Abstract
Medial and lateral elbow instability are both managed with different types of ligamentous repair and reconstruction techniques. The gold standard for ulnar collateral ligament (UCL) repair is ligamentous reconstruction performing techniques such as the modified Jobe or docking procedure, etc. Repair or reconstruction with a prolonged period of immobilization is generally utilized to fix instability of the lateral collateral ligament (LCL). The InternalBrace™ (Arthrex Inc.) can be utilized on the medial or lateral elbow to restore ligamentous stability (Dugas et al., Am J Sports Med 44(3):735–741, 2016; Greiner et al., Knee Surg Sports Traumatol Arthrosc 27(10):3269–3275, 2019). It is a collagen-coated suture implant that serves as a checkrein ligament. The internal brace decreases the stress experienced by the repaired/reconstructed ligament. This novel implant can be utilized to repair ligamentous injuries around the body such as the ankle joint (Yoo and Yang, J Orthop Traumatol 17(4):353–360, 2016). Dugas et al. were the first to describe utilizing the InternalBrace™ for UCL repair (Dugas et al., Am J Sports Med 44(3):735–741, 2016). Recent studies demonstrated that UCL repair augmented with internal bracing has an increased load to failure, less gap formation, and the same time zero strength as UCL reconstruction (Dugas et al., Am J Sports Med 44(3):735–741, 2016; Bodendorfer et al., Am J Sports Med 46(14):3495–501, 2018; Jones et al., Orthop J Sports Med 6(2):2325967118755991, 2018). Moreover, the InternalBrace™ has allowed athletes to return to play and perform rehabilitation earlier than UCL reconstruction (Wilk et al., J Orthop Sports Phys Ther 49(4):253–261, 2019; Moore et al., Orthop Clin North Am 50(3):383–389, 2019; Leasure et al., Am J Sports Med 47(4):928–932, 2019). It is believed that internal bracing is better suited for younger athletes with acute/subacute UCL tears and reconstruction is reserved for chronic tears (Dugas et al., Am J Sports Med 44(3):735–741, 2016; Moore et al., Orthop Clin North Am 50(3):383–389, 2019). Also, internal bracing can be used to augment LCL repair/reconstruction (Greiner et al., Knee Surg Sports Traumatol Arthrosc 27(10):3269–3275, 2019; Melbourne et al., JSES Int 4(2):224–230, 2020; Ellwein et al., Knee Surg Sports Traumatol Arthrosc [Internet], 2020; Scheiderer et al., Knee Surg Sports Traumatol Arthrosc 28(4):1195–201, 2020).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Internal brace
- Elbow
- Instability
- Dislocation
- Biomechanics
- Lateral collateral ligament
- Ulnar collateral ligament
- Docking
- Reconstruction
- Augmentation
Introduction
Management of elbow instability presents a challenge to the orthopedic surgeon. Both the lateral collateral ligament (LCL) and ulnar collateral ligament (LCL) play an integral role in providing stability to the elbow joint [1,2,3,4,5,6,7,8,9,10,11,12]. Generally, UCL injuries are seen in athletes such as pitchers, javelin throwers, or other overhead athletes [12, 13]. LCL injuries are usually associated with simple or complex elbow dislocations [12, 13]. There has been a significant increase in the number of UCL injuries diagnosed among athletes [1, 4, 14]. Similarly, there has been an increase in the number of UCL reconstructions performed on athletes as well [8, 15].
UCL repair had poor functional results in athletes when compared to UCL reconstruction [16,17,18]. Hence, UCL reconstruction techniques such as the docking or modified Jobe technique were rendered as the gold standard for surgical management of medial elbow instability. Conversely, there are newer studies demonstrating that UCL repair is a viable option in the young adult and adolescent patients with acute UCL tears [19, 20]. Dugas et al. were the first to describe performing UCL repair with internal brace augmentation [1]. This has since increased the interest in UCL repair with suture augmentation in acute/subacute UCL injuries because of the benefits afforded to patients. UCL repair augmented with internal bracing has shown to be equally or more biomechanically stable than UCL reconstruction [1, 4, 5]. Internal bracing has an increased load to failure and greater resistance to gap formation than traditional UCL reconstruction techniques [5]. A hallmark of UCL repair with internal bracing is earlier return to play (≈6 months) than UCL reconstruction (≈12 months) [8]. In addition, internal bracing has been shown to increase the biomechanical stability of UCL reconstruction such as the docking technique [8, 15].
There is still controversy on the preferred management of LCL insufficiency with regard to repairing or reconstructing the LCL [2, 9, 12]. However, internal bracing increases the biomechanical stability of both the repaired and reconstructed LCL. Utilizing the internal brace mitigates the need for external fixation or prolonged immobilization to protect repaired/reconstructed LCL [2, 9, 10]. It allows these patients to begin immediate range of motion exercises to help decrease incidence of postoperative stiffness.
The InternalBrace™ (Arthrex Inc.) technique is an important skill that the shoulder/elbow surgeon should have in his/her armamentarium. In this chapter, we provide the reader with a detailed technique of the InternalBrace™ with tips and tricks to ameliorate the difficult aspects of this procedure.
Indications
UCL repair is warranted after failure of a non-operative trial that includes physical therapy, non-steroidal anti-inflammatory drugs, and strengthening of the flexor/pronator mass. These patients usually have intractable medial elbow pain, and UCL injury is confirmed with magnetic resonance imaging (MRI). The UCL should be assessed for any degenerative changes because this dictates surgical management [7]. Also, the physician should inquire if patients are experiencing any ulnar nerve pathology. There is a subset of patients with medial elbow instability that have ulnar nerve pathology such as cubital tunnel syndrome or ulnar neuritis [12]. Generally, UCL reconstruction/repair is reserved for overhead athletes such as pitchers, gymnasts, javelin throwers, etc. [12]. UCL repair with internal bracing should be performed on patients with acute/subacute tears [1]. UCL reconstruction is performed on patients with chronic UCL tears [1, 7].
LCL repair is generally indicated in fracture dislocations of the elbow, namely, the terrible triad injury [12]. Also, LCL repair is warranted in symptomatic posterolateral rotatory instability (PLRI) of the elbow [11].
Contraindications
Patients who are unable to follow postoperative protocol such as non-weight bearing (NWB) or refuse to engage in physical therapy/rehabilitation.
Surgical Technique
Lateral Ulno-Humeral Ligament Reconstruction
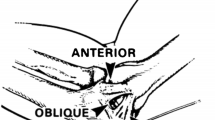
The standard lateral approach is made to the elbow centered over the lateral epicondyle. Sharp dissection is carried down to the lateral fascia where thick skin flaps are elevated. The origin of the extensor carpi radialis longus, brevis, and comminus is elevated from the lateral epicondyle, and close attention is made not stray posterior to the affect the ulno-humeral lateral complex. Usually in patients with trauma or a fracture with lateral instability, the surgeon will fall into the defect (Fig. 64.1). The lateral ulno-humeral complex usually tears off the humeral side exposing the elbow. Dissection is continued distally and posteriorly to expose the proximal olecranon opposite of the radial head. This will be the site for insertion for the first 4.75 swivel lock anchor with fiber tape (Arthrex, Naples, FL). The ideal starting point would be mid-way anterior-posterior on the olecranon and just opposite of the radial head. If the anchor is placed too far distally, the fiber tape can snap on the radial head causing pain particularly if a radial head implant is placed. If the anchor is placed to proximately, it does not provide adequate lateral support to the elbow. It is important that the hole be drilled obliquely, so the anchor will remain within the canal of the ulnar and not protrude out the ulna aspect to affect the ulna nerve (Fig. 64.2). It is very important to tap this drill hole as this is hard cortical bone and the anchor cannot be inserted without tapping the bone (Fig. 64.3). The anchor with the fiber tape and #2 fiber wire are inserted to the hole in the olecranon (Fig. 64.4). The fiber wire from the anchor is placed through the distal aspect of the lateral ulnar humeral complex for repair.
The second 4.75 swivel lock anchor (Arthrex, Naples, FL) will then be placed on the lateral epicondyle. The most ideal location is slightly anterior to the midline of the lateral epicondyle (Fig. 64.5). This is relatively an oblique edge, and it’s hard to get the most ideal stating point. It should be drilled obliquely, ending proximally so the anchor does not protrude into the olecranon fossa. The goal is to keep it mid-lined to in the humerus so it does not protrude either through the anterior or posterior aspects to the distal humerus. The humerus is drilled and tapped as again this is a hard, cortical bone and the anchor cannot be inserted unless the bone has been tapped. Fiber tape for the first anchor on the olecranon is then inserted into the second anchor, which is inserted into the humerus to form the internal brace (Fig. 64.6). The elbow is held at −30 full extension while the anchor is being placed. Usually the fiber tape self-tensions itself as anchor is being screwed into the humerus (Fig. 64.7). For localized lateral instability to the elbow, this internal brace immediately provides instability to the elbow (Figs. 64.8, 64.9, 64.10, and 64.11). The remaining #2 fiber wire is then placed in the proximal aspect of the lateral ulno-humeral complex and is tied. The remaining #2 fiber wire is placed distally and is tied, and then the two sutures are tied to themselves to further provide stability to the elbow. Lastly, the fiber tape that was inserted through the proximal anchor can be passed through the remaining part of the lateral ligament complex and is tied down. This can leave a bulky knot, and the knot is passed through the muscle, which decreases its irritability. The remaining part of the extensor muscular is then closed in a pants-over-vest fashion. The elbow is immobilized for 2 weeks and then placed in a hinge brace at −20° extension for 3 weeks, and then range- and motion-strengthening exercises are initiated. The internal brace is inserted (Fig. 64.12). Again, the ideal starting point is opposite to the radial head on the olecranon so the brace does not snap in the implant (Figs. 64.13 and 64.14).
Ulnar Collateral Ligament Reconstruction
The standard medial approach is made to the elbow centered about the medial epicondyle (Figs. 64.15, 64.16, and 64.17). Blunt dissection is carried down to avoid injury to branches of the medial antebrachial cutaneous nerve. These are identified distally and carefully protected. The ulnar nerves are identified and traced through the flexor carpi ulnaris. It’s a surgeon’s preference to continue to work around the nerve or for it to be transposed anteriorly following the procedure. The flexor carpi ulnaris is split, and the base of the coronoid and proximal olecranon is identified (Fig. 64.18). The ideal starting point for the anchor is mid-way anterior-posterior on the olecranon at the level of the coronoid process. The ulna is drilled obliquely as described before and tapped, and the 4.75 swivel lock anchor with fiber tape and fiber wire is inserted (Arthrex, Naples, FL) (Fig. 64.19). The ideal placement for the second anchor will be the base of the humeral epicondyle and slightly anterior if possible. The hole is drilled obliquely, so the anchor does not protrude into the olecranon fossa and stays within the confines of the distal humerus. The fiber tape from the first anchor is then passed through the second anchor after the drill hole has been tapped and inserted at the elbow −30° with full extension (Fig. 64.20). As before, the fiber tape usually self-tensions as you place the anchor (Fig. 64.21). The remaining #2 fiber wire for both anchors are passed through the medial ligament complex and tied to themselves. The remaining fiber tape on the humeral anchor can be passed through the remaining portion of the ulnar collateral ligament securing this part of the ligament. The knot can be bulky so the fiber tape knot is passed through the muscle of the flexor carpi ulnaris. At this point, the ulnar nerve can be transposed depending on the surgeon’s preference (Figs. 64.22, 64.23, and 64.24).
The elbow is immobilized for 2 weeks, and then a removable brace at −20° extension for 3 weeks and then regular strengthening exercises are then initiated through physical therapy (Figs. 64.25 and 64.26).
Tips and Tricks
-
Make sure to tap the drill holes before attempting to insert the anchor. In hard cortical bone, the anchor will not advance unless it is tapped.
-
Make sure to insert the anchors in an oblique fashion into the olecranon and the humerus. In this manner, the anchors will not protrude out the opposite cortex. This will decrease any irritation to the anchor and to avoid penetrating the olecranon inserted fossa in a humeral inserted anchor.
-
Ideally on the humerus the starting point for the drill hole should be anterior to the midline. Elbow ligament stability is important in particular in extension, and by placing the anchor slightly anterior, will tighten up the internal brace extension as compared to elbow flexion.
-
Tighten the fiber tape with the elbow at −30° at full extension. This will provide the most stability to the internal brace reconstruction.
-
Use the additional fiber wire on the anchors to further secure the collateral ligament complex, as well as the remaining fiber tape on the humeral anchor.
-
Remember the fiber tape knot can be quite bulky, and it is important to pass this through the muscle to decrease soft tissue irritation.
-
Pay close attention to the medial antebrachial cutaneous nerves through the medial cited approach. If these are lacerated, it can result in troublesome and problematic neuromas.
-
Transposition of the ulnar nerve is surgeon dependent.
Conclusion
Ligamentous reconstruction for UCL injuries is the gold standard for the management of UCL injuries. However, several studies demonstrated UCL repair with internal bracing is more biomechanically stable than UCL reconstruction techniques such as the docking technique or modified Jobe reconstruction [1, 4, 5]. The InternalBrace™ offloads the stress from the UCL repair while it is healing. UCL repair with the internal bracing increases load to failure and torsional stiffness with less gap formation than UCL reconstruction techniques [1, 5, 21, 22] and restores valgus stability similar to that of the native ligament [4]. The main feat of UCL repair with internal bracing for the athlete is earlier return to play and being able to participate in more rigorous physical training earlier than UCL reconstruction [4, 6,7,8, 22].
The orthopedic surgeon must thoroughly analyze if the patient is an ideal candidate for UCL repair with internal bracing. This procedure is usually offered to younger athletes that are eager to return to sports after failed non-operative management [7]. The UCL tissue must be healthy appearing and free of chronic degenerative changes such as fraying or fibrosis. Also, patients with large bony avulsions off the medial epicondyle or sublime tubercle are poor candidates for the procedure [7]. This bone loss associated with this procedure will compromise the ligamentous stability. Also, patients have to be committed to participating in a postoperative rehabilitation program.
The InternalBrace™ can be used to augment UCL reconstruction if primary repair cannot be performed on the patient [8, 15]. It decreases the stress placed on the allograft. Also, internal bracing is used to augment LCL repair/reconstruction as well [2, 9,10,11].
In summation, internal bracing is a novel procedure with several advantages and an important technique for the shoulder/elbow surgeon to understand. Future studies need to investigate the long-term functional outcomes of internal bracing, functionality of UCL repair with internal bracing in older athletes, and optimal sites for suture tape/anchor placement for LCL repair/reconstruction.
References
Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–41.
Greiner S, Koch M, Kerschbaum M, Bhide PP. Repair and augmentation of the lateral collateral ligament complex using internal bracing in dislocations and fracture dislocations of the elbow restores stability and allows early rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3269–75.
Yoo J-S, Yang E-A. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17(4):353–60.
Bodendorfer BM, Looney AM, Lipkin SL, Nolton EC, Li J, Najarian RG, et al. Biomechanical comparison of ulnar collateral ligament reconstruction with the docking technique versus repair with internal bracing. Am J Sports Med. 2018;46(14):3495–501.
Jones CM, Beason DP, Dugas JR. Ulnar collateral ligament reconstruction versus repair with internal bracing: comparison of cyclic fatigue mechanics. Orthop J Sports Med. 2018;6(2):2325967118755991.
Wilk KE, Arrigo CA, Bagwell MS, Rothermich MA, Dugas JR. Repair of the ulnar collateral ligament of the elbow: rehabilitation following internal brace surgery. J Orthop Sports Phys Ther. 2019;49(4):253–61.
Moore AR, Fleisig GS, Dugas JR. Ulnar collateral ligament repair. Orthop Clin North Am. 2019;50(3):383–9.
Leasure J, Reynolds K, Thorne M, Escamilla R, Akizuki K. Biomechanical comparison of ulnar collateral ligament reconstruction with a modified docking technique with and without suture augmentation. Am J Sports Med. 2019;47(4):928–32.
Melbourne C, Cook JL, Della Rocca GJ, Loftis C, Konicek J, Smith MJ. Biomechanical assessment of lateral ulnar collateral ligament repair and reconstruction with or without internal brace augmentation. JSES Int. 2020;4(2):224–30.
Ellwein A, Füßler L, Ferle M, Smith T, Lill H, Pastor M-F. Suture tape augmentation of the lateral ulnar collateral ligament increases load to failure in simulated posterolateral rotatory instability. Knee Surg Sports Traumatol Arthrosc [Internet]. 2020. Available from: https://doi.org/10.1007/s00167-020-05918-5.
Scheiderer B, Imhoff FB, Kia C, Aglio J, Morikawa D, Obopilwe E, et al. LUCL internal bracing restores posterolateral rotatory stability of the elbow. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1195–201.
Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS. Green’s operative hand surgery. Philadelphia: Elsevier; 2016.
Savoie FH, O’Brien M. Chronic medial instability of the elbow. EFORT Open Rev. 2017;2(1):1–6.
Urch E, Limpisvasti O, ElAttrache NS, Itami Y, McGarry MH, Photopoulos CD, et al. Biomechanical evaluation of a modified internal brace construct for the treatment of ulnar collateral ligament injuries. Orthop J Sports Med. 2019;7(10):2325967119874135.
Bernholt DL, Lake SP, Castile RM, Papangelou C, Hauck O, Smith MV. Biomechanical comparison of docking ulnar collateral ligament reconstruction with and without an internal brace. J Shoulder Elb Surg. 2019;28(11):2247–52.
Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83.
Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23(4):407–13.
Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23.
O’Connell RS, O’Brien M, Savoie FH. Primary repair of ulnar collateral ligament injuries of the elbow. Oper Tech Sports Med. 2020;28(2):150735.
Savoie FH 3rd, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066–72.
Bachmaier S, Wijdicks CA, Verma NN, Higgins LD, Greiner S. Biomechanical functional elbow restoration of acute ulnar collateral ligament tears: the role of internal bracing on gap formation and repair stabilization. Am J Sports Med. 2020;48(8):1884–92.
Dugas JR, Looze CA, Capogna B, Walters BL, Jones CM, Rothermich MA, et al. Ulnar collateral ligament repair with collagen-dipped FiberTape augmentation in overhead-throwing athletes. Am J Sports Med. 2019;47(5):1096–102.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Geissler, W.B., Purcell, K.F. (2022). Internal Brace for Elbow Instability. In: Geissler, W.B. (eds) Wrist and Elbow Arthroscopy with Selected Open Procedures. Springer, Cham. https://doi.org/10.1007/978-3-030-78881-0_64
Download citation
DOI: https://doi.org/10.1007/978-3-030-78881-0_64
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78880-3
Online ISBN: 978-3-030-78881-0
eBook Packages: MedicineMedicine (R0)