Abstract
The quest toward a specific biomarker for migraine stands among the biggest challenges of the last 50 years. Electrophysiological techniques are particularly suitable to study the nervous system in human beings. They are noninvasive, riskless and quite easy to perform and have a temporal resolution that cannot be achieved with other methods.
Among them, the visual-evoked modality is being widely studied for several decades. Higher amplitude of fundamental harmonic from steady-state visual stimulation is commonly found in episodic migraine. Many studies performed interictally in groups of episodic patients have shown a habituation deficit of visual evoked potentials, even if this finding has been a matter of controversy. An abnormal thalamic control of information reaching the cortex, which in turn causes an altered degree of lateral inhibition of the visual cortex, could be the key of this functional abnormality, which normalizes during or close to a migraine attack.
Along the same line, a habituation deficit has been demonstrated using a somatosensory modality (SSEPs), the magnitude of the habituation deficit being significantly correlated to the evolution of migraine. Additional works highlighted a less-efficient subcortical inhibition of sensory cortices.
As far as the auditory modality is concerned, a stronger stimulus intensity dependence of late, long-latency, auditory evoked cortical potentials (IDAP) was found between attacks in migraineurs compared with controls.
It seems also worthwhile to notice that an interhemispheric asymmetry of responses has been described using most sensory stimulations.
Using single-pulse transcranial magnetic stimulation (sTMS) over the visual cortex, a higher phosphene prevalence and a lower threshold were found in migraine with aura patients. Otherwise, resting-state motor or phosphene thresholds obtained with sTMS in episodic patients provided discrepant results.
In chronic migraine (CM), neurophysiologic signs of sensitization have been reported while recording SSEPs. Interestingly, a simultaneous analysis of SSEP habituation and thalamocortical loop activation in chronic subjects showed a neurophysiological pattern similar to that of ictal episodic migraine. In medication overuse headache patients, SSEPs suggested a persistent cortical sensitization. The recorded habituation abnormalities appear to vary according to the overused drug. Akin to results of SSEP studies, VEP amplitudes habituate normally during stimulus repetition in CM and may change with the transition from CM to episodic migraine, switching from normal to deficient habituation.
In conclusion, studies of evoked potentials in migraine show that the migraine brain processes sensory information differently from healthy subjects. The most frequently detected peculiarity during the migraine pain-free phase is an excessive cortical responsivity to almost any type of sensory stimulation. The cortical hyperresponsivity is not constant in migraine patients and may not be reproducible. The reasons for these between-studies discrepancies are multifaceted, and they reflect the complex pathophysiology of the disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Migraine
- evoked potentials
- Visual system
- Somatosensory system
- TMS
- Cognitive potentials
- Visual snow
- Blink reflex
- Pain-related evoked potentials
3.1 Introduction
Headache is a widespread symptom that frequently leads patients to consult a neurologist. Most recurrent headaches will occur in the context of a primary headache disorder, which can be classified based on the criteria of the new ICHD 3 classification (2018). Few chronic headaches are directly related to an identifiable underlying organic condition (secondary headaches). Even if the diagnosis of a primary headache is predominantly a matter of clinically based reasoning, the quest for a specific biomarker of various primary headaches (predominantly migraine) has been among the biggest challenges of the last 50 years.
Numerous paraclinical tests have been developed over the past decades and used to gather a better insight into primary migraines’ pathophysiology, but their usefulness and place in clinical practice are sometimes ill defined. Functional neuroimaging techniques, such as positron emission tomography and functional magnetic resonance imaging, offer a high spatial resolution, while electrophysiological techniques have an excellent temporal resolution and probably a better accessibility in daily neurological practice. Laboratory testing provided promising results but is usually restricted to tertiary headache centres.
Electrophysiology is particularly suitable to study the nervous system in human beings. It is noninvasive, riskless and relatively easy to perform. Briefly, the different components of the nervous system generate an electrical signal that reflects the summation of several action potentials and can be recorded using surface scalp electrodes. Transient evoked potentials are electrical potentials elicited in the nervous system after repeated stimulations (visual, auditory, somatosensory, etc.). Transcranial magnetic stimulation (TMS) allows evaluating temporal changes in cortical excitability.
Here, we will review the relevant data of electrophysiology using non-cognitive and non-painful evoked potentials performed in migraine and their interest for the phenotyping and diagnosis of long-lasting headache disorders.
3.2 Visual Evoked Potentials
Migraine is associated with prominent visual symptoms; it thus seemed logical to initially study the visual modality of evoked potentials. The latter is still the most studied evoked modality.
For more than six decades, the recording of visual evoked potentials (VEPs) has been used in neurophthalmological diagnostics as a complement to ophthalmological and neurological semiotics.
The recording of VEPs is a method that has the great advantage of exploring, in a noninvasive way, the functioning of the visual system. The VEP, in fact, represents the summation of electrical potentials recorded over the scalp, which mirrors the neurophysiological counterpart of the activity of the visual pathway up to Brodmann area 17.
Different types of visual stimulation paradigms have been used to study migraine pathophysiology.
The bioelectric activity of the innermost retinal layers (cells and ganglion fibres), explored through pattern electroretinogram recording, showed no abnormalities in migraine with and without aura [1, 2].
By using a repetition of the visual stimulus above 4 Hz, it is possible to obtain a stationary neurophysiological response over time, so-called steady-state (SS) response, that can be analysed using a Fourier transform, that is without the intervention of the examiner. A higher amplitude of the fundamental harmonic from SS stimulation is commonly found in episodic migraine with or without aura [3,4,5,6,7]. This abnormality returns to the normal range after a prophylactic treatment with femoxetine or propranolol [8]. In a multichannel study the connectivity between the SS-VEP response recorded from the cuneus and that recorded from the temporal poles and the anterior cingulate cortex increased with increased headache-free days elapsed since the last migraine attack [9]. Some researchers found that relative reduction in SS-VEP response with increasing contrast—an indirect measure of contrast gain—is more common in migraineurs, consistent with increase in feedback excitation driving increased inhibition and leading to increased perceptual surround suppression [10].
Studies that analysed the amplitude of flash or pattern evoked potentials were inconclusive as they found either an increase [11,12,13,14,15,16,17,18,19,20,21], a decrease [17, 22, 23], or a response similar to that in healthy subjects [11, 24,25,26,27,28,29,30,31]. However, since the gross portion of the neural activity is lost after the standard process of averaging an amount of traces, Lisicki et al. investigated VEPs using single-trial analysis, detecting greater VEP amplitudes in episodic migraine-without-aura patients than in healthy volunteers. Moreover, they observed that higher single-trial VEP amplitudes in migraine involve higher grey matter volume and peculiar pattern of functional connectivity in brain areas devoted to visual processing [32].
Another common finding in migraine is an increased asymmetry between the electrophysiological responses of the two hemispheres [1, 23, 33,34,35,36,37,38,39].
In recent years, most of the scientific literature on neurophysiology of migraine has focused on the study of habituation mechanisms. Habituation is a behavioural response decrement that results from repeated stimulations and does not involve sensory adaptation or fatigue, that is, a decrease in peripheral receptor activity. It is considered as a fundamental adaptive behaviour of the nervous system that allows selection of salient information among all ambient stimuli and is involved in learning and memory. In fact, by acquiring a high number of trials and averaging them off-line into successive blocks, it is possible to study the course of the amplitude of the potential over time. In healthy subjects, the amplitude of evoked potentials shows a reducing response during stimulus repetition, that is habituates normally [40].
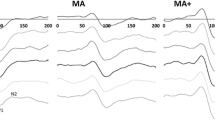
The majority of studies performed interictally in groups of episodic patients have shown a lack of reducing response, that is a habituation deficit, between the first and the following blocks of pattern-reversal VEPs [13, 26, 28, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] (Fig. 3.1).
Demonstrative recordings of pattern-reversal visual evoked potentials (VEPs) in a healthy volunteer (HV), a migraine–without-aura patient between attacks (MO) and a chronic migraine patient (CM). VEPs are six consecutive blocks of 100 averaged responses during uninterrupted stimulation. Compared to the healthy subject, the MO patient is characterized by a tendency to be lower N1-P1 amplitude of the first block of averaged responses and lack of habituation over successive blocks of responses, while the CM patient is characterized by an higher amplitude of the first block of averaged responses and normal habituation over successive blocks of responses
Habituation deficit was also found for visual evoked magnetoencephalographic (MEG) responses [62,63,64,65] and motion-onset VEPs evoked by the abrupt onset of visual motion, which are generated in extrastriate areas [53].
The habituation deficit of the visual system seems to have a genetic basis as it is also present in the unaffected relatives of migraine patients, defined at-risk [44, 66]. In addition, this abnormal processing of visual information changes in relation to where you are during the migraine cycle, being maximum as the distance from the last attack increases [20, 58] and minimum, normalizing, during an attack [49, 58, 62] and after pharmacological [45, 50] and non-pharmacological [42, 43, 51, 52, 67, 68] treatment. It might depend on sunlight irradiance [47] and the patient’s self-perceived stress [46]. Sunlight and genetics, among others, could perhaps account for some discrepancies between VEP studies, since not all of them retrieved a habituation deficit in the interictal phase [31, 41]. An anomalous thalamic control of the flow of information reaching the cortex [54], which in turn causes an altered degree of lateral inhibition of the visual cortex [58], studied by means of a windmill/dartboard pattern, seems to be at the basis of this functional anomaly. The mechanisms of cortical inhibition have also proved to be altered when the VEP technique of double visual stimulation was used in both migraine without [69] and with aura [70]. It is possible to intervene on the habituation curve in general and on its deficit in migraine during the interictal phase through various experimental methods, such as tonic pain [71], 3 min of forced hyperventilation [55], or 2 h of light deprivation [57]. The huge number of factors influencing the phenomenon of habituation may explain why some studies did not confirm this abnormal processing of visual information between migraine attacks [19, 31, 72,73,74,75,76,77,78]. We do not know whether these contradictory results are due to the enormous number of factors that can influence the final response after repeated visual stimulation or due to the lack of a diagnosis and blind analysis of the recordings, as others think [75]. Anyhow, lack of VEP amplitude habituation was detected even in patients affected by the recently described neurological condition called ‘visual snow’ syndrome [79,80,81], which may share pathophysiological mechanisms with migraine [82].
3.3 Somatosensory Evoked Potentials (SSEPs)
The recording of SSEPs is an objective and quantifiable measurement of the functioning of the lemniscal somatosensory system. The amplitude and latency of standard grand-averaged cortical median nerve SSEP response were normal in episodic migraine between attacks in most of the studies [59, 83,84,85,86,87,88,89,90], although increases in amplitude were reported in the only study that used magnetoencephalography [91]. The amplitude of the N20 SSEP component was delayed and reduced during a sensory aura in one patient, and both anomalies progressively returned within the range of normality during the subsequent headache phase [92].
As for the VEP amplitude, a lack of habituation to repetitive peripheral electrical stimulation has been observed to the SSEP amplitude (Fig. 3.2). This altered processing of sensory information was observed during the pain-free phase [59, 86, 93,94,95,96,97], normalizing immediately after a forced increase in cortical excitability [94, 97] and after a dietary ketogenic regimen [42], but not after anodal transcranial direct current stimulation of the temporal pole [43]. An abnormal thalamic control, through thalamic radiation, of the degree of cortical activation could explain the habituation deficit [94, 95]. Nonetheless, the magnitude habituation deficit is significantly correlated to the clinical evolution of migraine, since spontaneous worsening of the disease is associated with further reduced habituation, whereas spontaneous improvement is linked with enhanced habituation [96].
Demonstrative recordings of median nerve somatosensory evoked potentials (SSEPs) in a healthy volunteer (HV), a migraine-without-aura patient between attacks (MO) and a chronic migraine patient (CM). SSEPs are three consecutive blocks of 100 averaged responses during uninterrupted stimulation. Compared to the healthy subject, the migraineur is characterized by a lower N20-P25 amplitude of the first block of averaged responses and lack of habituation over successive blocks of responses, while the CM patient is characterized by an higher amplitude of the first block of averaged responses and normal habituation over successive blocks of responses
In partial agreement with the VEP results, during a migraine episode, initial response increased has been observed to the SSEP amplitude, while delayed responses showed normal habituation [93, 95]. This response pattern has been interpreted as a possible neurophysiological expression of a transient central sensitization process during an attack. As with VEPs, a reduced degree of lateral inhibition within the somatosensory cortex could help explain this habituation deficit, closely related to the degree of thalamocortical activation. In pain-free patients, the percentage of lateral inhibition correlated negatively with the days elapsed since the last migraine attack, the average duration of the attacks and the severity of the headache, measured on a VAS scale [98]. It is of interest that in migraine, a reduced inhibition of SSEP amplitude during both a sensory gating [99] or recovery cycle paradigm [88] after paired electrical stimuli was observed, which may be yet other findings in favour of a less-efficient subcortical inhibition of sensory cortices [100]. In fact, in adult migraineurs, shortened recovery cycle correlated with reduced thalamocortical activation as well as with clinical worsening [101]. Migraine prevention with topiramate normalized the abnormal recovery cycle [102].
Again, as with VEPs, a significant asymmetry between the two hemispheres was noted even when recording the N30 SSEP amplitudes [85]. In an old study comparing patients with mixed headache (migraine and tension-type headache) and pain-free controls, parietal cortical potential was found to increase in amplitude and more rapidly as the stimulus intensity increased, independent from having or not having headache during the testing session [103].
3.4 Auditory Evoked Potentials
After an acoustic stimulus, up to 30 waves can be recorded at cortical level: from the far-field ones generated at cochlear and acoustic nerve levels to those generated in the auditory cortex and associative acoustic centres. These responses are generally categorized into early, middle and late potentials. In most studies researchers were not able to find interictal abnormalities in the baseline parameters of early short-latency brainstem auditory evoked potentials (BAEP) [31, 33, 104,105,106,107], with the exception of a prolonged peak latency of wave V during [107] and between [108] attacks.
Some authors found significant I–III [109], III–V [25, 109], or I–V [25, 108, 109] BAEPs interpeak latency differences when comparing patients with controls and, in some case, even comparing patients recorded between attacks with those during attacks [107, 109]. In another study, all BAEP latencies increased and the V/I peak amplitude ratio decreased during the attacks [110].
Also with this neurophysiological method an interhemispheric asymmetry of the responses, specifically that of the interpeak latency I–V, has been detected [104, 106]. BAEP abnormalities did not change after flunarizine [104].
Deficient habituation mechanism of waves IV–V dispersion was found in migraine interictally in response to 40 dB clicks (but not to 55 and 70 dB clicks) in a blinded study, in which a direct relationship between BAEP amplitudes and blood 5-HT levels was also reported in controls but not in migraineurs [111].
Two studies [112, 113] but one [31] found stronger stimulus intensity dependence of late, long-latency, auditory evoked cortical potentials (IDAP) between attacks in migraineurs compared with healthy controls. Coherently with other neurophysiological data, IDAP normalizes during an attack [49]. Lack of habituation has also been reported for cortical auditory evoked responses for 70 dB [112], but not in another one [31]. An inverse correlation between amplitude habituation and IDAP has been reported [113] (Fig. 3.3). In a recent study, researchers assessed auditory middle-latency evoked potentials in a group of patients with vestibular migraine. They described a lack of habituation of Na-Pa amplitude to repetitive stimulation when compared with patients affected by Meniere’s disease and healthy subjects [114].
Demonstrative recordings of intensity-dependent auditory evoked potentials (IDAP) in a healthy volunteer (HV) and a migraine-without-aura patient between attacks (MO). IDAPs are three consecutive blocks of 50 averaged responses during uninterrupted stimulation (80 dB). Compared to the healthy subject, the migraineur is characterized by lack of N1-P2 amplitude habituation over successive blocks of responses
In an auditory P50 event-related potential paradigm, auditory sensory gating was markedly decreased in migraine patients compared with controls [115, 116], probably in a way that is related to reduced short-term habituation.
3.5 Single-Pulse Transcranial Magnetic Stimulation (sTMS)
Noninvasive magnetic stimulation of the brain is a well-established neurophysiological method to assess the excitability of the underlying cortical area. After the introduction of TMS in 1985 [117], several authors have used sTMS in migraine studies.
In migraine, both decreased [118, 119] and increased [120] phosphene threshold (PT) were reported when sTMS was applied over the visual cortex. Several studies also found no differences compared to controls [77, 121]. A systematic review of the studies using sTMS to assess visual phosphenes provided evidence for higher phosphene prevalence and lower threshold in migraine with aura patients compared with controls, but not in migraine-without-aura patients. They concluded that these results should be interpreted with caution [122]. In migraine, PT did not correlate with VEP amplitude and habituation [60] or with average pain intensity, disability assessment scales, gender, age, migraine subtype, migraine duration and use of hormone contraceptives [123]. Unfortunately, the assessment of PT has a clear shortcoming as it relies only on the subjective patient’s experience (describing positive visual phenomena or not). This concern is not retrieved in motor cortex TMS, where the threshold is assessed through an objective and recordable measure, the amplitude of motor evoked potential (MEP) recorded from a peripheral muscle. Like PTs, thresholds for MEPs were found to variate widely, being normal [51, 118, 124,125,126,127], increased [128,129,130], or reduced [131,132,133] in migraineurs. MEP thresholds were significantly increased in migraine after light deprivation, an experimental way to modulate subcortical and cortical activities, whereas they remained stable in controls [134]. However, some authors showed that these inconsistent findings resulted from variation in the cortical excitability related to the time interval between the ictal and interictal states of migraine [135].
Using paired-pulse TMS, intracortical facilitation was found in one study [136], but not in another [130]. The cortical silent period was normal [118, 136] or reduced [137, 138] in migraine patients between attacks. In migraine with aura patients, the conditioning of the cerebellum with TMS showed a significant deficit of cerebellar inhibition on the motor cortex compared with controls [139].
3.6 Evoked Potentials in Chronic Migraine (CM)
The mechanisms by which an episodic form of migraine becomes chronic are still unknown. Neurophysiology has also tried to help solve this issue.
One of the mechanisms supposed to be the basis of this process is central sensitization. According to its definition, that is increased responsiveness not only to noxious but also to innocuous peripheral stimuli, neurophysiological signs of sensitization have been reported recording SSEPs. Amplitudes of the parietal components were larger in patients experiencing CM or medication overuse headache (MOH) than in episodic migraine patients between attacks [93, 95, 140].
By the investigation of simultaneous SSEP habituation and thalamocortical loop activation in CM, researchers have observed a neurophysiological pattern similar to that of ictal episodic migraine. In fact, both episodic and chronic patients were characterized by higher initial amplitudes, reflecting cortical sensitization, and by response habituation over sequential block averages, resulting in a ‘transient’ cortical sensitization. In MOH, the initially higher SSEP amplitudes lacked habituation in subsequent block averages, that is further increase, resulting in a ‘persistent’ cortical sensitization [93]. Lack of SSEP amplitude habituation in MOH patients differed according to the overused drug, because amplitudes were smaller in triptan overusers than in patients overusing non-steroidal anti-inflammatory drugs (NSAIDs) or combined medications [93]. Interestingly, patients experiencing cutaneous allodynia exhibited greater SSEP amplitudes compared to those without allodynia, confirming this abnormal cortical response in the neurophysiological counterpart of central sensitization [59]. Moreover, the neurophysiological abnormalities of MOH are proportional to the duration of the chronic phase [93, 140]. These abnormalities in cortical responses to somatosensory stimulation appear to be strongly influenced by genetic factors [141]. That angiotensin-converting enzyme (ACE) polymorphism could affect neural plasticity was assessed by SSEP recording and the clinical features of MOH patients. The D/D ACE homozygote carriers exhibited the highest grand-averaged SSEP amplitudes (i.e. reflecting sensitization) and the most severe deficits in habituation, although other MOH patients overall did not habituate either. This abnormal neurophysiological pattern gradually disappeared in the D/I and I/I carriers, in whom the cortical response habituated normally [141].
In a recent study, we found that, contrary to the episodic migraine, the level of somatosensory cortex lateral inhibition is normal in CM patients without a previous history of medication overuse. Moreover, in contrast with the idea that deficient cortical inhibitory mechanism plays a pivotal role in the basic mechanisms of central sensitization in CM, we did not find a clear correlation between the degree of lateral inhibition and of sensitization [140]. Nonetheless, less-efficient subcortical inhibition of sensory cortices cannot be excluded, since in an MEG study of somatosensory gating, reduced parietal responses to paired-pulse stimuli were more pronounced in CM than in episodic migraineurs and healthy controls [99].
Compared with episodic migraine patients recorded interictally, CM patients showed greater initial mean block amplitude in recordings of magnetic VEPs [63]. Moreover, consistently with the above-mentioned SSEP studies [93, 95], VEP amplitudes habituate normally during stimulus repetition in CM [63, 142] and may change with the transition from CM to episodic migraine after topiramate treatment, switching from normal to deficient habituation [65].
A group of CM patients, most of them with MOH, had a steeper IDAP than healthy controls, which significantly flattened after greater occipital nerve block significantly reduced monthly days with headache [142].
By further exploring inhibitory circuits, Currà et al. [138] measured the transcranial magnetic stimulation (TMS)–induced cortical silent period (CSP) in a group of MOH patients. Despite the overall similarity in SP duration between MOH patients and healthy controls, subgroup analysis revealed that CSP duration was significantly shorter in triptan overusers than in the NSAID or triptan-plus-NSAID overuser groups. In MOH patients overall, CSP duration correlated positively with monthly tablet intake. However, this positive correlation was restricted to NSAID and triptan-plus-NSAID MOH subgroups; triptan overusers exhibited a negative correlation [138].
3.7 Conclusions
Studies of evoked potentials in migraine show that the migraine brain processes sensory information differently from the brain of healthy subjects. In fact, the most frequently detected peculiarity during the migraine pain-free phase is an excessive cortical responsiveness to any type of sensory stimulation (except olfactory stimulation). This over-responsiveness manifests either as an increased amplitude of the grand-average potential or as a deficit of habituation during a series of stereotyped stimulation. Besides this habituation deficit, migraineurs exhibit an increased intensity dependence of auditory evoked potentials, which was found to be correlated to the lack of habituation and perhaps to be its consequence. Habituation is a phenomenon intrinsically linked to learning and memory. Precisely as a function of the latter phenomenon, the brain can undergo a series of plastic modifications, which have been shown to be altered in migraine, when studied, for example, with repetitive TMS [143].
The cortical hyper-responsiveness is not constant in migraine patients and may not be reproducible. The reasons for these between-studies discrepancies are multifaceted, and they reflect the complex pathophysiology of the disease:
-
First, it was shown that the degree of habituation depended on technical parameters, for example the temporal or spatial frequencies of a visual pattern, or the blinding of the researchers performing the analysis, even if a recent publication actually found no difference between blinded and non-blinded habituation assessments of a same population [144]. Nonetheless, previous studies conducted in the same laboratory have shown that whether blinding the analysis [20, 53, 144] or attempting to blind the diagnosis [31, 75], the result remains unchanged.
-
Second, habituation is a dynamic parameter that provides interesting data about the current (‘cross-sectional’) CNS information processing. Sequential recordings have demonstrated that the cortical dysfunction level varied with the migraine cycle, being prominent with the increasing distance from the last attack and absent during an attack. In CM, the neurophysiological pattern is quite similar to that derived from recordings from patients with episodic migraines derived during an attack [95, 98] and was previously defined as a condition of ‘never-ending migraine attack’ [145].
-
Third, genetics appears to be a determinant factor of the interictal dysfunction leading to deficient habituation in migraine. Hence, habituation deficit could thus be an endophenotypic marker of a genetic predisposition to migraine, even if these conclusions cannot be applied to individuals.
-
Fourth, the habituation can be modulated by external interventions, especially drugs known to alleviate migraine attacks, as well as non-pharmacological intervening procedures.
Therefore, the sole habituation deficit cannot be considered as a formal diagnostic criterion of migraine, but could help in the case of atypical presentations. However, a multicentre study performed in 624 patients recently demonstrated that combining the recordings of visual (habituation) and auditory (intensity dependence) evoked potentials could characterize interictal episodic migraineurs with 83.4% sensitivity, 66.7% specificity and 81.1% accuracy [146].
Only now are we beginning to see the possibility that these functional abnormalities are extrinsic in morphofunctional abnormalities of the brain [147]. Further studies are needed to better understand the clinical correlates of this altered information processing in the migraine brain, also with the ultimate aim of intervening in a more targeted way both pharmacologically and non-pharmacologically.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- BAEP:
-
Brainstem auditory evoked potentials
- CM:
-
Chronic migraine
- CSP:
-
Cortical silent period
- ICHD:
-
International classification of headache disorders
- IDAP:
-
Intensity dependence auditory evoked cortical potentials
- MEG:
-
Magnetoencephalographic
- MEP:
-
Motor evoked potential (MEP)
- MOH:
-
Medication overuse headache
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- PT:
-
Phosphene threshold
- rTMS:
-
Repetitive transcranial magnetic stimulation
- SS:
-
Steady-state
- SSEPs:
-
Somatosensory evoked potentials
- sTMS:
-
Single-pulse transcranial magnetic stimulation
- TMS:
-
Transcranial magnetic stimulation
- VAS:
-
Visual analogue scale
- VEP:
-
Visual evoked potential
References
Shibata K, Osawa M, Iwata M. Simultaneous recording of pattern reversal electroretinograms and visual evoked potentials in migraine. Cephalalgia. 1997;17:742–7.
Nguyen B, McKendrick AM, Vingrys AJ. Simultaneous retinal and cortical visually evoked electrophysiological responses in between migraine attacks. Cephalalgia. 2012;32:896–907.
Nyrke T, Lang AH. Spectral analysis of visual potentials evoked by sine wave modulated light in migraine. Electroencephalogr Clin Neurophysiol. 1982;53:436–42.
Nyrke T, Kangasniemi P, Lang AH. Difference of steady-state visual evoked potentials in classic and common migraine. Electroencephalogr Clin Neurophysiol. 1989;73:285–94.
Nyrke T, Kangasniemi P, Lang AH. Transient asymmetries of steady-state visual evoked potentials in classic migraine. Headache. 1990;30:133–7.
Shibata K, Yamane K, Otuka K, et al. Abnormal visual processing in migraine with aura: a study of steady-state visual evoked potentials. J Neurol Sci. 2008;271:119–26.
Shibata K, Yamane K, Nishimura Y, et al. Spatial frequency differentially affects habituation in migraineurs: a steady-state visual-evoked potential study. Doc Ophthalmol Ophthalmol. 2011;123:65–73.
Nyrke T, Kangasniemi P, Lang AH, et al. Steady-state visual evoked potentials during migraine prophylaxis by propranolol and femoxetine. Acta Neurol Scand. 1984;69:9–14.
Mehnert J, Bader D, Nolte G, et al. Visual input drives increased occipital responsiveness and harmonized oscillations in multiple cortical areas in migraineurs. NeuroImage Clin. 2019;23:101815.
Nguyen BN, McKendrick AM, Vingrys AJ. Abnormal inhibition-excitation imbalance in migraine. Cephalalgia. 2016;36:5–14.
Mariani E, Moschini V, Pastorino G, et al. Pattern-reversal visual evoked potentials and EEG correlations in common migraine patients. Headache. 1988;28:269–71.
Lehtonen JB. Visual evoked cortical potentials for single flashes and flickering light in migraine. Headache. 1974;14:1–12.
Kalita J, Uniyal R, Misra UK, et al. Neuronal dysexcitability may be a biomarker of migraine: a visual evoked potential study. Clin EEG Neurosci. 2018;49:342–50.
Kennard C, Gawel M, Rudolph NM, et al. Visual evoked potentials in migraine subjects. Res Clin Stud Headache. 1978;6:73–80.
Connolly JF, Gawel M, Rose FC. Migraine patients exhibit abnormalities in the visual evoked potential. J Neurol Neurosurg Psychiatry. 1982;45:464–7.
Shibata K, Osawa M, Iwata M. Pattern reversal visual evoked potentials in classic and common migraine. J Neurol Sci. 1997;145:177–81.
Khalil NM, Legg NJ, Anderson DJ. Long term decline of P100 amplitude in migraine with aura. J Neurol Neurosurg Psychiatry. 2000;69:507–11.
Shibata K, Yamane K, Iwata M, et al. Evaluating the effects of spatial frequency on migraines by using pattern-reversal visual evoked potentials. Clin Neurophysiol. 2005;116:2220–7.
Sand T, White LR, Hagen K, et al. Visual evoked potential and spatial frequency in migraine: a longitudinal study. Acta Neurol Scand. 2009;189:33–7.
Coppola G, Bracaglia M, Di Lenola D, et al. Visual evoked potentials in subgroups of migraine with aura patients. J Headache Pain. 2015;16:92.
Lisicki M, D’Ostilio K, Coppola G, et al. Evidence of an increased neuronal activation-to-resting glucose uptake ratio in the visual cortex of migraine patients: a study comparing 18FDG-PET and visual evoked potentials. J Headache Pain. 2018;19 https://doi.org/10.1186/s10194-018-0877-8.
Polich J, Ehlers CL, Dalessio DJ. Pattern-shift visual evoked responses and EEG in migraine. Headache. 1986;26:451–6.
Tagliati M, Sabbadini M, Bernardi G, et al. Multichannel visual evoked potentials in migraine. Electroencephalogr Clin Neurophysiol. 1995;96:1–5.
Lai CW, Dean P, Ziegler DK, et al. Clinical and electrophysiological responses to dietary challenge in migraineurs. Headache. 1989;29:180–6.
Drake ME, Pakalnis A, Hietter SA, et al. Visual and auditory evoked potentials in migraine. Electromyogr Clin Neurophysiol. 1990;30:77–81.
Schoenen J, Wang W, Albert A, et al. Potentiation instead of habituation characterizes visual evoked potentials in migraine patients between attacks. Eur J Neurol. 1995;2:115–22.
Sener HO, Haktanir I, Demirci S. Pattern-reversal visual evoked potentials in migraineurs with or without visual aura. Headache. 1997;37:449–51.
Afra J, Cecchini AP, De Pasqua V, et al. Visual evoked potentials during long periods of pattern-reversal stimulation in migraine. Brain. 1998;121(Pt 2):233–41.
Afra J, Proietti Cecchini A, Sándor PS, et al. Comparison of visual and auditory evoked cortical potentials in migraine patients between attacks. Clin Neurophysiol. 2000;111:1124–9.
Wang W, Wang GP, Ding XL, et al. Personality and response to repeated visual stimulation in migraine and tension-type headaches. Cephalalgia. 1999;19:718–24.
Sand T, Vingen JV. Visual, long-latency auditory and brainstem auditory evoked potentials in migraine: relation to pattern size, stimulus intensity, sound and light discomfort thresholds and pre-attack state. Cephalalgia. 2000;20:804–20.
Lisicki M, D’Ostilio K, Coppola G, et al. Brain correlates of single trial visual evoked potentials in migraine: more than meets the eye. Front Neurol. 2018;9 https://doi.org/10.3389/fneur.2018.00393.
Benna P, Bianco C, Costa P, et al. Visual evoked potentials and brainstem auditory evoked potentials in migraine and transient ischemic attacks. Cephalalgia. 1985;5(Suppl 2):53–8.
Tsounis S, Milonas J, Gilliam F. Hemi-field pattern reversal visual evoked potentials in migraine. Cephalalgia. 1993;13:267–71.
Shibata K, Osawa M, Iwata M. Pattern reversal visual evoked potentials in migraine with aura and migraine aura without headache. Cephalalgia. 1998;18:319–23.
Logi F, Bonfiglio L, Orlandi G, et al. Asymmetric scalp distribution of pattern visual evoked potentials during interictal phases in migraine. Acta Neurol Scand. 2001;104:301–7.
Coutin-Churchman P, de Freytez A. Vector analysis of visual evoked potentials in migraineurs with visual aura. Clin Neurophysiol. 2003;114:2132–7.
Coppola G, Parisi V, Fiermonte G, et al. Asymmetric distribution of visual evoked potentials in patients with migraine with aura during the interictal phase. Eur J Ophthalmol. 2007;17:828–35.
Khalil NM, Nicotra A, Wilkins AJ. Asymmetry of visual function in migraine with aura: correlation with lateralisation of headache and aura. Cephalalgia. 2011;31:213–21.
Rankin CH, Abrams T, Barry RJ, et al. Habituation revisited: an updated and revised description of the behavioral characteristics of habituation. Neurobiol Learn Mem. 2009;92:135–8.
Rauschel V, Ruscheweyh R, Krafczyk S, et al. Test-retest reliability of visual-evoked potential habituation. Cephalalgia. 2016;36:831–9.
Di Lorenzo C, Coppola G, Bracaglia M, et al. Cortical functional correlates of responsiveness to short-lasting preventive intervention with ketogenic diet in migraine: a multimodal evoked potentials study. J Headache Pain. 2016;17:58.
Cortese F, Pierelli F, Bove I, et al. Anodal transcranial direct current stimulation over the left temporal pole restores normal visual evoked potential habituation in interictal migraineurs. J Headache Pain. 2017;18:70.
Lisicki M, Ruiz-Romagnoli E, D’Ostilio K, et al. Familial history of migraine influences habituation of visual evoked potentials. Cephalalgia. 2017;37:1082–7.
Ince F, Erdogan-Bakar E, Unal-Cevik I. Preventive drugs restore visual evoked habituation and attention in migraineurs. Acta Neurol Belg. 2017;117:523–30.
Lisicki M, Ruiz-Romagnoli E, Piedrabuena R, et al. Migraine triggers and habituation of visual evoked potentials. Cephalalgia. 2018;38:988–92.
Lisicki M, D’Ostilio K, Erpicum M, et al. Sunlight irradiance and habituation of visual evoked potentials in migraine: the environment makes its mark. Cephalalgia. 2018;38:1351–60.
Susvirkar AA, Velusami D, Srinivasan N. Evaluation of habituation to visual evoked potentials using pattern reversal among migraine individuals – a cross-sectional study. J Basic Clin Physiol Pharmacol. 2020;31 https://doi.org/10.1515/jbcpp-2019-0217.
Judit A, Sandor PS, Schoenen J. Habituation of visual and intensity dependence of auditory evoked cortical potentials tends to normalize just before and during the migraine attack. Cephalalgia. 2000;20:714–9.
Ozkul Y, Bozlar S. Effects of fluoxetine on habituation of pattern reversal visually evoked potentials in migraine prophylaxis. Headache. 2002;42:582–7.
Bohotin V, Fumal A, Vandenheede M, et al. Effects of repetitive transcranial magnetic stimulation on visual evoked potentials in migraine. Brain. 2002;125:912–22.
Fumal A, Coppola G, Bohotin V, et al. Induction of long-lasting changes of visual cortex excitability by five daily sessions of repetitive transcranial magnetic stimulation (rTMS) in healthy volunteers and migraine patients. Cephalalgia. 2006;26:143–9.
Bednář M, Kubová Z, Kremláček J. Lack of visual evoked potentials amplitude decrement during prolonged reversal and motion stimulation in migraineurs. Clin Neurophysiol. 2014;125:1223–30.
Coppola G, Ambrosini A, Di Clemente L, et al. Interictal abnormalities of gamma band activity in visual evoked responses in migraine: an indication of thalamocortical dysrhythmia? Cephalalgia. 2007;27:1360–7.
Coppola G, Currà A, Sava SL, et al. Changes in visual-evoked potential habituation induced by hyperventilation in migraine. J Headache Pain. 2010;11:497–503.
Coppola G, Currà A, Serrao M, et al. Lack of cold pressor test-induced effect on visual-evoked potentials in migraine. J Headache Pain. 2010;11:115–21.
Coppola G, Crémers J, Gérard P, et al. Effects of light deprivation on visual evoked potentials in migraine without aura. BMC Neurol. 2011;11:91.
Coppola G, Parisi V, Di Lorenzo C, et al. Lateral inhibition in visual cortex of migraine patients between attacks. J Headache Pain. 2013;14:20.
Kalita J, Bhoi SK, Misra UK. Is lack of habituation of evoked potential a biological marker of migraine? Clin J Pain. 2014;30:724–9.
Ambrosini A, Iezzi E, Perrotta A, et al. Correlation between habituation of visual-evoked potentials and magnetophosphene thresholds in migraine: a case-control study. Cephalalgia. 2016;36:258–64.
Ambrosini A, Coppola G, Iezzi E, et al. Reliability and repeatability of testing visual evoked potential habituation in migraine: a blinded case-control study. Cephalalgia. 2016; https://doi.org/10.1177/0333102416648656.
Chen W-T, Wang S-J, Fuh J-L, et al. Peri-ictal normalization of visual cortex excitability in migraine: an MEG study. Cephalalgia. 2009;29:1202–11.
Chen WT, Wang SJ, Fuh JL, et al. Persistent ictal-like visual cortical excitability in chronic migraine. Pain. 2011;152:254–8.
Chen WT, Lin YY, Fuh JL, et al. Sustained visual cortex hyperexcitability in migraine with persistent visual aura. Brain. 2011;134:2387–95.
Chen W-T, Wang S-J, Fuh J-L, et al. Visual cortex excitability and plasticity associated with remission from chronic to episodic migraine. Cephalalgia. 2012;32:537–43.
Sándor PS, Afra J, Proietti Cecchini A, et al. Familial influences on cortical evoked potentials in migraine. Neuroreport. 1999;10:1235–8.
Siniatchkin M, Sendacki M, Moeller F, et al. Abnormal changes of synaptic excitability in migraine with aura. Cereb Cortex (New York, NY 1991). 2012;22:2207–16.
Ranieri F, Coppola G, Musumeci G, et al. Evidence for associative plasticity in the human visual cortex. Brain Stimul. 2019;12:705–13.
Höffken O, Stude P, Lenz M, et al. Visual paired-pulse stimulation reveals enhanced visual cortex excitability in migraineurs. Eur J Neurosci. 2009;30:714–20.
Strigaro G, Cerino A, Falletta L, et al. Impaired visual inhibition in migraine with aura. Clin Neurophysiol. 2015;126:1988–93.
Coppola G, Serrao M, Currà A, et al. Tonic pain abolishes cortical habituation of visual evoked potentials in healthy subjects. J Pain. 2010;11:291–6.
Afra J, Ambrosini A, Genicot R, et al. Influence of colors on habituation of visual evoked potentials in patients with migraine with aura and in healthy volunteers. Headache. 2000;40:36–40.
Oelkers R, Grosser K, Lang E, et al. Visual evoked potentials in migraine patients: alterations depend on pattern spatial frequency. Brain. 1999;122:1147–55.
Sand T, Zhitniy N, White LR, et al. Visual evoked potential latency, amplitude and habituation in migraine a longitudinal study. Clin Neurophysiol. 2008;119:1020–7.
Omland PM, Nilsen KB, Uglem M, et al. Visual evoked potentials in Interictal migraine: no confirmation of abnormal habituation. Headache. 2013;53:1071–86.
Omland PM, Uglem M, Hagen K, et al. Visual evoked potentials in migraine: is the ‘neurophysiological hallmark’ concept still valid? Clin Neurophysiol. 2015;127:S1388–2457.
Omland PM, Uglem M, Engstrøm M, et al. Modulation of visual evoked potentials by high-frequency repetitive transcranial magnetic stimulation in migraineurs. Clin Neurophysiol. 2014;125:2090–9.
Viganò A, D’Elia TS, Sava SL, et al. Transcranial direct current stimulation (tDCS) of the visual cortex: a proof-of-concept study based on interictal electrophysiological abnormalities in migraine. J Headache Pain. 2013;14:23.
Unal-Cevik I, Yildiz FG. Visual snow in migraine with aura: further characterization by brain imaging, electrophysiology, and treatment - case report. Headache. 2015;55:1436–41.
Luna S, Lai D, Harris A. Antagonistic relationship between VEP potentiation and gamma power in visual snow syndrome. Headache. 2018;58:138–44.
Yildiz FG, Turkyilmaz U, Unal-Cevik I. The clinical characteristics and neurophysiological assessments of the occipital cortex in visual snow syndrome with or without migraine. Headache J Head Face Pain. 2019;59:484–94.
Puledda F, Ffytche D, O’Daly O, et al. Imaging the visual network in the migraine spectrum. Front Neurol. 2019;10:1325.
Montagna P, Zucconi M, Zappia M, et al. Somatosensory evoked potentials in migraine and tension headache. Headache. 1985;25:115.
Firenze C, Del Gatto F, Mazzotta G, et al. Somatosensory-evoked potential study in headache patients. Cephalalgia. 1988;8:157–62.
De Tommaso M, Sciruicchio V, Tota P, et al. Somatosensory evoked potentials in migraine. Funct Neurol. 1997;12:77–82.
Ozkul Y, Uckardes A. Median nerve somatosensory evoked potentials in migraine. Eur J Neurol. 2002;9:227–32.
Sakuma K, Takeshima T, Ishizaki K, et al. Somatosensory evoked high-frequency oscillations in migraine patients. Clin Neurophysiol. 2004;115:1857–62.
Valeriani M, Rinalduzzi S, Vigevano F. Multilevel somatosensory system disinhibition in children with migraine. Pain. 2005;118:137–44.
Coppola G, Vandenheede M, Di Clemente L, et al. Somatosensory evoked high-frequency oscillations reflecting thalamo-cortical activity are decreased in migraine patients between attacks. Brain. 2005;128:98–103.
Restuccia D, Vollono C, Del Piero I, et al. Somatosensory high frequency oscillations reflect clinical fluctuations in migraine. Clin Neurophysiol. 2012;123:2050–6.
Lang E, Kaltenhäuser M, Neundörfer B, et al. Hyperexcitability of the primary somatosensory cortex in migraine—a magnetoencephalographic study. Brain. 2004;127:2459–69.
Chayasirisobhon S. Somatosensory evoked potentials in acute migraine with sensory aura. Clin Electroencephalogr. 1995;26:65–9.
Coppola G, Currà A, Di Lorenzo C, et al. Abnormal cortical responses to somatosensory stimulation in medication-overuse headache. BMC Neurol. 2010;10 https://doi.org/10.1186/1471-2377-10-126.
Coppola G, De Pasqua V, Pierelli F, et al. Effects of repetitive transcranial magnetic stimulation on somatosensory evoked potentials and high frequency oscillations in migraine. Cephalalgia. 2012;32:700–9.
Coppola G, Iacovelli E, Bracaglia M, et al. Electrophysiological correlates of episodic migraine chronification: evidence for thalamic involvement. J Headache Pain. 2013;14:76.
Restuccia D, Vollono C, Virdis D, et al. Patterns of habituation and clinical fluctuations in migraine. Cephalalgia. 2014;34:201–10.
Kalita J, Bhoi SK, Misra UK. Effect of high rate rTMS on somatosensory evoked potential in migraine. Cephalalgia. 2017;37:1222–30.
Coppola G, Bracaglia M, Di Lenola D, et al. Lateral inhibition in the somatosensory cortex during and between migraine without aura attacks: correlations with thalamocortical activity and clinical features. Cephalalgia. 2016;36:568–78.
Hsiao F-J, Wang S-J, Lin Y-Y, et al. Somatosensory gating is altered and associated with migraine chronification: a magnetoencephalographic study. Cephalalgia. 2018;38:744–53.
Ugawa Y, Genba-Shimizu K, Kanazawa I. Somatosensory evoked potential recovery (SEP-R) in various neurological disorders. Electroencephalogr Clin Neurophysiol. 1996;100:62–7.
Restuccia D, Vollono C, Del Piero I, et al. Different levels of cortical excitability reflect clinical fluctuations in migraine. Cephalalgia. 2013;33:1035–47.
Vollono C, Ferraro D, Miliucci R, et al. The abnormal recovery cycle of somatosensory evoked potential components in children with migraine can be reversed by topiramate. Cephalalgia. 2010;30:17–26.
Marlowe N. Somatosensory evoked potentials and headache: a further examination of the central theory. J Psychosom Res. 1995;39:119–31.
Bussone G, Sinatra MG, Boiardi A, et al. Brainstem auditory evoked potentials in migraine patients in basal conditions and after chronic flunarizine treatment. Cephalalgia. 1985;5(Suppl 2):177–80.
Battistella PA, Suppiej A, Casara G, et al. Brainstem auditory evoked potentials (BAEPs) in childhood migraine. Headache. 1988;28:204–6.
Schlake HP, Grotemeyer KH, Hofferberth B, et al. Brainstem auditory evoked potentials in migraine--evidence of increased side differences during the pain-free interval. Headache. 1990;30:129–32.
Firat Y, Ozturan O, Bicak U, et al. Auditory brainstem response in pediatric migraine: during the attack and asymptomatic period. Int J Pediatr Otorhinolaryngol. 2006;70:1431–8.
Bánk J. Brainstem auditory evoked potentials in migraine after Rausedyl provocation. Cephalalgia. 1991;11:277–9.
Podoshin L, Ben-David J, Pratt H, et al. Auditory brainstem evoked potentials in patients with migraine. Headache. 1987;27:27–9.
Kochar K, Srivastava T, Maurya RK, et al. Visual evoked potential & brainstem auditory evoked potentials in acute attack & after the attack of migraine. Electromyogr Clin Neurophysiol. 2002;42:175–9.
Sand T, Zhitniy N, White LR, et al. Brainstem auditory-evoked potential habituation and intensity-dependence related to serotonin metabolism in migraine: a longitudinal study. Clin Neurophysiol. 2008;119:1190–200.
Wang W, Timsit-Berthier M, Schoenen J. Intensity dependence of auditory evoked potentials is pronounced in migraine: an indication of cortical potentiation and low serotonergic neurotransmission? Neurology. 1996;46:1404–9.
Ambrosini A, Rossi P, De Pasqua V, et al. Lack of habituation causes high intensity dependence of auditory evoked cortical potentials in migraine. Brain. 2003;126:2009–15.
Murofushi T, Goto F, Tsubota M. Vestibular migraine patients show lack of habituation in auditory middle latency responses to repetitive stimuli: comparison with Meniere’s disease patients. Front Neurol. 2020;11:24.
Ambrosini A, De Pasqua V, Afra J, et al. Reduced gating of middle-latency auditory evoked potentials (P50) in migraine patients: another indication of abnormal sensory processing? Neurosci Lett. 2001;306:132–4.
Siniatchkin M, Kropp P, Gerber W-D. What kind of habituation is impaired in migraine patients? Cephalalgia. 2003;23:511–8.
Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;325:1106–7.
Gunaydin S, Soysal A, Atay T, et al. Motor and occipital cortex excitability in migraine patients. Can J Neurol Sci. 2006;33:63–7.
Aurora SK, Ahmad BK, Welch KM, et al. Transcranial magnetic stimulation confirms hyperexcitability of occipital cortex in migraine. Neurology. 1998;50:1111–4.
Bohotin V, Fumal A, Vandenheede M, et al. Excitability of visual V1–V2 and motor cortices to single transcranial magnetic stimuli in migraine: a reappraisal using a figure-of-eight coil. Cephalalgia. 2003;23:264–70.
Chadaide Z, Arlt S, Antal A, et al. Transcranial direct current stimulation reveals inhibitory deficiency in migraine. Cephalalgia. 2007;27:833–9.
Brigo F, Storti M, Nardone R, et al. Transcranial magnetic stimulation of visual cortex in migraine patients: a systematic review with meta-analysis. J Headache Pain. 2012;13:339–49.
Ekkert A, Noreikaitė K, Valiulis V, et al. Migraine-linked characteristics of transcranial magnetic stimulation-induced phosphenes. J Integr Neurosci. 2019;18:463–6.
Werhahn KJ, Wiseman K, Herzog J, et al. Motor cortex excitability in patients with migraine with aura and hemiplegic migraine. Cephalalgia. 2000;20:45–50.
Brighina F, Palermo A, Daniele O, et al. High-frequency transcranial magnetic stimulation on motor cortex of patients affected by migraine with aura: a way to restore normal cortical excitability? Cephalalgia. 2010;30:46–52.
Brighina F, Cosentino G, Vigneri S, et al. Abnormal facilitatory mechanisms in motor cortex of migraine with aura. Eur J Pain. 2011;15:928–35.
Cosentino G, Fierro B, Vigneri S, et al. Cyclical changes of cortical excitability and metaplasticity in migraine: evidence from a repetitive transcranial magnetic stimulation study. Pain. 2014;155:1070–8.
Maertens de AN, Pepin JL, Schoenen J, et al. Percutaneous magnetic stimulation of the motor cortex in migraine. Electroencephalogr Clin Neurophysiol. 1992;85:110–5.
Bettucci D, Cantello R, Gianelli M, et al. Menstrual migraine without aura: cortical excitability to magnetic stimulation. Headache. 1992;32:345–7.
Afra J, Mascia A, Gérard P, et al. Interictal cortical excitability in migraine: a study using transcranial magnetic stimulation of motor and visual cortices. Ann Neurol. 1998;44:209–15.
van der Kamp W, Maassen VanDenBrink A, Ferrari MD, et al. Interictal cortical hyperexcitability in migraine patients demonstrated with transcranial magnetic stimulation. J Neurol Sci. 1996;139:106–10.
van der Kamp W, MaassenVanDenBrink A, Ferrari MD, et al. Interictal cortical excitability to magnetic stimulation in familial hemiplegic migraine. Neurology. 1997;48:1462–4.
Khedr EM, Ahmed M, Mohamed K. Motor and visual cortical excitability in migraineurs patients with or without aura: transcranial magnetic stimulation. Neurophysiol Clin. 2006;36:13–8.
Conforto A, Moraes MS, Amaro E, et al. Increased variability of motor cortical excitability to transcranial magnetic stimulation in migraine: a new clue to an old enigma. J Headache Pain. 2012;13:29–37.
Cortese F, Coppola G, Di Lenola D, et al. Excitability of the motor cortex in patients with migraine changes with the time elapsed from the last attack. J Headache Pain. 2017;18:2.
Siniatchkin M, Kröner-Herwig B, Kocabiyik E, et al. Intracortical inhibition and facilitation in migraine--a transcranial magnetic stimulation study. Headache. 2007;47:364–70.
Curra A, Pierelli F, Coppola G, et al. Shortened cortical silent period in facial muscles of patients with migraine. Pain. 2007;132:124–31.
Currà A, Coppola G, Gorini M, et al. Drug-induced changes in cortical inhibition in medication overuse headache. Cephalalgia. 2011;31:1282–90.
Brighina F, Palermo A, Panetta ML, et al. Reduced cerebellar inhibition in migraine with aura: a TMS study. Cerebellum. 2009;8:260–6.
Coppola G, Cortese F, Bracaglia M, et al. The function of the lateral inhibitory mechanisms in the somatosensory cortex is normal in patients with chronic migraine. Clin Neurophysiol. 2020;131:880–6.
Di Lorenzo C, Coppola G, Currà A, et al. Cortical response to somatosensory stimulation in medication overuse headache patients is influenced by angiotensin converting enzyme (ACE) I/D genetic polymorphism. Cephalalgia. 2012;32:1189–97.
Viganò A, Torrieri MC, Toscano M, et al. Neurophysiological correlates of clinical improvement after greater occipital nerve (GON) block in chronic migraine: relevance for chronic migraine pathophysiology. J Headache Pain. 2018;19:73.
Cosentino G, Fierro B, Brighina F. From different neurophysiological methods to conflicting pathophysiological views in migraine: a critical review of literature. Clin Neurophysiol. 2014;125:1721–30.
Ambrosini A, Coppola G, Iezzi E, et al. Reliability and repeatability of testing visual evoked potential habituation in migraine: a blinded case-control study. Cephalalgia. 2017;37:418–22.
Schoenen J. Is chronic migraine a never-ending migraine attack? Pain. 2011;152:239–40.
Ambrosini A, Kisialiou A, Coppola G, et al. Visual and auditory cortical evoked potentials in interictal episodic migraine: an audit on 624 patients from three centres. Cephalalgia. 2017;37:1126–34.
Coppola G, Parisi V, Di Renzo A, et al. Cortical pain processing in migraine. J Neural Transm. 2020;127:551–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Coppola, G., Magis, D. (2021). Evoked Potentials. In: Coppola, G., Chen, WT. (eds) Neurophysiology of the Migraine Brain. Headache. Springer, Cham. https://doi.org/10.1007/978-3-030-56538-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-56538-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-56537-4
Online ISBN: 978-3-030-56538-1
eBook Packages: MedicineMedicine (R0)