Abstract
The initiation of human cancer is primarily driven by carcinogenic substances including chemicals, radiations, viruses, and parasites. The carcinogenesis mechanism is a complex process in which cellular DNA mutations contribute to the initiation, which is the first step, and seems to be irreversible. The second stage is promoted over a long period and is largely reversible in initial stages. The key events for the carcinogenesis process tend to be epigenetic. Cancer genes are classified by their ability to regulate oncogenesis as the dominant oncogenes and recessive tumor suppressors. Activation of oncogenes may be due to the occurrence of mutations in these genes. Besides, a single sufficiently activated oncogene will initiate the entire process of the cancerous transition of a normal cell. Their function in cancer growth has been widely demonstrated in experimental studies involving viruses and chromosome translocations. Furthermore, micro-RNAs (miRNAs) are preserved throughout development and regulate gene expression during cell proliferation, growth, and even in cancer progression by an unidentified control mechanism. miRNAs also play a crucial function in malignancy. The discovery and elucidation of the carcinogenic molecular pathways of carcinogens provide a deeper understanding of how genetic manipulation influences the mechanism of neoplastic development. The current chapter explains the different mechanisms involved in the carcinogenesis process.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Cancer is a debilitating and life-threatening disease. 5–10% of human tumors are believed to be induced by virus and bacteria, and the remaining 90–95% by environmental factors due to alterations in genes. Among these, an additional 30% were induced with the consumption of tobacco-related products and the remaining by food, and environment-related chemicals. Cancer cells are generated by our own tissues, but several internal and external causes can be connected to the risk of getting cancer for a lifetime (Yokota 2000). Although cancer as such is not contagious, certain infections may serve as a stimulus to induce and facilitate the proliferation of cancer cells. In the 1970s, cancer was defined in a pathology text by Cappell and Anderson, who presented malignancy by describing a tumor as “an abnormal mass of tissue, the growth of which exceeds and is uncoordinated with that of the surrounding tissue, and that continues to grow in the same excessive manner after cessation of the stimulus that caused it”. The basis of cancer is monoclonal, so genetic mutations may arise on it, in order for a regular cell to alter its shape and become a neoplastic cell. Such genetic mutations change the proteins which the gene will codify under normal conditions and ultimately cause cancer (Mendelsohn et al. 2008; Vancheri 2016). Carcinogenesis may result from anyone or a mixture of chemical, physical-biological, and genetic disruptions to single cells in a multicellular animal. The analysis of the general carcinogenesis process takes into account the vast number of factors concerned, the prolonged period between the function of a cause and the clinical occurrence of the disease, which makes it hard to accept the pathophysiological importance of certain microorganisms. The carcinogenic substance is nucleophilic whether it functions directly or indirectly. The target of the carcinogenic component is chromosomal DNA, where a lesion can be replicated or reversed (Murphy and Charnay-Sonnek 2019).
The carcinogenesis theories can be grouped as follows: the theory of genetic mutation, the theory of aberrant differentiation, viral theory, and the theory of cell selection. A theory which is unanimously accepted is the multi-stage theory (Hart and Turturro 1988). Carcinogenesis is a complex process because there are several phases between the initial carcinogenic stimulation and the final cancer manifestation. The time between the exposure of a carcinogen on chromosomal genes and the emergence of a neoplastic cell population can be categorized into the following phases: initiation, promotion, and progression (Barrett 1993).
2 Phases of Carcinogenesis: Initiation, Promotion, and Progression
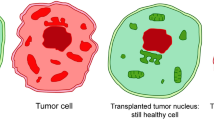
The incidence of tumors in humans and animals will rise in many different types of carcinogenic exposure, but it usually takes a long time before the carcinogenic risk of exposure is manipulated. Berenbaum and Schubik first introduced the concept of multi-stage carcinogenesis in 1948 (Berenblum and Shubik 1949), and later confirmed by studies. Foulds, L. (Neoplastic Development, Academic, New York, 1969), had the insight of its stage development in the evolutionary history of cancer and Berenblum pointed out three distinct stages: the phase of initiation, the phase of promotion, and the phase of progression (Rubin 1994; Weiss 2004). Certainly, the firsttwo phases help to explain the cell transformation mechanism, the third level dictates the conversion of a benign tumor into a malignant type, with malignancy sustaining and evolving (Fig. 2.1).
Phases of carcinogenesis: Carcinogenesis phases: initiation, promotion, progression. The effect of anyone or a combination of factors such as chemical, physical, biological, environmental, and/or genetic alterations on cells may eventually lead to carcinogenesis. Such modification initiates the cell which acquires/loses different functional aspects (proliferation conduct, cell death pathway modified, etc.). In the Promotion process, the activated clone is intensified, and the cell acquires metastatic potential through development as well as through mutations
The established multi-stage carcinogenic paradigm typically involves more than 80 alterations or modifications in the cancer genome, which are the key players for cancer growth pathways. Carcinogenesis hallmarks involve genetic alterations comprehending: maintaining proliferative signalling; preventing growth suppressors; suppressing apoptosis; facilitating replicative longevity; triggering angiogenesis; initiating invasion and metastasis; implanting energy metabolism, and preventing immune depletion (Hanahan and Robert 2017).
2.1 Initiation
During research on skin carcinogenesis in mice, the pathogenesis of initiation and promotion were initially identified and have since been extended to a range of other tissues and organisms (Abel et al. 2009). A regular cell endures an irreversible transition during the initiation phase of carcinogenesis, represented by an intrinsic ability for autonomous growth. For weeks to years, this potential for autonomous development persists latent, during that period the activated cell can be genetically differentiated from entire parenchymal cells in a particular tissue region. Spontaneous initiation will arise when the operation of DNA polymerase throughout normal cell proliferation or DNA repair becomes abnormal. Operational activation infers that cellular DNA alteration occurs at one or more locations inside the genome (Stratton et al. 2009; Vogelstein et al. 2013). This modification reflects a genetic mutational phenomenon. Within limited hours of exposure, there is metabolic activation of a carcinogen and its subsequent reaction to target DNA bases. Most tissues have the capacity over days or weeks to repair this damage. Currently accepted theory indicates that, if not initially restored by natural cellular processes, the carcinogen compromised DNA is transformed into a permanent genetic lesion through DNA replication. Therefore, the genetic lesion is then believed to be “secure” if a round of cell division occurs until the DNA damage is corrected. This effect can clarify the high prevalence of neoplasms in multiplying tissue, in which the cell turnover rate correlates with exposure to a carcinogen. Contrary to the initiation stage, the conversion of an initiated cell to a completely malignant neoplasm is typically a protracted phase, in animals lasting months and in human’s years (Oliveira et al. 2007). Depending on the possibility that most initiators are mutagenic or genotoxic, the changes that arise during initiation, trigger a permanent and inherited existence. Initiators associate in specific patterns with host cellular macromolecules and nucleic acids, usually entails the production of reactive species or free radicals that covalently attach in crucial cellular macromolecule nuclear sites.
Several pieces of evidence propose that contact of laboratory animals to chemicals with initiating operation inevitably leads to several neoplasms caused in a specified tissue. That specific neoplasm is regularly shown to have initially been monoclonal, started to emerge from a particular induced cell(Vincent and Gatenby 2008; Abel and DiGiovanni 2011). In addition to that, initiation is exponential and neoplasm yield is carcinogen concentration-dependent. Adding the dosage of initiator improves the frequency and abundance of resultant neoplasms, and decreases the time to neoplasm appearance. Since a round of cell proliferation will repair the initiating case, It is evident that initiation relies on the cell division (Barrett 1993; Grizzi et al. 2006). Yet the optimal dosage for maximum and minimum initiator response may differ between individuals.
2.2 Promotion
Many recognized carcinogens have both initiating and promoting action and, if consistently delivered, may cause neoplasms rapidly and with high yield. A cell that has experienced an irreversible transition enabling its eventual neoplastic transformation conversion may possibly be phenotypically identical from the neighboring standard parenchymal cells. It has, nevertheless, inherent potential for autonomous development if adequately stimulated. General characteristics of the initiator and promotor are summarized in Table 2.1.
Classically, promotion is called a portion of the multi-stage carcinogenic mechanism where particular substances, referred to as promoters, facilitate the production of neoplasms from the context of induced cell population. Typically, after initiation, a promoter is administered at some point, and the concentrations of the promoter used will be inadequate for cancer development. However, when the promoters are delivered at relatively high concentrations, and for over long periods, neoplasia can occur with no prior initiation. Under such circumstances, a promoter must be treated as a carcinogen. Further, when an agent is supplied concurrently with an initiator, which results in the production of neoplasms being accelerated, it is known to be a co-carcinogen instead of a promoter (Hecker 1978). Although certain promoters, like phorbol esters, maybe co-carcinogenic, not all promoters such as phenol, phenobarbital contain co-carcinogenicity and, alternatively, not that all co-carcinogenic are promoters. Promoters involve compounds such as drugs, phytochemicals, and hormones that are not genotoxic but somehow affect the transcription of the cellular DNA encoded genetic information. It has been proposed thatgene manipulation and instability can be induced by fostering agents. Many experimental evidences show that gene manipulation is specific to the feature of the treated promoter(Derelanko 2001; Cohen and Arnold 2011). Several promoters are assumed to achieve their results by association with receptors present in the cell surface, cytosol, or nucleus. Conversely, certain hydrophilic and hydrophobic promoters impose their activity at the cellular interfaces by their molecular configuration. Some promoters are mitogenic, promoting transcription of DNA and enhancing the proliferation of the cells. This can happen explicitly or, similarly, obliquely by manipulating cells with a shorter G1 process, thereby granting them a proliferative selective advantage. Tissue culture experiments have shown that such promoters hinder intercellular interaction (Loeb and Harris 2008).
Empirical evidence reveals that the molecule as a whole can influence the promotional impact and the compound activity is defined by the molecular settings. If the promoter undergoes metabolism, it inevitably results in the inactivation of the promoter. Promoters tend to have a fairly strong sensitivity to the tissue. For example, phenobarbital acts as a promoter in rat liver carcinoma, although not in the urinary tract. In comparison, 12-0-tetradecanoylphorbol-13-acetate is a strong neoplasm promoter for the skin and forestomach, which has no significant liver function. 3-tert-butyl-4-methoxyphenol and 2,6-ditert-butyl-4-methoxyphenol that serve as promoters in any one organ, act as an anti-promotor in second organ, and shows no impact in the other organ (Frenkel et al. 1993). Therefore, a promoter’s functional description may provide the description of the responsive tissue.
Experimental proof of the function of relatively high-fat food in fostering mammary cancer has been reported in rats subjected to mammary carcinogen 7,12-Dimethylbenz[a]anthracene (DMBA)(Zarbl et al. 1985). Likewise, bile acids are recognized as promoters in rat liver carcinogenesis, since they are modulated by fat intake(de Gerlache et al. 1987). Based on clinical epidemiology research, demographic-and gender-associated modulations of hormone rates of progesterone, estrogens, and androgens are inferred as possible promoters of breast cancer. Laboratory findings have shown consistently that these hormones help to facilitate mammary cancer in rats conducted with mammalian carcinogens along with pituitary prolactin (Clevenger et al. 2003). Hyperplasia and/or inflammation are induced by certain promoters. It is particularly valid in studies of epidermis initiation–promotion utilizing phorbol esters used for promotion activity but often seen in hepatocyte hyperplasia after treatment with mutagenic agents like phenobarbital. Phenobarbital induces temporary hepatocyte hyperplasia in the rat liver. It should be noted that certain substances can cause hyperplasia and inflammation which may occur without the promotion process (Lewis and Adams 1987).
2.3 Progression
The process of carcinogenic development is an extension of the tumor promotion step and proceeds from the fact that cell proliferation caused by stimulating factors enables the spread of cell damage acquired by initiation. Morphological characteristics prevail that the activated cells are clonally dispersed, consisting of constant clonal replication of the transformed cells, during which there is no modulation of growth and escape from the host resistance pathways (Ruddon 2010). The progression phase is demonstrated by karyotypic destabilization and the development of aneuploid, permanent, malignant cells (Olson 1992). During the progression process, some genetic and epigenetic changes may occur, frequently involving protooncogene stimulation and the suppression of tumor suppressor genes to act. Further, two major pathways also induce protooncogenes: where RAS gene family, point mutations can be found in specific genomic regions and MYC, RAF, HER2, and jun multigene families may be over-expressed, often contributing to chromosome segments containing such genes being amplified (Harris 1991). The presence of a genetic alteration in the former genome and the lack of quantifiable systemic changes in the latter differentiates the progression from the promotion. The emerging new technologies focused on histochemistry and on-site hybridization, will represent both structural genomic modifications and biochemical changes specific to tumor growth. Furthermore, oncogenic proteins allow us to distinguish between benign to malignant neoplasms in the various stages of development (Elder 2016). In certain scenarios, symptoms of more advanced malignancy may be identified before the neoplasm reaches macroscopic size; in other circumstances, well-defined slow-growing tumors may persist for years until a reasonably rapid transition to more destructive behavior (Conti 2010). Both cases of acceleration or retardation by extrinsic causes are prone to progression. Initiating agents tend to decide the direction and stage of progression and their prolonged invasion may accelerate the progression outcome beyond the minimum needed to cause a tumor; however, progression is independent of such carcinogenic agents until the initiation phase is sufficiently advanced (Polonara et al. 2012).
3 Mechanisms of Carcinogenesis
With the advancement of the latest developments of molecular biology, such as profiling of gene expression, systems biology, microRNAs , gene exploration, and pathway research, carcinogenesis is becoming even more complicated than merely being a clonal mutation of a cell that suffered twin genetic “hits” from a carcinogen. Such molecular changes result from the accumulation of genetic programs modifications that regulate the proliferation of cells and its lifespan, relations with adjacent cells, and the ability to hide from the immune response. That process ends to result in a mass of deregulated cells being produced. For a longer period, such a mass might be asymptomatic. It will also expand and disrupt the physiological processes, resulting in different manifestations of position and relative magnitude of the mass and the distribution of cancer cells throughout the body.
3.1 Oncogenes Activation
The cancer-targeted genes are found in hundreds that are distributed throughout the human genome. Human DNA is thought to contain around 23,000 genes. Thousand of those genes (3000–5000) encode for proteins that are implicated in cancer deregulated genetic processes. A defective gene may result in the development of excessive amounts of a vital protein, the production of an aberrant protein, or the complete lack of the protein (Croce 2008; Hartl and Bister 2013). A proto-oncogene is a natural gene that, after a genetic modification (mutation), can become an oncogene, resulting in enhanced transcription. Normally, proto-oncogenes code for proteins that regulate cell proliferation by transducing signals and conducting mitogenic signals. The oncogene protein is a tumor-inducing agent when activated. Best recognized proto-oncogenic sources include RAS, ERK, MYC, WNT, and TRK (Botezatu et al. 2016). The other oncogene BCR-ABL gene was located on the Philadelphia chromosome, a genetic mutation in chronic myelogenous leukemia caused by chromosome 9 and 22 t translocation (Pane et al. 2002).
Oncogene activation through structural alteration such as mutation, gene fusion, chromosomal rearrangement, and genome amplification or epigenetic change such as gene promoter hypomethylation, the microRNA expression gives an enhanced or deregulated expression; cells containing these modifications also have continuous growth or an enhanced rate of survival. For instance, mutation in KRAS gene transforms a protein located right inside the cell membrane into a signaling multiplier for cell development. This protein generally works as a signaling intermediate between surface growth factor receptors and molecular wiring systems that deliver growth signals to the nucleus for the cell replication to take effect. When the KRAS gene is mutated, the corresponding protein acts as a switch locked in the “on” position, generating a permanent division signal for the cells. KRAS mutations are common in many cancers, such as colorectal cancers (about 40% of cases), or lung adenocarcinomas (about 30% of cases). This triggered gene is considered an “oncogene,” since it facilitates the proliferation of cells (Jančík et al. 2010; Fearon 2011; Karachaliou et al. 2013) (Table 2.2).
A few cancer syndromes are triggered by hereditary proto-oncogene mutations that enable the oncogene. However, most oncogene mutations that develop cancer are inherited, not genetic. They usually enable oncogenes through chromosome rearrangements which leads to shifts in chromosomes that cause one gene to trigger the other and gene duplication which leads to extra copies of a gene that may contribute to the abundant generation of a certain protein.
3.2 Tumor Suppressor Gene Inactivation
Tumor suppressor genes (TSG) are the reverse hand of cell growth regulation, usually functioning to prevent cell proliferation and production of tumors. Such genes are defective or inactivated in several cancers, thus suppressing negative cell proliferation regulators and leading to excessive tumor cell proliferation. TSG operates to control cell growth and proliferation within the genome. They also assist with pathways for the repair of DNA and other essential cellular signals including the apoptosis pathway (Wang et al. 2018). The very first insight into the role of TSG resulted from studies concerning somatic cell hybridization, pioneered in 1969 by Henry Harris and his colleagues (Harris et al. 1969). There is a large chance of disordered cell development which can contribute to malignant tumour without the activated tumor suppressor genes. Loss of function mutations in TSG has also been reported in several forms of cancer comprising ovarian, kidney, colorectal, head and neck, pancreatic, uterine, breast, and bladder cancer.
In cancer, the failure of TSG activity happens, according to Knudson’s two-hit model theory, by removing or inactivating two alleles. It is now apparent that alterations in TSGs are suppressive at a specific cell level; thus, a point mutation in a TSG is not necessary to induce cancer. Some experiments, however, have described candidate TSGs that do not follow this normative description, including genes that are inactivated through epigenetic silencing rather than deletion. In addition, the inactivation of TSGs often includes proteasomal degradation by ubiquitination, irregular cellular localization, and transcriptional control (Wang et al. 2018). For eg, the TP53 gene encodes a protein that normally functions as an “emergency stop” to prevent the improper division of the cells. Mutation in this gene interferes with the protein, which is unable to resist cell proliferation when required. Mutations in TP53 occur in almost all types of cancer. Such a gene that contributes to the production of cancer by losing its role is called a tumor suppressor since its active products serve as a brake under normal conditions to subdue the cancer cell growth (Gariglio 2012) (Table 2.3).
3.3 Association Between Infectious Agents and Carcinogenesis
3.3.1 Oncogenic Virus
The carcinogenic mechanism includes multiple influencing factors that involve external conditions, diet, host characteristics, hereditary genetic features, and infectious agents. Infectious agents are essential because they reflect a major and preventable source of cancer from a public health perspective. The frequency of infection-attributable cancer was recorded in the global occurrence of cancer in 2018 as 18.1 million new cancer cases (17.0 million except nonmelanoma skin cancer) and 9.6 million cancer deaths (9.5 million except nonmelanoma skin cancer) (Bray et al. 2018). The International Agency for Research on Cancer (IARC) identifies seven viral factors which have been known to be carcinogenic which include Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV) , Epstein-Barr Virus (EBV) , Human Papilloma Virus (HPV) , Kaposi-Sarcoma Herpes Virus (Human Herpes Virus 8), Human Immunodeficiency Virus type 1 (HIV) and Human T-cell leukemia virus type I (HTLV-1) . The inductionof cancer formation by viruses includes sustained invasion of the organism. Long-term infection is hypothesized to cause cellular changes that predispose to the progression of cancer. Examples of recurrent infections correlated with ongoing inflammation include HBV and HCV infections. HBV and HCV are responsible for 54% and 31% of the worldwide reports of clinical hepatocellular carcinoma (HCC)(El-Serag 2012). Such a hepatotropic virus causes cirrhotic livers that may trigger the development of HCC.
Individuals with HIV have a slightly greater chance of some tumors relative to those of the same sex that are uninfected. Such tumors are considered malignancies associated with AIDS which include Kaposi sarcoma (a mesenchymal tumor, originates from lymphatic endothelial cells), cervical cancer, and Non-Hodgkin Lymphoma (Braoudaki and Tzortzatou-Stathopoulou 2011). However, certain forms of cancer, such as Hodgkin’s disease (HD), anal cancer, lung cancer, and testicular germ cell tumors, tend to occur frequently in HIV-infected individuals relative to the common population and are referred to as AIDS-associated cancers. HIV is a family of Retroviridae, RNA lentivirus. The viruses that belong to this group merge into the host genome and thus have the ability to induce direct induction mutations or cellular oncogene activation. Many members of the Retroviridae family, such as Mouse mammary tumor virus (MMTV), has a very well-defined association with mice’s tumors that are possibly mediated by the insertion of cellular genes in the breast tissue via hormone-response elements in the MMTV promoter (Hacein-Bey-Abina et al. 2008).
In addition, EBV, Human herpesvirus 8, HTLV-1 , and HPV, some of the carcinogenic viruses that have been identified and recognized, are tumor viruses that develop oncogenic viral proteins for carcinogenesis. Oncogenic viruses can transform cells by transferring viral oncogenes to a cell or by inducing cell proto-oncogenes (Zheng 2010). Virally mediated oncogenes release manipulating signaling molecules that deregulate regulation and proliferation of development, resulting in malignant transformation. Oncogenic viruses categorized into DNA and RNA tumor viruses are given below.
3.3.1.1 DNA Tumor Virus
EBV is a Herpesviridae family with double-stranded DNA that induces contagious mononucleosis. EBV induces a life-long persistent infection for other herpesviruses, so EBV is the main source of B-cell development in Burkitt’s lymphoma (Orem et al. 2007). This became the first human tumor diagnosed with an infectious agent. EBV has also become implicated in a variety of other cancers. The presence of the viral oncogene, latent membrane protein-1 (LMP1), in the case of EBV-lymphoma, turns cells into lymphoblasts by blocking cellular signal transduction. By contrast, the BamHI-A viral read frame-1 (BARF1) gene is expressed in most Nasopharyngeal Carcinoma (NPCs). In NPC pathology, BARF1 was established as an essential oncogene. Therefore, EBV has multiple oncogene expression profiles that are consistent with specific cancers. The incidence of EBV is highly prevalent impacting more than 90% of the world’s population, and only a limited percentage of affected people develop an EBV-attributable disease (Raab-Traub 2002; Brennan 2006).
3.3.1.2 RNA Tumor Virus
HCV is an RNA virus of the genus Flaviviridae family of hepaciviruses. HCV is not incorporated within the host genome and some key proteins have been identified as possible oncogenic candidates in vitro, including nonstructural (NS) protein 3, NS protein 4B including NS5A. It has been shown, that the HCV NS5A protein binds and sequesters the cellular p53 protein to the perinuclear membrane, which could be crucial to HCC growth (El-Serag 2012). HTLV-I is an HIV-related retrovirus that is associated with adult T-cell leukemia. Just 1% of HTLV-I contaminated people can experience leukemia, and only after a long delay time of 20–30 years. In comparison to HIV, HTLV-I infections are not linked with immunosuppression. However, HTLV-I encodes an oncogenic protein (Tax), which is known to bind to several cellular genes involved in the cell growth and control of cell cycle production, such as NFkB and p53. By encouraging synthesis and progression of the cell cycle, Tax is proposed to create a self-stimulating loop that induces increased proliferation of contaminated T-cells, and eventually leukemia (Shuh and Beilke 2005; Martin et al. 2016).
3.3.2 Oncogenic Bacteria
It is commonly thought that bacterial infections cause chronic infections and diseases , including cancer (Vogelmann and Amieva 2007). The involvement of bacteria in carcinogenesis is due to chronic inflammation triggered by recurrent bacterial infections and secondary metabolites (bacterial toxins) generated by chronic carcinogenic bacterial infections. Hence comprehending the carcinogenesis stimulated by bacteria could allow us to prevent and treat certain forms of cancers (Lax and Thomas 2002).
There could be different carcinogenic mechanisms caused by chronic bacterial infections. The presence and abundant release of inflammatory mediators is a common characteristic of chronic infections. Transcription factors like the nuclear factor-κB (NF-κB) family have been linked to inflammatory response-driven carcinogenesis (Karin and Greten 2005). Bacterial pathogens and even pro-inflammatory cytokines like TNF-α and IL-1 activate the mechanism for NF-κB. Further, the mentioned pathway involves the activation of IKK (inhibitor of nuclear factor kappa B) complex and the destruction of NF-κB inhibitors, thus trying to free NF-κB to reach the nucleus and mediate the intended transcriptional activity. Some of the genes related to apoptosis inhibition pathways , like p21, p53, and pRb, are found to be decreased in expression, while the genes associated with cell cycle regulation, such as cycline D1, CDK2 kinase, c-myc (cell cycle regulators), are significantly up-regulated by NF-κB. NF-κB often upregulates various cytokines, such as IL-1β, IL6, Vascular endothelial growth factor (VEGF) (proinflammatory and proangiogenic), but decreases TNF, thus promoting tumor development. In addition, the genes related to invasion and metastasis are also upregulated by NF-κB (Van Antwerp et al. 1996).
A limited list of possible bacterial toxins implicated in carcinogenesisis listed in Table 2.4. The toxins could either destroy the cells or manipulate the cellular processes that govern cell division, DNA damage, apoptosis, and differentiation. Such toxins interact either with the cell signaling factors or specifically with DNA. Harm to host cells may be caused by an enzymatic attack, by influencing DNA damage repair mechanisms or triggering persistent inflammatory reactions and generating free radicals (Herrera et al. 2005; Nath et al. 2010).
3.3.3 Oncogenic Parasites
Parasitic infections also have been known for years to be associated with human carcinogenicity. Helminth parasite infections such as schistosomiasis, opisthorchiasis, and clonorchiasis are extremely carcinogenic, however, malaria doesn’t seem to be causative to carcinogenesis. Whereas, the protozoan Trypanosoma cruzi, the causative agent of Chagas disease plays a dual role as a carcinogenic and an anti-cancer agent. Plasmodium falciparum involves additional transition events caused by the Epstein-Barr virus (EBV ) driven Burkitt lymphoma . When the red blood cells which are infected with the P. falciparum interact (via P. falciparum erythrocyte membrane protein 1’s CIDR1 domain) with the B cells that are infected with EBV, it leads to the proliferation of the infected B cells and also the activates the EBV. The interaction between iRBCs and EBV-infected B cells is also the result of an enhanced expression of Activation Mediated Cytidine Deaminase (AID). In specific, AID contributes to the breakdown of host DNA resulting the activation of oncogenes (c-Myc) (van Tong et al. 2017). Most of the parasitic infection is associated with carcinogenesis through inflammation and oxidative stress caused by parasite-derived molecules. Some of the parasites and the associated cancer types are listed in Table 2.5.
Chronic inflammation caused during infections with Opisthorchis, Clonorchis,and Schistosoma contributes to the stimulation of signal transduction pathways, including NF-κB , p53, Jak/Stat, and Rb, which may induce somatic mutations and/or trigger oncogenes. Further, the parasite metabolites secreted to the recipient microenvironment may induce various metabolic functions, especially oxidative stress, which promotes disruption to the chromosome DNA of proximal epithelial cells, particularly urothelial and cholangiocytes cells of the liver (van Tong et al. 2017). In addition, the physical disruption to the host infected cells during the growth of parasites, along with the successful tissue repair cycle, contributes to enhanced cell regeneration and proliferation, which is also correlated with DNA damage. Coupled parasitic organism-host association events like chronic inflammation, parasite-derived metabolites, and nuclear DNA damage contribute to a shift in cell differentiation, proliferation, and viability that, in turn, initiates and encourages malignancy (Vennervald and Polman 2009). However, thorough observations into such interactions and/or recognizing the functional implications of both parasite and host influences have not yet been obtained. Studies based on the detection of carcinogenic parasite influences through increasing the processes of host signal transduction pathways or oncogenes resulting in the activation of cancer propagation are also needed.
3.3.4 Oncogenic Fungi
The cancer causing mycotoxins could be exposed through absorption or by inhalation and also through the food that is infected. Asergillus flavus and Aspergillus parasiticus fungi species produce mycotoxins, and these mycotoxins which are termed as aflatoxins have been identified to be highly toxic (Gourama and Bullerman 1995). When the aflatoxins penetrate the cells, the cytochrome P450 metabolizes them, results in the production of aflatoxin-8, 9-epoxide. It is extremely reactive and unpredictable and involves attachment to DNA or to a cluster of protein with high affinity in order to be more stable and it forms aflatoxin-N7-guanine, which cause transverse mutation. It further influences the cell cycle directly by manipulating the p53 genome (Kew 2013).
Human beings are regularly exposed to mycotoxin, such as aflatoxins, ochratoxins, primarily from plant and animal sources. The health threats resulting through mycotoxins could be due to their potential toxicity, in specific their carcinogenicity potential. Mycotoxins, particularly aflatoxins, ochratoxin A (OTA), citrinin (CIT), patulin, fumonisin B, ochratoxin A, zearalenone, have been identified to induce cancer, which are summarized in Table 2.6. New knowledge of the genotoxicity of mycotoxin (formation of mycotoxin-DNA adducts), the function of mycotoxin in oxidative damage and the discovery of epigenetic modifications involved in mycotoxin carcinogenesis provide compelling evidence that mycotoxin carcinogenicity is driven by various signaling mechanisms that exists in humans (Ostry et al. 2017).
3.4 Involvement of MicroRNA in Cancer
Small regulatory RNAs may be classified into two main classes: microRNAs (miRNAs) and small RNAs interfering (siRNAs). miRNAs are short 22–25 long non-coding nucleotides that are retained throughout development, which regulate gene expression in multicellular organisms, plants, viruses, and bacteria mainly at transcription and post-transcription processes, although the yeast genome is considered to lack miRNA genes. miRNAs control specific gene transcription by breaking down the associated mRNA and/or inhibiting its translation process. Presently, miRNA ‘s vital mechanisms have been established to regulate the immune function, cell growth, differentiation, cell cycle, and carcinogenesis (Ahmad et al. 2013). In the human genome, miRNAs are likely to be present at least 400 numbers, and possibly as high as around 1000. Concerning complex evolution, the wide estimated number of miRNAs found in higher mammals may indicate their possible role in regulating more precise gene expression (Esquela-Kerscher and Slack 2006; Bushati and Cohen 2007). Annotation of miRNAs genome locations suggests that most miRNAs genes are situated in intergenic domains, they are often present inside exonic or intronic areas but in either context or anti-sense direction. Localized miRNAs have been referred to as ‘mirtrons’, present inside protein-encoding introns or non-encoding genes. miRNAs may be grouped as a single gene or placed as clusters containing a family of miRNAs typically linked in sequence and function. miRNAs are transcribed predominantly by RNA polymerase II (RNA pol II) out of their own promoter or from the promoter of the host gene they live in. miRNAs impose their genetic regulation activity mainly by defective base pairing to the 3′ UTR of its target mRNAs, resulting in depletion or translational suppression of mRNA. In cancer, miRNAs are frequently disordered with their patterns of expression being associated with clinically important tumor characteristics (Peng and Croce 2016).
miRNAs have recently been shown to function specifically in the development and advancement of cancer. The first proof of miRNAs being associated withhuman cancer results from chronic lymphocytic leukemia (CLL) research. The key chromosome region 13q14, which is regularly lost in CLL, but two miRNA genes like miR-15a and miR-16-1 are expressed within polycistronic RNA (Calin et al. 2004). Growing research indicates that human carcinogenesis may include an archetypal miRNA, let-7. The research documented the regular incidence of substantially decreased expression of family members of the let-7 miRNA genes in lung cancers. Such ideas of the possible biological activities of altered miRNA in human cancers are also strengthened by the detection of RAS as a target gene for let-7 (Yanaihara et al. 2006). In C. elegans, the let-7 family negatively controls the encoding of let-60 genes in tiny GTPases (RAS oncogenes homologs), while let-60/RAS deficiency suppresses the let-7 mutant phenotype. It has been found that the human RAS gene also comprises of various complementary let-7 sites and is controlled by let-7, which provides clues to a mechanistic explanation for let-7 changes in human lung cancer. Another archetypal miRNA, lin-4 could also contribute to carcinogenesis in humans (Hristova et al. 2005). Lin-14, the lin-4 target, is a transcription factor that regulates several downstream processes. miR-125b -mediated downregulation of lin-28 was indicated to lead to neuronal carcinoma, while miR-125b depletion was shown to have significant inhibitory effects on the proliferation of adult differentiated cancer cells rescued by co-transfected, mature miR-125b (Lee et al. 2005). However further studies need to be carried out to validate the significance and potential roles of miRNA signalling in carcinogenic processes.
3.5 Role of Epigenetics in Cancer
Epigenetic variations have a pertinent impact on cancer. Considerably, earlier this century, science and clinical associates specifically reported that epigenetics dysregulation leads to structural and inheritable changes in chromatin function impacting the whole epigenome without modifying the DNA sequence. This involves DNA methylation, post-translational histone alteration, and microRNA interference with RNA, and inactivation of primary cell regeneration pathways involved in carcinogenesis and its progression (Lee et al. 2005; Jones and Baylin 2007). These epigenetic changes will be stable to preserve the same cell lineage or dynamic to retaliate to the development and the environment signals of the cell (Jones and Takai 2001). A different kind of epigenetic mechanisms is sometimes diversified in different types of cancer, including the silencing of tumor suppressor genes (TSG) and stimulation of oncogenes by different patterns of CpG island methylation, histone modifications, and DNA binding protein impairment.
3.5.1 DNA Methylation
DNA methylation is possibly one of the most extensively studied epigenetic modification in mammals. It is quite stable and acts as a specific epigenetic memory of particular cells during the cell cycle throughout all generations. It can also control histone code expression and activity. DNA methylation mainly emerges in mammals by the covalent alteration of cytosine(C) residues which is bound to a guanine(G) by a phosphodiester bond in CpG dinucleotides. CpG dinucleotides are not uniformly dispersed throughout the human genome but rather focus in short CpG-rich DNA stretches called ‘CpG islands’ and wide repetitive sequence regions (Saxonov et al. 2006; Klose and Bird 2006; Sharma et al. 2010). Extensive hypomethylation of DNA by DNA methyltransferase enzymes such as DNA methyltransferase 1 (DNMT1), DNMT3a, and DNMT3b occurs during tumor formation in repetitive DNA elements and intergenic regions. Methylatable genomes forfeit sequences of CpG owing to mutability by the addition of methyl group to cytosine that will suddenly deaminate to thymine. For example, it can prevent transcriptional activity by inhibiting transcription factors from entering target-binding sites such as c-myc and Membrane-bound lytic mureintransglycosylaseF (MLTF). This tends to result in chromosomal aberrations, genomic instability, mutagenesis, and perhaps carcinogenicity (Jones 2003).
Consequently, DNA hypomethylation may result in the activation of growth-promoting genes such as R-Ras, cyclin D2, and mapsin (a member of the serpin family of serine protease inhibitors) in stomach cancer, S-100 in colorectal carcinoma, and MAGE (melanoma-associated antigen) in melanoma, and loss of imprinting (LOI) in carcinomas. In Wilms’ cancer, the hypomethylation-induced LOI of insulin-like growth factor 2 (IGF2), a significant autocrine growth factor, leads towards its pathological expression of biallelic, which is also associated with an elevated risk of colon cancer. Besides, altering gene-specific methylation can result in alterations in gene expression and the transformation of the malignant cell. Besides hypomethylation which influences genomic instability and stimulates proto-oncogenes, site-specific hypermethylationalsoleads to carcinogenesis by silencing genes that suppress tumors. From the early observation of the Rb promoter (a retinoblastoma-associated TSG) on CpG island hypermethylation, several other TSG, particularly p16 in non-small cell lung cancers, breast, prostate, and several other tumors, MLH1 1 in colorectal and uterine carcinomas and BRCA1 in breast cancer, has also been reported to endure in tumor-specific silencing by hypermethylation which further allows the cells to accrue additional genetic lesions resulting in a rapid progression of cancer. Hypermethylation of TP53, APC, and RASSF1A (Ras association domain-containing protein 1) promoter regions is identified as crucial epigenetic markers to detect cancer development (Coyle et al. 2007; Kanwal and Gupta 2012; Sanchis-Gomar et al. 2012).
3.5.2 Histone Modifications
Anomalous histone modifications are reported to serve as a crucial factor in the pathogenesis of many human diseases including cancer, neurodegenerative and inflammatory diseases. Histone proteins that constitute the nucleosome core have a C-terminal globular domain as well as an unstructured N-terminal tail. Several post-translational covalent modifications, including methylation, phosphorylation, acetylation, ubiquitination, will be carried out by histone N-terminal tails, the well-studied and most significant in chromosomal structure regulation and function contexts. The tendency of the protein to acetylate non-histone transcription factors, p53 and BCL6, is an aspect of the function of histone acetyltransferase (HAT) found by the different mutations in CBP and EP300. In addition to the absence of p53 and BCL6 acetylation , their transcriptional activator and repressor functions abrogate, making the subsequent cells very tumorigenic via aberrant pathways that sustain DNA damage duringapoptosis and cell cycle arrest (Sawan and Herceg 2010; Pasqualucci et al. 2011). H3tre11 is a particular substrate for tumor-specific pyruvate kinase M2 (PKM2) in transcription initiation mediated by Epidermal growth factor (EGF) and acetylation of histone 3 lysine 9 (H3K9), ensuing in tumor cell proliferation. H2Bser32p exists prevalently in human cells nevertheless, it is also comprehensively phosphorylated in skin cancer cells by RSK2 kinase (an RSK family kinase AGC). Janus kinase 2 (JAK2) is often shown to phosphorylate H3tyr41, further obstructing the heterochromatin protein 1α (HP1α) binding with chromatin . HP1α has been reported to associate directly with H3 via their chromo-shadow domain. The removal of HP1α from chromatin consequently results in constitutive activation of the JAK2 signaling pathway, including oncogene imo2, contributing to carcinogenesis (Shanmugam et al. 2018).
3.5.3 Dysregulation of miRNAs Expression
Transforms in miRNAs expression might be processed in several mechanisms involving chromosomal anomalies, binding of the transcription factor, and epigenetic modifications. During carcinogenesis, certain tumor suppressor miRNAs targeting growth-promoting genes are silenced. Likewise, miR-15 and 16 targeting BCL2, an antiapoptotic gene are suppressed in chronic lymphocytic leukemia while let-7 targeting oncogene, RAS is decreased in lung cancer (Sharma et al. 2010). BCL6, an oncogene is a major target of miR127 which performs as a TSG, so that the intense epigenetic regulation of its expression is an essential mechanism for bladder cancer (Bandres et al. 2009). Repression of miR-29 family through various epigenetic regulations was found to be reported in several carcinogenesis processes which include B-cell lymphomas, rhabdomyosarcoma, acute myeloid leukemia, chronic lymphocytic leukemia. For instance, some other downregulated miRNAs include let-7a-3 in lung cancers, miR-31 in several cancer progression, miR-23a in human leukemic Jurkat cells, miR-200b in prostate and hepatocellular carcinoma (HCC). In contrast, certain upregulated miRNAs also play a vital role in carcinogenesis namely miR-615 in prostate cancer, miR-224 in HCC, and miR-155 in breast cancer (Liu et al. 2013; Moutinho and Esteller 2017). Thus several studies have indicated that epigenetic regulation is responsible for most of the miRNome changes found in human cancer, which were eventually involved both in carcinogenesis and the development of metastases. Hence, it significantly elucidates that cancer cells undergo systemic alterations in the structure of chromatin involving the entire epigenome and that a whole mechanism pertinent to cell renewal is epigenetically dysregulated.
4 Conclusion
The prevalence of cancer in animals and humans can be increased by several different forms of carcinogenic exposure, but a longer period of time period is typically needed. Observations can be explained by the conversion of a normal cell into neoplasm due to complicated mechanisms and heritable alterations in multiple or single gene products. For chemical carcinogenesis, the three-stage model of initiation, promotion, and progression has established a framework, which is not sufficient to explain the carcinogenic method. Accumulation of data shows that almost 10 genetic trials in humans are implicated in common adult malignancies. The relevance and specific functions of known cancer-causing factors in many biological processes, including differentiation, proliferation and apoptosis, and carcinogenesis, have now become evident. Two distinct groups of genes, namely oncogenes (which may be activated) and tumor suppressor genes (which may be inactivated) are implicated in the development of cancer. The discovery of genes reponsible in carcinogenesis and the understanding of pathways for their stimulation or inhibition makes it possible to understand how carcinogens affect the phases of neoplastic evolution. In the form of mutagenic processes, carcinogens can heritably change cells by epigenetic modification and enhance the clonal growth of altered cells. Most carcinogens work by a variety of mechanisms, and their primary mode of action can differ based on the targeted tissue. With the understanding of specific gene manipulation, cellular response, events of biological activities in the spread of cancer cells, there are now new insights on some of the discoveries in the detection, prognosis, and treatment of cancer. Nevertheless, it is satisfying to notice some of the significant developments in this crucial field of cancer science. While immense obstacles exist, it is expected that all these lines of research will continue to clinical research.
References
Abate-Shen C (2000) Molecular genetics of prostate cancer. Genes Dev 14:2410–2434. https://doi.org/10.1101/gad.819500
Abel EL, DiGiovanni J (2011) Multistage carcinogenesis. Curr Cancer Res 6:27–51. https://doi.org/10.1007/978-1-61737-995-6_2
Abel EL, Angel JM, Kiguchi K, DiGiovanni J (2009) Multi-stage chemical carcinogenesis in mouse skin: fundamentals and applications. Nat Protoc 4:1350–1362. https://doi.org/10.1038/nprot.2009.120
Ahmad J, Hasnain SE, Siddiqui MA et al (2013) MicroRNA in carcinogenesis & cancer diagnostics: a new paradigm. Indian J Med Res 37(4):680–694
Alnuaimi AD, Wiesenfeld D, O’Brien-Simpson NM et al (2015) Oral Candida colonization in oral cancer patients and its relationship with traditional risk factors of oral cancer: a matched case-control study. Oral Oncol 51(2):139–145. https://doi.org/10.1016/j.oraloncology.2014.11.008
Aykut B, Pushalkar S, Chen R et al (2019) The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nature 574:264–267. https://doi.org/10.1038/s41586-019-1608-2
Baca SC, Prandi D, Lawrence MS et al (2013) Punctuated evolution of prostate cancer genomes. Cell 153:666–677. https://doi.org/10.1016/j.cell.2013.03.021
Baldus SE, Schaefer K-L, Engers R et al (2010) Prevalence and heterogeneity of KRAS, BRAF, and PIK3CA mutations in primary colorectal adenocarcinomas and their corresponding metastases. Clin Cancer Res 16:790–799. https://doi.org/10.1158/1078-0432.CCR-09-2446
Bandres E, Agirre X, Bitarte N et al (2009) Epigenetic regulation of microRNA expression in colorectal cancer. Int J Cancer 125:2737–2743. https://doi.org/10.1002/ijc.24638
Banu A, Lax AJ, Grigoriadis AE (2020) In vivo targets of Pasteurella Multocida toxin. Int J Mol Sci 21:2739. https://doi.org/10.3390/ijms21082739
Barrett JC (1993) Mechanisms of multistep carcinogenesis and carcinogen risk assessment. Environ Health Perspect 100:9–20. https://doi.org/10.1289/ehp.931009
Belhassen H, Jiménez-Díaz I, Arrebola JP et al (2015) Zearalenone and its metabolites in urine and breast cancer risk: a case-control study in Tunisia. Chemosphere 128:1–6. https://doi.org/10.1016/j.chemosphere.2014.12.055
Berenblum I, Shubik P (1949) An experimental study of the initiating stage of carcinogenesis, and a re-examination of the somatic cell mutation theory of cancer. Br J Cancer 3:109–118. https://doi.org/10.1038/bjc.1949.13
Boquet P (1999) Bacterial toxins inhibiting or activating small GTP-binding proteins. Ann N Y Acad Sci 886:83–90. https://doi.org/10.1111/j.1749-6632.1999.tb09403.x
Botezatu A, Iancu IV, Popa O et al (2016) Mechanisms of oncogene activation. In: Bulgin D (ed) New aspects in molecular and cellular mechanisms of human carcinogenesis. IntechOpen, Croatia
Braoudaki M, Tzortzatou-Stathopoulou F (2011) Tumorigenesis related to retroviral infections. J Infect Dev Ctries 5:751–758. https://doi.org/10.3855/jidc.1773
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Brennan B (2006) Nasopharyngeal carcinoma. Orphanet J Rare Dis 1:23
Bushati N, Cohen SM (2007) microRNA functions. Annu Rev Cell Dev Biol 23:175–205. https://doi.org/10.1146/annurev.cellbio.23.090506.123406
Calin GA, Sevignani C, Dumitru CD et al (2004) Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc Natl Acad Sci U S A 101(9):2999–3004. https://doi.org/10.1073/pnas.0307323101
Caputo R, Tuccillo C, Manzo BA et al (2003) Helicobacter pylori VacA toxin up-regulates vascular endothelial growth factor expression in MKN 28 gastric cells through an epidermal growth factor receptor-, cyclooxygenase-2-dependent mechanism. Clin Cancer Res 9:2015–2021
Chang Y-T, Chang M-C, Huang K-W et al (2014) Clinicopathological and prognostic significances of EGFR, KRAS and BRAF mutations in biliary tract carcinomas in Taiwan. J Gastroenterol Hepatol 29:1119–1125. https://doi.org/10.1111/jgh.12505
Cicenas J, Tamosaitis L, Kvederaviciute K et al (2017) KRAS, NRAS and BRAF mutations in colorectal cancer and melanoma. Med Oncol 34:26. https://doi.org/10.1007/s12032-016-0879-9
Clevenger CV, Furth PA, Hankinson SE, Schuler LA (2003) The role of prolactin in mammary carcinoma. Endocr Rev 24:1–27. https://doi.org/10.1210/er.2001-0036
Cohen SM, Arnold LL (2011) Chemical carcinogenesis. Toxicol Sci 120:S76–S92. https://doi.org/10.1093/toxsci/kfq365
Conti CJ (2010) Mechanisms of tumor progression. In: Comprehensive toxicology. Elsevier, pp 335–347
Coyle YM, Xie XJ, Lewis CM et al (2007) Role of physical activity in modulating breast cancer risk as defined by APC and RASSF1A promoter hypermethylation in nonmalignant breast tissue. Cancer Epidemiol Biomark Prev 16(2):192
Croce CM (2008) Oncogenes and cancer. N Engl J Med 358(5):502–511
de Gerlache J, Taper HS, Lans M et al (1987) Dietary modulation of rat liver carcinogenesis. Carcinogenesis 8:337–340. https://doi.org/10.1093/carcin/8.2.337
Derelanko MJ (2001) Carcinogenesis. In: Handbook of toxicology, 2nd edn. CRC Press, Boca Raton
El Adlouni C, Tozlovanu M, Naman F et al (2006) Preliminary data on the presence of mycotoxins (ochratoxin A, citrinin and aflatoxin B1) in black table olives “Greek style” of Moroccan origin. Mol Nutr Food Res 50:507–512. https://doi.org/10.1002/mnfr.200600055
Elder DE (2016) Melanoma progression. Pathology 48:147–154. https://doi.org/10.1016/j.pathol.2015.12.002
El-Serag HB (2012) Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 142(6):1264–1273.e1. https://doi.org/10.1053/j.gastro.2011.12.061
Eser S, Schnieke A, Schneider G, Saur D (2014) Oncogenic KRAS signalling in pancreatic cancer. Br J Cancer 111:817–822. https://doi.org/10.1038/bjc.2014.215
Esquela-Kerscher A, Slack FJ (2006) Oncomirs — microRNAs with a role in cancer. Nat Rev Cancer 6:259–269. https://doi.org/10.1038/nrc1840
Faïs T, Delmas J, Serres A et al (2016) Impact of CDT toxin on human diseases. Toxins (Basel) 8(7):220
Fearon ER (2011) Molecular genetics of colorectal cancer. Annu Rev Pathol 6:479–507. https://doi.org/10.1146/annurev-pathol-011110-130235
Foss FM, Zinzani PL, Vose JM et al (2011) Peripheral T-cell lymphoma. Blood 117(25):6756–6767
Frenkel K, Wei H, Bhimani R et al (1993) Inhibition of tumor promoter-mediated processes in mouse skin and bovine lens by caffeic acid phenethyl ester. Cancer Res 53:1255–1261
Gariglio P (2012) Oncogenes and tumor suppressor genes. In: Gariglio P (ed) Molecular oncology: principles and recent advances. Bentham Science Publishers, pp 64–82
Gelderblom WCA, Abel S, Smuts CM et al (2001) Fumonisin-induced hepatocarcinogenesis: mechanisms related to cancer initiation and promotion. Environ Health Perspect 109:291–300. https://doi.org/10.1289/ehp.01109s2291
Gourama H, Bullerman LB (1995) Aspergillus flavus and aspergillus parasiticus: Aflatoxigenic fungi of concern in foods and feeds†: a review. J Food Prot 58(12):1395–1404
Grizzi F, Di Ieva A, Russo C et al (2006) Cancer initiation and progression: an unsimplifiable complexity. Theor Biol Med Model 3:37
Hacein-Bey-Abina S, Garrigue A, Wang GP et al (2008) Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J Clin Invest 118(9):3132–3142. https://doi.org/10.1172/JCI35700
Hanahan D, Robert AW (2017) Biological hallmarks of cancer. Holland-Frei Cancer Med 1–10. https://doi.org/10.1002/9781119000822.hfcm002
Harris CC (1991) Molecular basis of multistage carcinogenesis. Princess Takamatsu Symp 22:3–19
Harris H, Miller OJ, Klein G et al (1969) Suppression of malignancy by cell fusion. Nature 223:363–368. https://doi.org/10.1038/223363a0
Hart RW, Turturro A (1988) Current views of the biology of cancer. In: Carcinogen risk assessment. Springer US, Boston, MA, pp 19–33
Hartl M, Bister K (2013) Oncogenes. In: Brenner’s encyclopedia of genetics, 2nd edn. Academic Press, San Diego
Hecker E (1978) Co-carcinogens or modulators of carcinogenesis. New aspects of the etiology of human tumors and of the molecular mechanisms of carcinogenesis. Naturwissenschaften 65:640–648. https://doi.org/10.1007/BF00401906
Herrera LA, Benítez-Bribiesca L, Mohar A, Ostrosky-Wegman P (2005) Role of infectious diseases in human carcinogenesis. Environ Mol Mutagen 45:284–303
Hou W, Liu J, Chen P et al (2014) Mutation analysis of key genes in RAS/RAF and PI3K/PTEN pathways in Chinese patients with hepatocellular carcinoma. Oncol Lett 8:1249–1254. https://doi.org/10.3892/ol.2014.2253
Hristova M, Birse D, Hong Y, Ambros V (2005) The Caenorhabditis elegans Heterochronic regulator LIN-14 is a novel transcription factor that controls the developmental timing of transcription from the insulin/insulin-like growth factor gene ins-33 by direct DNA binding. Mol Cell Biol 25:11059–11072. https://doi.org/10.1128/mcb.25.24.11059-11072.2005
Ishii A, Matsuoka H, Aji T et al (1994) Parasite infection and cancer: with special emphasis on Schistosoma japonicum infections (Trematoda). A review. Mutat Res Mol Mech Mutagen 305:273–281. https://doi.org/10.1016/0027-5107(94)90247-X
Jančík S, Drábek J, Radzioch D, Hajdúch M (2010) Clinical relevance of KRAS in human cancers. J Biomed Biotechnol 2010:1–13. https://doi.org/10.1155/2010/150960
Janku F, Lee JJ, Tsimberidou AM et al (2011) PIK3CA mutations frequently coexist with ras and braf mutations in patients with advanced cancers. PLoS One 6(7):e22769. https://doi.org/10.1371/journal.pone.0022769
Jones PA (2003) Epigenetics in carcinogenesis and cancer prevention. Ann N Y Acad Sci 983:213–219
Jones PA, Baylin SB (2007) The epigenomics of cancer. Cell 128(4):683–692
Jones PA, Takai D (2001) The role of DNA methylation in mammalian epigenetics. Science 293:1068–1070
Kamisawa T, Wood LD, Itoi T, Takaori K (2016) Pancreatic cancer. Lancet 388:73–85. https://doi.org/10.1016/S0140-6736(16)00141-0
Kanwal R, Gupta S (2012) Epigenetic modifications in cancer. Clin Genet 81(4):303–311
Karachaliou N, Mayo C, Costa C et al (2013) KRAS mutations in lung cancer. Clin Lung Cancer 14:205–214. https://doi.org/10.1016/j.cllc.2012.09.007
Karin M, Greten FR (2005) NF-κB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol 5:749–759. https://doi.org/10.1038/nri1703
Kempf VAJ, Volkmann B, Schaller M et al (2001) Evidence of a leading role for VEGF in Bartonella henselae -induced endothelial cell proliferations. Cell Microbiol 3:623–632. https://doi.org/10.1046/j.1462-5822.2001.00144.x
Kew MC (2013) Aflatoxins as a cause of hepatocellular carcinoma. J Gastrointest Liver Dis 22:305–310
Kim YI, Yu ES, Kim ST (1989) Intraductal variant of peripheral cholangiocarcinoma of the liver with Clonorchis sinensis infection. Cancer 63:1562–1566. https://doi.org/10.1002/1097-0142(19890415)63:8<1562::aid-cncr2820630819>3.0.co;2-8
Klose RJ, Bird AP (2006) Genomic DNA methylation: the mark and its mediators. Trends Biochem Sci 31:89–97. https://doi.org/10.1016/j.tibs.2005.12.008
Knasmüller S, Cavin C, Chakraborty A et al (2004) Structurally related mycotoxins ochratoxin a, ochratoxin B, and citrinin differ in their genotoxic activities and in their mode of action in human-derived liver (HepG2) cells: implications for risk assessment. Nutr Cancer 50(2):190–197. https://doi.org/10.1207/s15327914nc5002_9
Kwon O, Soung NK, Thimmegowda NR et al (2012) Patulin induces colorectal cancer cells apoptosis through EGR-1 dependent ATF3 up-regulation. Cell Signal 24:943–950. https://doi.org/10.1016/j.cellsig.2011.12.017
Lax AJ, Thomas W (2002) How bacteria could cause cancer: one step at a time. Trends Microbiol 10:293–299. https://doi.org/10.1016/S0966-842X(02)02360-0
Lee YS, Kim HK, Chung S et al (2005) Depletion of human micro-RNA miR-125b reveals that it is critical for the proliferation of differentiated cells but not for the down-regulation of putative targets during differentiation. J Biol Chem 280(17):16635–16641. https://doi.org/10.1074/jbc.M412247200
Leiderman YI, Kiss S, Mukai S (2007) Molecular genetics of RB1—the retinoblastoma gene. Semin Ophthalmol 22:247–254. https://doi.org/10.1080/08820530701745165
Lewis JG, Adams DO (1987) Inflammation, oxidative DNA damage, and carcinogenesis. Environ Health Perspect 76:19–27. https://doi.org/10.1289/ehp.877619
Lim JH (2011) Liver flukes: the malady neglected. Korean J Radiol 12:269. https://doi.org/10.3348/kjr.2011.12.3.269
Liu X, Chen X, Yu X et al (2013) Regulation of microRNAs by epigenetics and their interplay involved in cancer. J Exp Clin Cancer Res 32:96. https://doi.org/10.1186/1756-9966-32-96
Loeb LA, Harris CC (2008) Advances in chemical carcinogenesis: a historical review and prospective. Cancer Res 68(17):6863–6872
Ma Y-Y, Wei S-J, Lin Y-C et al (2000) PIK3CA as an oncogene in cervical cancer. Oncogene 19:2739–2744. https://doi.org/10.1038/sj.onc.1203597
Ma C, Wickham ME, Guttman JA et al (2006) Citrobacter rodentium infection causes both mitochondrial dysfunction and intestinal epithelial barrier disruption in vivo: role of mitochondrial associated protein (Map). Cell Microbiol 8:1669–1686. https://doi.org/10.1111/j.1462-5822.2006.00741.x
Martin OCB, Frisan T (2020) Bacterial genotoxin-induced DNA damage and modulation of the host immune microenvironment. Toxins (Basel) 12:63. https://doi.org/10.3390/toxins12020063
Martin JL, Maldonado JO, Mueller JD et al (2016) Molecular studies of HTLV-1 replication: an update. Viruses 8(2):1–22
Matsuda NM, Miller SM, Evora PRB (2009) The chronic gastrointestinal manifestations of Chagas disease. Clinics (Sao Paulo) 64:1219–1224. https://doi.org/10.1590/S1807-59322009001200013
Mendelsohn J, Howley PM, Israel MA et al (2008) The molecular basis of cancer. Elsevier, Philadelphia, PA
Mitreva M (2012) The genome of a blood fluke associated with human cancer. Nat Genet 44:116–118. https://doi.org/10.1038/ng.1082
Moutinho C, Esteller M (2017) MicroRNAs and epigenetics. Adv Cancer Res 135:189–220
Murphy AE, Charnay-Sonnek F (2019) Basis of carcinogenesis. Springer, Dordrecht, pp 1–17
Nath G, Gulati AK, Shukla VK (2010) Role of bacteria in carcinogenesis, with special reference to carcinoma of the gallbladder. World J Gastroenterol 16(43):5395–5404. https://doi.org/10.3748/wjg.v16.i43.5395
Oliveira PA, Colaço A, Chaves R et al (2007) Chemical carcinogenesis. An Acad Bras Cienc 79:593–616. https://doi.org/10.1590/S0001-37652007000400004
Olson RE (1992) Vitamins and carcinogenesis: an overview. J Nutr Sci Vitaminol (Tokyo) Spec No:313–316. https://doi.org/10.3177/jnsv.38.special_313
Orem J, Mbidde EK, Lambert B et al (2007) Burkitt’s lymphoma in Africa, a review of the epidemiology and etiology. Afr Health Sci 7:166–175. https://doi.org/10.5555/afhs.2007.7.3.166
Ostry V, Malir F, Toman J, Grosse Y (2017) Mycotoxins as human carcinogens—the IARC monographs classification. Mycotoxin Res 33:65–73. https://doi.org/10.1007/s12550-016-0265-7
Paik PK, Arcila ME, Fara M et al (2011) Clinical characteristics of patients with lung adenocarcinomas harboring BRAF mutations. J Clin Oncol 29(15):2046–2051. https://doi.org/10.1200/JCO.2010.33.1280
Palumbo E (2007) Association between schistosomiasis and Cancer. Infect Dis Clin Pract 15:145–148. https://doi.org/10.1097/01.idc.0000269904.90155.ce
Pane F, Intrieri M, Quintarelli C et al (2002) BCR/ABL genes and leukemic phenotype: from molecular mechanisms to clinical correlations. Oncogene 21:8652–8667. https://doi.org/10.1038/sj.onc.1206094
Pasqualucci L, Dominguez-Sola D, Chiarenza A et al (2011) Inactivating mutations of acetyltransferase genes in B-cell lymphoma. Nature 471:189–195. https://doi.org/10.1038/nature09730
Peng Y, Croce CM (2016) The role of microRNAs in human cancer. Signal Transduct Target Ther 1:15004
Pitt JI (2000) Toxigenic fungi and mycotoxins. Br Med Bull 56(1):184–192
Polonara G, Alvaro L, Regnicolo L (2012) Tumor progression. In: Imaging gliomas after treatment. Springer Milan, Milano, pp 151–156
Quiros RM, Ding HG, Gattuso P et al (2005) Evidence that one subset of anaplastic thyroid carcinomas are derived from papillary carcinomas due toBRAF andp53 mutations. Cancer 103:2261–2268. https://doi.org/10.1002/cncr.21073
Raab-Traub N (2002) Epstein–Barr virus in the pathogenesis of NPC. Semin Cancer Biol 12:431–441. https://doi.org/10.1016/S1044579X0200086X
Rahman N, Scott RH (2007) Cancer genes associated with phenotypes in monoallelic and biallelic mutation carriers: new lessons from old players. Hum Mol Genet 16:R60–R66. https://doi.org/10.1093/hmg/ddm026
Rubin H (1994) Experimental control of neoplastic progression in cell populations: Foulds’ rules revisited. Proc Natl Acad Sci U S A 91:6619–6623. https://doi.org/10.1073/pnas.91.14.6619
Ruddon RW (2010) Introduction to the molecular biology of cancer. Prog Mol Biol Transl Sci 95:1–8
Samba-Louaka A, Nougayrède J-P, Watrin C et al (2009) The Enteropathogenic Escherichia coli effector Cif induces delayed apoptosis in epithelial cells. Infect Immun 77:5471–5477. https://doi.org/10.1128/IAI.00860-09
Sanchis-Gomar F, Garcia-Gimenez JL, Perez-Quilis C et al (2012) Physical exercise as an epigenetic modulator: eustress, the “positive stress” as an effector of gene expression. J Strength Cond Res 26(12):3469–3472
Savage KI, Harkin DP (2015) BRCA1, a ‘complex’ protein involved in the maintenance of genomic stability. FEBS J 282:630–646. https://doi.org/10.1111/febs.13150
Sawan C, Herceg Z (2010) Histone modifications and cancer. Adv Genet 70:57–85
Saxonov S, Berg P, Brutlag DL (2006) A genome-wide analysis of CpG dinucleotides in the human genome distinguishes two distinct classes of promoters. Proc Natl Acad Sci U S A 103:1412–1417. https://doi.org/10.1073/pnas.0510310103
Schlenk RF, Döhner K, Krauter J et al (2008) Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med 358(18):1909–1918. https://doi.org/10.1056/NEJMoa074306
Scholte LLS, Pascoal-Xavier MA, Nahum LA (2018) Helminths and cancers from the evolutionary perspective. Front Med 5:90. https://doi.org/10.3389/fmed.2018.00090
Schwartz GG (2002) Hypothesis: does ochratoxin A cause testicular cancer? Cancer Causes Control 13:91–100. https://doi.org/10.1023/a:1013973715289
Seo JS, Ju YS, Lee WC et al (2012) The transcriptional landscape and mutational profile of lung adenocarcinoma. Genome Res 22:2109–2119. https://doi.org/10.1101/gr.145144.112
Shanmugam MK, Arfuso F, Arumugam S et al (2018) Role of novel histone modifications in cancer. Oncotarget 9:11414–11426. https://doi.org/10.18632/oncotarget.23356
Sharma S, Kelly TK, Jones PA (2010) Epigenetics in cancer. Carcinogenesis 31:27–36. https://doi.org/10.1093/carcin/bgp220
Shuh M, Beilke M (2005) The human T-cell leukemia virus type 1 (HTLV-1): new insights into the clinical aspects and molecular pathogenesis of adult t-cell leukemia/lymphoma (ATLL) and tropical spastic paraparesis/HTLV-associated myelopathy (TSP/HAM). Microsc Res Tech 68:176–196. https://doi.org/10.1002/jemt.20231
Smith AL, Robin TP, Ford HL (2012) Molecular pathways: targeting the TGF-β pathway for cancer therapy. Clin Cancer Res 18:4514–4521. https://doi.org/10.1158/1078-0432.CCR-11-3224
Sripa B, Bethony JM, Sithithaworn P et al (2011) Opisthorchiasis and Opisthorchis-associated cholangiocarcinoma in Thailand and Laos. Acta Trop 120(Suppl):S158–S168. https://doi.org/10.1016/j.actatropica.2010.07.006
Stratton MR, Campbell PJ, Futreal PA (2009) The cancer genome. Nature 458(7239):719–724
Therkildsen C, Bergmann TK, Henrichsen-Schnack T et al (2014) The predictive value of KRAS, NRAS, BRAF, PIK3CA and PTEN for anti-EGFR treatment in metastatic colorectal cancer: a systematic review and meta-analysis. Acta Oncol (Madr) 53(7):852–864
Tomizawa D, Kiyokawa N (2017) Acute lymphoblastic leukemia. In: Hematological disorders in children. Springer Singapore, Singapore, pp 33–60
Tomlinson IPM, Lambros MBK, Roylance RR, Cleton-Jansen AM (2002) Loss of heterozygosity analysis: practically and conceptually flawed? Genes Chromosomes Cancer 34(4):349–353
Travaglione S, Fabbri A, Fiorentini C (2008) The rho-activating CNF1 toxin from pathogenic E. coli: a risk factor for human cancer development? Infect Agent Cancer 3:4
Van Antwerp DJ, Martin SJ, Kafri T et al (1996) Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science 274(5288):787–789
van Tong H, Brindley PJ, Meyer CG, Velavan TP (2017) Parasite infection, carcinogenesis and human malignancy. EBioMedicine 15:12–23
Vancheri C (2016) Cancer. In: Idiopathic pulmonary fibrosis. European Respiratory Society, pp 151–159
Vennervald BJ, Polman K (2009) Helminths and malignancy. Parasite Immunol 31:686–696. https://doi.org/10.1111/j.1365-3024.2009.01163.x
Vincent TL, Gatenby RA (2008) An evolutionary model for initiation, promotion and progression in carcinogenesis. Int J Oncol 32(4):729–737
Vogelmann R, Amieva MR (2007) The role of bacterial pathogens in cancer. Curr Opin Microbiol 10:76–81. https://doi.org/10.1016/j.mib.2006.12.004
Vogelstein B, Papadopoulos N, Velculescu VE et al (2013) Cancer genome landscapes. Science 339:1546–1558. https://doi.org/10.1126/science.1235122
Wang L-H, Wu C-F, Rajasekaran N, Shin YK (2018) Loss of tumor suppressor gene function in human cancer: an overview. Cell Physiol Biochem 51:2647–2693. https://doi.org/10.1159/000495956
Weiss RA (2004) Multistage carcinogenesis. Br J Cancer 91:1981–1982. https://doi.org/10.1038/sj.bjc.6602318
Wu S, Lim K-C, Huang J et al (1998) Bacteroides fragilis enterotoxin cleaves the zonula adherens protein, E-cadherin. Proc Natl Acad Sci U S A 95:14979–14984. https://doi.org/10.1073/pnas.95.25.14979
Yanaihara N, Caplen N, Bowman E et al (2006) Unique microRNA molecular profiles in lung cancer diagnosis and prognosis. Cancer Cell 9(3):189–198. https://doi.org/10.1016/j.ccr.2006.01.025
Yokota J (2000) Tumor progression and metastasis. Carcinogenesis 21:497–503. https://doi.org/10.1093/carcin/21.3.497
Zanger P, Habscheid W, Kremsner PG, Dahm HH (2010) Schistosoma japonicum infection and rectal carcinoid tumour: underreported coincidence or neglected association? Epidemiol Infect 138:1289–1291. https://doi.org/10.1017/S095026880999152X
Zarbl H, Sukumar S, Arthur AV et al (1985) Direct mutagenesis of Ha-ras-1 oncogenes by N-nitroso-N-methylurea during initiation of mammary carcinogenesis in rats. Nature 315:382–385. https://doi.org/10.1038/315382a0
Zheng Z-M (2010) Viral oncogenes, noncoding RNAs, and RNA splicing in human tumor viruses. Int J Biol Sci 6(7):730–755. https://doi.org/10.7150/ijbs.6.730
Acknowledgements
The authors wish to acknowledge(i) DST-FIST (Grant No. SR/FST/LSI-639/2015(C)), (ii) UGC-SAP (Grant No. F.5-1/2018/DRS-II (SAP-II)), (iii) DST-PURSE (Grant No. SR/PURSE Phase 2/38 (G)),Rc S.O. (P)/DST-PURSE Phase II/P1464/2019, (iv) RUSA 2.0 [F. 24-51/2014-U, Policy (TN Multi-Gen), and (v) Department of Education, Govt. of India] and the University Science Instrumentation Centre (USIC), Alagappa University.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kiruthiga, C., Devi, K.P. (2021). Mechanisms Involved in Carcinogenesis. In: Jafari, S.M., Nabavi, S.M., Silva, A.S. (eds) Nutraceuticals and Cancer Signaling. Food Bioactive Ingredients. Springer, Cham. https://doi.org/10.1007/978-3-030-74035-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-74035-1_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-74034-4
Online ISBN: 978-3-030-74035-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)