Abstract
The use of fat grafting in breast surgery has become a well-established method with several indications. Although the roots of autologous fat grafting have hypoplasia indications, there are new, aesthetic, and revisional indications emerging that include conversions (e.g., breast implant replacement with fat) and hybrid/composite augmentation (e.g., implant enhancement to modify volume and/or shape). These options have indications for both simultaneous and delayed approaches.
This evolution in indications is particularly important given the advent of troubling conditions such as breast implant-associated anaplastic large-cell lymphoma, breast implant illness, and capsular contracture. But changing times and tastes, including patient’s desires to remove implants altogether, call for surgeons to also include these procedures as part of their armamentarium.
We will describe the new indications, types, and timing of augmentation together with the recommended technique in these different indications, specifically fat processing via the vibration technique using MicroAire technology and decanting.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Implant conversion
- Implant exchange with fat
- Hybrid breast augmentation
- Combined breast augmentation
- Aesthetic breast augmentation
- Fat transfer
- Fat grafting
- Autologous fat grafting
- Autologous breast augmentation
- Lipomodeling
- Composite breast augmentation
-
The main advantage of adding fat to a breast implant in a hybrid approach breast augmentation procedure is that the fat can be placed in selective areas, including the cleavage and around the implant to “soften the edges,” enhancing contour to a silicone implant and creating a much more natural look.
-
Implant conversion with fat involves removing a previously placed breast implant for reasons such as breast implant-associated anaplastic large-cell lymphoma (ALCL), breast implant illness (BII), and capsular contracture, and substituting in its place the patient’s own fat tissue.
-
It is preferable to perform implant conversion simultaneously with removing the implant, because the skin has already expanded.
-
Fat is grafted in two phases in the simultaneous conversion indication: one before removing the implant, and the other after removing the implant in the same session through separate incisions.
-
The method includes decanting for 10 min in a canister after harvesting the fat with a vibration device, specifically the PAL-650 Power-Assisted Liposuction from MicroAire®.
-
Because these indications are on the rise, our techniques should be ameliorated.
-
Fat grafting is used more and more in post-implant revision cases compared to what was previously done (i.e., only changing the implants).
-
The simultaneous hybrid approach is on the rise because the trend toward more natural results and more volume is increasing.
-
The eligibility criteria for implant conversion with fat and hybrid implant-fat breast augmentation/revision include excessive fat, a realistic expectation of volume increase, no history or family history of breast cancer, preoperative radiographic evaluation through ultrasound or MRI, and wish for autologous material.
1 Introduction
Autologous fat grafting (AFG) has become a central element in plastic surgery and has expanded well beyond its roots in reconstructive indications. Initially, AFG (also called autologous fat transfer, or AFT) was mainly used complementary to mastopexy procedures and breast construction post-cancer, or after mastectomy or breast-conserving surgery [1].
However, over time, AFG has also evolved into a procedure with aesthetic indications for conditions such as hypoplasia mamma, asymmetry, slight ptosis, and deformities such as tuberous breast. Fat grafting is often performed simultaneously with other procedures, such as abdominoplasty and gluteal augmentation. Fat grafting now has the reputation of being a surgical option with many beneficial characteristics: it is simple to perform and minimally invasive; it is an accessible, low-cost option for patients; and there is no risk of having immune reactions. In the world of modern plastic surgery, fat grafting is a widely accepted, valuable method with a wide range of potential applications, a favorable long-term safety profile, and high patient and physician satisfaction rates [2,3,4,5,6,7,8,9].
Now, largely due in part to emerging potential long-term implications of breast implants and changing tastes, AFG has made another jump in its evolution. Specifically, breast implant-associated anaplastic large-cell lymphoma (ALCL), breast implant illness (BII), capsular contracture, and modern demands for more natural results are expanding the indication spectrum to include conversions (i.e., alloplastic breast implant replacement with fat) and hybrid (also referred to as composite or combined) augmentation (i.e., implant enhancement to modify volume and/or shape) [2, 9,10,11,12,13,14,15,16,17,18,19]. This demand to remove existing implants and/or adding fat to the existing implant will surely be intensifying in the coming years.
The related techniques described here are relatively new, and we will describe the indications, types, and timing of augmentation together with the recommended fat processing technique in these different indications.
2 Definitions
Implant conversion with fat grafting is the removal of a previously placed breast implant and substituting in its place the patient’s own fat tissue. This can be performed as a simultaneous or delayed procedure.
A hybrid breast augmentation refers to a breast enlargement procedure using both implants and your own fat. This can also be performed as a simultaneous or delayed procedure. “Hybrid” procedures are also often referred to as “composite” or “combined”; hybrid refers to the dual-technique approach of fat with implant and does not refer to any specific implant type.
3 Indications
3.1 Implant Conversion with Fat Grafting (Table 64.1)
As previously mentioned, conditions such as ALCL, BII, severe capsular contracture, as well as just the changing attitudes about implants (“I am done with them”; “They have done their job”) and changing fashion have created a special need for some patients to move toward smaller and more natural combined augmentation, if not whole-cloth removal.
The main advantage of adding fat to a breast implant in a breast augmentation procedure is that the fat can be placed in selected areas in the cleavage and around the implant to “soften the edges” and give a much more natural look. Another advantage is that a smaller implant can be used when fat is being added.
The conversion could be simultaneous or delayed. The surgeon must do lipomodeling to other parts of the body as well, either simultaneously or delayed.
3.2 Hybrid Breast Augmentation (Table 64.2)
Hybrid breast augmentation is now considered a good alternative for women who want a substantial increase in breast volume but who do not have sufficient fat to achieve this result by fat transfer alone. Hybrid breast augmentation is especially suitable for women who have asymmetry, are thin, have a bony chest, and have a chest wall deformity such as an indented or prominent sternum, as well as for women who want the more natural look that fat transfer provides but desire more volume than can be achieved by fat alone.
In addition, this procedure is indicated for the following cases:
-
There is an insufficient amount of fat to do breast augmentation only with fat grafting.
-
The patient desires to have more than just the “artificial form” of breast augmentation/foreign bodies as implants.
-
The patient wishes to have more volume, specifically to increase the cleavage and upper pole areas, which are specific areas in which fat grafting achieves excellent results.
-
The patient wants to avoid the unnatural form of a breast implant.
-
There is a need to revise special areas, such as a revision after previous implant insertion (e.g., increasing the lower pole or the cleavage).
-
For mild cases of capsular contractures that do not necessitate implant removal, this procedure is appropriate.
-
For rippling in thin patients or for implants that are too large, this procedure is appropriate.
-
There is a need to do lipomodeling to other parts of the body, either simultaneously or delayed.
The simultaneous hybrid approach is most often indicated as an augmentation procedure, whereas the delayed approach is primarily indicated in cases of correction/revision.
4 The Oslo Plastikkirurgi Clinic Study
We retrospectively evaluated the indications and compared different fat processing methods for aesthetic breast augmentation.
The Oslo Plastikkirurgi Clinic has performed 204 breast augmentations using autologous fat grafting to treat hypoplasia mammae, breast asymmetry, implant conversion with fat, hybrid/combined augmentation, or deformities such as tuberous breast [9].
Five eligibility criteria must be met by patients to become a candidate for surgery: (1) excessive fat to be removed or corrected; (2) a realistic expectation of volume increase; (3) no history or family history of breast cancer; (4) radiographic evaluation through ultrasound or MRI; and (5) desire for an alternative to implants to avoid the use of foreign objects in the implant conversion indication.
The following guidelines and recommendations follow the process and procedures of the Oslo Plastikkirurgi Clinic. For a more detailed discussion, please see Part VIII in this book: Chap. 63 Aesthetic Breast Augmentation Using Autologous Fat Grafting: Indications, Patient Assessment, and Comparison Between Different Processing Methods in 204 Cases [9].
4.1 Patient Assessment
The assessments include medical history, BMI, ultrasound or MRI, and clinical examination of the fat deposits of the body.
Patient expectations are important to manage with any procedure involving fat grafting. We can achieve 1–2 cup sizes, or about 200–250 mL of fat per size for the bigger conversion cases. Of course, we can do more sessions to augment the results, provided that there is existing fat to harvest. For the hybrid approach, it is often satisfactory because the need for fat is not as huge as in conversion and it is limited to certain areas, as in rippling or augmentation of specific areas such as cleavage. Good information is required about the procedure because this is a process that takes at least 1 year. The BMI should preferably be under 30 to achieve figure-forming results.
5 Procedure Options and Their Methods and Techniques (Figs. 64.1 and 64.2)
5.1 Implant Conversion with Fat Grafting
As previously noted, conversions may be simultaneous or delayed depending on the individual case and assessments made therein. The methods and techniques of each are as follows.
Technical operation aspects for conversion. Upper left: Pre-op planning. Upper middle and upper right: Closed system; MicroAire and canister preparation. Middle left: Per-operative expansion. Middle second left: Filling the 60, 20, or 10 cc syringe from the canister. Middle right: First phase of grafting before removing the implant. Lower left: Implant and calcified capsule are removed. Lower middle: The plan of grafting (not deeper and not superficial). Lower right: A drawing calculation sheath to register the grafted amount of fat in the 4 quadrants of the breast and side per-operatively conducted by the anesthetist assistant, x is entry site
Technical operation’s aspects for simultaneous and delayed hybrid implant fat augmentation; post-implant enhancement, auto-prosthesis with fat, rippling, postmastectomy implant fat enhancement. Upper left: Pre-op planning. Upper second left: Closed system; MicroAire and canister preparation. Upper third left: Subfascial dissection for implant. Upper right: Per-operative packing av. subfascial pocket with gaze for hemostasis and expansion for 15 min. Middle left: Filling the 60 cc, 20 cc, or 10 cc syringe from canister. Middle second left: Grafting after inserting the implant. Middle third left: After suturing. Middle right: The plan for delayed hybrid grafting. Lower left and second left: Mastopexy augmentation with auto-prosthesis and fat showing the posterior flap. Lower third left: Planning rippling and smoothing the implant edges with fat. Lower right: Rigottomy before grafting in post-mastectomy case
5.2 Simultaneous Implant Conversion with Fat Grafting (Videos 64.1 and 64.2) (Figs. 64.3 and 64.4)
Liposuction is performed to harvest the fat cells from the patient’s donor areas.
Simultaneous conversion of breast implant: 35-year-old woman with simultaneous conversion of breast implant of 220 mL after 12 years; insertion with thin capsule. Augmentation was performed as delayed conversion in two sessions with MicroAire and decanting with 310/164 mL fat on the right side and 310/164 mL on the left side. Upper row: Preoperative. Lower row: 60 months post-op. Note the normal ptosis that the patient was seeking instead of capsular contracture
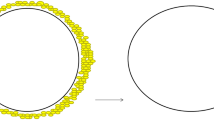
After tumescent liposuction to the breast and donor site as well as local anesthesia to the incision sites, a 3 mm multi-hole cannula is inserted with MicroAire PAL vibration to dissect the space between the skin and the capsule without any suction; this is done for approximately 5 min per site. This allows per-operative expansion to the recipient site and good hemostasis.
Then, the fat is harvested with a 4 mm Mercedes-type 3-hole cannula with the MicroAire PAL machine and collected to a 500 mL or 1000 mL canister. This will be set to decant for at least 10 min, during which time the recipient incision sites are sutured. Once completed, the liquid is emptied, and the rest of the fat is collected with a 10 or 60 mL syringe connected to a 3 mm cannula and grafted into the previously expanded area. Saturation of the fat is reached when the fat is squirting from the site, there is blanching, or there is hardness of the skin when the grafting is stopped.
Then, the submammary incision (or the previous implant incision) is reopened to remove the implant. If the capsule is thick and calcified, it should be removed in its entirety. The pocket is then irrigated with saline and hydrogen peroxide, and a circular incision from inside the pocket is made to facilitate healing and to prevent a sizable dead space. A drain is evaluated and inserted in case there is oozing, especially when removing a thick and calcified capsule.
After removing the implant, eliminating the “pocket” it had formerly occupied, a new second phase of grafting begins because more laxity of the skin and subcutaneous tissue emerges. The grafting is performed to correct the shape and augment the volume until blanching or squirting of the fat occurs. This reduces pressure within the breasts, thus allowing for the injection of additional fat. This fat is directed into the subcutaneous space. It is possible to add fat to the lower pole from the submammary incision, but it is advisable to do it from new, separate incisions medially and laterally. The submammary incision is closed at the end (Table 64.3).
The key to a successful simultaneous implant conversion with fat process is to embrace and per-operatively expand the subcutaneous space above the capsule and to augment the space with fat before carefully detaching the implant capsules and removing the breast implants. Furthermore, careful adding of fat after removing the implant can be performed because more space is available.
5.3 Delayed Implant Conversion with Fat Grafting (Figs. 64.5 and 64.6)
For various reasons, patients may come back for fat grafting after they have removed the implants. Potential reasons why patients return for fat grafting are because they thought they will not need additional volume, or because they thought they wanted or could live with the smaller breast without implants. Also, some patients may simply not know about this solution until after implant removal with another surgeon, so they seek a consult (second opinion) after learning about it.
Delayed conversion of implant with fat; 33-year-old woman with breast implant illness (BII), implant was removed 2 months earlier. Augmentation was performed as delayed conversion in two sessions with MicroAire and decanting with 300/270 mL of fat on the right side and 300/270 mL on the left side. Upper row: Preoperative with drawing; upper left showing the estimated grafted amount. Lower row: 7 months post-op
Delayed implant conversion with fat; 32-year-old woman. Indication: Conversion delayed, with fat grafting in two sessions after decanting and MicroAire, right: 220/215 mL and left: 215/195 mL. Middle row: 4 months after removal of the 200 mL implant, after 12 years with grade 3 capsular contracture. Note the severe retraction of the skin. Lower row: 18 months post-op. Although the result is not as optimal as it could be if the patient came for simultaneous conversion, the results yielded patient’s satisfaction. Note the bigger difference between the upper row with implants and the lower row after two sessions
In the cases of delayed conversions, some uneven skin retraction can occur, especially if there is a mild degree of ptosis after removing the implant—leaving an unpleasant form. In cases like these, the motto is “the sooner, the better.” The more time that has elapsed after the removal, the less favorable the conversion results will be, because the skin is shrinking and the whole subcutaneous and glandular space has reduced, which lessens the amount of fat possible to graft and makes blood circulation less favorable for subsequent surgery.
5.4 Hybrid Augmentation/Revision with Fat Grafting (Figs. 64.2, 64.7, 64.8, 64.9, and 64.10)
For revisions, the expectation is to have a smoother, less traumatic procedure than there was previously—when a revision of an implant almost always constitutes implant exchange and/or soft-tissue revision. Using fat is less traumatic, because we can isolate the areas where we can increase the volume with fat. There is also the reality of conditions such as ALCL, BII, and severe capsular contracture, where the need for this option is a matter of the patient’s health.
Delayed hybrid revision implant with fat in a 32-year-old. Treated for enhancing the lower pole and cleavage area and to soften the consistency of second-degree capsular contracture in two sessions: 325/110 mL on the right and 325/110 mL on the left. Upper row: Before operation. Upper left: Drawing before operation; note more volume in the planes to the lower pole. Upper 3 rights: pre-operative profiles. Lower row: lower left: 1-day post-op. Lower 3 rights: post-operative profiles: 36 months post-op
Delayed hybrid revision. Rippling with 350 ml submuscular implant; 1 year before complained about moderate rippling; request to soften the edges as the implant was too big. Two sessions with decanted fat were performed. Right: 150/175 mL and left: 150/175 mL. At the same time, an augmentation of the gluteal area with fat was performed. Upper row: Pre-op. Lower row, lower left: Per-op drawing. Lower three right: 8 months post-op. Note the enhancement of the cleavage area and the general effect on the whole breast
By choosing hybrid breast augmentation, the implant can easily be placed subfascially because we can support the cleavage and upper pole with fat. As a result, submuscular insertion will not be as necessary for patients who do not desire to undergo this approach; for example, with big implant volume and very thin patients, it is a limitation.
As with conversions, hybrid procedures may be simultaneous or delayed depending on the individual case and assessments made therein. The methods and techniques of each procedure are as follows.
5.5 Simultaneous Hybrid Augmentation with Fat Grafting (Video 64.3) (Figs. 64.7 and 64.10)
When a simultaneous hybrid treatment is performed, an implant is placed in the breast and AFG is performed and injected together with the implant. This requires a longer operation time but can give good results for women wanting more drastic results than what is achievable with fat grafting alone and helps soften the edges of the implant. The AFG volume in hybrid procedures can be estimated utilizing measurements based on implant volume/projection. This low-cost method can be applied to guide surgical decision-making in patients who are candidates for hybrid procedures. The advantage with this method is the ability to revise or augment specific areas, such as the cleavage or the upper or lower poles.
5.6 Delayed Hybrid Revision with Fat Grafting (Video 64.4) (Figs. 64.8 and 64.9)
In delayed hybrid procedures, the fat is injected at a later session after the implant is already in place.
One special challenge in the delayed option pertains to the appearance of rippling. Hybrid grafting is an especially good choice in cases where better results can be achieved with previous implants, sparing the need for a removal, exchange, or submuscular insertion. Another indication for a delayed hybrid procedure is to augment a certain area of the breast or to correct asymmetry.
Mastopexy augmentation with a posterior flap as auto-prosthesis and fat grafting can also be performed as another indication (Video 64.5).
5.7 Timing: Why Should We Do it at the Same Time and Not Delay?
Timing is a critical factor in breast augmentation conversions. This is because we already have an expanded skin and subcutaneous tissues that are often well vascularized (Fig. 64.6). Once the implants are removed, the skin will go through a retraction process that can give unevenness and asymmetry between the sides. If we modulated the breast directly, the skin would depose gently above the augmented parts and will have a better chance to be filled and symmetrical. We have seen the limitation of the amount of tissue reduced and fat grafted with more resorption when the patient came after removing the implant.
For the hybrid, it is preferable to do it simultaneously as well as because it goes into the planning about how much and where the fat and implant will build.
5.8 The Three Stages of Fat Grafting
Whether dealing with a conversion or hybrid augmentation/revision, standard fat grafting is commonly performed in three stages: (1) harvesting of the adipose tissue from a suitable donor site; (2) processing of the lipoaspirate to eliminate cellular debris, acellular oil, and excess infiltrated solution; and (3) grafting of the purified adipose tissue.
5.9 The Technique of Harvesting and Processing and Grafting of Fat
Both conversion and hybrid cases use decanting or gravity separation as methods of processing (vibration technique using MicroAire technology). This power-assisted technique leads to a time-dependent fractionation of the lipoaspirate in a completely closed system. After discarding the top and bottom layers, the fat can be transferred.
5.10 Harvesting and Anesthesia
Fat is most commonly harvested from the abdomen, thigh, buttocks, and inner knee region with a 4 mm multiperforated cannula, leading to a more aesthetic result and additional body sculpting. No significant differences regarding cell viability and volume retention of the previously mentioned donor sites are described in the literature.
For the fat transfer, a blunt 3 mm cannula is used, resulting in a reduced risk of intravascular injection, as well as maximized fatty tissue survival by injecting fat in small aliquots.
All procedures at the clinic were performed under total intravenous anesthesia (TIVA) plus tumescent anesthesia, which has been described to improve cell viability, reduce blood loss and pain, and ease the process of fat removal.
For a more detailed discussion, please refer to Part VIII in this book: Chap. 63 [9].
5.11 Postoperative Care
To prevent pressure on the fat and breast, patients were encouraged to wear a loose bra postoperatively. Patients were also strongly advised to keep their weight stable (i.e., do not gain or lose a considerable amount of weight) to achieve the optimal results.
5.12 Follow-Up
Clinical follow-up is needed and must include photographs both pre- and postoperatively. Surgeons should be generous with the second session, if there is enough fat to take (30% fat resorption is expected). We are under the impression that volume retention is superior in these indications compared with primary breast augmentation, because fat at the recipient site is well vascularized and there is often an expansion in the recipient site.
5.13 Resorption Rate and Residual Volume
The residual breast volume is evaluated after an average resorption time of 4 to 6 months. On examination, the volume should be stable without recent major postoperative breast changes (e.g., volume loss or ptosis).
5.14 Complications
Only minor complications (oil cysts and small fat necrosis) were reported in these patients.
In a study reported from the Oslo Plastikkirurgi Clinic study on 204 patients [9] with different indications who received fat grafting to the breast, 10 patients developed minor complications that were of no further concern and treated easily. One patient developed a benign small lump, a complication well known for its frequent occurrence after AFG. Two patients developed a small fat necrosis, one of which occurred along the patient’s mastopexy scar line. Only one patient showed signs of infection after the fat transfer, leading to an extremely low complication rate of 4% [2, 20].
However, as we know, the effects of factors such as local anesthesia, type of cannula, perioperative expansion, and amount of injected fat are still unclear. Further study is needed to determine whether these complications occur and, if so, to what extent.
5.15 Patient Satisfaction
Most patients were satisfied or very satisfied with their results. The positive reaction to the procedure can be explained by the natural feeling achieved and the improved fullness in the desired areas (e.g., upper pole, medially, asymmetric areas). These results were obtained without taking the risk of capsular formation and contractions. In addition to a more favorable breast volume and shape, a simultaneous reduction of unwanted body fat with body contour enhancement was achieved. For the hybrid revision patients, we were able to avoid implant removal while adjusting the form and volume by fat grafting. Patients who desired removal achieved their desired feeling of freedom while still retaining the desired and satisfactory volume.
Follow-up and satisfaction rates, which were evaluated by photographical, clinical, and patient assessment, have some limitations. The effects of factors such as local anesthesia, type of cannula, perioperative expansion, and amount of injected fat are still unclear.
5.16 Is it Cost Effective?
There is no other alternative for conversion for those who want to remove their implant and substitute it with fat. However, for hybrid implant fat augmentation, the cost is an issue for some patients. We should be aware to make sure that surgeons avoid pricing this procedure so high that patients will simply choose bigger implants. Price policy is an important factor in attracting patients and promoting new, useful, and desirable techniques such as fat grafting.
Even though AFG is more expensive and the actual intervention takes more time than a regular breast implant procedure, AFG is a good alternative for patients who want their implants removed, desire additional body contouring, or wish for a reasonable increase in breast volume.
5.17 Oncological Safety
In a single-center, case-control study of 137 patients, Rigotti and colleagues [21] could not confirm a significant effect of AFG on the recurrence of breast cancer in postmastectomy patients. Kronowitz and colleagues [22] verified the safety of fat grafting in a single-center, matched-controlled study of 1024 breasts.
In 2019, Stumpf and colleagues [23] published a retrospective cohort study on oncologic safety and AFG, and reported no significant difference in disease-free survival rates between 320 patients undergoing breast-conserving surgery with or without AFG.
No major complications were reported in either of the Oslo clinic cohorts [9]. These findings further support the conclusions reported by the previously mentioned authors.
Modern radiological technology has shown the ability to discriminate between neoplastic and necrotic calcifications, which makes the concern of interference with breast cancer screening redundant. Ørholt and colleagues [20] reported even lower numbers, with a major and minor complication rate of 1.6% and 0.5%, respectively. A total of 16.4% of the patients needed additional diagnostic imaging, and a biopsy was performed on 3.2% of them. Only the changes leading to further procedures should be considered as complications, rather than automatically considering all radiological changes as complications.
6 Conclusions
We should expect a considerable rise in demand for these implant conversion and hybrid procedures. Although the “traditional” implant era will not disappear soon, because as many as 35 million women have had breast implant surgery (70 million implants), we should be aware about these new indications and developments and make our techniques more efficient. Fat grafting as a completely independent approach, or by complementing traditional methods, allows soft-tissue augmentation and volume replacement, contour enhancement, and deformity correction with an additional side benefit of body contouring. It is a safe option that enjoys high satisfaction rates from surgeons and patients. Patients in both groups obtained a natural feeling and better fullness.
Because of ALCL, BII, capsular contracture, and general trends of our time to get lower and more natural feeling breasts, it looks like these indications will be increasing in the coming years as a reason to remove the implants. Our techniques should therefore be ameliorated. We must continue to pursue more evidence-based studies. More studies and longer follow-up studies are required.
It is preferable to perform implant conversion simultaneously because the skin is already expanded. Decanting for 10 min in a canister is performed after harvesting the fat with a vibration device using the PAL-650 Power-Assisted Liposuction from MicroAire®. The harvesting cannula was 4 mm, and the grafting cannula was 3 mm.
Abbreviations
- AFG:
-
Autologous fat grafting
- BIA-ALCL:
-
Breast implant-associated anaplastic large-cell lymphoma
- BII:
-
Breast implant illness
- TIVA:
-
Total intravenous anesthesia
References
American Society of Plastic Surgeons. National plastic surgery statistics. 2018. https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-full-report-2018.pdf. Accessed March 2020.
Sampaio Goes JC, Munhoz AM, Gemperli R. The subfascial approach to primary and secondary breast augmentation with autologous fat grafting and form-stable implants. Clin Plast Surg. 2015;42(4):551–64. https://doi.org/10.1016/j.cps.2015.06.017. Epub 2015 Aug 11. PMID: 26408443 Review
Nava MB, Blondeel P, Botti G, Casabona F, Catanuto G, Clemens MW, De Fazio D, De Vita R, Grotting J, Hammond DC, Harris P, Montemurro P, Mendonça Munhoz A, Nahabedian M, Pompei S, Rancati A, Rigotti G, Salgarello M, Scaperrotta G, Spano A, Stan C, Rocco N. International expert panel consensus on fat grafting of the breast. Plast Reconstr Surg Glob Open. 2019;7(10):e2426. https://doi.org/10.1097/GOX.0000000000002426. eCollection 2019 Oct. PMID: 31772879 Free PMC article
Coleman SR, Saboeiro AP. Primary breast augmentation with fat grafting. Clin Plast Surg. 2015;42(3):301–6. vii
Delay E, Garson S, Tousson G, Sinna R. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29(5):360–76.
Ho Quoc C, Taupin T, Guérin N, Delay E. Volumetric evaluation of fat resorption after breast lipofilling. Ann Chir Plast Esthet. 2015;60(6):495–9.
Khouri RK, Rigotti G, Cardoso E, Khouri RK, Biggs TM. Megavolume autologous fat transfer: part I. Theory Principles Plast Reconstr Surg. 2014;133(3):550–7.
Davis MJ, Perdanasari AT, Abu-Ghname A, Gonzalez SR, Chamata E, Rammos CK, Winocour SJ. Application of fat grafting in cosmetic breast surgery. Semin Plast Surg. 2020;34(1):24–9. https://doi.org/10.1055/s-0039-1700958. Epub 2020 Feb 15.PMID: 32071576 Review
Kalaaji A, Jönsson V, Baum M. Aesthetic breast augmentation using autologous fat grafting: indications, patient assessment, and comparison between different processing methods in 204 cases. Plastic and aesthetic regenerative surgery and fat grafting: clinical application and operative techniques. Springer Nature; 2021. Section XIII. Chapter XX
Auclair E, Blondeel P, Del Vecchio DA. Composite breast augmentation: soft tissue planning using implants and fat. Plast Reconstr Surg. 2013;132(3):558–68. https://doi.org/10.1097/PRS.0b013e31829ad2fa. PMID: 23985632
Auclair E, Anavekar N. Combined use of implant and fat grafting for breast augmentation. Clin Plast Surg. 2015;42(3):307–314, vii. https://doi.org/10.1016/j.cps.2015.03.005. Epub 2015 Jun 5. PMID: 26116936 Review
Auclair E, Marchac A, Kerfant N. Secondary composite breast augmentation: concept and outcomes, introduction to a layered approach. Aesthet Surg J. 2020;40(9):981–6.
Özalp B, Aydinol M. Breast augmentation combining fat injection and breast implants in patients with atrophied breasts. Ann Plat Surg. 2017;78(6):623–8.
Graf RM, Closs Ono MC, Pace D, Balbinot P, Pazio ALB, De Paula DR. Breast auto-augmentation (mastopexy and lipofilling): an option for quitting breast implants. Aesthet Plast Surg. 2019;43(5):1133–41. https://doi.org/10.1007/s00266-019-01387-5. Epub 2019 May 7
Del Vecchio D. SIEF—simultaneous implant exchange with fat: a new option in revision breast implant surgery. Plast Reconstr Surg. 2012;130(6):1187–96. https://doi.org/10.1097/PRS.0b013e31826d9c3c.
Hammond DC. Discussion: “SIEF”—Simultaneous implant exchange with fat: a new option in revision breast implant surgery. Plast Reconstr Surg. 2012;130(6):1197–8. https://doi.org/10.1097/PRS.0b013e3182717386. PMID: 23190804 No abstract available
Salibian AA, Frey JD, Bekisz JM, Choi M, Karp NS. Fat grafting and breast augmentation: a systematic review of primary composite augmentation. Plast Reconstr Surg Glob Open. 2019;7(7):e2340. eCollection. https://doi.org/10.1097/GOX.0000000000002340.
Kerfant N, Henry AS, Hu W, Marchac A, Auclair E. Subfascial primary breast augmentation with fat grafting: a review of 156 cases. Plast Reconstr Surg. 2017;139(5):1080e–5e. https://doi.org/10.1097/PRS.0000000000003299. PMID: 28445355
Maione L, Caviggioli F, Vinci V, Lisa A, Barbera F, Siliprandi M, Battistini A, Klinger F, Klinger M. Fat graft in composite breast augmentation with round implants: a new concept for breast reshaping. Aesthetic Plast Surg. 2018;42(6):1465–71. https://doi.org/10.1007/s00266-018-1240-9. Epub 2018 Sep 27.PMID: 30264274
Ørholt M, Larsen A, Hemmingsen MN, Mirian C, Zocchi ML, Vester-Glowinski PV, Herly M. Complications after breast augmentation with fat grafting: a systematic review. Plast Reconstr Surg. 2020;145(3):530e–7e.
Rigotti G, Marchi A, Stringhini P, Baroni G, Galiè M, Molino AM, et al. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthet Plast Surg. 2010;34(4):475–80.
Kronowitz SJ, Mandujano CC, Liu J, Kuerer HM, Smith B, Garvey P, et al. Lipofilling of the breast does not increase the risk of recurrence of breast cancer: a matched controlled study. Plast Reconstr Surg. 2016;137(2):385–93.
Stumpf CC, Zucatto ÂE, Cavalheiro JAC, de Melo MP, Cericato R, APS D, Biazús JV. Oncologic safety of immediate autologous fat grafting for reconstruction in breast-conserving surgery. Breast Cancer Res Treat. 2020;
Acknowledgement
The authors wish to thank Melanie Baumgartner, MD, for her contribution to this chapter in the beginning of the work.
Authors have no disclosures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Video 64.1
Simultaneous implant conversion with fat in a 35-year-old with MicroAire and decanting. Five years earlier, the patient had mastopexy augmentation with submuscular implant size of 275. The implant was removed, and 325 mL fat grafting was injected. Note the depression in the left vertical scar, which obliged us to make a lower entry incision) (PPTX 143998 kb)
Video 64.2
Simultaneous implant conversion with fat: 26-year-old woman who had a submuscular implant. 260/280 mL, implant conversion with capsular contracture grade 3. A conversion with fat grafting, 150 mL before removing the implant and 85 mL after removing the implant (PPTX 196438 kb)
Video 64.3
Simultaneous hybrid augmentation in a 29-year-old woman: 200-size round implants inserted subfascial with 125 mL fat graft was grafted around the implant per side between the fascia and the skin using MicroAire and decanting (PPTX 771276 kb)
Video 64.4
Delayed hybrid revision. Status after 350 mL submuscular implant insertion 1 year earlier in a 27-year-old woman; request to soften the edges as the implant. Two sessions of decanted fat were performed. Right: 150/175 mL and left: 150/175 mL. At the same time, an augmentation of gluteal area with fat was performed (PPTX 434952 kb)
Video 64.5
Mastopexy augmentation with posterior flap as auto-prosthesis and fat grafting, in 57-year-old woman, to augment the upper pole and cleavage areas. The fat was grafted (175 mL per side) through separate lateral and medial entry sites (PPTX 787882 kb)
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kalaaji, A., Jönsson, V. (2022). New Trends in Breast Augmentation with Fat Grafting: Implant Conversion with Fat and Hybrid Implant-Fat Breast Augmentation/Revision. In: Kalaaji, A. (eds) Plastic and Aesthetic Regenerative Surgery and Fat Grafting. Springer, Cham. https://doi.org/10.1007/978-3-030-77455-4_64
Download citation
DOI: https://doi.org/10.1007/978-3-030-77455-4_64
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-77454-7
Online ISBN: 978-3-030-77455-4
eBook Packages: MedicineMedicine (R0)