenesis of pituitary adenomas. J. Neurooncol. 117(3), 379–394 (2014). https://doi.org/10.1007/s11060-013-1354-5
P. de Robles, K.M. Fiest, A.D. Frolkis, T. Pringsheim, C. Atta, C. St Germaine-Smith, L. Day, D. Lam, N. Jette, The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. Neuro-Oncology 17(6), 776–783 (2015). https://doi.org/10.1093/neuonc/nou283
S. Ezzat, S.L. Asa, W.T. Couldwell, C.E. Barr, W.E. Dodge, M.L. Vance, I.E. McCutcheon, The prevalence of pituitary adenomas: a systematic review. Cancer 101(3), 613–619 (2004). https://doi.org/10.1002/cncr.20412
A. Fernandez, N. Karavitaki, J.A. Wass, Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin. Endocrinol. (Oxf.) 72(3), 377–382 (2010). https://doi.org/10.1111/j.1365-2265.2009.03667.x
J. Kuratsu, Y. Ushio, Epidemiological study of primary intracranial tumours in elderly people. J. Neurol. Neurosurg. Psychiatry 63(1), 116–118 (1997)
J. Liu, C. Li, Q. Xiao, C. Gan, X. Chen, W. Sun, X. Li, Y. Xu, J. Chen, K. Shu, T. Lei, Comparison of pituitary adenomas in elderly and younger adults: clinical characteristics, surgical outcomes, and prognosis. J. Am. Geriatr. Soc. 63(9), 1924–1930 (2015). https://doi.org/10.1111/jgs.13590
G. Minniti, V. Esposito, M. Piccirilli, A. Fratticci, A. Santoro, M.L. Jaffrain-Rea, Diagnosis and management of pituitary tumours in the elderly: a review based on personal experience and evidence of literature. Eur. J. Endocrinol. 153(6), 723–735 (2005). https://doi.org/10.1530/eje.1.02030
B.T. Bateman, J. Pile-Spellman, P.H. Gutin, M.F. Berman, Meningioma resection in the elderly: nationwide inpatient sample, 1998–2002. Neurosurgery 57(5), 866–872 (2005). Discussion 866–872
M. Locatelli, G. Bertani, G. Carrabba, P. Rampini, M. Zavanone, M. Caroli, E. Sala, E. Ferrante, S.M. Gaini, A. Spada, G. Mantovani, A. Lania, The trans-sphenoidal resection of pituitary adenomas in elderly patients and surgical risk. Pituitary 16(2), 146–151 (2013). https://doi.org/10.1007/s11102-012-0390-z
S.G. Rogne, A. Konglund, T.R. Meling, D. Scheie, T.B. Johannesen, P. Ronning, E. Helseth, Intracranial tumor surgery in patients >70 years of age: is clinical practice worthwhile or futile? Acta Neurol. Scand. 120(5), 288–294 (2009). https://doi.org/10.1111/j.1600-0404.2009.01157.x
M. Losa, P. Mortini, R. Barzaghi, P. Ribotto, M.R. Terreni, S.B. Marzoli, S. Pieralli, M. Giovanelli, Early results of surgery in patients with nonfunctioning pituitary adenoma and analysis of the risk of tumor recurrence. J. Neurosurg. 108(3), 525–532 (2008). https://doi.org/10.3171/JNS/2008/108/3/0525
S.C. Farrow, F.G. Fowkes, J.N. Lunn, I.B. Robertson, P. Samuel, Epidemiology in anaesthesia. II: Factors affecting mortality in hospital. Br. J. Anaesth. 54(8), 811–817 (1982)
A. Sankar, S.R. Johnson, W.S. Beattie, G. Tait, D.N. Wijeysundera, Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br. J. Anaesth. 113(3), 424–432 (2014). https://doi.org/10.1093/bja/aeu100
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4), 610–617 (1993). Discussion 617–618
P. Mortini, L.R. Barzaghi, L. Albano, P. Panni, M. Losa, Microsurgical therapy of pituitary adenomas. Endocrine 59(1), 72–81 (2018). https://doi.org/10.1007/s12020-017-1458-3
United Nations, D.o.E.a.S.A., Population Division: World Population Prospects: The 2015 Revision. Data Booklet. (2015). https://esa.un.org/unpd/wpp/Publications/Files/WPP2015_DataBooklet.pdf
H. Gittleman, Q.T. Ostrom, P.D. Farah, A. Ondracek, Y. Chen, Y. Wolinsky, C. Kruchko, J. Singer, V.R. Kshettry, E.R. Laws, A.E. Sloan, W.R. Selman, J.S. Barnholtz-Sloan, Descriptive epidemiology of pituitary tumors in the United States, 2004-2009. J. Neurosurg. 121(3), 527–535 (2014). https://doi.org/10.3171/2014.5.JNS131819
L. Ferrante, G. Trillo, E. Ramundo, P. Celli, M.L. Jaffrain-Rea, M. Salvati, V. Esposito, R. Roperto, M.F. Osti, G. Minniti, Surgical treatment of pituitary tumors in the elderly: clinical outcome and long-term follow-up. J. Neurooncol. 60(2), 185–191 (2002)
S.J. Benbow, P. Foy, B. Jones, D. Shaw, I.A. MacFarlane, Pituitary tumours presenting in the elderly: management and outcome. Clin. Endocrinol. (Oxf.) 46(6), 657–660 (1997)
C. Zoia, D. Bongetta, F. Guerrini, C. Alicino, A. Cattalani, S. Bianchini, R.J. Galzio, S. Luzzi, Outcome of elderly patients undergoing intracranial meningioma resection: a single center experience. J. Neurosurg. Sci. (2018). https://doi.org/10.23736/s0390-5616.18.04333-3
J. Hong, X. Ding, Y. Lu, Clinical analysis of 103 elderly patients with pituitary adenomas: transsphenoidal surgery and follow-up. J. Clin. Neurosci. 15(10), 1091–1095 (2008). https://doi.org/10.1016/j.jocn.2007.11.003
E.A. Pereira, P. Plaha, A. Chari, M. Paranathala, N. Haslam, A. Rogers, T. Korevaar, D. Tran, R. Olarinde, N. Karavitaki, A.B. Grossman, S.A. Cudlip, Transsphenoidal pituitary surgery in the elderly is safe and effective. Br. J. Neurosurg. 28(5), 616–621 (2014). https://doi.org/10.3109/02688697.2013.872225
P. Plaha, A. Chari, N. Haslam, E. Pereira, A. Rogers, T. Korevaar, N. Karavitaki, A. Grossman, S. Cudlip, Pituitary tumor surgery in the elderly: perioperative complications and long-term outcome. J. Neurol. Surg. B 73(S02), A125 (2012). https://doi.org/10.1055/s-0032-1314047
M.J. Puchner, U.J. Knappe, D.K. Ludecke, Pituitary surgery in elderly patients with acromegaly. Neurosurgery 36(4), 677–683 (1995). Discussion 683–674
M. Losa, G. Spatola, L. Albano, A. Gandolfi, A. Del Vecchio, A. Bolognesi, P. Mortini, Frequency, pattern, and outcome of recurrences after gamma knife radiosurgery for pituitary adenomas. Endocrine 56(3), 595–602 (2017). https://doi.org/10.1007/s12020-016-1081-8
L.R. Barzaghi, M. Losa, M. Giovanelli, P. Mortini, Complications of transsphenoidal surgery in patients with pituitary adenoma: experience at a single centre. Acta Neurochir. (Wien.) 149(9), 877–885 (2007). https://doi.org/10.1007/s00701-007-1244-8. Discussion 885–876
J.M. Sheehan, G.L. Douds, K. Hill, E. Farace, Transsphenoidal surgery for pituitary adenoma in elderly patients. Acta Neurochir. (Wien.) 150(6), 571–574 (2008). https://doi.org/10.1007/s00701-008-1581-2. Discussion 574
G. Minniti, M.L. Jaffrain-Rea, V. Esposito, A. Santoro, C. Moroni, J. Lenzi, G. Tamburrano, R. Cassone, G. Cantore, Surgical treatment and clinical outcome of GH-secreting adenomas in elderly patients. Acta Neurochir. (Wien.) 143(12), 1205–1211 (2001). https://doi.org/10.1007/s007010100015
J. Pospiech, D. Stolke, F.R. Pospiech, Surgical treatment of pituitary adenomas in elderly patients. Acta Neurochir. Suppl. 65, 35–36 (1996)
H.E. Turner, C.B. Adams, J.A. Wass, Pituitary tumours in the elderly: a 20 year experience. Eur. J. Endocrinol. 140(5), 383–389 (1999)
P. Del Monte, L. Foppiani, A. Ruelle, G. Andrioli, R. Bandelloni, P. Quilici, C. Prete, E. Palummeri, A. Marugo, D. Bernasconi, Clinically non-functioning pituitary macroadenomas in the elderly. Aging Clin. Exp. Res. 19(1), 34–40 (2007)
B. Fraioli, F.S. Pastore, S. Signoretti, G.M. De Caro, R. Giuffre, The surgical treatment of pituitary adenomas in the eighth decade. Surg. Neurol. 51(3), 261–266 (1999). Discussion 266–267
M. Kurosaki, D.K. Ludecke, J. Flitsch, W. Saeger, Surgical treatment of clinically nonsecreting pituitary adenomas in elderly patients. Neurosurgery 47(4), 843–848 (2000). Discussion 848–849
H.A. Marenco, S.T. Zymberg, P. Santos Rde, C.O. Ramalho, Surgical treatment of non-functioning pituitary macroadenomas by the endoscopic endonasal approach in the elderly. Arq. Neuropsiquiatr. 73(9), 764–769 (2015). https://doi.org/10.1590/0004-282X20150112
L. Mastronardi, A. Guiducci, F. Puzzilli, G. Maira, Anterior pituitary adenomas in patients aged more than 65 years: analysis of growth fraction (using the MIB-1 monoclonal antibody) and of clinical features in comparison to younger patients. Clin. Neurol. Neurosurg. 104(1), 44–48 (2002)
S. Yunoue, H. Tokimura, A. Tominaga, S. Fujio, P. Karki, S. Usui, Y. Kinoshita, M. Habu, F.M. Moinuddin, H. Hirano, K. Arita, Transsphenoidal surgical treatment of pituitary adenomas in patients aged 80 years or older. Neurosurg. Rev. 37(2), 269–276 (2014). https://doi.org/10.1007/s10143-013-0509-3. Discussion 276–267
R. Zhan, Z. Ma, D. Wang, X. Li, Pure endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary adenomas in the elderly: surgical outcomes and complications in 158 patients. World Neurosurg. 84(6), 1572–1578 (2015). https://doi.org/10.1016/j.wneu.2015.08.035
P.J. Wilson, S.B. Omay, A. Kacker, V.K. Anand, T.H. Schwartz, Endonasal endoscopic pituitary surgery in the elderly. J. Neurosurg. 128(2), 429–436 (2018). https://doi.org/10.3171/2016.11.JNS162286
Z. Memel, K. Chesney, D.J. Pangal, P.A. Bonney, J.D. Carmichael, G. Zada, Outcomes following transsphenoidal pituitary surgery in the elderly: a retrospective single-center review. Oper. Neurosurg. (Hagerstown) (2018). https://doi.org/10.1093/ons/opy109
R. Grossman, D. Mukherjee, K.L. Chaichana, R. Salvatori, G. Wand, H. Brem, D.C. Chang, A. Quinones-Hinojosa, Complications and death among elderly patients undergoing pituitary tumour surgery. Clin. Endocrinol. (Oxf.) 73(3), 361–368 (2010). https://doi.org/10.1111/j.1365-2265.2010.03813.x
K. Kovacs, N. Ryan, E. Horvath, W. Singer, C. Ezrin, Pituitary adenomas in old age. J. Gerontol. 35(1), 16–22 (1980)
A. Jahangiri, J.R. Wagner, S.W. Han, M.T. Tran, L.M. Miller, R. Chen, M.W. Tom, L.R. Ostling, S. Kunwar, L. Blevins, M.K. Aghi, Improved versus worsened endocrine function after transsphenoidal surgery for nonfunctional pituitary adenomas: rate, time course, and radiological analysis. J. Neurosurg. 124(3), 589–595 (2016). https://doi.org/10.3171/2015.1.JNS141543
L.R. Barzaghi, M. Medone, M. Losa, S. Bianchi, M. Giovanelli, P. Mortini, Prognostic factors of visual field improvement after trans-sphenoidal approach for pituitary macroadenomas: review of the literature and analysis by quantitative method. Neurosurg. Rev. 35(3), 369–378 (2012). https://doi.org/10.1007/s10143-011-0365-y. Discussion 378–369
D.L. Cohen, J.S. Bevan, C.B. Adams, The presentation and management of pituitary tumours in the elderly. Age Ageing 18(4), 247–252 (1989)
C.D. Andela, M. Scharloo, A.M. Pereira, A.A. Kaptein, N.R. Biermasz, Quality of life (QoL) impairments in patients with a pituitary adenoma: a systematic review of QoL studies. Pituitary 18(5), 752–776 (2015). https://doi.org/10.1007/s11102-015-0636-7
P. Mortini, Cons: endoscopic endonasal transsphenoidal pituitary surgery is not superior to microscopic transsphenoidal surgery for pituitary adenomas. Endocrine 47(2), 415–420 (2014). https://doi.org/10.1007/s12020-014-0365-0
P. Mortini, R. Barzaghi, M. Losa, N. Boari, M. Giovanelli, Surgical treatment of giant pituitary adenomas: strategies and results in a series of 95 consecutive patients. Neurosurgery 60(6), 993–1002 (2007). https://doi.org/10.1227/01.NEU.0000255459.14764.BA. Discussion 1003–1004
P. Mortini, M. Losa, R. Barzaghi, N. Boari, M. Giovanelli, Results of transsphenoidal surgery in a large series of patients with pituitary adenoma. Neurosurgery 56(6), 1222–1233 (2005). Discussion 1233
M. Losa, M. Valle, P. Mortini, A. Franzin, C.F. da Passano, M. Cenzato, S. Bianchi, P. Picozzi, M. Giovanelli, Gamma knife surgery for treatment of residual nonfunctioning pituitary adenomas after surgical debulking. J. Neurosurg. 100(3), 438–444 (2004). https://doi.org/10.3171/jns.2004.100.3.0438
M. Losa, P. Picozzi, M. Motta, M. Valle, A. Franzin, P. Mortini, The role of radiation therapy in the management of non-functioning pituitary adenomas. J. Endocrinol. Invest 34(8), 623–629 (2011). https://doi.org/10.3275/7618
M. Losa, C.A. Donofrio, R. Barzaghi, P. Mortini, Presentation and surgical results of incidentally discovered nonfunctioning pituitary adenomas: evidence for a better outcome independently of other patients’ characteristics. Eur. J. Endocrinol. 169(6), 735–742 (2013). https://doi.org/10.1530/EJE-13-0515
A. Agrawal, R. Cincu, A. Goel, Current concepts and controversies in the management of non-functioning giant pituitary macroadenomas. Clin. Neurol. Neurosurg. 109(8), 645–650 (2007). https://doi.org/10.1016/j.clineuro.2007.06.007
A.M. Musluman, T. Cansever, A. Yilmaz, A. Kanat, E. Oba, H. Cavusoglu, D. Sirinoglu, Y. Aydin, Surgical results of large and giant pituitary adenomas with special consideration of ophthalmologic outcomes. World Neurosurg. 76(1–2), 141–148 (2011). https://doi.org/10.1016/j.wneu.2011.02.009. Discussion 163–146
P. Picozzi, M. Losa, P. Mortini, M.A. Valle, A. Franzin, L. Attuati, C. Ferrari da Passano, M. Giovanelli, Radiosurgery and the prevention of regrowth of incompletely removed nonfunctioning pituitary adenomas. J. Neurosurg. 102(Suppl), 71–74 (2005)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Spina, A., Losa, M. & Mortini, P. Pituitary adenomas in elderly patients: clinical and surgical outcome analysis in a large series. Endocrine 65, 637–645 (2019). https://doi.org/10.1007/s12020-019-01959-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01959-0