Abstract
Myeloma bone disease (MBD) is present in up to 90% of multiple myeloma (MM) patients and is a product of osteolytic lesions due to dysregulated osteoblast and osteoclast function. Myeloma bone disease is a cause of significant morbidity and decreased quality of life in MM patients as it leads to several skeletal-related events including pathologic fractures, severe bone pain, and spinal cord compression. Bisphosphonate drugs and the monoclonal antibody denosumab are currently the only approved treatments for MBD, despite their potential severe adverse events such as osteonecrosis of the jaw. Further studies and the continued development of novel treatments for MBD are needed to better combat MBD. This chapter will review the available efficacy data of current bisphosphonate drugs in use and denosumab and their mechanisms of action, explore the pathways and potential targets involved in MBD, and review the current progress in the developments of a number of potential novel treatments for MBD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Multiple myeloma
- Myeloma bone disease
- Bisphosphonate drugs
- Pamidronate
- Zoledronic acid
- Denosumab
- Myeloma bone disease treatment
8.1 Myeloma Bone Disease
Multiple myeloma (MM) is a cancer of differentiated B lymphocytes (plasma cells) and is characterized by clonal proliferation of these plasma cells in the bone marrow, the secretion of a monoclonal protein, and osteolytic bone disease [1]. Myeloma bone disease (MBD) is present in up to 90% of patients and is a result of plasma cell proliferation, characterized by osteolytic lesions and the suppression of osteoblast differentiation and function [2]. Current International Myeloma Working Group (IMWG) guidelines require the presence of at least one osteolytic lesion to meet the criteria for MBD [3]. Myeloma bone disease leads to several skeletal-related events (SREs) including pathologic fractures, severe bone pain, and spinal cord compression which can result in the need for radiotherapy or surgical fixation [4]. In MM patients, pathologic fractures increase the risk of death by more than 20% compared to patients without fractures [5]. Hence, despite increasing overall survival (OS) for patients with multiple myeloma, MBD and secondary SREs can result in significant morbidity and reduced quality of life, highlighting the need for advancements in the current standard of care [1].
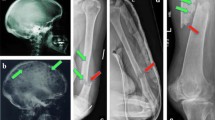
8.1.1 Diagnosis
Myeloma bone disease is diagnosed through the use of plain radiograph, whole body low dose computed tomography, or whole body magnetic resonance imaging skeletal surveys to detect the presence of osteolytic bone lesions [6]. Plain radiograph is the least sensitive available type of imaging, as a bone lesion needs to be at least 1 cm in size and associated with at least 30% loss of bone mineral content before it can be detected [7]. Despite this, most current guidelines recommend plain radiograph skeletal survey as the primary method for the detection of MBD, followed by the utilization of other modalities if there is a suspicion of MBD and conventional radiography is negative [3, 8]. Imaging findings such as osteoporosis, osteopenia, or compression fractures without the presence of osteolytic lesions is insufficient to meet the current criteria for MBD [6]. The IMWG has also noted that increased fluorodeoxyglucose uptake on positron emission tomography (PET) scan without an associated destructive bone lesion does not meet the criteria for MBD [3].
8.1.2 Pathogenesis
Myeloma bone disease occurs as a result of numerous interactions between plasma cells and various pathways that affect osteoclasts and osteoblasts, leading to overall bone loss and the development of lytic bone lesions [1]. While augmented osteoclast function is a key pathogenic mechanism in the development of MBD, the reduction in trabecular thickness, calcification rate, and osteoblast numbers in bone specimens from multiple myeloma patients suggest that dysfunctional osteoblast activity is a significant contributor [9].
Osteoblasts and osteoclasts are the major cells involved in bone remodeling, with other factors including osteocytes, cytokines, and hormones also contributing to the process [10]. Osteoclasts are large multinucleated cells derived from monocyte-macrophage lineage which generate enzymes that breakdown the bone mineral matrix [11]. Osteoblasts are mononuclear cells originating from mesenchymal stem cells which contain the enzyme alkaline phosphatase [12]. Immature osteoblasts secrete interleukin (IL)-6 that upregulates osteoclasts, while mature osteoblasts secrete osteoprotegerin (OPG) which inhibits the activation of osteoclasts [1]. Osteoblasts create the bone mineral matrix through the secretion of collagen and eventually become trapped as part of the mineralized matrix before differentiating into osteocytes [11]. Osteocytes communicate with surrounding cells in the bone surface and bone marrow via cytoplasmic projections and contribute factors such as receptor activator of nuclear factor kappa-B ligand (RANKL) and sclerostin that affect both osteoblastic and osteoclastic activity [13].
The normal signaling pathways are disrupted by interactions between malignant plasma cells (myeloma cells) and cells of the bone marrow microenvironment [14]. A group of mediators known as osteoclast-activating factors (OAFs) have been identified which include IL-6, interleukin-1 (IL-1), interleukin-3 (IL-3), macrophage-inhibitory protein 1 alpha (MIP-1ɑ), tumor necrosis factor-alpha (TNF-ɑ), hepatocyte growth factor (HGF), and vascular endothelial growth factor (VEGF) [14]. These OAFs affect various components of other pathways including the receptor activator of nuclear factor kappa-B (RANK), RANKL, and OPG. Additionally, certain molecules have been shown to inhibit osteoblast differentiation, including transforming growth factor-beta (TGF-β), HGF and Wnt-signaling inhibitors dickkopf-1 (DKK1), soluble frizzled-related protein-3 (sFRP3), and sclerostin [14].
In the early stages of MBD, myeloma cells secrete IL-1 and tumor necrosis factor (TNF) which stimulate osteoblast differentiation and recruitment to affected sites. These recruited osteoblasts in turn secrete IL-6, which recruits osteoclasts and is a myeloma growth factor [7]. Later in MBD, osteoblast numbers decrease secondary to unclear mechanisms; postulated to be related to osteoblast inhibitory factors or decorin, a proteoglycan produced by osteoblasts which causes an anti-myeloma effect by inhibiting TGF-β [1]. Myeloma also affects osteoprogenitor cells, disrupting the normal production of osteoblasts, resulting in a net effect of reduced osteoblast levels and over activation of osteoclasts and leading to the lytic bone lesions found on imaging in MBD [15]. Hence, any coupled bone remodeling between osteoclasts and osteoblasts is disordered in MM. The numerous factors that affect osteoclasts and osteoblasts and contribute to the pathogenesis of MBD and may be potential foci for bone targeted therapies and are explored in further detail below [4].
8.1.3 Osteoclastic Activation
8.1.3.1 The RANK/RANKL Pathway
The RANK/RANKL pathway plays a major role in osteoclast function and bone remodeling [4]. RANK is a transmembrane receptor that is expressed on the surface of osteoclast precursors, and RANKL is a membrane-bound protein on stromal cells of the osteoblast line and activated T lymphocytes [11]. The binding of RANKL to RANK triggers the maturation of osteoclast precursors into osteoclasts that bind to the bone surface and initiate bone resorption [14]. OPG is a cytokine secreted by osteoblasts and stromal cells that is a soluble decoy receptor for RANKL that inhibits osteoclast development; in MM patients OPG levels are reduced while RANKL levels are increased [4]. RANKL is produced by myeloma cells and increased RANKL expression by osteoblasts and bone marrow stromal cells can result from stimulation by other contributory cytokines such as increased levels of parathyroid hormone-related peptide [11]. This imbalanced ratio of RANKL to OPG results in a net increase in osteoclast stimulation and bone resorption. Treatments including thalidomide and autologous stem cell transplant can normalize the RANKL to OPG ratio, reducing bone resorption. Denosumab, a human monoclonal antibody (MoAb) targeting RANKL, prevents the activation of this signaling pathway and reduces the burden of MBD as well as progression of disease [16].
8.1.3.2 Interleukins
IL-3 stimulates osteoclast formation and inhibits osteoblast differentiation. IL-3 exerts its osteoclastogenic effect by inducing activin A production by macrophages, a factor involved in promoting osteoclast differentiation [11]. IL-3 also acts in conjunction with RANKL and MIP-1α to increase osteoclastogenesis [14]. Increased levels of IL-3 have been detected in studies of myeloma patient’s bone marrow plasma [17]. IL-6 augments osteoclast differentiation by simulating myeloma cells to secrete VEGF which activates osteoclasts via surface receptor binding [11]. IL-6 levels are lowered with DKK1 protein inhibition [14]. IL-17 promotes osteoclast activation and can result in osteolytic lesion formation, although this has been seen mainly in preclinical models [18].
8.1.3.3 Hepatocyte Growth Factor
HGF is produced by bone marrow stem cells (BMSCs) and myeloma cells. The binding of HGF to MET receptor on the surface of myeloma cells triggers downstream signaling via the RAS pathway, causing the growth of myeloma plasma cells and inhibiting apoptosis [11]. HGF also acts as a coupling factor between osteoclasts and osteoblasts and mediates autocrine regulation of osteoclasts and paracrine regulation of osteoblasts.
8.1.3.4 Notch Pathway
There are four Notch transmembrane receptors on myeloma cells that can bind to their ligands on the same cell or on adjacent BMSCs which results in the production of RANKL by the myeloma cells [11]. This generates a feedback loop which stimulates Notch2. The resulting Notch2 signaling cascade further stimulates osteoclast differentiation and proliferation. Inhibition of this pathway results in apoptosis of myeloma cells and inhibits osteoclastogenesis, representing a potential therapeutic target [11].
8.1.3.5 Chemokines
Certain chemokines are involved in osteoclastogenesis. Chemokine (C-C motif) ligand 3 (CCL-3) is secreted by myeloma cells. Chemokine (C-C motif) ligand 20 (CCL-20) is overexpressed in the multiple myeloma bone marrow. These chemokines induce osteoclastogenesis, and higher levels are detected in myeloma patients, correlating with the extent of bone disease [11]. Chemokine receptors including the CCL-3 receptor, CCR1 receptor, and CCR5 receptor are expressed on BMSCs, osteoclasts, osteoblast, and MM cells. The activation of these receptors attracts immature osteoclasts, promoting differentiation and stimulating RANKL and IL-6 [11]. Inhibitors of CCL-3 and its receptors are promising in preclinical studies for MBD therapy [16].
8.1.3.6 Activin A
When activin A binds to activin type 2A receptor, subsequent signaling results in increased bone resorption and reduced bone formation [16]. Activin A is elevated in myeloma patients, correlating with the extent MBD [11]. Activin A is further upregulated by IL-3, a cytokine released from the BMSCs of myeloma patients [16]. There is a synergistic effect between Activin A and RANKL, resulting in more potent stimulation of osteoclastogenesis. Preclinical studies have demonstrated that osteoclast formation is blocked following treatment with soluble activin receptor type 2A [11].
8.1.3.7 The TNF Superfamily
Key members of the TNF superfamily involved in MBD include TNF-α and B-cell activating factor (BAFF). TNF-α acts together with RANKL to induce osteoclast differentiation and growth and is elevated in MBD patients [11]. BAFF is secreted by myeloma cells, osteoclasts, and BMSCs, causing the activation of nuclear factor kappa-B (NF-κB), resulting in osteoclastogenesis and myeloma cell survival [14].
8.1.3.8 BTK and SDF-1α
Bruton’s tyrosine kinase (BTK) regulates osteoclast differentiation and is expressed in osteoclasts. Higher levels of BTK expression have been observed in myeloma patients [16]. BTK is linked to CXCR4 expression. The CXCR4SDF-1α pathway induces BTK activation, promoting osteoclastogenesis [11]. Inhibition of osteoclastic activity through agents like ibrutinib is being investigated in current clinical trials [19]. This could potentially be an added therapy in patients with severe myeloma bone disease.
8.1.4 Osteoblastic Suppression
8.1.4.1 The WNT Pathway
The Wnt-signaling pathway cascade ultimately results in gene expression favoring bone formation and imminent bone resorption [11]. It is activated via Wnt ligands and parathyroid hormone binding to receptors in the Wnt pathway. Preclinical models demonstrate that increased Wnt signaling inhibits the development of MBD [20]. Conversely, aberrant Wnt signaling can result in the proliferation of myeloma cells and the subsequent development of MBD [11]. This dysregulated Wnt pathway signaling contributes to the invasion of myeloma cells and is linked to their adhesion-mediated drug resistance [21]. The canonical Wnt pathway is inhibited by sclerostin , DKK1, and sFRP2. These proteins have been observed to be elevated in cases of MBD and may be potential therapeutic targets [11].
8.1.4.2 Sclerostin
Sclerostin is a protein encoded by the SOST gene and is produced by osteocytes. Sclerostin induces the apoptosis of mature osteoblasts and reduces osteoblast-driven bone formation [14]. It is an inhibitor of the canonical Wnt pathway through binding to LRP5/6 transmembrane receptors on osteoblasts, blocking the Wnt pathway cascade [11]. Sclerostin is secreted by myeloma cells and suppresses bone formation by inhibiting osteoblastogenesis while stimulating osteoclastogenesis by increasing the ratio of RANKL to OPG ratio [22]. High levels of sclerostin have been observed in patients with more severe disease and pathologic fractures at diagnosis [11]. Monoclonal antibodies against sclerostin are under investigation as a sole therapy for MBD and in conjunction with proteasome inhibitors (PI) [23].
8.1.4.3 DKK1
DKK1 inhibits the Wnt-signaling pathway by competitively binding LRP5/6 receptors and removing transmembrane proteins [14]. DKK1 inhibits osteoblastogenesis by blocking osteoblast differentiation and acts together with sclerostin resulting in osteoblast dysfunction [11]. DKK1 also indirectly increases osteoclastogenesis, by blocking the osteoclastogenesis inhibitor OPG and increasing the osteoclastogenesis activator RANKL [14]. Higher DKK1 levels have been observed in patients with more extensive MBD [24]. DKK1 expression can be utilized to predict early SREs, and reduced levels can be observed after myeloma treatment has commenced [11].
8.1.4.4 Periostin
Periostin is a protein produced by BMSCs that activates the integrin-AKT-FAK- β-catenin pathway and is implicated in the Wnt-signaling pathway [11]. High periostin levels in myeloma patients are associated with SREs, lytic bone lesions, and more advanced disease [25].
8.1.4.5 RUNX2/CBFA1 and IL-7
IL-7 reduces osteoblast differentiation and stimulates T lymphocytes to secrete RANKL. IL-7 reduces transcriptional levels of runt-related transcription factor 2 (RUNX2) via the noncanonical Wnt-signaling pathway [11]. RUNX2 is required for osteoblastogenesis, and both reduced levels of RUNX2 [12] and increased levels of IL-7 [14] have been observed in myeloma patients with MBD.
8.2 Indications for Bone Targeted Therapies
Bisphosphonate drugs are currently the only therapy approved in Australia for the treatment of MBD. The IMWG recommends considering bisphosphonate therapy [23], including patients with no visible lesions on conventional radiology [31]. It is difficult to accurately determine whether MM patients without radiological evidence of bone disease would benefit from bisphosphonates as most clinical trials did not stratify patients according to the presence of lytic lesions prior to treatment. Certainly, there is no indication that bisphosphonate therapy in the setting of smoldering myeloma or monoclonal gammopathy of uncertain significance (MGUS) reduces the time or likelihood of progression to MM [31].
8.3 Utility of Bone Resorption Markers to Guide Therapy
Currently, the use of bone turnover markers to guide therapy and predict response or disease progression in myeloma is controversial, with mixed results across studies and a lack of consensus regarding appropriate markers. International guidelines do not currently support the utilization of bone turnover or resorption markers to guide therapy given the lack of convincing evidence [31]. A recent study examining 123 patients with newly diagnosed multiple myeloma measured β-isomerized C-terminal telopeptide of collagen type I (β-CTX), which reflects the resorptive osteoclast activity, and bone-specific alkaline phosphatase (bALP) over a 12-month period [26]. This study found that bALP levels did not have a clear relationship with the degree of underlying bone disease; however, β-CTX levels were increased in those patients with underlying bone disease, with a correlation between the degree of bone lesions and β-CTX levels [26]. Hence, changes in β-CTX levels could potentially reflect the degree of MBD burden and may be a clinically useful marker. A small retrospective study of patients receiving bisphosphonate therapy found that increasing levels of β-CTX were linked to increased likelihoods of disease progression [27]. Several other studies have utilized urinary N-telopeptide of type 1 collagen (uNTX) as well as ALP to predict fracture risk in MM patients on bisphosphonates and concluded that these biomarkers did not correlate to fracture risk [28, 31]. Until further studies provide stronger evidence for the utility of bone turnover markers in guiding therapy for MBD, there is currently no support for their use.
8.4 Current Treatments for Myeloma Bone Disease
8.4.1 Bisphosphonates
8.4.1.1 Mechanism of Action
Bisphosphonates are the mainstay of MBD prevention and treatment. They are pyrophosphate analogs which bind with varying affinity to hydroxyapatite and become integrated into the bone matrix [31]. Bisphosphonates are then released from hydroxyapatite secondary to bone resorption and are potent inhibitors of osteoclast activity and signaling [4]. Bisphosphonates are absorbed by macrophages and mature osteoclasts and induce apoptosis via ATP metabolites [14]. The potency of different bisphosphonates is dependent on their binding affinity for hydroxyapatite; the nitrogen group in the phosphate-carbon-phosphate core of pamidronate and zoledronic acid renders them 100–10,000 times more potent than etidronate and clodronate, as seen in Table 8.1 [29].
8.4.1.2 Evidence in MBD
Treatment with pamidronate or zoledronic acid has been proven to improve symptoms related to MBD and prevent SREs. A 1996 study compared pamidronate with placebo in 392 MM patients demonstrated significant protection against SREs [30]. A non-inferiority trial comparing pamidronate with zoledronic acid for MBD demonstrated equivalence between the two therapies [4]. As a result, pamidronate and zoledronic acid have become the standard of care for MBD. There is currently some evidence for the use of oral clodronate, which has been shown to lower the incidence of SREs compared with placebo [31].
8.4.1.3 Comparison Between Bisphosphonates
Pamidronate and zoledronic acid are the two most commonly utilized bisphosphonates for MBD. They are nitrogen-containing bisphosphonates, which were proven to be superior at reducing SREs compared with non-nitrogen containing bisphosphonates in the MRC Myeloma IX trial [32]. A review of 20 studies found that zoledronic acid improved overall survival compared to placebo and etidronate, but not compared with other bisphosphonates [31]. An observational study comparing zoledronic acid with pamidronate found that patients treated with zoledronic acid had significantly less mortality and SREs compared with patients treated with pamidronate [33]. However, a randomized controlled trial comparing zoledronic acid with pamidronate found that they had similar efficacies in MBD [34]. Hence, current recommendations suggest the use of zoledronic acid or pamidronate as primary treatment for MBD.
8.4.1.4 Adverse Events
Bisphosphonates can cause several rare but serious side effects including osteonecrosis of the jaw, atypical femoral fractures, and renal impairment. More common side effects include acute phase reactions, injection site reactions, transient fevers, myalgias and flu-like symptoms, hypocalcemia, and hypophosphatemia [31]. Bisphosphonates also cause ocular side effects, which typically have a rapid onset ranging from within days to hours, such as conjunctivitis, uveitis, episcleritis, scleritis, and keratitis [35]. The more severe side effects are discussed in greater detail below.
8.4.1.5 Renal Impairment
The kidneys are responsible for 40% of bisphosphonate excretion via glomerular filtration and active tubular excretion, and as such, are extremely sensitive to bisphosphonates [4]. Both acute and chronic renal impairment can result from bisphosphonate therapy, but the level of kidney damage is related to blood drug levels [31]. Nephrotoxicity is directly linked to the maximum plasma concentration, bisphosphonate dose, and infusion time [4]. Renal impairment is seen equally with zoledronic acid and pamidronate however zoledronic acid has more potential for accumulation in the kidneys due to its prolonged half-life [4]. Kidney injury related to zoledronic acid is most often caused by tubular toxicity, and hence acute tubular necrosis. Comparatively, pamidronate more commonly causes acute kidney injury and nephrotic range proteinuria [31]. Patients with elevated creatinine levels at baseline are at higher risk of developing acute renal injury related to bisphosphonate treatment [36]. Dosing variations are required in renal impairment , as described in Table 8.2.
8.4.1.6 Osteonecrosis of the Jaw
Osteonecrosis of the jaw is a rare but serious side effect of bisphosphonate therapy. Characteristic features include exposed bone in the oral cavity, severe pain, necrosis, and increased risk of secondary infections at the site of osteonecrosis [4]. The symptoms preceding an osteonecrotic lesion include mucosal swelling, ulceration, loose dentition, pain, or a nonhealing socket after tooth extraction [4]. The pathogenic etiology of osteonecrosis of the jaw is not clear but thought to be related to reduced vascularity of the bones of the maxilla and mandible, risk of dental infections, and bone turnover suppression [31]. The anti-angiogenic properties of bisphosphonates also contribute to osteonecrosis risk, due to an interruption of blood supply [37]. The suppression of bone remodeling appears to play a major role, evidenced by the higher rates of osteonecrosis of the jaw associated with treatment with higher potency bisphosphonates like zoledronic acid [31]. Excessive inhibition of bone remodeling can occur secondary to the long half-life of bisphosphonates and potential accumulation if administered monthly [31]. Osteonecrosis may not only be due to bisphosphonate therapy but may be an outcome of bone modeling suppression, supported by animal models and given that osteonecrosis of the jaw can occur with denosumab therapy [38].
The risk factors for osteonecrosis of the jaw include potency, dosage, and exposure duration to bisphosphonate therapy [31]. Several studies have shown that the incidence of osteonecrosis of the jaw increases with longer exposure to bisphosphonate therapy. The median time to development of osteonecrosis of the jaw was shorter for intravenous administration compared to oral administration in a single center study; 34–54 months for intravenous versus 16 months for oral bisphosphonates [39]. Patients with preexisting dental disease or concomitant dental procedures had significant increases in the risk of osteonecrosis of the jaw. Dental extraction caused an approximately nine times higher risk of osteonecrosis of the jaw development [38]. Alterations within the genes that affect bone turnover and collagen formation, and metabolic bone diseases may also predispose patients to osteonecrosis of the jaw [40].
As such, dental assessment prior to initiation of bisphosphonate is recommended in order to minimize the risk of developing osteonecrosis of the jaw. Any existing lesions should be addressed prior to bisphosphonate therapy, and bisphosphonates should be withheld for 90 days before or after any dental extraction [31]. In the event of osteonecrosis of the jaw developing, bisphosphonate therapy should be discontinued until the lesion is healed and treatment has been given as required [23].
8.4.1.7 Subtrochanteric and Other Atypical Femoral Fractures
The symptoms of atypical femoral fractures can be subtle and preceded by thigh or groin pain prior to diagnosis [31]. Long-term bisphosphonate use is linked to the development of atypical femoral fractures in approximately 93.9% of cases [41]. The majority of atypical femoral fractures occur at the proximal femur, with a minority occurring at the subtrochanteric region along the femoral shaft [42].
8.4.1.8 Duration, Frequency, and Monitoring of Therapy
Doses for bisphosphonate therapy are adjusted for renal function as described in Table 8.2. Zoledronic acid is not recommended in creatinine clearance rates <30 mL/min given to the lack of available evidence. Pamidronate can be utilized in patients with significant renal disease, defined as having an estimated creatinine clearance of <30 mL/min. While expert guidelines do not currently include dosing guidelines in patients with a creatinine clearance of <30 mL/min, expert panels recommend that a reduced dose is used [43].
The American Society of Clinical Oncology (ASCO) guidelines suggest that bone targeted therapy continues for a period of at least 2 years, and if ceased, should resume upon multiple myeloma relapse with any new SREs [43]. The frequency of dosing is recommended to be around every 3–4 weeks with intravenous zoledronic acid or pamidronate, or daily for oral clodronate therapy [31]. Less frequent dosing may be considered in patients with responsive or stable disease. Three-month intervals of therapy may be considered in patients with inactive myeloma or on maintenance therapy [3].
Renal function should be monitored before each dose of pamidronate or zoledronic acid, and in the event of an acute rise in creatinine, therapy should be withheld until renal function normalizes within 10% of baseline [31]. Serum calcium and vitamin D levels should be reviewed intermittently during therapy and replaced as required. Intermittent review of albuminuria on a spot urine sample is recommended every 3–6 months, and if present should lead to further evaluation with a 24-h urine collection [43].
8.4.1.9 Future of Bisphosphonate Therapy
Bisphosphonates are the cornerstone of bone targeted therapy in MM. Despite adverse effects and the development of new therapies, bisphosphonates remain the standard of care for MBD in all major guidelines [44]. There is ongoing research evaluating different dosing strategies and administration schedules of bisphosphonates as sole therapy and in conjunction with new bone therapies. Denosumab , a human MoAb against RANKL, has recently been approved by the US Food and Drug Administration (FDA) for the treatment of MBD and was shown to be non-inferior to zoledronic acid in phase III randomized controlled trial [45]. Further agents under investigation include anti-DKK1 MoAbs, and therapies targeting activin A and CCR1 [16].
8.4.2 Denosumab
8.4.2.1 Mechanism of Action
Denosumab is a fully humanized MoAb that binds RANKL, preventing RANKL from activating RANK on the surface of osteoclasts. This inhibits osteoclast function and osteoclastogenesis by preventing the RANK–RANKL interaction [14]. Denosumab mimics the endogenous effects of OPG by lowering the amount of RANKL and thus decreasing the osteoclastogenesis [1]. Unlike bisphosphonates, denosumab does not become embedded in the bone mineral matrix but binds RANKL in the extracellular fluid and circulation to inhibit osteoclasts formation [10]. Denosumab is cleared from the circulation by the reticuloendothelial system and has a half-life of approximately 26 days [10].
8.4.2.2 Evidence in MBD
Denosumab has been approved by the FDA for the treatment of bone disease in solid organ cancers since 2010 but was not been approved for use in MBD until 2018. The approval of denosumab for use in MBD was largely based upon the results of phase III randomized, controlled trial of denosumab versus zoledronic acid in patients with newly diagnosed MM [45]. The study recruited 1718 patients, with 859 patients assigned to each arm of the study. In the denosumab treatment arm, subcutaneous denosumab 120 mg was given along with intravenous placebo every 4 weeks. In the zoledronic acid treatment arm, intravenous zoledronic acid 5 mg was given along with subcutaneous placebo every 4 weeks. The study showed that the median time to the first on-study SRE was similar between the denosumab and zoledronic acid arms (22.83 months with denosumab versus 23.98 months with zoledronic acid). Median progression free survival (PFS) was prolonged in the denosumab arm by 10.7 months compared to the zoledronic acid arm (P = 0.036). Prior to this landmark study, denosumab had been successfully studied in phase II and III trials in patients with solid organ cancer bone disease and those at high risk of developing bony metastatic disease, with results reporting that denosumab was equal to zoledronic acid in preventing or delaying SREs [16].
8.4.2.3 Adverse Events
The adverse events seen most commonly with denosumab therapy include neutropenia, thrombocytopenia, and anemia [45]. Renal toxicity is significantly lower in denosumab therapy compared with bisphosphonate therapy, and denosumab can be utilized in patients with poor baseline renal function without dose adjustment [46]. In a study of single-dose denosumab in patients with varying degrees of renal impairment, 15% of patients developed hypocalcemia. The severity of hypocalcemia appeared to relate to the severity of renal impairment, and two patients required hospitalization for treatment [46]. The serum nadir of hypocalcemia tends to appear approximately 10 days after administration of denosumab. Other associated adverse events include osteonecrosis of the jaw, nausea and vomiting, pneumonia, back pain, headache, arthralgia, and injection site reactions. Interestingly, in the phase III trial of denosumab versus zoledronic acid, the incidence of osteonecrosis of the jaw was not significantly different between denosumab and zoledronic acid arms [45].
8.4.2.4 Duration and Frequency of Therapy
Denosumab therapy is typically administered at 120 mg doses every 4 weeks subcutaneously with no dose adjustments required for renal impairment [45]. The length of therapy in MBD is not yet established given the recency of approval for denosumab therapy in this area. However, given the findings of the phase III trial of denosumab versus zoledronic acid, it can be extrapolated that denosumab may be dosed at the same length and frequency as current bisphosphonate guidelines. This is the area that currently needs further development as denosumab is incorporated into current treatment guidelines.
8.4.3 Novel Therapies
8.4.3.1 Anti-Sclerostin Antibodies
Sclerostin is a soluble Wnt antagonist produced by osteocytes, which binds to Wnt coreceptors LRP5/6 to inhibit the Wnt-signaling pathway during bone formation, leading to an increase in osteoclastogenesis via RANKL production and OPG inhibition [1]. Multiple myeloma results in elevated sclerostin expression, and a reciprocal decrease in osteoblast markers. Sclerostin expression has been observed to be restricted to osteocytes, presenting a potential therapeutic target [47]. Anti-sclerostin therapies such as romosozumab, a humanized anti-sclerostin MoAb, have shown improvements in bone formation and bone mineral density in osteoporosis [1]. The effects of anti-sclerostin treatment on MBD currently remain unknown.
Anti-sclerostin MoAbs have been effective in mouse models and humans in promoting bone formation in the context of osteoporosis [16]. Anti-sclerostin treatment in mice with multiple myeloma has resulted in the normalization of bone volumes by increasing trabecular bone volume and thickness, increased osteoblastogenesis, reduced osteolytic lesions, and reduced bone loss [1, 47]. These mouse models also demonstrated a potential link between DKK1 and sclerostin; as DKK1 appeared to control increases in sclerostin by inducing its release from osteoblasts [48]. Romosozumab has been shown to increase bone mineral density and bone formation in numerous studies, mainly in the setting of postmenopausal osteoporosis [48]. However, romosozumab has been shown to increase the risk of cardiovascular events by 2.5% [1].
Anti-sclerostin antibodies have also been shown to reduce bone marrow adipose tissue, which has a downstream effect of reducing signaling molecules such as adipokines and fatty acids that normally promote the growth of myeloma plasma cells and osteolytic lesions [49]. Overall, sclerostin inhibition has been demonstrated to be beneficial in postmenopausal osteoporosis but there is currently a lack of evidence to support its use in MM [50].
8.4.3.2 Anti-DKK1 Neutralizing Antibodies
The DKK1 protein negatively regulates the Wnt/β-catenin signaling pathway. DKK1 binds to LRP 5/6 receptors, causing β-catenin breakdown by the proteasome and reducing osteoblast differentiation [51]. DKK1 prevents the differentiation of stem cells into mature osteoblasts by downregulating the Wnt signaling required for osteoblast differentiation [11]. The undifferentiated stem cells secrete IL-6, promoting the expansion of myeloma cells which further secrete DKK1 [52]. DKK1 also causes an increase in the ratio of RANKL to OPG, increasing osteoclastogenesis and leading to the development of MBD [53].
DKK1 inhibition via a neutralizing antibody has been studied in murine and humanized MM models. Antibodies such as BHQ880 and DKN-01 aim to increase osteoblast differentiation and activity by DKK1 blockade and Wnt-signaling pathway modulation [54]. In vitro studies have observed that DKK1 inhibition promotes osteoblast differentiation and activity and inverts the negative effects of myeloma cells on osteoblast differentiation. These findings were demonstrated by the increased trabecular thickness of bone [55]. In vivo studies have demonstrated that DKK1 antibodies can improve bone formation, osteoblast numbers, and decrease lytic lesions [4].
A phase IB trial has evaluated the combination of DKK1 antibodies and bisphosphonate therapy in MM patients [56]. The study demonstrated that the combination therapy resulted in a delay in SREs and increased bone density. The contribution of DKK1 inhibition to these results is unclear.
Overall, DKK1 inhibition has been shown to positively affect osteoblastogenesis but the effects on osteoclastogenesis are currently unclear. The utility of DKK1 inhibition in MM at present may be limited as some myeloma patients do not show increased DKK1 levels, and DKK1 levels have been observed to decrease in later stages of the disease [57].
8.4.3.3 Activin Receptor Ligand Traps
Activin A is a cytokine that is upregulated in MM patients, especially in the setting of MBD. Activin A levels correlate with the severity of bone disease and disease stage [58]. Activin A inhibits bone mineralization by binding to the activin type 2A receptor, resulting in increased bone resorption and reduced bone formation [59]. Activin receptor ligand traps have been shown to increase markers of bone formation and decrease bone pain in MM patients [14].
A murine analog of sotatercept, a recombinant activin type 2A receptor ligand trap, has demonstrated dual anabolic and anti-bone resorptive effects in preclinical trials [60]. The safety and tolerability of sotatercept in combination with melphalan, prednisolone, and thalidomide have been evaluated in a phase IIA trial [60]. A total of 24 patients received sotatercept during the study, with three patients experiencing adverse events secondary to therapy. These three patients each experienced significant hypertension, which was resolved following antihypertensive therapy or interruption of sotatercept therapy. One patient had a grade five adverse event of sudden death following a second dose of sotatercept. The efficacy and safety of activin A receptor ligand traps for the treatment of MBD currently remains unclear. Further studies are required to the utility of this treatment in MBD.
8.4.3.4 Bruton’s Tyrosine Kinase (BTK) Inhibitors
BTK is expressed in many hematopoietic lineages and affects the development and function of B cells via B cell antigen receptor signaling pathways [16]. BTK inhibitors have proven efficacy in the setting of chronic lymphocytic leukemia. BTK is highly expressed in patients with MM and is involved in the promotion of osteoclastic bone resorption [61].
PCI-32765 (ibrutinib), a potent BTK inhibitor, has been shown to reduce osteoclast differentiation and bone resorption [19]. Ibrutinib has also resulted in a reduction of chemokine and cytokine secretion from osteoclasts.
Overall, BTK activation in MM facilitates osteoclast differentiation and osteoclastic bone resorption. BTK inhibitors such as ibrutinib appear to reduce this effect, and further investigations into this potential therapy for the management of MBD are warranted.
8.4.3.5 B Cell Activating Factor (BAFF) Neutralizing Antibodies
BAFF is a TNF superfamily member that promotes normal B cell development [62]. It is expressed by myeloma cells, osteoclasts, and bone marrow stromal cells, and is increased in MM patients and mediates survival of myeloma plasma cells in the bone marrow [16]. BAFF neutralizing antibodies have been tested in a mouse MM model [62]. Anti-BAFF treated animals showed decreased IL-6 receptor levels, suggesting anti-myeloma activity. Additionally, a survival advantage and reduction in radiologically evident lytic lesions were observed.
A phase I study examined tabalumab , a human MoAb against BAFF, in combination with the PI bortezomib in 48 patients [28]. Twenty of 46 evaluable patients achieved a partial response or better following the combination treatment, showing some promise for BAFF neutralizing antibodies.
Although early studies have so far promising results of BAFF neutralizing antibodies in both animals and humans, further studies are still required to fully assess the utility and impact of this therapy in MBD.
8.4.3.6 Transforming Growth Factor-β (TGF-β) Inhibitors
The TGF-β protein has been observed to result in increased tumor-induced bone disease, although the exact mechanism is unclear. Increased levels of TGF-β are released by osteoclasts in MBD [1]. The use of TGF-β inhibitor neutralizing antibody (1D11) in mice has been shown to improve the trabecular architecture and increase osteoblast differentiation in mouse MM models [63]. 1D11 in combination with bortezomib was shown to reduce tumor burden and bone disease, but 1D11 alone did not reduce tumor burden.
Thrombospondin 1 (TSP1) binds to and activates TGF-β. SRI31277, a TSP1 antagonist that acts by reducing TGF- β activation, has been tested in mice with MBD [64]. SRI31277 treatment resulted in a decrease in osteoclasts and an increase in osteoblastogenesis . It is unclear if these benefits would be seen in humans as only mice with highly osteolytic lesions and the human CAG-HPSE myeloma cell line were studied.
8.4.3.7 Parathyroid Hormone
Parathyroid hormone has been shown to be beneficial in osteoporotic bone disease via anabolic pathways at intermittent lower doses. The mechanism of action is thought to be due to the inhibition of sclerostin which normally promotes osteoclastogenesis, as well as direct activity on osteoblasts to promote osteoblastogenesis [65].
Treatment with teriparatide therapy has been linked to the development of MM in several case reports [66]. Additionally, it has been shown that high parathyroid hormone levels could facilitate the development of myeloma cells and have been correlated with a reduced progression free survival [67]. Conversely, a study of parathyroid hormone administration in murine MM models found an increase in bone mineral density via upregulation of osteoblasts [68].
Overall, there is minimal evidence to support the role for, and investigation of, parathyroid hormone therapy in the setting of MBD.
8.4.3.8 Proteasome Inhibitors
Bortezomib is a PI which impairs osteoclastogenesis and stimulates osteoblast differentiation, and hence actively modulating bone remodeling in MM [4]. Proteasome inhibitors produce an anabolic effect through the stimulation of osteoblast differentiation via the reduction of sclerostin levels, and the upregulation of BMP-2 and transcription factor RUNX2 via inhibition of proteasomal degradation [1].
It has been demonstrated that bortezomib therapy results in a reduction of sclerostin levels [58]. Patients with active MM and pathologic fractures at diagnosis possessed very high levels of sclerostin compared to other patient groups (relapsed myeloma, MGUS, and a control group). Higher sclerostin levels were associated with reduced survival with a median survival of 27 months for those with higher sclerostin levels versus 98 months for other patient groups [58]. Bortezomib monotherapy resulted in a significant reduction of sclerostin levels by almost 50%. Bortezomib has been shown to have anabolic activity leading to increased bone formation through promoting osteoblastogenesis and increasing bone mineral density.
Other PIs such as carfilzomib and ixazomib have also been shown to have bone anabolic effects similar to bortezomib [1]. Overall, PIs have been shown to improve MBD, disease control, and progression. They are a promising therapeutic in the setting of MBD.
8.4.3.9 Immunomodulatory Imide Drugs
Immunomodulatory imide drugs (IMiD) such as thalidomide, lenalidomide, and pomalidomide have a direct inhibitory effect on MM growth, as well as exerting an immunomodulatory effect and inhibiting angiogenesis [4]. Immunomodulatory imide drugs have been shown to reduce both osteoclastogenesis and growth factors associated with bone destruction [16]. Lenalidomide decreases RANKL secretion and increases OPG in MM patients, restoring the balance of RANKL and OPG and resulting in reduced osteoclast differentiation and activation. By decreasing RANKL secretion in MM patients, lenalidomide also causes OPG to increase, restoring the RANKL-OPG balance and resulting in reduced osteoclast formation and activation.
It has been demonstrated that thalidomide downregulates transcriptional factor PU.1 [69]. Lenalidomide and pomalidomide also both downregulate PU.1 expression in osteoclast precursors, causing a net reduction in osteoclast differentiation. Additionally, lenalidomide causes inhibition of the osteoclast-activating factors APRIL and BAFF [14].
Overall, it is clear that IMiDs have numerous effects on tumor growth, growth factors, and signaling proteins that result in a reduction in osteoclastogenesis . Further studies are warranted to further examine and understand the direct impacts of IMiDs on MBD.
8.5 Conclusion
Myeloma bone disease can result in significant associated morbidity and mortality. Effective therapies to combat the development and progression of MBD are crucial in maintaining quality of life, reducing cost, and improving overall survival. The current treatments available to combat MBD are limited to bisphosphonates and denosumab. Given the plethora of pathways and proteins involved in MBD, the potential targets for therapy are numerous. Further studies of novel agents, as well as studies of new combinations of existing and novel therapies, are needed to better manage MBD, reduce morbidity and mortality, and increase the quality of life and survival in patients with MM.
Abbreviations
- ASCO:
-
American Society of Clinical Oncology
- BAFF:
-
B cell activating factor
- bALP:
-
Bone-specific alkaline phosphatase
- BMSC:
-
Bone marrow stem cell
- BTK:
-
Bruton’s tyrosine kinase
- CCL:
-
Chemokine (C-C motif) ligand
- CCR:
-
Chemokine (C-C motif) receptor
- DKK1:
-
Dickkopf-1
- FDA:
-
US Food and Drug Administration
- HGF:
-
Hepatocyte growth factor
- IL:
-
Interleukin
- IMiD:
-
Immunomodulatory imide drug
- IMWG:
-
International Myeloma Working Group
- MBD:
-
Myeloma bone disease
- MGUS:
-
Monoclonal gammopathy of uncertain significance
- MIP-1α:
-
Macrophage-inhibitory protein 1 alpha
- MM:
-
Multiple myeloma
- NF-κB:
-
Nuclear factor kappa-B
- OAF:
-
Osteoclast-activating factor
- OPG:
-
Osteoprotegerin
- OS:
-
Overall survival
- PI:
-
Proteasome inhibitor
- RANK:
-
Receptor activator of nuclear factor kappa-B
- sFRP3:
-
Soluble frizzled-related protein 3
- SRE:
-
Skeletal related event
- TGF-β:
-
Transforming growth factor-beta
- TNF:
-
Tumor necrosis factor
- TNF-α:
-
Tumor necrosis factor-alpha
- TSP1:
-
Thrombospondin 1
- uNTX:
-
Urinary N-telopeptide of collagen type 1
- VEGF:
-
Vascular endothelial growth factor
- β-CTX:
-
Beta-isomerized C-terminal telopeptide of collagen type 1
References
Ring ES, Lawson MA, Snowden JA, Jolley I, Chantry AD. New agents in the treatment of myeloma Bone disease. Calcif Tissue Int. 2018;102(2):196–209.
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21–33.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–48.
Raje N, Roodman GD. Advances in the biology and treatment of bone disease in multiple myeloma. Clin Cancer Res. 2011;17(6):1278–86.
Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110(8):1860–7.
Lee OL, Horvath N, Lee C, Joshua D, Ho J, Szer J, et al. Bisphosphonate guidelines for treatment and prevention of myeloma bone disease. Intern Med J. 2017;47(8):938–51.
Edelstyn GA, Gillespie PJ, Grebbell FS. The radiological demonstration of osseous metastases. Experimental observations. Clin Radiol. 1967;18(2):158–62.
Bird JM, Owen RG, D’Sa S, Snowden JA, Pratt G, Ashcroft J, et al. Guidelines for the diagnosis and management of multiple myeloma 2011. Br J Haematol. 2011;154(1):32–75.
Bataille R, Chappard D, Marcelli C, Dessauw P, Sany J, Baldet P, et al. Mechanisms of bone destruction in multiple myeloma: the importance of an unbalanced process in determining the severity of lytic bone disease. J Clin Oncol. 1989;7(12):1909–14.
Hanley DA, Adachi JD, Bell A, Brown V. Denosumab: mechanism of action and clinical outcomes. Int J Clin Pract. 2012;66(12):1139–46.
Terpos E, Ntanasis-Stathopoulos I, Gavriatopoulou M, Dimopoulos MA. Pathogenesis of bone disease in multiple myeloma: from bench to bedside. Blood Cancer J. 2018;8(1):7.
Hameed A, Brady JJ, Dowling P, Clynes M, O’Gorman P. Bone disease in multiple myeloma: pathophysiology and management. Cancer Growth Metastasis. 2014;7:33–42.
Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med. 2011;17(10):1231–4.
Walker RE, Lawson MA, Buckle CH, Snowden JA, Chantry AD. Myeloma bone disease: pathogenesis, current treatments and future targets. Br Med Bull. 2014;111(1):117–38.
Stewart JP, Shaughnessy JD Jr. Role of osteoblast suppression in multiple myeloma. J Cell Biochem. 2006;98(1):1–13.
Webb SL, Edwards CM. Novel therapeutic targets in myeloma bone disease. Br J Pharmacol. 2014;171(16):3765–76.
Lee JW, Chung HY, Ehrlich LA, Jelinek DF, Callander NS, Roodman GD, et al. IL-3 expression by myeloma cells increases both osteoclast formation and growth of myeloma cells. Blood. 2004;103(6):2308–15.
Noonan K, Marchionni L, Anderson J, Pardoll D, Roodman GD, Borrello I. A novel role of IL-17-producing lymphocytes in mediating lytic bone disease in multiple myeloma. Blood. 2010;116(18):3554–63.
Tai YT, Chang BY, Kong SY, Fulciniti M, Yang G, Calle Y, et al. Bruton tyrosine kinase inhibition is a novel therapeutic strategy targeting tumor in the bone marrow microenvironment in multiple myeloma. Blood. 2012;120(9):1877–87.
Qiang YW, Shaughnessy JD Jr, Yaccoby S. Wnt3a signaling within bone inhibits multiple myeloma bone disease and tumor growth. Blood. 2008;112(2):374–82.
Kobune M, Chiba H, Kato J, Kato K, Nakamura K, Kawano Y, et al. Wnt3/RhoA/ROCK signaling pathway is involved in adhesion-mediated drug resistance of multiple myeloma in an autocrine mechanism. Mol Cancer Ther. 2007;6(6):1774–84.
Colucci S, Brunetti G, Oranger A, Mori G, Sardone F, Specchia G, et al. Myeloma cells suppress osteoblasts through sclerostin secretion. Blood Cancer J. 2011;1(6):e27.
Terpos E, Morgan G, Dimopoulos MA, Drake MT, Lentzsch S, Raje N, et al. International myeloma working group recommendations for the treatment of multiple myeloma-related bone disease. J Clin Oncol. 2013;31(18):2347–57.
Kaiser M, Mieth M, Liebisch P, Oberlander R, Rademacher J, Jakob C, et al. Serum concentrations of DKK-1 correlate with the extent of bone disease in patients with multiple myeloma. Eur J Haematol. 2008;80(6):490–4.
Terpos E, Christoulas D, Kastritis E, Bagratuni T, Gavriatopoulou M, Roussou M, et al. High levels of periostin correlate with increased fracture rate, diffuse MRI pattern, abnormal bone remodeling and advanced disease stage in patients with newly diagnosed symptomatic multiple myeloma. Blood Cancer J. 2016;6(10):e482.
Auzina D, Erts R, Lejniece S. Prognostic value of the bone turnover markers in multiple myeloma. Exp Oncol. 2017;39(1):53–6.
Pochintesta L, Mangiacavalli S, Cocito F, Pompa A, Albertini R, Pascutto C, et al. Serum C terminal telopeptide maintains its correlation with bone disease in patients with myeloma even under treatment with bisphosphonates. Leuk Lymphoma. 2014;55(6):1397–8.
Raje N, Vescio R, Montgomery CW, Badros A, Munshi N, Orlowski R, et al. Bone marker-directed dosing of zoledronic acid for the prevention of skeletal complications in patients with multiple myeloma: results of the Z-MARK study. Clin Cancer Res. 2016;22(6):1378–84.
Dunford JE, Thompson K, Coxon FP, Luckman SP, Hahn FM, Poulter CD, et al. Structure-activity relationships for inhibition of farnesyl diphosphate synthase in vitro and inhibition of bone resorption in vivo by nitrogen-containing bisphosphonates. J Pharmacol Exp Ther. 2001;296(2):235–42.
Berenson JR, Lichtenstein A, Porter L, Dimopoulos MA, Bordoni R, George S, et al. Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. Myeloma Aredia study group. N Engl J Med. 1996;334(8):488–93.
McCloskey EV, Dunn JA, Kanis JA, MacLennan IC, Drayson MT. Long-term follow-up of a prospective, double-blind, placebo-controlled randomized trial of clodronate in multiple myeloma. Br J Haematol. 2001;113(4):1035–43.
Morgan GJ, Davies FE, Gregory WM, Bell SE, Szubert AJ, Cook G, et al. Long-term follow-up of MRC myeloma IX trial: survival outcomes with bisphosphonate and thalidomide treatment. Clin Cancer Res. 2013;19(21):6030–8.
Sanfilippo KM, Gage B, Luo S, Weilbaecher K, Tomasson M, Vij R, et al. Comparative effectiveness on survival of zoledronic acid versus pamidronate in multiple myeloma. Leuk Lymphoma. 2015;56(3):615–21.
Rosen LS, Gordon D, Kaminski M, Howell A, Belch A, Mackey J, et al. Long-term efficacy and safety of zoledronic acid compared with pamidronate disodium in the treatment of skeletal complications in patients with advanced multiple myeloma or breast carcinoma: a randomized, double-blind, multicenter, comparative trial. Cancer. 2003;98(8):1735–44.
Fraunfelder FW, Fraunfelder FT. Bisphosphonates and ocular inflammation. N Engl J Med. 2003;348(12):1187–8.
Berenson JR, Yellin O, Crowley J, Makary A, Gravenor DS, Yang HH, et al. Prognostic factors and jaw and renal complications among multiple myeloma patients treated with zoledronic acid. Am J Hematol. 2011;86(1):25–30.
Santini D, Vincenzi B, Dicuonzo G, Avvisati G, Massacesi C, Battistoni F, et al. Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res. 2003;9(8):2893–7.
Badros A, Weikel D, Salama A, Goloubeva O, Schneider A, Rapoport A, et al. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol. 2006;24(6):945–52.
Mehrotra B, Ruggiero S. Bisphosphonate complications including osteonecrosis of the jaw. Hematology Am Soc Hematol Educ Program. 2006;356–60:515.
Katz J, Gong Y, Salmasinia D, Hou W, Burkley B, Ferreira P, et al. Genetic polymorphisms and other risk factors associated with bisphosphonate induced osteonecrosis of the jaw. Int J Oral Maxillofac Surg. 2011;40(6):605–11.
Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Min Res. 2010;25(11):2267–94.
Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, et al. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int. 2010;21(3):399–408.
Anderson K, Ismaila N, Flynn PJ, Halabi S, Jagannath S, Ogaily MS, et al. Role of bone-modifying agents in multiple myeloma: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2018;36(8):812–8.
Pozzi S, Raje N. The role of bisphosphonates in multiple myeloma: mechanisms, side effects, and the future. Oncologist. 2011;16(5):651–62.
Raje N, Terpos E, Willenbacher W, Shimizu K, Garcia-Sanz R, Durie B, et al. Denosumab versus zoledronic acid in bone disease treatment of newly diagnosed multiple myeloma: an international, double-blind, double-dummy, randomised, controlled, phase 3 study. Lancet Oncol. 2018;19(3):370–81.
Block GA, Bone HG, Fang L, Lee E, Padhi D. A single-dose study of denosumab in patients with various degrees of renal impairment. J Bone Min Res. 2012;27(7):1471–9.
Reagan MR, McDonald M, Terry R, Pettitt J, Le L, Mohanty S, et al. Anti-sclerostin treatment prevents multiple myeloma induced bone loss and reduces tumor burden. ASH Publication Blood. 2015;126(23):119.
Eda H, Santo L, Wein MN, Hu DZ, Cirstea DD, Nemani N, et al. Regulation of sclerostin expression in multiple myeloma by Dkk-1: a potential therapeutic strategy for myeloma bone disease. J Bone Min Res. 2016;31(6):1225–34.
Falank C, Fairfield H, Reagan MR. Signaling interplay between bone marrow adipose tissue and multiple myeloma cells. Front Endocrinol (Lausanne). 2016;7:67.
McClung MR, Grauer A, Boonen S, Bolognese MA, Brown JP, Diez-Perez A, et al. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014;370(5):412–20.
Pozzi S, Fulciniti M, Yan H, Vallet S, Eda H, Patel K, et al. In vivo and in vitro effects of a novel anti-Dkk1 neutralizing antibody in multiple myeloma. Bone. 2013;53(2):487–96.
Gunn WG, Conley A, Deininger L, Olson SD, Prockop DJ, Gregory CA. A crosstalk between myeloma cells and marrow stromal cells stimulates production of DKK1 and interleukin-6: a potential role in the development of lytic bone disease and tumor progression in multiple myeloma. Stem Cells. 2006;24(4):986–91.
Qiang YW, Chen Y, Stephens O, Brown N, Chen B, Epstein J, et al. Myeloma-derived Dickkopf-1 disrupts Wnt-regulated osteoprotegerin and RANKL production by osteoblasts: a potential mechanism underlying osteolytic bone lesions in multiple myeloma. Blood. 2008;112(1):196–207.
Heusschen R, Muller J, Duray E, Withofs N, Bolomsky A, Baron F, et al. Molecular mechanisms, current management and next generation therapy in myeloma bone disease. Leuk Lymphoma. 2018;59(1):14–28.
Fulciniti M, Tassone P, Hideshima T, Vallet S, Nanjappa P, Ettenberg SA, et al. Anti-DKK1 mAb (BHQ880) as a potential therapeutic agent for multiple myeloma. Blood. 2009;114(2):371–9.
Iyer SP, Beck JT, Stewart AK, Shah J, Kelly KR, Isaacs R, et al. A phase IB multicentre dose-determination study of BHQ880 in combination with anti-myeloma therapy and zoledronic acid in patients with relapsed or refractory multiple myeloma and prior skeletal-related events. Br J Haematol. 2014;167(3):366–75.
Tian E, Zhan F, Walker R, Rasmussen E, Ma Y, Barlogie B, et al. The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med. 2003;349(26):2483–94.
Terpos E, Kastritis E, Christoulas D, Gkotzamanidou M, Eleutherakis-Papaiakovou E, Kanellias N, et al. Circulating activin-A is elevated in patients with advanced multiple myeloma and correlates with extensive bone involvement and inferior survival; no alterations post-lenalidomide and dexamethasone therapy. Ann Oncol. 2012;23(10):2681–6.
Roodman GD. Osteoblast function in myeloma. Bone. 2011;48(1):135–40.
Abdulkadyrov KM, Salogub GN, Khuazheva NK, Sherman ML, Laadem A, Barger R, et al. Sotatercept in patients with osteolytic lesions of multiple myeloma. Br J Haematol. 2014;165(6):814–23.
Lee SH, Kim T, Jeong D, Kim N, Choi Y. The tec family tyrosine kinase Btk regulates RANKL-induced osteoclast maturation. J Biol Chem. 2008;283(17):11526–34.
Neri P, Kumar S, Fulciniti MT, Vallet S, Chhetri S, Mukherjee S, et al. Neutralizing B-cell activating factor antibody improves survival and inhibits osteoclastogenesis in a severe combined immunodeficient human multiple myeloma model. Clin Cancer Res. 2007;13(19):5903–9.
Nyman JS, Merkel AR, Uppuganti S, Nayak B, Rowland B, Makowski AJ, et al. Combined treatment with a transforming growth factor beta inhibitor (1D11) and bortezomib improves bone architecture in a mouse model of myeloma-induced bone disease. Bone. 2016;91:81–91.
Lu A, Pallero MA, Lei W, Hong H, Yang Y, Suto MJ, et al. Inhibition of transforming growth factor-beta activation diminishes tumor progression and osteolytic bone disease in mouse models of multiple myeloma. Am J Pathol. 2016;186(3):678–90.
Lombardi G, Di Somma C, Rubino M, Faggiano A, Vuolo L, Guerra E, et al. The roles of parathyroid hormone in bone remodeling: prospects for novel therapeutics. J Endocrinol Invest. 2011;34(7 Suppl):18–22.
Koski AM, Sikio A, Forslund T. Teriparatide treatment complicated by malignant myeloma. BMJ Case Rep. 2010;2010
Kang MG, Won EJ, Choi HW, Kim HR, Choi HJ, Park HR, et al. Serum parathyroid hormone is a new potential risk factor in multiple myeloma. Biomed Res Int. 2014;2014:804182.
Pennisi A, Ling W, Li X, Khan S, Wang Y, Barlogie B, et al. Consequences of daily administered parathyroid hormone on myeloma growth, bone disease, and molecular profiling of whole myelomatous bone. PLoS One. 2010;5(12):e15233.
Anderson G, Gries M, Kurihara N, Honjo T, Anderson J, Donnenberg V, et al. Thalidomide derivative CC-4047 inhibits osteoclast formation by down-regulation of PU.1. Blood. 2006;107(8):3098–105.
Acknowledgment
Many thanks to the reviewers of this manuscript and my coeditor Steven Trieu. This work was supported by NSW Pathology and the SWSLHD mid-career grant.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
McEwan, A., Ling, S.C. (2021). Bone Targeted Therapies. In: Ling, S.C., Trieu, S. (eds) Resistance to Targeted Therapies in Multiple Myeloma. Resistance to Targeted Anti-Cancer Therapeutics, vol 22. Springer, Cham. https://doi.org/10.1007/978-3-030-73440-4_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-73440-4_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73439-8
Online ISBN: 978-3-030-73440-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)