Abstract
An efficient operating theatre schedule contributes significantly to enhancing the efficiency of hospital operation management and plays a critical financial role in most hospital settings. In this paper, an operating room scheduling problem based on patient priority is investigated at tactical and operational levels subject to specific strategic decisions. At the tactical level, the main goal is to generate a cyclic time table, known as the master surgical schedule (MSS) and can be repeated over the planning horizon of several months to years. Operational level concerns about allocating patients to operating rooms and determining the day of surgeries, which is called the surgical case assignment problem (SCAP). To handle the problems at both decision levels simultaneously, known as the MSS-SCAP problem, an integer linear programming (ILP) model, called MSS-SCAP model, and a heuristic approach are proposed. The objective function is to maximize the total priority scores of the patients assigned to the surgical scheduling blocks over a given planning horizon. An adaptive ILP model is also proposed to solve the SCAP, taking into consideration the dynamics of the waiting list. The computational experiments are conducted using a set of random data to evaluate the performance of the proposed MSS-SCAP model and heuristic algorithm, in terms of solution quality and computation time. Our numerical results indicate that the proposed ILP is capable of yielded optimal solutions for the small-scale instances and near-optimal solutions for medium-size instances within 3,600 seconds. The proposed heuristic algorithm can generate quality solutions within 2 seconds for large-scale instances.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
In recent years, the efficiency of the Australian health care system has become an important area of interest, largely due to the growing costs in health care. Taking into account ageing population, increasing burden of chronic conditions, and growing patients’ expectations of health services, it is anticipated that the Australian Government expenditure on health care alone will increase from 4.2% of gross domestic product (GDP) in 2014–2015 to 5.7% in 2054–2055, or 260 billion in current dollars [3]. Although the Australian health care system generally has satisfactory outcomes by international standards, recent studies have revealed that the efficiency of the health sector could be improved by 20% through making the best use of the available resources [4].
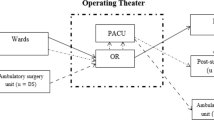
In a health care system, different stockholders have different interests and priorities. Although health care administrations’ goal is to decrease costs, patients expect to receive high-quality services as well as low charges and short waiting times. As a result, to address the efficiency gap and simultaneously satisfy all stockholder expectations, one solution is to employ systematic and evidence-based approaches, which facilitate significant improvements in quality, efficiency, safety and other aspects of operations [5]. Despite the fact that the focus of improving health care systems has largely been on policy, managing hospital operations plays an important role in enhancing the efficiency. Hospital managers are directly involved in actual care rather than the context [6]. Among all hospital departments, the operating theatre (OT) department, which usually consists of several operating rooms (ORs), is the most crucial and costliest due to its operational complexity and expensive resources. It is estimated that 60–70% of all hospital admissions are surgical and the OT department accounts for more than 40% of the total expenses of a hospital [7]. Therefore, any improvement in OT efficiency contributes to having an efficient health care delivery system as a whole. Since the current surgical scheduling and planning approaches do not live up to the hospital management expectations, the OT planning and scheduling problems have attracted the attention of many researchers recently [8]. In general, the OT planning and scheduling problem is a highly complex problem that entails the assignment of OT resources, such as rooms, equipment, nurses and surgeons to patients with the aim of improving efficiency and reducing patients’ waiting time in a way that balances all stockholder’s expectations. The problem is getting even more complex due to different patient characteristics, restricted capacities of upstream and downstream departments and inherent uncertainty of the surgical procedures. In the literature, surgeons are classified into the surgeon groups or surgical specialties if they are homogeneous and have the same medical and procedural requirements [11]. On the other hand, although elective surgeries can be planned in advance, non-elective surgeries are unexpected.
1.1 Literature Review
The characteristics of the different hospitals under study and the different national realities contribute to the diversity of the literature in OT planning and scheduling problems. From the structural point of view, the OT planning and scheduling decisions are made in three hierarchical levels including strategic, tactical and operational. These decision levels depend on each other, as the outcome of each level can affect the decisions on other levels in addition to being the input for the next level [7]. in the following, the main characteristics of these hierarchical levels are introduced.
At the strategic level, the main focus is to find out how many time blocks/slots should be assigned to each surgical specialty to find the ideal composition and volume of patients in a hospital [7, 9]. A time block is defined as the smallest time unit for which an operating room can be assigned to a specialty [20]. To this end, strategic planning is primarily a resource allocation problem and known as the case-mix planning problem (CMPP). For a detailed survey of literature on the CMPP, we refer the interested reader to Hof et al. [19].
At the tactical level, the capacity of ORs per day is shared among a variety of surgical specialties in order to provide a cyclic timetable, which is called the master surgical schedule (MSS) [14]. The main goal of an MSS is to assign surgical specialties, and not individual patients/surgeons, to time blocks [12]. To develop an MSS, historical data and actual/forecast patients’ demand, in the form of waiting lists, are utilized as critical inputs. In the literature, to construct an MSS three main strategies have been used, including block scheduling, open scheduling and modified block scheduling. In the block scheduling strategy, time blocks are assigned to surgical specialties, which can arrange their surgical cases only in their own blocks. In the open scheduling strategy, surgeons from different specialties can perform surgeries in the same time block. Moreover, modified block scheduling strategy is a mix of block and open scheduling strategies, which reserves some of the time blocks and assigns others to patients or specialties using an open scheduling strategy [11]. Although the open scheduling strategy is more flexible and provides a better assignment of the surgical cases in comparison with block scheduling, it is an uncommon strategy and rarely used in the health care industry. Hence, despite potential inefficiencies as a result of unbalanced block schedules, block scheduling is widely accepted to generate the MSS, due to its simplicity for both surgeons and managers [18].
In the literature, developing the MSS has been investigated as a combinatorial optimization problem. The main objective of this optimization problem is to provide an OT plan that optimizes the OT and surgical resource allocation and minimize the patients’ waiting time. A variety of constraints affect the development of MSS such as availability restrictions of medical staff and equipment, capacity limitation of resources, e.g. regular opening hours, number of upstream and downstream resources, and the uncertainty of surgical procedures as well as a restriction on the number of time blocks assigned to each specialty as the result of CMPP [2, 7, 12].
At the operational level, the assignment of an operating room and operating time to each patient, as well as sequencing surgeries in each operating room are determined over a short-term planning horizon [9]. To develop an operational plan a wide range of constraints should be taken into account. For example, structural constraints, which ensure a non-overlapping of surgeries in the same room or surgeons in different rooms at the same time, and resource constraints such as daily capacity restriction in each operating room are among the most important ones [1]. In the literature, generally, the OT planning and scheduling problems at the operational level have been solved as two main subproblems including the advance scheduling and the allocation scheduling. The advance scheduling, which is also called the surgical case assignment problem (SCAP) seeks to assign each patient to an operating room and a particular day for surgery over a planning horizon of 1–2 weeks. The allocation scheduling, also referred to as the surgical case sequencing problem (SCSP), concentrates on the timing aspects and sequencing of the assigned surgeries within each OR [15]. To address the subproblems at the operational level, a variety of solution approaches have been developed in the literature utilizing mathematical programming techniques, simulation and scenario-based analysis and analytical procedures. They mainly have been solved as a combinatorial optimization problem with the aim of achieving a trade-off among different stockholders’ interests [15, 17, 21].
1.2 Contribution of this Research
Much literature has investigated just one decision level of OT planning and scheduling problems. In other words, they solved the problem using multi-stage approaches, with each stage dealing with just one decision level [11]. The main reason is that solving the overall problem of all decision levels as multi-stage problems decreases the complexity of the problem. However, the three hierarchical decision levels depend on each other and the outcome of each level can be utilized as input to the other levels. Therefore, solving the problems on different decision levels concurrently provides more effective procedures and solutions. In some studies, all decision levels were investigated at the same time [10]. Other studies coped with the problems at tactical and operational levels simultaneously [2, 11, 16]. Despite the fact that recent studies have focused on the integrated MSS and SCAP scheduling problems at both tactical and operational levels, the proposed exact methods could not live up to medium- or large-size instances. This study investigates the integrated MSS-SCAP based on patient priority, which is the indicator of a patient’s surgery urgency. The main novelty of the integrated MSS-SCAP problem in this paper is the consideration of three fundamental factors altogether including consideration of patients’ priorities, strategic decisions and solving both MSS and SCAP problems concurrently. An ILP model, called MSS-SCAP model, is proposed to produce robust surgical scheduling. The MSS-SCAP model can optimally assign time blocks to specialties and determine the OR and surgery date for each patient over the planning horizon of medium term. To cope with the large-size instances, a heuristic approach is developed to provide high-quality solutions for the MSS-SCAP. Then to adapt operation-related dynamics and any unpredicted changes in the waiting list, given an MSS, an adaptive ILP is proposed to solve the SCAP as the multiple knapsack problem (MKP) over the planning horizon of one to several weeks.
The remainder of this paper is organized as follows. Section 11.2 introduces the problem statement, the assumptions as well as the mathematical models. In Sect. 11.3, the details of heuristic approach are provided. Computational experiments, which indicate the performance of the MSS-SCAP model and the heuristic approach, are reported in Sect. 11.4. Finally, the conclusion of the study and further research directions are presented in Sect. 11.5.
2 Problem Statement and Mathematical Models
In this section, the problem definition and assumptions are given. The mathematical models are then provided to solve the MSS-SCAP and SCAP. It should be noted that for the sake of integrity and simplicity, the symbols and definitions similar to [2] are used.
2.1 Problem Definition
The goal of the integrated MSS-SCAP is to provide a cyclic time table that allocates the time blocks of each OR and each day to the specialties, in addition to the determination of the OR and the surgery date per patient over the planning horizon. In this study, the block scheduling strategy is utilized to allocate specialties to time blocks. Although the duration of time blocks can vary, it is determined in advance. Pre-emption is not allowed, which means that, once a surgery starts, it cannot be interrupted. It is assumed that all surgeries of each specialty can be performed by any surgeon of that specialty and all ORs can be used by all specialties. The number of nurses, upstream and downstream resources such as number of ICU and ward beds are enough and do not force any bottleneck or restriction on the planning process. It is also assumed that the minimum and maximum OR times to be assigned to each specialty, as the output of CMPP at the strategic level, are given. Moreover, the surgeries can be scheduled during the working days from Monday to Friday (we only consider elective surgeries), which means that each week of the planning horizon includes 5 days. Table 11.1 summarizes the notations used in the paper.
2.2 The MSS-SCAP Model
In this section, the MSS-SCAP model is proposed to allocate the time blocks to specialties and assign patients to ORs as well as days over the planning horizon. Despite the fact that hospital managers assign time blocks to the specialties based on the equity and fairness criteria [10], the priority of a patient contributes to the urgency and importance of performing his/her surgery. In other words, in assignment of patients to ORs and dates, the patient with higher priority have precedence to be operated, which means that the larger priority score, the higher priority of surgery. Thus, to generate a distribution of time blocks among the specialties, patient priority should be taken into account. Nevertheless, only a few researches have taken patient prioritization into consideration [18]. To this end, the objective function of this study is to maximize the summation of assigned patient priority scores to ORs. The MSS-SCAP model is formalized as below:
The objective function is to maximize the summation of priority scores of assigned patients to ORs over the planning horizon. Using constraint (11.1), it is not possible to share a block between different specialties as per the block scheduling strategy. Based on constraint (11.2), patient p can be operated in block b of an operating room t during day d only if that time block is assigned to its specialty. Constraint (11.3) determines that a patient can be operated at most once during the planning horizon. Constraints (11.4) and (11.5) enforce the restrictions on the maximum and minimum numbers of hours that can be assigned to each specialty as the result of strategic decisions. Using Constraint (11.6), the total processing time of all assigned patients to a time block must not be greater than the duration of that time block. Constraint (11.7) is related to the definition of binary decision variables.
2.3 The Adaptive SCAP Model
An MSS usually is constructed to cover a planning horizon of one to several months. Then, considering this MSS, hospital administrations determine the staff rostering and equip ORs with required instruments. Making these decisions and providing the equipment entail spending lots of time and negotiating with different surgical specialties as well as going to great expense. Hence, hospital administrations do not tend to change the MSS over the planning horizon of medium term. On the other hand, in the real world, even excluding the uncertainty factors, the waiting list is dynamic due to the arrival of other elective patients with high priorities. One of the good approaches to handling this dynamic process is to generate a new SCAP solution, for each planning horizon of one to several weeks. Therefore, the MSS solution, which is provided by MSS-SCAP model, is kept constant but the SCAP solution will be updated. In other words, given the MSS, the SCAP solution takes into account new elective patients and will be updated whenever it is necessary.
In summary, at the first stage, the MSS-SCAP is solved and the assignment of time blocks to surgical specialties is considered as the MSS solution. Then, given this MSS solution, it is assumed that the SCAP solution can be updated to adapt the real-world dynamic conditions. Therefore, the overall SCAP is decomposed into several subproblems similar to the MKP, one for each surgical specialty, in which the patients correspond to the items and the blocks to the knapsacks.
The adaptive SCAP model per specialty s is illustrated as follows. Note that the parameter \(Q_{tsdb}\) is determined by the MSS solution, which can be the result of the MSS-SCAP model.
The objective function is to maximize the total priority scores of assigned patients to ORs and dates over the planning horizon of one to several weeks. Constraint (11.8) indicates that a patient can be operated at most once during the planning horizon. Constraint (11.9) restricts the processing time of all assigned patients, which belong to specialty s, to a time block that must not be greater than that time block duration. Based on constraint (11.10), all decision variables are binary.
Both of the proposed mathematical models focused on maximizing the total priority scores of assigned patients. However, in the real world, patients with higher priorities should be scheduled as soon as possible.
3 The Proposed Heuristic Algorithm
In order to generate high-quality solutions for MSS-SCAP in a reasonable amount of time and for large-scale instances, this study proposes a heuristic algorithm, which consists of the following steps:
Step 1: Sort all patients in a non-increasing order of their priority scores.
Step 2: Select patient p among unscheduled patients with the highest priority score. If there are some patients with the same priority scores, select the one with longer processing time. If their processing times are equal, select one of them randomly. Schedule the selected patient considering the following rules:
Using the first-fit strategy, assign the patient to the first available time block b, which belongs to the specialty of patient p. If the patient p is the first patient who is assigning to time block b, then by assigning this patient to time block b, its specialty is also assigned to that time block.
In each time block, only the patients with the same specialty s can be assigned.
By assigning patient p to a time block b, the total processing time of all patients assigned to that block must not exceed the capacity of that block.
The total amount of assigned hours to specialty s must not exceed the maximum number of OR hours that can be assigned to that specialty.
The time blocks containing assigned patients are considered prior to the unoccupied ones. This criterion seeks to reduce idle time and minimize the number of open ORs.
Step 3: Repeat Step 2 until all patients are scheduled or there is no available time in blocks over the planning horizon.
The numbers of operations in Steps 1 and 2 are \(O(P_{\max } \log P_{\max })\) and \(O(B_{\max } D_{\max } P_{\max })\), respectively. Thus, the run time of the proposed heuristic is \(O(P_{\max } \log P_{\max } + B_{\max } D_{\max } P_{\max })\).
4 Computational Results
To evaluate the performance of the proposed mathematical models and the heuristic algorithm, a numerical study is designed. The models were implemented via Gurobi 8.0.0 and the heuristic algorithm was coded by using Python Anaconda 3.6. The numerical study is carried out on a PC equipped with Intel Core i5 3.2 GHz CPU and 8 GB of RAM under Linux Ubuntu operating system. To generate the instances, some of the data are adopted from a data set provided by Spratt and Kozan [2]. The number of patients in the data set is 2802. Thus, in the present study the number of patients is selected from the set \(\{20,50,100,150,200,300,400,500,1000,1500,2000,2802\}\). In the data set of [2], the ratio of patients to specialties, i.e. \(I_{ps}\), is given. As a result, the number of specialties is selected from the set \(\{3,5,8,10,12\}\). The number of operating rooms is selected from \(\{2,4,5,10,15,20\}\). The number of days to plan the surgeries is selected from \(\{5,10,15,20\}\), meaning that the planning horizon ranges between 1 and 4 weeks. Each day of planning horizon consists of two time blocks and each block is 5 hours. Furthermore, surgery durations per each specialty are generated randomly from the lognormal distribution (the mean and variance are given in the data set [2]). Since the duration of each time block is 5hours, the lognormal distribution is truncated at 5hours to ensure that each surgery fits in a time block. The integer priority scores were also generated from a discrete uniform distribution of [1,100].
To evaluate the capability of the mathematical models and the heuristic algorithm, two types of experiments were performed. The first experiment includes only two operating rooms. Table 11.2 shows the results of this experiment. The average percentage of error (APE) for the heuristic is calculated as \(\frac{F_{Opt}-F_{H}}{F_{Opt}}\), where \(F_{Opt}\) is the objective value of the model as reported by Gurobi, and \(F_{H}\) is the objective value of the heuristic algorithm. The solution gap, which is provided by Gurobi, is presented as Gap. In addition, the average computation time of the heuristic and the model are presented as \(Time_{H}\) and \(Time_{Opt}\) (the maximum runtime for Gurobi is set to 3,600 seconds; in column \(Time_{Opt}\), − means that the time limit has been reached).
For the second experiment, the computational efficiency of the heuristic was investigated by increasing the number of patients and ORs. Table 11.3 shows the average times of the heuristic algorithm for different numbers of patients and ORs. As it is indicated, the average execution time of the heuristic algorithm is less than two seconds even for \(P_{\max }=2802\) and \(T_{\max }=20\). Therefore, the heuristic algorithm is quite efficient to solve the large-scale instances of the MSS-SCAP.
5 Conclusion and Future Work
This paper investigates the OR scheduling problem at tactical and operational levels concurrently, called MSS-SCAP, for maximizing the total priorities of assigned patients. The block scheduling strategy is used to allocate time blocks to specialties. To solve the MSS-SCAP, an ILP model and a heuristic algorithm have been proposed. In addition, an adaptive ILP model is suggested to solve the SCAP and cope with the dynamics of the real-world waiting list, given an MSS. To evaluate the proposed MSS-SCAP model and the heuristic algorithm, a numerical study has been developed. The computational results have shown that the heuristic algorithm has the capability to solve large-scale instances efficiently. Further research works will include the uncertainty of surgery durations and the restriction on the downstream facilities like the number of beds in the ICU Department. In addition, the problem can be extended to include a restriction on the availability of surgical teams on the days of surgery.
References
Addis B, Carello G, Tànfani E (2014) A robust optimization approach for the Advanced Scheduling Problem with uncertain surgery duration in Operating Room Planning- an extended analysis, working paper or preprint
Agnetis A, Coppi A, Corsini M, Dellino G, Meloni C, Pranzo M (2012) Long term evaluation of operating theater planning policies. Oper Res Health Care 1:95–104
Agnetis A, Coppi A, Corsini M, Dellino G, Meloni C, Pranzo M (2014) A decomposition approach for the combined master surgical schedule and surgical case assignment problems. Health Care Manag Sci 17:49–59
Aringhieri R, Landa P, Soriano P, Tnfani E, Testi A (2015) A two level metaheuristic for the operating room scheduling and assignment problem. Comput Oper Res 54:21–34
Australian Government, Productivity Commission (2006) Potential Benefits of the National Reform Agenda. Research Paper, Canberra, Australia
Australian Government, Productivity Commission (2015) Efficiency in Health. Research Paper, Canberra, Australia
Erdogan SA, Denton BT (2011) Surgery planning and scheduling. American Cancer Society, Wiley Encyclopedia of Operations Research and Management Science
Fei H, Chu C, Meskens N (2008) Solving a tactical operating room planning problem by a column-generation-based heuristic procedure with four criteria. Ann Oper Res 166:91
Guerriero F, Guido R (2011) Operational research in the management of the operating theatre: a survey. Health Care Manag Sci 14:89–114
Guido R, Conforti D (2017) A hybrid genetic approach for solving an integrated multi-objective operating room planning and scheduling problem. Comput Oper Res 87:270–282
Hof S, Fügener A, Schoenfelder J, JO B (2017) Case mix planning in hospitals: a review and future agenda. Health Care Manag Sci 20:207–220
Hussung T (2016) The role of hospital management in transforming healthcare. Husson University, Bangor, Canada
Jebali A, Diabat A (2017) A Chance-constrained operating room planning with elective and emergency cases under downstream capacity constraints. Comput Ind Eng 114:329–344
Kaplan G, Bo-Linn G, Carayon P, Pronovost P, Rouse W, Reid P, Saunders R (2013) Bringing a Systems Approach to Health. National Academy of Medicine, Discussion Paper, Washington, America
Koppka L, Wiesche L, Schacht M, Werners B (2018) Optimal distribution of operating hours over operating rooms using probabilities. Eur J Oper Res 267:1156–1171
Ma G, Beliën G, Demeulemeester E, Wang L (2009) Solving the strategic case mix problem optimally by using branch-and-price algorithms, In: proceeding paper
Marques I, Captivo ME (2015) Bicriteria elective surgery scheduling using an evolutionary algorithm, operations research for health care, ORAHS 2014. In: The 40th international conference of the EURO working group on operational research applied to health services, vol 7, pp 14–26
Marques I, Captivo ME, Vaz Pato M (2015) A bicriteria heuristic for an elective surgery scheduling problem. Health Care Manag Sci 18:251–266
Sieber T, Leibundgut D (2002) Operating room management and strategies in Switzerland: results of a survey. Eur J Anaesthesiology 19:415–423
Spratt B, Kozan E (2016) Waiting list management through master surgical schedules: a case study. Oper Res Health Care 10:49–64
Testi A, Tanfani E, Torre G (2007) A three-phase approach for operating theatre schedules. Health Care Manag Sci 10:163–172
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this paper
Cite this paper
Mashkani, O., Hwang, F.J., Salehipour, A. (2021). The Operating Room Scheduling Problem Based on Patient Priority. In: Ernst, A.T., Dunstall, S., García-Flores, R., Grobler, M., Marlow, D. (eds) Data and Decision Sciences in Action 2. Lecture Notes in Management and Industrial Engineering. Springer, Cham. https://doi.org/10.1007/978-3-030-60135-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-60135-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-60134-8
Online ISBN: 978-3-030-60135-5
eBook Packages: EngineeringEngineering (R0)