Abstract
Anticoagulants are widely used, especially in the elderly, for the prevention and treatment of thromboembolic complications and in high-risk post myocardial infarction. Above all, Vitamin K antagonists (VKAs) are predominantly prescribed in the general population. Unfortunately, due to VKAs intrinsic pharmacodynamic and pharmacokinetic properties (high interindividual variability, food interaction, narrow therapeutic window), routine management of VKAs can be challenging both for the patients and for the clinicians, consequently, the number of patients taking non-vitamin K oral anticoagulants (i.e., direct oral anticoagulants) is increased in the last years. In fact, direct oral anticoagulants (DOACs) have progressively been used owing to their shorter half-lives, rapid onset, and predictable pharmacodynamics.
In the elderly, the incidence of pharmacologically induced coagulopathy, in trauma or emergency invasive procedure, is responsible for a huge increase of bleeding complications that can be life-threatening. Consequently, the perioperative management of patients taking anticoagulant agents and undergoing surgery is particularly challenging. A precise balance has to be reached between the risk of bleeding and the risk of thromboembolism. Then, when a decision of stopping anticoagulant has been made, it is vital to determine the time of anticoagulation interruption, resumption, and the necessity of bridging. Furthermore, in emergency scenario, the reversal of the anticoagulant should be mandatory, not only to prevent but also to treat perioperative bleeding. In this situation, a specific reversal strategy has to be chosen on the basis of the type of anticoagulants.
In this chapter, we aimed to provide an overview of the current knowledge regarding the perioperative management of patients receiving anticoagulants and undergoing surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Oral anticoagulant therapy
- Vitamin K antagonists
- Direct oral anticoagulants
- Perioperative management
- Bleeding
- Thromboembolism
- Prothrombin complex concentrate
- Reversal of anticoagulation
- Invasive procedures
- Emergency surgery
1 Introduction
The perioperative management of patients receiving anticoagulant represents a real challenge in a daily clinical setting, especially in case of emergency invasive procedure. Interruption of anticoagulant increase thromboembolic risk; however, continuing anticoagulation increases the risk of bleeding associated with invasive procedures, both affecting mortality. The perioperative management is based on the balance between reducing the risk of thromboembolism and prevevnting excessive bleeding. The decision and the timing of the interruption are influenced by patient’s characteristic, type of surgery, type of anesthesia (i.e., general anesthesia, neuraxial anesthesia), and type of anticoagulants. Even if not conclusive, preliminary data suggests that the bleeding rate differs between different types of anticoagulants [1, 2]. Unfortunately, especially in the emergency setting, there is a lack of well designed clinical trials, consequently, the decision of anticoagulant interruption and reversal is often based on scarce evidence or routine clinical experience.
Once the decision of anticoagulant interruption has been made, additional issues to cope with are represented by the timing of the interruption and the necessity of bridging with a shorter-acting drug. The timing is strictly related to specific anticoagulant used, due to its half-lives and metabolism. Premature withdrawal is strictly connected to an increased risk of thromboembolism events (e.g., venous thromboembolism-VTE); however, at the same time, the agent should be stopped in sufficient time to obtain marginal or no residual anticoagulant effect to minimize bleeding complications [3,4,5]. Moreover, not only the appropriate time of interrupting perioperatively but also the proper time to resume anticoagulants postoperatively is challenging. Bridging anticoagulation consists of the administration of short-acting anticoagulant drugs, generally, subcutaneous injection of low-molecular-weight heparin (LMWH) or intravenous administration of unfractionated heparin (UFH), started on the day of vitamin K antagonists (VKAs) interruption in order to reduce thromboembolic complications [6, 7]. Unfortunately, bridging anticoagulation may increase periprocedural bleeding, then, bridging has to be reserved for patients with high thromboembolic risk (e.g., mechanical valve, high CHADS2 score, VTE in the previous 3 months) [8, 9].
Warfarin and other vitamin k antagonists are extensively used. The indications of VKAs are represented by prophylaxis and treatment of thromboembolic complications associated with atrial fibrillation (AF) and/or cardiac valve replacement; prophylaxis and treatment of venous thrombosis and pulmonary embolism (PE); Antiphospholipid syndrome; and high-risk post Myocardial infarction [10]. VKAs present several disadvantages. They require frequent monitoring (i.e., INR), have a narrow therapeutic range, and present several drug and food interactions. In the last years, in addition to heparin and VKAs, several new agents for the prevention and management of thromboembolic disease are released in the market. Direct oral anticoagulants (DOACs) include direct thrombin inhibitors (dabigatran, lepirudin, argatroban, desirudin, bivaluridin) and direct factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban). DOACs are currently approved for the treatment of VTE, VTE prophylaxis in orthopedic surgery, prevention of stroke, and thromboembolism in non-valvular atrial fibrillation [11, 12]. These drugs are not indicated in patients with severe renal impairment, with prosthetic heart valve, pregnancy, and antiphospholipid syndrome. DOACs pose specific new challenge because they present individual characteristics, pharmacokinetics, pharmacodynamics, and bleeding risks [12]. The advantages of DOACs include rapid onset, wide therapeutic window, shorter half-lives, and no food interactions without the necessity of coagulation monitoring. However, these drugs present liver or renal metabolism, consequently, DOACs have to be used with caution in patients with liver or renal impairment [13]. Not to be underestimated, recent studies have found interindividual variability in plasma drug levels of DOACs. The patients have a higher bleeding risk when the serum concentration of these drugs is high, whereas the patients present a high risk of thromboembolism when the serum concentration is low. Consequently, pharmacogenomics of DOACs and drug interaction can contribute to increasing the bleeding risk or the thrombotic risk of patients [14]. Even more, besides for Dabigatran, no specific antidote is available for DOACs.
Finally, the reversal of the anticoagulant could be required for emergency procedures, not only to prevent but also to treat perioperative bleeding. Conventionally, fresh frozen plasma (FFP) has been widely used as VKAs reversal agent. Furthermore, Prothrombin complex concentrates (PCC) represents an alternative strategy in order to reverse the effects of anticoagulation treatment. PCC contains coagulation factors II, IX, X, and VII derived from pooled plasma. Comparison between FFP and PCC [15, 16] shows that the use of PCC allows the reduction of volume requirements, thus preventing fluid overload, and the decrease of adverse immune-related risks. Other anticoagulant reversal option includes protamine, phytonadione, hemodialysis, oral-activated charcoal, antifibrinolytic agents (tranexamic agents, desmopressin). Even more, a specific reversal agent, Idarucizumab, is available for the reversal of Dabigatran [17].
2 Thrombotic Risk Vs. Bleeding Risk
Interruption of anticoagulant temporarily increases thromboembolic risk, consequently, it is vital to estimate the thromboembolic risk of a patient in order to decide whether to interrupt it or not. Evaluating thromboembolic risk is the first step in order to optimize perioperative antithrombotic management. Thromboembolic risk is categorized into low, moderate, and high-risk categories (Table 5.1).
The major factors that increase thromboembolic risk are:
-
Patients with atrial fibrillation: CHA2DS2VASCc (Congestive heart failure, Hypertension, Age > 75 years, Diabetes mellitus, Stroke or transient ischemic attack, or thromboembolism, vascular disease, sex category) calculates the stroke risk for patients with AF [18]. CHA2DS2VASc represented the updated version of CHADS2 score, providing a better stratification of low-risk patients [19, 20]. CHA2DS2VASc score includes the following stroke risk factors: congestive heart failure/left ventricular dysfunction, hypertension, age ≥ 75, diabetes, stroke, vascular disease, age 65–74, and sex category (female). The maximum score is 9. A CHA2DS2VASc of 0 (or 1 in female) outlines a low-risk patient not requiring anticoagulant agents. In males with CHA2DS2VASc of 3–4 the risk is moderate and oral anticoagulation should be considered. Finally, in case of a patient with a CHA2DS2-VASc score of 6 and above, oral anticoagulation therapy with a Vitamin K Antagonist (in case of valvular AF) or one of the non-VKA oral anticoagulant drugs (in case of non-valvular AF) is recommended [18]. The decision for thromboprophylaxis needs to be balanced with the risk of major bleeding, especially ICH. Above all HAS-BLED (Hypertension, Abnormal renal and liver function, Stroke, Bleeding, Labile INR, Elderly, Drugs or alcohol) is recommended for bleeding risk assessment (see below). It is important to highlight that CHA2DS2-VASc score has not been prospectively validated in the perioperative setting; however, it can be used to assess thromboembolic risk and the necessity of heparin bridging.
-
Prosthetic heart valves: prosthesis-related complications include embolic events, thrombosis, regurgitation, hemolytic anemia, patient-prosthesis mismatch. The anticoagulant agents indicated to prevent thrombosis and thromboembolic events are VKAs and heparin [21]. The risk of thrombosis is highest in the first months after surgical valve repair, consequently, all elective invasive procedures have to be postponed at least 3 months after valve surgery. In case of VKAs interruption, bridging with heparin has to be considered. In particular, International Normalized Ratio (INR) value should guide the decision on drug interruption, the necessity of bridging, or reversal agents. Even more, there are several elements to take into account in order to assess thromboembolic risk: the number, the type, and the location of the valvular prosthetic in addition to the presence of further cardiac risk factor (e.g., AF, congestive heart failure, previous stroke, hypertension, diabetes, age > 75 years) [22].
-
Recent venous thromboembolism: the risk of recurrent thrombosis is highest in the first 3 months after VTE events and declines over time, consequently, all elective invasive procedures have to be postponed at least for 3 months [23, 24]. The risk of VTE reoccurrence is also related to whether the VTE was due to a detectable factor (i.e., surgery, hospital admission), and whether this factor is transient (major surgery, immobility, pregnancy, estrogen therapy), or permanent risk factors (inherited thrombophilia, chronic heart failure, inflammatory bowel disease, malignancy). Thromboembolic risk is categorized into low, moderate, and high-risk categories [25]. Bridging anticoagulants has to be considered in case of interruption.
-
Recent arterial thromboembolism: due to AF, paradoxical embolism, thrombotic endocarditis, dilated contractile left ventricle, left ventricle aneurysm [26]. The risk of thrombosis is highest in the first month after the acute event and declines over time, consequently, all elective invasive procedures have to be delayed when possible.
The continuation of anticoagulants increases the risk of bleeding related with invasive procedures. In 2010, the International Society on Thrombosis and Haemostasis for surgical studies [27] has defined major bleeding as:
-
A fatal bleeding;
-
A symptomatic bleeding in a critical organ (i.e., intracranial, intraspinal, intraocular, retroperitoneal, pericardial, non-operated joint, intramuscular with compartment syndrome);
-
Bleeding in an extra surgical site causing a decrease in hemoglobin of ≥2 g/dL or requiring transfusion of ≥2 units of blood within 24–48 h to the bleeding;
-
Surgical site bleeding requiring a second intervention or a hemarthrosis responsible for delaying mobilization, wound healing;
-
Unexpected and prolonged surgical site bleeding responsible for hemodynamic instability, associated with a decrease in hemoglobin of ≥2 g/dL or requiring transfusion of ≥2 units of blood within 24 h to the bleeding.
This definition was followed by the definition of perioperative bleeding in adult cardiac surgery in 2014 [28].
The estimation of the bleeding risk is based on the type of surgery, urgency, and the type of anesthetic technique. Some types of procedures are associated with higher bleeding tendencies, like cardiovascular, urological, neuraxial, and intracranial surgery. Invasive procedures are categorized into low, moderate and high bleeding risks (Table 5.2) [29]. In particular, neuraxial anesthesia/surgery, as well as intracranial and cardiac surgery are specifically concerning regarding bleeding risk because of the serious complication linked to the bleeding.
Patients characteristics and medical history (e.g., age, renal function) also influence the bleeding risk; any comorbidities that may influence the coagulation cascade are all important elements to take into account [30]. HAS-BLED score is a scoring system developed for the evaluation of bleeding tendency in anticoagulated patients [31, 32]. HAS-BLED score assigns one point for each seven parameters included; hypertension, abnormal renal or liver function, stroke, bleeding tendency, labile INR, elderly age, antiplatelet drugs, or alcohol. The total score ranges between 0 and 9. HAS-BLED is recommended by the European Society of Cardiology (ESC) guidelines for the bleeding risk assessment in AF patients [18]. An HAS-BLED score of ≥3 indicates a high risk of bleeding [33].
By combining risk scores for patient comorbidity and type of surgery, we can stratify overall perioperative risk. In the case of high bleeding risk, the anticoagulant must be discontinued. If the patient presents also a high risk of thromboembolism, the anticoagulant has to be stopped for the shortest feasible time, bridging has to be considered and the anticoagulant has to be resumed as soon as possible. Furthermore, elective invasive procedures have to be postponed at least 3 months after valve surgery and recent episodes of arterial or venous thromboembolism, due to the highest risk of thrombosis during this period. However, if surgery cannot be postponed, a temporary vena cava filter has to be considered in patients with recent episodes of acute venous thromboembolism. On the other hand, in case of low bleeding risk procedure, anticoagulant agents can often be continued (e.g., dental procedure, skin biopsy, implantation of cardiac electronic device, catheter ablation for AF) [34,35,36]. When the decision to not interrupt VKAs agents has been taken, INR has not to be within the therapeutic range.
In elective surgery, preoperative evaluation process can include optimization of risk factors for bleeding (e.g., blood pressure control, anticoagulant management, treatment of anemia) in order to reach the best possible health status before surgery. In an emergency setting, the reversal may be required for urgent surgery/procedure or to treat perioperative bleeding (as discussed below). In this case, physicians have to choose specific agents with prothrombotic effects (i.e., vitamin K, PCC, FFP, Idarucizumab).
3 Timing of Anticoagulant Interruption and Resuming
Besides the intrinsic bleeding risk of the procedure, the main factor influencing the timing of stopping anticoagulant agents is represented by the elimination half-life of the drugs. Determining the time of anticoagulation interruption depends on the pharmacokinetic properties of the specific agent; particular attention has to be given to the renal function. Even more, laboratory tests (i.e., standard coagulation assays, quantitative assay of plasma drug concentration) can guide clinicians in decision-making [37]. An overview of pharmacokinetic properties, laboratory tests, and reversal strategy for anticoagulant agents is shown in Table 5.3.
-
VKAs: Warfarin competitively inhibits the enzyme vitamin K epoxide reductase, a protein essential for activating vitamin K [10]. Vitamin K is required for the synthesis of active clotting factors, such as coagulation factors II, VII, IX, and X, as well as protein C and protein S. Consequently, the depletion of Vitamin K due to warfarin action leads to a reduction of coagulation factors. INR is routinely used for VKAs in order to assess the coagulation status and the residual pharmacodynamic effects of VKAs. In order to obtain a good hemostatic status and reduce bleeding risk at the time of the surgery, Warfarin has to be discontinued 5 days before elective surgery [38]. Restart warfarin 12–24 h after surgery, generally the evening of the day after surgery, if an adequate hemostatic status has been obtained intraoperatively. Normalization of the INR may differ among patients, especially in the elderly, consequently, it is important to check Prothrombin time (PT) and INR prior to surgery and invasive procedure (e.g., neuraxial anesthesia) in order to confirm normalization of INR. Bridging has to be reserved in patients at very high risk of thromboembolism and in case of prolonged period of anticoagulant interruption.
-
DOACs: Thrombin has a fundamental role in hemostasis. Once activated, thrombin can activate factors XI, which in turn can lead to further generation of factor IXa, Xa, VIIIa, and Va; this mechanism serves as an amplification pathway for thrombin generation. Thrombin is central in sustaining the coagulation cascade by feedback activation of coagulation factor. Even more, Thrombin (IIa) converts soluble fibrinogen to insoluble fibrin and it also activates factor XIII; a protein with clot stabilization function. Finally, Thrombin activates platelet. Thrombin can be inhibited by the binding of different drugs to one or two of its three domains (i.e., the active site and exosites 1 and 2). Direct thrombin inhibitors (Dabigatran, Lepirudin, Argatroban, Desirudin, Bivaluridin) bind directly the thrombin to the active site or to the active site and Exosite I [39]. Exosite I is the site of the interaction between Thrombin and fibrinogen, factor V, protein C thrombomodulin, and thrombin receptors on platelets. On the other hand, direct factor Xa inhibitors (Rivaroxaban, Apixaban, and Edoxaban) bind the active site of factor Xa with a direct inhibitor mechanism [40]; inhibition of Xa prevents the amplification of thrombin generation. In fact, factors Xa acts at the convergence between the intrinsic and extrinsic coagulation cascade and it cleaves prothrombin to thrombin.
Elimination half-life of DOACs can be prolonged in renal and liver dysfunction, in the elderly and due to drug interactions. Consequently, renal and liver function has to be checked before surgery. DOACs generally do not require routine laboratory test monitoring; however, in an emergency setting, it is important to determine plasma drug concentration and their effect on coagulation. Laboratory tests can provide information on the residual anticoagulant effect of the anticoagulant agents. A normal PT/INR cannot be used for this purpose. Direct measurement of anti-factor Xa levels, calibrated to the specific anticoagulant, used to monitor anticoagulant effect can be misleading due to interindividual variability [41]. Especially in emergency clinical scenarios, viscoelastic tests have to be considered in order to obtain a global view of coagulation status and bleeding risk.
Dabigatran: an orally administered direct thrombin inhibitor with a half-life of 12–17 h. Absorption is not influenced by food intake. Eighty percent of the drug is eliminated unchanged by renal excretion, consequently, patient with renal impairment requires drug dose adjustment (patient with Creatinine clearance between 15–30 mL/min). Even more, interaction with G-glycoprotein inhibitors (e.g., rifampin, ketoconazole, verapamil) has to keep in mind due to the possible consequent increase of the anticoagulant effect of Dabigatran [42]. Dabigatran has to be discontinued 2–3 days before elective surgery, a longer interruption (2–4 days) is required in patients with severe renal impairment. Restart Dabigatran after surgery if an adequate hemostatic status has been obtained intraoperatively. However, due to the rapid onset of this drug (peak effects 2–3 h after administration), particular attention has to be given in resuming Dabigatran after procedures with a high risk of bleeding. Generally, bridging is not required due to intrinsic pharmacokinetic properties of Dabigatran; however, bridging has to be considered in patients at very high risk for postoperative thromboembolism and in case of prolonged anticoagulant interruption.
Rivaroxaban: an orally administered direct factor Xa inhibitor, with a half-life of 7–11 h. Patients with renal or hepatic impairment require drug dose adjustment. Rivaroxaban should not be used in severe renal impairment (creatinine clearance <15 mL/min) and in patients with severe hepatic dysfunction (Child-Pugh class B and C). Rivaroxaban shows interaction with dual G-glycoprotein and CYP-3A4 inhibitors effects (e.g., voriconazole, ketoconazole) [43]. Rivaroxaban has to be discontinued 2–3 days before elective surgery/invasive procedure; a longer or shorter interruption may be required in patients with severe renal impairment or for low bleeding risk procedures, respectively. Restart Rivaroxaban after surgery if an adequate hemostatic status has been achieved. Due to the rapid onset of action, postpone for 2–3 days the resuming of Rivaroxaban after procedures with high risk of bleeding. Bridging has to be reserved in patients with very high risk for postoperative thromboembolism and in case of prolonged anticoagulant interruption.
Apixaban: an oral direct factor Xa inhibitor with a half-life of 8–12 h. Patients assuming dual inhibitors of G-glycoprotein and CYP-3A4 and with severe renal impairment (Creatinine Clearance 15–30 mL/min) require drug dose adjustment [44]. Interrupt Apixaban 2–3 days before invasive procedures in patients with normal renal function; longer/shorter interval in case of high or low bleeding risk, respectively. Resume Apixaban when good hemostasis has been obtained. Similarly to Dabigatran and Rivaroxaban, Apixaban presents a rapid onset of action, consequently, postpone the recommencing of Rivaroxaban after procedures with high risk of bleeding. Bridging is generally not required; it has to be considered in patients at high risk of thromboembolism and in case of extended anticoagulant interruption. Endoxaban: an oral direct factor Xa inhibitor with a half-life of 10–14 h. Dose reduction is required in patients with renal impairment (Creatinine Clearance 15–50 mL/min). Discontinue Endoxaban 2–3 days before a procedure in patients with normal renal function; longer/shorter interval in case of high or low bleeding risk, respectively. Restart Endoxaban when hemostasis has been reached. Likewise, the aforementioned DOACs, postpone the resuming of Endoxaban after procedures with high risk of bleeding and bridging has to be considered in patients at high risk of thromboembolism and in case of extended anticoagulant interruption.
4 Bridging
Bridging consists of replacing long-acting with short-acting anticoagulants (LMWH/UFH) in order to minimize the risk of thromboembolism in high-risk patients or patients requiring a prolonged anticoagulant interruption. The goal of heparin bridging is to reduce the period the patient is not anticoagulated; thus, decreasing the risk for perioperative thromboembolism. Due to peculiar pharmacokinetics of DOACs (rapid onset and short half-life), bridging is generally reserved in patients assuming VKAs. Not to be underestimated, when prescribing heparin bridging therapy, it is important to monitor for heparin-induced thrombocytopenia [45].
Unfractionated heparin and low-molecular-weight heparin inhibit thrombin indirectly by binding antithrombin(AT). The binding of AT induces a conformational change in AT. The complex heparin–antithrombin can bind the exosite 2 on thrombin. UFH presents a much more efficient inactivator mechanism of Thrombin due to its intrinsic molecular conformation. LMWH lacks the longer chains of UFH and, consequently, has less binding efficacy to thrombin thus decreasing its ability to neutralize thrombin [46]. Even more, UFH, LMWH, and Fondaparinoux can inactivate factor Xa.
LMWHs have progressively substituted UFH; however, in patients with renal insufficiency, UFH has to be chosen because UFH dosing is not affected by renal clearance. Therapeutic dose of LMWH (1 mg/Kg subcutaneous) used for bridging should be stopped 12–24 h before surgery, whereas 4–6 h in case of therapeutic UFH administration (80 units/Kg bolus, 18 units/Kg/h intravenous continuous infusion). If an adequate hemostatic status has been obtained intraoperatively, restart bridging 24 h after surgery. In case of risk of bleeding, bridging should be delayed 48–72 h [38].
Patients at particular risk of thromboembolism and in which bridging is particularly appropriate are [47, 48]:
-
Mechanical mitral valve;
-
Non-bileaflet aortic valve;
-
≥2 Mechanical valves;
-
Aortic valve replacement and previous stroke;
-
Cardioembolic events;
-
VTE within the past 3 months;
-
VTE while in therapeutic anticoagulation;
-
AF with a very high risk of stroke.
5 Reversal and Management of Severe Bleeding
In case of emergency surgery or invasive procedures, there is not enough time to stop anticoagulant agents and, consequently, the risk of bleeding complications is increased. In this scenario, specific reversal factors are available; however, the decision to reverse is based on the balance between stopping and treat the bleeding versus the risk of clotting [48]. Unfortunately, there is a lack of strong evidence, consequently, the decision of reversal strategies is often based on expert panel or routine clinical experience.
The main indications of reversal are represented by [49];
-
Emergency invasive procedure;
-
Overdose (due to excessive intake, reduced drug elimination, or drug interactions);
-
Bleeding.
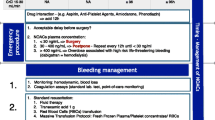
Obviously, in an emergency setting, the first approach to a patient on anticoagulant agents is based on the appropriate resuscitation support. Airway management, intravenous access placement, evaluation and treatment of the hemodynamic status, the management of hemorrhagic shock, the correction of body temperature, and pH/electrolyte disorders represent the initial management of unstable patients. It is vital to identify and treat quickly the site of bleeding (e.g., endoscopy, surgery, interventional radiology) [50]. Even more, bleeding assessment (site, rate of hemorrhage, amount of blood loss, bleeding into closed space-intracranial/retroperitoneal/compartment syndrome) is fundamental to decide whether to reverse anticoagulant effects or not. Packed red blood cell transfusion has to be considered depending on the rate of blood loss. Parallelly, a methodological management of patients on anticoagulant agents requires an accurate evaluation of medical and pharmacological history including: the type of anticoagulant, timing of last ingestion, the dose, other medications (possible interactions), and the evaluation of renal/liver function [51, 52]. This global evaluation aids clinicians to establish when choosing reversal. Routine anticoagulation (e.g., PT/INR) can be used to evaluate residual anticoagulation effects and orientate the reversal strategy in patients on VKAs or UFH [53]. However, these tests cannot be used to determine the degree of anticoagulation in patients on other anticoagulants. Measurement of plasma anti-factor Xa activity, calibrated to the specific anticoagulant, is generally used to monitor the anticoagulant effect; however, it can be deceiving due to interindividual variability [54]. For Dabigatran, ecarin clotting time (ECT) and diluted thrombin time (TT) can be used as surrogate to plasma drug concentration. However, those tests are not widely and promptly available [54, 55]. In an emergency setting, point of care viscoelastic test can provide useful aids of the anticoagulation status of patients; however, data are lacking on the correlation between drug concentration and anticoagulant effects [56].
Then, agent-specific strategies include:
-
UFH/LMWH: due to its short half-life, UFH reversal is rapidly achievable by stopping continuous infusion. However, UFH can be reversed using Protamine (1 mg Protamine/100 units UFH) [49]. No specific antidotes are available for LMWH; Protamine presents a partial effect on LMWH. In clinical trials, Ciraparantag has shown efficient reversal effects for LMWHs [57].
-
VKAs: several agents are available for VKAs reversal; vitamin K, PCC, and FFP. The strategy of reversal warfarin effects consists of omits warfarin and monitor INR. Then in case of supratherapeutic INR and minor bleeding, consider oral administration of Vitamin K (2.5–5 mg/day) and monitor INR after 24 h as long as bleeding control strategies. Repeat Vitamin K if needed. In major bleeding or emergency surgery, immediate reversal is required, then, administer PCC (25–50 units/kg) plus intravenous Vitamin K (5–10 mg) [48]. Vitamin K provides substrates to coagulation factors synthesize (e.g., factors II, VII, IX, X, protein C, and S). VKAs rapid reversal should be accomplished using PCC rather than FFP [48]. Four factors PCC contain factors II, VII, IX, and X. PCC is rapidly available, it provides rapid INR reversal, it allows the reduction of volume requirements thus preventing fluid overload, and the decrease of adverse immune-related risks in comparison to FFP [58]. Limitations of the use of PCC are represented by cost and availability.
-
DOACs: Given the short half-lives, interruption of these drugs can represent the only therapeutic strategy in case of minor bleeding. However, in major bleeding or emergent invasive procedure, an aggressive treatment is needed in order to achieve a good coagulation status. In patients with normal renal and hepatic function, drug elimination can require up to 24–48 h, whereas, this interval can be prolonged in patients with severe renal and/or hepatic dysfunction. Determine the residual anticoagulation effect of DOACs can be challenging and specific laboratory tests are not widely available. For Dabigatran and Rivaroxavaban a plasma concentration of 30 ng/mL or below is considered compatible with surgery [59]. Above this threshold, surgery must be postponed, and plasma drug concentration must be monitored. Otherwise, in emergency surgery and actively bleeding patients, a reversal has to be considered. A plasma level above 400 ng/mL represents a major hemorrhagic risk. Several reversal strategies can be chosen for DOACs. If the last drug dose was taken in the previous 2 h, gastric lavage with oral-activated charcoal can be used to reduce the plasma concentration of DOACs. Furthermore, hemodialysis can be considered for the elimination of supratherapeutic levels of Dabigatran; however, it is not always feasible, especially in hemodynamically unstable patients. A specific antidote is available only for Dabigatran; Idarucizumab, an FDA-approved human antibody fragment. Idarucizumab provides an immediate reversal of the anticoagulant effect of Dabigatran [60]. Due to its cost, the use of Idarucizumab has to be reserved in case of significant plasma drug levels and undergoing emergency procedures. For Rivaroxaban/Apixaban/Edoxaban, Andexanet alfa is currently under investigation as reversal agent. Furthermore, the administration of PCC (25–50 U/Kg) has to be reserved for active bleeding and life treating conditions due to the possible thromboembolic risk and when specific antidotes are not available. However, the evidence on the real risk of thromboembolism using PCC in emergency situations is scarce [61]. Due to its cost, short half-life, and a higher risk of INR rebound, recombinant factor VIIa is not recommended for emergency reversal [59]. Finally, the use of antifibrinolytic agents (i.e., tranexamic acid) and pro-hemostatic therapy (e.g., Desmopressin) to enhance hemostasis have to be considered in major bleeding [62]. The evidence regarding the role of these agents in DOACs-related bleeding is poor. However, their low risk of thrombosis and wide accessibility make these agents reasonable in the case of life-threatening bleeding or emergency settings.
6 Conclusions
The complex management of anticoagulants in patients undergoing surgery or invasive procedures required a deep knowledge of pharmacokinetics and pharmacodynamics of the different agents. It is vital to carry out a detailed anamnesis of the patients in order to identify possible interactions or comorbidities responsible for prolonged anticoagulant effects of these drugs. Furthermore, it is important to take into account the interindividual variability in plasma drug levels. A precise estimation of the bleeding versus thromboembolic risk has to be made in order to reach a clinical decision on whether to interrupt these drugs preoperatively or not. Laboratory tests can aid in clinical decision-making; however, these tests present specific limitations to bear in mind, especially for DOACs. In an emergency setting, a precise reversal strategy has to be chosen in order to prevent or treat bleeding complications.
References
Feeney JM, Santone E, DiFiori M, Kis L, Jayaraman V, Montgomery SC. Compared to warfarin, direct oral anticoagulants are associated with lower mortality in patients with blunt traumatic intracranial hemorrhage: a TQIP study. J Trauma Acute Care Surg. 2016;81(5):843–8.
Prexl O, Bruckbauer M, Voelckel W, Grottke O, Ponschab M, Maegele M, et al. The impact of direct oral anticoagulants in traumatic brain injury patients greater than 60-years-old. Scand J Trauma Resusc Emerg Med. 2018;26(1):20.
Palareti G. Recurrent venous thromboembolism: what is the risk and how to prevent it. Scientifica (Cairo). 2012;391734:2012.
Prandoni P, Noventa F, Ghirarduzzi A, Pengo V, Bernardi E, Pesavento R, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92(2):199–205.
Tran H, Joseph J, Young L, McRae S, Curnow J, Nandurkar H, et al. New oral anticoagulants: a practical guide on prescription, laboratory testing and peri-procedural/bleeding management. Australasian Society of Thrombosis and Haemostasis. Intern Med J. 2014;44(6):525–36.
Bridging Anticoagulation. Is it needed when warfarin is interrupted around the time of a surgery or procedure? Circulation. 2012;125:e496–8.
Nazha B, Spyropoulos AC. The BRIDGE trial: what the hospitalist should know. J Hosp Med. 2016;11(9):652–7.
Ayoub K, Nairooz R, Almomani A, Marji M, Paydak H, Maskoun W. Perioperative heparin bridging in atrial fibrillation patients requiring temporary interruption of anticoagulation: evidence from Meta-analysis. J Stroke Cerebrovasc Dis. 2016;25:2215–21.
Jaffer AK, Ahmed M, Brotman DJ, Bragg L, Seshadri N, Qadeer MA, et al. Low-molecular-weight-heparins as periprocedural anticoagulation for patients on long-term warfarin therapy: a standardized bridging therapy protocol. J Thromb Thrombolysis. 2005;20(1):11–6.
Tadros R, Shakib S. Warfarin—indications, risks and drug interactions. Aust Fam Physician. 2010;39(7):476–9.
Lee LH. DOACs—advances and limitations in real world. Thromb J. 2016;14(Suppl 1):17.
Almarshad F, Alaklabi A, Bakhsh E, Pathan A, Almegren M. Use of direct oral anticoagulants in daily practice. Am J Blood Res. 2018;8(4):57–72.
Ribic C, Crowther M. Thrombosis and anticoagulation in the setting of renal or liver disease. Hematol Am Soc Hematol Educ Program. 2016;2016(1):188–95.
Kanuri SH, Kreutz RP. Pharmacogenomics of novel direct oral anticoagulants: newly identified genes and genetic variants. J Pers Med. 2019;9(1):7.
Barillari G, Pasca S, Barillari A, De Angelis V. Emergency reversal of anticoagulation: from theory to real use of prothrombin complex concentrates. A retrospective Italian experience. Blood Transfus. 2012;10(1):87–94.
Baker RI, Coughlin PB, Gallus AS, Harper PL, Salem HH, Wood EM. Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis and Haemostasis. Med J Aust. 2004;181:492–7.
Idarucizumab. Aust Prescr. 2016;39(5):183.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719–47.
Lip GY. Can we predict stroke in atrial fibrillation? Clin Cardiol. 2012;35(Suppl 1):21–7.
Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;d124:342.
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Baron-Esquivias G, Baumgartner H, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012;33:2451–96.
Whitlock RP, Sun JC, Fremes SE, Rubens FD, Teoh KH. Antithrombotic and thrombolytic therapy for valvular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e576S–600S.
Douketis JD, Foster GA, Crowther MA, Prins MH, Ginsberg JS. Clinical risk factors and timing of recurrent venous thromboembolism during the initial 3 months of anticoagulant therapy. Arch Intern Med. 2000;160:3431–6.
Jimenez D, Diaz G, Marin E, Vidal R, Sueiro A, Yusen RD. The risk of recurrent venous thromboembolism in patients with unprovoked symptomatic deep vein thrombosis and asymptomatic pulmonary embolism. Thromb Haemost. 2006;95:562–6.
Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315–52.
Lyaker MR, Tulman DB, Dimitrova GT, Pin RH, Papadimos TJ. Arterial embolism. Int J Crit Illn Inj Sci. 2013;3(1):77–87.
Schulman S, Angeras U, Bergqvist D, Eriksson B, Lassen MR, Fisher W. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. 2010;8:202–4.
Dyke C, Aronson S, Dietrich W, Hofmann A, Karkouti K, Levi M, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg. 2014;147:1458–63.e1.
Spyropoulos AC, Al-Badri A, Sherwood MW, Douketis JD. Periprocedural management of patients receiving a vitamin K antagonist or a direct oral anticoagulant requiring an elective procedure or surgery. J Thromb Haemost. 2016;14(5):875–85.
Tafur AJ, McBane R 2nd, Wysokinski WE, Litin S, Daniels P, Slusser J, et al. Predictors of major bleeding in peri-procedural anticoagulation management. J Thromb Haemost. 2012;10(2):261–7.
Zhu W, He W, Guo L, Wang X, Hong K. The HAS-BLED score for predicting major bleeding risk in anticoagulated patients with atrial fibrillation: a systematic review and meta-analysis. Clin Cardiol. 2015;38(9):555–61.
Roldan V, Marin F, Manzano-Fernandez S, Gallego P, Vilchez JA, Valdes M, et al. The HAS-BLED score has better prediction accuracy for major bleeding than CHADS2 or CHA2DS2-VASc scores in anticoagulated patients with atrial fibrillation. J Am Coll Cardiol. 2013;62:2199–204.
Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126:860–5.
Perry DJ, Noakes TJ, Helliwell PS. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. Br Dent J. 2007;203(7):389–93.
Sticherling C, Marin F, Birnie D, Boriani G, Calkins H, Dan GA, et al. Antithrombotic management in patients undergoing electrophysiological procedures: a European Heart Rhythm Association (EHRA) position document endorsed by the ESC Working Group Thrombosis, Heart Rhythm Society (HRS), and Asia Pacific Heart Rhythm Society (APHRS). Europace. 2015;17(8):1197–214.
Shahi V, Brinjikji W, Murad MH, Asirvatham SJ, Kallmes DF. Safety of uninterrupted warfarin therapy in patients undergoing cardiovascular endovascular procedures: a systematic review and meta-analysis. Radiology. 2016;278(2):383–94.
Ten Cate H, Henskens YM, Lancé MD. Practical guidance on the use of laboratory testing in the management of bleeding in patients receiving direct oral anticoagulants. Vasc Health Risk Manag. 2017;13:457–67.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S–50S.
Lee CJ, Ansell JE. Direct thrombin inhibitors. Br J Clin Pharmacol. 2011;72(4):581–92.
Mueck W, Schwers S, Stampfuss J. Rivaroxaban and other novel oral anticoagulants: pharmacokinetics in healthy subjects, specific patient populations and relevance of coagulation monitoring. Thromb J. 2013;11(1):10.
Takatsuki S, Kimura T, Sugimoto K, Misaki S, Nakajima K, Kashimura S, et al. Real-world monitoring of direct oral anticoagulants in clinic and hospitalization settings. SAGE Open Med. 2017;5:2050312117734773.
Stollberger C, Finsterer J. Relevance of P-glycoprotein in stroke prevention with dabigatran, rivaroxaban, and apixaban. Herz. 2015;40(Suppl 2):140–5.
Mueck W, Kubitza D, Becka M. Co-administration of rivaroxaban with drugs that share its elimination pathways: pharmacokinetic effects in healthy subjects. Br J Clin Pharmacol. 2013;76(3):455–66.
Frost CE, Byon W, Song Y, Wang J, Schuster AE, Boyd RA, et al. Effect of ketoconazole and diltiazem on the pharmacokinetics of apixaban, an oral direct factor Xa inhibitor. Br J Clin Pharmacol. 2015;79(5):838–46.
Ahmed I, Majeed A, Powell R. Heparin induced thrombocytopenia: diagnosis and management update. Postgrad Med J. 2007;83(983):575–82.
Danielsson A, Raub E, Lindahl U, Bjork I. Role of ternary complexes, in which heparin binds both antithrombin and proteinase, in the acceleration of the reactions between antithrombin and thrombin or factor Xa. J Biol Chem. 1986;261(33):15467–73.
Baron TH, Kamath PS, McBane RD. Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med. 2013;368(22):2113–24.
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D, et al. American College of Surgeons’ Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg. 2018;227:521–36e1.
Thomas S, Makris M. The reversal of anticoagulation in clinical practice. Clin Med (Lond). 2018;18:314–9.
Weinberger J, Cipolle M. Optimal reversal of novel anticoagulants in trauma. Crit Care Clin. 2017;33(1):135–52.
Faraoni D, Levy JH, Albaladejo P, Samama CM. Updates in the perioperative and emergency management of non-vitamin K antagonist oral anticoagulants. Crit Care. 2015;19:203.
Dincq AS, Lessire S, Douxfils J, Dogné JM, Gourdin M, Mullier F. Management of non-vitamin K antagonist oral anticoagulants in the perioperative setting. Biomed Res Int. 2014;2014:385014.
Kuruvilla M, Gurk-Turner C. A review of warfarin dosing and monitoring. Proc (Baylor Univ Med Cent). 2001;14(3):305–6.
Nutescu EA, Dager WE, Kalus JS, Lewin JJ 3rd, Cipolle MD. Management of bleeding and reversal strategies for oral anticoagulants: clinical practice considerations. Am J Health Syst Pharm. 2013;70:1914–29.
Cuker A, Siegal DM, Crowther MA, Garcia DA. Laboratory measurement of the anticoagulant activity of the non-vitamin K oral anticoagulants. J Am Coll Cardiol. 2014;64(11):1128–39.
Eller T, Busse J, Dittrich M, Flieder T, Alban S, Knabbe C, et al. Dabigatran, rivaroxaban, apixaban, argatroban and fondaparinux and their effects on coagulation POC and platelet function tests. Clin Chem Lab Med. 2014;52:835–44.
Ansell JE, Bakhru SH, Laulicht BE, Steiner SS, Grosso MA, Brown K, et al. Single-dose ciraparantag safely and completely reverses anticoagulant effects of edoxaban. Thromb Haemost. 2017;117(2):238–45.
Koutrouvelis A, Abouleish A, Indrikovs A, Alperin J. Case scenario: emergency reversal of oral anticoagulation. Anesthesiology. 2010;113(5):1192–7.
Pernod G, Albaladejo P, Godier A, Samama CM, Susen S, Gruel Y, et al. Management of major bleeding complications and emergency surgery in patients on long-term treatment with direct oral anticoagulants, thrombin or factor-Xa inhibitors: proposals of the working group on perioperative haemostasis (GIHP)–March 2013. Arch Cardiovasc Dis. 2013;106(6–7):382–93.
Pollack CV Jr, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA, et al. Idarucizumab for dabigatran reversal–full cohort analysis. N Engl J Med. 2017;377(5):431–41.
Schulman S, Ritchie B, Nahirniak S, Gross PL, Carrier M, Majeed A, et al. Reversal of dabigatran-associated major bleeding with activated prothrombin concentrate: a prospective cohort study. Thromb Res. 2017;152:44–8.
Keeling D, Tait RC, Watson H. Peri-operative management of anticoagulation and antiplatelet therapy. Br J Haematol. 2016;175(4):602–13.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Brogi, E., Coccolini, F., Forfori, F. (2021). Reversing the Effect of Anticoagulants Safety in Patients Undergoing Emergency Surgery. In: Latifi, R., Catena, F., Coccolini, F. (eds) Emergency General Surgery in Geriatrics . Hot Topics in Acute Care Surgery and Trauma. Springer, Cham. https://doi.org/10.1007/978-3-030-62215-2_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-62215-2_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-62214-5
Online ISBN: 978-3-030-62215-2
eBook Packages: MedicineMedicine (R0)