Abstract
There has been a tremendous progress in our understanding of the anatomy, kinematics, and biomechanics of the distal radioulnar joint (DRUJ) in the past 30 years. Along with this understanding, there evolved new methods of managing pathologies of the joint. This chapter summarizes the current understanding of the anatomy and biomechanics of the DRUJ and then discusses the design considerations and scientific basis of the APTIS total distal radioulnar joint replacement system. We also present the surgical technique and briefly discuss our clinical experience and results with this implant along with some case studies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The functional importance of the distal radioulnar joint has been ignored and misunderstood for a long time, resulting in the distal ulna being amputated, fused, and modified in ways that the function of the distal radioulnar joint disappeared, leaving the patient with considerable disability. Historically, it was Claude Bernard in 1851 [1] who published on the resection of the ulnar head, followed by others including Moore in 1880 [2]. Thirty years later Darrach [3] proposed that the resection be made subperiosteal. The failures of the available techniques led Kapandji, whose chief was Sauvé [4] (based on the findings of Baldwin [5] that in cases of ankylosis of the DRUJ, removing a piece of the ulnar shaft could restore pronation/supination), to perform fusion of the distal radioulnar joint with resection of a segment proximal to the head of the ulna and create a pseudoarthrosis at that point to maintain pronation and supination. However, the problem of instability of the end of the ulna persisted albeit at a more proximal level.
In the 1980s and the 1990s, interest in distal radioulnar joint (DRUJ) increased, with studies that allowed us to appreciate kinematics, biomechanics, and anatomy of DRUJ [6,7,8,9,10,11,12,13]. These studies resulted in a better understanding and a reasoned therapeutic approach to the clinical problems that affect the distal radioulnar joint.
Pathologies that affect DRUJ include arthritic problems of inflammatory, degenerative, and traumatic origin, genetic conditions such as Madelung deformity and Ehlers-Danlos syndrome, sports conditions such as epiphyseal arrest of the distal radius found in the gymnast, and arrest of the ulnar epiphysis. The innumerable techniques [14,15,16,17,18,19,20,21,22] that attempt to solve the problems of the distal radioulnar joint available in the literature are an indicator of the lack of a definitive solution to this problem that not only causes pain and functional disability but can also deleteriously affect the patient’s quality of life and health like his/her social function (work, sports activities, relationship with friends and family), physical function, vitality, and even his state of mental function. When applicable, the patient’s inability to return to work further affects his/her economic and mental well-being.
Anatomy and Kinematics
A bicondylar joint connects the radius to the ulna through (1) the annular ligament over the head of the radius, (2) the triangular fibrocartilage complex (TFCC) (Fig. 10.1) that holds the distal radius of the ulnar head, and (3) the interosseous membrane [12]. The distal radioulnar joint is in fact a “hemi-joint,” with the other half being the proximal radioulnar joint (PRUJ).
Any phenomenon that alters the PRUJ or the relative length of the bones of the forearm, or that creates an abnormal angulation, can influence the functioning of the DRUJ whose axis of pronation/supination is formed by an imaginary line that passes through the center of the head of the radius proximally and through the fovea of the head of the ulna distally, such that the distal radius rotates over the ulnar head (Fig. 10.2).
The distal hemi-component of the radioulnar joint consists of bone ends and a ligament-stabilizing system. The head of the ulna and the sigmoid fossa of the radius (Fig. 10.3) constitute the articular bone elements. An important anatomical aspect is that the articular surface of the sigmoid fossa resembles an inverted hemi-cone, which prints a “corkscrew or corkscrew effect” on the head of the ulna during pronation/supination giving rise to an axial piston movement. Thus, during pronation there is a relative shortening of the radius, and as a consequence there is a relative distal axial displacement or “lengthening” of the ulnar head. In supination the opposite happens and there is a relative “shortening” of the ulnar head. In reality, the ulnar head does not move; it is the radius that shortens as it passes over the ulnar head during pronation. The radius also moves palmarly during pronation and dorsally during supination; this movement is the one that tenses the triangular fibrocartilage and limits the angle of movement.
When analyzing the articular surfaces of the DRUJ, it is observed that the sigmoid fossa is shallow with a 60-degree arc while the ulnar head arc is 105 degrees (Fig. 10.4). This makes the joint intrinsically incongruous, so that maximum joint contact exists only during the neutral or zero pronation/supination position. At maximum pronation, the radius moves, and only the deep dorsal ligament maintains it with minimal contact with the ulnar head, which makes the joint susceptible to dorsal subluxation; however, during supination, the contact between the ulna and the radius is increased because the palmar edge of the sigmoid fossa extends toward the ulnar side and the palmar ligament is stronger than the dorsal ligament, so the palmar subluxation is less frequent. It is necessary to remember that when we lift heavy objects, we supinate the forearm so that the biceps and the brachialis work in unison. In neutral or pronation position only, the brachialis flexes the elbow actively. For this reason, the anatomy of the sigmoid fossa has been created with greater contact during supination than during pronation. There are four types of sigmoid notches as described by Tolat et al. [23]: (a) flat face, (b) ski slope, (c) type C, and (d) type S.
The kinematics of the DRUJ during pronation/supination is really complex and far from a simple rotational movement of the radius over the head of the ulna. The combination of movements in the three axes of space (rotation with back-palmar displacement, translation, and axial displacement or piston) is happening concurrently. There is a relative anatomical incongruity of the joint components with a tendency to subluxation in the extreme positions, more in pronation than in supination; the need for a DRUJ stabilizer is evident. This role is played by the triangular fibrocartilage complex (TFCC).
Biomechanics
Many surgical techniques have been developed based on the concept that the main function of DRUJ is pronation and supination [3, 4, 14, 16,17,18,19,20,21]. The rotation of the radius on the head of the ulna is a function that depends on the muscular action and is not directly dependent on the joint itself. Thus, in those patients in whom this joint has been sacrificed by surgical techniques that eliminates the head of the ulna or fuses it and creates a proximal osteotomy, all have pronation and supination despite the fact that the joint has been removed. However, these patients have limited load bearing capacity, and can experience weakness if painful and even activities like lifting a glass of water can be affected. As we discussed earlier, elbow flexion and therefore weight lifting against gravity are functions of the brachialis muscle, which is inserted distal to the coronoid process. This muscle flexes the elbow in all positions of pronation and supination; however, the biceps muscle only flexes the elbow once it passes from the neutral position to the supination, and its maximum flexion force of the elbow is after complete supination. The brachioradial muscle or long supinator is only activated by trying to avoid the extension of the elbow, either with co-contraction with the triceps or by load against gravity.
Hagert in 1992 demonstrated for the first time that the main function of the DRUJ is to support weight and transmit these forces to the elbow through the ulna [12]. Thus, the hand together with the radius forms a functional unit that rests on the head of the ulna, which is “the cornerstone” that supports the weight. In the neutral position of rotation of the forearm, there is maximum articular contact between the bone ends. Hagert [11] demonstrated in cadavers that after eliminating the ulnar head, the distal end of the osteotomized ulna takes the place and function of the ulnar head. Consequently, there was a convergence and contact of the ulna toward the radius when a weight was applied.
This new concept of load articulation of the DRUJ has morphological correlation when analyzing the trabecular arrangement of the distal end of the ulna. Under normal conditions there is a close relationship of the trabecular pattern of the bone and the function it performs according to Wolff’s law. Bone loading areas are characterized by a decrease in the spongy pattern with the trabeculae condensing at the cortical level. These findings agree with Hagert’s theory that the ulnar head is the support point of the functional unit that forms the hand with the radius.
How is the load transmitted during prone/supination? As we saw earlier, in the extreme positions of pronation and supination, there is a tendency of subluxation of the radius in relation to the head of the ulna with little contact between the bone surfaces. If, in these situations, a load is applied (to hold a weight), dislocation would necessarily occur if the ligament components of the TFC did not come into play. The initial studies of Ekenstam and Hagert [24] on the functioning of the ligaments of the DRUJ found that the palmar radioulnar ligament tensed in pronation while the dorsal radioulnar ligament tensed in supination. Subsequently, Acosta et al. [11] showed that the ligaments that were inserted in the fovea had a totally different function. During the neutral state of rotation, in which there is maximum contact between the articular surfaces of the DRUJ, both ligament components of the TFC were in a relaxed position. As pronation was established and contact between articular surfaces with a tendency to subluxation of the distal radius was reduced following the force of gravity, the dorsal ligament component of the TFC tightened, being maximal in the extreme pronation position. During the supination, the findings were compatible; it was the palmar component that tensed.
The theory of DRUJ as a load bearing joint would be summarized as follows: in a neutral state of rotation, the large part of the load is supported by joint surfaces, in pronation where this bone contact is minimal and there is a tendency to palmar subluxation of the distal radius, the load is transmitted mainly through the dorsal component of the tightened TFC, and it undergoes stretching with deformation that is measurable, and subsequently transmits the load to the rest of the ulna. The opposite would happen during supination. Recent observations by the authors in fresh cadavers and in patients who suffered disarticulation of the wrist due to different causes showed that the previous theory can be more complex if the two components (superficial and deep fascicle) of the TFC ligaments are considered (Fig. 10.5). Probably, the tension of the dorsal ligament (deep fascicle) during pronation and the palmar (deep fascicle) during supination is the main element in the stabilization of the DRUJ. But the superficial fascicles, with less stabilizing role, may complement and help in stabilization. Thus, during pronation the deep dorsal fascicle is tensioned, which prevents palmar displacement of the radius, and the palmar superficial fascicle is wrapped around the styloid, exerting a blocking effect that supports and prevents the displacement of the radius toward the dorsum. The opposite would occur during supination, with the deep fascicle of the palmar ligament being the main actor and the dorsal superficial fascicle the secondary actor that helps in stabilization of the DRUJ.
Design Considerations
Milch [25] recognized that amputating the head of the ulna because of length difference was not a good idea and reported removing a segment of the ulna shaft to correct this problem. In spite of his report, the procedures of Darrach [3] and Sauvé-Kapandji [4] were augmented in 1986 by Bower [16] and Watson et al. [17].
Recognition of the impingement syndrome by Bell et al. [26] and the demonstration of the dynamic impingement by Lees and Scheker [27] have shown that when the ulnar head is excised, the radius is going to fall off the stump of the ulna regardless of the procedure (Fig. 10.6 a, b, and c). To solve the impingement problems, a myriad of unipolar implants that required ligament reconstruction and the presence of the sigmoid notch were created. A large number of implants eroded into the ulnar part of the radius with loosening and dislocation of the implants.
The sigmoid notch can present with varied orientation as shown by the works of De Smet and Fabry [28] and different shapes as shown by Tolat et al. [23]. This anatomical peculiarity reduces the longevity of the hemiarthroplasties.
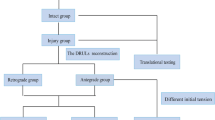
Confronted with patients with radioulnar impingement after salvage procedures and others with severe forearm injuries where the sigmoid notch and the radioulnar ligaments were absent where the surgical solutions were inadequate, we designed an implant that would work in conditions where there were no sigmoid notch and no radioulnar ligaments.
There was a need of an implant that would be self-stabilizing, maintaining the total range of motion and allowing weight bearing.
The original implants were made of stainless steel with an ulnar stem of 3 mm in diameter and 22 centimeters long and three-point fixation. In a subsequent modification, cobalt-chrome alloy is utilized to construct the implant, where the function of the sigmoid notch is replaced by a metal plate that contours to the ulnar border of the radius and has a distal hemi-cavity. The ulnar head function is replaced by an ulnar stem which is press fit to the ulnar medullary cavity. It has a titanium plasma spray on its distal third for bone ingrowth inside the ulnar canal and has a highly polished Morse-taper peg distally where an ultra-high molecular weight polyethylene (UHMWPE) ball is placed, which sits in the hemi-cavity, and a cover that completes the assembly.
The total Aptis arthroplasty is composed of four elements (Fig. 10.7):
-
1.
Radial plate with 3, 4, or 5 holes depending on whether the small, medium, or large plate is used. The plates have at their distal end a small peg (radial side) that helps to position it correctly and a hemisphere (ulnar side). The plates, of three sizes, are pre-molded to be placed on the ulnar face of the radius, in 6–7 cm distal to the interosseous crest. The fixation to the radius is achieved by means of its small peg, which is introduced in the ulna-radial direction and through the holes of the plate by means of 3.5-mm screws.
-
2.
Cover with a transverse screw, which will serve as a cover to the hemisphere of the radial plate.
-
3.
Ulnar head made of ultra-high-density polyethylene.
-
4.
An 11-cm ulnar stem, long and with porous titanium coating on its distal third to facilitate bone incorporation. The stems have a polished extension between the base of the ball and the porous coating part to prevent the escape of bone marrow that in the past created ectopic bone (Fig. 10.8). The rod is ribbed to allow greater rotational stability and is slightly tapered to facilitate insertion. Also, at the distal end of the stem, that is, outside the ulna, a pin is incorporated, to which the prosthetic ulnar head is fitted. The ulnar stem is available in four diameters, with different neck lengths, which will be used mainly in cases where the distal ulna has been lost or it is necessary to resect a greater amount of distal ulna. Thus, the articular surface of the prosthesis is made up of the aforementioned ultra-high-density polyethylene head, inserted into the plug of the ulnar stem, and the metal surface of the plate and cover hemispheres, respectively.
The design of the implant allows full range of pronation and supination, radial migration, lifting capacity, and variable angle of rotation, and it is self-stabilizing. The implant comes in three sizes, small locking (number 10), medium locking and unlocking (number 20), and large unlocking (number 30). The stems are available in 4 diameters from 4, 4.5, 5, and 6 mm, and the length of the collar of the stems is 1–4 cm for those cases with much distal ulna excised. Originally only those cases missing the ulnar head were treated with implants, as we gained experience with its behavior; we included primary osteoarthritic patients, cases of rheumatoid arthritis, post-tumor resection, and congenital conditions like Ehlers-Danlos and Madelung deformities.
Surgical Procedure
The procedure is generally accomplished under axillary block. An iodine plastic wrap is used to avoid contact between the implant (the stem specially) and the skin. A tourniquet is applied for visualization. A 10-cm longitudinal incision in the shape of a hockey stick is made along the ulnar border of the distal forearm, in the interval between the fifth and sixth dorsal compartments, 8 cm over the distal forearm, and 2 cm distally oblique from ulnar to radial. Care is taken to avoid damage to the sensory branch of the ulnar nerve. The skin and subcutaneous flap are elevated from the forearm fascia up to the radial wrist extensors. A rectangular ulnar-based fascia/retinacular flap is created with enough width to cover the head of the implant; it includes the most proximal 3 mm of the extensor retinaculum. This flap will be used later to create a buffering barrier between the prosthesis and the extensor carpi ulnaris (ECU). The dissection is continued between the extensor digiti quinti minimi and the ECU until the ulna is encountered and the extensor digiti quinti minimi is elevated from the ulna together with the extensor indicis proprius (EIP); this leads us to the dorsum of the interosseous membrane which is exposed. The sensory branch of the posterior interosseous nerve is divided to avoid avulsion of the nerve from the thumb. The extensor communis is elevated by placing an elevator between the extensor mass and the radius. The ECU tendon sheet is opened completely up to its insertion at the base of the fifth metacarpal. This avoids pressure of the tendon against the distal end of the implant. The remaining head of the ulna, if present, is then excised 2 cm from the distal end of the ulnar head. At this stage, the radial attachment of the triangular fibrocartilage, if found intact, is left undisturbed. If left in situ, this structure can provide a barrier between the prosthesis and the carpal bones. The ulnar shaft is then retracted volarly, thus ensuring access to the radius. The interosseous membrane is elevated from the radius along the distal 8 cm of the interosseous crest. The radial trial plate is then placed over the interosseous crest of the radius, and its volar border is aligned with the volar surface of the radius. Care is taken to ensure that at least 3 mm of the sigmoid notch lies distal to the end of the plate. Depending on the anatomy encountered, the distal radius may require contouring. Often the volar lip of the sigmoid notch has to be removed with a saw blade or a medium-sized burr ball to create a flat surface to ensure proper seating of the radial plate. After the position of the trial plate has been deemed appropriate—meaning parallel to the volar shaft of the radius and at least 3 mm proximal to the end of the radius—a 1.4-mm (0.054-in) K-wire is inserted in one of the holes at the distal end of the trial as well as the most proximal hole. An image intensifier is used to check the position of the trial, both in anteroposterior and lateral positions. If no adjustment is needed, a 2.5-mm drill bit is used with the provided guide to drill the screw hole at the oval opening, the proper screw length is gauged, the hole is tapped, and the appropriate length 3.5-mm screw is placed. The image intensifier is used again to confirm plate positioning and proper screw length. With confirmation of the length of the screw and good plate contact with the bone, the distal K-wire is removed, and the hole for the radial peg is drilled with appropriate drill bit. When the surgeon is satisfied, the trial component is removed, the area profusely is irrigated, and the prosthesis radial component is installed. If necessary, a soft mallet is used to achieve good contact between the radial plate and the ulnar border of the radius. After the last screw is placed in position, a final check of the radial plate to confirm screw length and position is performed with the image intensifier. Attention is now turned to the ulna. With the forerarm fully pronated, a measuring device with an appropriate colored ball (blue for large implant; black for medium sized and small implants) is positioned such that the ball is fitting into the hemi socket of the radial component and the measuring device is juxtaposed aginst the ulnar shaft. This enables the surgeon to assess the exact amount of ulna to be resected. After final resection of the distal ulna, a 2.3-mm (0.090-in) guide wire is inserted into the ulnar medullary canal to act as a centralizer for a cannulated drill bit of the predetermined size. It is important that the guide wire surpass the length of the drill bit to avoid penetrating the ulnar cortex. The cannulated drill bit is introduced for a length of 11 cm. Next, a medullary broach of appropriate size is inserted into the canal to bevel the distal ulna and plane its distal end. The medullary canal is now thoroughly irrigated, and the stem of the ulnar component is introduced leaving the polished peg showing distal to the rim of the socket. The UHMW polyethylene ball is placed over the distal peg or pivot, and the ulnar component is positioned within the hemi-socket of the radial component. Finally, the other half of the radial socket or cover is positioned and secured with a transverse screw. The image intensifier is once again used to confirm adequacy of the overall position. Full range of motion is confirmed. The fascia/retinacular flap is placed between the prosthesis and the ECU tendon and sutured to the radius. This prevents tenosynovitis of the ECU and provides a cushion over the implant, especially for a patient with little subcutaneous adipose tissue. The tourniquet is released, and complete hemostasis is secured. The skin is then closed with interrupted sutures and a bulky soft dressing is applied.
Postoperative Protocol
The wound is kept dry and clean in a bulky soft dressing for 2 weeks, at which time the skin sutures are removed. Immediate full range of motion is encouraged. Lifting is allowed as soon as the patient has recovered from the anesthetic, and after full recovery is limited to 20 lb (9 kg). In vitro testing showed that ultimate load to failure was between 148 and 186 lb with an average of 169 lb (76 kg), at which point the highly polished peg and the end of the ulna stem bent. By limiting lifting to no more than 20 lb, the patient has a margin of safety of seven times.
Results (Figs. 10.9 and 10.10)
Our combined cases surpass 400 patients; of those 263 have more than 5 years of follow up, and 128 had more than 2 procedures before the total DRUJ was implanted. The average preoperative grip strength measured with a dynamometer (Jamar II, Jamar Dynamometer, Bolingbrook, IL) was 38.3 lb (17.4 kg) on the affected side and 70 lb (32 kg) on the opposite side. The postoperative grip strength increased to a mean of 44.5 lb (20.2 kg) on the operated side. Mean postoperative grip strength, evaluated with a dynamometer (Jamar II, Jamar Dynamometer), was 63.4% of the contralateral unaffected side. Before surgery, patients could lift an average of 2.6 lb (1.2 kg) with the affected side, limited by pain; after surgery, they were able to lift an average of 11.6 lb (5.3 kg). Patients subjectively scored preoperative pain on a scale from 0 to 5 at an average of 3.8, and postoperative pain at a mean of 1.3. Mean pronation was 79° (range 15–90°) and mean supination was 72° (range 30–90°) at final follow-up. Seventy percent of our patients have had at least one previous procedure; some had failed “ulna stabilization” with tendon sling procedures, allograft tendon interposition, and failed ulnar head replacement. Of this group of patients, 1 had 14 previous procedures. Most of these patients have been incapacitated for a prolonged period of time because of pain. This has led to a lack of use, causing muscle atrophy in both the arm and the forearm. For this reason, these previously operated patients were often weaker than those who received the device as their first procedure or those on whom the replacement was performed shortly after the failed previous procedure. Rampazzo et al. [29] noticed while evaluating those patients with implants under the age of 40 years that when the implant was performed, primarily the results were much better in regard to postoperative pain, strength, and speed of recovery. Postoperative complications were seen in 26 cases. Two patients had low-degree soft tissue infection that resolved with antibiotic treatment. Both patients had multiple previous operations. Two patients had ECU tenosynovitis due to too large implant; now we have a smaller implant for those cases. This was successfully treated by creating a fascial flap that was interposed between the implant and the ECU tendon. A fascial flap is now performed routinely at the initial implantation surgery. Eight patients had ectopic bone formation around the distal ulna and were treated successfully with surgical excision. This ectopic calcification was caused by the bone marrow escaping around the original stem that had no extended collar. After the stem had 1-cm extended collar, the ulnar canal is sealed, and no other cases of ectopic bone have been seen. Of the patients with ectopic bone formation, six patients had ECU tendinitis that settled after excision of the ectopic bone . One patient, at the 1-year follow-up X-ray, was noticed to have some ulna resorption in the distal segment of the ulna where she had an ulna shortening 6 months before the replacement arthroplasty. At present, the ulna stem remains well secured and she is symptom-free.
(a) This patient had wrist arthrodesis with wide excision of the distal ulna. There is no radioulnar impingement in the unloaded position. (b) However, with load bearing, there is radioulnar impingement that causes pain and weakness of grip. (c) Radiograph of DRUJ replacement arthroplasty with Aptis implant showing the implants in good alignment. (d, e, and f) The patient is now able to lift weights that he was unable to do
(a and b) This young patient underwent attempted bilateral Sauvé-Kapandji procedures with severe disability. (c) Radiographs showing bilateral Aptis total distal radioulnar joint implants. (d and e) Full restoration of function with load bearing capacity was possible after Aptis total distal radioulnar joint replacement arthroplasties
At the time of this writing, the longest follow-up with the Aptis DRUJ prosthesis is 15 years. No prosthesis had to be removed because of excessive wear, loosening, or material failure. There have been four implants removed because of unknown preoperatively allergy three to nickel and one to cobalt-chrome and three due to late infections, requiring those of allergies to be replaced by implants made of titanium. Those with infections were treated by removing the implants, extensive curettage, and bone substitute with antibiotic inserted in the defects, replacing the implants 3–6 months later. Galvis et al. [30] reported excellent recovery in cases of rheumatoid arthritis with dislocated distal radius and ruptured tendons. The Aptis DRUJ prosthesis is an alternative to the other salvage procedures that allows full range of motions as well as the ability to grip and lift weights encountered in daily living.
Conclusions
The distal radioulnar joint is a weight bearing joint and together with the proximal radioulnar joint forms a complete unit that helps in load transmission from the hand and wrist to the elbow. Although the ability to pronate and supinate is important, it has the ability to lift loads that helps better define function. When this joint is affected by injury or disease, it is important to reconstruct the DRUJ and restore the loading capacity of the joint. The Aptis total distal radioulnar joint replacement system was designed to help in restoring the load bearing capacity of the forearm, and our clinical experience shows that it has been successful in this endeavor.
References
Bernard CH, Huette CH. In: Buren WHV, Isaacs CE, editors. Illustrated manual of operated surgery and surgical anatomy. New York: HBailliere; 1857.
Moore EM. Three cases illustrating luxation of the ulna in connection with Colles’ fracture. Med Record. 1880;17:305.
Darrach W. Forward dislocation at the inferior radio-ulnar joint with fractures of the lower third of radius. Ann Surg. 1912;56:801.
Sauvé L, Kapandji M. Nouvelle technique de traitement chirurgical des luxations récidivantes isolées de l’extrémité inférieure du cubitus. J Chir. 1936;7:589.
Baldwin W. Orthopaedic surgery of the hand and wrist. London: Henry Frowde, Hodder & Stoughton; 1921. p. 241–82.
Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist- anatomy and function. J Hand Surg. 1981;6A:153–72.
Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop. 1984;187:26–35.
Thiru RG, Ferlic DC, Clayton ML, McClure DCT. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg (Am). 1986;11(2):258–63.
Mikic ZD. Detailed anatomy of the articular disc of the distal radioulnar joint. Clin Orthop. 1989;245:123–32.
Chidgey LK. Histologic anatomy of the triangular fibrocartilage. Hand Clinic. 1991;7:249–62.
Acosta R, Hnat B, Scheker LR. Distal radio-ulnar ligament motion during supination and pronation. J Hand Surg. 1993;18B:502–5.
Hagert CG. The distal radioulnar joint in relation to the whole forearm. Clin Orthop. 1992;275:56–64.
Linscheid RL: Biomechanics of. the distal radioulnar joint. Clin Orthop. 1992;275:46–55.
Kessler I, Hecht O. Present application of the Darrach procedure. Clin Orthop. 1970;72:254–60.
Tsai TM, Stillwell JH. Repair of chronic subluxation of the distal radioulnar joint (ulnar dorsal) using flexor carpi ulnaris tendon. J Hand Surg. 1984;9B:289–94.
Bowers WH. Distal radio-ulnar joint arthroplasty: the hemi-resection interposition. J Hand Surg. 1985;10A:169–72.
Watson HF, Ryu J, Burgess RC. Matched distal ulnar resection. J Hand Surg. 1986;11A:812–7.
Breen TF, Jupiter JB. Extensor carpi ulnaris and flexor carpi ulnaris tenodesis of the unstable distal ulna. J Hand Surg. 1989;14A:612–7.
Leslie BM, Carlson G, Ruby LK. Results of ECU tenodesis in rheumatoid wrist undergoing a distal ulnar resection. J Hand Surg. 1990;15A:547–51.
Sanders RA, Frederick HA, Hontas R. The Sauvé-Kapandji procedure: a salvage operation for the distal radio-ulnar joint. J Hand Surg. 1991;19A:1125–9.
Tsai TM, Shimizu H, Adkins P. A modified extensor carpi ulnaris tenodesis with Darrach procedure. J Hand Surg. 1993;18A:697–702.
Scheker LR, Severo A. Ulnar shortening for the treatment of early Post-traumatic osteoarthritis at the distal Radioulnar joint. J Hand Surg. 2001;26B(1):41–4.
Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg Br. 1996;21(5):587–94.
af Ekenstam FW, Hagert CG. The distal radioulnar joint. The influence of geometry and stability of the distal radioulnar joint. Scand J Plast Reconstr Surg. 1985;19:27.
Milch H. So called dislocation of the lower end ulna. Ann Surg. 1942;116:282–92.
Bell MJ, Hill RJ, McMurtry RY. Ulnar impingement syndrome. J Bone Joint Surg. 1985;67B:126–9.
Lees VC, Scheker LR. The radiological demonstration of dynamic ulnar impingement. J Hand Surg. 1997;22B:448–50.
De Smet L, Fabry G. Orientation of the sigmoid notch of the distal radius: determination of different types of the distal radioulnar joint. Acta Orthopaedica Belgica. 1992;59(3):269–72.
Rampazzo A, Gharb BB, Brock G, Scheker LR. Functional outcomes of the Aptis-Scheker distal radioulnar joint replacement in patients under 40 years old. J Hand Surg Am. 2015;40(7):1397–403.
Galvis EJ, Pessa J, Scheker LR. Total joint arthroplasty of the distal radioulnar joint for rheumatoid arthritis. J Hand Surg Am. 2014;39(9):1699–704.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gupta, A., Scheker, L.R. (2021). Design Considerations for Distal Radioulnar Joint Arthroplasty. In: King, G.J.W., Rizzo, M. (eds) Arthroplasty of the Upper Extremity. Springer, Cham. https://doi.org/10.1007/978-3-030-68880-6_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-68880-6_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-68879-0
Online ISBN: 978-3-030-68880-6
eBook Packages: MedicineMedicine (R0)