Abstract
From 1997 through today, more than 400 magnetic compression anastomoses have been performed in Japan. In this chapter, we describe how it was put to practical use through the process of developing this technique including the animal experiments. We also describe which magnets are desirable and which transport methods are most suitable. Although this procedure and stenosis are inseparably related, the best way to prevent the stenosis is also described. Explanations and discussions are focused on various findings and interesting cases obtained from the accumulation of over 400 cases.
Magnet compression anastomosis is an excellent anastomosis method that does not require general anesthesia or open surgery, has no leaks, and is expected to be further developed in the future.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Magnetic compression anastomosis
- Magnetic compression revision for stenosis
- Samarium-cobalt magnet
- Frequent balloon dilatation
- Extracorporeal magnetic guidance
- Sideways transport method
- Pulling up method
Introduction
In 1989, we hit on this idea of magnetic compression anastomosis (MCA) from an accidental case of a 2-year-old girl who had swallowed small magnets that are sold and generally used to relieve shoulder stiffness in Japan. She was brought to the emergency room at our university hospital complaining of abdominal pain. It was revealed that she had swallowed 13 small magnets because “she was hungry” (Fig. 16.1). An abdominal computed tomography (CT) study showed complete obstruction of the bowel loops. A barium enema study showed that 3 magnets were in the cecum and the remaining 10 were outside of the colon, probably in the ileum (Fig. 16.2). The decision was made to perform open abdominal surgery to relieve the obstruction. During surgery, it was found that the terminal ileum was adhered to the cecum and the magnets had created an anastomosis between these two anatomical structures. The remanence of each small magnet was only 1200 gauss (Fig. 16.3). It was then that we realized that we could create such an anastomosis between organs if we could keep each organ in contact for a sufficient period of time using strong magnets (Fig. 16.4).
The concept of mechanical anastomosis was first proposed by Denan in 1821 and refined by Murphy in 1892 [1] at a time when lengthy abdominal surgery was still considered dangerous. Later, their mechanical anastomosis method was superseded by suturing devices because abdominal surgery became safer. Magnetic compression anastomosis (MCA) was also proposed, but was not used clinically due to many difficulties such as the lack of confirmation of magnet safety, no convenient method for delivery of the magnet to the stenosis site, and a high rate of acute restenosis [2,3,4]. In fact, clinical use did not occur until we applied this method without surgery and general anesthesia in 1997 and presented the results in 1998 [5, 6]. Since then, more than 400 MCA procedures have been performed in Japan. Yamanouchi have been involved in almost all cases [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24].
In this chapter, we describe the results of basic experiments, the materials and methods used, results, typical clinical cases, and problems encountered during the many MCA procedures that have been performed since the report in 1998.
Magnetic Compression Anastomosis
Basic Experimental Results
Multiple experiments were performed in rat and mongrel canine models to confirm the feasibility of MCA. In order to create an anastomosis, two rare-earth magnets (samarium-cobalt compound, 4 mm in diameter and 1.8 mm in thickness, with a remanence of 2300 gauss) were placed in each rat, one in the cecum and the other in the transverse colon (Fig. 16.5). The magnets in the cecum and transverse colon mated and subsequently created a fistulous anastomosis. The anastomosis was confirmed radiologically by a barium enema study (Fig. 16.6). Our experimental studies in rats confirmed that this method was safe and economical. Unlike with anastomoses created surgically, no white linear ischemic scar or inflammatory change was found at the site of the anastomosis after sacrifice (Fig. 16.7). Hematoxylin-eosin-stained pathological specimens obtained from the anastomotic site postmortem were checked for infiltration of inflammatory cells. The specimens were also stained with Masson’s trichrome dye to check the state of the anastomosis layer by layer. Hardly any inflammatory change was found at the anastomotic site. Some multinucleated giant cells were found but without infiltration of inflammatory cells, suggesting that apoptosis may be involved in the process of forming an MCA. Furthermore, the site of the anastomosis was found to have an intact layer-by-layer structure, which cannot be obtained by surgical suturing (Fig. 16.8). Thus, we were finally able to create an MCA successfully. We determined that the optimal magnet strength was between 2000 and 4500 gauss. Magnets weaker than 2000 gauss failed to create an anastomosis and there was a risk of anastomotic leak with magnets stronger than 4500 gauss.
Infiltration of inflammatory cells , which is usually seen in surgical specimens, is not noted at the anastomotic site on hematoxylin-eosin staining. Some multinucleated giant cells were found not to show infiltration of inflammatory cells. This finding suggests that apoptosis may participate in magnetic compression anastomosis (left). The anastomotic site shows wonderful layer-to-layer structure on Masson’s trichrome staining (right)
We conducted further experiments to identify the key to maintaining the anastomosis. Studies in rat models confirmed that the main difference between the MCA and Gambee methods is that a fibrin net appears around an MCA within a few days but not around a Gambee anastomosis until 1–3 weeks (Figs. 16.9 and 16.10). Next, we investigated how the layer-by-layer structure was formed. TUNEL staining of specimens showed that many cells were in an apoptotic state, suggesting that apoptosis has an important role in structural remodeling at the site of the anastomosis (Fig. 16.11). Our experiments in rats also suggested that the MCA method could be used in humans if the magnets used were strong enough (see Fig. 16.4).
The time course (24 hours to 1 week) of magnetic compression anastomosis and Gambee anastomosis. The main difference between the two methods is that a fibrin net appears around the site of the magnetic compression anastomosis within a few days but not around the site of the Gambee anastomosis until 1–3 weeks later
Diagram showing magnetic compression anastomosis and Gambee anastomosis . The major difference between the two anastomosis methods is that fibrin net appears around the magnetic compression anastomosis site in a few days, but it does not appear around the Gambee anastomosis site until 1–3 weeks later
Materials and Methods
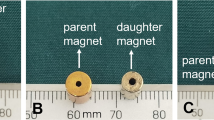
Types of Magnets
Rare-earth magnets were already known to be strong magnets at the time we first started performing these procedures. There are two main types of rare-earth magnets, namely, samarium-cobalt magnet and neodymium-iron-boron magnet. Samarium-cobalt magnets (Magna Co., Ltd. Tokyo, Japan) were used for enteroenteric, bilioenteric, and biliobiliary anastomoses because neodymium magnets are usually nickel plated to prevent oxidation and thus are corrosive and biologically toxic. The two disk magnets were placed separately in the organs to be anastomosed and the joined magnets were excreted mainly in the feces after mating, usually within 1–2 weeks after an enteroenteric anastomosis. We designated the magnet placed at the distal site as the parent magnet and that placed at the proximal site as the daughter magnet (Fig. 16.12). However, two cylindrical magnets are usually used for a bilioenteric or biliobiliary MCA. The parent magnet is placed in the ascending jejunal limb, duodenum, or common bile duct (CBD) and the daughter magnet is placed in an intrahepatic bile duct (Fig. 16.13).
Diagram showing the process of enteroenteric magnetic compression anastomosis . First, the parent magnet in most cases is transported across the stenosis, which is temporarily dilated by a balloon catheter. In other cases, the parent magnet is transported from the anal side. The daughter magnet is then positioned, and the magnets are mated. The soft tissue compressed by the magnets is finally removed from the anastomotic site and the new lumen provides an adequate tract
Diagrams showing the process of bilioenteric and biliobiliary magnetic compression anastomosis . The figure on the left shows an anastomosis between the intrahepatic bile duct and the ascending jejunal limb or duodenum. The figure on the right shows an anastomosis between the intrahepatic bile duct and common bile duct. In some cases, the intrahepatic bile ducts may include the common bile duct
The safety of the magnetic force and of a magnet itself when placed in the digestive tract is thought to be confirmed by the following observation. Cattle are known to like the taste of iron and often accidentally swallow iron nails that can puncture the wall of the stomach. To combat this problem, cattle are often fed magnets that enter the fourth stomach where they can attract an ingested iron nail and prevent its tip from piercing the stomach wall (Fig. 16.14). There are no problems with the milk and meat produced by cattle, which have these magnets in place lifelong.
Cows are known to accidentally swallow iron nails that can puncture the stomach. Farmers in Japan and the United States insert a cow magnet into the fourth stomach to prevent injury by iron nails. The magnets are left in the stomach for the cow’s entire lifetime. The upper magnet is a new model to prevent iron nails from flaring. The lower magnet is an older model
Samarium-cobalt magnets were used to create enteroenteric and bilioenteric or biliobiliary MCA. Two disk magnets are used in enteroenteric MCA. The size of each magnet depends on the intended site of the anastomosis. For example, in the case of a gastroduodenal or gastrojejunal anastomosis, two disk magnets of the same size are used because when mated they can be removed from the stomach easily via an endoscope or are excreted uneventfully. However, in the case of ileus it is recommended that the parent magnet should not enter the dead-end loop, so the parent magnetic has a diameter that is 5 mm larger than that of the daughter magnet. If the mated magnet was to enter the dead-end bowel loop, it would be almost impossible to remove nonsurgically. Four types of disk magnets are commonly used in enteroenteric MCA (Fig. 16.15). These magnets are 15–22.5 mm in diameter, 5 mm in thickness, and have total remanence (magnetic strength) values in the range of 3200–2000 gauss. A small disk magnet is stronger than a large magnet if the thickness is the same. In children with esophageal atresia, smaller magnets with a diameter of 10–12.5 mm and a thickness of 5 mm are used. There are two holes in each disk magnet. The hole on the side of the magnet is called the side hole for the guidewire to transport. The hole on the top is called the top hole for lifting with a thread to perform magnetic compression revision of stenosis.
Four types of disk magnets commonly used in enteroenteric magnetic compression anastomosis . They range in diameter from 15 mm to 22.5 mm and have a thickness of 5 mm. The remanence is shown beside the photograph of each magnet. Each disk magnet has two holes, namely a “side hole” for the guidewire and a “top hole” for lifting with a thread to perform the magnetic compression revision for stenosis procedure
Two types of cylindrical magnet are used in bilioenteric or biliobiliary MCA. The parent magnet is 5 mm in diameter and 5 or 6 mm in length with a nylon snare for the forceps of the endoscope. The daughter magnet is 4 mm in diameter and 9 mm in length with a guidewire for manipulation (Fig. 16.16).
How to Transport and Remove the Magnet
We initially considered that an endoscope could be used to transport the magnet, but found that pushing the magnet over the guidewire was more effective than using the endoscope in enteroenteric MCA procedures. However, the endoscope is useful as a base when pushing the magnet over the guidewire. The guidewire is also useful for holding the magnet temporarily when bent to 30 degrees at 5 cm from the tip (Fig. 16.17). In some cases, extracorporeal magnetic guidance is very effective when holding and moving the magnet (Fig. 16.18). Extracorporeal magnetic guidance is also necessary when placing the magnet deeper within the bowel loops; an endoscope cannot reach deep within the jejunum or ileum and there was no endoscope that could enter the small intestine when we initially started performing MCA procedures. Insertion of an ileus tube made guidance easier than expected (see Fig. 16.20, left). However, this method cannot be used in obese patients because the extracorporeal magnetic force cannot reach the target depth in the body. The mated magnets are usually excreted via the bowel loop in which the parent magnet was placed. The mated magnets are heavier, and thus sometimes taking more time than expected to pass through the bowel loops.
Radiographic image of magnetic compression anastomosis performed to create a ρ-anastomosis between the jejunum and the blind end of the jejunum. The parent magnet, which was transported over the guidewire and bent 30 degrees at 5 cm from the tip (black arrow), is placed in the jejunal. The thick line over the guidewire is the pusher (white arrow), which is used to push and release the magnet
In bilioenteric or biliobiliary MCA , an endoscope is required to transport the parent magnet into the ascending jejunal limb, duodenum, or CBD through the ampulla of Vater. The daughter magnet is attached to the guidewire, which is placed with deflection to create a pushing force. Using this pushing force, the mated magnets are moved into the ascending jejunal limb or CBD. The mated magnets are endoscopically removed in bilioenteric or biliobiliary cases. In some cases, the mated magnets can be released from the guidewire attached to the daughter magnet by pushing hard over the guidewire because the portion to which the guidewire is attached is designed to be released by strong external force. The mated magnets are excreted via the fecal route.
A Clinical Study
We performed a study involving 422 patients who had a stenosis in the intestine or CBD with a gap between the organs to be anastomosed of <3 cm on fluoroscopy using Gastrografin or abdominal CT. The patients (266 males, 156 females) had a mean age of 65.5 (range, aged 1–91) years. Four patients who underwent enteroenteric anastomosis required two procedures because of acute stenosis and one patient required bilioenteric anastomosis twice because of restenosis after 6 months. Therefore, a total of 427 procedures (206 enteroenteric anastomoses, 189 bilioenteric or biliobiliary anastomoses, and 32 magnetic compression revision for stenosis [MCRS] ; described later) were performed. The most common cause of stenosis was postoperative complications in the enteroenteric, bilioenteric, or biliobiliary MCA cases. Informed consent was obtained from all patients or their guardians after they had received a detailed explanation of the procedure. Various representative clinical cases are described in the next section.
Representative Clinical Cases
A Case of Ileocolostomy
The patient was a woman in her 80s with chronic postoperative adhesive ileus. Surgery was contraindicated because of severe cardiac dysfunction, so an ileus tube had been placed percutaneously after gastrostomy a number of years earlier. Follow-through and barium enema studies were performed simultaneously to assess the possibility of MCA. The ileum and descending colon were next to one another (Fig. 16.19) with no other bowel loop in between, suggesting that the patient was a suitable candidate for MCA. The swallowed daughter magnet was moved along the ileus tube under extracorporeal magnetic guidance. The parent magnet was placed endoscopically, after which the two magnets were mated (Fig. 16.20). Endoscopic observation 10 days later showed passage of feces through the anastomosis. The endoscopic view showed a better anastomosis than we had ever seen with surgery. It would be impossible to create such a smooth anastomosis surgically. No inflammatory changes were noted around the anastomotic site (Fig. 16.21). A pathological specimen obtained from the area between the magnets showed each layer of the two bowel loops to be well preserved (Fig. 16.22). This was the first case of enteroenteric MCA performed in humans.
Radiographic images showing an ileus tube that was placed percutaneously after gastrostomy many years earlier. Follow-through and barium enema studies were performed simultaneously. Microcolon due to no passage of fecal material can be identified. The ileum and descending colon are next to each other (arrow), and there is no other bowel loop between the two structures
After 10 days, endoscopic observation showed feces passing through the anastomosis. This endoscopic view showed a much better anastomosis than we had ever seen with surgery. It is impossible to create such a smooth anastomosis surgically. No inflammatory changes were noted around the anastomosis site
A pathological specimen between the magnets showed each layer of the two bowel loops were well preserved without deterioration (Masson’s trichrome staining). The lower thick zone is the muscular layer of the small intestine, and the upper thin zone is that of the large intestine. Note that the basic structure of the two intestinal walls is well preserved, although cells have disappeared, probably due to ischemic necrosis
A Case of Gastroduodenal Anastomosis
The patient was a man in his 40s. Intake of solids was difficult because of scarring from a duodenal ulcer, and he had been on a liquid diet for approximately 6 months. He did not want to undergo distal gastrectomy because both his parents had died during surgery, so he chose MCA for gastroduodenal anastomosis. It was hard to transport the parent magnet across the pyloric stenosis, which was temporarily dilated by a balloon catheter. Disk magnets measuring 17.5 mm are often used in this type of anastomosis, but 15-mm disk magnets were the limit in this case because of the severe stenosis. Transport of the daughter magnet was easier, and the two magnets mated immediately (Fig. 16.23). Two weeks later, the mated magnets had been released and were excreted. Acute stenosis is often noted after gastroduodenal MCA, but is easily controlled by frequent balloon dilatation (FBD) , which is necessary once or twice weekly for several weeks (Fig. 16.24). At the 3-year follow-up, the anastomotic site showed good patency with smooth mucosal union. Now that he could have enough food, the patient was fat enough to misunderstand (Fig. 16.25).
The parent magnet (15 mm in diameter, 5 mm in thickness) placed in the fourth part of the duodenum after difficult passage across a pyloric stenosis, which was temporarily dilated by a balloon catheter. The 15-mm parent magnet was at the limit of the size able to enter through a pyloric stenosis. The daughter magnet (15 mm in diameter, 5 mm in thickness) was endoscopically placed in the body of the stomach. The magnets were finally mated and excreted after 14 days
A Case of Postoperative Occlusion After Low Anterior Resection
The patient was a man in his 70s who had undergone a low anterior resection 5 years earlier with stoma closure 3 years earlier and suddenly developed ileus because of complete obstruction of the anastomotic site (Fig. 16.26). Reoperation was predicted to be difficult because the site of the obstruction was located deep within the small pelvic cavity. Therefore, MCA was planned by swallowing the daughter magnet. The daughter magnet reached the blind end of the descending colon within a few days. The parent magnet was placed in the rectum by digital manipulation. The two magnets were mated in position uneventfully (Fig. 16.27) and excreted 10 days later. The created fistulous tract was not fully covered by normal mucosa, so balloon dilatation was applied several times to prevent stenosis. Fecal passage was also thought to work as good dilatation force in this case (Fig. 16.28). Good patency of the tract was observed at discharge, and the patient has had no problems since (Fig. 16.29).
The daughter magnet (17.5 mm in diameter, 5 mm in thickness) was swallowed and reached the blind end of the descending colon within a few days. The parent magnet (the same size as the daughter magnet) was carried into the rectum by digital manipulation. The two magnets were mated in position uneventfully
A Case of Postoperative Occlusion After Low Anterior Resection
The patient was a man in his 60s who had developed a leak-related anastomotic occlusion after a low anterior resection, which was treated by creating a colostomy in the transverse colon. The surgeons were reluctant to perform repeat surgery because the site of obstruction was deep within the small pelvic cavity and there was concern about possible ineffective suturing and recurrence of leak as a result of multiple diverticula in the descending colon (Fig. 16.30). Therefore, the plan was to perform an MCA via the transverse colostomy; however, surgical staples created by automatic suture apparatus were identified in the stricture (Fig. 16.31). At that time, it was unknown if surgical staples would be severed by MCA. Nevertheless, MCA was performed, and the mated magnets were excreted 2 weeks later without any problems related to the surgical staples (Fig. 16.32). Radiographs revealed numerous surgical staples within the specimen (Fig. 16.33). Therefore, MCA is possible even if there are surgical staples between the magnets (Fig. 16.34). Balloon dilatation was applied on several occasions to prevent stenosis. Fecal passage was also thought to work as good dilatation force in this case. The patient returned to normal life after 3 weeks.
Staples left by automatic suture apparatus can be seen at the obstruction site (arrow). The daughter magnet (20 mm in diameter, 5 mm in thickness) was transported over the guidewire through a transverse colostomy. The parent magnet (the same size as the daughter magnet) was carried into the rectum by digital manipulation. Finally, the two magnets were placed in position with no problems
A Case of ρ-Anastomosis Between the Jejunum and Blind End of the Jejunum After Total Gastrectomy
The patient was a man in his 50s who had been experiencing difficulties with oral intake and developed aspiration pneumonia. He had undergone total gastrectomy with Roux-en-Y reconstruction for gastric cancer 10 years earlier. Postoperatively, a stricture gradually developed in the jejunum, causing elongation and formation of multiple diverticula in the blind end of the jejunum. The stricture also caused reflux of food materials and digestive juices, which led to the aspiration pneumonia (Fig. 16.35). We planned to create a ρ-anastomosis by MCA between the jejunum and blind end of the jejunum after total gastrectomy (Fig. 16.36). After successful creation of the ρ-anastomosis between the blind end of the jejunum and the main route of the jejunum, a gastrointestinal study confirmed that the dilation of the blind portion had resolved, with flow of contrast medium into the main route of the jejunum via the ρ-anastomosis. The patient was able to resume oral intake and the aspiration pneumonia improved. He has returned to normal life and is doing very well (Fig. 16.37).
A Case of Ileocolostomy
The patient was a man in his 40s who was urgently admitted to hospital with a small bowel perforation. It was difficult to anastomose the small bowel loops in one sitting because of severe adhesions resulting from tuberculous peritonitis. Therefore, an ileostomy and an ascending colostomy were placed (Fig. 16.38). The patient was found to be HIV positive postoperatively. The surgeons hesitated to reoperate to perform an anastomosis because of the severe adhesions. Therefore, enteroenteric MCA was attempted between the ileostomy and colostomy because the ostomies were close in position (Fig. 16.39). The distance from each ostomy was so short that the two magnets could be carried by forceps. The two magnets mated closely in parallel such that there were no inclusions between the magnets (Fig. 16.40). The magnets were excreted 8 days later. Dilatation by digital manipulation was performed several times because the anastomotic site was very close to each ostomy. After successful creation of an ileocolostomy, each ostomy was closed surgically (Fig. 16.41).
A Case of MCA Between An Esophagostomy and Gastric Tube
The patient was a man in his 60s who had undergone esophagectomy with gastric tube reconstruction. An anastomotic leak had developed, which was treated by esophagostomy. The plan was to perform an MCA of the esophagostomy and gastric tube after all inflammation and leaking had settled. The parent magnet (12.5 mm in diameter, 5 mm in thickness) was transported from the jejunostomy over the guidewire, and the daughter magnet (the same size as the parent magnet) was placed via the esophagostomy by digital manipulation. However, the gap between the two magnets was wide (7 cm) and the magnets were unable to mate. Twelve disk magnets were then used as the daughter magnet, which resulted in successful mating (Fig. 16.42). The esophagostomy was closed after removal of the mated magnets. Balloon dilatation was performed once or twice a month for about a year, and local triamcinolone acetonide injections were administered via an endoscope on several occasions. An endoscopic study showed smooth elongation of the esophagus (confirmed in a biopsy specimen) connecting to the gastric tube (Fig. 16.43). Eventually, no further dilatation was needed, and the patient was able to resume eating normally.
After removal of the mated magnets, the esophagostomy was closed. Balloon dilatation was performed once or twice monthly for about a year, and a local injection of triamcinolone acetonide were administered via an endoscope on several occasions. Endoscopy showed a smooth anastomosis site with elongation of the esophagus. Finally, no further dilatation was needed, and the patient was able to resume eating normally at mealtimes
A Case of Choledochoduodenostomy
The patient was a man in his 40s with a diagnosis of chronic alcohol-related pancreatitis who had had multiple hospital admissions for acute pancreatitis. Interventional relief consisting of an anastomosis between the dilated main pancreatic duct and stomach was planned (Figs. 16.44 and 16.45). The patient’s episodes of acute pancreatitis had ceased completely after successful creation of the pancreaticogastrostomy. However, a few years later he developed obstructive jaundice due to fibrosis resulting from advanced chronic pancreatitis. Percutaneous transhepatic biliary drainage (PTBD) was performed (Fig. 16.46). An MCA between the CBD and duodenum was planned because the CBD was located beneath the second portion of the duodenum. The daughter magnet was carried via the PTBD route and the parent magnet was transported endoscopically. The magnets mated easily and passed into the duodenum after 2 weeks (Fig. 16.47). The internalized PTBD tube functioned as a tract between the CBD and duodenum and was exchanged every 2–4 weeks for approximately 6 months. Good flow of contrast medium from the CBD to the duodenum was noted when the PTBD tube was removed 6 months later (Fig. 16.48). Follow-up biliary scintigraphy 4 years later showed good flow into the bowel loops through the anastomotic site between the CBD and duodenum (Fig. 16.49).
Attacks of acute pancreatitis had ceased to occur in this patient after successful creation of a pancreaticogastrostomy . However, a few years later, fibrosis caused by the patient’s chronic pancreatitis advanced and he developed obstructive jaundice. Therefore, percutaneous transhepatic biliary drainage was performed
After successful creation of an anastomosis between the common bile duct and duodenum, the tract was kept patent by the internalized percutaneous transhepatic biliary drainage tube, which was exchanged every 2–4 weeks for about 6 months (left). Good flow of contrast medium from the common bile duct to the duodenum was noted when the percutaneous transhepatic biliary drainage tube was removed after approximately 6 months
A Case of MCA Between the Intrahepatic Bile Duct and a Roux-en-Y Jejunal Limb
The patient was a man in his 60s who developed obstructive jaundice as a postoperative complication of laparoscopic cholecystectomy. Therefore, a Roux-en-Y choledochojejunostomy was performed. However, his obstructive jaundice recurred 3 years later. A PTBD tube was inserted at that time. Cholangiography through the PTBD route showed complete obstruction at the anastomotic site (Fig. 16.50). The surgeons were reluctant to perform repeat surgery because of severe adhesions and instead planned an MCA between the intrahepatic bile duct and the Roux-en-Y jejunal limb. The parent magnet was transported under extracorporeal magnetic guidance along the ileus tube because no endoscope that could enter the small intestine was available at that time (Fig. 16.51). Successful creation of the MCA was confirmed by cholangiography through the PTBD route after 12 days. The mated magnets were released from the guidewire, which was attached to the daughter magnet, by pushing firmly over the guidewire. The mated magnets were excreted within a few days (Fig. 16.52). The tract was kept patent by an internalized tube stent for about a year. The tube was exchanged every 2–4 weeks on an outpatient basis.
Obstructive jaundice as a complication 3 years after laparoscopic cholecystectomy. Percutaneous transhepatic biliary drainage was performed. Cholangiography through the percutaneous transhepatic biliary drainage route showed complete obstruction at the anastomotic site. Repeat surgery was not desirable because severe adhesions were expected. A magnetic compression anastomosis (between the intrahepatic bile duct and a Roux-en-Y jejunal limb) was planned
Successful creation of a magnetic compression anastomosis was confirmed by cholangiography through the percutaneous transhepatic biliary drainage route. The mated magnets were released from the guidewire attached to the daughter magnet by pushing firmly on the pusher over the guidewire. The tract was kept patent by an internalized tube stent that was exchanged every 2–4 weeks and left in place for about 1 year
A Case of Choledochocholedochostomy
The patient was a man in his 90s who had undergone an open cholecystectomy for gallstones. After surgery, complete obstruction of the CBD occurred as a result of cholangitis due to leakage, so PTBD was performed (Fig. 16.53). A biliobiliary MCA of CBD was planned. The daughter magnet was brought to the blind end of the CBD via the PTBD route. The parent magnet was then transported endoscopically into the CBD through the ampulla of Vater. The two magnets mated immediately (Fig. 16.54). Successful anastomosis of the CBD was achieved after removal of the internalized tube stent from the PTBD, which was exchanged every 2–4 weeks for 6 months (Fig. 16.55). The patient was able to return to normal life without the need for repeat surgery.
A Case of MCA Between the Intrahepatic Bile Ducts
The patient was a woman in her 50s who had received a living donor left-lobe liver graft and hepaticocholedochostomy and developed a biliary occlusion 1 month following her transplant. A cholangiographic study via the PTBD and CBD routes revealed that the CBD was connected to B4 but not to B2 and B3 (Fig. 16.56). An MCA between the intrahepatic bile ducts was planned. The magnets were inserted via the PTBD and CBD routes. There was still a wide gap of about 30 mm between the magnets on postoperative day (POD) 1. However, both magnets were mated on POD 28 (Fig. 16.57). A fistulous tract was successfully created between the intrahepatic bile ducts, and an internalized tube stent was placed to maintain the patency of the tract (Fig. 16.58). The tube stent was exchanged every 2–4 weeks in the outpatient clinic and was removed uneventfully 1 year later.
A Case of Creation of a New Cystic Duct Between the Gallbladder and CBD by MCA
The patient was a woman in her 70s who had developed obstructive jaundice as a result of lower bile duct cancer. PTBD and percutaneous transhepatic gallbladder drainage (PTGBD) had been instituted to control cholecystitis and obstructive jaundice. She was not a candidate for surgery, and how to manage the PTBD and PTGBD to increase her quality of life posed a major problem (Fig. 16.59). Therefore, we devised a plan whereby a new cystic duct was created to bring together the gallbladder and CBD, after which an endoscopic retrograde biliary drainage stent was placed within the newly fashioned duct. The PTBD and PTGBD routes were able to be removed (Fig. 16.60).
The percutaneous transhepatic gallbladder drainage route separate from the percutaneous transhepatic biliary drainage route. The patient had a lower bile duct cancer that was not indicated for surgery. To increase the patient’s quality of life, the plan was to unify both routes and internalize via a new cystic duct, which was created by a magnetic compression anastomosis between the gallbladder and the common bile duct
The magnets were inserted separately via the percutaneous transhepatic gallbladder and biliary drainage routes. Both magnets mated and a new cystic duct was created between the gallbladder and common bile duct. An endoscopic retrograde biliary drainage stent was then placed through the new cystic duct. The percutaneous transhepatic gallbladder and biliary drainage tubes were then removed
Magnetic Compression Revision for Stenosis
Next, we started to apply MCA as a treatment for stenosis in the gastrointestinal tract as well as creating a bypass route. Two disk magnets of the same size are usually used for this purpose. The parent magnet is transported across the stenosed site after balloon dilation of the stenosis. After mating, the stenotic site is pinched out by the two magnets. This strategy is very effective for an esophageal stricture, for which it is impossible to make a bypass route by MCA (Fig. 16.61) [17].
Diagram showing the process of magnetic compression revision for stenosis . First, the parent magnet is transported across the stenosis, which is temporarily dilated by a balloon catheter. The daughter magnet is then positioned and the magnets are mated. The structure at the site of the stenosis is compressed by the magnets, which are finally removed from the gastrointestinal tract
Representative Clinical Cases
A Case of Magnetic Compression Revision for Stenosis After Distal Gastrectomy
The patient was a woman in her 70s who had undergone distal gastrectomy with Roux-en-Y reconstruction. Postoperative oral intake was almost impossible because of complete obstruction at the anastomotic site between the stomach and jejunum. Endoscopic observation showed excess mucosa at the orifice, but no resistance to insertion of the endoscope. Balloon dilatation was performed unsuccessfully on many occasions (Fig. 16.62). We then planned MCRS to address the excess mucosa. A cone coaxial transporter was devised to carry the pair of magnets (Fig. 16.63). This transporter allows the magnets to be retained in the center of the bowel lumen without bias such that the newly created tract runs in the center of the bowel lumen (Fig. 16.64). Good flow of contrast medium through the anastomotic site confirmed that the MCRS was successful. Endoscopy after MCRS confirmed disappearance of the excess mucosa and reappearance of the orifice that had previously been hidden. The patient was able to resume normal oral intake without the need for further surgery (Fig. 16.65).
Complete obstruction can be seen at the anastomosis on a gastrointestinal study after distal gastrectomy with reconstruction of a Roux-en-Y jejunal limb. Endoscopy shows that the lumen is filled with excess mucosa (arrow). However, the endoscope was inserted easily without resistance. Balloon dilatation was performed many times but unsuccessfully
Apparatus for cone coaxial transport of a parent and daughter magnet. The parent magnet is attached to the caramel-colored cone to make insertion easy. The magnets are positioned at either side of the stenosis. The advantage of this method is that the magnets are kept in the center of the bowel lumen without bias, so the newly created tract runs along the center of the bowel lumen
A Case of MCRS After Esophagectomy
The case was a man in his 50s who had undergone esophagectomy with reconstruction by colon interposition after a previous total gastrectomy. A year later, he developed a stricture at the anastomotic site after a leak-related infection (Fig. 16.66) and required bougie dilatation once or twice a week. At this time, he was eating very small amounts of food at 1.5-hour intervals because he could not eat a normal amount of food at his usual mealtimes. MCRS was planned to remove the stricture. The parent magnet was carried by a sideways transport and pulling up method because this type of stricture can be strong (Fig. 16.67). Using this method, the parent magnet works like an arrowhead that can be easily pushed through the gap in the stricture. The parent magnet works as an anchor for the strings used for pulling up after it is carried across the stricture (Figs. 16.68 and 16.69). The new tract was found to have a wide bore after successful MCRS. An endoscopic study showed improvement of the stricture (Fig. 16.70). The patient did not need further bougie dilatation and was able to resume eating normally.
Results
Technical Success
Mating of the magnets is almost always achieved when sufficient time is available. Three patients who received enteroenteric anastomoses succumbed to their underlying disease before movement of the magnets was seen. Successful creation of an anastomosis was confirmed in all, but 3 of 203 the remaining patients. The overall success rate was 98.5% for enteroenteric MCA (200/203 cases), 97.9% for bilioenteric or biliobiliary MCA (185/189 cases), and 87.5% for MCRS (28/32 cases).
Complications
Emergency laparotomy was required in a patient who received a colocolonic anastomosis after a loop of small bowel became trapped between magnets placed in two large bowel loops. Two further patients required corrective surgery after creation of the anastomosis because the transverse colon became trapped between the magnets in the stomach and duodenum. One patient who received an MCA between the ileum and colon for ileus required surgical removal of the mated magnets because they had passed into the blind iliac loop. Some patients complained of mild abdominal pain until the day after placement of the magnets, which was relieved by analgesics. Leakage was identified in one patient who received an MCA colocolostomy. Leakage was predicted in this case because the oral side of the colon showed marked dilatation without decompression. This was treated by percutaneous drainage. No other complication has been encountered so far.
Discussion
Although the original concept of mechanical compression anastomosis was first proposed as far back as 1821 [1] and refined in 1892, the magnets available at that time were not strong enough to apply sufficient compression to create an anastomosis. After strong permanent magnets became available, Saveliev and Cope proposed the use of MCA in 1993 and 1995, respectively [2,3,4]. However, there were still many problems to solve such as whether the magnets were safe, the incidence of leaks, an effective method for delivering the magnets to various sites in the bowel, and prevention of acute occlusion. Accordingly, this method did not enter clinical use until our early efforts in 1997 [5, 6].
MCA can be performed only when the two target points for anastomosis are relatively close to each other. The magnets strongly attract each other when the distance between them is 3 cm or less. If the distance between the target points for anastomosis is about 3 or 4 cm on plain abdominal radiographs or abdominal CT scans, an endoscope can be used to push one of the magnets to within 3 cm of the other, so that mating is facilitated. Mating of the magnets was achieved at this distance in many cases, so it can be considered as a reasonable standard. Of course, there may be cases in the future where anastomosis cannot be achieved even at a shorter distance or in which anastomosis is possible over a longer distance. Enteroenteric MCA can be attempted over a longer distance because the intestine is more mobile, which makes it possible to create an anastomosis. Bilioenteric MCA is also possible at a distance of more than 3 cm if both magnets are held in place for several days. However, it is difficult to keep the parent magnet in place for this length of time because of peristalsis. In such cases, we fix the parent magnet to the bowel wall endoscopically using gauze and clips (Figs. 16.71 and 16.72).
There are two types of rare-earth magnets , namely, samarium-cobalt and neodymium-iron-boron . We use samarium-cobalt magnets because they have been confirmed in several experiments to be more stable, more heat resistant, and biologically safe. The neodymium-iron-boron magnet is usually plated with nickel to prevent oxidation, so is corrosive and biologically toxic. No allergic reactions to the samarium-cobalt magnet have been observed. All magnets were removed or excreted from the body within 2 weeks to a few months, so the potential long-term effects of the magnetic force need not be considered. Mild blunt pain was observed after insertion of the magnets in 12% of enteroenteric MCA cases. This pain was thought to be related to pinpoint ischemia caused by compression of the magnets in the bowel loop. The progress of the MCA is clearly indicated by the position of the magnets on follow-up plain radiography, a decrease in discharge of bile juice, and the color of secretions.
We did not coat the surface of the magnet with resin or paint in our first 2 or 3 years of performing MCA procedures. However, after encountering a case in which the magnet was eroded by gastric juices (Fig. 16.73), we started coating the magnets with nylon resin to protect them from these juices. No further cases of erosion have occurred since we started taking this precaution.
The same case as shown in Figs. 16.44–16.49. The parent magnet appeared to be eroded on a plain radiograph. The mated magnets were removed after successful creation of the anastomosis and observed in detail. The magnets were found to be very sensitive to gastric acid even they are made of a sintered ceramic
The magnet has a side hole and a top hole. The side hole is mainly used for transport of the magnet over the guidewire or when crossing a stricture, as with sideways transport and the pulling up method. The top hole is used for pulling up to pinch the stenosis in MCRS (see Fig. 16.15). These magnets are not commercially available currently, but will be available for clinical use in the future.
There is inevitably a risk of stenosis every time an MCA is created. Stenosis occurred after the first bilioenteric anastomosis was performed, so the MCA was repeated. The anastomotic site was dilated using a balloon immediately after the magnets moved, which may have damaged the mucosa of the duodenum and CBD when the anastomosis was created, thereby leading to the stenosis. We placed a tube stent to maintain the patency of the tract for 6 months after this case instead of using balloon dilatation as in bilioenteric or biliobiliary MCA cases. However, a stenosis occurred in another bilioenteric MCA case 6 months after removal of a tube stent; MCA was not repeated in this case because we were able to place a tube stent immediately via the PTBD route. The tube stent was kept in place for about 12 months thereafter. There have been no other cases of stenosis requiring balloon dilatation since we started placing a tube stent for 12 months. The tube stent needs to be exchanged every 2–4 weeks in the outpatient clinic to keep it clean. There have been no recurrences of stenosis from the second case of bilioenteric anastomosis onward and no complications, such as retrograde cholangitis, during follow-up. Therefore, it seems reasonable to continue using our present bilioenteric or biliobiliary MCA strategy.
Stenosis may also occur in cases with enteroenteric MCA . Stenosis develops in more than 80% of gastroduodenal or gastrojejunal MCA cases after removal of the mated magnets. Endoscopic investigations show that early detachment of the mated magnets seems to be the cause of the stenosis. Areas without mucosal union occur when the mated magnets are detached prematurely; these areas become ulcerated and then contract when scar tissue forms, leading to restenosis (Figs. 16.74 and 16.75).
Our accumulated experience suggests that stenosis occurs in about 10–20% of cases soon after creation of a total enteroenteric anastomosis. Our immediate objective is to solve this problem. Based on our endoscopic findings, it seems that a stenosis is most likely to occur when the magnet starts to move before the anastomotic site is sufficiently covered by mucosa. One solution may be to use weaker magnets so that the anastomosis takes longer to form, thereby allowing sufficient time for development of the mucosa. Another solution would be to attach a flanged cylindrical stent to the magnets (15 mm in diameter) so that they remain in place for longer after creation of the anastomosis (Fig. 16.76). We have performed mongrel canine experiments to determine whether there is a relationship between the risk of ulceration and the amount of time the flanged cylindrical stent is left in place after MCA gastroduodenostomy [13, 14]. Ulceration at the anastomotic site did not occur when the stent was indwelling for 4 weeks, but did occur when it was indwelling for 2 weeks (Figs. 16.77 and 16.78). We used a flanged cylindrical stent in one patient with a satisfactory result; however, delivery of the stent was problematic, and we do not plan to use this type of stent again until a more straightforward delivery method is found. If we use a larger disk magnet, the rate of stenosis may decrease. However, there is a limit to the size of the magnet that can be used, which is at most about 20 mm in diameter. The best way to prevent acute stenosis is frequent balloon dilatation (FBD ; see Fig. 16.24), which is necessary once or twice weekly for several weeks. We have encountered very few stenoses since adopting this method, even in patients with gastroduodenal or gastrojejunal anastomoses. Although FBD can be performed easily in the upper gastrointestinal tract, it is more difficult to perform in deeper intestinal structures, such as the ileum or colon. In addition to FBD, it is also important to recover oral intake and close a colostomy as soon as possible because passage of food or feces works as a bougie at the anastomotic site. Two cases of leakage after FBD were noted when the anastomotic site was expanded excessively; percutaneous drainage was required in both cases. Therefore, it is important to gradually dilate the anastomotic site when performing FBD.
Two flanged cylindrical stents are mated. The stents are always used as a pair. Each stent is a cylinder with a 3200-gauss samarium-cobalt permanent magnet at one end (arrowheads) and a flange at the other (arrows). The cylindrical stent and its flange are made of silicon rubber (left). The parent flange tube stent is in the duodenum (D) and the daughter stent is in the stomach (S). Note that the mated magnets are compressing the walls (arrow) of the stomach and duodenum (right)
A photograph obtained by opening a mongrel canine gastric wall at the time of sacrifice. The flanged cylindrical stents are still in place at the anastomotic site in a dog from the 2-week indwelling group (left). A macroscopic view from the duodenal side in a dog from the 2-week indwelling group. An ulcer (arrow) can be clearly seen at the anastomotic site (right)
Smooth mucosal union can be seen with no ulceration at the anastomotic site in the 4-week indwelling group. The fine red line (arrow) between the gastric (S) and duodenal (D) mucosa may represent fresh mucosa (left). Photomicrograph showing that the anastomotic site (arrows) is fully covered by fresh mucosa, although muscular union is still underway. The left specimen is hematoxylin-eosin stained and the right is Masson’s trichrome-stained. The upper part is the stomach (S) and the lower part is the duodenum (D) on each photomicrograph (right)
Only two of our cases have needed endoscopic local injection of triamcinolone acetonide to control contraction of scar tissue. However, it is unknown how effective these were, given that several attempts were required to hit the injection.
We have performed more than 20 MCA procedures involving the jejunum and blind end of the jejunum to treat stenosis that developed in the jejunum after total gastrectomy. Our experience has been that the probability of stenosis occurring somewhere in the jejunum after total gastrectomy is about 1 in 300–500 cases. We did have one interesting case of jejunal stenosis after total gastrectomy [23]. This patient developed complete obstruction of the jejunum 1 year after total gastrectomy with Roux-en-Y reconstruction. The obstructed site was only 4 cm below the surgical anastomosis line, not in the main route of the jejunum. MCRS was performed, after which the patient was able to resume eating (Fig. 16.79). We believe that stenosis may occur in the jejunum because the osmotic pressure is difficult to adjust at this site after total gastrectomy. In such cases, repeat surgery is difficult because the operative site is very deep and good results cannot be expected in the presence of severe peritoneal adhesions. MCRS should be considered rather than repeat surgery in such circumstances.
Anastomotic leak is one of the complications of a surgical anastomosis procedure. However, we have encountered almost no leaks after MCA or MCRS. There was only one case of leakage after MCA in a patient in whom colocolostomy was performed to straddle a colon cancer at the splenic flexure because the oral side of the markedly dilated colon was not decompressed, and the leak was predicted.
Damaged to vessels trapped between the magnets is frequently raised as a potential problem with this MCA method. A number of animal experiments have shown that even relatively large vessels that supply the stomach and intestinal tract undergo gradual involution when compressed by the magnets, and new vessels are created that bypass the site of compression to maintain blood flow. However, in our experiments in rats, compression of major vessels, such as the superior mesenteric artery, by the magnets resulted in a mortality rate of up to 60%, suggesting that an anastomosis with the potential to affect large vessels should be performed with the utmost care. In practice, gastroduodenal anastomosis raises such a possibility. Fortunately, we have not experienced this complication. When an enteroenteric MCA is performed, the patient should be observed carefully for severe abdominal pain immediately after the procedure to predict such an event. Bilioenteric or biliobiliary anastomosis rarely involves blood vessels because the magnets are small. Therefore, investigating blood flow in the hepatic artery and portal vein by abdominal ultrasonography does not make much sense.
In the case of bilioenteric MCA , the Roux-en-Y jejunal limb could not be reached with an endoscope at the time we started performing these procedures, so a different method was used to place the parent magnet in the jejunal limb. Our method of extracorporeal magnetic guidance via which the parent magnet is transported alongside the ileus tube was primitive but was very easy to perform and efficient because the correct direction was indicated by the tube and the intestinal tract was straightened, making it simple to move the magnet. Extracorporeal magnetic guidance was performed by alternating of the poles to move the intracorporeal parent magnet forward or across the plica circulares. The poles of the extracorporeal magnets were simply alternated by flipping the magnets back and forth (see Fig. 16.20). Today, a parent magnet can be easily transported into the Roux-en-Y jejunal limb because an endoscope that can enter the small intestine has become available in the past 10 years. This method is expected to be useful when MCA is performed in deep bowel loops, where a small intestine endoscope does not reach in all clinical situations.
In many cases of enteroenteric MCA , an interesting finding is that there is a change in angle between the axis of the mated magnets and the vertical axis (Fig. 16.80). Endoscopic observation revealed that this phenomenon is attributable to the many holes opening around the rim of the magnet, which finally connect and become like the lid of a can (Fig. 16.81). This finding is a good indicator of how well enteroenteric MCA is proceeding.
In bilioenteric or biliobiliary MCA cases, the guidewire attached to the daughter magnet shows a similar change in that the bending of the guidewire is gradually extended. This is because the mated magnets are pushed out to the other side by the guidewire. This finding is also a good indicator of how bilioenteric or biliobiliary MCA is proceeding (Fig. 16.82).
Some patients underwent an MCA or MCRS procedure after implantation of a pacemaker without any particular problems. However, it must be remembered that MRI is absolutely contraindicated while the magnets are in the body.
Conclusion
If magnets can be mated without any problems, the success rate of these procedures should be almost 100%. The advantages of MCA and MCRS are that general anesthesia is not required, the anastomosis can be performed without laparotomy, and no leak occurs. However, there are still many unknown with this new method. No absolute contraindications to MCA or MCRS have been found in our experience so far. However, its limits have yet to be determined, and further research is needed before this method can be used in other clinical settings.
References
Murphy JB. Cholecysto-intestinal, gastro-intestinal, entero-intestinal and approximation without suture. Med Record (NY). 1982;42:665–76.
Saveliev VS, Avaliani MV, Bashirov AD. Endoscopic magnetic cholecystodigestive anastomosis. Personal technique for palliative treatment of distal bile duct obstruction. J Laparoendosc Surg. 1993;3:99–113.
Cope C. Creation of compression gastroenterostomy by means of the oral, percutaneous, or surgical introduction of magnets: feasibility study in swine. JVIR. 1995;6:539–45.
Cope C. Evaluation of compression cholecystogastric and cholecystojejunal anastomoses in swine after peroral and surgical introduction of magnets. JVIR. 1995;6:546–52.
Yamanouchi E, Kawaguchi H, Endo I, Arakawa H, Yamaguchi T, Sakuyama K. A new interventional method: magnetic compression anastomosis with rare-earth magnets. Cardiovasc Intervent Radiol (United States). 1998;21(Suppl(1)):S155.
Yamanouchi E, Kawaguchi H, Endo I, Arakawa H, Yamaguchi T, Sakuyama K. A new interventional method of anastomosis with magnets: magnetic compression anastomosis in five clinical cases. Radiology. 1998;209(P):567.
Yamanouchi E, Sugiura T, Nakamura R, Kushiya H, Sakai F, Okawa T, et al. Further development of magnetic compression anastomosis by extracorporeal magnetic guidance: three clinical cases in bowel loops. Cardiovasc Intervent Radiol (United States). 1999;22(Suppl(2)):S174.
Yamanouchi E, Sugiura T, Sakai F, Kumano R, Takada K, Yamaguchi T. Further development of magnetic compression anastomosis by extracorporeal magnetic guidance: four clinical bowel loop cases. Radiology. 1999;213(P):302.
Yamanouchi E, Sugiura T, Nakamura R, Yasuda Y, Machida H, Fujimura M. Review of 22 clinical cases of magnetic compression anastomosis (MCA). JVIR. 2000;11(2):265.
Yamanouchi E, Machida H, Sugiura T, Yasuda Y, Nakamura R, Fujimura M, Sakai F. Review of 25 clinical cases of magnetic compression anastomosis (MCA). Cardiovasc Intervent Radiol (United State). 2000;23(Supp 1):S157.
Yamanouchi E, Sugiura T, Yasuda Y, Machida H, Nakamura R, Sakai F, et al. Review of 30 cases of magnetic compression anastomosis (MCA). Radiology. 2000;217(P):584.
Yamanouchi E, Ikeda T, Nakamura R, Kumano R, Izumo T, Daimon T, Ueno M, Kobayashi K. Review of 40 clinical cases of magnetic compression anastomosis (MCA). Cardiovasc Intervent Radiol (United State). 2000;24(Supp 1):S190.
Machida H, Yamanouchi E, Sugiura T, Yasuda Y, Nakamura R, Fujimura M, Sakai F. A proposal for a new stent (Eigorotta Yamachicchi Stent) with magnetic compression anastomosis. Cardiovasc Intervent Radiol (United State). 2000;23(Supp 1):S157.
Yamanouchi E, Kumano R, Sugiura T, Matsumoto J, Hayakawa M, Imanishi Y, Ikeda T, Nakamura R, Kobayashi KC, Omae K, Iinuma Y, Oonishi T. A proposal of a new stent (Eigorotta Yamachicchi Stent) for magnetic compression anastomosis (MCA). Radiology. 2001;221(P):106.
Takao S, Matsuo Y, Shinchi H, Nakajima S, Aikou T, Iseji T, Yamanouchi E. Magnetic compression anastomosis for benign obstruction of the common bile duct. Endoscopy. 2001;33(11):988–90.
Yamanouchi E, Kumano R, Sugiura T, Matsumoto J, Hayakawa M, Imanishi Y, Ikeda T, Nakamura R, Kobayashi KC, Omae K, Iinuma Y, Oonishi T. Review of 43 clinical cases of magnetic compression anastomosis (MCA). Radiology. 2001;221(P):107.
Yamanouchi E, Kumano R, Nakayama M, Omae K, Iinuma Y, Matsumoto J, Oonishi T, Hayakawa M, Imanishi Y. Magnetic compression revision anastomosis for stenosis. Cardiovasc Intervent Radiol (United States). 2002;25(Suppl(2)):S209.
Yamanouchi E, Kumano R, Kobayashi K, Hattori T, Matsumoto J, Oonishi T, Hayakawa M, Tani I. Treatment for bowel or biliary obstruction by magnetic compression anastomosis. J Nippon Med Sch. 2002;69(5):471–5.
Yamanouchi E, Kumano R, Kobayashi K, Hattori T, Matsumoto J, Oonishi T, Hayakawa M, Tani I. Review of 59 clinical cases of magnetic compression anastomosis (MCA). Radiology. 2002;225(P):220–1.
Okajima H, Kotera A, Takeichi T, Ueno M, Ishiko T, Hirota M, Asonuma K, Yamanouchi E, Inomata Y. Magnet compression anastomosis for bile duct stenosis after duct-to-duct biliary reconstruction in living donor transplantation. Liver Transpl. 2005;11(4):473–5.
Itoi T, Yamanouchi E, Ikeda, Sofuni A, Tsuchiya T, Tsuchida A, Kasuya K, Moriyasu F. Magnetic compression anastomosis: a novel technique for canalization of severe hilar bile duct strictures. Endoscopy. 2005;37:1248–51.
Nakaseko Y, Shiba H, Yamanouchi E, Takano Y, Sakamoto T, Imazu H, Ashida H, Yanaga K. Successful treatment of stricture of duct-to-duct biliary anastomosis after living-donor liver transplantation of the left lobe: a case report. Transplant Proc. 2017;49:1644–8.
Kamada T, Ohdaira H, Takeuchi H, Takahashi J, Marukuchi R, Suzuki N, Narihiro S, Hoshimoto S, Yoshida M, Yamanouchi E, Suzuki Y. Magnetic compression anastomosis for nonanastomotic stenosis of the proximaljejunum after total gastrectomy with Rouxen-Y reconstruction: a case report. Surgical Case Reports 2020;6:167.
Kamada T, Ohdaira H, Takeuchi H, Takahashi J, Ito E, Suzuki N, Narihiro S, Yoshida M, Yamanouchi E, Suzuki Y. New Technique for Magnetic Compression Anastomosis Without Incision for Gastrointestinal Obstruction. Journal of the American College of Surgeons. 2020;232:170–77.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yamanouchi, E., Kumano, R., Ohdaira, H., Suzuki, Y. (2021). Magnetic Compression Anastomosis and Magnetic Compression Revision for Stenosis. In: Gagner, M. (eds) Magnetic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-73947-8_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-73947-8_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73946-1
Online ISBN: 978-3-030-73947-8
eBook Packages: MedicineMedicine (R0)