Abstract
Climbing is one of the fastest growing sports world-wide. As the sport continues to grow and climbers are more frequently seen in orthopedic clinics it is important to understand the injuries associated with climbing. The majority of injuries are not from falls but from overuse and over training and most commonly occur in the upper extremities. Injuries can be categorized into acute and chronic. This chapter will cover both the acute and chronic injuries associated with climbing. We will provide a context for how these injuries occur for those not familiar with the sport and discuss the treatment options.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Climbing is one of the fastest growing sports world-wide with up to 44.5 million climbers according to the International Federation of Climbing in their 2019 annual report [1]. With the recent addition of climbing to the 2020 Olympic Games, the popularity of the sport is only continuing to grow. Climbing is a sport that may be practiced across generations. Many climbers start out in childhood and may continue the sport well into their 70s or more. Genders are equally represented throughout the different disciplines and the scope of difficulty of any particular discipline can be extremely broad. Climbers as a group are highly detail oriented and deeply in-tune with their bodies similar to ballet dancers or violin players, and are focused on maximizing their body’s potential. The sport often requires extreme and technical body positions which can push the body’s limits.
Unlike the fields of play in many sports which are relatively controlled regarding environmental conditions, climbers may face an incredible array of climate and environmental hazards. For example, most climbing competitions are held indoors or on protected, specially constructed man-made walls with artificial holds where environmental conditions are well controlled and rarely play a role in the execution of the sport. On the other hand, Alpine mountaineering, ice climbing, and traditional climbing may take place in austere settings where extremes of temperature, altitude, and remoteness may significantly increase objective danger (Fig. 14.1). Additionally, this sport is often practiced in extremely remote international locations where first responders and rescue may be limited or non-existent. Therefore, climbing, as opposed to other more traditional sports, requires the participant to be their own first responder in the event of an injury and indeed, many climbers are highly trained as first responders.
Climbing encompasses several different disciplines all which have their own unique spectrum of injury. These different types of climbing may be broadly grouped into the following categories: Sport climbing and competition, traditional (trad) climbing, ice climbing, Alpine mountaineering, and bouldering. The various types carry their own risk categories. For instance, sport climbing and indoor climbing is relatively controlled with attachments to secure equipment and controlled surfaces, while traditional alpine climbing, or ice climbing, for example, has more risk, and more injuries due to the unpredictability of the terrain and the environments involved [1, 2]. Bouldering, while performed low to the ground, does not utilize ropes and can consequently have the highest risk of falls and traumatic lower extremity injuries. Additionally, bouldering involves more explosive positions and higher loads and can therefore lead to more tendinopathies and overuse injuries as well. Climbing is generally performed with a belayed rope attached to another person, or to equipment that acts as a safeguard in the event of a fall. The majority of falls in climbing are wall collisions rather than ground falls, which is contrary to public perception [3]. A wall collision is when the climber falls a short distance, is caught by their safety belay rope, then swings into the wall, colliding side on with the wall. A ground fall is, as it sounds, a fall from height on to the ground.
The tendency to view climbing as a reckless or overly dangerous sport is a common misconception. There are a reported 4.2 injuries per 1000 h of climbing, compared to 15.7 and 9.8 injuries per 1000 h in football and basketball, respectively [4,5,6]. Different climbing environments effect this rate; indoor climbing, for instance, only has a reported injury rate of 0.2 injuries per 1000 h [7].
Injuries in rock climbing can be divided into acute and chronic. While some acute injuries do result from falls, others are due to the unique stresses and positions of climbing and unrelated to falls all together (Fig. 14.2). Chronic or overuse injuries are exceedingly common in climbing with over 2/3 of participants reporting an overuse injury requiring treatment during their career [8]. Up to 75% of all climbing injuries, acute and chronic, involve the upper extremity, with 60% of those involving the hand or fingers [9]. In the following chapter, we will review the common acute and chronic injuries specific to climbing as well as address treatment tips for caring for the climbing athlete.
2 Acute Injuries
2.1 Hand
Tendon injuries account for 52% of all hand/finger injuries in climbers [10]. Lacerations are also common at 15% of reported injuries. Fractures can occur during falls with 12% involving the wrist and 7% involving the fingers [11].
While it is easy to understand how fractures may be associated with falls, acute injuries to the tendons require an additional understanding of climbing. Climbers utilize multiple specialized grips to maintain contact with the climbing surface and facilitate movement. The type of grip a climber uses depends on the size and shape of the available hold and the climbers body positions. See Fig. 14.3 for images and descriptions of some of the common grip positions.
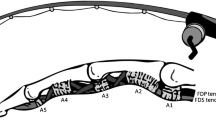
Pulley ruptures are common in climbers affecting approximately 25% of elite climbers [10, 11]. This is understandable when considering studies demonstrating that crimp and hanging grip positions can lead to forces in excess of 450 N on the A2 pulley and 269 N on the A4 pulley [12, 13], with reported forces required to rupture the pulley of only 400 N and 137 N, respectively, for the A2 and A4 pulley [14,15,16,17]. A pulley rupture can often be felt as a pop with pain at the time of injury. The climber will present with pain and swelling over the volar surface of the finger and point tenderness at the site of injury. If the A2 or A4 pulley is completely ruptured, bowstringing of the tendon may be seen with resisted flexion.
MRI is the most common imaging modality for diagnosing pulley injuries although ultrasound also has value in providing a dynamic exam. On MRI, a ruptured pulley can result in volar displacement of the tendon from the underlying phalanges by greater than 2 mm [11].
Conservative treatment is often adequate for grade I–III injuries with an initial immobilization period of 10–14 days in a volar splint followed by functional therapy with putty or compression balls utilizing pulley protection with tape or thermoplastic splints. Sporting activities can typically resume in 6–8 weeks after a grade III injury. Surgical reconstruction is only indicated for grade IV injuries with multiple described techniques in the literature [18, 19] (Table 14.1).
2.2 Shoulder
Shoulder dislocations with bankart lesions, SLAP tears, or posterior labral tears can occur in rock climbing. While many of these lesions can be treated conservatively, it is important to acknowledge the extreme risk a potential subsequent dislocation or instability event may have in rock climbers, possibly causing them to fall and suffer an injury or be unable to regain hold on the wall due to their dislocated shoulder. We characterize these athletes as consequence athletes, meaning that the consequence of the dislocations may be worse than the dislocation itself.
Posterior labral tears associated with shoulder pain that limit activity are treated with a short course of physical therapy, then surgery if not resolved in 4–6 weeks. Bankart lesions in first time dislocators without bone loss are often treated more aggressively with operative labral repair in order to prevent future dislocations and potential bone loss in this population which places high demands on their upper extremities. However, if there is any concern for bone loss, we are aggressive at recommending a Latarjet procedure for these injuries. Arthroscopic bankarts have an average failure rate ranging from 10% to 20% [20] in the literature, while the Latarjet is consistently reported at 2–5% [20]. In the climbing population with the severe risks associated with subsequent dislocation as mentioned above, the reduced failure rate of the Latarjet is especially appealing. In our practice, there have been no limitations to the functional abilities of even the most elite climbers, and the procedure has consistently low failure rates.
Many asymptomatic climbers may have SLAP tears on MRI and treating physicians should be careful attributing pain to this finding. However, true symptomatic SLAP tears in climbers can occur. While some may occur acutely, the majority of these are due to repetitive microtrauma similar to other competitive overhead athletes [21, 22]. Operative treatment of SLAP tears in overhead athletes have inconsistent results with return to sport rates ranging from 22% to 75% [23]. Rather than a repair, climbers with symptomatic SLAP tears are at times better treated with a tenodesis of the long head of the biceps tendon. In our practice, we prefer a robust construct for this population. We perform a mini-open subpectotal tenodesis with a biceps button, backed up with a tenodesis screw.
Other common shoulder pathology in climbers are AC joint sprains, muscle strains of the latissimus dorsi, rhomboid, or trapezius [24]. These can generally be treated with functional therapy. Ruptures of the long head of the biceps have been reported, and these are often best addressed with an open tenodesis though some patients may do well with non-surgical management.
2.3 Elbow
Elbow pain is the third most common complaint of elite rock climbers [25]. Acute “climber’s elbow” is defined as tears of the brachialis muscle at the muscle-tendon junction [26]. These tears present as pain in the cubital fossa. They can be distinguished from ruptures of the distal biceps by resisted elbow motion. Pain on resisted flexion with forearm in supination is due to biceps injuries, while pain with resisted elbow flexion with the am in pronation is due to a brachialis injury [25]. Climbers should focus on pull-ups with the forearm pronated during training to help strengthen the brachialis and prevent these injuries. Acute, complete tears of the brachialis can be diagnosed with MRI and should be treated surgically. Repair is ideally performed within 1–2 weeks, patients are then placed in a splint at 90° for 1 week, and progressive extension is accomplished with an elbow brace over the next 8 weeks.
3 Lower Extremity
While upper extremity injuries are more common in rock climbing overall, the lower extremities are more likely to suffer fractures due to ground or wall falls [27, 28]. Falls from as little as 8 ft can lead to fracture of the calcaneus, talus, or ankle joint [27]. Ligamentous injuries such as ankle sprains are also common [29, 30]. These injuries are particularly common in bouldering, but can also occur in indoor or sport climbing if the athlete falls before reaching the first security attachment for their rope, or are dropped by their belayer [27].
3.1 Knee
Knee injuries are less common in climbing [10, 31]. While ligament tears and fractures can occur with fall, the majority of knee-related injuries are due to the extreme positions required in climbing. The high step position, the drop knee position, and the heel hook have been identified as especially hazardous for the climber’s knee [32]. In the high step position, the athlete’s weight is mostly on one leg which is position in maximum knee flexion with a flexed, externally rotated and adducted hip. The drop knee is a similar knee position with an internally rotated hip. The heel hook position uses the heel to apply pressure on a hold while pulling on the foot by flexing the knee via strong hamstring contraction [32] (see Fig. 14.4).
Medial meniscus tears are the most common knee injury with a reported incidence of 28% [32]. These occur predominately in the high step and drop knee positions. IT band sprains represent 19.5% of knee injuries and occur exclusively in the heel hook position [32].
The heel hook position is a cause of posterior cruciate ligament (PCL) injuries in climbers [33]. While PCL injuries generally occur with a posterior directed force on a flexed knee [34], the heel hook position places extreme load in an anterior to posterior direction on a slightly flexed or even hyper extended knee and can overload the PCL.
In addition to PCL injuries, proximal tibial-fibular joint (PTFJ) injuries have been associated with the heel hook position. PTFJ injuries have a wide array of presentations from frank dislocations, to discomfort during activity, or symptoms related to irritation of the common peroneal nerve [35,36,37]. The common mechanism for injuries to the PTFJ are falling onto a flexed knee or excessive rotation of the knee with the foot planted on the ground. However, the heel hook position leads to extreme loading of the lateral knee with forced external rotation of the leg and also places the PTFJ in its most susceptible position [37, 38]. Physical exam can diagnose PTFJ instability. With the knee flexed to 90° to relax the LCL and biceps femoris, the fibular head is held between the thumb and index finger and translated anterolaterally [39]. Instability is usually encountered in the anterior direction as the posterior ligamentous complex is structurally weaker and more susceptible to injury [35, 39, 40]. Lateral and AP radiographs can help diagnose a frank PTFJ dislocation; however, MRI can be useful to confirm the diagnosis in the setting of more subtle instability. The MRI may show joint effusions of the PTFJ, bone edema at the proximal tibia, or visible ligamentous disruption of the posterior tibiofibular ligament [40]. PTFJ instability can be treated conservatively with protected weight bearing and bracing; however conflicting results have been reported with up to 23% of patients failing non-operative treatment [37]. Operative treatment is indicated when conservative measures have failed or in cases of frank and irreducible dislocations. Our preferred reconstruction technique is with bone tunnels in the fibular head and proximal tibia using a hamstring autograft or allograft fixed with tenodesis screws to reconstruct the posterior tibiofibular ligament.
3.2 Ankle/Foot
Fractures of the ankle, heel, and foot are common in climbers as mentioned above. These injuries should undergo standard orthopedic treatment guidelines for fractures. Many of them will require surgery considering climbers are mostly young, highly active patients with high functional demands [27].
Peroneal tendon dislocations are rare injuries, but can be seen in rock climbers [10, 27]. Patients present with pain at the lateral ankle and often report an audible pop with the foot in plantar flexion and maximum inversion, while placing extreme forces on the big toe while climbing—the pop is from a traumatic rupture of the peroneal retinaculum. Climbers generally do not tolerate conservative treatment of these injuries and operative repair is indicated [41, 42]. In acute cases, direct repair of the retinaculum is often possible, and a periosteal flap can be utilized to bolster the repair if required [27]. Patients are immobilized for 6 weeks postoperatively and can begin climbing activities again at 8 weeks.
4 Chronic Injuries
The majority of injuries in climbing are chronic overuse injuries [8, 43]. Much of this is related to excessive climbing specific training without adequate rest and recovery between training sessions [44]. Older climbers may be more susceptible to these injuries [45]; however, as climbing becomes more popular and younger climbers begin to specialize at an earlier age, additional chronic injuries are emerging in the younger population from early specialization [46].
4.1 Hand/Wrist
Tendonitis of the hand and wrist is the most common injury reported in climbers [10, 45]. Pain at the wrist or forearm can be diagnosed on exam based on knowledge of tendon insertion sites. The most common tendons involved are the FDP and FDS although FCU tendonitis is also common [25]. Chronic tendonitis can lead to hypertrophic tendons, and commonly results in carpal tunnel syndrome, reported in up to 25% of elite climbers [47].
Digital collateral ligament strains are common in high frequency climbers due to excessive torsion in certain grip positions. Once strained, the collateral ligaments rarely return to their same level of tension and stability [25]. Buddy taping to adjacent digits can help provide support to the injured collaterals as well as prevent the offending position. Chronic collateral ligament injury and subsequent IP joint instability leads to early IP joint OA seen frequently in climbers. Climbers will frequently present with IP joint effusion and early spurring and other signs of OA on imaging [47, 48]. While OA of the digits is seen commonly at the DIP joint in the general population, climbers may develop this characteristic swelling and fixed flexion at the PIP joint and at an early age.
Extensor hood syndrome is a constellation of arthritic changes affecting the tendon sheaths of the fingers [3]. Extensive climbing can predispose to OA of the digits, leading to bone spurs of the IP joints irritating the tendons and further exacerbating the tendonitis [49]. This generally presents with tenderness to palpation dorsally at the extensor hoods and is commonly accompanied by joint swelling, as well as 3–5° of extensor lag [50]. It is treated conservatively with rest, NSAIDs, and occasionally injections.
Young climbers, especially those doing excessive climbing or finger training for climbing, are susceptible to epiphyseal fractures of the phalanges [10]. They occur most frequently at the PIP joints, and the patient may present with pain or tenderness at the dorsal aspect of the joint [51]. Young climbers rarely report an acute traumatic event when diagnosed with these injuries, leading to the theory that the fractures are stress related and possibly the result of repetitive microtrauma and overloading the developing joint [46]. Injuries identified less than 4 weeks old are treated with 3 weeks of splinting followed by functional therapy. When identified over 4 weeks, malunions or fibrous unions can lead to complete separation of the epiphysis from its attachments and chronic deformity [46]. When identified late, there is no indication for splinting, and these epiphyseal fractures can be treated with rest and functional rehab only.
4.2 Elbow
Medial and lateral epicondylitis are both common in climbers and reported as a frequent cause of discomfort, especially in older climbers [45]. Similar to the general population, conservative treatment is typically successful with rest, bracing, and therapy. Chronic epicondylitis can lead to hypertrophy and occasionally nerve entrapment syndromes at the elbow [3].
Acute “climber’s elbow” was described in the previous section as an acute rupture of the brachialis muscle. Chronic “climber’s elbow” is also prevalent and is a result of a constellation of tendinopathies. Strenuous traversing climbs or any route requiring strong and prolonged flexion and pronation of the elbow with insufficient biceps brachii activation leads to compensatory firing of the brachialis and can lead to tendonitis [52]. Pain is again at the anterior elbow with flexion in a pronated forearm position. Treatment is conservative with rest for 2–4 weeks with resumption of low intensity climbing. When symptoms resolve and a gradual increase in intensity as tolerated [3, 25, 52].
Elbow osteoarthritis is common and can present at a young age in active climbers. The mechanism is likely similar to that seen in finger joints in climbers with repetitive microtrauma leading to progressive cartilage damage and destruction of the articular surface. In this active population, elbow arthritis can lead to limitations in motions with flexion contractures, and pain with terminal extension. As in the general population, treatment is conservative focusing on rest, anti-inflammatory medications, and therapy to strengthen the surrounding supporting musculature. In more advanced cases, or prior to large climbing trips, steroid injections can help with pain control. If conservative treatment fails or the loss of motion becomes too debilitating, the bony overgrowth can be treated with arthroscopic osteochondroplasty.
4.3 Shoulder
As with the elbow, tendonitis is common in the shoulder. Rotator cuff tendonitis, internal impingement, subacromial impingement, and biceps tendonitis are excessively common in climbers [3, 10, 26, 52, 53]. In our experience, internal impingement with contact of the underside of the rotator cuff with the glenoid rim in repetitive abducted external rotation is particularly prevalent in this population [54]. These can almost always be treated conservatively with therapy alone although targeted steroid injections can also be helpful to break the cycle of inflammation and allow pain-free therapy. Therapy is focused on scapular stabilization and proprioception. Upper trapezial dominance is particularly common and can be reversed with appropriate strengthening measures. Less common pathologies such as nerve entrapment of the supra scapular nerve as well as thoracic outlet syndromes have also been identified in climbers [55].
Subcoracoid impingement can be seen in the general population; however, it commonly has a different pathology in climbers. In the general population, subcoracoid impingement is often due to an abnormally short or excessively curved coracoid leading to abnormalities in the space between the acromial arch and the rotator cuff, leading to irritation and pain [56, 57]. In climbers, the space limitation is due to hypertrophy of the subscapularis muscle and tendon due to a combination of strength from frequent use as well as hypertrophy from chronic inflammation [55]. Additionally, asymptomatic shoulder anterior hyperlaxity common in climbers can further decrease the subacromial interval and lead to compression [55]. Coracoid impingement can be diagnosed on physical exam with pain in the cross arm adduction, forward elevation, and internal rotation position. Treatment is again conservative, with therapy and injections. An arthroscopic subcoracoid decompression can be performed if conservative measures fail.
4.4 Ankle
While tendonitis of the ankle is common in climbers, an injury pattern more unique to them are OCD lesions. Frequent, minor falls onto the ankle and ankle sprains predispose climbers to posttraumatic OCD [3, 27]. These injuries, which are potential complications of sprains or fractures, can be easily missed on radiographs alone and the treating provider should have a high index of suspicion, ordering an MRI when suspected [27]. The talus is a common site for climber OCD lesions. These often require operative treatment with cartilage restorative procedure such as an autologous chondrocyte transplant [58], osteochondral allograft [59], or matrix-associated autologous chondrocyte transplantation [60].
4.5 Foot
Chronic foot conditions in climbing are generally the result of climbing shoes (see Fig. 14.5). Climbing shoes are specifically designed and engineered to give climbers maximal performance advantages in grip and stability while standing on small edges with precision. They are generally worn two sizes smaller than casual shoes; the shoes are designed with a front point and often a semi-rigid flex similar to a ballet shoe. This causes compression of the first and fifth metatarsal joints, as well as tightening of the plantar fascia [61, 62]. Climbers are willing to suffer for advantages in performance. Between 80% and 90% of climbers reported pain while wearing their climbing shoes [27, 62]. Frequent consequences include calluses, nail bed infection, subungual hematomas, and nerve compression syndromes of the foot [27, 61,62,63]. Hallux valgus deformity is common in athletes who have climbed for greater than 5 years [3, 27, 61].
Variations of the climbing shoe. (a) Shows a moderate arch exaggeration with a prominent hooked distal toe. (b, c) Show various angles of a high arch variation with a slightly flatter toe. The advantage of these shoe positions is shown in (d) with demonstration of using the tip of the toe to support much of the climber’s body weight on a hold
5 Pearls for Treating Climbers
Injury prevention and continued therapy in climbers is critical. Excessive climbing without additional training can lead to muscle imbalance; strengthening of opposing muscle groups, maintaining flexibility, and low weight, high repetition exercises are critical. It is important to emphasize the necessity of recovery. Rest between rigorous climbing sessions can help prevent overuse injuries. As climbers age, they must be aware that longer rest periods may be required to avoid over strain. An important aspect of treating climbers is an awareness of the medical hazards of participating in a sport in such potentially extreme environments. Frost bite, cerebral edema, pulmonary edema, altitude sickness, snow blindness, heat exhaustion, dehydration—an awareness of these medical issues must be a part of the medical knowledge of the physician hoping to take care of the climbing community.
References
Schöffl V, Morrison A, Schöffl I, Küpper T. The epidemiology of injury in mountaineering, rock and ice climbing. Med Sport Sci. 2012;58:17–43.
Schöffl V, Morrison A, Schwarz U, Schöffl I, Küpper T. Evaluation of injury and fatality risk in rock and ice climbing. Sports Med. 2010;40(8):657–79.
Peterson C, Ceraulo A. Caring for climbers. Curr Sports Med Rep. 2015;14(5):397–403.
Schöffl V, Küpper T, Hartmann J, Schöffl I. Surgical repair of multiple pulley injuries—evaluation of a new combined pulley repair. J Hand Surg Am. 2012;37(2):224–30.
Folkl AK. Characterizing the consequences of chronic climbing-related injury in sport climbers and boulderers. Wilderness Environ Med. 2013;24(2):153–8.
Schweizer A. Sport climbing from a medical point of view. Swiss Med Wkly. 2012;142:w13688.
Schöffl VR, Hoffmann G, Küpper T. Acute injury risk and severity in indoor climbing-a prospective analysis of 515,337 indoor climbing wall visits in 5 years. Wilderness Environ Med. 2013;24(3):187–94.
Grønhaug G. Self-reported chronic injuries in climbing: who gets injured when? BMJ Open Sport Exerc Med. 2018;4(1):e000406.
Rooks MD. Rock climbing injuries. Sports Med. 1997;23(4):261–70.
Schöffl V, Popp D, Küpper T, Schöffl I. Injury trends in rock climbers: evaluation of a case series of 911 injuries between 2009 and 2012. Wilderness Environ Med. 2015;26(1):62–7.
Chang CY, Torriani M, Huang AJ. Rock climbing injuries: acute and chronic repetitive trauma. Curr Probl Diagn Radiol. 2016;45(3):205–14.
Bollen SR. Injury to the A2 pulley in rock climbers. J Hand Surg Br. 1990;15(2):268–70.
Roloff I, Schöffl VR, Vigouroux L, Quaine F. Biomechanical model for the determination of the forces acting on the finger pulley system. J Biomech. 2006;39(5):915–23.
Lin GT, Amadio PC, An KN, Cooney WP, Chao EY. Biomechanical analysis of finger flexor pulley reconstruction. J Hand Surg Br. 1989;14(3):278–82.
Lin GT, Cooney WP, Amadio PC, An KN. Mechanical properties of human pulleys. J Hand Surg Br. 1990;15(4):429–34.
Widstrom CJ, Doyle JR, Johnson G, Manske PR, McGee R. A mechanical study of six digital pulley reconstruction techniques: Part II. Strength of individual reconstructions. J Hand Surg Am. 1989;14(5):826–9.
Widstrom CJ, Johnson G, Doyle JR, Manske PR, Inhofe P. A mechanical study of six digital pulley reconstruction techniques: Part I. Mechanical effectiveness. J Hand Surg Am. 1989;14(5):821–5.
Odobescu A, Radu A, Brutus J-P, Gilardino MS. Modified flexor digitorum superficialis slip technique for A4 pulley reconstruction. J Hand Surg Eur Vol. 2010;35(6):464–8.
Clark TA, Skeete K, Amadio PC. Flexor tendon pulley reconstruction. J Hand Surg Am. 2010;35(10):1685–9.
Bliven KCH, Parr GP. Outcomes of the Latarjet procedure compared with Bankart repair for recurrent traumatic anterior shoulder instability. J Athl Train. 2018;53(2):181–3.
Lichtenberg S, Magosch P, Habermeyer P. [Superior labrum-biceps anchor complex]. Orthopade. 2003;32(7):616–26.
Schöffl V, Popp D, Dickschass J, Küpper T. Superior labral anterior-posterior lesions in rock climbers—primary double tenodesis? Clin J Sport Med. 2011;21(3):261–3.
Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929–36.
Shea KG, Shea OF, Meals RA. Manual demands and consequences of rock climbing. J Hand Surg Am. 1992;17(2):200–5.
Holtzhausen LM, Noakes TD. Elbow, forearm, wrist, and hand injuries among sport rock climbers. Clin J Sport Med. 1996;6(3):196–203.
Bollen SR. Soft tissue injury in extreme rock climbers. Br J Sports Med. 1988;22(4):145–7.
Schöffl V, Küpper T. Feet injuries in rock climbers. World J Orthop. 2013;4(4):218–28.
Buzzacott P, Schöffl I, Chimiak J, Schöffl V. Rock climbing injuries treated in US emergency departments, 2008–2016. Wilderness Environ Med. 2019;30(2):121–8.
Backe S, Ericson L, Janson S, Timpka T. Rock climbing injury rates and associated risk factors in a general climbing population. Scand J Med Sci Sports. 2009;19(6):850–6.
Nelson NG, McKenzie LB. Rock climbing injuries treated in emergency departments in the U.S., 1990–2007. Am J Prev Med. 2009;37(3):195–200.
Lutter C, El-Sheikh Y, Schöffl I, Schöffl V. Sport climbing: medical considerations for this new Olympic discipline. Br J Sports Med. 2017;51(1):2–3.
Lutter C, Tischer T, Cooper C, Frank L, Hotfiel T, Lenz R, Schöffl V. Mechanisms of acute knee injuries in bouldering and rock climbing athletes. Am J Sports Med. 2020;48(3):730–8.
Thompson RN, Hanratty B, Corry IS. ‘Heel hook’ rock-climbing maneuver: a specific pattern of knee injury. Clin J Sport Med. 2011;21(4):365–8.
Krämer K-L, Jani L, Grifka J, Scharf H-P, Schleberger R, Zacher J, Kommission Leitlinien der Allianz Deutscher Orthopäden. Guidelines in orthopaedic surgery. A first step. Orthopade. 1999;28(3):236–42.
Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974;101:186–91.
Dennis JB, Rutledge BA. Bilateral recurrent dislocations of the superior tibiofibular joint with peroneal-nerve palsy. J Bone Joint Surg. 1958;40(5):1146–8.
Kruckeberg BM, Cinque ME, Moatshe G, Marchetti D, DePhillipo NN, Chahla J, LaPrade RF. Proximal tibiofibular joint instability and treatment approaches: a systematic review of the literature. Arthroscopy. 2017;33(9):1743–51.
Scott J, Lee H, Barsoum W, van den Bogert AJ. The effect of tibiofemoral loading on proximal tibiofibular joint motion. J Anat. 2007;211(5):647–53.
Curatolo CM, Bach G, Mutty CE, Marzo JM. Review of common clinical conditions of the proximal tibiofibular joint. Am J Orthop. 2018;47(12) https://doi.org/10.12788/ajo.2018.0105.
Burke CJ, Grimm LJ, Boyle MJ, Moorman CT, Hash TW. Imaging of proximal tibiofibular joint instability: a 10 year retrospective case series. Clin Imaging. 2016;40(3):470–6.
Brage ME, Hansen ST. Traumatic subluxation/dislocation of the peroneal tendons. Foot Ankle. 1992;13(7):423–31.
Arrowsmith SR, Fleming LL, Allman FL. Traumatic dislocations of the peroneal tendons. Am J Sports Med. 1983;11(3):142–6.
Forrester JD, Tran K, Tennakoon L, Staudenmayer K. Climbing-related injury among adults in the United States: 5-year analysis of the National Emergency Department Sample. Wilderness Environ Med. 2018;29(4):425–30.
Lum ZC, Park L. Rock climbing injuries and time to return to sport in the recreational climber. J Orthop. 2019;16(4):361–3.
Lutter C, Hotfiel T, Tischer T, Lenz R, Schöffl V. Evaluation of rock climbing related injuries in older athletes. Wilderness Environ Med. 2019;30(4):362–8.
Hochholzer T, Schöffl VR. Epiphyseal fractures of the finger middle joints in young sport climbers. Wilderness Environ Med. 2005;16(3):139–42.
Heuck A, Hochholzer T, Keinath C. [MRT of the hand and wrist of sport climbers. Imaging of injuries and consequences of stress overload]. Radiologe. 1992;32(5):248–54.
Rohrbough JT, Mudge MK, Schilling RC. Overuse injuries in the elite rock climber. Med Sci Sports Exerc. 2000;32(8):1369–72.
Allenspach P, Saupe N, Rufibach K, Schweizer A. Radiological changes and signs of osteoarthritis in the fingers of male performance sport climbers. J Sports Med Phys Fitness. 2011;51(3):497–505.
Schöffl V, Hochholzer T, Schöffl I. Extensor hood syndrome—osteophytic irritation of digital extensor tendons in rock climbers. Wilderness Environ Med. 2010;21(3):253–6.
Jones G, Johnson MI. A critical review of the incidence and risk factors for finger injuries in rock climbing. Curr Sports Med Rep. 2016;15(6):400–9.
Peters P. Orthopedic problems in sport climbing. Wilderness Environ Med. 2001;12(2):100–10.
Bollen SR. Upper limb injuries in elite rock climbers. J R Coll Surg Edinb. 1990;35(6):S18–20.
Drakos MC, Rudzki JR, Allen AA, Potter HG, Altchek DW. Internal impingement of the shoulder in the overhead athlete. J Bone Joint Surg Am. 2009;91(11):2719–28.
Schöffl V, Schneider H, Küpper T. Coracoid impingement syndrome due to intensive rock climbing training. Wilderness Environ Med. 2011;22(2):126–9.
Roche SJ, Kennedy MT, Butt AJ, Kaar K. Coracoid impingement syndrome: a treatable cause of anterior shoulder pain. Ir J Med Sci. 2006;175(3):57–61.
Radas CB, Pieper H-G. The coracoid impingement of the subscapularis tendon: a cadaver study. J Shoulder Elb Surg. 2004;13(2):154–9.
Koulalis D, Schultz W, Heyden M. Autologous chondrocyte transplantation for osteochondritis dissecans of the talus. Clin Orthop Relat Res. 2002;395(395):186–92.
Lin JS, Andersen LB, Juliano PJ. Effectiveness of composite bone graft substitute plugs in the treatment of chondral and osteochondral lesions of the talus. J Foot Ankle Surg. 2010;49(3):224–31.
Dickschas J, Welsch G, Strecker W, Schöffl V. Matrix-associated autologous chondrocyte transplantation combined with iliac crest bone graft for reconstruction of talus necrosis due to villonodular synovitis. J Foot Ankle Surg. 2012;51(1):87–90.
van der Putten EP, Snijder CJ. Shoe design for prevention of injuries in sport climbing. Appl Ergon. 2001;32(4):379–87.
Killian RB, Nishimoto GS, Page JC. Foot and ankle injuries related to rock climbing. The role of footwear. J Am Podiatr Med Assoc. 1998;88(8):365–74.
Peters P. Nerve compression syndromes in sport climbers. Int J Sports Med. 2001;22(8):611–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 ISAKOS
About this chapter
Cite this chapter
Cooper, J.D., Hackett, T. (2021). Climbing. In: Rocha Piedade, S., Neyret, P., Espregueira-Mendes, J., Cohen, M., Hutchinson, M.R. (eds) Specific Sports-Related Injuries. Springer, Cham. https://doi.org/10.1007/978-3-030-66321-6_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-66321-6_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-66320-9
Online ISBN: 978-3-030-66321-6
eBook Packages: MedicineMedicine (R0)