Abstract
PCOS is a quite frequent reproductive disease that affects 5–20% of the female population. Though specific diagnostic criteria have been established, probably they need an update according to the new insights recently ascertained, that is, insulin resistance (IR) and compensatory hyperinsulinemia. In addition, new specific insights have been demonstrated in animal models of PCOS that suggest a clear role of a neuroendocrinological impairment that might occur during prenatal life and/or after birth affecting the regular function of the reproductive axis. All these aspects suggest that PCOS might have a certain grade of epigenetic origins that might be implemented by familial predisposition to specific dismetabolic diseases such as diabetes. We will try to focus on these aspects to give an update on the putative therapeutical possibilities.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
5.1 Introduction
Polycystic ovary syndrome (PCOS) is a heterogeneous condition affecting between 5 and 20% of fertile women [1]. It is the most common cause of anovulation and therefore of infertility, characterized by hyperandrogenism with the arrest of follicular development, esthetic problems (acne, hirsutism, alopecia), and frequently associated with metabolic alterations such as insulin resistance or overweight/obesity.
Although several diagnostic criteria have been proposed (Rotterdam, Androgen Excess and PCOS Society, National Institutes of Health), the diagnosis of PCOS is still based on the Rotterdam criteria (2003) [2], which require the presence of two out of three main features of the syndrome: chronic anovulation that means oligo−/amenorrhea, hyperandrogenism (clinical and/or bio-humoral), and polycystic ovaries at ultrasound [3].
Over the years a very variable spectrum of clinical manifestations has been highlighted, variously combined in different patterns, so that four different possible phenotypes can be identified (Table 5.1).
The common features of these patients are the well-known presence of an inappropriate gonadotropin secretion, often characterized by elevated LH levels compared to FSH levels, this last reduced up to lower than 30%, and an increased LH/FSH ratio (>2.5), due to the increased amplitude of LH pulses, this being the cause of ovarian hyperandrogenism. In addition to the well-known clinical symptoms, PCOS is also characterized by a series of metabolic problems such as obesity, present in 25–50% of the patients, and hyperinsulinemia that occurs in up to 50% of subjects. Indeed, extensive literature has shown that insulin resistance is very common in PCOS, independently from BMI.
Insulin resistance is a biological compensatory event that induces the elevation of insulin concentrations (hyperinsulinemia) in order to keep the glycemic values within the normal range. It is present in 50–80% of women with PCOS and obesity and in 15–30% of PCOS with normal weight [4, 5, 6]. During pregnancy, women with PCOS have a greater risk of incurring complications such as gestational diabetes, hypertensive disorders, preeclampsia, HELLP syndrome, and preterm birth, especially if they have a compensatory hyperinsulinism [7].
5.2 Physiopathology of the PCOS Patients
5.2.1 Weight and Metabolism
It is well-known how reproductive axis and body weight are tightly linked. Depending on the bodily disposition of the fat, obesity is classified into gynoid obesity, in which the fat is distributed in the lower part of the body, i.e., buttocks and thighs, and android obesity, in which the fat is located centrally at abdominal, mesenteric, and visceral level [8]. The substantial difference of this different conformation relies in the fact that the adipose tissue accumulated at the abdominal level is metabolically more active, more sensitive to catecholamines and less to insulin, and releases higher amount of triglycerides, and this is considered a direct index of cardiovascular risk. In fact, the Waist Hip Ratio determination (WHR) is an excellent index to assess the degree of obesity, quantifying the amount of intra-abdominal fat. In a subject with BMI > 25 kg/m2, a ratio greater than 0.80 is a clear sign of android obesity, while a ratio lower than 0.75 is an index of gynoid obesity. The waist circumference, more than BMI, is directly correlated with the risk of developing Metabolic Syndrome (MS); in fact it is included among the diagnostic criteria for MS drawn up by the Adult Treatment Panel III (ATIII), which considers as a risk factor a waist circumference equal or greater than 102 cm in males and 88 cm in women [8].
As a result of this excess of weight, in particular in women, an alteration of reproductive capacity is frequently observed. The adipose tissue is not inert, but it is a real endocrine organ, with effects at both peripheral and central level, which unlike the other endocrine systems is poorly controlled and modulated in its action by the hypothalamic area or by other endocrine systems: in fact, fat cells are able not only to aromatize androgens into estrogens but also to release hormonal signals (adiponectin, leptin), acting directly on the CNS and regulating food intake, energy expenditure, and reproductive function. An excessive intake of food influences the balance of our metabolic and endocrine systems up to modulating the hypothalamus, which is the control unit that regulates and coordinates the whole metabolic-hormonal system, with consequent abnormal release of hypothalamic tropins and irregular menstrual cycle, from oligomenorrhea and anovulation, up to amenorrhea. In the brain all the signals relating to the nutritional state, such as the excess as well as the weight defect, are recorded and processed as function of time and quite often are negatively recorded. The metabolic signals arriving at the hypothalamic level are transmitted by leptin and adiponectin (both hormones produced in adipocytes), Ghrelin, and many other neurotransmitters, modulating the release of hypothalamic GnRH. When the hypothalamic function is negatively affected, functional disorders result (i.e., PCOS, hypothalamic amenorrhea, etc.). In humans and nonhuman primates, the majority of hypothalamic GnRH neurons are located more dorsally in the medial basal hypothalamus, in the infundibulum, and in the periventricular region. They are surrounded by the centers that control the sleep-wake rhythm, thermoregulation, hunger/satiety, and glycemic control: modifications of the function of these centers, induced by peripheral signals, lead to an alteration in the production and pulsatile release of GnRH that affects the reproductive function, triggering oligomenorrhea, anovulation, and/or amenorrhea.
5.2.2 Hyperandrogenism
Although PCOS is a syndrome, we have always tried to understand where hyperandrogenism is triggered: abnormalities of the metabolic control (diabetes, thyroid diseases), malfunctioning at ovarian level (ovarian cysts, atresic follicles), or hyperandrogenism caused by endocrine diseases such as those of adrenal gland (exaggerated adrenarche, Cushing’s syndrome, adrenal hyperplasia). However, only 3% of PCOS hyperandrogenism is due to an isolated adrenal disease [9] (Table 5.2).
Androgens and its precursors are normally produced at ovarian and adrenal level in approximately equal amounts, respectively, under LH and ACTH control. Androgens, however, do not have a negative feedback or a neuroendocrine mechanism that directly regulates/controls their production. In fact, the androgenic production from the ovary has intra-ovarian mechanisms, in order to optimize the synthesis of androgens, estrogens, and folliculogenesis: androgens are obviously the substrate for the production of estrogens, but if they are present in exaggerated amount, they block ovulation. The ovarian androgenic hypersecretion, typical of PCOS patients, appears to be caused by a mechanism of desensitization of thecal cells to LH, which however limit excessive androgenic production; on the other hand, the amount of androgens produced is under paracrine control, which essentially acts on the activity of the cytochrome p450c17 that limits the formation of steroid hormones.
Whatever triggers PCOS, the aromatase activity at ovarian level is altered. It is well-known that in the ovaries the production of estradiol is linked to the correct aromatization of androgens in estrogens: whenever a metabolic factor, such as a compensatory hyperinsulinemia, induced by peripheral insulin resistance, alters this equilibrium, androgen production increases, and aromatase activity is abnormally reduced.
The failure of the conversion of androgens to estradiol and the resulting hyperandrogenism induce reduced hepatic SHBG synthesis, promoting the increase of plasmatic free androgens levels and a higher bioactive availability, thus promoting the onset of clinical signs such as hirsutism and acne [6]. Furthermore, the excess of androgens negatively modulates the function of insulin in the liver and at peripheral level: in fact it has been shown that testosterone negatively modulates the transmission of the intracellular insulin signal, reducing both the number and the efficiency of glucose transporters (GLUT-4), generating/improving insulin resistance mechanisms [10]. All such facts in women with PCOS promote also an excess of IGF-1 other than of insulin, with a further increase of androgens’ levels, caused by the aromatase deficiency and by SHBG levels decrease, with the consequent increase of the amount of free androgens, which are biologically active and deeply affecting the reproductive axis. The importance of nutritional status for the proper functioning of the reproductive axis is thus further emphasized.
5.2.3 Insulin Resistance
Insulin, as already mentioned, plays a role on the synthesis of androgens modulating the cytochrome P450-17alpha, and its levels correlate with glycemia. When performing the oral glucose tolerance test (OGTT) in a patient with a suspect of insulin resistance, we must not focus on blood glucose levels only since the metabolic homeostasis reacts to control blood glucose levels inducing the release of insulin up to 10 times the amount of insulin normally necessary. Prevention is therefore the most powerful tool we have. Through a correct lifestyle and the use of insulin-sensitizers (like Metformin), we can be helpful in managing these conditions.
Insulin resistance and hyperinsulinemia are the elements that most frequently determine the clinical and biochemical difference between PCOS patient with overweight/obesity from those with normal weight. When obesity and insulin resistance occur together with an android-type distribution of adipose tissue, despite having absolute values of androgens only moderately increased, SHBG levels are reduced, and the clinical signs of hyperandrogenism become more evident. In PCOS without insulin resistance, the amount of free androgens is lower, and the clinical manifestations linked to hyperandrogenism are less marked.
In this context, the data obtained from the OGTT becomes essential. Similar to other endocrine diseases, such as in girls with hypo-GH, we find an insulin response to the glucose load similar to that observed in obese patients: in fact, the GH deficiency triggers a compensatory mechanism modifying both cortisol and insulin secretions, in order to compensate the lack of GH, thus inducing a compensatory hyperinsulinemia. The result of this is an insulin response to glucose load in normal-weight patients with GH deficiency paradoxically similar to that observed in obese or PCOS patients.
Another important aspect recently investigated is the involvement of liver in this endo-metabolic framework. The well-known NAFLD (Nonalcoholic Fatty Liver Disease) is the result of insulin resistance, which leads to an accumulation of fat in the liver; it has been recently shown that the liver produces two hormones, HGF (Hepatocyte Growth Factor) and betatrophin, both involved in a system that modulates the compensatory response of beta-pancreatic cells to insulin resistance. Betatrophin modulates in a direct way the proliferation of beta cells in case of insulin resistance in order to increase the amount of insulin and thus to obtain a better control of glycemia and glucose uptake from the plasmatic circulation [11]; HGF is a growth factor that plays a key role in the connection, via the opioidergic and neuroaminergic pathways, of the brain-liver-pancreas axis, modulating the adaptive response of the pancreas to insulin resistance [11].
Studies on animal models have hypothesized that insulin receptors are also present at central level, in particular localized on kisspeptin-secreting neurons that stimulate GnRH neurons. Under compensatory hyperinsulinemia, an excessive activity of kisspeptin-secreting neurons has been observed, thus inducing an increase of GnRH release. Neuroendocrinology of obese patients, therefore, described a direct link between CNS and metabolism, and in particular, there is a metabolic-induced modulation of several neuroendocrine activities [12].
It is well-known that insulin resistance is due to several conditions that can act already during the prenatal period, such as gestational diabetes and obesity during pregnancy, or that can act after birth as in case of children with IUGR (Intrauterine Growth Restriction), where hyperinsulinemia represents a compensatory defensive mechanism that allows the low-in-weight infants to store energy, survive, and thus reach quickly a more appropriate body weight. Insulin resistance may also be linked to receptor or signal transduction defects or to genetic factors such as familial diabetes, but when obesity occurs during adulthood the mechanism triggering the gain of weight is clear [11].
5.3 New Perspectives in the Pathogenesis of PCOS
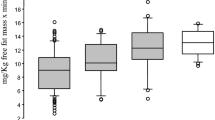
A recent review collected the results from several studies on animal models and rationally hypothesized a primarily neuroendocrine origin of PCOS [13]: in particular, since hyperandrogenism is present in 60% of PCOS patients, the effects of high androgen levels have been assessed. In these animal models the exposure to high androgen levels during prenatal life or during the first months of life induces the onset of the typical features of PCOS: clinical manifestations of hyperandrogenism, hypersecretion of LH, ultrasonographic evidence of polycystic ovaries, ovulatory dysfunction, increased amount of fat mass, hypertrophy of fat cells, and also insulin resistance. Probably the androgen receptor (AR) plays an essential role in the pathogenesis of PCOS: AR is expressed in the structures of the hypothalamic-pituitary-ovarian axis, as well as in adipocytes and in hepatocytes. However, the role played by androgens in central nervous system (CNS) is probably predominant, since in knock-out animal model for AR in the brain and undergoing to states of hyperandrogenism a much more marked reduction in the typical manifestations of PCOS has been observed compared to the knock-out model for AR only at ovarian level [13] (Fig. 5.1).
Different sites of AR action in generating the characteristic features of PCOS. In particular, silencing AR at the level of the CNS and generating states of hyperandrogenism in the rats did not induce the reproductive and metabolic traits of PCOS; therefore the loss of central AR function protects from the onset of PCOS more than the loss of function of AR in the ovaries (modified from [13])
A frequent characteristic of the PCOS patient is the increased frequency and amplitude of LH pulse. This reflects the increased stimulation of GnRH neurons: on animal models it has been observed that these neurons do not express receptors for androgens, progesterone, and alpha-estrogens. Interestingly the negative and positive feedback at central level is not played on GnRH neurons, and these mechanisms are indirect. In fact, recently two neuronal groups have been identified: kisspeptin/neurokinin B/dynorphin neurons (KNDy), which act with a mechanism depending on the levels of circulating estrogens, and the GABAergic neurons of the arcuate nucleus, which guarantee a stimulatory effect on the GnRH-secreting neurons [14]. The kisspeptin-secreting neurons have two locations: one group is in anteroventral periventricular nucleus (AVPV) and is sensitive to low levels of circulating estrogens, generating a positive feedback on GnRH-secreting neurons; the other is in the arcuate nucleus and is activated by high levels of estrogen, thus playing the negative feedback on the GnRH pulse generator.
On such basis, androgen receptors have been proposed as potential modulator of the KNDy system [15]: in fact, it has been observed that prenatal exposure to hyperandrogenic states leads to a drop of innervation by the KNDy system on GnRH-secreting neurons, negatively affecting the negative feedback action. On such basis, it has been postulated that the KNDy system could become a “putative” therapeutic target to modulate the activity of the pulse generator GnRH/LH, in order to reduce the frequency of LH pulse, the circulating levels of LH, and testosterone [15]. In contrast, hyperandrogenism in the prenatal life generates an increased innervation of GABAergic neurons of the arcuate nucleus on the GnRH-secreting neurons, increasing their activity.
A model linked to adipocyte dysfunction as a trigger of PCOS pathophysiology has also been proposed, and a role of androgen receptors at the ovarian level in the development of the PCOS reproductive tracts cannot be excluded. However, the role that androgens play at the central level is emblematic in the development and pathogenesis of the typical characteristics of PCOS, although it obviously remains to determine how prenatal exposure to androgens in humans modifies the pathways acting on the hypothalamus. This experimental model lets us postulate a potential role of those molecules blocking androgen receptors, thus generating again at the central level an equilibrium among the various neurotransmitters/systems for the reactivation/resumption of the correct functionality of the reproductive axis. Certainly, the exposure to hyperandrogenic states during prenatal life is a relevant epigenetic cofactor for the triggering and development of PCOS.
5.4 Genetics, Metabolism, and PCOS
Data regarding genetic mutations directly linked to the onset of PCOS are particularly scarce. A 2017 study conducted on animal models with a selective mutation of the PTEN gene (phosphatase and TENsin homolog) in ovarian theca cells showed the occurrence of numerous reproductive characteristics typical of PCOS, including alteration of menstrual cyclicity, anovulation, high levels of circulating androgens, and characteristic PCO-like ovarian aspect. We recall that in the absence of the PTEN protein, which takes part to the cascade of insulin signaling, the correct mechanism of glucose transporters is altered [16]. Considering the frequency of insulin resistance in PCOS, attention was given to carbohydrate metabolism and, in particular, to the epimerase, responsible for the transformation of myo-inositol (MYO) into D-chiro-inositol (DCI), which has been reported to reduce functionality or expression in patients with hyperinsulinemia and PCOS, especially in those who have familial diabetes [17]. There are two main isoforms of inositols working in the transmission of the metabolic signal of numerous peptide hormones. Other than insulin, also TSH and FSH have inositols as element of the post-receptor signaling. Whereas inositol participates and promotes glucose transport into the cells, glucose oxidative use, and glycogen storage, it is well worth considering the possibility of inositols’ integrative use in PCOS as well as in diabetes. The amount of MYO present inside the cells is in balance with all other inositol isoforms and when required is transformed into DCI by the epimerase which is expressed in a tissue-specific way and guarantees the conversion in the various districts [18]. In diabetic patients or in case of insulin resistance, a lower amount of DCI was found in urine reflecting a lower insulin-sensitivity than in the general population, supporting the hypothesis that there may be an anomalous function/expression of the epimerase which should guarantee the synthesis of DCI, inducing the worsening of insulin resistance and a compensatory hyperinsulinemia [19].
It has been proposed that the primum movens of PCOS was a dysfunctional ovarian hyperandrogenism, caused by a lack of regulation in androgen secretion. Recently it has been shown that this characteristic occurs in two thirds of PCOS patients, who show an excessive production of 17OH-P in response to gonadotropin stimulation [20]. The third remaining is a population of atypical and heterogeneous PCOS, in which hyperandrogenism has an adrenal origin, associated or not with obesity [20]. Approximately half of the women with PCOM (polycystic ovarian morphology) have a dysfunctional ovarian hyperandrogenism related to a defect of steroidogenesis [20]: in fact in vitro theca cells of women with PCOS show an intrinsic dysregulation of steroidogenesis, compatible with what observed in vivo, with a high expression of steroidogenetic enzymes and in particular of the cytochrome p450c17, an enzyme responsible for androgens production in case of excessive synthesis, present at gonadal and adrenal levels. Recently DENND1A.V2, a protein promoting steroidogenesis, has been identified in androgen-producing cells, differentially expressed in neoplastic and normal cells, which in normal theca cells reproduced the PCOS phenotype observed in vitro [20].
The etiology of dysfunctional ovarian hyperandrogenism certainly remains multifactorial: as already mentioned, it seems to be triggered by a complex interaction between predisposing congenital factors and promoting environmental factors such as insulin resistance and obesity, both characterized by an inheritance component. In fact, obesity is associated with the increased ovarian androgenic production, primarily due to systemic conditions of hyperinsulinemia, but also to an increased production of inflammatory cytokines. Metabolic syndrome related to obesity and insulin resistance occurs in about half of women with PCOS and compensatory hyperinsulinemia that is classically observed with tissue-specific effects, creating the worsening of hyperandrogenism.
In fact, PCOS evolves from the interaction between various genetic and environmental factors: among hereditary factors, we include PCOM, hyperandrogenism, insulin resistance, and defects in insulin secretion; the environmental factors include prenatal exposure to a hyperandrogenic environment, reduced fetal growth (IUGR), small for gestational age (SGA) newborn, and acquired obesity. The great variety of biological processes involved in glucose metabolism and steroidogenesis, associated to many possible environmental conditions, makes the pathogenesis multifactorial and the syndrome particularly heterogeneous. Therefore, other studies are needed to understand the exact triggers of the pathophysiology of PCOS in order to act on hyperandrogenism, anovulation, and hyperinsulinemia [20, 21].
Since 1968, studies have suggested an important role of genetics in the etiology of PCOS [22]: in fact first-degree relatives of patients with PCOS have an increased risk of being themselves affected compared to the general population [23], and it has been observed a greater correspondence of pathology between monozygotic twins compared to heterozygotes [24], concluding that the genetic component contributes more than 70% to the pathogenesis. However, studies based on the genes candidate for the pathogenesis of PCOS did not lead to concrete results. To date, numerous new loci and genes have been identified as candidates for the pathogenesis of PCOS through the Genome-Wide Association Studies (GWAS), which is a new approach to the study of the genome to understand the genetic basis of many complex diseases, using a survey of the variations of genes observed in patients affected by the same disease. Unfortunately these loci identified by the GWAS explained less than 10% of the genetic component of PCOS, because this method allows studying only the most common variants, while the less frequent and rarer variants, which however could have a big impact in generating the syndrome and the various possible phenotypes, are not yet detectable [25].
Certainly this disease cannot be explained by a limited number of variants [26]: in this context, a process of massive sequencing of the genome has begun, probably leading to its complete analysis, looking for rare genetic variants that contribute to the pathogenesis of PCOS and mapping the genetic variants that generate the different phenotypes of the syndrome [26]. More genetic knowledge, in association with epigenetic studies on PCOS, could help us to understand more clearly the pathogenesis of this syndrome, creating practical implications as a simpler and earlier diagnosis of the patient’s specific phenotype, which would allow treating and preventing the possible associated pathologies in an extremely personalized way.
5.5 The Management of Infertility in PCOS Patients
Since up to now the etiology of PCOS has not been completely defined, the therapeutic options are not specifically organized, and many treatments remain today off-label. Up to now, several approaches and attempts have been tested to induce ovulation in PCOS patient: we will discuss the main and most commonly used methods.
5.5.1 Lifestyle Modification
Obesity obviously has a negative impact on the fertility of women with PCOS: it decreases the chances of conception because of the reduced number of spontaneous ovulatory cycles and the high percentage of spontaneous abortions, as well as the risk of complications during pregnancy and adverse perinatal outcomes. Lifestyle modification therefore is the first and most basic therapeutic approach, which includes the combination of a hypocaloric diet, constant physical activity to improve metabolic and anthropometric features (body weight, WHR, and fat mass/lean mass ratio), and a psychological support if it is necessary [27]. Furthermore, the reduction of both insulin and androgens plasma levels favors the restoration of menstrual and ovulatory cycles, improving reproductive outcomes in PCOS women.
Diet and regular exercise should therefore be always recommended as the first line of treatment for patients with PCOS with BMI > 25 kg/m2, in particular in case of obesity [28], but these issues seem to be effective even in normal-weight PCOS patients, independently from the body weight and even if there is no concrete weight loss, since it simply improves the metabolic risk factors associated with PCOS [29].
The lifestyle modification therefore starts from a hypocaloric diet (500–1000 fewer calories per day) in association with physical exercise (20–60 min of physical activity a day, from 3 to 5 times a week) for 6 months. Any doctor who takes care of this patient has to lead to a change of the lifestyle with an adequate counseling, making the patient understand that the ultimate purpose is the good health as well as the restoration of the reproductive function. If the patient’s compliance is poor, it has to be considered the opportunity to have a psychological support.Despite the appropriate lifestyle changes, in case of strong hyperinsulinemia or extreme difficulty in weight loss, it is possible to introduce Metformin for 6 months or more, which has been shown to favor the decline in BMI, with an important reduction of subcutaneous fat and the recovery of menstrual cyclicity, better than a correct lifestyle associated with placebo [30].
It is essential to investigate the insulin response to the oral glucose tolerance test (OGTT), at least at times 0 and 90′, to understand the relationship between blood glucose and insulin response and to evaluate how they change after meals. Weight loss is the driving force, even if modest, but sufficient to reduce the metabolic risk. In women with PCOS, lifestyle changes improve body composition and reduce hyperandrogenism and insulin resistance [28].
To underline the importance of lifestyle change regardless of any therapy, a well-established study has evaluated the effect of treatment with Metformin (850 mg/day) or only of lifestyle change (weight loss of 7% and physical activity for 150 min per week) in a group of subjects with impaired glucose tolerance [29]: for each subject the presence of metabolic syndrome was evaluated before and after the observational period. The results of this study show that the lifestyle change allows more positive effects on reduction of glucose plasma levels and of the risk of metabolic syndrome, both in terms of prevention of the development of the disease and improvement of basic metabolic conditions. Treatment with Metformin has been shown to be effective in preventing or delaying the onset of diabetes, but with less efficacy than having a different lifestyle.
Therefore, any pharmacological treatment that aims to improve the metabolic setting must be associated to an intervention of lifestyle correction. Women with overweight and PCOS show, other than a greater incidence of menstrual cycle alterations (oligo−/amenorrhea, anovulation, polymenorrhea), various metabolic alterations (hyperinsulinemia, diabetes, abdominal obesity), and they are also more exposed to the risk of developing cardiovascular diseases in young age, or in any case within 50 years: in fact insulin resistance and hyperinsulinemia have a negative impact at vascular level where they interact with the vasoactive factors, such as endothelin and nitric oxide, generating processes of alteration of vasodilation, predisposing to hypertension. In practice, nutrition and metabolic features are closely linked with the neuroendocrine world, compromising the reproductive function of any young woman with PCOS predisposing to pathologies that occur during adult or pre-menopausal period such as diabetes and cardiovascular diseases up to estrogen-dependent cancers.
5.5.2 Bariatric Surgery
Current guidelines suggest that bariatric surgery should be considered only in cases of grade III obesity, i.e., with BMI ≥40 kg/m2, or ≥ 35 kg/m2 in association with comorbidity who have failed to lose weight after 6 months of correct diet and regular physical activity [31]. This type of surgery is effective for weight loss, improves fertility outcomes in obese patients with PCOS, restores menstrual cycle and ovulation, and reduces hyperandrogenism and insulin resistance [31]. Obviously patients must be informed that there are risks related to this type of surgery, both linked to the surgery itself and to the onset of numerous possible complications during a pregnancy that arose after such surgery, which should be considered at high risk for preterm delivery, small-for-gestational age infants, stillbirth, or neonatal death, while the risk of gestational diabetes and of large-for-gestational age infants is reduced [32]. Therefore, bariatric surgery has to be considered as the last possible therapeutic option, exposing the body to a sudden weight loss associated with the onset of possible intestinal malabsorption. It is evident that bariatric surgery is only an “extrema ratio” for the management of PCOS patients, and the omen is that it will never become necessary.
5.5.3 Metformin
Metformin, a synthetic biguanide, is an oral hypoglycemic agent, considered the first-line treatment in type 2 diabetes mellitus. It works by reducing hepatic glucose production and intestinal glucose uptake, while increasing glucose uptake at peripheral level by skeletal muscle and liver. Being therefore an insulin-sensitizing agent, it is used in PCOS to reduce serum insulin concentrations and thus improve the metabolic setting in these patients, favoring the recovery of ovulatory cycles. In our clinical practice the starting dose is 250 mg twice a day 15 min before lunch and dinner, which can be increased up to 500–1000 mg after 15 days, with a gradual increase in dosage to avoid common gastrointestinal side effects. Although lifestyle modification is by far the first line of treatment in obese patients with PCOS and infertility, Metformin can be a valuable support in achieving weight loss. A recent meta-analysis [30] including 12 studies for a total of 608 patients has shown that the combination of Metformin and lifestyle modification in PCOS patients is more effective in weight loss than diet and physical activity alone [30]. A recent Cochrane review [33] that included 42 trials evaluating the beneficial effects of Metformin in women with PCOS has shown an increase in ovulatory cycles and pregnancy rates in the Metformin arm compared to placebo.
Although in this type of patients Metformin induces a higher rate of ovulatory cycles than placebo [34], it should not be considered the first-line treatment of chronic anovulation, since there are specific ovulation inducers, such as Clomiphene Citrate (CC) and Letrozole that both induce better results in terms of ovulation rate, number of pregnancies, and live births [35].However, the association between Metformin and CC, which should be considered for those patients not responding to treatment with CC alone, reported by a Cochrane review [33], provides only limited evidences on the efficacy of the association of these two products. To confirm this data, two meta-analyses [36, 37] have also been done on PCOS patients undergoing ART, and the administration of Metformin has been reported not to increase the pregnancy rate but to reduce the risk of the ovarian hyperstimulation syndrome (OHSS).
In conclusion, Metformin represents an important tool in the management of obese PCOS patients, being an insulin-sensitizing agent that acts by improving the metabolic profile and favoring weight loss; however, there are only relative effects on the increase in the pregnancy rate and live births. However, it remains a low-cost therapy, with good tolerability, though some gastrointestinal side effects that are dose-dependent and a good safety profile. It does not require a constant monitoring and does not induce multiple pregnancies. We might consider its prescription in association with supplements therapy, such as inositols and alpha-lipoic acid, which can further improve its effectiveness.
5.5.4 Clomiphene Citrate
Clomiphene citrate is a “selective estrogen receptor modulator” (SERM) that competes with endogenous estrogens on their receptor-binding sites. It is characterized by an anti-estrogenic effect that modifies the cervical mucus composition and endometrial receptivity, events that could favor implantation or conception after correctly inducing ovulation. It is anyway considered the treatment of choice in anovulatory PCOS patients. The starting dose is 50 mg a day for 5 days (from the third–fourth to the seventh–eighth day of the menstrual cycle depending on the protocols) and can be increased up to a maximum of 150 mg a day. However, resistance to Clomiphene is a very frequent event, which occurs in 15–40% of women with PCOS [38]. The percentage of ovulation in women with PCOS after CC administration is approximately 75–80%, while pregnancy is observed in 22% of cases [39]. This discrepancy of about 40% between the percentage of ovulation and pregnancy is probably due to the hypoestrogenic effect of CC on the endometrium and cervical changes of mucus.
Treatment with CC is generally suggested for a period not exceeding 6 months. Observations referred to a cumulative rate of success for the whole treatment cycle up to 65% [39].
In a large meta-analysis [40], including 57 trials and 8082 women, the most common ovulation induction protocols have been compared: all pharmacological treatments such as CC, Metformin, CC in association with Metformin, Letrozole, Tamoxifen, ovarian drilling, and follicle stimulating hormone (FSH) have been shown to be more effective than placebo in terms of ovulation or pregnancy rates. Compared to Letrozole, Clomiphene alone has shown lower rates of ovulation, pregnancy, and live births, probably due to its endometrial anti-proliferative effect.
A recent systematic review [41], focused on the effects of CC and other ovulation-inducing agents in women with anovulatory cycles, confirmed these results. Obviously, CC has shown lower efficacy in terms of reproductive outcomes compared to exogenous gonadotropins [42], considered a second-line intervention in anovulatory PCOS women if the starting treatments were ineffective, since their use is expensive, requires constant monitoring, and may be associated with side effects such as multiple pregnancies and/or ovarian hyperstimulation syndrome (OHSS).To date, CC remains the most widely used treatment worldwide for ovulation induction in PCOS patients [39, 43]: it is taken orally, and it is cheap, effective, and safe, substantially free of side effects, even if literature reports same cases of multiple pregnancies.
5.5.5 Letrozole
Letrozole is an aromatase inhibitor and is commonly used to induce ovulation, generally as an alternative treatment to Clomiphene, especially in CC-resistant women. Its use as ovulation inducer is off-label or even prohibited in some countries of the world: in some studies, it has been associated with teratogenic effects on the fetus [44] and is burdened by important side effects linked to hypoestrogenism, typical of premenopausal symptoms. The mechanism of action consists in the inhibition of the aromatase enzyme, which converts androgens into estrogens at the ovarian level, peripheral tissues, and brain levels. As there is no estrogen receptor antagonism, it acts through a negative feedback mechanism at the central level, which generally determines the growth of a single dominant follicle. The starting dose is 2.5 mg a day for 5 days, from the third to the seventh day of the menstrual cycle. The dose can be increased up to a maximum of 7.5 mg for 5 days.
Despite the important side effects of Letrozole, numerous clinical trials have demonstrated the higher efficacy compared to Clomiphene, in terms of ovulation, pregnancy rate, and live birth rates [45]. In a large multicenter study of 750 women with PCOS and infertility [46], who received Letrozole or CC, the greater efficacy of Letrozole in terms of ovulation rate (61.7 vs 48.35%; p < 0.001) and higher cumulative live birth rate (27.5 vs 19.1%; p = 0.007) has been demonstrated compared to women treated with CC, except for a subgroup of women with BMI <30 kg/m2, in which both treatments showed the same efficacy in terms of live birth rate. The greater efficacy of Letrozole could be probably explained since it has no direct antiestrogen effects on cervical mucus and on the endometrium and by its short half-life [46].
In conclusion, Letrozole can be considered as a potential therapeutic option for ovulation induction, even more effective than Clomiphene especially in obese PCOS patients, but certainly characterized by greater side effects.
5.5.6 Ovarian Drilling
Laparoscopic ovarian drilling can be considered a second-line treatment for PCOS patients with CC-resistant infertility [39]. Usually it is suggested to make 3 to 8 small perforations on the surface of each ovary with a depth and a diameter of about 1–2 mm using either heat (monopolar or bipolar electrocautery) or laser with comparable outcomes [47]. With this procedure, there is a partial destruction of the ovarian cortex and a sharp drop in the levels of androgens produced by this area, with a fall in LH and an increase in FSH plasma levels, thus inducing a correct follicular recruitment up to ovulation [48].
In a recent meta-analysis conducted on 484 participants, comparing the effects of unilateral vs bilateral ovarian drilling, there were no differences between the two techniques in terms of ovulation, pregnancy rate, number of live births, or abortion rate, with no differences in serum AMH concentrations after 6 months of surgical treatment, which therefore support the fact of not to have a negative impact on the ovarian reserve.
In the last Cochrane review [49], there were no differences in terms of live birth rate comparing the surgical technique, the use of exogenous gonadotropins, or aromatase inhibitors. This surgical technique is therefore indicated in patients resistant to CC or Letrozole and especially if a diagnostic laparoscopy is needed for other indications, such as the evaluation of tubal patency. However, similar to any surgical procedure, it can be associated with numerous post-operative complications, including the formation of intra-abdominal adhesions and the reduction of the ovarian reserve if the procedure is not performed correctly.
5.5.7 Gonadotropins and IVF
Gonadotropins (Follicle Stimulating Hormone (FSH) or Human Menopausal Gonadotropin (HMG)) represent a good putative treatment for patients with PCOS and anovulation, in which Clomiphene or Letrozole has not been effective. Such treatments are classically performed in ART (Assisted Reproductive Techniques).
Exogenous gonadotropins work by increasing circulating FSH levels and stimulating directly follicular growth. The recommended starting dose in PCOS patients to avoid hyperstimulation is 37.5–75 IU/day [39]; in particular the identification of the optimal dose is generally obtained after a few stimulation cycles following several attempts. Subsequently, when the follicles reach an average diameter of 18 mm, a single dose of hCG-r 250 μg or hCG-u 5000 IU is used to trigger ovulation. If the recruited follicles are too numerous (3 or more follicles greater than 14 mm in diameter), the hCG is not administered to avoid the risk of ovarian hyperstimulation or multiple pregnancies. The treatment should be repeated up to a maximum of 6 cycles. Using low-dose step-up protocols, the ovulation of a single follicle rate is nearly 70%, while pregnancy rate is 20% per cycle [39].
A recent Cochrane review [50] compared the effectiveness of various gonadotropin preparations in women with PCOS resistant to Clomiphene and showed no differences in terms of live birth rates or incidence of OHSS (urinary FSH, recombinant FSH, or HMG), demonstrating that outcomes are linked more on the administered dose of gonadotropins than on the preparation used. Combination therapy with Metformin has been shown to be effective in improving the effects of gonadotropins, increasing the live birth rates compared to administration of gonadotropins alone (OR 2.46, 95% CI 1.36 to 4.46) [51].
Exogenous gonadotropins are clearly more effective in promoting pregnancy than Clomiphene; however they are particularly expensive drugs with possible side effects (OHSS, multiple pregnancies); therefore they should be administered under strict ultrasound monitoring.Ovarian stimulation associated with IVF techniques is considered the third-line treatment in PCOS patients with chronic anovulation, especially recommended if other infertility factors are associated such as tubal pathologies, male subfertility, advanced woman age, and severe endometriosis [39].Single embryo-transfer procedure is essential to reduce the risk of multiple pregnancies, which is one of the most frequent complications when using gonadotropins.
Despite the high number of cycles suspended in PCOS patients, pregnancy and live births rate is comparable to those of non-PCOS women [52]. The use of GnRH antagonists also reduces the risk of ovarian hyperstimulation syndrome (OHSS), whose incidence is significantly higher in PCOS patients (15% vs 3%) [53].
5.5.8 Inositols
Recently the approach to PCOS has considered the possibility to treat the insulin resistance with specific integrative compounds that can counteract the metabolic impairment(s) that trigger anovulation and/or menstrual irregularities. In this perspective, inositols, in particular myo-inositol (MI) and D-chiro-inositol (DCI), the two most important isoforms, have become widely used in these last years.
Inositol is a molecule structurally similar to glucose. It is involved in numerous biological processes including transmission of insulin post-receptor signaling as well as in other protein hormones such as TSH and FSH [17]. It can be either taken with diet or synthesized by the human body. Both myo-inositol and D-chiro-inositol have the same chemical structure and differ only in the position of the hydroxyl group: in vivo, DCI is synthesized starting from MI by an epimerase, whose functionality or expression is probably reduced in hyperinsulinemic PCOS patients especially in case of familial diabetes [17]. In fact supplementation with MI or DCI or a combination of these products significantly improves the metabolic profile in PCOS patients, but in presence of diabetic relatives DCI seems to be more effective [17, 54].
Myo-inositol can be synthesized starting from glucose-6-phosphate, which is isomerized and then dephosphorylated [55], but the greater portion comes from the diet. At the intracellular level myo-inositol is transformed into phosphatidyl-myo-inositol, a precursor of inositol 3-phosphate, which acts as a intracellular second messenger in the cascade triggered by various peptide hormones [56, 57, 58]: in fact, the inositols are second messengers not only of the intracellular insulin signaling pathway, to reduce plasma levels via a greater cellular glucose uptake especially in the liver and skeletal muscles, but also of other protein hormones such as TSH and FSH [17, 59]. This aspect is relevant, since inositol administration can also improve the hormonal profile in terms of reproductive capacity, thanks to a better transduction of the FSH signal at the ovarian level.
Inositols take part in different ways in the post-receptor insulin-induced signal. There are two main routes in transmission of the metabolic signal of insulin: one is phosphatidyl-inositol 3-phosphate pathway, which through various steps activates a protein kinase PKB/Akt, allowing the translocation of GLUT-4 vesicles to the plasma membrane, to increase glucose transport into the cells through a facilitated diffusion mechanism, essentially in skeletal and cardiac muscle and in adipose tissue [60]; the other pathway is mediated by the G protein, which triggers a series of steps that lead to the release of a DCI molecule, which favors the glycogen storage in the cytosol and glucose oxidative use in the mitochondria. Therefore, the action of the two main inositol isoforms is very relevant in the control of numerous peptide hormone signals, as well as a diet that guarantees an adequate intake and a good MYO-to-DCI conversion mechanism through the epimerase activity [60]. Considering that inositol promotes mechanisms of glucose transport into the cells, glucose oxidative use, and glycogen storage, it is necessary to consider the possibility of its integrative use in diabetes and in PCOS (Fig. 5.2).
Schematic representation of insulin signaling proposed by Larner et al. (modified from [17]). The insulin binding to its receptor (IR) activates a signal via two different and parallel pathways. In the first pathway, the substrates of the insulin receptor (IRS) activate various proteins (PI3K, PDK, PKB/Akt) in order to activate PKB/Akt and induce glucose transporter 4 (GLUT-4) translocation to the plasma membrane to upload glucose. The second pathway IR via G protein (Gp) causes the hydrolysis of glycosylphosphatidylinositol (GPI), which releases an inositol phosphoglycan containing D-chiro-inositol, which acts as second messenger of insulin (INS-2). INS-2 enhance glucose storage (GS) as glycogen in the cytosol and also glucose oxidative use in the mitochondria. Relevant the fact that mitochondria synthetize alpha lipoic acid (ALA) that activates PKB/Akt independently from insulin signal. (modified from [17]). GSK3 Glycogen synthase kinase 3, PDH pyruvate dehydrogenase, PDHP pyruvate dehydrogenase phosphatase, PDK phosphoinositide-dependent kinase, PI3K phosphoinositide 3 kinase, PKB/Akt protein kinase B/Akt, PP2Ca phosphoprotein phosphatase 2C alpha
The amount of MYO present inside the cells is in balance with the other isoforms and when required is transformed as previously described into DCI by an epimerase which acts in a tissue-specific manner and therefore guarantees the useful conversion in the various districts [18]. In diabetes or insulin resistance, a lower amount of DCI was found in urine and in insulin-sensitive tissues than in the general population, thus demonstrating that an abnormal epimerase function/expression may exist, contributing to the worsening of insulin resistance and compensatory hyperinsulinemia [19]. In 1999 Nestler administered 1200 mg/day of DCI to obese PCOS patients for 8 weeks and demonstrated an improvement of insulin sensitivity and reduced circulating levels of androgens; subsequently it was shown that DCI increased the occurrence of ovulatory cycles and was also effective in normal-weight PCOS [61]. Other authors have subsequently shown a predominant role of MYO at ovarian level, positively correlating with oocyte quality and estradiol concentration in the follicular fluid [62]; in fact, in PMA cycles MYO improves oocytes and embryos qualities [63], so certainly the ovarian metabolic and endocrine pattern does not require high concentrations of DCI [64]. However, most of the organs like liver, skeletal muscle, and kidneys need DCI, since it plays a role for the correction of insulin resistance, fundamental for the good functioning of the reproductive system.
In 2012 Unfer [63] summarized the outcomes of 21 studies and observed that the administration of MYO in PCOS patients improved metabolic and hormonal parameters, reduced BMI, and promoted menstrual cycle and fertility [63]. However, in 2012 it was shown that MYO, when administered to obese PCOS patients with regular fasting insulin values (<12 microU/ml), did not induce improvements on the metabolic profile in terms of insulin response to oral glucose load, demonstrating that obesity alone is not sufficient to justify hyperinsulinemia, which is probably due to a deficit of synthesis/release of DCI-IPG [65], suggesting MYO was not metabolically effective in all patients. So the activity/expression of the epimerase enzyme was suspected to be altered in diabetic or PCOS patients with diabetic relatives [66], suggesting that DCI may be more effective in these subjects. Indeed it has been shown that daily DCI administration at the dosage of 500 mg improves insulin sensitivity in all patients with insulin resistance more efficiently in PCOS patients with familial diabetes [67, 68].
Therefore both MYO and DCI seem to be potentially effective, but the presence of diabetic relatives must be discriminant in the choice of their use, as in these subjects the conversion of MYO to DCI may not be optimal [67, 68]. Since DCI has strong metabolic effects, while MYO perform an important action in ovary, in some cases it could be useful to supplement a combination of both. A recent Consensus Conference proposed the use of a combination of them, close to their physiological plasma concentrations, guaranteeing systemic and ovarian benefits [69] and the prevention of the metabolic syndrome as well the risk of gestational diabetes.A recent meta-analysis, including 10 RCTs and 601 women [70], showed that supplementation with inositol improves the ovulatory rate and frequency of menstrual cycle compared to placebo. However, a recent review denies these data in terms of reproductive outcomes [71]: inositol, administered to PCOS patients undergoing ICSI cycles, does not improve oocyte quality and pregnancy rates, while DCI seems to have controversial role.
In conclusion, there are numerous evidences that demonstrate the efficacy of these integrative products and that both are able to modulate the reproductive and metabolic function in PCOS patients: according to a recent review [17] anamnestic data might be relevant to the choice of inositol integration, so we have to investigate diabetes predisposition and/or familial diabetes. It is advisable to evaluate this therapeutic option especially considering that it has no side effects and can be associated with lifestyle modification, and in combination with Metformin or ovulation induction treatments.
5.5.9 Alpha-Lipoic Acid
Recently another product was reported to be of great interest in the management of insulin resistance in PCOS patients, that is, alpha-lipoic acid (ALA). In animal models ALA modulates and increases the use of glucose via the activation of AMPK (adenosine monophosphate-activated protein kinase) in skeletal muscle and favoring the activation of GLUT-4 [72, 73]. Recently it has also been proposed as an adjuvant therapy in several endocrinopaties including diabetes [74, 75].
We recently reported that the administration of 400 mg of ALA per day was able to improve insulin sensitivity in obese PCOS patients, regardless of the presence of diabetic relatives [76]. In fact ALA induced a significant reduction in insulin levels after oral glucose load both in patients with or without diabetic relatives. Recent studies have shown that the lipoic acid synthase (LASY), responsible for the lipoic acid synthesis at the mitochondrial level in mammals as well as in humans, is poorly expressed in case of type I and II diabetes [77, 78]. The endogenous ALA modulates the use of glucose, activating the enzyme AMPK in skeletal muscle [17], which in turn activates GLUT-4, the main glucose transporter into the cells [73], reducing the amount of insulin necessary to maintain correct blood glucose levels (Fig. 5.2). Indeed we have shown that the exogenous administration of ALA, probably through the above described mechanism, corrects insulin resistance in PCOS patients. Our data showed that insulin sensitivity improves after treatment with ALA in all PCOS patients, especially in patients with diabetic relatives, probably because in these patients there is a defect of endogenous synthesis of ALA due to the defect of the enzyme responsible for its production, as previously discussed [77, 78].
Interestingly only in patients with diabetic relatives, a significant reduction of plasma triglyceride and transaminase levels was observed. These last are generally at the higher limits of normality, thus supporting the hypothesis that ALA has its own specific efficacy in the liver, in particular reducing the risk of steatosis classically described as NAFLD (nonalcoholic fatty liver disease). It should be observed that under treatment with ALA no changes in hormonal parameters were observed, that is, no change in terms of gonadotropin or androgen plasma levels, consequently no improvement in hormonal and reproductive profiles.
However, it remains a product of great importance for the correction of metabolic impairments of PCOS patients, improving insulin sensitivity and protecting liver function, thus preventing the onset of NAFLD and diabetes. It is therefore a useful strategy to combine ALA with MYO or DCI, as recently reported in our recent studies, which demonstrated the high metabolic and endocrine/reproductive efficiency of both the associations [79, 80]. Indeed, considering that innumerable studies have nowadays demonstrated inositol efficacy in the correction of metabolic status, hormonal values, and therefore fertility, it is advisable to evaluate the integrative option of the association with alpha-lipoic acid, evaluating anamnestic history, in particular the presence of diabetic relatives.
5.6 Conclusions
The available options to induce ovulation in PCOS patients are a lot and various: side effects, costs, and compliance of the patients need to be attentively evaluated, to have a personalized tailored choice, considering the clinical history and previous attempts, but also carefully evaluating the clinical and familial story, BMI, and PCOS phenotype. Considering the specific physiopathological characteristics of PCOS, it is essential that physicians take them in great consideration to make the best choice of treatment for the PCOS patient.
References
Norman RJ, Dewailly D, Legro RS. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97.
Teede HJ. Recommendations from the international evi-dence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. Published online July 19, 2018. 2018; https://doi.org/10.1093/humrep/dey256.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus WorkshopGroup. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 2004; 81(1): p. 19–25.
Ciampelli M, Fulghesu AM, Cucinelli F, Pavone V, Ronsisvalle E, Guido M, Caruso A, Lanzone A. Impact of insulin and body mass index on metabolic and endocrine variables in polycystic ovary syndrome. Metabolism. 1999;48:167–72.
Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, Carmina E, Chang J, Yildiz BO, Laven JS, Boivin J, Petraglia F, Wijeyeratne CN, Norman RJ, Dunaif A, Franks S, Wild RA, Dumesic D, Barnhart K. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-sponsored 3rd PCOS consensus workshop group. Fertil Steril. 2012;97:28–38.
Genazzani AD, Ricchieri F, Lanzoni C. Use of metformin in the treatment of polycystic ovary syndrome. Womens Health (Lond). 2010;6:577–93.
Joham AE, et al. Polycystic ovary syndrome, obesity, and pregnancy. Semin Reprod Med. 2016;34:93–101.
Genazzani AD, Vito G, Lanzoni C, Strucchi C, Mehmeti H, Ricchieri F, Mbusnum MN. La Sindrome metabolica Menopausale. Giorn. It. Ost. Gin. 2005;11/12:487–93.
The Pathogenesis of Polycystic Ovary Syndrome (PCOS): The Hypothesis of PCOS as Functional Ovarian Hyperandrogenism Revisited. Robert L. Rosenfield and David A. Ehrmann. Endocrine Reviews, October 2016, 37(5):467–520.
Ciaraldi TP, el Roeiy A, Madar Z, Reichart D, Olefsky JM, Yen SS. Cellular mechanisms of insulin resistance in polycystic ovarian syndrome. J Clin Endocrinol Metab. 2002;75:577–83.
Araùjo TG, Oliveira AG, Saad MJ. Insulin-resistance-associated compensatory mechanisms of pancreatic Beta cells: a current opinion. Front Endocrinol (Lausanne). 2013;4:146.
Sliwowska JH, Fergani C, Gawałek M, Skowronska B, Fichna P, Lehman MN. Insulin: its role in the central control of reproduction. Physiol Behav. 2014;133:197–206. Epub 2014 May 27
Walters KA, Gilchrist RB, Ledger WL, Teede HJ, Handelsman DJ, Campbell RE. New perspectives on the pathogenesis of PCOS: neuroendocrine origins. Trend in Endocrinology and metabolism. in press
Navarro VM. New insights into the control of pulsatile GnRH release: the role of Kiss1/neurokinin B neurons. Front Endocrinol (Lausanne). 2012;3:48.
Walters KA, et al. The role of central androgen receptor actions in regulating the hypothalamic–pituitary–ovarian axis. Neuroendocrinology. 2018;106:389–400.
Lan ZJ, Krause MS, Redding SD, Li X, Wu GZ, Zhou HX, Bohler HC, Ko C, Cooney AJ, Zhou J, Lei ZM. Selective deletion of Pten in theca-interstitial cells leads to androgen excess and ovarian dysfunction in mice. Mol Cell Endocrinol. 2017;444:26–37. Epub 2017 Jan 28
Genazzani AD. Inositol as putative integrative treatment for PCOS. Reprod Biomed Online. 2016;33:770–80.
Larner J. D-chiro-inositol: its functional role in insulin action and its deficit in insulin resistance. Int J Exp Diabetes Res. 2002;3:47–60.
Baillargeon JP, Nestler JE. Commentary: polycystic ovary syndrome: a syndrome of ovarian hypersensitivity to insulin? J Clin Endocrinol Metab. 2006;91:22–4.
Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): the hypothesis of PCOS as functional ovarian Hyperandrogenism revisited. Endocr Rev. 2016;37(5):467–520.
Raiane P. Crespo, Tania A. S. S. Bachega, Berenice B. Mendonça, Larissa G. Gomesl. An update of genetic basis of PCOS pathogenesis. Arch Endocrinol Metab. 2018;62/3.
Cooper HE, Spellacy WN, Prem KA, Cohen WD. Hereditary factors in the stein-Leventhal syndrome. Am J Obstet Gynecol. 1968;100(3):371–87.
Kahsar-Miller MD, Nixon C, Boots LR, Go RC, Azziz R. Prevalence of polycystic ovary syndrome (PCOS) in first-degree relatives of patients with PCOS. Fertil Steril. 2001;75(1):53–8.
Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI. Heritability of polycystic ovary syndrome in a Dutch twin-family study. J Clin Endocrinol Metab. 2006;91(6):2100–4.
Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, et al. Finding the missing heritability of complex diseases. Nature. 2009;461(7265):747–53.
de Bruin C, Dauber A. Insights from exome sequencing for endocrine disorders. Nat Rev Endocrinol. 2015;11(8):455–64.
Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011;7:CD007506.
Balen AH, Morley LC, Misso M, Franks S, Legro RS, Wijeyaratne CN, et al. The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Hum Repr Update. 2016;22:687–708.
Poehlman ET, Dvorak RV, DeNino WF, Brochu M, Ades PA. Effects of resistance training and endurance training on insulin sensitivity in nonobese, young women: a controlled randomized trial. The Journal of Clinical Endocrinol and Metab. 2000;85:2463–8.
Naderpoor N, Shorakae S, de Courten B, Misso ML, Moran LJ, Teede HJ. Metformin and lifestyle modification in polycystic ovary syndrome: systematic review and meta-analysis. Hum Reprod Update. 2015;21:560–74.
Malik SM, Traub ML. Defining the role of bariatric surgery in polycystic ovarian syndrome patients. World J Diabetes. 2012;3:71–9.
Johansson K, Cnattingius S, Näslund I, Roos N, Trolle-Lagerros Y, Granath F, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814–24.
Morley LC, Tang T, Yasmin E, Norman RJ, Balen AH. Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database Syst Rev. 2017;11:CD003053.
Practice Committee of the American Society for Reproductive Medicine. Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): a guideline. Fertil Steril. 2017; 108(3).
Siebert TI, Viola MI, Steyn DW, Kruger TF. Is metformin indicated as primary ovulation induction agent in women with PCOS? A systematic review and metaanalysis. Gynecol Obstet Investig. 2012;73:304–13.
Palomba S, Falbo A, La Sala GB. Effects of metformin in women with polycystic ovary syndrome treated with gonadotrophins for in vitro fertilisation and intracytoplasmic sperm injection cycles: a systematic review and meta-analysis of randomised controlled trials. BJOG. 2013;120(3):267–76.
Huang X, Wang P, Tal R, Lv F, Li Y, Zhang X. A systematic review and metaanalysis of metformin among patients with polycystic ovary syndrome undergoing assisted reproductive technology procedures. Int J Gynaecol Obstet. 2015;131:111–6.
Abu Hashim H, Foda O, Ghayaty E. Combined metformin clomiphene in clomiphene-resistant polycystic ovary syndrome: a systematic review and metaanalysis of randomized controlled trials. Acta Obstet Gynecol Scand. 2015;94:921–30.
Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome. Hum. Reprod. 2008; 23: p. 462–77.
Wang R, Kim BV, van Wely M, Johnson NP, Costello MF, Zhang H, et al. Treatment strategies for women with WHO group II anovulation: systematic review and network meta-analysis. BMJ. 2017;356:j138.
Gadalla MA, Huang S, Wang R, Norman RJ, Abdullah SA, El Saman AM, et al. Effect of clomiphene citrate on endometrial thickness, ovulation, pregnancy and live birth in anovulatory women: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(1):64–76.
Brown J, Farquhar C. Clomiphene and other antioestrogens for ovulation induction in polycystic ovarian syndrome. Cochrane Database Syst Rev. 2016;12:CD002249.
Fields E, Chard J, James D, Treasure T. Guideline Development Group. Fertility (update): summary of NICE guidance. BMJ. 2013; 346: p. 650.
Tulandi T, Martin J, Al-Fadhli R, Kabli N, Forman R, Hitkari J, Librach C, Greenblatt E, Casper RF. Congenital malformations among 911 newborns conceived after infertility treatment with letrozole or clomiphene citrate Fertil Steril. 2006;85(6):1761–5. Epub 2006 May 2.
Hu S, Yu Q, Wang Y, Wang M, Xia W, Zhu C. Letrozole versus clomiphene citrate in polycystic ovary syndrome: a meta-analysis of randomized controlled trials. Arch Gynecol Obstet. 2018;297(5):1081–8.
Legro RS, Brzyski RG, Diamond MP, Coutifaris C, Schlaff WD, Casson P, et al. NICHD reproductive medicine network. Letrozole versus clomiphene for infertility in the polycystic ovary syndrome. N. Engl. J. Med. 2014;371(2):119–29.
Hueb CK, Dias-Junior JA, Abrão MS, Filho EK. Drilling: medical indications and surgical technique. Rev Assoc Med Bras. 2015;61:530–5.
Seow KM, Juan CC, Hwang JL, Ho LT. Laparoscopic surgery in polycystic ovary syndrome: reproductive and metabolic effects. Semin Reprod Med. 2008;26(1):101–10.
Farquhar C, Brown J, Marjoribanks J. Laparoscopic drilling by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2012;6:CD001122.
Weiss NS, Nahuis M, Bayram N, Mol BW, Van der Veen F, van Wely M. Gonadotropins for ovulation induction in women with polycystic ovarian syndrome. Cochrane Database Syst Rev. 2015;9:CD010290.
Bordewijk EM, Nahuis M, Costello MF, Van der Veen F, Tso LO, Mol BW, et al. Metformin during ovulation induction with gonadotrophins followed by timed intercourse or intrauterine insemination for subfertility associated with polycystic ovary syndrome. Cochrane Database Syst Rev. 2017;24(1):CD009090.
Li HW, Lee VC, Lau EY, Yeung WS, Ho PC, Ng EH. Cumulativen live-birth rate in women with polycystic ovary syndrome or isolated polycystic ovaries undergoing in-vitro fertilisation treatment. J Assist Reprod Genet. 2014;31:205–11.
Soave I, Marci R. Ovarian stimulation in patients in risk of OHSS. Minerva Ginecol. 2014;66(2):165–78.
Baillargeon JP, Diamanti-Kandarakis E, Ostlund RE Jr, Apridonidze T, Iuorno MJ, et al. Altered d-chiro-inositol urinary clearance in women with polycystic ovary syndrome. Diabetes Care. 2006;29:300–5.
Loewus MW, Wright RW Jr, Bondioli KR, Bedgar DL, Karl A. Activity of myo-inositol-1-phosphate synthase in the epididymal spermatozoa of rams. J Reprod Fertil. 1983;69:215–20.
Buttner J. Johann Joseph von Scherer (1814–69). The early history of clinical chemistry. J Clin Chem Clin Biochem. 1978;16:478–83.
Thomas RM, Nechamen CA, Mazurkiewicz JE, Ulloa-Aguirre A, Dias JA. The adapter protein APPL1 links FSH receptor to inositol 1,4,5-trisphosphate production and is implicated in intracellular Ca2_ mobilization. Endocrinology. 2011;152:1691–701.
Unfer V, Proietti S, Gullo G, Porcare G, Carlomagno G, Bizzarri M. Polycystic ovary syndrome: features, diagnostic criteria and treatments. Endocrinol Metab Synd. 2014;3:2. https://doi.org/10.4172/2161-1017.1000136.
Thomas RM, Nechamen CA, Mazurkiewicz JE, Ulloa-Aguirre A, Dias JA. The adapter protein APPL1 links FSH receptor to inositol 1,4,5-trisphosphate production and is implicated in intracellular ca(2+) mobilization. Endocrinology. 2011;152:1691–701.
Croze ML, Soulage CO. Potential role and therapeutic interests of myo-inositol in metabolic diseases. Biochimie. 2013;95:1811–27.
Iuorno MJ, Jakubowicz DJ, Baillargeon JP, Dillon P, Gunn RD, Allan G, Nestler JE. Effects of d-chiroinositol in lean women with the polycystic ovary syndrome. Endocr Pract. 2002;8:417–23.
Chiu TT, Rogers MS, Law EL, Briton-Jones CM, Cheung LP, Haines CJ. Follicular fluid and serum concentrations of myo-inositol in patients undergoing IVF: relationship with oocyte quality. Hum Reprod. 2002;17:1591–6.
Unfer V, Carlomagno G, Dante G, Facchinetti F. Effects of myo-inositol in women with PCOS: a systematic review iof randomized controlled trials. Gynecol Endocrinol. 2012;28:509–15.
Rosalbino I, Raffone E. Does ovary need D-chiroinositol? J Ovarian Res. 2012;5:14.
Cheang KI, Baillargeon JP, Essah PA, Ostlund RE Jr, Apridonize T, Islam L, Nestler JE. Insulin-stimulated release of D-chiro-inositol-containing inositolphosphoglycan mediator correlates with insulin sensitivity in women with polycystic ovary syndrome. Metab Clin Exp. 2008;57:1390–7.
Larner J, Brautigan DL, Thorner MO. D-chiro-inositol glycans in insulin signaling and insulin resistance. Mol Med. 2010;16:543–52.
Genazzani AD, Santagni S, Rattighieri E, Chierchia E, Despini G, Marini G, Prati A, Simoncini T. Modulatory role of D-chiro-inositol (DCI) on LH and insulin secretion in obese PCOS patients. Gynecol Endocrinol. 2014b;30:438–43.
La Marca A, Grisendi V, Dondi G, Sighinolfi G, Cianci A. The menstrual cycle regularization following D-chiro-inositol treatment in PCOS women: a retrospective study. Gynecol Endocrinol. 2015;31:52–6.
Facchinetti F, Bizzarri M, Benvenga S, D'Anna R, Lanzone A, Soulage C, et al. Results from the international consensus conference to on myo-inositol and dchiroinositol in obstetrics and gynecology: the link between metabolic syndrome and PCOS. European Journal of Obstet., Gynecol., Reprod. Biol. 2015; 195: p. 72e6.
Pundir J, Psaroudakis D, Savnur P, Bhide P, Sabatini L, Teede H, et al. Inositol treatment of anovulation in women with polycystic ovary syndrome: a meta-analysis of randomised trials. BJOG. 2018;125(3):299–308.
Mendoza N, Pérez L, Simoncini T, Genazzani A. Inositol supplementation in women with polycystic ovary syndrome undergoing intracytoplasmicsperm injection: a systematic review and meta-analysis of randomized controlled trials. Reprod Biomed Online. 2017;35(5):529–35.
Lee WJ, Song KH, Koh EH, Won JC, Kim HS, et al. Alphalipoic acid increases insulin sensitivity by activating AMPK in skeletal muscle. Biochem Biophys Res Commun. 2005;332:885–91.
Shen QW, Zhu MJ, Tong J, Ren J, Du M. Ca2+/calmodulindependent protein kinase kinase is involved in AMP-activated protein kinase activation by alpha-lipoic acid in C2C12 myotubes. Am J Physiol Cell Physiol. 2007;293:C1395–403.
Gomes MB, Negrato CA. Alpha-lipoic acid as a pleiotropic compound with potential therapeutic use in diabetes and other chronic diseases. Diabetol Metab Syndr. 2014;6(1):80. https://doi.org/10.1186/1758-5996-6-80.
Scaramuzza A, Giani E, Radaelli F, Ungheri S, Macedoni M, Giudici V, Bosetti A, Ferrari M, Zuccotti GV (2015) Alpha-lipoic acid and antioxidant diet help to improve endothelial dysfunction in adolescents with type 1 diabetes: a pilot study. J Diabetes Res. https://doi.org/10.1155/2015/474561.
Genazzani AD, Shefer K, Della Casa D, Prati A, Napolitano A, Manzo A, Despini G, Simoncini T. Modulatory effects of alpha-lipoic acid (ALA) administration on insulin sensitivity in obese PCOS patients. J Endocrinol Investig. https://doi.org/10.1007/s40618-017-0782-z.
Morikawa T, Yasuno R, Wada H. Do mammalian cells synthesize lipoic acid? Identification of a mouse cDNA encoding a lipoic acid synthase located in mitochondria. FEBS Lett. 2001;498:16–21.
Padmalayam I, Hasham S, Saxena U, Pillarisetti S. Lipoic acid synthase (LASY): a novel role in inflammation, mitochondrial function, and insulin resistance. Diabetes. 2009;58:600–8.
Genazzani AD, Prati A, Santagni S, Ricchieri F, Chierchia E, Rattighieri E, Campedelli A, Simonicini T, Artini PG. Differential insulin response to myo-inositol administration in obese polycystic ovary syndrome patients. Gynecol Endocrinol. 2012 Dec;28(12):969–73. https://doi.org/10.3109/09513590.2012.685205.
Genazzani AD, Prati A, Simoncini T, Napolitano A. Modulatory role of D-chiro-inositol and alpha lipoic acid combination on hormonal and metabolic parameters of overweight/obese PCOS patients. Eur Ginecol Obstet. in press
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 International Society of Gynecological Endocrinology
About this chapter
Cite this chapter
Prati, A., Genazzani, A.R., Genazzani, A.D. (2021). Pathogenesis of PCOS: From Metabolic and Neuroendocrine Implications to the Choice of the Therapeutic Strategy. In: Genazzani, A.R., Ibáñez, L., Milewicz, A., Shah, D. (eds) Impact of Polycystic Ovary, Metabolic Syndrome and Obesity on Women Health. ISGE Series. Springer, Cham. https://doi.org/10.1007/978-3-030-63650-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-63650-0_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-63649-4
Online ISBN: 978-3-030-63650-0
eBook Packages: MedicineMedicine (R0)