Abstract
Brain death is primarily a clinical diagnosis, but at times when examination cannot be completed or is uncertain, the ancillary tests need to be carried out. Ultrasonography used for detection of cerebral circulatory arrest has an advantage of being non-invasive, inexpensive, complication free and a quick technique. Transcranial Doppler (TCD), cervical colour Doppler and optic nerve sheath diameter are the various modalities which use ultrasound to provide an estimation of cerebral blood flow or intracranial pressure. Out of these TCD is the most reliable and validated technique helpful in the diagnosis of brain death. Certain prerequisites have to be fulfilled before carrying out the examination to decrease the possibility of false-positive and -negative results. The various waveforms seen with progressive increase in ICP are oscillating waveform, short systolic spikes and disappearance of intracranial flow. The other test, cervical colour Doppler, has not been included in the list of standard ancillary tests. However, it is especially of help in patients having absent bone window or when TCD-trained physician is not available. Ultrasonography for optic nerve sheath diameter is a simple, non-invasive, rapid bedside test for diagnosis of raised ICP. A sustained trend of high values points towards cerebral deterioration and possibly brain death if corrective measures fail. But it fails to differentiate BD patients from comatose patients. Thus, out of all TCD is the most sensitive and specific ultrasonographic technique for confirmation of cerebral circulatory arrest. For this reason, it is now increasingly being included as a first-line ancillary test in country-specific guidelines.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Brain death
- Ancillary tests
- Transcranial Doppler
- Oscillatory waveform
- Cervical colour Doppler
- Optic nerve sheath diameter
Brain death is an irreversible cessation of all functions of brain, including brainstem. The three cardinal features include coma, absence of brainstem reflexes and apnoea. It is reasonable that the time between the diagnosis and declaration of brain death should be short, so that organ harvesting for the purpose of transplantation can be carried out before their function gets compromised.
1 Pathophysiology of Brain Death
The main inciting event which leads to brain damage is the rise in intracranial pressure. Any severe head injury, cerebrovascular accident or cerebral anoxia due to any reason causes neuronal damage. The ensuing inflammatory cascade of events leads to activation of various neurotransmitters, dysregulation of ion channels and damage to blood-brain barrier, resulting in progressively increasing cerebral oedema. As a result, the intracranial pressure becomes high, and the low-pressure bridging veins get compressed resulting in increase in cerebral venous pressure [1]. As the intracranial pressure further increases, the cerebral blood flow decreases inside the intracranial cavity. With loss of autoregulation, the cerebral perfusion becomes pressure dependent and there is risk of global hypoperfusion with any decrease in blood pressure. This further perpetuates the damage and ultimately a state of irreparable and irreversible damage follows. The blood flow inside the intracranial cavity completely ceases and swollen brain may herniate through foramen magnum or dural folds. Herniation may lead to permanent brainstem damage affecting major vital centres and cranial nerves leading to the clinical state of brain death. The pressure gradients generated inside the cranial cavity can also cause early brainstem herniation and focal ischemia of the vital control centres resulting in death.
2 Diagnosis
It is primarily a clinical diagnosis and ancillary tests are not mandatory to perform and are categorised as optional only. However, in situations when examination cannot be completed or results obtained are uncertain, the role of ancillary tests becomes important (Table 18.1). The confirmatory tests establish either loss of electrical activity or cessation of blood flow. These are
-
Four-vessel cerebral angiography
-
EEG
-
Evoked potentials
-
Transcranial Doppler (TCD)
-
Radionuclide imaging
-
CTA/CT perfusion/MRA
-
Cervical colour Doppler sonography
The criteria of their use in the diagnosis of brain death vary worldwide. The demonstration of absent cerebral flow is included as a mandatory test in France and in children below 1 year of age in Italy. It is also essential to carry out these tests in the presence of confounding factors or in situations where brainstem reflexes cannot be carried out. Similarly, EEG is required as a mandatory test in Italy, Japan and France and is one of the most commonly used tests though country-specific variations exist. However, it is rendered unreliable under the effect of sedatives and hypothermia. Cerebral angiography is considered the gold standard for diagnosis of cerebral circulatory arrest (CCA). However, it is invasive, needs transportation of patient and is time consuming. The other tests like radionuclide imaging and perfusion scans are expensive and time consuming. The possibility of false results, susceptibility to confounding factors and non-standardisation affect the other diagnostic modalities [2].
One of these ancillary tests is transcranial Doppler (TCD) which has been considered as an optional confirmatory test for the diagnosis of BD in several guidelines across the world [3, 4]. It uses ultrasonography for assessing blood flow in basal cerebral arteries and helps in the confirmation of cerebral circulatory arrest. The reported sensitivity and specificity range from 70 to 100% and 97 to 100%, respectively [5, 6]. The agreement between TCD and angiography for confirmation of BD has been found to be 100% [7]. In Europe, cerebral angiography is the most common first-line test followed by TCD for confirmation of BD [8]. However at many places angiography is less preferred over TCD because of its invasiveness. In another retrospective study, TCD was seen to be useful as a first-line confirmatory test or as a specific prognosticator in such cases. The early and repetitive examinations depicting CCA pattern are particularly useful in such cases [9]. Both TCD and transcranial colour-coded sonography can be used as confirmatory tests. The colour duplex scanning has an additional advantage that it allows direct visualisation of the vessel lumen. The waveform patterns obtained are similar in both. The advantages and disadvantages of TCD are listed in Table 18.2.
The results of a meta-analysis by Chang and colleagues suggest that transcranial Doppler is a highly accurate ancillary test for brain death confirmation. However, as transcranial Doppler evaluates cerebral circulatory arrest and not the brainstem function, this limitation needs to be taken into account when interpreting the results of the meta-analysis [10].
3 TCD Procedure
It involves use of a low-frequency ultrasonography transducer (2 MHz) placed at relatively thin bone windows to insonate the basal intracranial arteries and estimate cerebral blood flow velocity. The major vessels studied by TCD are internal carotid artery (ICA), middle cerebral artery (MCA), anterior cerebral artery (ACA), posterior cerebral artery (PCA), basilar artery and vertebral artery. The different bone windows used for TCD are transtemporal, suboccipital, transorbital and submandibular. The ultrasonic waves emitted from transducer are reflected back from moving erythrocytes with a change in frequency that is directly proportional to the velocity of moving cells. The blood flow towards and away from the probe is displayed as positive waveform and negative waveform with respect to baseline. The different arteries are identified based on the window used, depth of insonation and direction of waveform. Cerebral blood flow velocity (CBFV) is derived from a standard equation which uses speed of incident wave, wave pulse frequency and change in angle of incident and reflector beam. It is also dependent on several other physiologic factors. Other than the calculation of CBFV, waveform analysis provides information about parameters like cerebrovascular resistance, autoregulatory status, estimation of cerebral perfusion pressure (CPP) and intracranial pressure (ICP) also. The CBFV gives an indirect estimation of intracranial vessel diameter. Increase in CBFV can be seen in conditions of hyperdynamic flow, stenosis or vasospasm. Similarly, decrease in CBFV points towards hypotension, increased ICP or decrease in intracranial blood flow as seen in brain death.
Before carrying out TCD, few prerequisites have been defined for diagnosing CCA. These include established cause of coma consistent with irreversible loss of brain function, exclusion of hypotension, hypothermia, metabolic derangements and clinical evaluation by two experts showing no evidence of cerebral and brainstem function [11]. The patient should be normocapnic, tachycardia should not be >120/min and systolic blood pressure should be >90 mm Hg. An experienced trained physician should be available for carrying out TCD examination. The cerebral circulatory arrest precedes brain death by approximately 24 h. This is the period when TCD is especially useful for early confirmation of brain death and organ retrieval [12].
The technical prerequisites of TCD [13] for diagnosing CCA are:
-
A high-pass filter ≤50 Hz should be used.
-
Gain should be increased.
-
Sample volume should be set at ≥15 mm.
-
Envelope should be switched off.
During TCD examination, bilateral insonation should be performed by placing probes either at temporal bone for MCA or at suboccipital transcranial window for vertebrobasilar vessels.
Calculation of CPP can be done non-invasively by TCD and it correlates well with the CPP measured by invasive ICP monitor. The positive predictive value for diagnosing CPP <60 mm Hg is 94% [14]. It is more useful as a trend monitor rather than considering an absolute value.
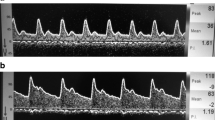
A diagnosis of CCA on TCD is confirmed if following waveforms are obtained on two examinations performed at least 30 min apart. The appearance of following waveforms is due to the different stages of progressively increasing ICP (Figs. 18.1 and 18.2).
-
An oscillating waveform (systolic forward flow and diastolic reverse flow)
-
Short systolic spikes
-
Disappearance of intracranial flow
Transcranial Doppler in brain death. Transcranial Doppler shows reverberating or oscillating pattern of flow in all but the left posterior cerebral artery (L-PCA, right inferior corner rectangle) where there is complete absence of flow. Findings confirm brain death. Reverberating or absent flow is diagnostic of brain death. “Reprinted from Seminars in Ultrasound, CT and MRI, 39 (5), Tanvir Rizvi, Prem Batchala, Sugoto Mukherjee. Brain Death: Diagnosis and Imaging Techniques, 515–529, Copyright (2019) with permission from Elsevier”
With increase in ICP, higher pulsatility is evident in cerebral arteries (high pulsatility index). At the point when ICP is equal to the diastolic blood pressure, the brain is perfused only in systolic cycle and when end-diastolic velocity is zero. Gradually, as ICP equals to the mean blood pressure, the blood flow ceases during both cycles. The point at which ICP increases to such an extent that no blood can flow into intracranial cavity is evident as oscillatory waveform with equal area under positive and negative waves. This may be explained by the elasticity and compliance of arterial musculature. The systolic forward flow in large basal arteries and diastolic reverse flow produced by microcirculatory obstruction result in zero net flow. This to and fro movement can be appreciated in patent arteries. This usually corresponds to the angiographic picture of CCA [15]. Gradually, with ICP reaching systolic blood pressure, low-amplitude short systolic spikes are seen ending up in total disappearance of waveforms. The systolic peak is less than 50 cm/s and lasts for less than 200 ms in early systole, with absent flow signal during rest of the cycle. Disappearance of intracranial blood flow indicates cerebral circulatory arrest. A mean CBFV in MCA <10 cm/s for more than 30 min is not compatible with survival. It is better to insonate both MCA and BA for demonstration of CCA with a repeat test performed at an interval of 30 min to ensure irreversibility of finding. Corroborating these findings with extracranial demonstration of similar blood flow changes bilaterally in common carotid artery, ICA, VA is also important. On the other hand, flow in external carotid arteries will be normal as the arrest of blood flow usually occurs at the level of carotid bifurcation. Absent cerebral blood flow has to be differentiated from ultrasonic transmission problems. A previous successful examination through the same window and waveforms depictive of brain death seen on the opposite site usually rules out ultrasonic transmission problem.
Dominguez-Roldan studied the difference in waveforms in patients who were brain dead having a supratentorial or infratentorial lesion. In patients with supratentorial lesions, the oscillatory flow pattern was more common. However in patients with infratentorial lesions, systolic spikes were more commonly seen [16].
Use of TCD for central retinal vessel waveform analysis and blood flow variables may have a potential to be developed as an ancillary test in paediatric population to determine brain death [17].
3.1 False-Positive and False-Negative Results
The typical waveforms indicative of brain death are produced as a result of changes between ICP and cerebral blood flow. There are certain situations when typical TCD waveforms indicative of CCA are not identified. In such cases, persistent blood flow pattern may be seen in patients with decompressive craniectomies, skull fractures and intraventricular drains; in small children with open fontanelle; or in patients with brainstem injuries [18]. The loss of ICP generation fails to elicit changes in intracranial CBF. Such conditions require other confirmatory studies for diagnosis of brain death. TCD is highly accurate as an ancillary test but it should be remembered that it evaluates CCA rather than brainstem death.
False-positive TCD findings may also be seen in aneurysm rupture at the time when there is a sudden surge in ICP. Also, in the early stage after cardiac arrest, there will be CCA before the patient’s circulation returns. In both these situations, CCA is transient and the patient cannot be labelled as brain dead. A repeat examination performed 30 min later will show normal waveforms. Other conditions in which false-positive findings are obtained are ICA distal occlusion and aortic insufficiency. Thus, this makes clinical examination and fulfilment of prerequisites for performing the TCD ultrasonography important.
An inexperienced operator may be unable to insonate the vessel or misinterpret the waveforms. Thus, it is operator dependent and extremely essential to have a trained physician. The transorbital window can be used in such cases to visualise carotid siphon [19].
Thus, TCD is an ancillary test used for confirmation of clinical diagnosis of brain death. It should be considered in conjunction with the clinical condition. If performed by a trained operator, it is a quite sensitive and specific test.
3.2 Other Tests
Few other tests are also useful for diagnosis of brain death though these are not validated as confirmatory tests.
3.2.1 Cervical Colour Doppler
In cases where insonation window is absent or definitive flow patterns cannot be ascertained, the cervical colour Doppler may be used to confirm CCA. The procedure is performed bilaterally in a technique similar to TCD using 5 or 7.5 MHz Doppler probe but through a cervical approach. This helps to visualise the flow patterns in extracranial ICA and VA. The submandibular and suboccipital window are used for insonation of extracranial ICA and VA, respectively. The waveform patterns indicative of CCA are same as discussed before. ICA occlusion and anatomical conditions may preclude successful examination. The sensitivity for confirming CCA has been found to be 78–80% and has been suggested to be considered as a complementary test [20].
Still, CCD has not been included in the list of standard ancillary tests. However, it is especially of help in patients having absent bone window or when TCD-trained physician is not available.
3.2.2 Optic Nerve Sheath Diameter
The optic nerve is covered by a dural sheath containing cerebrospinal fluid inside it which is in direct continuation with intracranial subarachnoid space. This optic nerve is loosely attached to dural sheath in the retrobulbar part. At the time of increase in ICP, there is shift of CSF into this distensible part (3 mm behind the globe) giving rise to increase in optic nerve sheath diameter which is thus taken as a surrogate of raised ICP. This diameter can be measured by CT, MRI or ultrasound.
Ultrasonography for optic nerve sheath diameter is a simple, non-invasive, rapid bedside test for diagnosis of raised ICP. High-frequency linear probes (7.5–10 MHz) are placed gently on closed upper eyelid of a patient in an axial plane to visualise the retrobulbar area. The globe appears as a round dark structure with optic nerve seen as black strip-like structure at the back of the globe. The probe is adjusted to display the entry of optic nerve into the globe at the centre of the image. After freezing this picture, callipers are used to measure the ONSD at 3 mm behind the papilla. A mean of three readings of ONSD is calculated to obtain the final value. ONSD measurement as a surrogate for ICP can be especially useful to screen patients when invasive monitoring is not possible or not indicated.
A value ranging from 4.8 to 6 mm correlates with increased ICP [21]. Brain death is a state of tremendous increase in ICP and this should be evident on ONSD also. Studies have shown that mean ONSD is much greater in patients who were brain dead (0.72 ± 0.05 versus 0.53 ± 0.06) [22]. Moreover, a range of ONSD values from 0.68 to 0.75 cm with ICP values from 28 to 54 mm Hg have been noted in brain-dead patients [23]. The ONSD is significantly higher in patients with BD but it cannot differentiate BD patients from comatose patients who have raised ICP but are not clinically brain dead [24]. The patients with decompressive craniectomies will not have an ICP rise to an extent of inducing cessation of intracerebral blood flow. As a result, ONSD values fail to provide reliable information in such patients [23].
Thus, ONSD is a non-invasive test which can be quickly performed and sustained trend of high values points towards cerebral deterioration and possibly brain death if corrective measures fail.
To conclude, ultrasound when used for detection of CCA has advantages of being a non-invasive, inexpensive, complication free and a quick technique. TCD is the most reliable and sensitive ultrasonographic technique for confirmation of CCA. For this reason, it is now coming up as a first-line ancillary test more often in country-specific guidelines.
References
Nakagawa Y, Tsuru M, Yada K. Site and mechanism for compression of the venous system during experimental intracranial hypertension. J Neurosurg. 1974;41:427–34.
Wijdicks EFM. Brain death worldwide: accepted fact but no global consensus in diagnostic criteria. Neurology. 2002;58:20.
Wijdicks EFM, Varelas PN, Gronseth GS, Greer DM. Evidence-based guideline update: determining brain death in adults: Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1911–8. 181e242a8
Walter U, Schreiber J, Kaps M. Doppler and duplex sonography for the diagnosis of the irreversible cessation of brain function (‘brain death’): current guidelines in Germany and neighbouring countries. Ultraschall Med. 2016;37:558–78.
De Freitas GR, Andre C. Sensitivity of transcranial Doppler for confirming brain death: a prospective study of 270 cases. Acta Neurol Scand. 2006;113:426–32.
Kuo JR, Chen CF, Chio CC, et al. Time dependent validity in the diagnosis of brain death using transcranial Doppler sonography. J Neurol Neurosurg Psychiatry. 2006;77:646–9.
Poularas J, Karakitsos D, Kouraklis A, Kostakis A, De Groot E, et al. Comparison between transcranial color Doppler ultrasonography and angiography in the confirmation of brain death. Transplant Proc. 2006;38:1213–7.
Citerio G, Murphy PG. Brain death: the European perspective. Semin Neurol. 2015;35:139–44.
Sharma D, Souter MJ, Moore AE, Lam AM. Clinical experience with transcranial Doppler ultrasonography as a confirmatory test for brain death: a retrospective analysis. Neurocrit Care. 2011;14:370–6.
Chang JJ, Tsivgoulis G, Katsanos AH, Malkoff MD, Alexandrov AV. Diagnostic accuracy of transcranial Doppler for brain death confirmation: systematic review and meta-analysis. AJNR Am J Neuroradiol. 2016;37:408–14.
Hassler W, Steinmetz H, Gawlowski J. Transcranial Doppler ultrasonography in raised intracranial pressure and in intracranial circulatory arrest. J Neurosurg. 1988;68:745–51.
Dosemeci L, Dora B, Yilmaz M, Cengiz M, Balkan S, Ramazanoglu A. Utility of transcranial Doppler ultrasonography for confirmatory diagnosis of brain death: two sides of the coin. Transplantation. 2004;77:71–5.
Widder B, Görtler M, Widder G. Doppler- und Duplexsonographie der hirnversorgenden. Arterien. 6th ed. Berlin: Springer; 2004.
Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD. Cerebral perfusion pressure in head injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg. 1998;88:802–8.
Hassler W, Steinmetz H, Pirschel J. Transcranial Doppler study of intracranial circulatory arrest. J Neurosurg. 1989;71:195–201.
Dominguez-Roldan JM, Garcia-Alfaro C, Jimenez-Gonzalez PI, Rivera-Fernandez V, Hemandez-Hazanas F, Perez-Bemal J. Brain death due to supratentorial masses: diagnosis using transcranial Doppler ultrasonography. Transplant Proc. 2004;36:2898–900.
Riggs BJ, Choen JS, Shivakumar B, et al. Doppler ultrasonography of the central retinal vessels in children with brain death. Pediatr Crit Care Med. 2017;18:258–64.
Cabrer C, Dominguez-Roldan MM, Trias E, Paredas D, et al. Persistence of intracranial diastolic flow in transcranial Doppler sonography exploration of patients in brain death. Transplant Proc. 2003;35:1642–3.
Dominguez-Roldan JM, Jimenez Gonzalez PI, Garcia-Alfaro V, Rivera-Fernandez V, Hernandez HF. Diagnosis of brain death by transcranial Doppler ultrasonography: solutions for cases of difficult sonic windows. Transplant Proc. 2004;36:2896–7.
Pedicelli A, Bartocci M, Lozupone E, D’Argento F, Alexandre A, Garignano G, et al. The role of cervical color Doppler ultrasound in the diagnosis of brain death. Neuroradiology. 2019;61:137–45.
Kristiansson H, Nissborg E, Bartek J Jr, Andresen M, Reinstrup P, Romner B. Measuring elevated intracranial pressure through noninvasive methods: a review of the literature. J Neurosurg Anesthesiol. 2013;25:372–85.
Arijana L-H, Simicevic DJ, Popovic IM, Puretic MB, Cvetkovic VV, Gopcevic A, et al. New trends in neurosonology and cerebral hemodynamics - an update. Pers Med. 2012;1:414–6.
Toscano M, Spadetta G, Pulitano P, Rocco M, Di Piero V, Mecarelli O, Vicenzini E. Optic nerve sheath diameter ultrasound evaluation in intensive care unit: possible role and clinical aspects in neurological critical patients daily monitoring. Biomed Res Int. 2017;2017:7.
Topcuoglu MA, Arsava EM, Bas DF, Kozak HH. Transorbital ultrasonographic measurement of optic nerve sheath diameter in brain death. J Neuroimaging. 2015;25:906–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mahajan, C., Kapoor, I., Prabhakar, H. (2021). Brain Death. In: Robba, C., Citerio, G. (eds) Echography and Doppler of the Brain. Springer, Cham. https://doi.org/10.1007/978-3-030-48202-2_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-48202-2_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-48201-5
Online ISBN: 978-3-030-48202-2
eBook Packages: MedicineMedicine (R0)