Abstract
It is plausible that auditory symptoms can become comorbidity with Chikungunya (CHIK) virus infections. The exact etiology is not known due to the lack of full literature as well as the lower number of reports regarding the incidence of hearing related issues in the affected persons. Moreover, in the developing and under-developed countries (which is where the infection is more prevalent), hearing difficulties are usually not reported until it is significantly noticeable by the patient or affecting quality of life (which is dependent on the listening needs of the individual). It has been reported that the neurotropic nature of the CHIK virus can have effect on the auditory and associated neurons. As demyelination neuropathy is mostly reported in patients with CHIKinfection (Chandak et al., Neurol India 57:177–181, 2009), it is possible that a similar demyelination can be the cause of the auditory symptom, such as in case of Auditory Neuropathy Spectrum Disorder (ANSD) presentations. It is also likely that, if the virus crosses and reaches the cochlea it can have similar effect of other viral infections in the cochlea such as rubella and herpes simplex, which can cause varying degrees of atrophy of organ of corti, striavascularis and/or tectorial membrane.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chikungunya
- Viral infections
- Neuropathy
- Neuro-virulence
- Spectrum disorder
- Auditory system
- Auditory nerve
- Demyelination
- Atrophy
1 Introduction
Chikungunya (CHIK) virus is gradually rising to be a “global public health menace”, that affects millions of people from across the world, majorly in the tropical and sub-tropical countries (Petersen and Powers 2016). The CHIK, a single stranded RNA virus, is mostly transmitted by vector mosquitoes such as Aedesaegypti and Aedesalbopictus, belonging to the Alpha virus genus. In some cases, vertical maternal fetal transmission have also been reported (Robillard et al. 2006). Once infected, the virus utilizes an incubation period of up to a week before the symptoms start appearing. The CHIK infection spreads to wherever the vectors move and are more common in tropical countries. Increased travel from one place to the other by humans and the capacity of CHIK to produce high levels of infection, and mutation also contribute to its fast spread. The most common symptoms include elevated body temperatures, joint pain and swelling, rash, headache, tiredness etc.
According to the World Health Organization, this viral infection, first identified in Tanzania in 1952, has spread to at least 40 countries including Asia, Africa, Europe and America (World Health Organisation, 2017). Phylogenetic analyses carried out on CHIK virus identifies its four different genotypes—Asian/Caribbean, West African, Eastern/Central/South African and Indian Ocean Line (Moizeis et al. 2018). The major difference between these genotypes lies in their transmission cycles.
The CHIK virus is detected through laboratory testing (microscopic presence of CHIK virus and its Immunoglobulin M analyses). A reverse transcription polymerase chain reaction can also be used; however its sensitivity remains weak (Johnson et al. 2016).
2 Clinical Presentations
CHIK virus fever widely varies according to clinical manifestations. Samples were collected from the residents of a CHIK virus hit area in Southern Thailand and tested for the presence of the virus (Nakkhara et al. 2013). Although 61.9% of the samples tested were positive for the virus, 47.1% of the positive tested were asymptomatic. The authors concluded that even though the transmission is based on the environmental conditions, symptoms are dependent on “personal biologic factors and social setting”. Individuals aged above 30 years with Rh positive blood groups were found to be more susceptible to the virus. In addition, males were 1.3 times more likely to be affected by the disease than females (Kumar et al. 2010). Once infected, the individuals may be debilitated to work as there can be a reduction in dexterity, mobility and reaction.
The symptomatic cases are mostly characterized by a triad of symptoms which include ocular manifestations like conjunctivitis, retinitis etc. In some cases, the CHIK virus infection also exhibits neurological complications such as encephalitis, bulbar palsy, acute disseminated encephalomyelitis, cerebellitis, myelopathy, radiculoneuropathy, carpel tunnel syndrome and tremors were reported (Anand et al. 2019). Other signs like peripheral neuropathy and myeloneuropathy have also been presented with CHIK virus infection. The neuropathy was mostly caused by the demyelination of the neurons. Studies carried out in South India found that individuals with CHIK virus infection also had some ocular signs such as anterior uveitis, optic neuritis, retrobulbar neuritis and dendritic lesions (Chandak et al. 2009; Lalitha et al. 2007). The prognosis for the above mentioned visual difficulties were reported to be good and most patients recovered completely (Lalitha et al. 2007). Some other atypical manifestations like cardiovascular, respiratory, vascular, renal, hepatic, gastrointestinal and adrenal system have also been noticed by some authors (Mehta et al. 2018; Anand et al. 2019; Chandak et al. 2009).
3 Chikungunya Virus Effect on the Auditory System
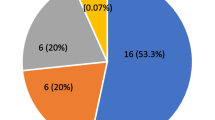
Amongst CHIK virus infected persons, 60% reported facing some kind of comorbidities, which was more in individuals who had the onset of disease at an older age (mean age: 54.2 years). Such patients also had lesser recovery rates. Of this, six percent of the individuals reported sustained severe to profound hearing loss (Couturier et al. 2012). There are other instances where bilateral mild to severe sensorineural hearing loss has been reported with CHIK virus infection (Dutta et al. 2011).
Therefore, development of hearing difficulty or hearing related problems, though less encountered, are prevailing amongst neurological complication post CHIK virus infection. In a case study carried out in Colombia, it was observed that a child acquired mild hearing impairment, with altered auditory evoked potential, after 13 months of CHIK virus infection (Alvarado-Socarras et al. 2016).
There are also instances where sudden sensorineural hearing loss was reported one week post onset of CHIK virus fever, which was preceded by tinnitus. The hearing difficulty was associated with other aural symptoms such as fullness in the ear, severe giddiness, nausea and vomiting. Upon audiological testing, the patient was diagnosed as having profound hearing loss. The probable etiology was routed to “atrophy of organ of corti, striavascularis and tectorial membrane with variable loss of neuronal population” during the virus attack (Bhavana et al. 2008).
4 Peripheral Neuropathy
Peripheral neuropathy has been associated with CHIK virus infected patients. Its symptoms usually are linked with the conditions where it is gradually progressive. When this happens in the auditory system, the condition is termed as auditory neuropathy spectrum disorder (ANSD). In ANSD (which is a “cochlear afferent disorder”), it is sound transduction that is majorly affected. This is mostly accounted to primary demyelination of neurons and axonal loss (Starr et al. 1996). It is likely that the CHIK virus follows similar pathology within the inner ear and causes the various auditory symptoms.
ANSD can happen at three different levels—pre-synaptic, synaptic (at the ribbon synapse between inner hair cells and the auditory nerve) and post synaptic where it causes a disruption in the VIII cranial nerve activity. This disruption mostly arises either due deafferentiation (reduced number of activated auditory nerve fibers) which in most cases of axonal type of neuropathy or due to reduced neural synchrony occurs mostly in demyelinating neuropathies (Rance and Starr 2015). Since CHIK virus has been associated with demyelination of nerve cells and its neurotoxic nature established, ANSD is very likely neurological comorbidity in individuals with CHIK fever, if the virus enters the auditory system.
The possibility exists that neural hearing loss may be present in individuals having CHIK virus infection. Prabhu (2015), observed such findings in a 14 year old boy with complaint of a decline in his hearing and increase in humming tinnitus (catastrophic) in both his ears along with difficulty in understanding speech onset after the attack of CHIK fever. These were also associated with vertigo and Tullio phenomenon. The boy also had mild form of depression. Upon detailed investigation, he was found to have bilateral mild sensorineural hearing loss (rising configuration) with poor speech identification scores. Abnormal or absent auditory brainstem response and cervical vestibular evoked myogenic potential recordings were obtained for this patient. This along with the findings in otoacoustic emissions indicated the presence of retrocochlear pathology like ANSD.
Hence, a test battery approach is mandatory to diagnose and habilitate individuals with hearing impairment post CHIK virus infection. The audiological test battery for post CHIK virus infestation should include pure tone audiometry and speech audiometry to understand the degree of loss of sensitivity. Speech audiometry results also can help in predicting the neuronal ability to conduct speech sounds. An immittance audiometry need to be carried out which includes both tympanometry as well as reflexometry to understand the middle ear status of the individual. Otoacoustic emissions can be measured to obtain information about the cochlear status and the outer hair cell functioning. Auditory evoked responses such as brainstem evoked response audiometry, vestibular evoked myogenic potentials etc. need to be administered to rule out retrocochlear pathology such as ANSD. Further testing can be decided based on the findings from these mentioned tests. The rehabilitative options suggested to the patient will also vary depending on these test results.
5 Conclusion
It is intriguing that such a small single stranded RNA virus can cause such a varied genre of symptoms in humans. It is quite evident that CHIK virus can lead to auditory deficit, probably as a result of demyelination of neurons leading to neuropathy or toxicity caused in the inner ear. However, there is dearth of literature to point out exact signs and symptoms or prognostic factors associated with this viral infection in the auditory system. It is likely that the symptoms vary depending on the extent of the spread and severity of the infection.
If a person reports with hearing loss onset after CHIK virus infection, it is important that a complete audio-vestibular test battery approach be administered. A single test cannot give a clear information about the patient’s audio-vestibular profile. Multiple tests have to be carried out and correlated before reaching a diagnostic conclusion.
Hence, a test battery approach is mandatory to diagnose and habilitate individuals with hearing impairment post CHIK virus infection. The audiological test battery for individuals post CHIK virus infestation should include pure tone audiometry and speech audiometry to understand the degree of loss of sensitivity. Speech audiometry results also can help in predicting the neuronal ability to conduct speech sounds. An immittance audiometry need to be carried out which includes both tympanometry as well as reflexometry to understand the middle ear status of the person. Otoacoustic emissions can be measured to obtain information about the cochlear status and the outer hair cell functioning. Auditory evoked responses such as brainstem evoked response audiometry, vestibular evoked myogenic potentials etc. need to be administered to rule out retrocochlear pathology such as ANSD. Further testing can be decided based on the findings from the mentioned tests. The rehabilitative options suggested to the patient will also vary depending on these test results.
References
Alvarado-Socarras JL, Ocampo-Gonzalez M, Vargas-Soler JA, Rodriguez-Morales A, Franco-Paredes C. Congenital and Neonatal Chikungunya in Colombia. J Pediatr Infect Dis Soc. 2016;5(3):17–20. https://doi.org/10.1093/jpids/piw021.
Anand KS, Agrawal AK, Garg J, Dhamija RK, Mahajan RK. Spectrum of neurological complications in chikungunya fever: experience at a tertiary care centre and review of literature. Troplical Doctor. 2019;28–9. https://doi.org/10.1177/0049475518825219.
Bhavana K, Tyagi I, Kapila RK. Chikungunya virus induced sudden sensorineural hearing loss. Int J Pediatr Otorhinolaryngol. 2008;72:257–9. https://doi.org/10.1016/j.ijporl.2007.09.022.
Chandak NH, Kashyap RS, Kabra D, Karandikar P, Saha SS, Morey SH, Daginawala HF. Neurological complications of Chikungunya virus infection. Neurol India. 2009;57(2):177–81. https://doi.org/10.4103/0028-3886.51289.
Couturier E, Guillemin F, Mura M, Le L, Valk HD, Virion J, Simon F. Impaired quality of life after chikungunya virus infection: a 2-year follow-up study. Rheumatology. 2012;51(March):1315–22. https://doi.org/10.1093/rheumatology/kes015.
Dutta P, Khan SA, Khan AM, Borah J, Chowdhury P, Mahanta J. First evidence of chikungunya virus infection in Assam, Northeast India. Trans R Soc Trop Med Hyg. 2011;105(6):355–7. https://doi.org/10.1016/j.trstmh.2011.02.004.
Johnson BW, Russell BJ, Goodman CH. Laboratory diagnosis of chikungunya virus infections and commercial sources for diagnostic assays. J Infect Dis. 2016;214:471–4. https://doi.org/10.1093/infdis/jiw274.Laboratory.
Kumar NCVM, Nadimpalli M, Vardhan VR, Gopal SDVR. Association of ABO blood groups with Chikungunya virus. Virol J. 2010;7(1).
Lalitha P, Rathinam S, Banushree K, Maheshkumar S, Vijayakumar R, Sathe P. Ocular involvement associated with an epidemic outbreak of chikungunya virus infection. Am J Ophthalmol. 2007;144(4):552–6. https://doi.org/10.1016/j.ajo.2007.06.002.
Mehta R, Gerardin P, Alexandre C, Brito A De, Solomon T, Brito ML. The neurological complications of chikungunya virus: a systematic review. Rev Med Virol. 2018;28(3). https://doi.org/10.1002/rmv.1978
Moizeis RNC, Fernandes TAA de M, Guedes PM da M, Pereira HWB, Lanza DCF, Azevedo JWV de, Fernandes JV, et al. Chikungunya fever: a threat to global public health. Pathog Glob Health. 2018;112(4), 182–94. https://doi.org/10.1080/20477724.2018.1478777
Nakkhara P, Chongsuvivatwong V, Thammapalo S. Risk factors for symptomatic and asymptomatic chikungunya infection. Trans R Soc Trop Med Hyg. 2013;107(September):789–96. https://doi.org/10.1093/trstmh/trt083.
Petersen LR, Powers AM. Chikungunya: epidemiology. F1000Research. 2016;5, 1–8. https://doi.org/10.12688/f1000research.7171.1
Prabhu P. Acquired auditory neuropathy spectrum disorder after an attack of chikungunya: case study. Eur Arch. 2015;273(1):257–61. https://doi.org/10.1007/s00405-015-3578-9.
Rance G, Starr A. Pathophysiological mechanisms and functional hearing consequences of auditory neuropathy. Brain. 2015;138(11):3141–58. https://doi.org/10.1093/brain/awv270.
Robillard P, Boumahni B, Gerardin P, Michault A, Fourmaintraux A, Schuffenecker I, Barau G. Vertical maternal fetal transmission of the Chikungunya virus. Presse Med. 2006;35(May):785–8.
Starr A, Picton TW, Kim R. Pathophysiology of auditory neuropathy. In Auditory neuropathy; 1996. p. 741–53.
World Health Organisation. WHO | Chikungunya. WHO. 2017. https://doi.org/10.1016/S1726-4901(10)70043-5.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Prabhu, P., Gafoor, S.A. (2021). Effect of Chikungunya Viral Infection on the Auditory System. In: Ahmad, S.I. (eds) Human Viruses: Diseases, Treatments and Vaccines . Springer, Cham. https://doi.org/10.1007/978-3-030-71165-8_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-71165-8_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71164-1
Online ISBN: 978-3-030-71165-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)