Abstract
Acute myeloid leukemia (AML) is the most common indication for allogeneic hematopoietic stem cell transplant (HSCT). Decision-making around allogeneic HSCT for AML patients in first remission should be based on the estimated risks of relapse and non-relapse mortality (NRM). Risk of relapse is most strongly informed by testing for cytogenetics, somatic mutations, and minimal residual disease (MRD) testing. Several risk scores based on the Hematopoietic Cell Transplant-Co-morbidity Index are available to estimate the risk of NRM using patient comorbidities, and these should be calculated prior to HSCT to inform decision-making. Conditioning chemotherapy should be individualized based on patient comorbidities. In younger fit patients, high-intensity or myeloablative conditioning is generally preferred to reduce relapse. In older (>65 years) patients or those with significant comorbid conditions, reduced intensity conditioning regimens are likely preferred. In vivo T-cell depletion with anti-thymocyte globulin and post-transplant cyclophosphamide reduces the risk of chronic graft-versus-host disease without a significant increase in risk of relapse. HLA-matched related relatives are preferred as donors although unrelated, haploidentical, and umbilical cord blood donors are all possible alternatives for patients without this option. Relapse remains a major problem following alloHSCT and use of chimerism monitoring and MRD testing can be used to inform treatments to prevent relapse including withdrawal of immunosuppression, donor lymphocyte infusion, and hypomethylating agents.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Allogeneic
- Autologous
- Stem cell
- Transplantation
- Conditioning regimens
- Acute myeloid leukemia
- Graft versus host disease
- Comorbidity assessment
- Minimal residual disease
1 Introduction
Allogeneic hematopoietic stem cell transplantation (alloHSCT) is generally considered the most effective post-remission therapy in acute myeloid leukemia (AML) to prevent disease relapse. The efficacy of alloHSCT to treat AML is dependent on two factors: (1) high-dose conditioning chemotherapy and (2) recognition and killing of leukemia cells by the donor immune system, or graft-vs-leukemia (GvL) effect. AML is the most frequent indication for alloHSCT with over 3000 transplants performed annually in the USA and Canada which appears to be increasing [1]. The use of alloHSCT is still limited by several factors including donor availability and high rates of non-relapse mortality (NRM) compared to non-transplant strategies. Nevertheless, even with the availability of several new agents in AML, alloHSCT remains a key part of therapy for many AML patients and is more frequently being used to treat older patients. We review indications for alloHSCT in AML, approach to assessing patient fitness, autologous HSCT, conditioning regimens, donor sources, and post-transplant monitoring and interventions to prevent relapse.
2 Allogeneic Stem Cell Transplant in First Remission
2.1 Impact of Genetics
Patients with newly diagnosed AML are assigned to a risk group to estimate the probability of remission, relapse, and long-term overall survival (OS). Risk status is primarily determined through genetic testing, incorporating results from cytogenetic and somatic mutational testing. Estimation of risk of relapse with chemotherapy treatment in first complete remission (CR1) is essential when considering up-front HSCT. As a rule of thumb, alloHSCT reduces the risk of relapse by approximately half compared to consolidation chemotherapy or autoHSCT [2]. Nevertheless, alloHSCT does not abrogate genetic and other disease prognostic factors, and the probability of cure is still related to these characteristics.
Early studies often showed a benefit of HSCT in AML patients in CR1 relative to chemotherapy consolidation [3]. These studies were limited by a lack of randomization to account for numerous confounding factors influencing outcomes in transplant and non-transplant groups. Several prospective trials have attempted to address this using “Genetic Randomization.” In these trials, AML patients were assigned to alloHSCT or no alloHSCT (chemotherapy consolidation, auto-transplant, or observation) based on the presence of a matched sibling donor. This allows for a less biased comparison of the “donor vs. no-donor” groups using intention-to-treat (ITT) analysis.
A meta-analysis including 24 prospective trials using genetic randomization to assess the impact of alloHSCT in AML patients in CR1 found improved RFS (HR 0.80, 95% CI 0.74–0.86) and OS (HR 0.90, 95% CI 0.82–0.97) in patients with an available matched related donor [4]. In subset analysis, this benefit was only observed in patients with intermediate and adverse but not favorable risk cytogenetics. Based on the calculated HRs, the estimated 5-year OS in the intermediate and adverse risk group was 45% vs. 52% and 20% vs. 31% in no-donor vs. donor group, respectively. These results also have limitations and included trials published over a 20-year time span, and supportive care for HSCT and AML care has improved over time. In addition, not all patients in the donor group received alloHSCT which could underestimate the treatment effect of this intervention. Despite these limitations, these results support the use of alloHSCT in eligible patients with intermediate and adverse risk cytogenetics in CR1. This meta-analysis did not define prognostic risk using somatic mutations in genes (e.g., NPM1, FLT3, and CEPBA) that also inform risk assessment. A retrospective analysis by the German–Austrian AML Study Group did not find a benefit of having an HLA-matched donor in patients with normal karyotype and NPM1mut without FLT3ITD suggesting that other genetically defined favorable risk AML patients also do not have an OS benefit from alloHSCT in CR1 [5].
A decision to offer alloHSCT in CR1 depends on a balance between the anticipated reduction in the risk of relapse and risk of non-relapse mortality (NRM). In general, most patients within the ELN intermediate risk group and all patients in the adverse risk group should be considered for alloHSCT if eligible and a suitable donor exists. Nevertheless, estimated NRM with alloHSCT in AML patients is usually at least 20% which must be offset by a reduction in the risk of relapse [6]. Several groups, including the ELN, have published guidelines outlining the balance between relapse risk and NRM to consider alloHSCT, and adaptation of this is shown in Table 7.1 [2]. This type of decision-making framework is useful, but an individualized approach is still needed and additional considerations include: (1) Patient preferences and expectations, (2) additional prognostic information from next-generation sequencing (NGS) panels, and (3) minimal residual disease (MRD) testing and other disease characteristics.
Given the complexity of estimating prognosis in an individual patient, computer-assisted modeling may be an important approach to incorporate clinical, cytogenetic, and somatic mutational data into transplant decision-making. Gerstung et al. [7] have reported on a precision-medicine-based tool developed using large datasets of AML patients to support clinical decision making (https://cancer.sanger.ac.uk/aml-multistage/). This tool estimates relapse, NRM, and OS outcomes at 3 years using alloHSCT and non-HSCT therapy, although its use has not yet been validated in a clinical setting.
2.2 Impact of MRD
Minimal or measurable residual disease (MRD) testing can also be used to risk stratify patients for transplant decision-making. The HOVON-SAKK group has reported a study investigating the prognostic impact of MRD using NGS and multiparameter flow cytometry (MFC) [8]. This study measured MRD in AML patients in first CR/CRi after two cycles of intensive induction chemotherapy. The 4-year relapse incidence was 73.3% for patients in whom both NGS and MFC were positive, 52.3% among those who were positive by NGS only, 49.8% among those who were positive by MFC only, and 26.7% for those not positive by either technique. The combined use of the two methods was predictive of relapse, RFS and OS in multivariate analysis. The study found that receipt of alloHSCT was associated with lower relapse incidence and better RFS, suggesting that patients with positive MRD after two cycles of chemotherapy should be considered for alloHSCT in CR1.
The relative impact of MRD in AML patients in CR1 treated with alloHSCT, autologous HSCT (autoHSCT) and chemotherapy have also been reported in a separate retrospective study of HOVON-SAKK trials [9]. MRD, as measured by MFC, was “positive” (>0.1%) in ~25% of patients and was associated with higher relapse incidence (4 years: 54% vs. 32%, p < 0.001) and OS (4 years: 50 vs. 65%, p = 0.002) [9]. Interestingly, patients with MRD ≤0.1% and those >0.1% had a similar reduction in relapse incidence with alloHSCT relative to chemotherapy or autoHSCT consolidation, suggesting that GvL is present regardless of MRD status. In patients with MRD <0.1% OS at 4 years was greater in those that received chemotherapy or autoHSCT vs. alloHSCT (71 vs. 60%), suggesting no benefit and possibly harm with alloHSCT in the low-risk group. In comparison, in patients with MRD >0.1% OS at 4 years was similar (47 vs. 53%).
Mutations in NPM1 are present in approximately 30% of AML patients, and the prognostic value of MRD monitoring of NPM1mut has been reported in several studies [10, 11]. A subset analysis of the ALFA-0702 trial reported on outcomes of NPM1mut patients treated with alloHSCT or chemotherapy [10]. In this study, NPM1mut was measured by RT-qPCR following induction in blood and bone marrow samples taken in CR1. A <4 log reduction in NPM1mut was associated with a higher relapse incidence and poorer OS outcomes, when compared to those that achieved >4 log reduction. In patients achieving >4 log reduction, OS and DFS were similar regardless of receipt of alloHSCT, whereas DFS and OS were significantly improved in patients receiving alloSCT as post-remission therapy with <4 log reduction. This is a small retrospective analysis but suggests that MRD results can be used to select patients for alloHSCT.
Presence of MRD detected immediately prior to undergoing alloHSCT also has prognostic significance. The Fred Hutchinson Cancer Research Center (FHCRC) has reported on MRD testing in AML patients (n = 359) undergoing myeloablative alloHSCT in CR1 or CR2 [12]. MRD was assessed on pre-transplant bone marrow samples by MFC and was detected in 24% of patients. Within this group, twice as many patients had adverse cytogenetics and secondary AML. The incidence of relapse at 3 years was 67% and 22% (p < 0.001) in the MRD-positive and -negative groups, respectively. In fact, outcomes of the MRD-positive group were identical to patients with active disease, suggesting that detecting MRD by flow cytometry before alloHSCT is associated with a poor prognosis. The authors of this study did not find a threshold at which MRD appeared to confer a worse prognosis.
Not all detectable MRD pre-transplant appears to confer an equally poor prognosis. A similar study by the FHCRC group measured MRD in patients with NPM1mut AML in remission by MFC and NGS [13]. The authors reported that the NGS methodology was approximately tenfold more sensitive than MFC. Patients in this study with detectable MRD by MFC prior to alloHSCT had significantly higher relapse incidence and lower RFS. In contrast, patients with detectable MRD by NGS alone did not have a higher relapse incidence or worse RFS than MRD-negative patients, suggesting that prognostic relevance of MRD pre-transplant depends on the level of disease and molecular subtype. MRD is a useful tool to further refine prognosis, particularly in favorable and intermediate risk AML patients. Nevertheless, the optimal use of MRD testing in decision-making around transplant requires well-designed prospective studies and ideally standardization of testing between centers.
3 Allogeneic Stem Cell Transplant Beyond First Remission
3.1 Outcomes Beyond First CR
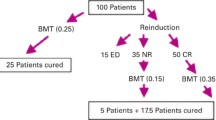
The prognosis for patients with relapsed or refractory (R/R) AML is poor with a chance of long-term survival less than 20% [14,15,16]. This may be improved with the availability of new treatments; however, alloHSCT remains the main curative option for these patients. Factors associated with improved outcome include younger age, favorable risk cytogenetics, late relapse (~>1 year), and no prior receipt of alloHSCT. The Dutch-Belgian group has reported a simple prognostic score incorporating these four factors which divides patients into favorable, intermediate, and poor risk categories [14]. The 5-year OS was reported as 46%, 18%, and 4%, respectively. This type of tool is useful in counseling patients; however, the majority of this cohort fit into an intermediate (24%) or poor risk category (67%).
The majority of R/R AML patients do not have durable remissions following reinduction chemotherapy or targeted agents and alloHSCT should be considered in eligible patients [17]. Nevertheless, outcomes of alloHSCT beyond CR1 appear to be poorer, which may relate to increased TRM and incidence of relapse. Longer-term DFS in AML patients undergoing alloHSCT in CR2 has been reported to range between 40% and 50% [15, 17]. It is important to emphasize that the majority of patients with R/R AML do not go on to receive alloHSCT, in part due to failure to achieve a second durable remission. An analysis of younger patients treated on MRC trials found that only 37% in first relapse received alloHSCT [17]. Survival at 5 years was 44% for those treated with alloHSCT and 21% for those who did not undergo alloHSCT. Interestingly, in subset analyses, patients with favorable risk cytogenetics did not have improved 5-year survival with allograft (35% (alloHSCT) vs. 44% (no-alloHSCT)), whereas patients with intermediate (47% (alloHSCT) vs. 15% (no-alloHSCT)) and poor risk (34% (alloHSCT) vs. 0% (no-alloHSCT)) cytogenetics did benefit. Despite this, we suggest alloHSCT should be offered to eligible patients in CR2 or greater regardless of cytogenetics [2, 18].
3.2 Outcomes with Active Disease
Previous studies report the probability of achieving a CR with intensive chemotherapy in R/R AML patients is approximately 50% in younger patients and 20–30% in older patients [17, 19]. In patients who do not achieve CR, prognosis is very poor and alloHSCT with active disease is an option for some patients. There have been several studies of AML patients with chemo-refractory active disease treated with alloHSCT, and the longer-term DFS is reported as ~10–30% [20]. An EBMT registry-based report of AML patients (n = 852) undergoing myeloablative (MA) alloHSCT with active disease between 2000 and 2012 found a 2-year OS and DFS of 30% and 25%, respectively [21]. A similar study of CIBMTR patients reported outcomes for AML patients with active disease undergoing myeloablative alloHSCT from 1995 to 2004 [22]. OS at 3 years was 19% with the incidence of death at 100 days post-transplant 39%, primarily related to leukemia. This study also included patients (19%) who were in first relapse and did not undergo reinduction chemotherapy before conditioning, although results were similar in this group. Multivariate analysis of baseline factors showed that survival was worse with duration of remission <6 months, circulating blasts, a mismatched unrelated donor, a related donor other than an HLA-matched sibling, poor PS (Karnofsky or Lansky score less than 90), and poor-risk cytogenetics. The authors developed a prognostic score based on these factors with four categories: 0, 1, 2, ≥3. These categories accounted for 13%, 29%, 30%, and 28% of patients, respectively, and 3-year OS in these risk groups was 42%, 28%, 15%, and 6%, respectively.
These results suggest that some patients with active disease can be cured with alloHSCT; however, the reported outcomes are based on a selected group and are not applicable to all patients with active disease. AlloHSCT has potential for significant harm in this setting and risk for significant morbidity related to transplant coupled with a low chance of cure, makes this type of approach impractical for many centers with limited resources. Other treatment options including clinical trials, lower intensity therapy or best supportive care, and palliative care may be a preferred approach in many patients with AML and active disease.
4 Autologous Stem Cell Transplant
AutoHSCT is also a potential post remission therapy in AML, however is less commonly used than alloHSCT. AutoHSCT relies on high-dose conditioning chemotherapy to eradicate residual leukemia cells, without the potential for GvL effect. There is no GVHD with autoHSCT and NRM and longer-term morbidity is lower than alloHSCT, making its use appealing in some patients including those without a suitable donor. Three prospective RCTs comparing autoHSCT to chemotherapy consolidation have reported a lower relapse incidence with autoHSCT which is shown in Table 7.2 [23,24,25]. Of these studies, one showed a late OS benefit with autoHSCT [24] although this was not found in the other studies [23, 25]. Retrospective registry analyses show a higher relapse incidence with autoHSCT relative to alloHSCT using matched sibling, T-cell replete haplo-identical sibling and unrelated donors [26,27,28]. However, all of these studies showed similar long-term OS for both autoHSCT and alloHSCT, related to higher NRM in the latter group [26,27,28]. One study reported an OS advantage with autoHSCT compared to alloHSCT using mismatched unrelated donors [28].
Despite evidence of efficacy, treatment of AML with autoHSCT is less frequently used in the modern era, and in Europe accounts for <10% of transplants in CR1 [1, 29]. This may be related to increased donor availability for alloHSCT with the use of haploidentical sibling, cord, and unrelated donors and perhaps a perceived decrease in NRM over time with alloHSCT. AutoHSCT is also limited by concerns around graft contamination with leukemic cells, and historically, there have been many attempts to perform graft-purging although the impact of this is unclear [30].
It appears that autoHSCT is most effective in AML patients with intermediate-risk genetic changes [28, 31,32,33] and recent ELN guidelines include autoHSCT as a post-remission therapy option for this group [34]. There is evidence that MRD can also be used to select patients who will benefit from autoHSCT. The GIMEMA AML1310 trial addresses this and performed MRD testing by MFC in intermediate-risk patients following the first consolidation cycle [35]. Patients with negative MRD received consolidation with autoHSCT, whereas MRD-positive patients were preferentially treated with alloHSCT. The results of this study have been presented in abstract form and 2-year OS and DFS of 78.6% and 61.4% vs. 69.8% and 66.6% in the MRD-negative vs. -positive groups, respectively. Outcomes in the intermediate-risk group receiving autoHSCT were similar to good-risk patients (also treated with autoHSCT), providing some evidence for autoHSCT in a selected MRD-negative group. Further work needs to be done to define the role of this therapy, and autoHSCT should be included as a post remission option in frontline clinical trials in fit patients with intermediate risk and favorable risk disease and negative MRD.
5 Assessing Fitness for HSCT
Several models are available to estimate both risk of NRM and survival benefit to optimize decisions about a patient suitability for HSCT. Historically, age has been used as a selection criterion for alloHSCT referrals. Nevertheless, age alone is a poor prognostic factor. Reduced intensity conditioning (RIC) has extended the use of alloHSCT to older adults and patients ineligible for MAC alloHSCT. This necessitates the requirement for objective tools to further refine the balance of risk–benefit associated with HSCT.
5.1 The HCT-Specific Comorbidity Index (HCT-CI)
The HCT-CI was initially developed from the Charlson Comorbidity Index (CCI) and is the most widely accepted model for the assessment of fitness prior to alloHSCT [36]. It was developed in a cohort of 1055 patients with different hematological diseases who received alloHSCT after nonmyeloablative (n = 249) or myeloablative (n = 761) conditioning. The HCT-CI includes 17 comorbidities with each scored from 1 to 3 (Table 7.3). In the validation set, HCT-CI scores showed higher sensitivity than the CCI scores in capturing comorbidities. HCT-CI scores of 1–2 and ≥3 were found in 34% and 28% of patients, while only 10% and 3% of patients had CCI scores of 1 and ≥2, respectively. The HCT-CI scores of 0, 1–2, and ≥3 showed good discrimination of NRM (14%, 21%, and 41%) and survival (71%, 60%, and 34%), respectively.
The prognostic capacity of the HCT-CI has been augmented by the addition of age to build a composite comorbidity/age index using a dataset of 3033 allogeneic HCT recipients [37]. In multivariate models, age >40 years has been shown to impact NRM as equivalent to a single comorbidity with a score of 1. The composite comorbidity/age index provides a more accurate estimate of biological age, and patients should be evaluated with the composite comorbidity/age score, incorporating the impact of comorbidities and age, as well as disease characteristics for selection of the most beneficial transplant strategy. Regardless of age, patients with low scores should be considered for randomized clinical trials or offered higher-intensity regimens. An exception is patients older than 65 years as there are limited data on usage of high-dose regimens beyond this age. Likewise, regardless of age, patients with higher scores are more suitable candidates for less intense regimens.
The HCT-CI can be further augmented by the addition of three markers: ferritin, albumin, and platelet count [38]. The prognostic capacity of an augmented comorbidity/age index was investigated among 724 recipients of allogeneic HCT from HLA-mismatched (n = 345), haploidentical (n = 117), and umbilical cord blood (UCB, n = 262) grafts between 2000 and 2013. Patients with scores of <4 had better survival compared to those with scores of ≥4 and received HLA-mismatched (55% versus 39%, p < 0.0008), HLA-haploidentical (58% versus 38%, p = 0.01), or UCB grafts (67% versus 48%, p = 0.004), respectively. These results support the use of comorbidity assessment as a valid prognostic tool among the recipients of alloHCT from alternative graft sources. Table 7.3 describes the definitions of the augmented comorbidity/age index [39].
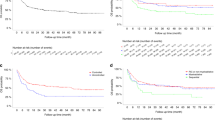
The prognostic role of comorbidities has been specifically assessed among patients with AML (n = 391) or MDS (n = 186) who received either nonmyeloablative (n = 125) or high-dose conditioning (n = 452) [40]. In multivariate analyses of risk factors, high HCT-CI scores and high disease risk were the most significant factors predicting NRM (p < 0.0001 and p = 0.004), OS (p < 0.0001 and p < 0.0001), and RFS (p < 0.0001 and p < 0.0001), respectively. Therefore, all patients were stratified into four risk groups incorporating both comorbidities and disease-risk (Table 7.4). Rates of 2-year OS were 70% and 78% among AML/MDS patients with HCT-CI scores of 0–2 and low-risk disease following nonmyeloablative and high-dose HCT, respectively, and they were 57% and 51%, respectively, if patients had high-risk AML/MDS. Results suggested that AML/MDS patients with low comorbidity burden are candidates for prospective randomized studies to determine the role of conditioning intensity. Unsurprisingly, patients with higher HCT-CI scores (≥3) overall had inferior survivals, in particular, those with high-risk AML/MDS (OS of 29% and 24%, respectively). The poor survival rates were due to more relapses (49%) among nonmyeloablative recipients and more frequent NRM (46%) among high-dose recipients (Fig. 7.1) [40]. A systematic methodology for data acquisition and consistent guidelines for comorbidity coding are summarized in a Web-based calculator (www.hctci.org) [41].
Risk stratification of patients with acute myeloid leukemia/myelodysplasia and receiving allogeneic hematopoietic cell transplantation (HCT). Group I (gray) included HCT-specific comorbidity index (CI) scores 0–2 plus low disease risk; group II (yellow) included HCT-CI scores 0–2 plus intermediate and high disease risks; group III (blue) included HCT-CI scores ≥3 plus low disease risks; and group IV (red) included HCT-CI scores ≥3 plus intermediate and high disease risks. NRM, nonrelapse mortality; OS, overall survival; RFS, relapse-free survival. (From Sorror et al.: J Clin Oncol Vol. 25, 2007: 4246–4254. Reprinted with permission. © 2007 American Society of Clinical Oncology. All rights reserved)
5.2 The HCT-CI and Disease Risk Index
While patient-specific variables have a significant impact on NRM, disease-specific variables should be also taken into consideration as a predictor of post-transplant relapse when counseling patients regarding the feasibility of alloHSCT. In a recent analysis including 942 alloHSCT recipients with AML/MDS, a novel prognostic model, hematopoietic cell transplant-composite risk (HCT-CR), was developed and validated by combining the refined disease risk index (DRI-R) and comorbidity/age index to prognosticate for outcomes [42]. The HCT-CR index stratified patients into four risk groups: low-risk patients with low/intermediate DRI-R and comorbidity/age ≤3 (N = 272); intermediate-risk patients with low/intermediate DRI-R and comorbidity/age >3 (N = 168); high-risk patients with high/very high DRI-R and comorbidity/age ≤3 (N = 284); and very high-risk patients with high/very high DRI-R and comorbidity/age >3 (N = 184). Patients with higher HCT-CR scores had significantly worse outcomes compared to those with lower scores. The low-risk group, intermediate, high, and very high-risk groups had adjusted HR of 1.37 (p < 0.04), 2.08 (p < 0.001), and 2.92 (p < 0.001), respectively. The HCT-CR model provided better discriminative capacity for OS prediction compared with all prior models independently, including cytogenetic risk group, DRI-R, and comorbidity/age model (C-statistics: 0.62, 0.55, 0.60, and 0.54, respectively) (p < 0.001).
Similar results were demonstrated in another recent analysis of 959 alloHSCT recipients between 2000 and 2013 at the University of Minnesota for hematological malignancies (66% with leukemia) [43]. The HCT-CI was combined with DRI to produce a composite disease risk and HCT comorbidity index (DRCI). The new model stratified patients into six risk groups with discrete outcomes. Patients with very-high risk DRCI had worse 2-year OS compared with patients with very low-risk DRCI, 34% versus 74%, respectively (p < 0.01). In multivariable model adjusted for patient age and donor type, the DRCI was an independent predictor of overall mortality, relapse risk, DFS, and GVHD-free/RFS. These results suggest that patient-related factors should simultaneously be considered with disease-specific variables to better risk stratify outcomes of patients with AML/MDS undergoing alloHSCT.
5.3 Comprehensive Geriatric Assessment (CGA)
Older patients experience additional age-specific health vulnerabilities relative to younger patients. Unfortunately, performance status assessment tools such as KPS and European Cooperative Oncology Group performance status (ECOG) do not provide a comprehensive evaluation of health status. CGA could potentially reveal these vulnerabilities; however, it has several domains, and identification of the most relevant predictors on outcomes in alloHSCT requires further studies. In a recent analysis of outcomes of 527 alloHSCT recipients who were 60 years or older, 40% with AML, the incidence of post-transplant delirium was strongly associated with pre-transplant fall in the preceding year, use of potentially inappropriate medications, low platelet count, and impaired renal function in multivariate models; while age older than 70 years and impaired activities of daily living were significantly associated with post-transplant fall, both assessed at day 100 [44]. Both delirium (HR 1.66; 95% CI, 1.09–2.52; p < 0.023) and fall (HR 2.14; 95% CI 1.16–3.95; p < 0.026) were significantly associated with increased NRM at 100 days; further fall (HR 1.93; 95% CI 1.18–3.14; p = 0.016), but not delirium, was significantly associated with reduced OS. Improved understanding and identification of the most significant predictors of outcomes among CGA tools is of prime importance. The majority of these variables are potentially targetable with preemptive interventions to improve the outcomes in older patients.
5.4 Recommended Models
The augmented comorbidity/age index is a relatively simple tool that could be used in the daily clinical practice to council patients on potential risks of post-transplant NRM. An online calculator is available to provide the HCT-CI score at www.hctci.org. All patients 60 years or older should additionally be assessed using domains of CGA. This approach aims at revealing potential targets for peri-transplant interventions to improve outcomes and post-transplant quality of life.
6 Conditioning Regimens and Donor Type
6.1 Conditioning Regimens
Conditioning regimens given prior to alloHSCT create immunologic and physical space to allow for engraftment and for eradication of residual leukemia cells. Therefore, conditioning consists of a lymphodepleting component, which targets the host lymphoid system and a myeloablative component which theoretically should target the host stem cells as well as the remaining malignant cells. The conditioning regimen influences risk of GVHD, TRM, relapse incidence, and OS. Nevertheless, there is no “one-size fits all” approach to the selection of a conditioning regimen, which needs to be tailored to disease characteristics, patient fitness, and comorbidities.
Traditionally, conditioning regimens can be classified based on the reversibility of cytopenia into myeloablative conditioning (MAC), non-myeloablative (NMA) and reduced intensity conditioning regimes (RIC). MAC leads to irreversible cytopenia and requires stem cell support. In contrast, NMA protocols cause minimal cytopenias and can be given without stem cell support but are currently not favored especially in AML patients with advanced disease due to high relapse rates [45]. RIC is positioned between MA and NMA, causes profound, but not irreversible cytopenia which requires stem cell support [46].
Early studies comparing myeloablative CyTBI and BuCy regimens suggested that TBI resulted in improved survival outcomes with lower relapse incidence, TRM, and improved OS [47, 48]. These findings have not been confirmed in recent registry-based studies, which report equivalent or improved outcomes with BuCy compared to CyTBI [49, 50]. This may relate to widespread use of IV busulfan dosing in modern eras, which has more predictable absorption and pharmacokinetics with lower toxicity and risk of veno-occlusive disease (VOD) than oral busulfan used in older studies [51, 52]. High-dose TBI regimens are infrequently used in AML partly due to the long-term toxicities with TBI, such as endocrine dysfunction, cataracts, and risk of second cancers.
Several strategies may reduce toxicity associated with MAC regimens including the use of pharmaco-kinetic (PK)-guided busulfan dosing, avoidance of dual alkylator regimens, and treosulfan-based regimens [53,54,55,56,57,58]. Reduced intensity conditioning (RIC) regimens have improved the tolerability and safety of alloHSCT in older patients and those with comorbidities.
Retrospective studies have found that RIC regimens result in lower rates of TRM with a higher risk of relapse [59]. Two recent prospective trials have compared RIC vs. MAC alloHSCT in relatively young, fit patients with AML with conflicting results. One study by the BMT-CTN found a significantly higher relapse incidence with RIC regimens with worse OS, and the trial was stopped early due to this [60]. In contrast, two European trials comparing RIC vs. MAC regimens in AML in CR1 found similar OS with each regimen [61, 62]. However, differences in trial design, donor source, and age adjustment make comparisons between these studies difficult.
There is also evidence that MAC is less beneficial in AML patients with high-risk disease and complex karyotypes [63,64,65,66,67]. With this in mind, FLAMSA-RIC, a sequential approach combining intensive chemotherapy, RIC, and prophylactic donor lymphocyte infusions (DLI) was developed demonstrating promising results in adverse risk AML patients [68,69,70,71,72]. However, to further improve and personalize conditioning regimens, there is a need to better understand the interaction between the microenvironment and disease biology. In addition, the potential incorporation of targeted agents into conditioning regimes should be explored to reduce disease burden and thus relapse after alloHSCT. In general, we suggest that fit, younger patients (<65 years) should receive MAC regimens although this remains an individualized decision based on patient comorbidities and estimated risk of NRM.
6.2 Donor Type
Historically, a graft from an HLA-matched sibling donor (MSD) has been the ideal and in general is still the preferred donor choice. There are three graft sources for alloHSCT: bone marrow (BM), peripheral blood stem cells (PBSC), and cord blood (CB). Anasetti et al. recently compared in a large randomized Phase 3 trial PBSC and BM from unrelated donors in patients undergoing alloHSCT [73]. The authors did not detect significant survival differences between both arms, although the PBSC group had a higher risk of cGvHD and lower risk of graft failure. Although the trial did not exclusively focus on AML patients (~50% of patients), it confirmed previous retrospective analyses [74, 75]. In the setting of RIC, the positive effect of PBSC on OS and LFS was more pronounced as recently shown by Savani et al. in a retrospective analysis [76].
Despite PBSC being the main stem cell source for HSCT in adults, the use of alternative graft sources such as haploidentical donors, mainly through the introduction of post-transplant cyclophosphamide (PT-Cy) is increasing [1, 29]. In a large retrospective analysis, Ringden et al. [77] compared relapse and survival in AML/ALL patients, receiving MSD HSCT to patients that received T-cell-replete or T-cell-depleted haploidentical HSCT. There was no difference in RI between recipients of haploidentical and matched sibling grafts, but a significantly higher NRM in the haploidentical group. Similar to unrelated donors, using PB as graft source for haploidentical HSCT has been associated with increased grade II–IV GvHD, but without a significant effect on survival outcomes [78].
Comparing the outcomes of haploidentical HSCT with MSD in AML in CR1, Salvatore et al. found that in intermediate-risk AML patients receiving a haploidentical graft exhibited a less favorable outcome with decreased LFS and OS and higher NRM, whereas in adverse-risk AML patients, the outcomes were similar [79]. Although the use of CB as graft source has been decreasing, data from Milano et al. suggest that OS is superior in acute leukemia and MDS patients receiving CB compared to HLA-mismatched unrelated donors in the presence of MRD [80]. Several reports have shown that CB as graft can provide a therapeutic benefit in AML patients regardless of age and risk stratification [81,82,83,84]. There is no clear evidence for superiority of haploidentical grafts vs. HLA-mismatched unrelated donors [85]. Therefore, based on the available data, MSD remain the first-choice donor for AML patients in first remission.
6.3 Role of T-Cell Depletion
GvHD is one of the leading causes of NRM and morbidity after allogeneic HSCT. In addition to standard GVHD prophylaxis strategy, in vivo T-cell depletion with antithymocyte globulin (ATG) has been developed to reduce the incidence of especially cGvHD. Multiple randomized studies evaluated the use of ATLG (former ATG-Fresenius) or thymoglobulin, both produced from immunized rabbits, for GvHD prophylaxis in patients who underwent alloHSCT from unrelated as well as HLA-identical matched donors [86,87,88,89]. Overall, the use of ATG was associated with a lower incidence of cGvHD without affecting OS and relapse incidence, suggesting a broader use of ATG for related and unrelated donor transplants. Due to its potent effect on proliferating T cells as GvHD prophylaxis for haploidentical HSCT, PT-Cy has been investigated for allogeneic HSCT in the setting of matched related and unrelated donors alone or in combination with immunosuppressive therapy. Initial promising results for PT-Cy for alloHSCT with matched related and unrelated donors receiving BM as graft as single agent in hematological malignancies with cGVHD rates <15% prompted the further investigation of PT-Cy in alloHSCT [90, 91]. PT-Cy as single immunosuppressive agent for allo-HSCT with PBSC as graft source was associated with severe aGvHD and an increased NRM, prompting investigations of PT-Cy in combination with other immunosuppressive drugs. In fact, the combination of PT-Cy with a calcineurin inhibitor enhanced its effect on GvHD prophylaxis in particular severe cGvHD for PBSC and BM from MSD and MUD, thus reducing mortality and improving survival [92,93,94]. Although randomized trials are still lacking, PT-Cy appears to be a reasonable alternative for in vivo T-cell depletion and may have a cost advantage over ATG. A promising approach for ex vivo T-cell depletion is αβ T-cell depletion to overcome the HLA disparity for patients undergoing haploidentical HSCT as well as HLA-matched HSCT [95]. However, clinical trials comparing αβ T-cell depletion with other immunosuppressive approaches are still absent.
7 Maintenance Therapy and Monitoring for Relapse
7.1 Maintenance Therapy
Disease relapse remains the most frequent cause of death following HSCT, underscoring the need for novel approaches with maintenance and pre-emptive therapies [96]. Hypomethylating agents (HMAs) are attractive options for maintenance therapy as they can be delivered in the outpatient setting and are well tolerated. Maintenance using decitabine has been compared in an RCT following chemotherapy and does not reduce relapse in this setting [97]. Following alloHSCT, HMAs may augment GvL through increased expression of tumor antigens such as WT1 on leukemic cells [98]. In addition, pre-clinical models show that HMAs expand regulatory T-cell populations, suggesting they may not increase risk of GVHD [98, 99]. Several non-randomized studies have evaluated HMAs post-HSCT [100,101,102,103]. These agents have acceptable safety and tolerability, although the optimal dose appears to be lower than for up-front treatment [100, 103]. The EFS and OS reported in these trials is promising; however a prospective, randomized trial is needed to evaluate the efficacy of HMAs in the post-HSCT setting.
Targeted therapy, such as tyrosine kinase inhibitors, can prevent relapse in Philadelphia positive ALL and CML post-HSCT, and targeted agents could play a similar role in AML (PMID 20005967). FLT3-mutated AML is a suitable candidate to investigate post-HSCT maintenance as relapse remains high despite the availability of several FLT3-inhibitors. Promising results using sorafenib maintenance in FLT3-positive AML have been reported in retrospective studies relative to historical controls [104, 105]. Recently, the results of an RCT by the German/Austrian group evaluating sorafenib maintenance was reported in abstract form [106]. In this trial, patients with FLT3-ITD mutated AML in CR1 or beyond were randomized to either placebo or sorafenib 400 mg PO BID started day +60 to +100 post-HSCT and continued for 24 months. The primary endpoint of RFS was 85% vs. 53% at 2 years in the sorafenib and placebo group, respectively (HR = 0.39; 95% CI 0.18–0.85; p = 0.013). There was a higher rate of relapse in the placebo-treated group but no difference in NRM between groups. OS was also higher in the sorafenib-treated patients (HR = 0.45; 95% CI 0.20–0.97, p = 0.03). The rates of acute and chronic GVHD were similar between groups; however, it appeared that skin toxicity and electrolyte abnormalities were more frequent with sorafenib. This suggests sorafenib maintenance can prevent relapse in this group of AML patients, and several studies evaluating maintenance therapy using other FLT3-inhibitors are ongoing.
7.2 Pre-emptive Treatment for MRD and Mixed Chimerism
There is growing evidence that pre-emptive treatment for early or low burden disease with immunomodulation and other therapies may prevent relapse in AML following HSCT [107,108,109]. Monitoring of chimerism following alloHSCT is used to assess risk of disease relapse and graft failure. “Full chimerism” refers to a state of complete engraftment of donor cells in the recipient, and this is often determined in a specific lineage (e.g., lymphoid, CD34+). Chimerism is frequently assessed by monitoring polymorphic short-tandem repeats (STR) of <10 nucleotides or microsatellite regions. Several other methods are possible including FISH for X and Y chromosomes in opposite sex donors, qPCR analysis of single-nucleotide polymorphisms (SNP), and insertion/deletions (Indels) [110]. Multiple studies have shown that mixed or increasing chimerism in lymphoid or CD34+ compartments is associated with higher risk of relapse [111,112,113]. The chance of mixed chimerism is increased following RIC regimens and with use of a BM graft; however, mixed chimerism at early time points is also common following MAC regimens [112]. Risk of relapse appears to be lower in patients achieving full lymphoid chimerism at early time points following both RIC and MAC regimens in patients with AML [114].
It is important to emphasize that mixed or increasing chimerism is not however synonymous with disease relapse, and the timing and threshold determine test characteristics [115]. This is relevant as treatment of mixed chimerism with rapid taper of immunosuppression or donor-lymphocyte infusion (DLI) can have significant toxicity by provoking severe GVHD. A study from by Wong et al. highlights the tradeoff of chimerism testing and reported a 100-day T lymphoid chimerism threshold of 85% had a high specificity (87.5%) but low sensitivity (46.7%) for relapse, with positive and negative predictive values of 38.9% and 90.6%, respectively. Withdrawal of immunosuppression and pre-emptive DLI are commonly used for mixed chimerism, and there is evidence that this reduces relapse. A prospective study of pre-emptive DLI for mixed chimerism in pediatric AML patients found that patients with mixed chimerism had lower EFS than those with full chimerism (80% vs. 30%, p < 0.001) [116]. EFS was improved better in patients with mixed chimerism that received pre-emptive treatment with withdrawal of immunosuppression or DLI (n = 13) than those that did not (n = 7), and the 3-year EFS was 46% and 0%, respectively.
Treatment with azacitidine may also be effective in treating mixed chimerism and preventing relapse. The RELAZA trial used preemptive treatment with azacitidine for mixed chimerism or detectable MRD post-HSCT in patients with AML and MDS (n = 59) [107]. In this study, chimerism was measured using STR in CD34+ sorted cells at intervals of 3–4 weeks during the first 8 months after HSCT and every 7–8 weeks from months 8 to 24. Patients with chimerism <80% (n = 20) were eligible for treatment with azacitidine and withdrawal of immunosuppression, and in this group, 50% had an increase of chimerism >80%. Nevertheless, 65% (n = 13) of patients entering the treatment phase ultimately relapsed with a median time of 231 days from the detection of MC <80%. In the RELAZA-2 trial by the same group, MRD testing was incorporated to identify AML patients at high risk for relapse following HSCT. Detection of NPM1mut and core-binding factor transcripts by RT-qPCR following HSCT has been shown to predict relapse [108, 117]. In this trial, CD34+ chimerism testing (n = 108) was performed in addition to MRD testing using RT-qPCR for NPM1mut (n = 77) or fusion transcripts DEK-NUP214 (n = 1), RUNX1-RUNX1T1 (n = 9), or CBFB1-MYH11 (n = 10). Patients were offered treatment with azacitidine on the basis of chimerism <80% (n = 19) or MRD positivity (n = 34), and 40% had an MRD or chimerism response and 19% had stable MRD or chimerism. The 1-year OS and PFS was 76 and 42%, respectively.
The exact benefit of interventions based on chimerism and MRD monitoring is difficult to determine given the non-randomized nature of these studies. Despite these limitations, pre-emptive treatment with taper of IST and DLI should be considered in patients with mixed or increasing chimerism or detectable MRD. In patients deemed to be at high risk of severe GVHD with this approach, treatment with azacitidine could be an alternative approach to prevent or delay relapse.
8 Conclusion
In conclusion, alloHSCT has an important role in the upfront treatment of intermediate and high-risk AML patients. Patients determined to have a high risk for relapse based on MRD testing may also benefit from alloHSCT in first remission. AutoHSCT is a potential option in patients with intermediate-risk AML without detectable MRD. Patients with R/R AML should be targeted to receive alloHSCT if eligible as this remains the primary curative option. Selection of conditioning regimens should be individualized; however, myeloablative regimens are preferred in fitter, younger patients. A formalized assessment of a patient’s comorbidities should be performed prior to HSCT using a tool such as the HCT-CI or augmented HCT-CI to estimate the risk of NRM and guide patient discussions and inform management. Significant work remains to reduce NRM with HSCT, and a major obstacle to this remains GVHD which appears to be reduced with lymphodepletion using ATG and PT-Cy. Relapse remains the major cause of death following HSCT, and randomized prospective trials are needed to investigate the role of maintenance and pre-emptive therapy for MRD.
References
D’Souza A, Fretham, C (2018) Current uses and outcomes of hematopoietic stem cell transplantation – summary slides CIBMTR website 2018. Available from: https://www.cibmtr.org/Pages/index.aspx
Cornelissen JJ, Gratwohl A, Schlenk RF, Sierra J, Bornhauser M, Juliusson G, et al. The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat Rev Clin Oncol. 2012;9(10):579–90.
Appelbaum FR, Dahlberg S, Thomas ED, Buckner CD, Cheever MA, Clift RA, et al. Bone marrow transplantation or chemotherapy after remission induction for adults with acute nonlymphoblastic leukemia. A prospective comparison. Ann Intern Med. 1984;101(5):581–8.
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301(22):2349–61.
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358(18):1909–18.
Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood. 2016;127(20):2427–38.
Gerstung M, Papaemmanuil E, Martincorena I, Bullinger L, Gaidzik VI, Paschka P, et al. Precision oncology for acute myeloid leukemia using a knowledge bank approach. Nat Genet. 2017;49(3):332–40.
Jongen-Lavrencic M, Grob T, Hanekamp D, Kavelaars FG, Al Hinai A, Zeilemaker A, et al. Molecular minimal residual disease in acute myeloid leukemia. N Engl J Med. 2018;378(13):1189–99.
Versluis J, Kalin B, Zeijlemaker W, Passweg J, Graux C, Manz MG, Vekemans MC, Biemond BJ, Legdeur M, van Marwijk Kooy M, de Weerdt O, Wijermans PW, Hoogendoorn M, Bargetzi MJ, Kuball J, Schouten HC, van der Velden V, Janssen J, Pabst T, Lowenberg B, Jongen-Lavrencic M, Schuurhuis G, Ossenkoppele G, Cornelissen JJ. Graft-versus-leukemia effect of allogeneic stem-cell transplantation and minimal residual disease in patients with acute myeloid leukemia in first complete remission. JCO Precis Oncol. 2017; https://doi.org/10.1200/PO.17.00078.
Balsat M, Renneville A, Thomas X, de Botton S, Caillot D, Marceau A, et al. Postinduction minimal residual disease predicts outcome and benefit from allogeneic stem cell transplantation in acute myeloid leukemia with NPM1 mutation: a study by the Acute Leukemia French Association Group. J Clin Oncol. 2017;35(2):185–93.
Ivey A, Hills RK, Simpson MA, Jovanovic JV, Gilkes A, Grech A, et al. Assessment of minimal residual disease in standard-risk AML. N Engl J Med. 2016;374(5):422–33.
Araki D, Wood BL, Othus M, Radich JP, Halpern AB, Zhou Y, et al. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual disease-based definition of complete remission? J Clin Oncol. 2016;34(4):329–36.
Zhou Y, Othus M, Walter RB, Estey EH, Wu D, Wood BL. Deep NPM1 sequencing following allogeneic hematopoietic cell transplantation improves risk assessment in adults with NPM1-mutated AML. Biol Blood Marrow Transplant. 2018;24(8):1615–20.
Breems DA, Van Putten WL, Huijgens PC, Ossenkoppele GJ, Verhoef GE, Verdonck LF, et al. Prognostic index for adult patients with acute myeloid leukemia in first relapse. J Clin Oncol. 2005;23(9):1969–78.
Forman SJ, Rowe JM. The myth of the second remission of acute leukemia in the adult. Blood. 2013;121(7):1077–82.
Ganzel C, Sun Z, Cripe LD, Fernandez HF, Douer D, Rowe JM, et al. Very poor long-term survival in past and more recent studies for relapsed AML patients: the ECOG-ACRIN experience. Am J Hematol. 2018;93:1074.
Burnett AK, Goldstone A, Hills RK, Milligan D, Prentice A, Yin J, et al. Curability of patients with acute myeloid leukemia who did not undergo transplantation in first remission. J Clin Oncol. 2013;31(10):1293–301.
Network NCC (2019) Acute myeloid leukemia (version 2.2019). Available from: https://www.nccn.org/professionals/physician_gls/pdf/aml.pdf
Ravandi F, Ritchie EK, Sayar H, Lancet JE, Craig MD, Vey N, et al. Vosaroxin plus cytarabine versus placebo plus cytarabine in patients with first relapsed or refractory acute myeloid leukaemia (VALOR): a randomised, controlled, double-blind, multinational, phase 3 study. Lancet Oncol. 2015;16(9):1025–36.
Gyurkocza B, Lazarus HM, Giralt S. Allogeneic hematopoietic cell transplantation in patients with AML not achieving remission: potentially curative therapy. Bone Marrow Transplant. 2017;52(8):1083–90.
Nagler A, Savani BN, Labopin M, Polge E, Passweg J, Finke J, et al. Outcomes after use of two standard ablative regimens in patients with refractory acute myeloid leukaemia: a retrospective, multicentre, registry analysis. Lancet Haematol. 2015;2(9):e384–92.
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, et al. Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol. 2010;28(23):3730–8.
Vellenga E, van Putten W, Ossenkoppele GJ, Verdonck LF, Theobald M, Cornelissen JJ, et al. Autologous peripheral blood stem cell transplantation for acute myeloid leukemia. Blood. 2011;118(23):6037–42.
Burnett AK, Goldstone AH, Stevens RM, Hann IM, Rees JK, Gray RG, et al. Randomised comparison of addition of autologous bone-marrow transplantation to intensive chemotherapy for acute myeloid leukaemia in first remission: results of MRC AML 10 trial. UK Medical Research Council Adult and Children’s Leukaemia Working Parties. Lancet. 1998;351(9104):700–8.
Zittoun RA, Mandelli F, Willemze R, de Witte T, Labar B, Resegotti L, et al. Autologous or allogeneic bone marrow transplantation compared with intensive chemotherapy in acute myelogenous leukemia. European Organization for Research and Treatment of Cancer (EORTC) and the Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto (GIMEMA) Leukemia Cooperative Groups. N Engl J Med. 1995;332(4):217–23.
Gorin NC, Labopin M, Piemontese S, Arcese W, Santarone S, Huang H, et al. T-cell-replete haploidentical transplantation versus autologous stem cell transplantation in adult acute leukemia: a matched pair analysis. Haematologica. 2015;100(4):558–64.
Keating A, DaSilva G, Perez WS, Gupta V, Cutler CS, Ballen KK, et al. Autologous blood cell transplantation versus HLA-identical sibling transplantation for acute myeloid leukemia in first complete remission: a registry study from the Center for International Blood and Marrow Transplantation Research. Haematologica. 2013;98(2):185–92.
Saraceni F, Labopin M, Gorin NC, Blaise D, Tabrizi R, Volin L, et al. Matched and mismatched unrelated donor compared to autologous stem cell transplantation for acute myeloid leukemia in first complete remission: a retrospective, propensity score-weighted analysis from the ALWP of the EBMT. J Hematol Oncol. 2016;9(1):79.
The European Society for Blood and Marrow Transplantation (2017) EBMT annual report 2017. European Society for Blood and Marrow Transplantation. 1 Mar 2018
Lowenberg B, Voogt P. Autologous stem-cell transplantation and purging. J Clin Oncol. 1996;14(8):2194–6.
Cornelissen JJ, Versluis J, Passweg JR, van Putten WL, Manz MG, Maertens J, et al. Comparative therapeutic value of post-remission approaches in patients with acute myeloid leukemia aged 40-60 years. Leukemia. 2015;29(5):1041–50.
Limvorapitak W, Barnett MJ, Hogge DE, Forrest DL, Nevill TJ, Narayanan S, et al. Outcomes of intermediate risk karyotype acute myeloid leukemia in first remission undergoing autologous stem cell transplantation compared with allogeneic stem cell transplantation and chemotherapy consolidation: a retrospective, propensity-score adjusted analysis. Clin Lymphoma Myeloma Leuk. 2018;18(11):e481–e91.
Saraceni F, Bruno B, Lemoli RM, Meloni G, Arcese W, Falda M, et al. Autologous stem cell transplantation is still a valid option in good- and intermediate-risk AML: a GITMO survey on 809 patients autografted in first complete remission. Bone Marrow Transplant. 2017;52(1):163–6.
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47.
Venditti A, Piciocchi A, Candoni A, Melillo L, Calafiore V, Cairoli R, De Fabritiis P, Storti G, Salutari P, Lanza F, Martinelli G, Luppi M, Mazza, P, Falini B, Cuneo A, Specchia G, Fabbiano F, Tafuri A, Ronci B, Tieghi A, Fracchiolla N, Capelli D, Foà R, Ronco F, La Sala E, Fazi P, Maurillo L, Buccisano F, Del Principe M, Lo Coco F, Arcese W, Amadori S (2017) Risk-adapted, MRD-directed therapy for young adults with newly diagnosed acute myeloid leukema: results of the AML 1310 trial of the GIMEMA group. iN: EHA annual meeting, 23 June 2017, Madrid
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912–9.
Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB, et al. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol. 2014;32(29):3249–56.
Vaughn JE, Storer BE, Armand P, Raimondi R, Gibson C, Rambaldi A, et al. Design and validation of an augmented hematopoietic cell transplantation-comorbidity index comprising pretransplant ferritin, albumin, and platelet count for prediction of outcomes after allogeneic transplantation. Biol Blood Marrow Transplant. 2015;21(8):1418–24.
Elsawy M, Storer BE, Milano F, Sandmaier BM, Delaney C, Salit RB, et al. Prognostic performance of the augmented hematopoietic cell transplantation-specific comorbidity/age index in recipients of allogeneic hematopoietic stem cell transplantation from alternative graft sources. Biol Blood Marrow Transplant. 2019;25(5):1045–52.
Sorror ML, Sandmaier BM, Storer BE, Maris MB, Baron F, Maloney DG, et al. Comorbidity and disease status based risk stratification of outcomes among patients with acute myeloid leukemia or myelodysplasia receiving allogeneic hematopoietic cell transplantation. J Clin Oncol. 2007;25(27):4246–54.
Sorror ML. How I assess comorbidities before hematopoietic cell transplantation. Blood. 2013;121(15):2854–63.
Kongtim P, Parmar S, Milton DR, Perez JMR, Rondon G, Chen J, et al. Impact of a novel prognostic model, hematopoietic cell transplant-composite risk (HCT-CR), on allogeneic transplant outcomes in patients with acute myeloid leukemia and myelodysplastic syndrome. Bone Marrow Transplant. 2018;24:S107.
Bejanyan N, Brunstein CG, Cao Q, Lazaryan A, Ustun C, Warlick ED, et al. Predictive value of disease risk comorbidity index for overall survival after allogeneic hematopoietic transplantation. Blood Adv. 2019;3(3):230–6.
Lin RJ, Hilden PD, Elko TA, Dahi PB, Shahrokni A, Jakubowski AA, et al. Burden and impact of multifactorial geriatric syndromes in allogeneic hematopoietic cell transplantation for older adults. Blood Adv. 2019;3(1):12–20.
Cornelissen JJ, Blaise D. Hematopoietic stem cell transplantation for patients with AML in first complete remission. Blood. 2016;127(1):62–70.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15(12):1628–33.
Blaise D, Maraninchi D, Archimbaud E, Reiffers J, Devergie A, Jouet JP, et al. Allogeneic bone marrow transplantation for acute myeloid leukemia in first remission: a randomized trial of a busulfan-Cytoxan versus Cytoxan-total body irradiation as preparative regimen: a report from the Group d’Etudes de la Greffe de Moelle Osseuse. Blood. 1992;79(10):2578–82.
Ringden O, Ruutu T, Remberger M, Nikoskelainen J, Volin L, Vindelov L, et al. A randomized trial comparing busulfan with total body irradiation as conditioning in allogeneic marrow transplant recipients with leukemia: a report from the Nordic Bone Marrow Transplantation Group. Blood. 1994;83(9):2723–30.
Copelan EA, Hamilton BK, Avalos B, Ahn KW, Bolwell BJ, Zhu X, et al. Better leukemia-free and overall survival in AML in first remission following cyclophosphamide in combination with busulfan compared with TBI. Blood. 2013;122(24):3863–70.
Nagler A, Rocha V, Labopin M, Unal A, Ben Othman T, Campos A, et al. Allogeneic hematopoietic stem-cell transplantation for acute myeloid leukemia in remission: comparison of intravenous busulfan plus cyclophosphamide (Cy) versus total-body irradiation plus Cy as conditioning regimen—a report from the acute leukemia working party of the European group for blood and marrow transplantation. J Clin Oncol. 2013;31(28):3549–56.
Mitsuhashi K, Kako S, Shigematsu A, Atsuta Y, Doki N, Fukuda T, et al. Comparison of cyclophosphamide combined with total body irradiation, oral busulfan, or intravenous busulfan for allogeneic hematopoietic cell transplantation in adults with acute lymphoblastic leukemia. Biol Blood Marrow Transplant. 2016;22(12):2194–200.
Nagler A, Labopin M, Gorin NC, Ferrara F, Sanz MA, Wu D, et al. Intravenous busulfan for autologous stem cell transplantation in adult patients with acute myeloid leukemia: a survey of 952 patients on behalf of the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Haematologica. 2014;99(8):1380–6.
Alatrash G, Kidwell KM, Thall PF, Di Stasi A, Chen J, Zope M, et al. Reduced intensity vs. myeloablative conditioning with fludarabine and PK-guided busulfan in allogeneic stem cell transplantation for patients with AML/MDS. Bone Marrow Transplant. 2018;54(8):1245–53.
Andersson BS, de Lima M, Thall PF, Wang X, Couriel D, Korbling M, et al. Once daily i.v. busulfan and fludarabine (i.v. Bu-Flu) compares favorably with i.v. busulfan and cyclophosphamide (i.v. BuCy2) as pretransplant conditioning therapy in AML/MDS. Biol Blood Marrow Transplant. 2008;14(6):672–84.
Chae YS, Sohn SK, Kim JG, Cho YY, Moon JH, Shin HJ, et al. New myeloablative conditioning regimen with fludarabine and busulfan for allogeneic stem cell transplantation: comparison with BuCy2. Bone Marrow Transplant. 2007;40(6):541–7.
Liu H, Zhai X, Song Z, Sun J, Xiao Y, Nie D, et al. Busulfan plus fludarabine as a myeloablative conditioning regimen compared with busulfan plus cyclophosphamide for acute myeloid leukemia in first complete remission undergoing allogeneic hematopoietic stem cell transplantation: a prospective and multicenter study. J Hematol Oncol. 2013;6:15.
Rambaldi A, Grassi A, Masciulli A, Boschini C, Mico MC, Busca A, et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015;16(15):1525–36.
Shimoni A, Labopin M, Savani B, Hamladji RM, Beelen D, Mufti G, et al. Intravenous busulfan compared with treosulfan-based conditioning for allogeneic stem cell transplantation in acute myeloid leukemia: a study on behalf of the Acute Leukemia Working Party of European Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2018;24(4):751–7.
Ringden O, Labopin M, Ehninger G, Niederwieser D, Olsson R, Basara N, et al. Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol. 2009;27(27):4570–7.
Scott BL, Pasquini MC, Logan BR, Wu J, Devine SM, Porter DL, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation for acute myeloid leukemia and myelodysplastic syndromes. J Clin Oncol. 2017;35(11):1154–61.
Bornhauser M, Kienast J, Trenschel R, Burchert A, Hegenbart U, Stadler M, et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 2012;13(10):1035–44.
Lioure B, Bene MC, Pigneux A, Huynh A, Chevallier P, Fegueux N, et al. Early matched sibling hematopoietic cell transplantation for adult AML in first remission using an age-adapted strategy: long-term results of a prospective GOELAMS study. Blood. 2012;119(12):2943–8.
Brands-Nijenhuis AV, Labopin M, Schouten HC, Volin L, Socie G, Cornelissen JJ, et al. Monosomal karyotype as an adverse prognostic factor in patients with acute myeloid leukemia treated with allogeneic hematopoietic stem-cell transplantation in first complete remission: a retrospective survey on behalf of the ALWP of the EBMT. Haematologica. 2016;101(2):248–55.
Ciurea SO, Labopin M, Socie G, Volin L, Passweg J, Chevallier P, et al. Relapse and survival after transplantation for complex karyotype acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation and the University of Texas MD Anderson Cancer Center. Cancer. 2018;124(10):2134–41.
Poire X, Labopin M, Cornelissen JJ, Volin L, Richard Espiga C, Veelken JH, et al. Outcome of conditioning intensity in acute myeloid leukemia with monosomal karyotype in patients over 45 year-old: a study from the acute leukemia working party (ALWP) of the European group of blood and marrow transplantation (EBMT). Am J Hematol. 2015;90(8):719–24.
Poire X, Labopin M, Maertens J, Yakoub-Agha I, Blaise D, Ifrah N, et al. Allogeneic stem cell transplantation in adult patients with acute myeloid leukaemia and 17p abnormalities in first complete remission: a study from the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT). J Hematol Oncol. 2017;10(1):20.
Solh MM, Solomon SR, Morris LE, Zhang X, Holland HK, Bashey A. The dilemma of conditioning intensity: when does myeloablative conditioning improve outcomes for allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2019;25(3):606–12.
Bohl S, von Harsdorf S, Mulaw M, Hofmann S, Babiak A, Maier CP, et al. Strong impact of extramedullary involvement in high-risk AML patients with active disease receiving the FLAMSA conditioning regimen for HSCT. Bone Marrow Transplant. 2016;51(7):994–6.
Heinicke T, Labopin M, Schmid C, Polge E, Socie G, Blaise D, et al. Reduced relapse incidence with FLAMSA-RIC compared with busulfan/fludarabine for acute myelogenous leukemia patients in first or second complete remission: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2018;24(11):2224–32.
Malard F, Labopin M, Stuhler G, Bittenbring J, Ganser A, Tischer J, et al. Sequential intensified conditioning regimen allogeneic hematopoietic stem cell transplantation in adult patients with intermediate- or high-risk acute myeloid leukemia in complete remission: a study from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2017;23(2):278–84.
Saraceni F, Labopin M, Brecht A, Kroger N, Eder M, Tischer J, et al. Fludarabine-treosulfan compared to thiotepa-busulfan-fludarabine or FLAMSA as conditioning regimen for patients with primary refractory or relapsed acute myeloid leukemia: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT). J Hematol Oncol. 2019;12(1):44.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23(24):5675–87.
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR, et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367(16):1487–96.
Holtick U, Albrecht M, Chemnitz JM, Theurich S, Skoetz N, Scheid C, et al. Bone marrow versus peripheral blood allogeneic haematopoietic stem cell transplantation for haematological malignancies in adults. Cochrane Database Syst Rev. 2014;(4):CD010189.
Ringden O, Labopin M, Bacigalupo A, Arcese W, Schaefer UW, Willemze R, et al. Transplantation of peripheral blood stem cells as compared with bone marrow from HLA-identical siblings in adult patients with acute myeloid leukemia and acute lymphoblastic leukemia. J Clin Oncol. 2002;20(24):4655–64.
Savani BN, Labopin M, Blaise D, Niederwieser D, Ciceri F, Ganser A, et al. Peripheral blood stem cell graft compared to bone marrow after reduced intensity conditioning regimens for acute leukemia: a report from the ALWP of the EBMT. Haematologica. 2016;101(2):256–62.
Ringden O, Labopin M, Ciceri F, Velardi A, Bacigalupo A, Arcese W, et al. Is there a stronger graft-versus-leukemia effect using HLA-haploidentical donors compared with HLA-identical siblings? Leukemia. 2016;30(2):447–55.
Ruggeri A, Labopin M, Bacigalupo A, Gulbas Z, Koc Y, Blaise D, et al. Bone marrow versus mobilized peripheral blood stem cells in haploidentical transplants using posttransplantation cyclophosphamide. Cancer. 2018;124(7):1428–37.
Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, et al. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103(8):1317–28.
Milano F, Gooley T, Wood B, Woolfrey A, Flowers ME, Doney K, et al. Cord-blood transplantation in patients with minimal residual disease. N Engl J Med. 2016;375(10):944–53.
Eckfeldt CE, Randall N, Shanley RM, Yohe S, Bejanyan N, Dolan M, et al. Umbilical cord blood transplantation is a suitable option for consolidation of acute myeloid leukemia with FLT3-ITD. Haematologica. 2016;101(8):e348–51.
Sandhu KS, Brunstein C, DeFor T, Bejanyan N, Arora M, Warlick E, et al. Umbilical cord blood transplantation outcomes in acute myelogenous leukemia/myelodysplastic syndrome patients aged >/=70 years. Biol Blood Marrow Transplant. 2016;22(2):390–3.
Warlick ED, Peffault de Latour R, Shanley R, Robin M, Bejanyan N, Xhaard A, et al. Allogeneic hematopoietic cell transplantation outcomes in acute myeloid leukemia: similar outcomes regardless of donor type. Biol Blood Marrow Transplant. 2015;21(2):357–63.
Weisdorf D, Eapen M, Ruggeri A, Zhang MJ, Zhong X, Brunstein C, et al. Alternative donor transplantation for older patients with acute myeloid leukemia in first complete remission: a center for international blood and marrow transplant research-eurocord analysis. Biol Blood Marrow Transplant. 2014;20(6):816–22.
Lee CJ, Savani BN, Mohty M, Labopin M, Ruggeri A, Schmid C, et al. Haploidentical hematopoietic cell transplantation for adult acute myeloid leukemia: a position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2017;102(11):1810–22.
Bacigalupo A, Lamparelli T, Bruzzi P, Guidi S, Alessandrino PE, di Bartolomeo P, et al. Antithymocyte globulin for graft-versus-host disease prophylaxis in transplants from unrelated donors: 2 randomized studies from Gruppo Italiano Trapianti Midollo Osseo (GITMO). Blood. 2001;98(10):2942–7.
Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR, et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol. 2009;10(9):855–64.
Kroger N, Solano C, Wolschke C, Bandini G, Patriarca F, Pini M, et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N Engl J Med. 2016;374(1):43–53.
Walker I, Panzarella T, Couban S, Couture F, Devins G, Elemary M, et al. Pretreatment with anti-thymocyte globulin versus no anti-thymocyte globulin in patients with haematological malignancies undergoing haemopoietic cell transplantation from unrelated donors: a randomised, controlled, open-label, phase 3, multicentre trial. Lancet Oncol. 2016;17(2):164–73.
Kanakry CG, Tsai HL, Bolanos-Meade J, Smith BD, Gojo I, Kanakry JA, et al. Single-agent GVHD prophylaxis with posttransplantation cyclophosphamide after myeloablative, HLA-matched BMT for AML, ALL, and MDS. Blood. 2014;124(25):3817–27.
Luznik L, Bolanos-Meade J, Zahurak M, Chen AR, Smith BD, Brodsky R, et al. High-dose cyclophosphamide as single-agent, short-course prophylaxis of graft-versus-host disease. Blood. 2010;115(16):3224–30.
Mielcarek M, Furlong T, O’Donnell PV, Storer BE, McCune JS, Storb R, et al. Posttransplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood. 2016;127(11):1502–8.
Rashidi A, Slade M, DiPersio JF, Westervelt P, Vij R, Romee R. Post-transplant high-dose cyclophosphamide after HLA-matched vs haploidentical hematopoietic cell transplantation for AML. Bone Marrow Transplant. 2016;51(12):1561–4.
Ruggeri A, Labopin M, Bacigalupo A, Afanasyev B, Cornelissen JJ, Elmaagacli A, et al. Post-transplant cyclophosphamide for graft-versus-host disease prophylaxis in HLA matched sibling or matched unrelated donor transplant for patients with acute leukemia, on behalf of ALWP-EBMT. J Hematol Oncol. 2018;11(1):40.
Locatelli F, Merli P, Pagliara D, Li Pira G, Falco M, Pende D, et al. Outcome of children with acute leukemia given HLA-haploidentical HSCT after alphabeta T-cell and B-cell depletion. Blood. 2017;130(5):677–85.
D’Souza A, Fretham C (2018) Current uses and outcomes of hematopoietic cell transplantation (HCT): CIBMTR summary slides. Available from: https://www.cibmtr.org
Boumber Y, Kantarjian H, Jorgensen J, Wen S, Faderl S, Castoro R, et al. A randomized study of decitabine versus conventional care for maintenance therapy in patients with acute myeloid leukemia in complete remission. Leukemia. 2012;26(11):2428–31.
Goodyear OC, Dennis M, Jilani NY, Loke J, Siddique S, Ryan G, et al. Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood. 2012;119(14):3361–9.
Choi J, Ritchey J, Prior JL, Holt M, Shannon WD, Deych E, et al. In vivo administration of hypomethylating agents mitigate graft-versus-host disease without sacrificing graft-versus-leukemia. Blood. 2010;116(1):129–39.
Craddock C, Jilani N, Siddique S, Yap C, Khan J, Nagra S, et al. Tolerability and clinical activity of post-transplantation azacitidine in patients allografted for acute myeloid leukemia treated on the RICAZA trial. Biol Blood Marrow Transplant. 2016;22(2):385–90.
de Lima M, Giralt S, Thall PF, de Padua SL, Jones RB, Komanduri K, et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer. 2010;116(23):5420–31.
de Lima M, Oran B, Champlin RE, Papadopoulos EB, Giralt SA, Scott BL, et al. CC-486 maintenance after stem cell transplantation in patients with acute myeloid leukemia or myelodysplastic syndromes. Biol Blood Marrow Transplant. 2018;24(10):2017–24.
Pusic I, Choi J, Fiala MA, Gao F, Holt M, Cashen AF, et al. Maintenance therapy with decitabine after allogeneic stem cell transplantation for acute myelogenous leukemia and myelodysplastic syndrome. Biol Blood Marrow Transplant. 2015;21(10):1761–9.
Brunner AM, Li S, Fathi AT, Wadleigh M, Ho VT, Collier K, et al. Haematopoietic cell transplantation with and without sorafenib maintenance for patients with FLT3-ITD acute myeloid leukaemia in first complete remission. Br J Haematol. 2016;175(3):496–504.
Xuan L, Wang Y, Huang F, Jiang E, Deng L, Wu B, et al. Effect of sorafenib on the outcomes of patients with FLT3-ITD acute myeloid leukemia undergoing allogeneic hematopoietic stem cell transplantation. Cancer. 2018;124(9):1954–63.
Burchert A, Bug G, Finke J, Stelljes M, Rollig C, Wäsch R, Bornhäuser M, Berg T, Lang F, Ehninger G, Serve H, Zeiser R, Wagner E, Kroeger N, Wolschke C, Schleuning M, Elmaagacli A, Götze K, Schmid C, Jost E, Wolf D, Böhm A, Thiede C, Haferlach T, Bethge W, Harnisch S, Wittenberg M, Rospleszcz S, Neubauer A, Brugger M, Strauch K, Schade-Brittinger C, Metzelder S (2018) Sorafenib as maintenance therapy post allogeneic stem cell transplantation for FLT3-ITD positive AML: results from the randomized, double-blind, placebo-controlled multicentre sormain trial. iN: ASH annual meeting, San Diego
Platzbecker U, Wermke M, Radke J, Oelschlaegel U, Seltmann F, Kiani A, et al. Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: results of the RELAZA trial. Leukemia. 2012;26(3):381–9.
Wang Y, Wu DP, Liu QF, Qin YZ, Wang JB, Xu LP, et al. In adults with t(8;21)AML, posttransplant RUNX1/RUNX1T1-based MRD monitoring, rather than c-KIT mutations, allows further risk stratification. Blood. 2014;124(12):1880–6.
Yan CH, Liu DH, Liu KY, Xu LP, Liu YR, Chen H, et al. Risk stratification-directed donor lymphocyte infusion could reduce relapse of standard-risk acute leukemia patients after allogeneic hematopoietic stem cell transplantation. Blood. 2012;119(14):3256–62.
Clark JR, Scott SD, Jack AL, Lee H, Mason J, Carter GI, et al. Monitoring of chimerism following allogeneic haematopoietic stem cell transplantation (HSCT): technical recommendations for the use of short tandem repeat (STR) based techniques, on behalf of the United Kingdom National External Quality Assessment Service for Leucocyte Immunophenotyping Chimerism Working Group. Br J Haematol. 2015;168(1):26–37.
Hoffmann JC, Stabla K, Burchert A, Volkmann T, Bornhauser M, Thiede C, et al. Monitoring of acute myeloid leukemia patients after allogeneic stem cell transplantation employing semi-automated CD34+ donor cell chimerism analysis. Ann Hematol. 2014;93(2):279–85.
Huisman C, de Weger RA, de Vries L, Tilanus MG, Verdonck LF. Chimerism analysis within 6 months of allogeneic stem cell transplantation predicts relapse in acute myeloid leukemia. Bone Marrow Transplant. 2007;39(5):285–91.
Lee HC, Saliba RM, Rondon G, Chen J, Charafeddine Y, Medeiros LJ, et al. Mixed T lymphocyte chimerism after allogeneic hematopoietic transplantation is predictive for relapse of acute myeloid leukemia and myelodysplastic syndromes. Biol Blood Marrow Transplant. 2015;21(11):1948–54.
Baron F, Maris MB, Sandmaier BM, Storer BE, Sorror M, Diaconescu R, et al. Graft-versus-tumor effects after allogeneic hematopoietic cell transplantation with nonmyeloablative conditioning. J Clin Oncol. 2005;23(9):1993–2003.
Wong E, Mason K, Collins J, Hockridge B, Boyd J, Gorelik A, et al. Prognostic limitations of donor T cell chimerism after myeloablative allogeneic stem cell transplantation for acute myeloid leukemia and myelodysplastic syndromes. Biol Blood Marrow Transplant. 2017;23(5):840–4.
Rettinger E, Willasch AM, Kreyenberg H, Borkhardt A, Holter W, Kremens B, et al. Preemptive immunotherapy in childhood acute myeloid leukemia for patients showing evidence of mixed chimerism after allogeneic stem cell transplantation. Blood. 2011;118(20):5681–8.
Shayegi N, Kramer M, Bornhauser M, Schaich M, Schetelig J, Platzbecker U, et al. The level of residual disease based on mutant NPM1 is an independent prognostic factor for relapse and survival in AML. Blood. 2013;122(1):83–92.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sanford, D., Elsawy, M., Kuchenbauer, F. (2021). The Role of Stem Cell Transplant in the Therapy of Acute Myeloid Leukemia (AML). In: Faderl, S.H., Kantarjian, H.M., Estey, E. (eds) Acute Leukemias. Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-53633-6_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-53633-6_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53632-9
Online ISBN: 978-3-030-53633-6
eBook Packages: MedicineMedicine (R0)