Abstract
Bone involvement represented by osteolytic bone disease (OBD) or osteopenia is one of the pathognomonic and defining characteristics of multiple myeloma (MM). Nearly 90 % of patients with MM develop osteolytic bone lesions, frequently complicated by skeletal-related events (SRE) such as severe bone pain, pathological fractures, vertebral collapse, hypercalcemia, and spinal cord compression. All of these not only result in a negative impact on quality of life but also adversely impact overall survival. OBD is a consequence of increased osteoclast (OC) activation along with osteoblast (OB) inhibition, resulting in altered bone remodeling. OC number and activity are increased in MM via cytokine deregulation within the bone marrow (BM) milieu, whereas negative regulators of OB differentiation suppress bone formation. Inhibition of osteolysis and stimulation of OB differentiation leads to reduced tumor growth in vivo. Therefore, novel agents targeting OBD are promising therapeutic strategies not only for the treatment of MM OBD but also for the treatment of MM. Several novel agents in addition to bisphosphonates are currently under investigation for their positive effect on bone remodeling via OC inhibition or OB stimulation. Future studies will look to combine or sequence all of these agents with the goal of not only alleviating morbidity from MM OBD but also capitalizing on the resultant antitumor activity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The past two decades have seen remarkable advances in our understanding of the biology of multiple myeloma (MM) and in the introduction of novel therapies. Novel treatments including thalidomide [1], lenalidomide [2], and the proteasome inhibitor bortezomib [3] have led to significant improvements in 5-year relative overall survival, from nearly 28.8 % in the early 1990s to 34.7 % in the previous decade [4]. Although MM remains incurable, MM patients are living longer, and the focus is centered on maximizing quality of life for patients with MM.
Bone involvement represented by osteolytic bone disease (OBD) or osteopenia is one of the pathognomonic and defining characteristic of MM [5]. Although the ratio of patients presenting with bone involvement is variable, nearly 90 % of patients with MM develop osteolytic bone lesions, frequently complicated by skeletal-related events (SRE) such as severe bone pain, pathological fractures, vertebral collapse, hypercalcemia, and spinal cord compression, resulting in a need for radiation or open reduction internal fixation (ORIF) [6–10]. Importantly, 40–50 % of MM patients develop pathologic fractures, and it increases the risk of death by more than 20 % compared with patients without fractures [8, 11]. These data indicate how OBD negatively impact both patients’ quality of life and survival, and highlight the importance of focusing on treatment strategies to alleviate OBD in MM.
OBD results from the disruption of the delicate balance between osteoclasts (OCs), osteocytes, osteoblasts (OBs), and bone marrow stromal cells (BMSCs) activity. MM cells stimulate OC function and inhibit OB differentiation, resulting in bone resorption and consequent OBD. The abnormal bone marrow (BM) microenvironment in OBD provides a permissive niche that enables MM cell growth [9, 12–14]. Consequently, several novel agents and combinations are aimed at restoring bone homeostasis by targeting either OC or/and OB activity. In fact, inhibition of osteolysis and stimulation of OB differentiation leads to reduced tumor growth in vivo [13, 15]. Therefore, novel agents targeting OBD are also promising therapeutic strategies for the treatment of MM. Here, we discuss the pathogenesis of OBD and focus on advances in our understanding of its biology and therapeutic implications.
2 The Biology of Bone Metabolism
Under normal physiologic states, osteocytes, OCs and OBs result in balanced bone resorption and formation maintaining normal homeostasis. In adult bone, 90–95 % of all bone cells are represented by osteocytes while OCs and OBs are less than 10 % [16]. Osteocytes act as main regulators of bone homeostasis for OCs, considered bone resorption cells, and OBs considered bone formation cells. Osteocyte viability and function is regulated by mechanical loading, several cytokines includes well as glucocorticoids [16–18]. Osteocytes secrete several cytokines which regulate the activity of both OCs and OBs such as sclerostin, dickkopf-1 (Dkk-1), the receptor activator of nuclear factor-kappa B ligand (RANKL), and osteoprotegerin (OPG) [16]. The receptor activator of nuclear factor-kappa B (RANK), its ligand RANKL, and OPG, the decoy receptor of RANKL, play a pivotal role as central regulators of OC function. RANK-RANKL signaling activates a variety of downstream signaling pathways required for OC development. It plays a significant role in stimulating OC differentiation and maturation. Interestingly, apoptotic osteocytes release apoptotic bodies expressing RANKL to stimulate OC differentiation [19]. These data suggest that osteocytes are able to recruit OCs to sites of remodeling. Osteocytes also regulate OB differentiation via sclerostin and Dkk-1 which block canonical Wnt signaling by binding to low-density lipoprotein receptor-related protein (LRP) 5 and 6 (Wnt receptors) on the surface of OBs [16]. OBs and BMSCs also express OPG and RANKL, and regulate OC differentiation. Because OPG is a Wnt canonical signaling target [20], osteocyte also regulates OC differentiation via regulation of Wnt signaling activity in OBs. On the other hand, OCs express semaphorin 4D (Sema4D) and inhibit OB differentiation [21]. These processes are well balanced in healthy bones to maintain the bones quality and mass (Fig. 1).
3 MM Bone Disease
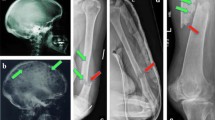
In MM, the osteocyte-OC-OB axis is disrupted, stimulating bone resorption and inhibiting new bone formation with resultant development of pathognomonic osteolytic lesions (Fig. 2).
Myeloma Bone Disease. MM cells produce IL-3, DcR3, CCL3, MIP-1β, VEGF, TNFα, and RANKL. MM cells also adhere to BMSCs via VLA-4 and VCAM-1 interaction, and lead to the secretion of RANKL, SDF-1a, IL-6, BAFF, VEGF, and activin A. Moreover, MM cells stimulate CCL3 and IL-11 expression in osteocytes. OCs secrete CCL3 and activin A by MM cells stimulation. These cytokines stimulate OC differentiation and activity. MM cells also inhibit OPG expression in BMSCs and OBs resulting in stimulation of OC differentiation. On the other hand, MM cells produce IL-3, IL-7, TNFα, TGFβ, and Dkk-1. MM cells also stimulate activin A expression in BMSCs. These cytokines inhibit OB differentiation. Stimulated OCs destroy bone matrix, and release several tumor growth factor from bone. Moreover, OCs and BMSCs express several cytokines. These cytokines mediate MM cell survival and proliferation
3.1 Osteoclasts in Myeloma Bone Disease
The pathogenesis of OBD in MM is primarily associated with generalized OC activation. BM biopsies from MM patients show a correlation between tumor burden, OC numbers, and resorptive surface [22, 23]. Furthermore, OC activity has positive correlation with disease activity [24, 25]. The main cytokines involved in OC differentiation and activity in MM OBD are RANKL/OPG, decoy receptor 3 (DcR3), CCL3 (also known as macrophage inflammatory protein (MIP)-1α), MIP-1β, tumour necrosis factor-alpha (TNFα), interleukin (IL)-3, IL-6, IL-11, Stromal derived factor-1 alpha (SDF-1a), B-cell activating factor (BAFF), activin A, and VEGF.
MM cells stimulate OC differentiation by producing IL-3 [26], DcR3 [27, 28], CCL3, MIP-1β [29–31], VEGF [32], TNFα, [33, 34] and RANKL [35–38]. MM cells also adhere to BMSCs via very late antigen (VLA)-4 and vascular cell adhesion molecule (VCAM)-1 interaction leading to the secretion of cytokines including RANKL, SDF-1a, IL-6, BAFF, VEGF, and activin A which in turn positively affect OC differentiation and activation [9, 14, 32, 39–43]. MM cells stimulate not only RANKL expression, but also inhibit OPG expression, leading to an increase in RANKL/OPG ratio in BMSCs and OBs which in turn strongly stimulate OC differentiation [24, 44]. In addition to BMSCs and OBs, MM cells also stimulate CCL3 and pro-osteoclastogenic cytokine, IL-11 in osteocytes [45]. Moreover, OCs secrete CCL3 and activin A, and stimulate OC differentiation and activation by themselves [9, 31]. BM macrophages stimulated by IL-3 also secrete activin A [46]. All these cytokines stimulate OC differentiation and activity, and contribute to the development of MM OBD.
3.1.1 CCL3
CCL3 is a pro-inflammatory cytokine belonging to the CC chemokine subfamily. High CCL3 levels were found in MM patients’ BM serum and it correlates with OBD and survival [30]. Interestingly, fibroblast growth factor receptor 3 (FGFR3) overexpression in MM with t(4,14) results in upregulation of CCL3 expression [47]. CCL3 modulates OC differentiation by binding to G-protein coupled receptors, CCR1 and CCR5, and activating ERK and AKT signaling pathways. CCL3 has the ability to stimulate OC differentiation not only from monocytes but also from immature dendritic cells by transdifferentiation [48]. In the tumor niche, MM cells and OCs are the main source for CCL3 that promotes MM cell migration and survival, along with stimulation of osteoclastogenesis [49, 50]. Vallet et al. also showed that CCL3 reduces bone formation by inhibiting OB function by ERK activation and followed by down regulation of the osteogenic transcription factor, osterix [31]. Importantly, a small molecule CCR1 antagonist inhibits CCL3-induced osteoclastogenesis and OC support of MM cells [51].
3.1.2 RANKL to OPG Ratio
Many of the cytokines which stimulate OC differentiation and activity act through RANKL and OPG. Increase of the RANKL to OPG ratio results in bone loss in several cancers and inflammatory diseases including rheumatoid arthritis [52–54]. In MM patients, BM plasma levels of RANKL are increased, whereas OPG expression is decreased compared with normal volunteers and patients with MGUS [35]. Importantly, low levels of OPG in serum correlate with advanced OBD in MM [55]. The relevance of the RANKL/OPG pathway in mediating OC differentiation and activation in MM has been further confirmed in several murine models of MM OBD. Treatment with OPG or OPG-like molecules prevented both bone destruction and MM growth in vivo [36, 56]. Interestingly, specific anti-MM strategies such as thalidomide and autologous BM transplantation improved OBD by normalizing the RANKL to OPG ratio [57, 58]. Therefore, the RANKL-OPG axis is one of the important targets in the development of novel therapeutic strategies for MM bone disease.
3.2 Bone Marrow Stromal Cells and Osteoblasts in Myeloma Bone Disease
Besides OCs, BMSCs and OBs derived from BMSCs, play an important role in the development of OBD in the presence of MM cells. MM cells stimulate OC differentiation directly by secreting OC-activating factors (OAFs) and, indirectly, by stimulating OAFs secretion such as RANKL, Activin A and VEGF in BMSCs and OBs [14, 35, 36, 59, 60]. Adhesion of MM to BMSCs leads to RANKL and VEGF secretion by BMSCs via p38 MAPK activation [59, 60]. Moreover, the sequestosome 1, p62 is an upstream regulator of p38 MAPK and NF-κB signaling pathway, activated in BMSCs by MM cell adhesion. Inhibition of p62 in BMSCs represses OC differentiation and MM cell proliferation [61]. These data suggest that p62 is a novel promising target in MM OBD. Adhesion of MM to BMSCs and immature OBs also leads to IL-6 secretion via NF-κB signaling [42, 43, 62] and X-box-binding protein 1 (XBP1) signaling [63] pathway. IL-6 stimulates MM cell proliferation and inhibition of MM plasma cell apoptosis [64] in addition to OC differentiation. Moreover, adhesion of MM cells also stimulates BAFF expression in BMSCs via NF-κB signaling [41]. BAFF is a MM cell survival factor and it rescues MM cells from apoptosis induced by IL-6 deprivation and dexamethasone via activation of NF-κB, phosphatidylinosiol-3 (PI-3) kinase/AKT, and MAPK pathways in MM cells and induction of a strong upregulation of Mcl-1 and Bcl-2 antiapoptotic proteins [65, 66]. Secreted IL-6 and BAFF also stimulates the serine/threonine kinase Pim-2 expression in MM cells via activation of NF-κB and JAK2/STAT3 pathway, resulting in MM cell survival [67]. Furthermore, MM cells stimulate activin A expression in BMSCs via Jun N-terminal kinase-dependent (JNK) activation [9]. Importantly, high activin A levels in MM patients are associated with advanced bone disease and advanced features of MM [68]. Secreted Activin A inhibits OB differentiation in addition to the growth stimulatory effects on OCs. MM cells also stimulate Pim-2 expression in BMSCs/OBs by IL-3, IL-7, TNF-a, TGF-β and activin A secretion, and inhibit OB differentiation [69].
3.2.1 Wnt Canonical Signaling in BMSCs and OBs
Wnt canonical signaling plays an important role in OB differentiation. Some Wnt proteins bind to both Frizzled and LRP 5 and 6, and activate Wnt canonical signaling. Activated Wnt signaling induces nuclear translocation of β-catenin protein resulting in stimulation of OB differentiation by activation of major OB transcription factors [70]. Wnt antagonists, such as Dkk-1, sclerostin and secreted frizzled related proteins (sFRPs) inhibit Wnt canonical signaling activity by blocking Wnt proteins binding to Wnt receptors. Thus, these Wnt antagonists act as negative regulators for OB differentiation. In MM OBD, OB differentiation is strongly inhibited. MM cells secrete several Wnt antagonists such as Dkk-1 [71], sFRP-2 [72], sFRP-3 [73] and inhibit Wnt canonical signaling. High Dkk-1 levels have been detected in MM patients’ serum and have been correlated with MM bone lesions [71]. Also high circulating levels of sclerostin, encoded by the SOST gene, have been found in newly diagnosed MM patients, and correlates with MM disease stage and fractures [74]. There is a report that MM cells produce sclerostin [75], however, we and others [76] could detect very little sclerostin or SOST mRNA expression in MM cell lines. The source and role of sclerostin in MM OBD therefore remains to be defined. Importantly, Wnt antagonists inhibit OPG expression as OPG is a target of Wnt canonical signaling [20], and increase the RANKL to OPG ratio. They are responsible not only for suppression of OB differentiation and activity but also for stimulation of OC differentiation and activity in MM OBD.
3.3 Osteocytes in Myeloma Bone Disease
Osteocytes act as main regulators of bone homeostasis in healthy bone [16]. A recent study showed that MM patients have a significantly lower number of viable osteocytes than healthy controls, and that osteocyte death correlates with the presence of bone lesions [45]. Besides a lower number of viable osteocytes has been observed in the MM patients, no significant difference in the expression of sclerostin, an osteocyte marker, in biopsies of MM patients bone and healthy controls osteocyte was observed [45]. On the other hand, higher circulating levels of sclerostin have been found in newly diagnosed MM patients as mentioned before [74]. These data suggest that there might be other alternate sources of sclerostin in addition to osteocytes in MM. Moreover, MM cells stimulate osteoclastogenic cytokines, CCL3 and IL-11 expression in pre-osteocytes leading to increased OC differentiation [45]. Further investigations regarding the role of osteocytes in MM OBD are underway.
4 Treatment of Myeloma—Related Osteolytic Bone Disease
Current treatment strategies in MM have led to significant improvements in 5-year relative overall survival, but patients continue to relapse, and no definitive cure has been as yet achieved. Given the improved survival of MM patients, treatment of OBD has taken on a new relevance as the focus is now largely on quality of life. Until recently, therapeutic options for MMOBD-included bisphosphonates, radiotherapy, and surgery. These therapies are aimed at reducing the development of new osteolytic lesions and preventing SREs such as bone pain, pathological fractures, vertebral collapse, hypercalcemia, and spinal cord compression. Interestingly, several studies using novel bone-targeted agents suggest that restoring bone homeostasis may lead to tumor growth inhibition. These promising preclinical results have set the stage for clinical evaluation of novel strategies targeting MM via restoring bone homeostasis. Table 1 provides a list of bone-directed agents, their roles, targets, and stage of clinical development.
4.1 Bisphosphonates
Bisphosphonates represent the standard of care for MM OBD. Nitrogen-containing bisphosphonates such as pamidronate (PAM) or zoledronic acid (ZA), more potent than PAM, reduce osteoclast activity through inhibiting farnesyl pyrophosphate synthase (FPPS) [77]. Bisphosphonates prevent OB and osteocyte apoptosis with a different mechanism from the effect on OCs [78–80]. Bisphosphonates induce ERK activation without nuclear accumulation in OBs and osteocytes. Activated ERK stimulates p90RSK and induces phosphorylation of the cytoplasmic substrates, BAD and C/EBP, which are required for OB and osteocyte survival [81].
Bisphosphonates have a well-established role in the treatment of osteoporosis [82, 83] and metastatic bone involvement from solid tumors [84–86]. In MM, treatment with bisphosphonate significantly reduces pain related to OBD and prevents SREs. Monthly infusion of PAM reduces bone pain and SREs compared with placebo [87]. PAM also significantly improved quality of life, with decreases in pain scores seen within a month. Moreover, Major et al. reported that ZA was superior to PAM for the treatment of hypercalcemia of malignancy including MM [88] although Rosen et al. reported the efficacy of ZA in preventing SREs in MM was comparable to that of PAM [84].
In addition to their role in OBD, bisphosphonates may also have an antitumor effect. The Austrian Breast and Colorectal Cancer Study Group 12 (ABCSG-12) trial showed that the administration of zoledronic acid every 6 months for 3 years reduced the risk of disease recurrence in estrogen-receptor—positive breast cancer patients [89] although no improvement was seen in the rate of disease-free survival in another study [90]. In MM, The MRC Myeloma IX trial compared ZA and oral clodronate in newly diagnosed patients and found that ZA reduced mortality by 16 % and increased median overall survival from 44.5 to 50.0 months (P = 0.04) [91]
4.1.1 Osteonecrosis of the Jaw
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is one of the most serious complications of bisphosphonates [92, 93]. BRONJ is traditionally defined as exposed, necrotic bone in the jaw that does not heal after 8 weeks and is generally painful. Histologically, several tissue alterations such as honeycombed-like necrotic bone with residual vital bone, inflammatory cellular elements, and hypernucleated osteoclasts are observed in BRONJ [94–96]. ZA is associated with the highest risk of BRONJ, attributed to its increased potency, and earlier studies suggested an incidence of 4–11 %, correlating with duration of exposure [97, 98]. In the MRC Myeloma IX trial, the cumulative incidence of BRONJ was 3–4 % at a median follow-up of 3.7 years [99]. It is clear that trauma, infection, and reduced vascularity including dental extractions play important roles, however, the exact etiopathogenetic mechanism of BRONJ still remains unclear. Further studies are necessary to evaluate the detailed mechanism of BRONJ development.
4.2 Denosumab
Denosumab is an OC inhibitor that plays a role in the supportive care of MM OBD. It is a monoclonal antibody, given subcutaneously, that inhibits OC activity through targeting RANKL. Denosumab is approved for increasing bone density in patients with osteoporosis and for preventing SREs in patients with metastatic bone disease [100]. It has been recently reported that denosumab causes osteosclerosis [101], and hypercalcemia has been observed following discontinuation of denosumab [102] in children. In MM, although a favorable trend was observed, denosumab was equivalent to ZA in delaying time to first on-study SRE [103]. Denosumab is not currently FDA approved for use in patients with MM; a larger, ongoing phase III study (ClinicalTrials.gov identifier: NCT01345019) is comparing it with ZA in this disease setting.
4.3 OPG Agonists
OPG is a decoy receptor for RANKL, and it blocks OC differentiation and activation. In MM patients, BM plasma levels of OPG is decreased compared with normal volunteers and patients with MGUS [35]. Importantly, low levels of OPG in serum correlate with advanced OBD in MM [55]. Treatment with OPG or OPG-like molecules prevented both bone destruction and MM growth in vivo [36, 56]. A Phase I study of a recombinant OPG construct (AMGN-0007) was conducted in MM patients with OBD, and decreased NTX/creatinine levels was observed [104].
4.4 CCR1 Inhibitors
The CCL3/CCR1 pathway stimulates OC differentiation, MM cell survival and migration, and inhibits OB differentiation suggesting that CCL3/CCR1 is a relevant target in MM OBD. Both antisense sequence and neutralizing antibody against CCL3 effectively inhibited tumor growth and restored bone remodeling in a mouse model of MM OBD [15, 105]. Similar results have been shown with a clinical grade small molecule CCR1 antagonist, MLN3897 (Millennium Pharmaceuticals) [51]. In addition to these molecules, several CCR1 antagonists were evaluated for MM OBD [106, 107]. Future clinical trials using CCR1 inhibition strategies in patients with MM OBD will help to confirm these promising preclinical results.
4.5 Anti-BAFF—Neutralizing Antibody
In MM, BAFF is expressed by monocytes, macrophages, dendritic cells, T cells, neutrophils, MM cells, and OCs [65, 108–111]. BAFF is a MM cell survival factor and rescues MM cells from apoptosis induced by IL-6 deprivation and dexamethasone via activation of NF-kB, PI-3 kinase/AKT, and MAPK kinase pathways and induction of a strong upregulation of the Mcl-1 and Bcl-2 antiapoptotic proteins [65]. In vivo—neutralizing antibodies against BAFF (LY2127399, Eli Lilly) significantly inhibit tumor burden and, importantly, reduce OBD and OC differentiation in preclinical setting [66]. On the basis of these results, a clinical trial combining BAFF-neutralizing antibody with proteasome inhibitor, bortezomib is currently ongoing, preliminary results from Raje et al. reported the treatment was well tolerated and 22 of the 48 patients enrolled achieved a partial remission or better (https://ash.confex.com/ash/2012/webprogram/Paper52052.html).
4.6 Activin A Antagonists
Activin A is secreted by BMSCs and OCs in MM OBD. Activin A stimulates OC differentiation and inhibits OB formation in MM OBD. Activin A can be targeted by a chimeric antibody RAP-011 (Acceleron Pharma), derived from the fusion of the extracellular domain of type II activin receptor (ActRIIA) and the constant domain of the murine IgG2a [112]. RAP-011 enhances OB mineralization and increases bone density in an osteoporotic mouse model. In MM, RAP-011 reversed OB inhibition, improved MM bone disease, and inhibited tumor growth in an in vivo humanized MM model [9]. In human, ACE-011 which is the humanized counterpart of RAP-011 effectively decreased bone resorption markers, C-terminal type 1 collagen telopeptide (CTX) and TRACP-5b and increased bone formation marker, serum levels of bone-specific alkaline phosphatase (BSALP) in postmenopausal women [113]. It has been shown in vitro that lenalidomide, a well known and approved treatment strategy for relapsed MM, stimulates activin A secretion on BMSCs via an Akt-mediated increase in JNK signaling [14]. Clinical trials for ACE-011 with Lenalidomide + Dexamethasone are ongoing and evaluating its role in MM (ClinicalTrials.gov identifier: NCT01562405).
4.7 Dkk-1 Antagonists
Dkk-1 plays one of the key roles in mediating OB inhibition in MM [71]. Therefore, treatment strategies to block Dkk-1 activity have been developed. In vitro assays show that inhibition of Dkk-1 via a specific neutralizing antibody promotes OB differentiation and function and reverses the negative effect of MM cells on OB differentiation [114, 115]. Moreover, in vivo studies using both murine and humanized murine models of MM-induced bone disease showed increased bone formation, OB numbers, and improvement of osteolytic lesions by Dkk-1 inhibition [115–117]. Importantly, blocking Dkk-1 also resulted in reduction of tumor growth, mainly as an indirect effect via modification of the tumor microenvironment [115]. Therefore, Dkk-1 inhibition via a neutralizing antibody restores bone homeostasis and may have an inhibitory effect on tumor growth. Currently, ongoing clinical trials combining Dkk-1 neutralizing antibody and bisphosphonates will test these promising preclinical results. In particular, ZA in combination with the proanabolic agent BHQ880, a fully human anti-Dkk-1 monoclonal antibody, has being studied in a phase I clinical trial (ClinicalTrials.gov identifier: NCT00741377). BHQ880 was also tested in a phase II clinical trial in smoldering MM (ClinicalTrials.gov identifier: NCT01302886) and preliminary results showed that BHQ880 significantly stimulated the vertebral strength by qCT from a baseline of 3 % (P = 0.002) (https://ash.confex.com/ash/2012/webprogram/Paper48568.html).
4.8 Sclerostin Neutralizing Antibody
Several studies have already demonstrated the importance of sclerostin in osteoporosis [118, 119], and inhibition of sclerostin represents an important strategy in the treatment of bone conditions with high catabolism. In fact, clinical trials with sclerostin neutralizing antibodies, romosozumab and blosozumab for the treatment of postmenopausal osteoporosis are ongoing and preliminary results have shown increase of bone mineral density [120–122]. In MM, higher circulating levels of sclerostin have been found in newly diagnosed MM patients, and it correlated with MM disease stage and fractures [74]. These data underscore the importance of targeting sclerostin for treatment of MM OBD. However, the source and role of sclerostin in MM OBD still remains unclear. Further studies about sclerostin’s role in MM and application of sclerostin neutralizing antibody to MM OBD are expected.
4.9 Bortezomib
Bortezomib is a proteasome and NF-kB signaling pathway inhibitor with potent anti-MM activity. Bortezomib also inhibits MM-BMSC interactions, impairs osteoclastogenesis, and stimulates mesenchymal stem cell differentiation to OB and, therefore, actively modulates bone remodeling in MM [123–125]. The anabolic effects of bortezomib are associated with Runx2 upregulation via inhibition of proteasomal degradation. Runx2 is a critical transcription factor in early OB differentiation and modulates the expression of the OB-specific transcription factor osterix [125, 126]. The anti-OC effects of bortezomib are mediated by p38 inhibition at early time points and, at later time points, by impairment of NF-kB signaling and AP1 inhibition [123]. These effects have been confirmed in the clinical setting by upregulation of OB activation markers (BSALP and osteocalcin) and downregulation of bone resorption markers (CTX and TRACP-5b) as well as decrease of Dkk-1 and sRANKL in patients treated with bortezomib [127].
4.10 Carfilzomib
In contrast to bortezomib, carfilzomib is a new proteasome inhibitor that is associated with a very low incidence of peripheral neuropathy. Carfilzomib is a structural analog of the microbial natural product epoxomicin that selectively inhibits the chymotrypsin-like activity of both the constitutive proteasome and the immunoproteasome [128]. It was recently approved in July 2012 for patients with MM experiencing disease progression after prior therapy with bortezomib and an immunomodulatory drug. Carfilzomib strongly stimulates OB calcification and inhibits OC differentiation in addition to the antitumor effect [129–131]. Moreover, we showed carfilzomib reversed OB inhibition, improved MM bone disease, and inhibited tumor growth in an in vivo disseminated MM model [131]. Interestingly, we could not see upregulation of OB differentiation marker in OBs in the presence of higher concentration of carfilzomib although the concentration of carfilzomib strongly stimulates OB calcification. Further studies are necessary to evaluate the detailed mechanism of carfilzomib effect on OBs.
4.11 Bruton’s Tyrosine Kinase Inhibitors
Bruton’s tyrosine kinase (Btk) belongs to the Tec family of tyrosine kinases. The activation of Btk regulates B-cell development and antibodies production. Thus, Btk pathway is a potential therapeutic target in a variety of B-cell malignancies, including Waldenström’s macroglobulinemia, diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma and chronic lymphocytic leukemia [132]. In MM, we showed that Btk inhibitor, CC-292 strongly inhibits OC activity and improves MM OBD [131]. It decreased only INA-6 MM cell line viability in higher concentration, however, had negligible direct in vitro effects on other MM cells viability or in animal models. On the other hand, the other Btk inhibitors, PCI-32765 (ibrutinib) and LFM-A13 have shown to display some antitumor effect in MM xenograft mouse model when INA-6 MM cells were used [133, 134]. More investigations are needed to reveal the role of Btk inhibitors in the MM OBD.
4.12 Pim Inhibitor
MM cells upregulate Pim-2 expression in BMSCs/OBs and inhibit OB differentiation [69]. Meanwhile, IL-6, produced by BMSCs, BAFF, and APRIL, produced by OCs, stimulate Pim-2 expression in MM cells via activation of NF-κB and JAK2/STAT3 pathway, resulting in MM cell survival [67]. Importantly, Pim inhibitor prevents bone destruction while suppressing MM tumor burden in MM model mouse [69]. Pim-2 may become a new target for not only MM OBD but also MM treatment.
5 Conclusion
Our understanding of the biology of MM OBD was remarkably advanced in these decades. Although OCs are a critical player in the pathogenesis of bone disease, other BM microenvironmental cells such as osteocytes, OBs, and BMSCs are affected in MM and contribute to the development of MM OBD. Many novel targets for MM OBD have been discovered following these insights. Effective therapeutic strategies to overcome MM-induced OBD should target the osteocyte-OB-OC axis, combining bone-anabolic with anticatabolic agents. Such novel agents for MM OBD restoring bone balance in MM represent a novel strategy to overcome osteolytic disease and, more provocatively, to create a hostile niche for MM tumor growth. Although there are still many unknown parts in MM OBD, further investigations will reveal these and a wide range of targeted therapies may become available to treat MM OBD more effectively in the near future.
References
Singhal S, Mehta J, Desikan R et al (1999) Antitumor activity of thalidomide in refractory multiple myeloma. N Engl J Med 341:1565–1571
Dimopoulos M, Spencer A, Attal M et al (2007) Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med 357:2123–2132
Richardson PG, Barlogie B, Berenson J et al (2003) A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med 348:2609–2617
Brenner H, Gondos A, Pulte D (2008) Recent major improvement in long-term survival of younger patients with multiple myeloma. Blood 111:2521–2526
Raje N, Roodman GD (2011) Advances in the biology and treatment of bone disease in multiple myeloma. Clin Cancer Res 17:1278–1286
Coleman RE (1997) Skeletal complications of malignancy. Cancer 80:1588–1594
Roodman GD (2010) Pathogenesis of myeloma bone disease. J Cell Biochem 109:283–291
Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R (2007) Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer 110:1860–1867
Vallet S, Mukherjee S, Vaghela N et al (2010) Activin A promotes multiple myeloma-induced osteolysis and is a promising target for myeloma bone disease. Proc Natl Acad Sci USA 107:5124–5129
Vallet S, Raje N (2011) Bone anabolic agents for the treatment of multiple myeloma. Cancer Microenviron 4:339–349
Sonmez M, Akagun T, Topbas M, et al (2008) Effect of pathologic fractures on survival in multiple myeloma patients: a case control study. J Exp Clin Cancer Res 27:11-9966-27-11
Podar K, Chauhan D, Anderson KC (2009) Bone marrow microenvironment and the identification of new targets for myeloma therapy. Leukemia 23:10–24
Edwards CM, Edwards JR, Lwin ST et al (2008) Increasing Wnt signaling in the bone marrow microenvironment inhibits the development of myeloma bone disease and reduces tumor burden in bone in vivo. Blood 111:2833–2842
Scullen T, Santo L, Vallet S et al (2013) Lenalidomide in combination with an activin A-neutralizing antibody: preclinical rationale for a novel anti-myeloma strategy. Leukemia 27:1715–1721
Choi SJ, Oba Y, Gazitt Y et al (2001) Antisense inhibition of macrophage inflammatory protein 1-alpha blocks bone destruction in a model of myeloma bone disease. J Clin Invest 108:1833–1841
Bonewald LF (2011) The amazing osteocyte. J Bone Miner Res 26:229–238
Aguirre JI, Plotkin LI, Stewart SA et al (2006) Osteocyte apoptosis is induced by weightlessness in mice and precedes osteoclast recruitment and bone loss. J Bone Miner Res 21:605–615
Kitase Y, Barragan L, Qing H et al (2010) Mechanical induction of PGE2 in osteocytes blocks glucocorticoid-induced apoptosis through both the beta-catenin and PKA pathways. J Bone Miner Res 25:2657–2668
Kogianni G, Mann V, Noble BS (2008) Apoptotic bodies convey activity capable of initiating osteoclastogenesis and localized bone destruction. J Bone Miner Res 23:915–927
Baron R, Kneissel M (2013) WNT signaling in bone homeostasis and disease: from human mutations to treatments. Nat Med 19:179–192
Negishi-Koga T, Shinohara M, Komatsu N et al (2011) Suppression of bone formation by osteoclastic expression of semaphorin 4D. Nat Med 17:1473–1480
Valentin-Opran A, Charhon SA, Meunier PJ, Edouard CM, Arlot ME (1982) Quantitative histology of myeloma-induced bone changes. Br J Haematol 52:601–610
Taube T, Beneton MN, McCloskey EV, Rogers S, Greaves M, Kanis JA (1992) Abnormal bone remodelling in patients with myelomatosis and normal biochemical indices of bone resorption. Eur J Haematol 49:192–198
Terpos E, Szydlo R, Apperley JF et al (2003) Soluble receptor activator of nuclear factor kappaB ligand-osteoprotegerin ratio predicts survival in multiple myeloma: proposal for a novel prognostic index. Blood 102:1064–1069
Politou M, Terpos E, Anagnostopoulos A et al (2004) Role of receptor activator of nuclear factor-kappa B ligand (RANKL), osteoprotegerin and macrophage protein 1-alpha (MIP-1a) in monoclonal gammopathy of undetermined significance (MGUS). Br J Haematol 126:686–689
Lee JW, Chung HY, Ehrlich LA et al (2004) IL-3 expression by myeloma cells increases both osteoclast formation and growth of myeloma cells. Blood 103:2308–2315
Colucci S, Brunetti G, Mori G et al (2009) Soluble decoy receptor 3 modulates the survival and formation of osteoclasts from multiple myeloma bone disease patients. Leukemia 23:2139–2146
Brunetti G, Oranger A, Mori G et al (2010) The formation of osteoclasts in multiple myeloma bone disease patients involves the secretion of soluble decoy receptor 3. Ann N Y Acad Sci 1192:298–302
Abe M, Hiura K, Wilde J et al (2002) Role for macrophage inflammatory protein (MIP)-1alpha and MIP-1beta in the development of osteolytic lesions in multiple myeloma. Blood 100:2195–2202
Uneda S, Hata H, Matsuno F et al (2003) Macrophage inflammatory protein-1 alpha is produced by human multiple myeloma (MM) cells and its expression correlates with bone lesions in patients with MM. Br J Haematol 120:53–55
Vallet S, Pozzi S, Patel K et al (2011) A novel role for CCL3 (MIP-1alpha) in myeloma-induced bone disease via osteocalcin downregulation and inhibition of osteoblast function. Leukemia 25:1174–1181
Gupta D, Treon SP, Shima Y et al (2001) Adherence of multiple myeloma cells to bone marrow stromal cells upregulates vascular endothelial growth factor secretion: therapeutic applications. Leukemia 15:1950–1961
Nanes MS (2003) Tumor necrosis factor-alpha: molecular and cellular mechanisms in skeletal pathology. Gene 321:1–15
Kitaura H, Sands MS, Aya K et al (2004) Marrow stromal cells and osteoclast precursors differentially contribute to TNF-alpha-induced osteoclastogenesis in vivo. J Immunol 173:4838–4846
Giuliani N, Bataille R, Mancini C, Lazzaretti M, Barille S (2001) Myeloma cells induce imbalance in the osteoprotegerin/osteoprotegerin ligand system in the human bone marrow environment. Blood 98:3527–3533
Pearse RN, Sordillo EM, Yaccoby S et al (2001) Multiple myeloma disrupts the TRANCE/ osteoprotegerin cytokine axis to trigger bone destruction and promote tumor progression. Proc Natl Acad Sci USA 98:11581–11586
Roux S, Meignin V, Quillard J et al (2002) RANK (receptor activator of nuclear factor-kappaB) and RANKL expression in multiple myeloma. Br J Haematol 117:86–92
Colucci S, Brunetti G, Rizzi R et al (2004) T cells support osteoclastogenesis in an in vitro model derived from human multiple myeloma bone disease: the role of the OPG/TRAIL interaction. Blood 104:3722–3730
Michigami T, Shimizu N, Williams PJ et al (2000) Cell-cell contact between marrow stromal cells and myeloma cells via VCAM-1 and alpha(4)beta(1)-integrin enhances production of osteoclast-stimulating activity. Blood 96:1953–1960
Hideshima T, Chauhan D, Hayashi T et al (2002) The biological sequelae of stromal cell-derived factor-1alpha in multiple myeloma. Mol Cancer Ther 1:539–544
Tai YT, Li XF, Breitkreutz I et al (2006) Role of B-cell-activating factor in adhesion and growth of human multiple myeloma cells in the bone marrow microenvironment. Cancer Res 66:6675–6682
Chauhan D, Uchiyama H, Akbarali Y et al (1996) Multiple myeloma cell adhesion-induced interleukin-6 expression in bone marrow stromal cells involves activation of NF-kappa B. Blood 87:1104–1112
Uchiyama H, Barut BA, Mohrbacher AF, Chauhan D, Anderson KC (1993) Adhesion of human myeloma-derived cell lines to bone marrow stromal cells stimulates interleukin-6 secretion. Blood 82:3712–3720
Sezer O, Heider U, Zavrski I, Kuhne CA, Hofbauer LC (2003) RANK ligand and osteoprotegerin in myeloma bone disease. Blood 101:2094–2098
Giuliani N, Ferretti M, Bolzoni M et al (2012) Increased osteocyte death in multiple myeloma patients: role in myeloma-induced osteoclast formation. Leukemia 26:1391–1401
Silbermann R, Bolzoni M, Storti P et al (2014) Bone marrow monocyte-/macrophage-derived activin A mediates the osteoclastogenic effect of IL-3 in multiple myeloma. Leukemia 28:951–954
Masih-Khan E, Trudel S, Heise C et al (2006) MIP-1alpha (CCL3) is a downstream target of FGFR3 and RAS-MAPK signaling in multiple myeloma. Blood 108:3465–3471
Rivollier A, Mazzorana M, Tebib J et al (2004) Immature dendritic cell transdifferentiation into osteoclasts: a novel pathway sustained by the rheumatoid arthritis microenvironment. Blood 104:4029–4037
Han JH, Choi SJ, Kurihara N, Koide M, Oba Y, Roodman GD (2001) Macrophage inflammatory protein-1alpha is an osteoclastogenic factor in myeloma that is independent of receptor activator of nuclear factor kappaB ligand. Blood 97:3349–3353
Lentzsch S, Gries M, Janz M, Bargou R, Dorken B, Mapara MY (2003) Macrophage inflammatory protein 1-alpha (MIP-1 alpha) triggers migration and signaling cascades mediating survival and proliferation in multiple myeloma (MM) cells. Blood 101:3568–3573
Vallet S, Raje N, Ishitsuka K et al (2007) MLN3897, a novel CCR1 inhibitor, impairs osteoclastogenesis and inhibits the interaction of multiple myeloma cells and osteoclasts. Blood 110:3744–3752
Mancino AT, Klimberg VS, Yamamoto M, Manolagas SC, Abe E (2001) Breast cancer increases osteoclastogenesis by secreting M-CSF and upregulating RANKL in stromal cells. J Surg Res 100:18–24
Moschen AR, Kaser A, Enrich B et al (2005) The RANKL/OPG system is activated in inflammatory bowel disease and relates to the state of bone loss. Gut 54:479–487
Romas E, Gillespie MT, Martin TJ (2002) Involvement of receptor activator of NFkappaB ligand and tumor necrosis factor-alpha in bone destruction in rheumatoid arthritis. Bone 30:340–346
Seidel C, Hjertner O, Abildgaard N et al (2001) Serum osteoprotegerin levels are reduced in patients with multiple myeloma with lytic bone disease. Blood 98:2269–2271
Croucher PI, Shipman CM, Lippitt J et al (2001) Osteoprotegerin inhibits the development of osteolytic bone disease in multiple myeloma. Blood 98:3534–3540
Terpos E, Politou M, Szydlo R et al (2004) Autologous stem cell transplantation normalizes abnormal bone remodeling and sRANKL/osteoprotegerin ratio in patients with multiple myeloma. Leukemia 18:1420–1426
Terpos E, Mihou D, Szydlo R et al (2005) The combination of intermediate doses of thalidomide with dexamethasone is an effective treatment for patients with refractory/relapsed multiple myeloma and normalizes abnormal bone remodeling, through the reduction of sRANKL/osteoprotegerin ratio. Leukemia 19:1969–1976
Nguyen AN, Stebbins EG, Henson M et al (2006) Normalizing the bone marrow microenvironment with p38 inhibitor reduces multiple myeloma cell proliferation and adhesion and suppresses osteoclast formation. Exp Cell Res 312:1909–1923
Ishitsuka K, Hideshima T, Neri P et al (2008) p38 mitogen-activated protein kinase inhibitor LY2228820 enhances bortezomib-induced cytotoxicity and inhibits osteoclastogenesis in multiple myeloma; therapeutic implications. Br J Haematol 141:598–606
Hiruma Y, Honjo T, Jelinek DF et al (2009) Increased signaling through p62 in the marrow microenvironment increases myeloma cell growth and osteoclast formation. Blood 113:4894–4902
Urashima M, Chauhan D, Uchiyama H, Freeman GJ, Anderson KC (1995) CD40 ligand triggered interleukin-6 secretion in multiple myeloma. Blood 85:1903–1912
Xu G, Liu K, Anderson J et al (2012) Expression of XBP1 s in bone marrow stromal cells is critical for myeloma cell growth and osteoclast formation. Blood 119:4205–4214
Dankbar B, Padro T, Leo R et al (2000) Vascular endothelial growth factor and interleukin-6 in paracrine tumor-stromal cell interactions in multiple myeloma. Blood 95:2630–2636
Moreaux J, Legouffe E, Jourdan E et al (2004) BAFF and APRIL protect myeloma cells from apoptosis induced by interleukin 6 deprivation and dexamethasone. Blood 103:3148–3157
Neri P, Kumar S, Fulciniti MT et al (2007) Neutralizing B-cell activating factor antibody improves survival and inhibits osteoclastogenesis in a severe combined immunodeficient human multiple myeloma model. Clin Cancer Res 13:5903–5909
Asano J, Nakano A, Oda A et al (2011) The serine/threonine kinase Pim-2 is a novel anti-apoptotic mediator in myeloma cells. Leukemia 25:1182–1188
Terpos E, Kastritis E, Christoulas D et al (2012) Circulating activin-A is elevated in patients with advanced multiple myeloma and correlates with extensive bone involvement and inferior survival; no alterations post-lenalidomide and dexamethasone therapy. Ann Oncol 23:2681–2686
Hiasa M, Teramachi J, Oda A et al (2015) Pim-2 kinase is an important target of treatment for tumor progression and bone loss in myeloma. Leukemia 29:207–217
Westendorf JJ, Kahler RA, Schroeder TM (2004) Wnt signaling in osteoblasts and bone diseases. Gene 341:19–39
Tian E, Zhan F, Walker R et al (2003) The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med 349:2483–2494
Oshima T, Abe M, Asano J et al (2005) Myeloma cells suppress bone formation by secreting a soluble Wnt inhibitor, sFRP-2. Blood 106:3160–3165
Giuliani N, Morandi F, Tagliaferri S et al (2007) Production of Wnt inhibitors by myeloma cells: potential effects on canonical Wnt pathway in the bone microenvironment. Cancer Res 67:7665–7674
Terpos E, Christoulas D, Katodritou E et al (2012) Elevated circulating sclerostin correlates with advanced disease features and abnormal bone remodeling in symptomatic myeloma: reduction post-bortezomib monotherapy. Int J Cancer 131:1466–1471
Colucci S, Brunetti G, Oranger A et al (2011) Myeloma cells suppress osteoblasts through sclerostin secretion. Blood Cancer J 1:e27
Delgado-Calle J, Bellido T, Roodman GD (2014) Role of osteocytes in multiple myeloma bone disease. Curr Opin Support Palliat Care 8:407–413
Favus MJ (2010) Bisphosphonates for osteoporosis. N Engl J Med 363:2027–2035
Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T (1999) Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest 104:1363–1374
Kogianni G, Mann V, Ebetino F et al (2004) Fas/CD95 is associated with glucocorticoid-induced osteocyte apoptosis. Life Sci 75:2879–2895
Plotkin LI, Manolagas SC, Bellido T (2006) Dissociation of the pro-apoptotic effects of bisphosphonates on osteoclasts from their anti-apoptotic effects on osteoblasts/osteocytes with novel analogs. Bone 39:443–452
Plotkin LI, Aguirre JI, Kousteni S, Manolagas SC, Bellido T (2005) Bisphosphonates and estrogens inhibit osteocyte apoptosis via distinct molecular mechanisms downstream of extracellular signal-regulated kinase activation. J Biol Chem 280:7317–7325
Black DM, Cummings SR, Karpf DB et al (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Black DM, Delmas PD, Eastell R et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Rosen LS, Gordon D, Kaminski M et al (2003) Long-term efficacy and safety of zoledronic acid compared with pamidronate disodium in the treatment of skeletal complications in patients with advanced multiple myeloma or breast carcinoma: a randomized, double-blind, multicenter, comparative trial. Cancer 98:1735–1744
Rosen LS, Gordon D, Tchekmedyian S et al (2003) Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial—the Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. J Clin Oncol 21:3150–3157
Saad F, Gleason DM, Murray R et al (2004) Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst 96:879–882
Berenson JR, Lichtenstein A, Porter L et al (1996) Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. Myeloma Aredia Study Group. N Engl J Med 334:488–493
Major P, Lortholary A, Hon J et al (2001) Zoledronic acid is superior to pamidronate in the treatment of hypercalcemia of malignancy: a pooled analysis of two randomized, controlled clinical trials. J Clin Oncol 19:558–567
Gnant M, Mlineritsch B, Stoeger H et al (2011) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol 12:631–641
Coleman RE, Marshall H, Cameron D et al (2011) Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med 365:1396–1405
Morgan GJ, Davies FE, Gregory WM et al (2010) First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet 376:1989–1999
Raje N, Woo SB, Hande K et al (2008) Clinical, radiographic, and biochemical characterization of multiple myeloma patients with osteonecrosis of the jaw. Clin Cancer Res 14:2387–2395
Woo SB, Hellstein JW, Kalmar JR (2006) Narrative [corrected] review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med 144:753–761
Basso FG, Turrioni AP, Hebling J, de Souza Costa CA (2013) Effects of zoledronic acid on odontoblast-like cells. Arch Oral Biol 58:467–473
Bagan J, Scully C, Sabater V, Jimenez Y (2009) Osteonecrosis of the jaws in patients treated with intravenous bisphosphonates (BRONJ): a concise update. Oral Oncol 45:551–554
Wimalawansa SJ (2008) Insight into bisphosphonate-associated osteomyelitis of the jaw: pathophysiology, mechanisms and clinical management. Expert Opin Drug Saf 7:491–512
Dimopoulos MA, Kastritis E, Anagnostopoulos A et al (2006) Osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates: evidence of increased risk after treatment with zoledronic acid. Haematologica 91:968–971
Zervas K, Verrou E, Teleioudis Z et al (2006) Incidence, risk factors and management of osteonecrosis of the jaw in patients with multiple myeloma: a single-centre experience in 303 patients. Br J Haematol 134:620–623
Morgan GJ (2011) Further analyses of the Myeloma IX Study. Lancet 378:768–769
Yee AJ, Raje NS (2012) Denosumab, a RANK ligand inhibitor, for the management of bone loss in cancer patients. Clin Interv Aging 7:331–338
Kobayashi E, Setsu N (2015) Osteosclerosis induced by denosumab. Lancet 385:539-6736(14)61338-6. Epub 2014 Oct 28
Gossai N, Hilgers MV, Polgreen LE, Greengard EG (2015) Critical hypercalcemia following discontinuation of denosumab therapy for metastatic giant cell tumor of bone. Pediatr Blood Cancer
Henry DH, Costa L, Goldwasser F et al (2011) Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 29:1125–1132
Body JJ, Greipp P, Coleman RE et al (2003) A phase I study of AMGN-0007, a recombinant osteoprotegerin construct, in patients with multiple myeloma or breast carcinoma related bone metastases. Cancer 97:887–892
Oyajobi BO, Franchin G, Williams PJ et al (2003) Dual effects of macrophage inflammatory protein-1alpha on osteolysis and tumor burden in the murine 5TGM1 model of myeloma bone disease. Blood 102:311–319
Oba Y, Lee JW, Ehrlich LA et al (2005) MIP-1alpha utilizes both CCR1 and CCR5 to induce osteoclast formation and increase adhesion of myeloma cells to marrow stromal cells. Exp Hematol 33:272–278
Dairaghi DJ, Oyajobi BO, Gupta A et al (2012) CCR1 blockade reduces tumor burden and osteolysis in vivo in a mouse model of myeloma bone disease. Blood 120:1449–1457
Novak AJ, Darce JR, Arendt BK et al (2004) Expression of BCMA, TACI, and BAFF-R in multiple myeloma: a mechanism for growth and survival. Blood 103:689–694
Mackay F, Browning JL (2002) BAFF: a fundamental survival factor for B cells. Nat Rev Immunol 2:465–475
Moore PA, Belvedere O, Orr A et al (1999) BLyS: member of the tumor necrosis factor family and B lymphocyte stimulator. Science 285:260–263
Moreaux J, Cremer FW, Reme T et al (2005) The level of TACI gene expression in myeloma cells is associated with a signature of microenvironment dependence versus a plasmablastic signature. Blood 106:1021–1030
Pearsall RS, Canalis E, Cornwall-Brady M et al (2008) A soluble activin type IIA receptor induces bone formation and improves skeletal integrity. Proc Natl Acad Sci USA 105:7082–7087
Ruckle J, Jacobs M, Kramer W et al (2009) Single-dose, randomized, double-blind, placebo-controlled study of ACE-011 (ActRIIA-IgG1) in postmenopausal women. J Bone Miner Res 24:744–752
Pozzi S, Fulciniti M, Yan H et al (2013) In vivo and in vitro effects of a novel anti-Dkk1 neutralizing antibody in multiple myeloma. Bone 53:487–496
Fulciniti M, Tassone P, Hideshima T et al (2009) Anti-DKK1 mAb (BHQ880) as a potential therapeutic agent for multiple myeloma. Blood 114:371–379
Yaccoby S, Ling W, Zhan F, Walker R, Barlogie B, Shaughnessy JD Jr (2007) Antibody-based inhibition of DKK1 suppresses tumor-induced bone resorption and multiple myeloma growth in vivo. Blood 109:2106–2111
Heath DJ, Chantry AD, Buckle CH et al (2009) Inhibiting Dickkopf-1 (Dkk1) removes suppression of bone formation and prevents the development of osteolytic bone disease in multiple myeloma. J Bone Miner Res 24:425–436
Hoeppner LH, Secreto FJ, Westendorf JJ (2009) Wnt signaling as a therapeutic target for bone diseases. Expert Opin Ther Targets 13:485–496
Lewiecki EM (2011) New targets for intervention in the treatment of postmenopausal osteoporosis. Nat Rev Rheumatol 7:631–638
McClung MR, Grauer A, Boonen S et al (2014) Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med 370:412–420
McColm J, Hu L, Womack T, Tang CC, Chiang AY (2014) Single- and multiple-dose randomized studies of blosozumab, a monoclonal antibody against sclerostin, in healthy postmenopausal women. J Bone Miner Res 29:935–943
Clarke BL (2014) Anti-sclerostin antibodies: utility in treatment of osteoporosis. Maturitas 78:199–204
von Metzler I, Krebbel H, Hecht M et al (2007) Bortezomib inhibits human osteoclastogenesis. Leukemia 21:2025–2034
Zangari M, Esseltine D, Lee CK et al (2005) Response to bortezomib is associated to osteoblastic activation in patients with multiple myeloma. Br J Haematol 131:71–73
Mukherjee S, Raje N, Schoonmaker JA et al (2008) Pharmacologic targeting of a stem/progenitor population in vivo is associated with enhanced bone regeneration in mice. J Clin Invest 118:491–504
Giuliani N, Morandi F, Tagliaferri S et al (2007) The proteasome inhibitor bortezomib affects osteoblast differentiation in vitro and in vivo in multiple myeloma patients. Blood 110:334–338
Terpos E, Heath DJ, Rahemtulla A et al (2006) Bortezomib reduces serum dickkopf-1 and receptor activator of nuclear factor-kappaB ligand concentrations and normalises indices of bone remodelling in patients with relapsed multiple myeloma. Br J Haematol 135:688–692
Kuhn DJ, Chen Q, Voorhees PM et al (2007) Potent activity of carfilzomib, a novel, irreversible inhibitor of the ubiquitin-proteasome pathway, against preclinical models of multiple myeloma. Blood 110:3281–3290
Hurchla MA, Garcia-Gomez A, Hornick MC et al (2013) The epoxyketone-based proteasome inhibitors carfilzomib and orally bioavailable oprozomib have anti-resorptive and bone-anabolic activity in addition to anti-myeloma effects. Leukemia 27:430–440
Ha SW, Weitzmann MN, Beck GR Jr (2014) Bioactive silica nanoparticles promote osteoblast differentiation through stimulation of autophagy and direct association with LC3 and p62. ACS Nano 8:5898–5910
Eda H, Santo L, Cirstea DD et al (2014) A novel Bruton’s tyrosine kinase inhibitor CC-292 in combination with the proteasome inhibitor carfilzomib impacts the bone microenvironment in a multiple myeloma model with resultant antimyeloma activity. Leukemia 28:1892–1901
Brown JR (2013) Ibrutinib in chronic lymphocytic leukemia and B cell malignancies. Leuk Lymphoma
Tai YT, Chang BY, Kong SY et al (2012) Bruton tyrosine kinase inhibition is a novel therapeutic strategy targeting tumor in the bone marrow microenvironment in multiple myeloma. Blood 120:1877–1887
Bam R, Ling W, Khan S et al (2013) Role of Bruton’s tyrosine kinase in myeloma cell migration and induction of bone disease. Am J Hematol 88:463–471
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Eda, H., Santo, L., David Roodman, G., Raje, N. (2016). Bone Disease in Multiple Myeloma. In: Roccaro, A., Ghobrial, I. (eds) Plasma Cell Dyscrasias. Cancer Treatment and Research, vol 169. Springer, Cham. https://doi.org/10.1007/978-3-319-40320-5_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-40320-5_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40318-2
Online ISBN: 978-3-319-40320-5
eBook Packages: MedicineMedicine (R0)