Abstract
During ageing, losses in muscle mass and muscle strength are common. Unfavourable changes in muscle architecture and neurological activation of muscle tissue decrease the unit-specific muscular output, also known as muscle quality. Together, the losses in the muscular domains lead to lower physical functioning and thereby jeopardise one's independence and quality of life.
This chapter explains the age-related declines in muscle mass and quality, and how nutrition and exercise can be strategically used to prevent and counter these declines. Due attention is given to the role of nutrition and exercise in light of age-related syndromes and critical life events where muscular losses are accelerated.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Together with exercise, good nutrition is key for optimal muscle health and physical functioning. When people get older, their level of physical functioning becomes an important factor in their quality of life. The body's physical condition determines the level of independence and the activities one can join and is therefore of vital importance for healthy ageing. Thereby, physical functioning is the foundation of the extent to which an older person can still be physically, mentally, and socially active. The aim of this article is to explain how physical functioning normally declines during ageing and how this decline can be prevented or addressed with nutrition and exercise strategies.
1 Age-Related Physical Decline
A high level of physical functioning is hard to maintain throughout ageing. During ageing, several biological processes have to be fought to preserve as much of the functional capacities a person has around the age of thirty. Estimations show that after the age of thirty, people lose around three to eight per cent of muscle mass every decade (Holloszy 2000, Melton et al. 2000). Such loss implies that if a person has 35 kg of muscle mass at the age of 30, this person might end up with between 23 and 30 kg muscle mass remaining at the age of 80. One of the reasons for this age-related loss in muscle mass is a decreased exposure to anabolic stimuli later in life, such as physical activity (McPhee et al. 2016), protein intake (Tieland et al. 2012a) and anabolic hormones (Morley 2017). Additionally, the anabolic response to these stimuli is blunted in older people, a phenomenon that is termed anabolic resistance (Burd et al. 2013).
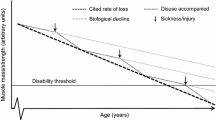
Underneath this visible muscle mass decline, a change that is less obvious, but arguably as important, is happening: a declining muscle strength. During ageing, muscle strength is decreasing at a much faster rate than muscle mass does (Fig. 14.1). The estimated loss in muscle strength is between 10 and 20% per decade up to the age of 70 (Hughes et al. 2001) and between 20 and 30% in the decades thereafter (Goodpaster et al. 2006). The loss in muscle strength is considered a more important risk factor for functional decline than the loss in muscle mass (Schaap et al. 2013). Muscle strength might, therefore, be more relevant than muscle mass for quality of life of older adults. This notion is confirmed by the work of Balogun et al. (Balogun et al. 2017). They compared community-dwelling older adults in the lowest 20% of handgrip strength or lower-limb muscle strength with those with normal strength levels, and found a significant and clinically meaningful lower health-related quality of life over ten years of follow-up for those with low strength. The associations between low appendicular mean mass and health-related quality of life were weaker, indicating that muscle strength is a stronger determinant of quality of life than muscle mass (Balogun et al. 2017).
The observation that muscle strength is lost at a higher rate than mass reveals that muscle function is not solely determined by muscle mass. The functioning of a muscle beyond its mass can be called muscle quality (Barbat-Artigas et al. 2012). A pragmatic definition of muscle quality is function per mass and can be calculated as muscle strength or power per unit of mass, volume or cross-sectional area (Barbat-Artigas et al. 2012). A more sophisticated way of evaluating muscle quality is to examine the determinants of relative muscle strength themselves (Correa-de-Araujo et al. 2017). Four important determinants of muscle quality are type II muscle fiber atrophy, mitochondrial functioning, fat infiltration, and neuromuscular activation (Fig. 14.2). The bottom layer of Fig. 14.2 shows the lifestyle factors that can improve determinants of muscle quality (explained in part 4).
2 Ageing Syndromes
Over the last decades, several forms of physical dysfunction have been classified into ageing phenotypes. The most important syndromes that are not always related to diseases are malnutrition, sarcopenia and frailty. Here, we shortly touch upon these three phenotypes and describe how they can be addressed via nutritional therapies.
Malnutrition is defined as ‘a state resulting from lack of intake or uptake of nutrition that leads to altered body composition (decreased fat free mass) and body cell mass leading to diminished physical and mental function and impaired clinical outcome from disease’ (Cederholm et al. 2017) It can be assessed via multiple screening tools, such as MNA, MST, SNAQRC and NUFFE, which are tailored to various settings (Power et al. 2018). The estimated prevalence of malnutrition is 11% in community-dwelling older adults (Schilp et al. 2012) and even higher in more vulnerable populations, with 35% in those receiving home-care (Schilp et al. 2012) and 38% in patients admitted to geriatric wards (Kruizenga et al. 2016). Malnutrition is strongly related to morbidity (Abizanda et al. 2016), mortality (McMinn et al. 2011) and functional impairments (Kiesswetter et al. 2014).
A clinical nutritional treatment against malnutrition is oral nutritional supplementation (ONS). These supplements contain all macro- and micronutrients and have shown to be effective in increasing body weight (Milne et al. 2009). Novel formulations of ONS aim to additionally target the physical condition of patients via potent nutrients such as whey protein, leucine, HMB, ursolic acid, and vitamin D (Grootswagers et al. 2018; Deutz et al. 2016; Bauer et al. 2015). These novel formulations have shown promising results on hospital readmission, chair stand test, and gait speed (Grootswagers et al. 2018; Deutz et al. 2016; Bauer et al. 2015).
Sarcopenia is defined as ‘a progressive and generalised skeletal muscle disorder that is associated with increased likelihood of adverse outcomes including falls, fractures, physical disability and mortality’ (Cruz-Jentoft et al. 2019). It is prevalent in an estimated 10% of the older adult population (Shafiee et al. 2017), and has clear detrimental effects on quality of life and independent living of older adults (Dos Santos et al. 2017; Franzon et al. 2019; Tsekoura et al. 2017) New guidelines have put muscle function central in the sarcopenia diagnosis (Cruz-Jentoft et al. 2019), which can be measured as handgrip strength or chair rise test time. Sarcopenia can also be screened for via the SARC-F questionnaire (Malmstrom et al. 2016). The recommended treatment of sarcopenia consists of resistance exercise, ideally in combination with protein or leucine and vitamin D when deficient (Morley 2018, Morley et al. 2010). Recently, sarcopenia was assigned an ICD-10 code (Anker et al. 2016), which greatly advances the recognition of sarcopenia by the international medical community.
Frailty is defined as ‘A medical syndrome with multiple causes and contributors that is characterised by diminished strength, endurance, and reduced physiologic function that increases an individual's vulnerability for developing increased dependency and/or death (Morley et al. 2013)’ and is prevalent in around 10% in women and 5% in men (Collard et al. 2012). Frailty is usually assessed by Fried's criteria (Fried et al. 2001). The distinction between frailty and sarcopenia lies in the multidimensional nature of frailty, covering not only physical declines but also cognitive and social deteriorations. Treatment options for frailty include physical exercise, protein and vitamin D (Artaza-Artabe et al. 2016).
Malnutrition, sarcopenia and frailty share common determinants, such as weight loss and muscle weakness. The overlap in the phenotypes leads to the co-existence of multiple phenotypes within the same patient (Cederholm 2015). Researchers, therefore, advised striving towards interventions that treat all three conditions, for instance, by targeting common risk factors (Verstraeten et al. 2021).
3 Critical Life Events
The gradual course of physical decline, as described in paragraph 1, reflect population means. However, on the individual level, such a gradual decline is most often no reality. During critical life events, muscle mass, muscle quality and physical functioning can decline rapidly. For instance, during ten days of bed rest, older adults lose around 1 kg of leg lean mass (Kortebein et al. 2007) and 11% of muscle strength (Kortebein et al. 2008). Importantly, the acute declines in muscle-related measures differ between individuals and are strongly related to the patient's age. For instance, for the same amount of bed rest, a young individual loses only 25% of what an older person loses (LeBlanc et al. 1992). The exact reasons for the large differences between young and older adults during similar periods of bed rest remain to be elucidated, but higher cortisol levels and reduced response to anabolic stimuli in older adults seem to play a role (English and Paddon-Jones 2010).
Critical life events are important time-frames for nutritional interventions. With nutrition and exercise, losses in muscle mass and muscle quality can be minimised, possibly preserving independence in daily activities. During and after a hospital stay and other forms of bed rest, careful monitoring of a patient's dietary intake, nutritional intake and physical activity is important. Lifestyle interventions within the capabilities of the patient, and the possibilities of the setting, are recommended to be administered when needed (English and Paddon-Jones, 2010). These interventions should try to include resistance exercise (or, if impossible, aerobic exercise or exercise mimetics) (Kouw et al. 2019), combined with supplementation with anabolic nutrients such as protein (English and Paddon-Jones 2010), leucine (English et al. 2015), or β-hydroxy β-methyl butyric acid (Deutz et al. 2013).
Often, these critical life events occur unannounced and are the result of acute injuries or diseases. In the case of elective surgeries, such as planned joint replacements, preparation for the critical life event is possible. This idea led to the concept of prehabilitation, or the better in, better out concept (Hoogeboom et al. 2014). In the weeks leading to surgery, patients are prepared via exercise training programs, often in combination with nutrition. Prehabilitation programs aim to increase muscle mass and function, to create extra capacity to better deal with the inevitable losses during hospital stays. The time window to train patients is short, on average around four weeks (Moran et al. 2016; Hughes et al. 2019). A high-intensity aerobic interval and resistance exercise training, in combination with protein supplementation, improves muscle mass by 4% and muscle strength by 10%, just enough to prevent losses during hospital stay (Grootswagers et al. 2020) (Fig. 14.3).
The projected trajectory of the potential of prehabilitation to prevent net losses in muscle mass in older adults during hospitalisation, after plotting the increase found in Grootswagers et al. (Grootswagers et al. 2020)(a, + 5.4%) and the decrease adapted from Kouw et al.[12] (b, −3.4%). The orange dotted line represents the starting level of the quadriceps cross-sectional area
4 Nutrition and Exercise
Physical functioning can be directly improved via exercise training (Chou et al. 2012). Therefore, exercise is the central aspect of the treatment of sarcopenia (Phu et al. 2015). The role of nutrition is often more indirect and supportive of exercise training, but the potential of nutrition deserves not to be overlooked. Some nutrients have clear anabolic properties and play important roles in muscle protein synthesis, muscle mass maintenance, and muscle repair. Other nutrients are involved in mechanisms that can improve the muscle output, such as force, power and endurance, by improving nutrient availability in the muscle, by improving the quality of the muscle tissue architecture or by improving the neurological activation mechanisms of the muscle.
The main anabolic nutrient is protein. The consumption of proteins elevates concentrations of amino acids and insulin in the bloodstream. The increased concentrations of these anabolic compounds are signaled by receptors located in the sarcolemma and increase the activity of the mammalian target of rapamycin (mTOR) pathway, which is the central pathway in muscle protein synthesis stimulation (McCarthy and Esser 2010) (Fig. 14.4). Leucine, an essential amino acid, has a direct stimulating effect on mTOR (Son et al. 2019) and is proposed as a key amino acid in muscle anabolism (Drummond and Rasmussen 2008). Interestingly, some of the pathways via which protein leads to muscle anabolism are proposed to underly an effect of protein on bone mass, too (Text box 1). Importantly, over the course of ageing, the response to anabolic stimuli is blunted. This anabolic resistance can be overcome by increasing the nutrient dosage and by increasing physical activity (Burd et al. 2013).
Increasing muscle mass is not the only mode of action via which nutrition and exercise can improve physical performance during ageing. Nutrients are involved in many more pathways that determine muscle output, such as muscle architecture, muscle energetics and neurological activation of the skeletal muscle tissue. The most important determinants of muscle quality where nutrients can play a role are (1) type-II atrophy, (2) mitochondrial dysfunction, (3) fat infiltration and (4) decreased neurological activation. The way in which nutrition and exercise can improve each of these four aspects of muscle quality will be explained below.
4.1 Type-II Atrophy
Specific type II muscle fibre atrophy is an important determinant of age-related decreases in muscle mass and quality. In muscle tissue, we distinguish two fibre types: type I and type II (Schiaffino and Reggiani, 2011). Type I fibres have a higher abundance of mitochondria and oxidative enzymes (Schiaffino 2010) and are more abundant in the skeletal muscle tissue of endurance athletes (Wilson et al. 2012). The type II fibres (including type IIa, IIb and IIx) have a higher glycolytic enzyme activity than type I fibres have (Essén et al. 1975), but they are more prone to fatigue (Talbot and Maves, 2016). Type II fibres are more abundant in the skeletal muscle tissue of sprinters and weight lifters (Wilson et al. 2012). During ageing, specific atrophy of type II muscle fibre size occurs. Research shows that the size of type II muscle fibres is 10 to 40% smaller in older compared to young adults (Nilwik et al. 2013; Dreyer et al. 2006; Kosek et al. 2006; Verdijk et al. 2014). Interestingly, one study showed that the difference in type II fibre size fully explained between-group differences in quadriceps size (Nilwik et al. 2013).
The cross-sectional area of type II muscle fibres does not only correlate with muscle mass but also with leg strength (Verdijk et al. 2010). Targeting age-related type II fibre atrophy is, therefore, a potential strategy to improve muscle quality. Studies show promising results on improving type II fibre size via resistance exercise (Charette et al. 1991; Campbell et al. 1999; Hagerman et al. 2000; McGuigan et al. 2001; Claflin et al. 2011; Kryger and Andersen 2007; Suetta et al. 2008; Karavirta et al. 2011; Leenders et al. 2013; Frank et al. 2016; Holwerda et al. 2018; Pyka et al. 1994; Trappe et al. 2000). It should be noted that there is an equal amount of RCTs that fail to show improvements in type II fibre size (Taaffe et al. 1996; Sipila et al. 1997; Godard et al. 2002; Campbell et al. 2002; Brose et al. 2003; Slivka et al. 2008; Cooke et al. 2014; Snijders et al. 2019; Strandberg et al. 2019; Trappe et al. 2001; Mero et al. 2013; Mitchell et al. 2015; Bechshoft et al. 2017), which could be due to different training regimens or duration, sample characteristics, or low sample size. Other types of exercise, such as endurance exercise and electrostimulation, do not seem to improve type II fibre size.
Protein could theoretically augment resistance exercise-induced improvements in type II fibre size by allowing muscle protein synthesis after resistance exercise (Tipton et al. 1999). However, only one trial (Dirks et al. 2017) of a total of nine showed positive effects of protein supplementation on type II fibre size in older adults. Moreover, trials with leucine (Leenders et al. 2011), vitamin D (Vaes et al. 2018; Ceglia et al. 2013), antioxidants (Gouzi et al. 2019), creatine (Brose et al. 2003; Cooke et al. 2014) and chromium picolinate (Campbell et al. 1999, 2002) failed to improve type II fibre size in older adults, suggesting that this determinant of muscle quality should be targeted predominantly via resistance exercise. Resistance exercise could be combined with supplementation of anabolic nutrients to obtain postulated additional improvements in type II fibre size (Little and Phillips, 2009), but this strategy needs further investigation in older adults.
4.2 Mitochondrial Dysfunction
Apart from focussing on improving muscle strength via increasing the size of type II fibres, another promising strategy to improve muscle quality is by improving mitochondrial functioning in skeletal muscle tissue. Due to the specific atrophy of type II fibers, muscles of older adults have a higher proportion of type I fibres, which have a greater abundance of mitochondria (Schiaffino 2010). Yet, the number of mitochondria and the mitochondrial oxidative capacity are reduced in older individuals (Sun et al. 2016). Sarcopenic individuals show an even further reduced mitochondrial oxidative capacity (Migliavacca et al. 2019). In these individuals, the biosynthesis of nicotinamide adenine dinucleotide (NAD+) is also repressed (Migliavacca et al. 2019). Studies show that lower mitochondrial functioning relates to lower physical performance in older adults (Santanasto et al. 2016; Coen et al. 2013).
Nutrition might stimulate mitochondrial functioning via multiple targets (Wesselink et al. 2019). For instance, dietary intake of NAD+-precursors, such as vitamin B3 and tryptophan, can lead to increased levels of NAD+ (Rajman et al. 2018; Liu et al. 2018). Moreover, certain bio-actives, such as ursolic acid, seem to directly improve mitochondrial biogenesis in mice models (Chen et al. 2017a). In older adults, the few trials that have tested the effects of different nutrients, or bio-actives, on mitochondrial functioning all found positive results (Pollack et al. 2017; Taub et al. 2016; Alway et al. 2017; de Oliveira et al. 2017). Regarding muscle quality, targeting the mitochondria might be the approach that is most adaptive to subtle changes in the environments, such as obtained by nutritional interventions. Apart from interventions with nutrients or bio-actives, endurance training and high-intensity interval training seem effective in improving mitochondrial functioning too.
4.3 Fat Infiltration
The third determinant of muscle quality is the infiltration of fat tissue in the muscle. The cross-sectional images of quadriceps muscle tissue presented in Fig. 14.5 show a clear presence of intramuscular adipose tissue (IMAT) in the 66-year-old person (B) compared to the 24-year-old person (A) (McLeod et al. 2016). While IMAT does contribute to quadriceps volume and to apparent muscle mass, it negatively affects muscle strength (Akazawa et al. 2017, Akazawa et al. 2018) or muscle endurance (Akazawa et al. 2017). Fat infiltration is, therefore, an illustrative cause of a loss in muscle quality, as it directly decreases the muscle strength per unit of muscle size. Fat infiltration may be an essential risk factor for functional decline (Visser et al. 2005). The first studies in older adults show that exercise programs can decrease IMAT (Ikenaga et al. 2017) or prevent IMAT accumulation (Goodpaster et al. 2008). That IMAT accumulation in the muscle is preventable by lifestyle is also visible in Fig. 5c. This quadriceps belongs to a 66-year-old male with a high level of physical activity. The quadriceps of this person shows amounts of IMAT that are more comparable to those of the 24-year-old male (A) than to those of the 66-year-old sedentary male (B). This suggests that physical activity might diminish the effects of ageing on IMAT accumulation. Yet, exercise interventions in older adults have yielded conflicting results.
Cross-sectional image of a quadriceps of (A) a 24-year old male, (B) a 66-year old male and (C) a 66-year old male with a high level of physical activity. Adapted from McLeod et al. 2016a (McLeod et al. 2016b), under CC BY 4.0 license (http://creativecommons.org/licenses/by/4.0/), and with changes in the number of panels, panel identification letters, and textual description within figures
Apart from physical activity, nutrition might play a role in IMAT accumulation too. Increased IMAT is observed in older adults at risk of malnutrition (Akazawa et al. 2019), with diabetes (Schafer et al. 2010), and it is related to increased insulin resistance (Albu et al. 2005; Goodpaster et al. 2000). These findings highlight the metabolic aspects of IMAT and suggest a role for nutritional interventions to prevent or decrease IMAT build up. The first dietary interventions aimed at lowering IMAT in older adults have been finished recently, with positive results for supplementing whey protein and vitamin D (Yamada et al. 2019; Englund et al. 2019).
4.4 Neurological Activation
In some cases, the loss in strength output of a muscle is not caused by morphological changes within the muscle tissue but by decreased neuromuscular activation and the loss of motor units (Clark and Fielding, 2012). Typically during ageing, we observe a loss in voluntary activation (Rozand et al. 2020). That is, the maximum force output generated by a patient's nervous system is lower than the maximum output that can be generated with electrostimulation of the muscle. Decreased voluntary activation is related to decreased physical functioning in older adults (Clark et al. 2011, 2010; Reid et al. 2014). Vitamin D (Dhesi et al. 2004) and homocysteine-lowering nutrients vitamin B6, B12 and folate (Longstreth et al. 1996a, Soumaré et al. 2006) are postulated to improve neuromuscular activation. However, the direct effect of these nutrients on neuromuscular outcomes are rarely measured (Kougias et al. 2018). Nutrients tested in randomised controlled trials that do show to improve neuromuscular activation in older adults are creatine (Stout et al. 2007), milk fat globule membrane (Minegishi et al. 2016) and N-3 fatty acids (Rodacki et al. 2012). The exercise regimens that are most effective in improving neuromuscular activation are resistance training and power training.
5 Future
The future of nutrition and exercise for the maintenance of physical functioning during ageing is exciting. Many nutrients have been identified as possible factors in physical functioning. In this final section of the chapter, an overview of the most promising nutrients is given, as well as special attention to the foreseen consequences of a transition to more plant based protein sources.
5.1 Vitamin B6, B12 and Folate
The three vitamins B6, B12 and folate act together in the one-carbon pathway, via which they suppress concentrations of homocysteine. Lowering homocysteine concentrations could be a successful strategy to improve physical functioning. Suppressed homocysteine relates to better performance in different domains of physical functioning (Vidoni et al. 2017; Kuo et al. 2007; van Schoor et al. 2012). Elevated homocysteine concentrations could hamper the functioning of mitochondria (Chen et al. 2017b, Ganapathy et al. 2011; Veeranki and Tyagi, 2013) and endothelia (Loscalzo 1996) and are related to increased white matter intensities, which affect the functioning of lower extremities (Longstreth et al. 1996b, Soumare et al. 2006). Therefore, these three B-vitamins could play a role in preserving functional capacities during ageing. Indeed, in the last years, a couple of studies have identified a possible role for B-vitamins in the maintenance of physical functioning during ageing (Behrouzi et al. 2019; Grootswagers et al. 2021; Balboa-Castillo et al. 2018; Struijk et al. 2018).
5.2 Omega-3 Fatty Acids and Vitamin D
Fatty fish species, such as salmon, herring and mackerel, are rich in omega-3 fatty acids and vitamin D, and intake of these types of fish are related to improved physical functioning in older adults (Struijk et al. 2018, Rondanelli et al. 2020). Omega-3 fatty acids have anti-inflammatory properties and could thereby target inflammageing (Dupont et al. 2019), one of the hallmarks of ageing. Additionally, omega-3 fatty acids can attenuate anabolic resistance by improving insulin sensitivity and endothelial functioning (Dupont et al. 2019, Smith et al. 2011). When combined with anabolic nutrients such as protein and amino acids, omega-3 fatty acids can improve muscle mass and functioning in older adults (Di Girolamo et al. 2014).
Vitamin D could influence muscle functioning by regulating protein synthesis and mitochondrial functioning (Domingues-Faria et al. 2017). Vitamin D status is related to improved physical functioning in older adults (Bischoff-Ferrari et al. 2004) and seems to be protective against falls (Bischoff-Ferrari et al. 2009). Where we already saw interactions between vitamin B6, B12 and folate, and between omega-3 fatty acids and protein intake, vitamin D has an interaction with calcium (Lips 2012). These interactions indicate the importance of food matrices: the natural form of foods in which nutrients present themselves together, such as protein, omega-3 fatty acids and vitamin D in fish, or vitamin D and calcium in dairy products. On a higher level, there seems to be an interaction between food items, clustered as food patterns, such as the Mediterranean diet, which is related to improved functionality at higher ages (Shahar et al. 2012; Critselis and Panagiotakos 2020; Milaneschi et al. 2011).
5.3 Hormetins
Hormetins are a special group of nutrients, as these components of food often do not have clear biological functions but do seem to play important roles in preventing age-related declines in functioning (Rattan 2008). These compounds cause mild stress in cells. Mild stress is postulated to yield beneficial effects via supercompensation, a phenomenon most known from exercise physiology. Exercise is a stressor for many body systems, but the recovery and supercompensation of the stress improve the functionality of these systems. The overall mechanism is called hormesis and works in a similar fashion, where mild stressors to the body, cells, or systems improve the functionality (Gems and Partridge 2008, Rattan 2008). Nutritional hormetins include flavonoids, resveratrol, antioxidants, and ursolic acid. Ursolic acid has shown potential in inhibiting muscle atrophy (Kunkel et al. 2011, 2012) and stimulating mitochondrial functioning (Chen et al. 2017a, Grootswagers et al. 2018). Resveratrol was found to improve mitochondrial functioning (Alway et al. 2017; Pollack et al. 2017) and type-II fiber size (Alway et al. 2017). Flavonoids are part of polyphenols and are found in dark chocolate, tea, coffee, fruits and vegetables, and have been related to improved mitochondrial functioning (Taub et al. 2016) and muscle mass maintenance (Salucci and Falcieri, 2020). There are many more compounds in natural foods that classify as hormetins, and the research outlook into these compounds in relation to ageing is exciting.
5.4 Protein Transition
Societal and governmental pressures lead to more and more people transiting from animal-based protein sources to plant-based protein sources. Animal protein has always been considered superior to plant protein in muscle anabolism (Gorissen and Witard, 2018). The quality of these animal proteins, which is based on amino acid composition and bio-availability, is overall higher than that of plant protein. It is therefore not surprising that studies have found greater acute muscle protein synthesis responses to animal products in comparison to soy, wheat or rice protein (Gorissen et al. 2016, Hartman et al. 2007, Phillips 2012, Tang et al. 2009, Wilkinson et al. 2007, Yang et al. 2012). Also, in longitudinal studies, indications for a muscle mass, preserving superiority of animal protein have been found (McLean et al. 2016). On the other hand, there have been some studies that found results suggesting an advantageous role for plant protein in the preservation of physical functioning (Dawson-Hughes et al. 2010; Behrouzi et al. 2019), possibly via alkaline properties (Dawson-Hughes et al. 2008). However, it is possible that in these studies, that were cross-sectional in nature, a confounding effect of dietary quality was present. After all, diets containing many plant proteins also contain many vitamins, minerals, fibers, hormetins and other bioactive compounds found in plants. There is a clear need for controlled, long-term, diet-based studies scrutinising the true consequences of shifting towards plant-based diets in older adults. These diet-based studies should follow a more holistic approach to balance the reductionistic dominance in current evidence – in other words, investigating meals or diets instead of single foods or ingredients (Burd et al. 2019).
5.5 Implementation of Effective Interventions
Over the years, many effective lifestyle treatments against malnutrition, sarcopenia and frailty have been identified. Unfortunately, many of these interventions do not find their way to practice (van Dongen 2019). Only by proper implementation of successful interventions in clinical practice, older adults can benefit from the wealth of knowledge that is being acquired by science. Proper implementation is thus very important but also a time-consuming activity. As an example, we showcase the implementation process of an intervention called ProMuscle. ProMuscle started as a clinical trial in 2010 and proved the efficacy of resistance training in combination with protein supplementation on lean body mass and physical performance in frail older adults (Tieland et al. 2012b, Tieland et al. 2012c). The clinical trial was translated to practice and piloted in 2014 (van Dongen et al. 2017) and after adaptations tested for effectiveness in a large practical study between 2016 and 2018 (van Dongen et al. 2020), where it proved to be effective. These positive effects in practice led to the awarding of an official entry in the Dutch Centre of Healthy Living database of governmental approved effective interventions. In future steps, the ProMuscle intervention will be further implemented into regional and national care patterns. With a path of 10 years between clinical study and the official recognition, this example clearly shows that a great effort is needed to successfully implement effective lifestyle treatments in practice. However, the societal impact and the benefits for older adults of proper implementation do evidently outweigh this effort.
6 Conclusion
To conclude, declining physical functioning during ageing is a serious problem. Lifestyle interventions have great potential in preventing and treating losses in muscle mass, muscle quality and physical functioning. These interventions should be well-timed and should employ the nutrition-exercise synergism as well as the combined effects of different nutrients in holistic approaches.
Textboxes:
1: Bone
Textbox 1
Aside from the declining muscle mass and muscle quality during ageing, decreases in bone health play important roles in age-related declines in physical abilities. Bone mass declines gradually after the age of 30, and in women, steeply after menopause. Reduced bone mass severely increases the risk of fractures and can result in osteoporosis, a geriatric phenotype prevalent in 9–38% of women and 1–8% of men (Wade et al. 2014). Nutrition plays an important role in bone mass retention during ageing. Notoriously, vitamin D and calcium are related to improved bone health, but supplementation studies are inconclusive (Zhao et al. 2017). Protein intake might play a more important role by stimulation IGF-1 and by increasing dietary calcium uptake (Dolan and Sale 2019), and higher protein intake is indeed related to reduced fracture risk (Groenendijk et al. 2019). Interestingly, vitamin D, calcium and protein are typically present in animal-based foods. A purely plant-based diet might thus jeopardise bone health, a notion that indeed has been observed in longitudinal observational studies, where vegans showed to have 15 times higher fracture risk compared to omnivores (Tong et al. 2020).
References
Abizanda P, Sinclair A, Barcons N, Lizán L, Rodríguez-Mañas L (2016) Costs of malnutrition in institutionalized and community-dwelling older adults: a systematic review. J Am Med Dir Assoc 17:17–23
Akazawa N, Harada K, Okawa N, Tamura K, Moriyama H (2018) Muscle mass and intramuscular fat of the quadriceps are related to muscle strength in non-ambulatory chronic stroke survivors: a cross-sectional study. PLoS One 13:e0201789
Akazawa N, Okawa N, Hino T, Tsuji R, Tamura K, Moriyama H (2019) Higher malnutrition risk is related to increased intramuscular adipose tissue of the quadriceps in older inpatients: a cross-sectional study. Clin Nutr 39:2586–2592
Akazawa N, Okawa N, Tamura K, Moriyama H (2017) Relationships between intramuscular fat, muscle strength and gait independence in older women: a cross-sectional study. Geriatr Gerontol Int 17:1683–1688
Albu JB, Kovera AJ, Allen L, Wainwright M, Berk E, Raja-Khan N, Janumala I, Burkey B, Heshka S, Gallagher D (2005) Independent association of insulin resistance with larger amounts of intermuscular adipose tissue and a greater acute insulin response to glucose in African American than in white nondiabetic women. Am J Clin Nutr 82:1210–1217
Alway SE, McCrory JL, Kearcher K, Vickers A, Frear B, Gilleland DL, Bonner DE, Thomas JM, Donley DA, Lively MW, Mohamed JS (2017) Resveratrol enhances exercise-induced cellular and functional adaptations of skeletal muscle in older men and women. J Gerontol A Biol Sci Med Sci 72:1595–1606
Anker SD, Morley JE, von Haehling S (2016) Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle 7:512–514
Artaza-Artabe I, Sáez-López P, Sánchez-Hernández N, Fernández-Gutierrez N, Malafarina V (2016) The relationship between nutrition and frailty: Effects of protein intake, nutritional supplementation, vitamin D and exercise on muscle metabolism in the elderly. A systematic review. Maturitas 93:89–99
Balboa-Castillo T, Struijk EA, Lopez-Garcia E, Banegas JR, Rodriguez-Artalejo F, Guallar-Castillon P (2018) Low vitamin intake is associated with risk of frailty in older adults. Age Ageing 47:872–879
Balogun S, Winzenberg T, Wills K, Scott D, Jones G, Aitken D, Callisaya ML (2017) Prospective associations of low muscle mass and function with 10-year falls risk, incident fracture and mortality in community-dwelling older adults. J Nutr Health Aging 21:843–848
Barbat-Artigas S, Rolland Y, Zamboni M, Aubertin-Leheudre M (2012) How to assess functional status: a new muscle quality index. J Nutr Health Aging 16:67–77
Bauer JM, Verlaan S, Bautmans I, Brandt K, Donini LM, Maggio M, McMurdo ME, Mets T, Seal C, Wijers SL, Ceda GP, de Vito G, Donders G, Drey M, Greig C, Holmback U, Narici M, McPhee J, Poggiogalle E, Power D, Scafoglieri A, Schultz R, Sieber CC, Cederholm T (2015) Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomised, double-blind, placebo-controlled trial. J Am Med Dir Assoc 16:740–747
Bechshoft RL, Malmgaard-Clausen NM, Gliese B, Beyer N, Mackey AL, Andersen JL, Kjaer M, Holm L (2017) Improved skeletal muscle mass and strength after heavy strength training in very old individuals. Exp Gerontol 92:96–105
Behrouzi Pariya, Grootswagers Pol, Keizer Paul L C, Smeets Ellen T H C, Feskens Edith J M, Lisette CPGM, de Groot, Fred A van Eeuwijk, (2019) Dietary intakes of vegetable protein, folate, and vitamins B-6 and B-12 are partially correlated with physical functioning of dutch older adults using copula graphical models. J Nutr 150(3):634–643
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J (2009) Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. Bmj 339:b3692
Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, Dawson-Hughes B (2004) Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged > or =60 y. Am J Clin Nutr 80:752–758
Brose A, Parise G, Tarnopolsky MA (2003) Creatine supplementation enhances isometric strength and body composition improvements following strength exercise training in older adults. J Gerontol A Biol Sci Med Sci 58:11–19
Burd NA, Gorissen SH, van Loon LJ (2013) Anabolic resistance of muscle protein synthesis with aging. Exerc Sport Sci Rev 41:169–173
Burd NA, Mckenna CF, Salvador AF, Paulussen KJM, Moore DR (2019) Dietary protein quantity, quality, and exercise are key to healthy living: a muscle-centric perspective across the lifespan. Front Nutr 6
Campbell WW, Joseph LJ, Anderson RA, Davey SL, Hinton J, Evans WJ (2002) Effects of resistive training and chromium picolinate on body composition and skeletal muscle size in older women. Int J Sport Nutr Exerc Metab 12:125–135
Campbell WW, Joseph LJ, Davey SL, Cyr-Campbell D, Anderson RA, Evans WJ (1999) Effects of resistance training and chromium picolinate on body composition and skeletal muscle in older men. J Appl Physiol 1985(86):29–39
Cederholm T (2015) Overlaps between frailty and sarcopenia definitions. Nestle Nutr Inst Workshop Ser 83:65–69
Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, Compher C, Correia I, Higashiguchi T, Holst M (2017) ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 36:49–64
Ceglia L, Niramitmahapanya S, da Silva Morais M, Rivas DA, Harris SS, Bischoff-Ferrari H, Fielding RA, Dawson-Hughes B (2013) A randomised study on the effect of vitamin D(3) supplementation on skeletal muscle morphology and vitamin D receptor concentration in older women. J Clin Endocrinol Metab 98:E1927–E1935
Charette SL, McEvoy L, Pyka G, Snow-Harter C, Guido D, Wiswell RA, Marcus R (1991) Muscle hypertrophy response to resistance training in older women. J Appl Physiol 1985(70):1912–1916
Chen J, Wong HS, Leong PK, Leung HY, Chan WM, Ko KM (2017a) Ursolic acid induces mitochondrial biogenesis through the activation of AMPK and PGC-1 in C2C12 myotubes: a possible mechanism underlying its beneficial effect on exercise endurance. Food Funct 8:2425–2436
Chen S, Dong Z, Zhao Y, Sai N, Wang X, Liu H, Huang G, Zhang X (2017b) Homocysteine induces mitochondrial dysfunction involving the crosstalk between oxidative stress and mitochondrial pSTAT3 in rat ischemic brain. Sci Rep 7:6932
Chou C-H, Hwang C-L, Wu Y-T (2012) Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: a meta-analysis. Arch Phys Med Rehabil 93:237–244
Claflin DR, Larkin LM, Cederna PS, Horowitz JF, Alexander NB, Cole NM, Galecki AT, Chen S, Nyquist LV, Carlson BM, Faulkner JA, Ashton-Miller JA (2011) Effects of high- and low-velocity resistance training on the contractile properties of skeletal muscle fibers from young and older humans. J Appl Physiol 1985(111):1021–1030
Clark DJ, Fielding RA (2012) Neuromuscular contributions to age-related weakness. J Gerontol A Biol Sci Med Sci 67:41–47
Clark DJ, Patten C, Reid KF, Carabello RJ, Phillips EM, Fielding RA (2010) Impaired voluntary neuromuscular activation limits muscle power in mobility-limited older adults. J Gerontol A Biol Sci Med Sci 65:495–502
Clark DJ, Patten C, Reid KF, Carabello RJ, Phillips EM, Fielding RA (2011) Muscle performance and physical function are associated with voluntary rate of neuromuscular activation in older adults. J Gerontol A Biol Sci Med Sci 66:115–121
Coen PM, Jubrias SA, Distefano G, Amati F, Mackey DC, Glynn NW, Manini TM, Wohlgemuth SE, Leeuwenburgh C, Cummings SR, Newman AB, Ferrucci L, Toledo FG, Shankland E, Conley KE, Goodpaster BH (2013) Skeletal muscle mitochondrial energetics are associated with maximal aerobic capacity and walking speed in older adults. J Gerontol A Biol Sci Med Sci 68:447–455
Collard RM, Boter H, Schoevers RA, OUDE VOSHAAR, R. C. (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60:1487–1492
Cooke MB, Brabham B, Buford TW, Shelmadine BD, McPheeters M, Hudson GM, Stathis C, Greenwood M, Kreider R, Willoughby DS (2014) Creatine supplementation post-exercise does not enhance training-induced adaptations in middle to older aged males. Eur J Appl Physiol 114:1321–1332
Correa-De-araujo R, Harris-Love MO, Miljkovic I, Fragala MS, Anthony BW, Manini TM (2017) The need for standardised assessment of muscle quality in skeletal muscle function deficit and other aging-related muscle dysfunctions: a symposium report. Front Physiol 8:87–87
Critselis E, Panagiotakos D (2020) Adherence to the Mediterranean diet and healthy ageing: current evidence, biological pathways, and future directions. Crit Rev Food Sci Nutr 60:2148–2157
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, writing group for the european working group on sarcopenia in older P, The extended group for E (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Dawson-Hughes B, Castaneda-Sceppa C, Harris SS, Palermo NJ, Cloutier G, Ceglia L, Dallal GE (2010) Impact of supplementation with bicarbonate on lower-extremity muscle performance in older men and women. Osteoporos Int 21:1171–1179
Dawson-Hughes B, Harris SS, Ceglia L (2008) Alkaline diets favor lean tissue mass in older adults. Am J Clin Nutr 87:662–665
de Oliveira GV, Morgado M, Conte-Junior CA, Alvares TS (2017) Acute effect of dietary nitrate on forearm muscle oxygenation, blood volume and strength in older adults: a randomised clinical trial. PLoS One 12:e0188893
Deutz NE, Matheson EM, Matarese LE, Luo M, Baggs GE, Nelson JL, Hegazi RA, Tappenden KA, Ziegler TR (2016) Readmission and mortality in malnourished, older, hospitalized adults treated with a specialized oral nutritional supplement: a randomized clinical trial. Clin Nutr 35(1):18–26. https://doi.org/10.1016/j.clnu.2015.12.010
Deutz NEP, Pereira SL, Hays NP, Oliver JS, Edens NK, Evans CM, Wolfe RR (2013) Effect of β-hydroxy-β-methylbutyrate (HMB) on lean body mass during 10 days of bed rest in older adults. Clin Nutr 32:704–712
Dhesi JK, Jackson SH, Bearne LM, Moniz C, Hurley MV, Swift CG, Allain TJ (2004) Vitamin D supplementation improves neuromuscular function in older people who fall. Age Ageing 33:589–595
di Girolamo FG, Situlin R, Mazzucco S, Valentini R, Toigo G, Biolo G (2014) Omega-3 fatty acids and protein metabolism: enhancement of anabolic interventions for sarcopenia. Curr Opin Clin Nutr Metab Care 17:145–150
Dirks ML, Tieland M, Verdijk LB, Losen M, Nilwik R, Mensink M, de Groot L, van Loon LJC (2017) Protein supplementation augments muscle fiber hypertrophy but does not modulate satellite cell content during prolonged resistance-type exercise training in frail elderly. J Am Med Dir Assoc 18:608–615
Dolan E, Sale C (2019) Protein and bone health across the lifespan. Proc Nutr Soc 78:45–55
Domingues-Faria C, Boirie Y, Walrand S (2017) Vitamin D and muscle trophicity. Curr Opin Clin Nutr Metab Care 20:169–174
dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB (2017) Sarcopenia and physical independence in older adults: the independent and synergic role of muscle mass and muscle function. J Cachexia Sarcopenia Muscle 8:245–250
Dreyer HC, Blanco CE, Sattler FR, Schroeder ET, Wiswell RA (2006) Satellite cell numbers in young and older men 24 hours after eccentric exercise. Muscle Nerve 33:242–253
Drummond MJ, Rasmussen BB (2008) Leucine-enriched nutrients and the regulation of mammalian target of rapamycin signalling and human skeletal muscle protein synthesis. Curr Opin Clin Nutr Metab Care 11:222–226
Dupont J, Dedeyne L, Dalle S, Koppo K, Gielen E (2019) The role of omega-3 in the prevention and treatment of sarcopenia. Aging Clin Exp Res 31:825–836
English KL, Mettler JA, Ellison JB, Mamerow MM, Arentson-Lantz E, Pattarini JM, Ploutz-Snyder R, Sheffield-Moore M, Paddon-Jones D (2015) Leucine partially protects muscle mass and function during bed rest in middle-aged adults1,2. Am J Clin Nutr 103:465–473
English KL, Paddon-Jones D (2010) Protecting muscle mass and function in older adults during bed rest. Curr Opin Clin Nutr Metab Care 13:34–39
Englund DA, Kirn DR, Koochek A, Zhu H, Travison TG, Reid KF, von Berens A, Melin M, Cederholm T, Gustafsson T, Fielding RA (2019) Corrigendum: nutritional supplementation with physical activity improves muscle composition in mobility-limited older adults, the VIVE2 study: a randomised, double-blind, placebo-controlled trial. J Gerontol A Biol Sci Med Sci 74:1993
Essén B, Jansson E, Henriksson J, Taylor AW, Saltin B (1975) Metabolic characteristics of fibre types in human skeletal muscle. Acta Physiol Scand 95:153–165
Frank P, Andersson E, Ponten M, Ekblom B, Ekblom M, Sahlin K (2016) Strength training improves muscle aerobic capacity and glucose tolerance in elderly. Scand J Med Sci Sports 26:764–773
Franzon K, Zethelius B, Cederholm T, Kilander L (2019) The impact of muscle function, muscle mass and sarcopenia on independent ageing in very old Swedish men. BMC Geriatr 19:153
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, cardiovascular health study collaborative research G (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Ganapathy PS, Perry RL, Tawfik A, Smith RM, Perry E, Roon P, Bozard BR, Ha YJ, Smith SB (2011) Homocysteine-mediated modulation of mitochondrial dynamics in retinal ganglion cells. Invest Ophthalmol vis Sci 52:5551–5558
Gems D, Partridge L (2008) Stress-response hormesis and aging: “that which does not kill us makes us stronger.” Cell Metab 7:200–203
Godard MP, Gallagher PM, Raue U, Trappe SW (2002) Alterations in single muscle fiber calcium sensitivity with resistance training in older women. Pflugers Arch 444:419–425
Goodpaster BH, Chomentowski P, Ward BK, Rossi A, Glynn NW, Delmonico MJ, Kritchevsky SB, Pahor M, Newman AB (2008) Effects of physical activity on strength and skeletal muscle fat infiltration in older adults: a randomised controlled trial. J Appl Physiol 1985(105):1498–1503
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Goodpaster BH, Thaete FL, Kelley DE (2000) Thigh adipose tissue distribution is associated with insulin resistance in obesity and in type 2 diabetes mellitus. Am J Clin Nutr 71:885–892
Gorissen SHM, Horstman AMH, Franssen R, Crombag JJR, Langer H, Bierau J, Respondek F, van Loon LJC (2016) Ingestion of wheat protein increases in vivo muscle protein synthesis rates in healthy older men in a randomised trial. J Nutr 146:1651–1659
Gorissen SHM, Witard OC (2018) Characterising the muscle anabolic potential of dairy, meat and plant-based protein sources in older adults. Proc Nutr Soc 77:20–31
Gouzi F, Maury J, Heraud N, Molinari N, Bertet H, Ayoub B, Blaquiere M, Bughin F, de Rigal P, Poulain M, Pincemail J, Cristol JP, Laoudj-Chenivesse D, Mercier J, Prefaut C, Pomies P, Hayot M (2019) Additional effects of nutritional antioxidant supplementation on peripheral muscle during pulmonary rehabilitation in COPD patients: a randomized controlled trial. Oxid Med Cell Longev 2019:5496346
Groenendijk I, den Boeft L, van Loon LJC, de Groot LCPGM (2019) High versus low dietary protein intake and bone health in older adults: a systematic review and meta-analysis. Comput Struct Biotechnol J 17:1101–1112
Grootswagers P, et al (2020) A 4-week exercise and protein program improves muscle mass and physical functioning in older adults - a pilot study. Exp Gerontol 141:111094
Grootswagers P, Mensink M, Berendsen AAM, Deen CPJ, Kema IP, Bakker SJL, Santoro A, Franceschi C, Meunier N, Malpuech-Brugère C, Bialecka-Debek A, Rolf K, Fairweather-Tait S, Jennings A, Feskens EJM, Lisette CPGM, de Groot (2021) Vitamin B-6 intake is related to physical performance in European older adults: results of the New Dietary Strategies Addressing the Specific Needs of the Elderly Population for Healthy Aging in Europe (NU-AGE) study. Am J Clin Nutr 113(4):781–789
Grootswagers P, Smeets E, de Groot L (2018) A novel oral nutritional supplement improves gait speed in Dutch older adults with (risk of) undernutrition. Clin Nutr 37:S6
Hagerman FC, Walsh SJ, Staron RS, Hikida RS, Gilders RM, Murray TF, Toma K, Ragg KE (2000) Effects of high-intensity resistance training on untrained older men. I. Strength, cardiovascular, and metabolic responses. J Gerontol A Biol Sci Med Sci 55:B336–B346
Hartman JW, Tang JE, Wilkinson SB, Tarnopolsky MA, Lawrence RL, Fullerton AV, Phillips SM (2007) Consumption of fat-free fluid milk after resistance exercise promotes greater lean mass accretion than does consumption of soy or carbohydrate in young, novice, male weightlifters. Am J Clin Nutr 86:373–381
Holloszy JO (2000) The biology of aging. Mayo Clin Proc 75(Suppl, S3–8):discussion S8–9
Holwerda AM, Overkamp M, Paulussen KJM, Smeets JSJ, van Kranenburg J, Backx EMP, Gijsen AP, Goessens JPB, Verdijk LB, van Loon LJC (2018) Protein supplementation after exercise and before sleep does not further augment muscle mass and strength gains during resistance exercise training in active older men. J Nutr 148:1723–1732
Hoogeboom TJ, Dronkers JJ, Hulzebos EHJ, van Meeteren NLU (2014) Merits of exercise therapy before and after major surgery. Curr Opin Anaesthesiol 27:161–166
Hughes MJ, Hackney RJ, Lamb PJ, Wigmore SJ, Christopher Deans DA, Skipworth RJE (2019) Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg 43:1661–1668
Hughes VA, Frontera WR, Wood M, Evans WJ, Dallal GE, Roubenoff R, Fiatarone Singh MA (2001) Longitudinal muscle strength changes in older adults: influence of muscle mass, physical activity, and health. J Gerontol A Biol Sci Med Sci 56:B209–B217
Ikenaga M, Yamada Y, Kose Y, Morimura K, Higaki Y, Kiyonaga A, Tanaka H (2017) Effects of a 12-week, short-interval, intermittent, low-intensity, slow-jogging program on skeletal muscle, fat infiltration, and fitness in older adults: randomised controlled trial. Eur J Appl Physiol 117:7–15
Karavirta L, Hakkinen A, Sillanpaa E, Garcia-Lopez D, Kauhanen A, Haapasaari A, Alen M, Pakarinen A, Kraemer WJ, Izquierdo M, Gorostiaga E, Hakkinen K (2011) Effects of combined endurance and strength training on muscle strength, power and hypertrophy in 40–67-year-old men. Scand J Med Sci Sports 21:402–411
Kiesswetter E, Pohlhausen S, Uhlig K, Diekmann R, Lesser S, Uter W, Heseker H, Stehle P, Sieber CC, Volkert D (2014) Prognostic differences of the Mini Nutritional Assessment short form and long form in relation to 1-year functional decline and mortality in community-dwelling older adults receiving home care. J Am Geriatr Soc 62:512–517
Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ (2007) Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 297:1772–1774
Kortebein P, Symons TB, Ferrando A, Paddon-Jones D, Ronsen O, Protas E, Conger S, Lombeida J, Wolfe R, Evans WJ (2008) Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci 63:1076–1081
Kosek DJ, Kim JS, Petrella JK, Cross JM, Bamman MM (2006) Efficacy of 3 days/wk resistance training on myofiber hypertrophy and myogenic mechanisms in young vs. older adults. J Appl Physiol (1985) 101:531–544
Kougias DG, Das T, Perez AB, Pereira SL (2018) A role for nutritional intervention in addressing the aging neuromuscular junction. Nutr Res 53:1–14
Kouw IWK, Groen BBL, Smeets JSJ, Kramer IF, van Kranenburg JMX, Nilwik R, Geurts JAP, ten Broeke RHM, Poeze M, van Loon LJC, Verdijk LB (2019) One week of hospitalization following elective hip surgery induces substantial muscle atrophy in older patients. J Am Med Dir Assoc 20:35–42
Kruizenga H, van Keeken S, Weijs P, Bastiaanse L, Beijer S, Huisman-de Waal G, Jager-Wittenaar H, Jonkers-Schuitema C, Klos M, Remijnse-Meester W, Witteman B, Thijs A (2016) Undernutrition screening survey in 564,063 patients: patients with a positive undernutrition screening score stay in hospital 1.4 d longer. Am J Clin Nutr 103:1026–1032
Kryger AI, Andersen JL (2007) Resistance training in the oldest old: consequences for muscle strength, fiber types, fiber size, and MHC isoforms. Scand J Med Sci Sports 17:422–430
Kunkel SD, Elmore CJ, Bongers KS, Ebert SM, Fox DK, Dyle MC, Bullard SA, Adams CM (2012) Ursolic acid increases skeletal muscle and brown fat and decreases diet-induced obesity, glucose intolerance and fatty liver disease. PLoS One 7:e39332
Kunkel SD, Suneja M, Ebert SM, Bongers KS, Fox DK, Malmberg SE, Alipour F, Shields RK, Adams CM (2011) mRNA expression signatures of human skeletal muscle atrophy identify a natural compound that increases muscle mass. Cell Metab 13:627–638
Kuo HK, Liao KC, Leveille SG, Bean JF, Yen CJ, Chen JH, Yu YH, Tai TY (2007) Relationship of homocysteine levels to quadriceps strength, gait speed, and late-life disability in older adults. J Gerontol A Biol Sci Med Sci 62:434–439
Leblanc AD, Schneider VS, Evans HJ, Pientok C, Rowe R, Spector E (1992) Regional changes in muscle mass following 17 weeks of bed rest. J Appl Physiol 1985(73):2172–2178
Leenders M, Verdijk LB, van der Hoeven L, van Kranenburg J, Hartgens F, Wodzig WK, Saris WH, van Loon LJ (2011) Prolonged leucine supplementation does not augment muscle mass or affect glycemic control in elderly type 2 diabetic men. J Nutr 141:1070–1076
Leenders M, Verdijk LB, van der Hoeven L, van Kranenburg J, Nilwik R, Wodzig WK, Senden JM, Keizer HA, van Loon LJ (2013) Protein supplementation during resistance-type exercise training in the elderly. Med Sci Sports Exerc 45:542–552
Lips P (2012) Interaction between vitamin D and calcium. Scand J Clin Lab Invest Suppl 243:60–64
Little JP, Phillips SM (2009) Resistance exercise and nutrition to counteract muscle wasting. Appl Physiol Nutr Metab 34:817–828
Liu L, Su X, William JQ, Sheng H, Kristin K, David WF, Philip R, Le Z, Karthikeyani C, Eileen W, Marie M, Timothy JM, Joseph AB, Joshua DR (2018) Quantitative analysis of nad synthesis-breakdown fluxes. Cell Metab 27(5):1067-1080.e5
Jr Longstreth WT, Manolio TA, Arnold A, Burke GL, Bryan N, Jungreis CA, Enright PL, O’leary D, Fried L (1996a) Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people. The Cardiovascular Health Study. Stroke 27:1274–1282
Longstreth WT, Manolio TA, Arnold A, Burke GL, Bryan N, Jungreis CA, Enright PL, Oleary D, Fried L (1996b) Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people - The cardiovascular health study. Stroke 27:1274–1282
Loscalzo J (1996) The oxidant stress of hyperhomocyst(e)inemia. J Clin Investig 98:5–7
Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE (2016) SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 7:28–36
McCarthy JJ, Esser KA (2010) Anabolic and catabolic pathways regulating skeletal muscle mass. Curr Opin Clin Nutr Metab Care 13:230–235
McGuigan MR, Bronks R, Newton RU, Sharman MJ, Graham JC, Cody DV, Kraemer WJ (2001) Resistance training in patients with peripheral arterial disease: effects on myosin isoforms, fiber type distribution, and capillary supply to skeletal muscle. J Gerontol A Biol Sci Med Sci 56:B302–B310
McLean RR, Mangano KM, Hannan MT, Kiel DP, Sahni S (2016) Dietary protein intake is protective against loss of grip strength among older adults in the framingham offspring cohort. J Gerontol Ser-Biol Sci Med Sci 71:356–361
McLeod M, Breen L, Hamilton DL, Philp A (2016) Live strong and prosper: the importance of skeletal muscle strength for healthy ageing. Biogerontology 17:497–510
Mcminn J, Steel C, Bowman A (2011) Investigation and management of unintentional weight loss in older adults. BMJ 342:d1732
McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H (2016) Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology 17:567–580
Joseph Melton III K, Khosla S, Crowson CS, O’Connor MK, O’Fallon WM, Riggs BL (2000) Epidemiology of sarcopenia. J Am Geriat Soc 48(6):625–630
Mero AA, Hulmi JJ, Salmijarvi H, Katajavuori M, Haverinen M, Holviala J, Ridanpaa T, Hakkinen K, Kovanen V, Ahtiainen JP, Selanne H (2013) Resistance training induced increase in muscle fiber size in young and older men. Eur J Appl Physiol 113:641–650
Migliavacca E, Tay SKH, Patel HP, Sonntag T, Civiletto G, Mcfarlane C, Forrester T, Barton SJ, Leow MK, Antoun E, Charpagne A, Seng Chong Y, Descombes P, Feng L, Francis-Emmanuel P, Garratt ES, Giner MP, Green CO, Karaz S, Kothandaraman N, Marquis J, Metairon S, Moco S, Nelson G, Ngo S, Pleasants T, Raymond F, Sayer AA, Ming Sim C, Slater-Jefferies J, Syddall HE, Fang Tan P, Titcombe P, Vaz C, Westbury LD, Wong G, Yonghui W, Cooper C, Sheppard A, Godfrey KM, Lillycrop KA, Karnani N, Feige JN (2019) Mitochondrial oxidative capacity and NAD(+) biosynthesis are reduced in human sarcopenia across ethnicities. Nat Commun 10:5808
Milaneschi Y, Bandinelli S, Corsi AM, Lauretani F, Paolisso G, Dominguez LJ, Semba RD, Tanaka T, Abbatecola AM, Talegawkar SA, Guralnik JM, Ferrucci L (2011) Mediterranean diet and mobility decline in older persons. Exp Gerontol 46:303–308
Milne AC, Potter J, Vivanti A, Avenell A (2009) Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev CD003288
Minegishi Y, Ota N, Soga S, Shimotoyodome A (2016) Effects of nutritional supplementation with milk fat globule membrane on physical and muscle function in healthy adults aged 60 and over with semiweekly light exercise: a randomised double-blind, placebo-controlled pilot trial. J Nutr Sci Vitaminol (tokyo) 62:409–415
Mitchell CJ, Oikawa SY, Ogborn DI, Nates NJ, Macneil LG, Tarnopolsky M, Phillips SM (2015) Daily chocolate milk consumption does not enhance the effect of resistance training in young and old men: a randomised controlled trial. Appl Physiol Nutr Metab 40:199–202
Moran J, Guinan E, McCormick P, Larkin J, Mockler D, Hussey J, Moriarty J, Wilson F (2016) The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: a systematic review and meta-analysis. Surgery 160:1189–1201
Morley JE (2017) Hormones and Sarcopenia. Curr Pharm Des 23:4484–4492
Morley JE (2018) Treatment of sarcopenia: the road to the future. J Cachexia Sarcopenia Muscle 9:1196–1199
Morley JE, Argiles JM, Evans WJ, Bhasin S, Cella D, Deutz NE, Doehner W, Fearon KC, Ferrucci L, Hellerstein MK, Kalantar-Zadeh K, Lochs H, Macdonald N, Mulligan K, Muscaritoli M, Ponikowski P, Posthauer ME, Rossi Fanelli F, Schambelan M, Schols AM, Schuster MW, Anker SD (2010) Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc 11:391–396
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J, Fried LP, Guralnik JM, Katz PR, Malmstrom TK, McCarter RJ, Gutierrez Robledo LM, Rockwood K, Von Haehling S, Vandewoude MF, Walston J (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14:392–397
Nilwik R, Snijders T, Leenders M, Groen BB, van Kranenburg J, Verdijk LB, van Loon LJ (2013) The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol 48:492–498
Phillips SM (2012) Nutrient-rich meat proteins in offsetting age-related muscle loss. Meat Sci 92:174–178
Phu S, Boersma D, Duque G (2015) Exercise and sarcopenia. J Clin Densitom 18:488–492
Pollack RM, Barzilai N, Anghel V, Kulkarni AS, Golden A, O’Broin P, Sinclair DA, Bonkowski MS, Coleville AJ, Powell D, Kim S, Moaddel R, Stein D, Zhang K, Hawkins M, Crandall JP (2017) Resveratrol improves vascular function and mitochondrial number but not glucose metabolism in older adults. J Gerontol A Biol Sci Med Sci 72:1703–1709
Power L, Mullally D, Gibney ER, Clarke M, Visser M, Volkert D, Bardon, L, de Van der Schueren MAE, Corish CA (2018) A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings – A MaNuEL study. Clinical Nutrition ESPEN 24:1–13
Pyka G, Lindenberger E, Charette S, Marcus R (1994) Muscle strength and fiber adaptations to a year-long resistance training program in elderly men and women. J Gerontol 49:M22–M27
Rajman L, Chwalek K, Sinclair DA (2018) Therapeutic potential of NAD-boosting molecules: the in vivo evidence. Cell Metab 27:529–547
Rattan SI (2008) Hormesis in aging. Ageing Res Rev 7:63–78
Reid KF, Pasha E, Doros G, Clark DJ, Patten C, Phillips EM, Frontera WR, Fielding RA (2014) Longitudinal decline of lower extremity muscle power in healthy and mobility-limited older adults: influence of muscle mass, strength, composition, neuromuscular activation and single fiber contractile properties. Eur J Appl Physiol 114:29–39
Rodacki CL, Rodacki AL, Pereira G, Naliwaiko K, Coelho I, Pequito D, Fernandes LC (2012) Fish-oil supplementation enhances the effects of strength training in elderly women. Am J Clin Nutr 95:428–436
Rondanelli M, Rigon C, Perna S, Gasparri C, Iannello G, Akber R, Alalwan T , Freije Afnan M (2020) Novel insights on intake of fish and prevention of sarcopenia: all reasons for an adequate consumption. Nutrients 12(2):307
Rozand V, Sundberg CW, Hunter SK, Smith AE (2020) Age-related deficits in voluntary activation: a systematic review and meta-analysis. Med Sci Sports Exerc 52:549–560
Salucci S, Falcieri E (2020) Polyphenols and their potential role in preventing skeletal muscle atrophy. Nutr Res 74:10–22
Santanasto AJ, Coen PM, Glynn NW, Conley KE, Jubrias SA, Amati F, Strotmeyer ES, Boudreau RM, Goodpaster BH, Newman AB (2016) The relationship between mitochondrial function and walking performance in older adults with a wide range of physical function. Exp Gerontol 81:1–7
Schaap LA, Koster A, Visser M (2013) Adiposity, muscle mass, and muscle strength in relation to functional decline in older persons. Epidemiol Rev 35:51–65
Schafer AL, Vittinghoff E, Lang TF, Sellmeyer DE, Harris TB, Kanaya AM, Strotmeyer ES, Cawthon PM, Cummings SR, Tylavsky FA, Scherzinger AL, Schwartz AV (2010) Fat infiltration of muscle, diabetes, and clinical fracture risk in older adults. J Clin Endocrinol Metab 95:E368–E372
Schiaffino S (2010) Fibre types in skeletal muscle: a personal account. Acta Physiol (oxf) 199:451–463
Schiaffino S, Reggiani C (2011) Fiber types in mammalian skeletal muscles. Physiol Rev 91:1447–1531
Schilp J, Kruizenga HM, Wijnhoven HA, Leistra E, Evers AM, van Binsbergen JJ, Deeg DJ, Visser M (2012) High prevalence of undernutrition in Dutch community-dwelling older individuals. Nutrition 28:1151–1156
Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R (2017) Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord 16:21
Shahar DR, Houston DK, Hue TF, Lee J-S, Sahyoun NR, Tylavsky FA, Geva D, Vardi H, Harris TB (2012) Adherence to mediterranean diet and decline in walking speed over 8 years in community-dwelling older adults. J Am Geriatr Soc 60:1881–1888
Sipila S, Elorinne M, Alen M, Suominen H, Kovanen V (1997) Effects of strength and endurance training on muscle fibre characteristics in elderly women. Clin Physiol 17:459–474
Slivka D, Raue U, Hollon C, Minchev K, Trappe S (2008) Single muscle fiber adaptations to resistance training in old (>80 yr) men: evidence for limited skeletal muscle plasticity. Am J Physiol Regul Integr Comp Physiol 295:R273–R280
Smith GI, Atherton P, Reeds DN, Mohammed BS, Rankin D, Rennie MJ, Mittendorfer B (2011) Dietary omega-3 fatty acid supplementation increases the rate of muscle protein synthesis in older adults: a randomised controlled trial. Am J Clin Nutr 93:402–412
Snijders T, Nederveen JP, Bell KE, Lau SW, Mazara N, Kumbhare DA, Phillips SM, Parise G (2019) Prolonged exercise training improves the acute type II muscle fibre satellite cell response in healthy older men. J Physiol 597:105–119
Son SM, Park SJ, Lee H, Siddiqi F, Lee JE, Menzies FM, Rubinsztein DC (2019) Leucine signals to mTORC1 via its metabolite acetyl-coenzyme A. Cell Metab 29:192-201.e7
Soumare A, Elbaz A, Ducros V, Tavernier B, Alperovitch A, Tzourio C (2006) Cross-sectional association between homocysteine and motor function in the elderly. Neurology 67:985–990
Soumaré A, Elbaz A, Ducros V, Tavernier B, Alpérovitch A, Tzourio C (2006) Cross-sectional association between homocysteine and motor function in the elderly. Neurology 67:985–990
Stout JR, Sue Graves B, Cramer JT, Goldstein ER, Costa PB, Smith AE, Walter AA (2007) Effects of creatine supplementation on the onset of neuromuscular fatigue threshold and muscle strength in elderly men and women (64–86 years). J Nutr Health Aging 11:459–464
Strandberg E, Ponsot E, Piehl-Aulin K, Falk G, Kadi F (2019) Resistance training alone or combined with N-3 PUFA-rich diet in older women: effects on muscle fiber hypertrophy. J Gerontol A Biol Sci Med Sci 74:489–494
Struijk EA, Lana A, Guallar-Castillon P, Rodriguez-Artalejo F, Lopez-Garcia E (2018) Intake of B vitamins and impairment in physical function in older adults. Clin Nutr 37:1271–1278
Suetta C, Andersen JL, Dalgas U, Berget J, Koskinen S, Aagaard P, Magnusson SP, Kjaer M (2008) Resistance training induces qualitative changes in muscle morphology, muscle architecture, and muscle function in elderly postoperative patients. J Appl Physiol 1985(105):180–186
Sun N, Youle RJ, Finkel T (2016) The mitochondrial basis of aging. Mol Cell 61:654–666
Taaffe DR, Pruitt L, Pyka G, Guido D, Marcus R (1996) Comparative effects of high- and low-intensity resistance training on thigh muscle strength, fiber area, and tissue composition in elderly women. Clin Physiol 16:381–392
Talbot J, Maves L (2016) Skeletal muscle fiber type: using insights from muscle developmental biology to dissect targets for susceptibility and resistance to muscle disease. Wiley Interdiscip Rev Dev Biol 5:518–534
Tang JE, Moore DR, Kujbida GW, Tarnopolsky MA, Phillips SM (2009) Ingestion of whey hydrolysate, casein, or soy protein isolate: effects on mixed muscle protein synthesis at rest and following resistance exercise in young men. J Appl Physiol 107:987–992
Taub PR, Ramirez-Sanchez I, Patel M, Higginbotham E, Moreno-Ulloa A, Roman-Pintos LM, Phillips P, Perkins G, Ceballos G, Villarreal F (2016) Beneficial effects of dark chocolate on exercise capacity in sedentary subjects: underlying mechanisms. A double blind, randomised, placebo controlled trial. Food Funct 7:3686–3693
Tieland M, Karin J, den Berg BV, van Loon Luc JC, de Groot Lisette CPGM (2012a) Dietary protein intake in community-dwelling, frail, and institutionalized elderly people: scope for improvement. Eur J Nutr 51(2):173–179
Tieland M, Dirks ML, van der Zwaluw N, Verdijk LB, van de Rest O, de Groot LC, van Loon LJ (2012b) Protein supplementation increases muscle mass gain during prolonged resistance-type exercise training in frail elderly people: a randomised, double-blind, placebo-controlled trial. J Am Med Dir Assoc 13:713–719
Tieland M, van de Rest O, Dirks ML, van der Zwaluw N, Mensink M, van Loon LJ, de Groot LC (2012c) Protein supplementation improves physical performance in frail elderly people: a randomised, double-blind, placebo-controlled trial. J Am Med Dir Assoc 13:720–726
Tipton KD, Ferrando AA, Phillips SM, Doyle D, JR (1999) Postexercise net protein synthesis in human muscle from orally administered amino acids. Am J Physiol 276:E628–E634
Tong TYN, Appleby PN, Armstrong MEG, Fensom GK, Knuppel A, Papier K, Perez-Cornago A, Travis RC, Key TJ (2020) Vegetarian and vegan diets and risks of total and site-specific fractures: results from the prospective EPIC-Oxford study. BMC Med 18:353
Trappe S, Godard M, Gallagher P, Carroll C, Rowden G, Porter D (2001) Resistance training improves single muscle fiber contractile function in older women. Am J Physiol Cell Physiol 281:C398-406
Trappe S, Williamson D, Godard M, Porter D, Rowden G, Costill D (2000) Effect of resistance training on single muscle fiber contractile function in older men. J Appl Physiol 1985(89):143–152
Tsekoura M, Kastrinis A, Katsoulaki M, Billis E, Gliatis J (2017) Sarcopenia and its impact on quality of life. Adv Exp Med Biol 987:213–218
Vaes AMM, Tieland M, Toussaint N, Nilwik R, Verdijk LB, van Loon LJC, de Groot L (2018) Cholecalciferol or 25-hydroxycholecalciferol supplementation does not affect muscle strength and physical performance in prefrail and frail older adults. J Nutr 148:712–720
van Dongen EJ, Leerlooijer JN, Steijns JM, Tieland M, de Groot LC, Haveman-Nies A (2017) Translation of a tailored nutrition and resistance exercise intervention for elderly people to a real-life setting: adaptation process and pilot study. BMC Geriatr 17:25
Van Dongen EJI (2019) Dietary protein and resistance exercise training for community-dwelling older adults : intervention adaptation, implementation and effectiveness. Wageningen University
van Dongen EJI, Haveman-Nies A, Doets EL, Dorhout BG, de Groot LCPGM (2020) Effectiveness of a diet and resistance exercise intervention on muscle health in older adults: promuscle in practice. J Am Med Dir Assoc 21:1065-1072.e3
van Schoor NM, Swart KM, Pluijm SM, Visser M, Simsek S, Smulders Y, Lips P (2012) Cross-sectional and longitudinal association between homocysteine, vitamin B12 and physical performance in older persons. Eur J Clin Nutr 66:174–181
Veeranki S, Tyagi SC (2013) Defective homocysteine metabolism: potential implications for skeletal muscle malfunction. Int J Mol Sci 14:15074–15091
Verdijk LB, Snijders T, Beelen M, Savelberg HH, Meijer K, Kuipers H, van Loon LJ (2010) Characteristics of muscle fiber type are predictive of skeletal muscle mass and strength in elderly men. J Am Geriatr Soc 58:2069–2075
Verdijk LB, Snijders T, Drost M, Delhaas T, Kadi F, van Loon LJ (2014) Satellite cells in human skeletal muscle; from birth to old age. Age (dordr) 36:545–547
Verstraeten LMG, van Wijngaarden JP, Pacifico J, Reijnierse EM, Meskers CGM, Maier AB (2021) Association between malnutrition and stages of sarcopenia in geriatric rehabilitation inpatients: Resort. Clin Nutr
Vidoni ML, Pettee Gabriel K, Luo ST, Simonsick EM, Day RS (2017) Vitamin B12 and homocysteine associations with gait speed in older adults: the baltimore longitudinal study of aging. J Nutr Health Aging 21:1321–1328
Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, Simonsick EM, Harris TB (2005) Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci 60:324–333
Wade S, Strader C, Fitzpatrick L, Anthony M, O’Malley C (2014) Estimating prevalence of osteoporosis: examples from industrialised countries. Arch Osteoporos 9:1–10
Wesselink E, Koekkoek WAC, Grefte S, Witkamp RF, van Zanten ARH (2019) Feeding mitochondria: potential role of nutritional components to improve critical illness convalescence. Clin Nutr 38:982–995
Wilkinson SB, Tarnopolsky MA, Macdonald MJ, Macdonald JR, Armstrong D, Philips SM (2007) Consumption of fluid skim milk promotes greater muscle protein accretion after resistance exercise than does consumption of an isonitrogenous and isoenergetic soy-protein beverage. Am J Clin Nutr 85:1031–1040
Wilson JM, Loenneke JP, Jo E, Wilson GJ, Zourdos MC, Kim JS (2012) The effects of endurance, strength, and power training on muscle fiber type shifting. J Strength Cond Res 26:1724–1729
Yamada M, Kimura Y, Ishiyama D, Nishio N, Otobe Y, Tanaka T, Ohji S, Koyama S, Sato A, Suzuki M, Ogawa H, Ichikawa T, Ito D, Arai H (2019) Synergistic effect of bodyweight resistance exercise and protein supplementation on skeletal muscle in sarcopenic or dynapenic older adults. Geriatr Gerontol Int 19:429–437
Yang Y, Churchward-Venne TA, Burd NA, Breen L, Tarnopolsky MA, Phillips SM (2012) Myofibrillar protein synthesis following ingestion of soy protein isolate at rest and after resistance exercise in elderly men. Nutr Metab 9
Zhao JG, Zeng XT, Wang J, Liu L (2017) Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: a systematic review and meta-analysis. JAMA 318:2466–2482
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
Conflict of Interest
All authors declare they have no conflict of interest.
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Grootswagers, P., Mensink, M., de Groot, L. (2021). Nutrition and Exercise to Maintain Physical Functioning During Ageing. In: Rattan, S.I.S., Kaur, G. (eds) Nutrition, Food and Diet in Ageing and Longevity. Healthy Ageing and Longevity, vol 14. Springer, Cham. https://doi.org/10.1007/978-3-030-83017-5_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-83017-5_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-83016-8
Online ISBN: 978-3-030-83017-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)