Abstract
Transcranial Doppler (TCD/TCCS) is very useful to establish the diagnosis of cerebral circulatory arrest that accompanies brain death. A complete TCD/TCCS study to establish the diagnosis of cerebral circulatory arrest requires a complete study of the anterior and posterior cerebral circulation. There are three sonographic patterns compatible with the diagnosis of cerebral circulatory arrest: diastole-systole separation, reverberant flow, and isolated systolic spikes. The absence of blood flow velocities’ insonation in patients who had previously been insonated is considered by some to be compatible with the diagnosis of cerebral circulatory arrest. Transcranial Doppler has its main limitation of use in patients in whom there are closed-vault defects.
Instrumental tests for the determination of brain death (including TCD/TCCS) have their main indication when the concept of whole brain death (WBD) is being used or the clinical diagnosis (clinical examination / apnea test) is incomplete.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Transcranial Doppler sonography
- Brain death
- Cerebral circulatory arrest
- Brain death determination
- Reverberant blood flow
- Systolic spikes
-
1.
To determine brain death, a patient has to have suffered a medically and surgically irreversible structural brain injury.
-
2.
Transcranial Doppler is very useful to support the diagnosis of cerebral circulatory arrest that accompanies the determination of Death by Neurological Criteria (DNC).
-
3.
In order to establish the diagnosis of cerebral circulatory arrest by means of TCD/TCCS, we must contemplate the study of the anterior and posterior cerebral circulation.
-
4.
There are three sonographic patterns compatible with the diagnosis of cerebral circulatory arrest: a) diastole-systole separation pattern, b) reverberant blood flow velocity pattern, and c) isolated systolic spike pattern. The absence of insonation in patients who had previously been insonated is considered by some to be compatible with the diagnosis of cerebral circulatory arrest.
-
5.
Transcranial Doppler (TCD), like other auxiliary studies that estimate cerebral blood flow through blood flow velocities, has its main limitation in patients in whom there is no cranial hermetism (craniectomy, external ventricular drain, etc.).
-
6.
Ancillary tests for the DNC (including Transcranial Doppler) have their main indication when the concept of global brain death is being used or it is not possible to complete the neurological examination and/or apnea test.
1 Introduction
Defining and determining death as the loss of circulatory-respiratory or cardiopulmonary function enjoys near-universal acceptance, across cultures and religious traditions. A more recent way of defining and determining death (brain death or Death by Neurological Criteria) has a fairly broad international acceptance as a medically valid and legal way to determine and define death, but there is a lack of international consensus about what diagnostic criteria are appropriate.
In 1968, from the Ad Hoc Committee of the Harvard Medical School, the concept of “brain death” was born [1], although this term probably tries to define “the death of the person based on neurological criteria.” In 2010, the American Academy of Neurology (AAN) updated a practice guideline to outline the necessary examination to evaluate a patient for brain death.
The diagnosis of brain death is one of the most important and relevant tasks to intensive care unit (ICU) physicians following severe brain injury. In order to determine Death by Neurological Criteria (DCN), a patient has to have suffered a medically and surgically irreversible structural brain injury.
2 Concepts of Death by Neurological Criteria (DNC)
There are currently three main concepts of death based on neurological criteria. This translates into three different concepts of brain death: a) global brain death, b) brainstem death, and c) neocortical death.
2.1 Whole Brain Death
Whole brain death (WBD) is the standard for determining death used in the United States and most European countries. WBD is defined as the irreversible cessation of all functions of the entire brain, including the brain stem, except the spinal cord. In order to establish this diagnosis, a clinical examination must be carried out to demonstrate the absence of brainstem activity, as well as an instrumental test that demonstrates the existence of some of the brain phenomena associated with brain death (cessation of brain bioelectrical activity, cerebral circulatory arrest). Global encephalic death occurs either in supratentorial processes in which a face-flow deterioration is produced or in posterior fossa processes that initially produce a deterioration in the activity of the brain stem that follows a complete and irreversible cessation of brain activity.
2.2 Brainstem Death
Brainstem death is the standard for neurological death used in Canada, India, and the United Kingdom. Brainstem death is the irreversible loss of the capacity for consciousness combined with the irreversible loss of the capacity to breathe. It is based on proving the irreversible absence of the brainstem function. The diagnosis of brainstem death is based on the clinical examination [2]. In order to establish this diagnosis, it is not necessary to prove the absence of brain functions, so it is not necessary to perform instrumental tests. Brainstem death may occur as a consequence of the facial-caudal deterioration due to supratentorial lesions, although it may also occur as a consequence of primary lesions of the cerebellum and brain stem culminating in a complete cessation of the brain activity, without requiring rostral-caudal deterioration with involvement of the supratentorial structures.
2.3 Neocortical Death
It is based on the fact that the content of consciousness is the key defining element of human life [3]. Therefore, in those circumstances in which there is a complete and irreversible absence of the content of the consciousness, the diagnosis of death could be established based on neurological criteria. A clinical state equivalent to neocortical death would be the situation of a permanent vegetative state with apathetic syndrome.
Of the three concepts mentioned, the most developed at present are: the concept of global encephalic death and the concept of brainstem death.
3 Determination of Death by Neurological Criteria (DNC)
When the concept of whole brain death is used, the diagnosis of brain death is based on the demonstration of the irreversible absence of neurological activity of the central nervous system, except for the spinal cord, as well as the demonstration of some of the intracranial phenomena closely associated with brain death, such as the cessation of brain bioelectrical activity or cerebral circulatory arrest.
To establish the irreversible absence of central nervous system functions, a complete clinical examination of the neurological functions with an anatomical substrate in the brain stem is essential.
These criteria apply to adults only in the context of the primary principles:
-
1.
Determination of structural and irreversible cause of brain injury.
-
2.
Determination of the medical and surgical futility.
-
3.
Exclude confounders.
-
4.
Determination of the brainstem reflexes.
-
5.
Test of apnea.
Prior to the complete diagnosis of brain death, it is necessary to rule out the presence of factors that could confuse the diagnosis and thus fulfill certain prerequisites, among which are arterial hypotension, severely induced hypothermia, the effects of muscle relaxant drugs or central nervous system depressant drugs, and electrolyte disorders. All these factors must be corrected before beginning the clinical and/or auxiliary diagnosis.
In order to establish the diagnosis of brain death, the complete and irreversible absence of brainstem activity must be confirmed. This requires a complete clinical examination of the brain stem, which should include the presence or absence of the following brainstem reflexes:
All components of the examination must be tested after all confounders have been excluded.
-
1.
Photomotor reflex (absence of pupillary response in both eyes).
-
2.
Corneal reflex.
-
3.
Occulocephalic reflex.
-
4.
Occulovestibular reflex.
-
5.
Absence of facial muscle movements to a noxious stimulus.
-
6.
Absence of pharyngeal and tracheal reflex:
-
1.
Absence of the gag reflex.
-
2.
Absence of cough response.
-
1.
It is also necessary to demonstrate the absence of ventilatory activity by means of the apnea test. Stimulation of the respiratory center should be performed by increasing carbon dioxide (CO2) levels to more than 20 mmHg (arterial blood) above the patient’s baseline values [4,5,6].
When the concept of death is used by Neurological Criteria based on the irreversible absence of brainstem activity (brainstem death), it is only necessary to confirm the absence of clinical activity by means of a complete clinical examination of the brain stem, and it is not necessary to prove the existence of other intracranial phenomena associated with brainstem death, since these refer fundamentally to supratentorial phenomena, which are essentially brain based.
When, on the contrary, we are using the concept of global encephalic death, it is necessary not only to carry out a complete clinical examination that demonstrates the absence of activity of the encephalic trunk, but it is also necessary to confirm the absence of brain activity. At this point, since the brain stem has no activity, it is not possible by clinical methods to access knowledge of brain function, so it is essential to use auxiliary methods that explore the phenomena associated with brain death.
4 Intracranial Phenomena and Death by Neurological Criteria
The mechanism most frequently involved in the development of brain death (although not the only one) is intracranial hypertension, which causes the cessation of intracranial circulation. As a consequence of this, a global encephalic ischemia is produced, with underlying metabolic disorders that compromise neurotransmission (more edema and more intracranial hypertension), to later produce an irreversible global brain damage. That is why as phenomena intimately associated with encephalic death (especially when the concept of global encephalic death is used), there is the cessation of intracranial circulation as the main actor, the cessation of brain bioelectrical activity, and the development of profound metabolic disorders due to the resulting ischemic-anoxic process.
Cerebral circulatory arrest, one of the phenomena most frequently associated with brain death, is sometimes the mechanism generating brain death, while on other occasions it is a consequence of it. Thus, in primary vascular processes, such as occlusion of the large arteries at the base of the skull, brain death occurs as a consequence of global brain ischemia. In other cases, the existence of large space-occupying lesions or a large cerebral edema is responsible for the cessation of intracranial circulation. In these patients, the increase in intracranial pressure, equal to the average blood pressure, makes the cerebral perfusion insufficient to meet the encephalic metabolic needs, and consequently triggers, irreversibly, the cessation of all central nervous system functions.
Cerebral circulatory arrest is a progressive phenomenon, not an instantaneous one. It is also often asymmetrical when the phenomenon is compared in the two cerebral hemispheres. Depending on the mechanism of cessation of circulation, an asymmetry of circulatory arrest can also be observed in the period before brain death is established when supratentorial regions are compared with infratentorial regions.
Therefore, it is important to remember that TCD (in the dynamic evaluation of cerebral hemodynamics) is based on the phenomenon of recording systolic patterns in intracranial arteries (circle of Willis) without evidence of diastolic flow to determine a pattern of cessation in cerebral circulation.
5 Transcranial Doppler (TCD): Utility and Prerequisites
Before using the TCD as an ancillary test for DNC diagnosis, the following prerequisites must be present:
-
1.
Coma with a known cause that is irreversible.
-
2.
Imaging that explains the comatose state.
-
3.
Absence of spontaneous respirations.
-
4.
Exclusion: Hypothermia, major correctable metabolic or endocrine disturbance, toxics, sedative medications, neuromuscular blocking agents.
-
5.
Achievement of normal systolic blood pressure.
5.1 Preliminary Clinical Examination
Given that a complete clinical examination of the brain stem is essential for the diagnosis of brain death, evidencing the absence of brain activity, it is recommended that a clinical examination be performed prior to the use of Doppler. The use of Doppler would not make sense if clinical data of brainstem activity still persist, since in no case could the diagnosis of death be made.
The diagnostic accuracy of transcranial Doppler for brain death has not been confirmed in all settings [7].
5.2 Intracranial Pressure Stability
The stability of the intracranial pressure is also an essential element for the diagnosis, since it is possible to observe, in a transitory way, phenomena of cerebral circulatory arrest coinciding with intracranial hypertension waves which give way when these hypertension waves are controlled. It is true that on many occasions, stable and maintained intracranial hypertension accompanies brain death, and on many instances, this is the main physiopathological mechanism that generates it [8].
6 TCD as Ancillary Test: Determination of Cerebral Circulatory Arrest in DNC
If a clinical examination with apnea test is consistent with brain death, an ancillary test is not required. The insonation of the blood flow velocities in cerebral basal arteries (circle of Willis) for determination of brain death does not differ initially from the TCD insonation techniques described for other pathologies:
-
1.
Probe:
Low-frequency probe (2 MHz).
-
2.
Initial acoustic window:
Transtemporal window (bilateral)
-
3.
Insonation depth:
Middle cerebral artery (MCA) is between 45–65 mm and 70–100 mm for the basilar artery (BA). The depth will be shallower (30–50 mm) when performing sounding [9, 10] in children. It is important to take into consideration the depth at which the scan is performed, the direction and sense of the signal detected, and also the response of the sounded artery to the compression maneuvers of the carotid arteries at neck level.
However, for the diagnosis of cerebral circulatory arrest in order to establish the diagnosis of DNC, it is essential to take into consideration a series of prerequisites that will avoid the misinterpretation of the results (blood flow velocities and spectral Doppler waveform) from the TCD. It is also necessary to take into account some specific technical strategies in the case of cerebral circulatory arrest, since in certain circumstances the insonation of intracranial arteries in patients where intracerebral flow has ceased requires alternatives to standard insonation techniques [11].
When ancillary test is utilized, only one test is required for the determination of DNC.
7 TCD: Sonography Patterns of Cerebral Circulatory Arrest and DNC
The diagnosis of cerebral circulatory arrest through TCD is supported by the appearance of at least one blood flow velocity pattern characteristic of cerebral circulatory arrest in all insonated intracranial vessels [12, 13]. It is important to note that although these patterns are usually associated with increased pulsatility index, and increased resistance index, these values are not really relevant for diagnosis. It is important to consider the trends in the flow patterns of the circle of Willis. The most important aspect for the diagnosis of cerebral circulatory arrest is the existence of zero blood flow velocity at the end of the diastole (absence of flow at the end of the diastole in spectral Doppler wave). In the telediastolic period, in a situation of circulatory arrest, no blood enters into the brain, so the cerebral perfusion pressure (CPP) is abolished.
7.1 Description of the Sonographic Patterns
The use of the TCD has allowed us to verify how the cessation of cerebral circulation until brain death is a process that begins (especially in supratentorial pathology that occurs with endocranial hypertension) with a progressive decrease in the diastolic blood flow velocity. This is followed by a separation of the diastolic wave (at the end of the diastole) and the systolic wave, an inversion of the diastolic blood flow velocity wave (reverberant flow), and a disappearance of the diastolic velocity wave with persistence only of the systolic spike (CPP ≈ zero) [14].
7.1.1 The Diastole-Systole Separation Blood Flow Pattern (Fig.39.1)
It is characterized by the absence of positive blood flow velocity (flow to the probe) at the end of the diastole. This pattern is the least frequent of the three patterns compatible with circulatory arrest, is usually of short duration, and represents the beginning of the cessation of arterial circulation in the vessel examined.
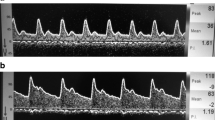
7.1.2 The Reverberant Blood Flow Pattern (Figs. 39.2, 39.3, and 39.4)
It is characterized by the presence of a retrograde blood flow velocity (moving away from the tube) in the diastolic period. It represents retrograde blood flow with no effective diastole (increased brain impedance) preventing adequate CPP. It is usually a pattern that precedes the isolated systolic spike pattern.
7.1.3 The Systolic Spike Blood Flow Pattern (Fig. 39.5)
It is characterized by the existence of antegrade cerebral blood flow velocity (CBFV) (which is directed toward the probe) during the systolic phase, with the absence of diastolic blood flow velocity (end-diastolic volume (EDV)). (CPP ≈ zero). This pattern represents the final hemodynamic stage of cerebral circulatory arrest.
Several hours, or days, after circulatory arrest is established, it is often impossible to insulate the arteries at the base of the skull in any period of the circulatory cycle. However, the absence of flow in a patient in whom flow had previously been recorded is considered by some groups to be a sonographic finding compatible with the diagnosis of brain death.
To complete the diagnosis of cerebral circulatory arrest, it is necessary that all intracranial vessels have one of the three blood flow velocity patterns compatible with circulatory arrest [15]. It is not necessary for the establishment of the diagnosis of circulatory arrest that all the sonographic patterns are similar in the insonated arteries.
There is no standard recording duration for each of the arteries, although some authors recommend a recording duration of 30 seconds. However, what is really important is that the blood pressure is normalized and the intracranial pressure stabilized, avoiding recording during transient elevations of intracranial pressure [16].
8 Transcranial Doppler and Death by Neurological Criteria: Some Limitations
There are several situations that must be considered when using Transcranial Doppler as an ancillary test:
8.1 Transient Cerebral Circulatory Arrest
Cerebral circulatory arrest is the pathophysiological result of an interaction between mean blood pressure (mean arterial pressure (MAP)) and intracranial pressure (ICP), variables that define CPP, in a closed compartment such as the skull. Under certain circumstances, for example, severe arterial hypotension or the presence of transient increases in intracranial pressure (Lundberg waves) [17, 18], a phenomenon of transient cerebral circulatory arrest may occur, which can be demonstrated by means of Transcranial Doppler and which only shows the interrelationship between mean arterial pressure and pressure within the intracranial compartment, this being neither a situation of irreversible cerebral circulatory arrest nor a false positive of TCD in the diagnosis of brain death.
8.2 Cerebral Circulatory Arrest Is Not Synonymous with Brain Death
It is important to note that no single instrumental test is sufficient, by itself, to establish the diagnosis of brain death. The absence of cerebral blood flow velocities and the absence of cerebral bioelectrical activity are phenomena intimately associated with brain death. However, none of these phenomena are synonymous with brain death. They must be supported by a complete clinical examination that explores and evidences the absence of brainstem activity. Currently, there is no instrumental test that is synonymous with brain death that can replace the clinical diagnosis used to establish the diagnosis of brain death.
8.3 Patients with Primary Injury Limited to the Brain Stem
In some cases of patients in whom the neurological impairment is not face-flow, but ascending (the initial neurological damage occurs in the posterior fossa), it is possible to observe the persistence of blood flow velocities at the level of the anterior circulation in patients who meet clinical criteria for brain death. This is due to the absence of intracranial hypertension in the supratentorial territory, and should not be interpreted as a false negative of ultrasound diagnosis but as an inadequate interpretation and indication of the TCD ; conceptually, when the concept of brainstem death is used it is not necessary to demonstrate the absence of supratentorial activity.
8.4 Closed-Vault Defects
The existence of a defect in the skull (fractures, hemi-craniectomy, etc.) may cause the normal balance between intracranial and extracranial pressures to be modified; this may influence the results of the instrumental tests used for the diagnosis of brain death, especially those that indirectly explore the cerebral blood flow (or blood flow velocities), causing them to lose diagnostic accuracy.
Flowers et al. [19] determine as possible causes of persistent cerebral blood flow accompanying the situation of brain death:
-
1.
External or internal drains of the cerebrospinal fluid (CSF).
-
2.
Decompressive craniectomies.
-
3.
Large fractures of the base of the skull.
-
4.
In children, the existence of open fontanelles.
Therefore, in these circumstances the use of tests that attempt to estimate brain blood flow, such as TCD by blood flow velocities’ measurement, may determine a false negative result for the diagnosis of brain death and the diagnosis of brain death should not be excluded. Ancillary tests that measure other physiological variables associated with brain death, such as brain electrical activity , are suggested [10, 20].
9 TCD and DNC: Technical Difficulties
There are some clinical situations in which TCD insonation for the diagnosis of brain death is especially difficult:
9.1 Elderly Women
In this cohort of patients, in addition to the difficulties inherent in insonation for brain death, there is also the difficulty of finding an appropriate acoustic window, in the general population, there will be 15–20% of patients who will not have an adequate transtemporal acoustic window.
9.2 Inadequate Hemodynamic and Intracranial Conditions
For reliable TCD insonation, optimization of the patient’s blood pressure and intracranial pressure is important. A TCD study to complement the brain death study should not be performed if the patient does not have an optimized systemic blood pressure.
It is also important to avoid performing studies during transitory elevations of intracranial pressure (Lundberg waves), since with these it is possible to have a transitory cerebral circulatory arrest in the cerebral artery with reversible cessation of cerebral blood flow velocities.
10 TCD and DNC: Technical Issues to Consider
When performing TCD for the support of diagnosis of brain death, in addition to the limitations mentioned above, certain technical aspects of the equipment used should be taken into account that will not only facilitate insonation but also increase the diagnostic accuracy of the technique.
10.1 Filter Control
When a TCD is performed in order to establish the persistence or absence of diastolic blood flow velocity, a key element in the diagnosis of cerebral circulatory arrest, it is important to avoid the existence of a phenomenon such as signal hyperfiltration. When high filter levels are used, it is possible not to detect the existence of the diastolic blood flow (in the case that it is low) because it is masked by the filtering of the equipment.
10.2 Optimization of the Power Ultrasound Beam
During the diagnosis of brain death by TCD, it is important to increase the diagnostic sensitivity of the test to the maximum. To do this, and especially in those patients with a difficult acoustic window, it is advisable to increase the power of the ultrasound beam during the first phase of the test until the sonographic location of the artery is made, and the power can be decreased once the artery is located, and until the best quality of insonation is achieved.
10.3 Orbital Acoustic Window
In cases where it is impossible to sound the arteries of the anterior circulation through the temporal window, the use of the orbital window is suggested in order to establish the absence of blood flow velocities at the level of the carotid artery [21, 22]. To do this, the standardized rules for insonation of the carotid artery through this acoustic window must be followed, and the optimization of the sample volume is important in order to isolate, from a sonographic point of view, the different sections of the carotid siphon. The absence of telediastolic blood flow velocity at the level of both carotid siphons suggests the absence of blood flow in anterior circulation.
11 Transcranial Doppler in the Diagnosis of Brain Death: Evidence
According to the Task Force Group on Cerebral Death of the Neurosonology Research Group of the World Federation of Neurology, transcranial Doppler is a reliable method for the diagnosis of brain death [15].
The transcranial Doppler technique has been used for the diagnosis of brain death for more than 20 years [23]. In general, the sensitivity and specificity of the technique for brain death ranges from 91 to 100% and 97 to 100%, respectively [24,25,26,27].
In a systematic review of 859 patients [28] (56.1% of whom had confirmed brain death using clinical criteria), the diagnostic sensitivity of transcranial Doppler was 0.90 (95% CI.0.87–0.92) and the overall specificity was 0.98 (95% CI.0.96–0.99).
12 Transcranial Doppler in the Diagnosis of Brain Death: Advantages and Disadvantages
The use of TCD in the diagnosis of brain death has advantages and disadvantages over other techniques used for the same purpose.
12.1 Advantages
-
1.
It is performed at the patient’s bedside. Transcranial Doppler devices are portable.
-
2.
The TCD shows the cerebral circulatory arrest as a process. It is not uncommon to observe asynchronies in cerebral circulatory arrest in different intracranial territories. It is possible to see circulatory arrest in one hemisphere, without it having yet been completed in the contralateral; or circulatory arrest in supratentorial territory [29], without it having yet manifested itself in infratentorial territory.
In either case, it should be taken into account that to complete the diagnosis of brain death, by this auxiliary test, the absence of circulation in all intracranial arterial territories must be confirmed.
-
3.
It is a technique of simple interpretation. It is sufficient to observe the absence of telediastolic blood flow velocity in all intracranial territories (presence of some of the three sonographic patterns compatible with absence of blood flow velocity).
-
4.
It is a technique of easy replication. The technique can be performed repeatedly without the need to mobilize the patient outside the intensive care unit (ICU).
-
5.
Blood flow velocity rate measurements per se with the TCD are not interfered by central nervous system depressant drugs.
12.2 Disadvantages
-
1.
Possible existence of blood flow velocity rates by TCD in patients who are in a situation of brain death; that is to say, a “false negative” for the diagnosis of brain death. This may occur in cases of absence of cranial hermetism due to decompressive craniectomies, external or internal drainage of the cerebrospinal fluid, or large base fractures of the skull. These potential disadvantages are shared with other instrumental tests that analyze cerebral blood flow in similar circumstances.
-
2.
The absence of acoustic window. This is especially possible in older female patients, or in any patient where several days have elapsed since the cessation of intracranial arterial circulation. The use of the orbital window for carotid siphon insonation [21] may be a suitable option to overcome this problem when anterior circulation cannot be insonated through the transtemporal window.
-
3.
Dependence on the operator technique. There are no significant differences in sonographic findings between two operators adequately trained in TCD.
13 Conclusion
Transcranial Doppler is an extraordinarily useful technique to support the diagnosis of Death by Neurological Criteria (DNC). As other diagnostic techniques, it requires adequate operator training to be performed correctly.
In order to know the usefulness of the technique, its indication must be clearly established, and it must be fundamentally used in the diagnosis of brain death when the concept of whole brain death is being used. An adequate physiopathological knowledge of the intracranial phenomena associated with whole brain death helps to understand the sonographic expression of the circulatory arrest that accompanies brain death.
References
A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA. 1968;205(6):337–40.
Pallis C. ABC of brain stem death. Prognostic significance of a dead brain stem. Br Med J (Clin Res Ed). 1983;286(6359):123–4.
Brierley JB, Graham DI, Adams JH, Simpsom JA. Neocortical death after cardiac arrest. A clinical, neurophysiological, and neuropathological report of two cases. Lancet. 1971;2(7724):560–5.
Practice parameters for determining brain death in adults (summary statement). The Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1995;45(5):1012–4.
Dominguez-Roldan JM, Barrera-Chacon JM, Murillo-Cabezas F, Santamaria-Mifsut JL, Rivera-Fernandez V. Clinical factors influencing the increment of blood carbon dioxide during the apnea test for the diagnosis of brain death. Transplant Proc. 1999;31(6):2599–600.
Wijdicks EF, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74(23):1911–8.
Cestari M, Gobatto ALN, Hoshino M. Role and limitations of transcranial Doppler and brain death of patients on veno-arterial extracorporeal membrane oxygenation. ASAIO J. 2018;64(4):e78.
Li Y, Liu S, Xun F, Liu Z, Huang X. Use of transcranial Doppler ultrasound for diagnosis of brain death in patients with severe cerebral injury. Med Sci Monit. 2016;22:1910–5.
Lobo CL, Cancado RD, Leite AC, Dos Anjos AC, Pinto AC, Matta AP, et al. Brazilian Guidelines for transcranial doppler in children and adolescents with sickle cell disease. Rev Bras Hematol Hemoter. 2011;33(1):43–8.
Verlhac S. Transcranial Doppler in children. Pediatr Radiol. 2011;41 Suppl 1:S153–65.
Sloan MA, Alexandrov AV, Tegeler CH, Spencer MP, Caplan LR, Feldmann E, et al. Assessment: transcranial Doppler ultrasonography: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2004;62(9):1468–81.
Rajagopal R, Gupta A. Transcranial Doppler flow patterns in brain death: "Storm before the calm". Neurol India. 2017;65(3):671–2.
Hashemian SM, Delavarkasmaei H, Najafizadeh K, Mojtabae M, Ardehali SH, Kamranmanesh MR, et al. Role of transcranial Doppler sonography in diagnosis of brain death: a single center study. Tanaffos. 2016;15(4):213–7.
Dominguez-Roldan JM, Murillo-Cabezas F, Munoz-Sanchez A, Santamaria-Mifsut JL, Villen-Nieto J. Changes in the Doppler waveform of intracranial arteries in patients with brain-death status. Transplant Proc. 1995;27(4):2391–2.
Sharma D, Souter MJ, Moore AE, Lam AM. Clinical experience with transcranial Doppler ultrasonography as a confirmatory test for brain death: a retrospective analysis. Neurocrit Care. 2011;14(3):370–6.
Latin American consensus on the use of transcranial Doppler in the diagnosis of brain death. Rev Bras Ter Intensiva. 2014;26(3):240–52.
Kirkham FJ, Levin SD, Padayachee TS, Kyme MC, Neville BG, Gosling RG. Transcranial pulsed Doppler ultrasound findings in brain stem death. J Neurol Neurosurg Psychiatry. 1987;50(11):1504–13.
Steinmetz H, Hassler W. Reversible intracranial circulatory arrest in acute subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1988;51(10):1355–6.
Flowers WM Jr, Patel BR. Persistence of cerebral blood flow after brain death. South Med J. 2000;93(4):364–70.
Cabrer C, Dominguez-Roldan JM, Manyalich M, Trias E, Paredes D, Navarro A, et al. Persistence of intracranial diastolic flow in transcranial Doppler sonography exploration of patients in brain death. Transplant Proc. 2003;35(5):1642–3.
Dominguez-Roldan JM, Jimenez-Gonzalez PI, Garcia-Alfaro C, Rivera-Fernandez V, Hernandez-Hazanas F. Diagnosis of brain death by transcranial Doppler sonography: solutions for cases of difficult sonic windows. Transplant Proc. 2004;36(10):2896–7.
Algin O, Gundogdu G, Izdes S, Keles GE, Solaroglu I. Diagnosis of brain death by orbital Doppler ultrasound: a comparative research study. Turk Neurosurg. 2015;25(2):256–62.
Hadani M, Bruk B, Ram Z, Knoller N, Spiegelmann R, Segal E. Application of transcranial doppler ultrasonography for the diagnosis of brain death. Intensive Care Med. 1999;25(8):822–8.
Hassler W, Steinmetz H, Pirschel J. Transcranial Doppler study of intracranial circulatory arrest. J Neurosurg. 1989;71(2):195–201.
Zurynski Y, Dorsch N, Pearson I, Choong R. Transcranial Doppler ultrasound in brain death: experience in 140 patients. Neurol Res. 1991;13(4):248–52.
Hassler W, Steinmetz H, Gawlowski J. Transcranial Doppler ultrasonography in raised intracranial pressure and in intracranial circulatory arrest. J Neurosurg. 1988;68(5):745–51.
Petty GW, Mohr JP, Pedley TA, Tatemichi TK, Lennihan L, Duterte DI, et al. The role of transcranial Doppler in confirming brain death: sensitivity, specificity, and suggestions for performance and interpretation. Neurology. 1990;40(2):300–3.
Chang JJ, Tsivgoulis G, Katsanos AH, Malkoff MD, Alexandrov AV. Diagnostic accuracy of transcranial Doppler for brain death confirmation: systematic review and meta-analysis. AJNR Am J Neuroradiol. 2016;37(3):408–14.
Dominguez-Roldan JM, Garcia-Alfaro C, Jimenez-Gonzalez PI, Rivera-Fernandez V, Hernandez-Hazanas F, Perez-Bernal J. Brain death due to supratentorial masses: diagnosis using transcranial Doppler sonography. Transplant Proc. 2004;36(10):2898–900.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Algorithm
Algorithm

ABCD Airway-Breathing-Circulation-Disability, ABP Arterial blood pressure, EEG: Electroencephalogram, ICP Intracranial pressure, NMB Neuromuscular blockers, CCA Cerebral circulatory arrest, MCA Middle cerebral artery, BA Basilar artery, US Ultrasound
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Domínguez Roldán, J.M., Alfaro, C.G., de la Torre Gómez, R.E. (2022). Death by Neurological Criteria (DNC) in ICU: Usefulness of Transcranial Doppler (TCD). In: Rodríguez, C.N., et al. Neurosonology in Critical Care . Springer, Cham. https://doi.org/10.1007/978-3-030-81419-9_39
Download citation
DOI: https://doi.org/10.1007/978-3-030-81419-9_39
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-81418-2
Online ISBN: 978-3-030-81419-9
eBook Packages: MedicineMedicine (R0)