Abstract
The etiology of cognitive decline in Lewy body parkinsonism, including Parkinson disease (PD), is not only multifactorial but also heterogeneous and likely related to cumulative and interactive effects between changes in neurotransmitter functions, proteinopathies (α-synuclein, β-amyloid, tau), neuroinflammation, and -, vascular-, metabolic-, and other changes. Glucose metabolic studies have shown mixed subcortical and cortical changes in Parkinson disease with dementia (PDD). For example, incident dementia in idiopathic PD is heralded by decreased metabolism of visual association (Brodmann area 18) and posterior cingulate cortices with additional involvement of the caudate nucleus. Subsequent progression to dementia is associated with mixed subcortical, especially thalamic, and widespread cortical changes that involve the mesiofrontal lobes also. Neurotransmitter-specific PET imaging shows early and prominent nigrostriatal dopaminergic losses in PD, with no major differences between PD and PDD. Therefore, caudate nucleus, limbic, and mesofrontal dopaminergic denervations do not appear alone sufficient for development of PDD. Cholinergic imaging studies have shown relatively mild losses in PD without dementia but more prominent decreases in PDD. This suggests significant cholinergic pathology underlying progressive cognitive decline in PD. Average dopaminergic and cholinergic denervation does not appear to differ between PDD and dementia with Lewy bodies (DLB), supporting the view that PDD and DLB lie on a common disease spectrum. In vivo PET imaging studies show variable β-amyloid binding in PDD with prevalence of pathologic amyloid deposition higher in DLB compared to PDD. However, despite the relatively lower binding levels compared to Alzheimer disease (AD), β-amyloid deposition contributes to cognitive impairment early in the course of cognitive decline in PD, suggesting a lower symptomatic threshold for amyloid deposition compared to normal aging and AD.
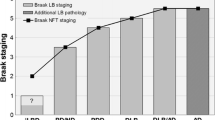
Emerging in vivo tau PET studies in Parkinsonian dementias show tau binding in cortical areas that have distinct distribution compared to AD. These preliminary tau imaging studies suggest a gradual increase of tau binding with appearance of absent/low binding in cognitively normal PD, low binding in cognitively impaired PD, intermediate binding in DLB, and highest binding in AD. Neuroinflammatory imaging studies shed new light on possible mechanistic factors underlying cognitive decline in Lewy body parkinsonism. Finally, medical comorbidities associated with systemic cardiovascular, metabolic, and inflammatory changes appear to contribute to the pathophysiological heterogeneity of the Lewy body dementias.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acetylcholine
- Alzheimer disease
- Amyloid
- Dementia with Lewy bodies
- Dopamine
- Neuroinflammation
- Parkinson disease
- Parkinson disease with dementia
- Positron emission tomography
- Tau
1 Introduction
PD patients are at increased risk of developing dementia. The prevalence estimates of dementia in PD range from 24% to 31% (Aarsland et al. 2005), with over 80% of patients developing dementia after a disease duration of 20 years (Hely et al. 2008). Cognitive impairment in PD probably reflects several processes, including degeneration of subcortical neurotransmitter (esp. cholinergic and dopaminergic) projection systems and proteinopathies (including α-synuclein Lewy body and β-amyloid plaque and neurofibrillary tangles) (Hirsch et al. 1987; Zweig et al. 1989; Gibb 1989; Mahler and Cummings 1990; Churchyard and Lees 1997; Jellinger 2000, 2006). Lewy body dementias are a diverse entity for which clinical criteria attempt to define subtypes (McKeith et al. 1996; Bohnen et al. 2017). One of these, dementia with Lewy bodies (DLB) is the second most frequent type of all dementias, associated with a clinical phenotype including neuropsychiatric disturbances (prominent visual hallucinations, depression) and variability in arousal and attention, antedating or shortly following the onset of extrapyramidal motor symptoms (McKeith et al. 2005). An arbitrary but generally accepted distinction has been made in current International Consensus diagnostic criteria between patients presenting with developing parkinsonism and dementia concurrently (DLB) versus those with developing parkinsonism more than 1 year prior to the onset of dementia (PDD) (McKeith et al. 1996, 2005, 2017; Emre 2003). There is, however, substantial debate whether these two clinically defined diagnostic entities should be kept separately or not (McKeith et al. 2017; Postuma et al. 2015). For example, the recent Movement Disorder Society clinical diagnostic criteria do not consider the presence of dementia as an exclusion for the diagnosis of PD (regardless of when motor parkinsonism occurs relative to cognitive or behavioral changes) (Postuma et al. 2015, 2018). For example, clinically defined DLB patients could be labeled as “PDD with Lewy bodies subtype” (Postuma et al. 2015). In contrast, the 1-year rule has been upheld in recently updated consensus diagnostic criteria for DLB (McKeith et al. 2017). REM sleep behavior disorder is now also a core clinical feature. Furthermore, imaging biomarkers (cardiac [I-123]metaiodobenzylguanidine, MIBG, sympathetic myocardial scintigraphy dopamine transporter, DAT, SPECT, [F-18]fluorodeoxyglucose (FDG) PET) are now used as “indicative” biomarkers. If one of these is positive, only one out of the four core clinical features is needed to make the probable DLB diagnosis (McKeith et al. 2017).
The term Parkinsonian dementia will be used in this chapter to reflect both PDD and DLB, together, unless specified separately. The chapter will first review global cerebral changes in Parkinsonian dementia based on findings in [F-18]fluorodeoxyglucose (FDG) PET studies followed by a discussion of dopaminergic and cholinergic neurotransmitter studies, a summary of the in vivo imaging literature on proteinopathies in PD, particularly, deposition of fibrillary β-amyloid and tau, and ends with a review of neuroinflammatory PET studies.
2 Glucose Metabolic Changes in Parkinsonian Dementia
In vivo FDG-PET is a minimally invasive diagnostic imaging procedure used to evaluate the pattern of cerebral glucose metabolism. Resting-state FDG-PET studies have shown similar metabolic reductions in Parkinsonian dementia to those recognized in Alzheimer disease (AD), affecting the posterior cingulate and precuneus cortex as well as the association neocortices, including the temporoparietal more than the prefrontal regions (Albin et al. 1996). There is relative preservation of the primary sensorimotor cortex, basal ganglia, thalamus, and cerebellum (Minoshima et al. 1994; Womack et al. 2011). In PDD, the primary visual cortex in the occipital lobe may be reduced, whereas it is relatively unaffected in AD (Vander Borght et al. 1997). Metabolic reductions generally follow a similar topographic pattern in PDD and DLB (Albin et al. 1996). Figure 16.1 show typical topographic metabolic differences between the major types of dementia.
FDG PET scan showing serial axial images and surface-rendered z-score maps of significant hypometabolism relative to a normal control database showing selective mesial occipital hypometabolism in a patient with DLB. Additional temporoparietal and mild frontal association cortical hypometabolism is typical both of DLB and of AD
The consistent observation of a metabolic reduction in the medial occipital cortex in Parkinsonian dementia suggests the use of functional brain imaging as a potential clinical diagnostic aid to differentiate DLB from AD (Minoshima et al. 2001). Minoshima et al. found that the presence of occipital hypometabolism distinguished DLB from AD with 90% sensitivity and 80% specificity in a study using a post-mortem diagnostic validation (Minoshima et al. 2001). The sensitivity in discriminating DLB and AD using FDG PET was greater than using clinical diagnostic criteria that were applied retrospectively to the data from medical chart review (Minoshima et al. 2001; Luis et al. 1999). Glucose metabolic preservation of the mid or posterior cingulate gyrus (so-called cingulate island sign) may help to distinguish DLB from AD (Lim et al. 2009; Imabayashi et al. 2016).
Longitudinal studies in initially non-demented PD subjects offer an opportunity to study the metabolic pattern of incident dementia. We previously reported the results of a prospective cohort study where we compared changes in regional cerebral glucose metabolism in PD patients with incident dementia after 2–6 years of follow-up compared to patients who remained non-demented (Bohnen et al. 2011). We found that incident dementia in idiopathic PD initially presented as a predominant hypometabolic pathology in the visual association cortex (Brodmann area 18) and the posterior cingulum and precuneus. Although hypometabolism of the cuneus and precuneus remained most prominent, progression of dementia was associated with mixed subcortical and widespread cortical changes that also involve the mesiofrontal lobes. The anterior cingulate cortex, which has distinct connections and behavioral attributes from the posterior cingulate, remained relatively spared. The PDD converter patients also demonstrated relative sparing of the primary sensorimotor cortex, a pattern similar to AD and DLB. Isolated occipital glucose hypometabolism is not specific for Parkinsonian dementia and can also be seen in non-demented PD patients (Bohnen et al. 1999). Recent longitudinal studies using FDG PET in PD consistently show hypometabolism in the posterior regions in early stage of cognitive normal PD that later converts from cognitively normal PD to PDD (Bohnen et al. 2011; Tard et al. 2015; Baba et al. 2017; Firbank et al. 2017).
Resting-state glucose metabolic imaging studies have been analyzed using voxel-based principal component analysis to characterize metabolic brain networks underlying cognitive dysfunction in PD (Huang et al. 2007). A specific factor, identified as the PD-related cognitive spatial covariance pattern (PDCP), is characterized by metabolic reductions in frontal and parietal association areas and relative increases in the cerebellar vermis and dentate nuclei. The PDCP can be quantitatively expressed as a numerical network score in individual subjects and will allow quantitative comparison of FDG PET scan findings over time to track progression of cognitive disease or response to treatment in PD (Mattis et al. 2016; Ko et al. 2017).
3 Dopaminergic PET Imaging in Parkinsonian Dementia
The basal ganglia and the neurotransmitter dopamine (DA) have been key targets for research exploring the pathophysiology underlying PD and its associated cognitive impairment. Several radiotracers have been employed previously to image nigrostriatal DA nerve terminals, including ligands metabolized by dopamine-synthetic enzymes such as [F-18]fluorodopa (FDOPA), synaptic vesicular monoamine transporter type 2 (VMAT2) ligands such as [C-11]dihydrotetrabenazine (DTBZ), and dopamine plasmalemmal DA reuptake transporter (DAT) ligands such as the cocaine analogue [C-11]WIN 35,428 (Garnett et al. 1978; Frey et al. 1996; Frost et al. 1993). The caudate nucleus has more prominent non-motor, cognitive, and affective connections, whereas the putamen plays a more direct role in motor functions (Alexander et al. 1986). Dopaminergic PET studies have shown prominent reductions of putaminal greater than caudate nucleus DA in PD (Fig. 16.2, top row) (Frey et al. 1996).
Example of [C-11]dihydrotetrabenazine vesicular monoamine transporter type 2 (DTBZ VMAT2), [C-11]Pittsburgh compound B β-amyloid (PiB), and [F-18]AV-1451 tau PET scans for three Parkinsonian dementia subjects (columns A, B, and C). All scans are at the same transaxial slice. The top row shows nigrostriatal dopaminergic denervation patterns typical of Parkinsonian dementia. The middle-row shows variable cortical β-amyloid deposition with no significant deposition in Subject A and higher levels of increased amyloid deposition in subjects B and C. The bottom-row shows elevated levels of tau deposition in the occipital temporal junction cortex in Subjects B and C, with no appreciable binding in subject A. None of the amyloid and tau PET are at binding levels that can be typically observed in Alzheimer disease
Dopaminergic mesolimbic and mesocortical pathways that innervate parts of the limbic system and the mesiofrontal neocortex (Bjorklund and Lindvall 1984) may affect cognitive functions in PD (Kovari et al. 2003; Williams-Gray et al. 2009). An FDOPA study found relative differences in FDOPA uptake in the anterior cingulum, ventral striatum and right caudate nucleus in PDD compared to non-demented PD patients using voxel-based analysis (Nagano-Saito et al. 2004; Holthoff et al. 1994; Ito et al. 2002). These data suggest that dementia in PD is associated with impaired mesolimbic and caudate dopaminergic function. However, a subsequent FDOPA study also found evidence of significant reductions in the caudate nuclei, anterior cingulate, and mesolimbic and mesofrontal cortices in non-demented PD patients compared to normal control subjects (Klein et al. 2010). Furthermore, these authors did not find significant differences in striatal or extra-striatal cortical FDOPA activity between non-demented PD versus Parkinsonian dementia patients (Klein et al. 2010). Although striatal and limbofrontal dopaminergic denervation is involved in specific cognitive functions in PD (Christopher et al. 2014), other FDOPA PET studies have also failed to find differences in striatal activity between PDD and non-demented PD patients (Hilker et al. 2005). Similar findings were reported in a [F-18]FP-CIT dopamine transporter PET study, where patients with PDD did not differ from non-demented PD patients in caudate nucleus or putaminal activity (Song et al. 2013). Furthermore, a longitudinal dopamine transporter [F-18]FP-CIT study found progressive decreases in striatal dopaminergic activity that correlated with changes in metabolic motor network and clinical motor scores but not with metabolic cognitive network changes in PD (Huang et al. 2007). Therefore, caudate nucleus, limbic, and mesofrontal dopaminergic denervations alone do not appear sufficient for the development of dementia in PD (Klein et al. 2010). With respect to PDD versus DLB, Klein et al. did not find significant differences in striatal, limbic, or mesofrontal FDOPA uptake between the two clinical subtypes of Parkinsonian dementia (Klein et al. 2010). Patients with DLB have comparable VMAT2 nigrostriatal losses compared to PD, but there is no evidence of significant nigrostriatal denervation in AD (Villemagne et al. 2011, 2012). Therefore, findings of occipital hypometabolism, or the cingulate island sign on FDG PET, or of presynaptic nigrostriatal DA deficits can be used to distinguish PDD and DLB from AD (Lim et al. 2009; Imabayashi et al. 2016; Villemagne et al. 2011; Koeppe et al. 2005; Hu et al. 2000; Burke et al. 2011).
4 Cholinergic PET Imaging in Parkinsonian Dementia
Parkinson disease is viewed traditionally as a motor syndrome secondary to nigrostriatal dopaminergic denervation. However, some motor and non-motor impairments may result from an intricate interplay of comorbid pathology and neurotransmitter deficiencies that extend beyond the loss of dopaminergic nigral neurons (Muller and Bohnen 2013). For example, cholinergic denervation can occur early in PD, and progressive cholinergic denervation has been consistently associated with the presence of dementia in this disorder (Hilker et al. 2005; Shimada et al. 2009; Shinotoh et al. 1999; Bohnen et al. 2003). Imaging results are consistent with post-mortem evidence that basal forebrain cholinergic system degeneration appears early in PD and worsens with the appearance of dementia (Ruberg et al. 1986; Roy et al. 2016). Impairment or degeneration of the cholinergic system plays a significant role in the progressive cognitive decline in PD (Perry et al. 1985).
There are two major sources of cholinergic projections in the brain. The nucleus basalis of Meynert/diagonal band of Broca/medial septum complex provides the principal cholinergic input to the entire cortical mantle and degenerates in PD (Mesulam and Geula 1988; Liu et al. 2015). The pedunculopontine nucleus, a brainstem locomotor center, provides cholinergic inputs to the basal ganglia, thalamus, cerebellum, several brainstem nuclei, and the spinal cord (Heckers et al. 1992) and also degenerates in PD (Lee et al. 2000). Acetylcholinesterase (AChE) PET imaging can assess cholinergic terminal integrity, with cortical activity reflecting basal forebrain projections and thalamic uptake reflecting pedunculopontine nucleus integrity.
Previous studies have found cognitive correlates of cortical cholinergic activity in PD (Shimada et al. 2009; Bohnen et al. 2006), whereas subcortical (pedunculopontine nucleus-thalamic) activity has been associated with a history of falls, sensory integration of postural control, and symptoms of REM sleep behavior disorder (Muller et al. 2013; Bohnen et al. 2009; Gilman et al. 2010; Kotagal et al. 2012).
We also found that low-range cholinergic activity in the thalamus, more robustly than the neocortex, was associated with symptoms of REM sleep behavior disorder (Kotagal et al. 2012). This finding provides a possible mechanism to explain to reported link between presence of REM sleep behavior disorder and risk of dementia in PD (Marion et al. 2008). In contrast to the degeneration of the basal forebrain complex in AD, the cholinergic innervation of the striatum (mainly originating from striatal interneurons) and of the thalamus (mainly originating from the brainstem) appears to remain relatively intact in AD (Mesulam 2004). The more selective cholinergic denervation of the cerebral cortex may explain the lower frequency of REM sleep behavior disorder in AD compared to Parkinsonian dementia (Gagnon et al. 2006). Cholinergic system degeneration may provide a conceptual framework to explain why PD patients with greater postural instability and gait disturbances are at an increased risk of developing dementia (Alves et al. 2006; Taylor et al. 2008). Our recent vesicular acetylcholine transporter [F-18]FEOBV-PET study confirmed subcortical reductions in DLB (Nejad-Davarani et al. 2019).
5 Multitracer PET Imaging Studies: Dopaminergic and Cholinergic Imaging Studies in PD and Parkinsonian Dementia
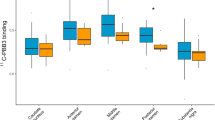
Several multitracer PET studies have been conducted to examine the combined effects of dopaminergic and cholinergic losses on clinical symptoms of Parkinsonian dementia. We reported findings of [C-11]dihydrotetrabenazine VMAT2 and AChE [C-11]PMP-PET studies in 101 patients with PD without dementia (Bohnen et al. 2012). We found that patients with lower cortical AChE activity had significantly reduced cognitive performance scores for verbal learning, executive, and attention functions compared to patients with preserved cortical cholinergic activity. Analysis of covariance showed that global cognitive functions scores had independent regression with both cortical AChE activity and nigrostriatal VMAT2 binding. We did not find evidence either of exclusive cholinergic or dopaminergic substrates for specific cognitive domains to identify neurotransmitter-specific cognitive circuits. Although dopamine modulates corticostriatal circuits and performance on executive tasks such as working memory (Goldman-Rakic 1998) and attentional control (Williams-Gray et al. 2008), we found evidence of independent cholinergic and dopaminergic effects underlying these functions in PD. These findings indicate that multiple neurotransmitter deficits likely contribute in parallel to cognitive impairment in PD (Kehagia et al. 2010). Moreover, we also found evidence of an interactive effect (so-called “compensatory” hypothesis) between nigrostriatal and cholinergic changes in PD, where combined losses of these two neurotransmitter system result in more severe cognitive impairment, whereas cognition is relatively preserved in the setting of dopaminergic losses but preserved cholinergic integrity (Bohnen et al. 2015).
There are two studies that have directly compared FDOPA- and AChE-PET imaging studies in patients with PD and Parkinsonian dementia (Klein et al. 2010; Hilker et al. 2005). Hilker and colleagues performed MP4A AChE- and FDOPA-PET studies in 17 non-demented PD and 10 PDD patients (Hilker et al. 2005). Data were compared to 31 age-matched controls. Compared to normal controls, striatal FDOPA uptake was significantly decreased in PD and PDD; however, no differences in FDOPA uptake were observed between these two groups. Global cortical MP4A binding was severely reduced in PDD (29.7%, p < 0.001 versus controls), but only moderately decreased in PD (10.7%, p < 0.01 versus controls). The PDD group had lower cortical MP4A uptake rates than did patients with PD. In a subsequent study, this group of investigators also reported on FDOPA-, MP4A-, and FDG-PET findings in eight PDD, six DLB, and nine non-demented PD and age-matched control subjects (Klein et al. 2010). They reported reduced FDOPA uptake in the striatum and in limbic and associative prefrontal areas in all Parkinsonian patient groups. Patients with PDD and patients with DLB showed severe MP4A and FDG reductions in the neocortex with a gradient of worsening deficits from frontal to occipital regions. Significant differences between PDD and DLB were not found with any of the radioligands used. Patients with PD without dementia had mild cholinergic deficits and no significant FDG reductions versus controls. The authors concluded that patients with PDD and DLB share the same dopaminergic and cholinergic deficit profile, and that cholinergic deficits seem to be crucial for the development of Parkinsonian dementia.
We previously performed a triple ligand PET analysis in PD patients who were recruited based on risk factors for PDD and showed evidence of independent cognitive contributions of not only individual neurotransmitter changes (dopamine, acetylcholine) but also β-amyloidopathy (Shah et al. 2016). These data indicate that proteinopathy and neurotransmitter changes may make incremental and possibly interactive contributions to cognitive impairment in PD at risk of dementia. It is plausible that heterogeneous combinations of neurotransmitter and proteinopathy changes may define endophenotypes within the cognitive dementia syndrome of PDD (Modreanu et al. 2017).
6 Fibrillary β-Amyloid PET Imaging in Parkinsonian Dementia
Neurodegenerative disorders are characterized by progressive dysfunction of specific populations of neurons. Neuronal loss is often associated with extra- and intracellular accumulations of misfolded proteins, typical of many neurodegenerative proteinopathies (Jellinger 2012). For example, extracellular fibrillary amyloid deposits characterize AD, and intracellular inclusions, such as Lewy bodies, containing α-synuclein, are characteristic of PD (Irvine et al. 2008). Although Parkinsonian dementia by definition is characterized by the presence of intraneuronal Lewy inclusion bodies, β-amyloid deposition can also be associated with Parkinsonian dementia, albeit to varying degree (Compta et al. 2011). The relative contributions of cortical and subcortical Aβ-amyloid deposition to cerebral dysfunction are unclear, and there are varying reports regarding the extent of β-amyloid depositions in PD versus PDD. Previous β-amyloid PET imaging studies using the Pittsburgh compound B (PiB) ligand have generally shown higher fibrillary β-amyloid burden in DLB compared to PDD (Rowe et al. 2007; Maetzler et al. 2009; Edison et al. 2008; Gomperts et al. 2008). For example, Johansson et al. did not find evidence of abnormal PiB retention in early stage PD subjects (Johansson et al. 2008). Maetzler and colleagues found abnormal cortical PiB binding in two out of ten PDD subjects (Maetzler et al. 2008). Edison et al. found high global cortical amyloid burden in DLB, but not in PDD (Edison et al. 2008). In the PDD patients, 2 out of 12 patients had both elevated cortical and striatal PiB retention. However, increased striatal PiB activity was also seen in two out of ten PDD patients who had no abnormal cortical retention. Interestingly, a post-mortem study found greater frequency of striatal β-amyloid deposition in PDD compared to PD (Kalaitzakis et al. 2008) and may imply a role of intrinsic striatal pathology in PDD. Gomperts et al. compared cortical PiB retention in PD, PDD, DLB, AD, and control groups and found higher cortical amyloid burden in DLB, at levels comparable to AD. Amyloid deposition in the PDD group was low, comparable to the PD and NC groups (Gomperts et al. 2008). However, a study by Foster and colleagues found no major differences in the degree of cortical nor caudate nucleus PiB binding between groups of PD (without or with mild cognitive impairment), PDD, or DLB (Foster et al. 2010) with the majority of subjects in each group having low-level PIB binding.
These observations are consistent with a literature review on in vivo β-amyloid PET imaging findings in Lewy body disorder that PD patients both without and with mild cognitive impairment (MCI) have a lower incidence (average 6% and 11%, respectively) of AD-range β-amyloid deposition compared to elderly normal subjects (about 15% on average) and that PDD patients have a lower frequency of β-amyloid binding (average 27%, range 0–80%) compared to patients with DLB (mean of 57% with a range from 33% to 100%) (Frey and Petrou 2015). An [F-18]florbetaben β-amyloid PET study using visual assessment confirmed these observations of very low AD-range amyloidopathy in mild and non-demented PD (none out of 33) (Mashima et al. 2017). As is the case in AD, the degree of amyloidopathy may be a function of ApoE ε4 allele genotype status (Donaghy et al. 2015).
A post-mortem correlation study of in vivo amyloid imaging in three PDD subjects found that two subjects had abnormal cortical amyloid binding on PET imaging (Burack et al. 2010). At autopsy, all three patients had abundant cortical Lewy bodies but were classified as low-probability AD based on NIA-Reagan criteria. The two amyloid PET-positive individuals had abundant diffuse β-amyloid plaques but only sparse neuritic plaques and intermediate neurofibrillary tangle pathology. The amyloid PET-negative subject had rare diffuse plaques, no neuritic plaques, and low neurofibrillary tangle burden. These post-mortem correlates confirm that [11C]PiB-PET is specific for fibrillar β-amyloid molecular pathology but may detect levels of deposition below thresholds for the pathological diagnosis of comorbid AD (Burack et al. 2010). Figure 16.2 (middle row) shows a pattern of mildly increased cortical β-amyloid activity in Parkinsonian dementia patients.
Findings of generally higher (or more frequently elevated) global cortical amyloid burden in DLB than in PDD suggest that cortical fibrillary β-amyloid deposition is not a requisite for PDD (Petrou et al. 2015). However, it may differentially contribute to the temporal manifestations and/or nature of the neurobehavioral phenotype of Parkinsonian dementia. Whether a combination of amyloid and Lewy body pathology exacerbates the memory and other cognitive problems in DLB is unclear, but it is likely it accelerates the dementia process, whereas Lewy body pathology alone may lead to a slower dementing process in PDD (Ballard et al. 2006; Petrou et al. 2012).
There are several studies that have directly correlated β-amyloid burden and cognitive performance in PD and PDD. We performed [C-11]PIB PET imaging in 40 patients with PD at high risk for development of dementia (Petrou et al. 2012). Detailed neuropsychological testing and [C-11]DTBZ VMAT2 PET imaging were also performed. We found that elevated cerebral PiB binding to levels seen in patients with AD were infrequent (only 6 of 40 subjects; 15%). Significant correlation was noted between cortical PiB binding and global composite cognitive function (r = −0.55, p < 0.005). Principal component analysis identified a factor with significant component loadings on cognitive parameters and PiB binding, but without significant striatal VMAT2 binding or other PD feature loadings. Although average cortical PIB binding in PD was in the range below than those commonly used to classify PiB-PET scans as typical of AD, these apparent low binding values have significant correlation with cognitive function. However, a subsequent literature review concluded inconsistent correlations between cognitive functions and β-amyloid deposition, at least in non-longitudinal analyses (Donaghy et al. 2015). In contrast, longitudinal cognitive analyses have shown that baseline amyloidopathy in the precuneus at baseline was associated with more rapid progression to cognitive decline and Parkinsonian dementia (Gomperts et al. 2013, 2016a). Importantly, there may be a confounder in the literature where most in vivo β-amyloid PET imaging studies have focused on amyloid deposition in the cortex only. Neuropathological studies point to an important role for striatal amyloidopathy where striatal β-amyloid deposition is substantially greater in PDD compared to non-demented PD (Kalaitzakis et al. 2008, 2011; Halliday et al. 2011; Dugger et al. 2012). These post-mortem findings agree with our in vivo imaging observations showing that striatal amyloidopathy was present in about half of the patients who had abnormal cortical amyloid binding. We found significantly lower cognitive performance for combined cortical and striatal β-amyloid deposition compared to cortical-only binding (Shah et al. 2016). Subcortical amyloidopathy may be another modifying factor for the presence of cognitive decline in PD. More recently, we found that striatal, especially nucleus accumbens, and limbocortical amyloidopathy was a determinant of apathy ratings in PD (Zhou et al. 2020). These findings were independent from the degree of nigrostriatal denervation and clinical ratings of depression, anxiety, or cognitive impairment confirming our prior observations that even low levels of amyloidopathy in PD or PDD have significant cognitive and neurobehavioral consequences. The lower symptomatic threshold of amyloidopathy in Lewy body parkinsonism may reflect compounding effects of the co-existence of other neurodegenerations, such as α-synucleinopathy, monoaminergic, and cholinergic denervations, and underlie a decreased cognitive reserve capacity in PD.
7 Tau PET Imaging in Parkinsonian Dementia
In recent years several candidate radiotracers have been developed to assess in vivo the distribution pattern of tau neurofibrillary tangles pathology. This pathology is commonly seen in AD (Braak and Braak 1995). The most commonly used radiotracer is [F-18] AV-1451, which strongly correlates with post-mortem evidence of neurofibrillary tau tangles (Marquie et al. 2015; Smith et al. 2019). Several studies have performed tau PET imaging in PD and Parkinsonian dementia (Table 16.1).
Hansen and colleagues have detected absent to low [18F] AV-1451 PET binding in PD subjects with or without mild cognitive impairment, but no binding among control subjects (Hansen et al. 2017). The investigators found no significant correlations between AV-1451 and cognitive dysfunction at this stage in the disease. In contrast, a [F-18]AV-1451 PET study in DLB patients found slightly higher AV-1451 binding in inferolateral temporal and parietal/precuneus in DLB compared to control subjects (Gomperts et al. 2016a). The increased tau binding in these regions correlated well with cognitive changes as measured by both the Mini-Mental State Examination (MMSE) and the Clinical Dementia Rating scale. In another AV-1451 PET study involving 18 AD subjects and 15 DLB patients, the AD subjects showed substantially higher AV-1451 uptake than the DLB group (Kantarci et al. 2017), with the former having the highest uptake in medial temporal and the DLB group having the lowest in this region. However, when compared to 90 healthy control subjects, the DLB patients showed higher AV-1451 uptake in the posterior temporoparietal and occipital cortex. However, there was no association between clinical measures (such as cognition, visual hallucination, motor Parkinsonism, and the presence of REM sleep behavior disorder) and AV-1451 retention in posterior temporoparietal and occipital regions (Kantarci et al. 2017). A subsequent larger AV-1451 PET imaging study from the same group compared 33 probable DLB patients, 18 posterior cortical atrophy (PCA) patients, and 100 control subjects (Nedelska et al. 2019). The DLB group showed overall moderate AV-1451 uptake in temporal, parietal, occipital, and frontal cortices compared to control subjects. These data also show that DLB patients have a different tau deposition pattern compared to prototypical AD.
Smith and colleagues evaluated AV-1451 retention in the substantia nigra and globus pallidus in 11 PD, 6 DLB, 18 PDD, and 44 control subjects and found significantly decreased binding in the substantia nigra in PDD compared to the other groups (PD, DLB, and controls) (Smith et al. 2019).
Interestingly, decreased uptake in the substantia nigra correlated with worse motor function in PD, PDD, and DLB. It should be noted that lower AV-1451 binding in the nigra reflects loss of neuromelanin, an off-target binding site for this radioligand (Hansen et al. 2016). Increased parietal tau binding was also associated with executive impairment in patients with synucleinopathies (Smith et al. 2018).
Lee and colleagues performed a multitracer PET study using AV-1451 tau and [F-18]florbetaben amyloid PET scans in 12 PD with normal cognition, 22 PD with cognitive impairment, 18 DLB, 25 AD patients, and 25 normal controls (Lee et al. 2018). These authors found that DLB subjects had higher level of binding of AV-1451 in the primary sensorimotor, visual cortices, and parietal-temporal cortices compared with the controls. Interestingly, when the analysis was limited to amyloid-positive DLB patients, AV-1451 binding in the same regions increased suggesting a possible interaction. Intriguingly, when compared to AD, amyloid-positive DLB patients had a higher level of binding in primary sensorimotor and visual cortices regions, and a lower in lateral and medial temporal cortices, parahippocampal cortices, and hippocampus (Lee et al. 2018). Notably, there was no increased level of binding in any regions among amyloid-negative DLB when comparing to the AD group. Unlike significant correlations between tau binding and cognition in the AD group, tau binding in the DLB patients did not correlate significantly with cognitive or motor measures. However, a strong correlation was observed between all cortical regions in AV-1451 PET binding and MMSE scores in the cognitively impaired PD group.
Studies have suggested that AV-1451 binding appears to gradually increase from cognitively normal PD (none to lowest), cognitively impaired PD (low), DLB (intermediate) to AD (highest) (Hall et al. 2017). High tau burden can mostly be observed in the occipital visual association cortices, suggesting an atypical profile of tau progression in Parkinsonian dementia that deviates from the classical Braak AD staging. Figure 16.2 (bottom row) show examples of tau PET imaging findings in patients with Parkinsonian dementia.
8 Neuroinflammation Imaging in Parkinsonian Dementia
Neuroinflammation is an important factor in the pathophysiology of dementia, including Parkinsonian dementia (Mrak and Griffin 2007). Biomarkers of mitochondrial translocator protein (TSPO) functions, like [C-11]PK11195 PET, can be used to assess microglial activation in vivo. For example, microglial activation was found to be present in the substantia nigra and putamen in both PD and DLB patients using this PET measure (Iannaccone et al. 2013). Interestingly, there was higher uptake in the caudate and a more extended microglial activation pattern in the cerebellum and several cortical regions in DLB patients compared to PD. This may suggest a possible disease propagation pattern (Iannaccone et al. 2013). In a study in patients with PDD, increased PK11195 PET binding was seen in the cingulum (anterior and posterior), basal ganglia, and the occipital, parietal, temporal, and frontal cortical regions (Edison et al. 2013). Furthermore, microglial activation was less extensive in PD compared to PDD. Interestingly, there was a significant correlation between microglial activation and cognitive changes suggesting inflammation-induced neuronal dysfunction in the PDD patients (Edison et al. 2013). Multi-tracer studies have found inconsistent relationships between glucose metabolic or amyloidopathy changes and the extent of microglial activation in PDD (Iannaccone et al. 2013; Edison et al. 2013; Fan et al. 2015; Femminella et al. 2016).
Interesting observations came from a single-subject clinical and multi-modal imaging study concerning tau ([F-18]AV-1451), β-amyloid ([C-1111]-PIB), and neuroinflammation ([C-11]-PK11195) in a probable DLB patient, which showed an AD-like pattern in [C-11]-PIB images, but not in the tau and neuroinflammation study (Mak et al. 2019). High tau binding in the primary visual cortex overlapped with high TSPO binding as observed in the [C-11]-PK11195 PET scan (Mak et al. 2019).
Although microglial activation may be a driving factor in the disease process in PDD, it is also clear that neuroinflammatory mechanisms are complex and remain poorly understood. For example, neuroinflammation could also be protective depending on the stage and condition of the dementing process (Stefaniak and O’Brien 2016). There is a clear need for longitudinal multi-modal imaging studies to help to disentangle the effects of inflammation across different stages of the disease and carefully relate these to clinical symptoms.
9 Discussion
Cognitive impairment in PD likely results from a combination of different pathologies in this pleomorphic neurodegeneration. Degeneration of subcortical systems, such as the dopaminergic nigrostriatal projection and the basal forebrain cholinergic corticopetal systems, plus neurodegeneration associated with cortical depositions of α-synuclein, intraneuronal hyperphosphorylated tau tangles, and β-amyloid are likely mutual contributors to cognitive impairment in PD (Kehagia et al. 2010; Compta et al. 2011). Glucose metabolic imaging studies have shown evidence of both posterior (parieto-occipital cortical) and anterior (frontal cortical and caudate nucleus) hypometabolism in PDD (Bohnen and Albin 2011). These regional changes may reflect distinct cognitive syndromes in PD with cognitive impairment. For example, Williams-Gray and colleagues reported that more posterior cortically-based cognitive defects evolved over time into dementia, whereas frontostriatal executive deficits were not associated with subsequent dementia risk per se (Williams-Gray et al. 2009). It is plausible that the glucose metabolic changes in the caudate nucleus and frontal cortex may in part be associated with dopaminergic denervation (Polito et al. 2012), whereas the more posterior cortical changes may in part be associated with cholinergic denervation or tau pathology (Klein et al. 2010; Williams-Gray et al. 2013). These data agree with dopaminergic PET studies showing that dopaminergic denervation of the caudate nucleus and fronto-limbic system alone is not sufficient for Parkinsonian dementia (Klein et al. 2010; Hilker et al. 2005). Cholinergic imaging studies agree with post-mortem evidence suggesting that primary basal forebrain cholinergic system degeneration significantly potentiates with the appearance of dementia. PET assessment of subcortical pedunculopontine nucleus-thalamic cholinergic denervation in PD has been associated with REM sleep behavior disorder (Kotagal et al. 2012). If basal forebrain cholinergic lesions develop in parallel, this may explain why RBD is a reported harbinger for the development of dementia in PD (Postuma et al. 2012). Furthermore, the association between a history of falls and subcortical cholinergic denervation in PD may in part provide additional insight into why PD patients with postural instability and gait disorders also appear at higher risk of developing dementia. The comorbid presence of two neurodegenerations (α-synuclein and β-amyloidopathy) in some patients with Parkinsonian dementia may suggest additive or even synergistic detrimental interactions of these proteinopathies (Tsigelny et al. 2008). This may explain findings that even low levels of cerebral amyloidopathy are significantly related to cognitive impairment in PD (Petrou et al. 2015, 2012). These data are further consistent with post-mortem findings that the presence of cortical amyloid pathology may be associated with a shorter time to development of PDD (Compta et al. 2011). Cerebrospinal fluid amyloid β42 levels also have independent prediction of future cognitive decline in non-demented PD patients, supporting a significant role of Alzheimer pathology in the development of Parkinsonian dementia (Siderowf et al. 2010).
Emerging evidence of tau PET studies suggest a gradient of tau binding in Parkinsonian dementia from lowest in cognitively normal PD to low in cognitively impaired PD (low) to highest in DLB. The presence of amyloidopathy or neuroinflammation may be a possible driving force for tau deposition, at least in primary sensorimotor and visual cortices in Parkinsonian dementia.
Further studies are needed to determine the differential contributions of heterogeneous patterns of not only neurotransmitter changes and proteinopathies, but also neuroinflammation, to the cognitive and neurobehavioral phenotypes of the Parkinson syndrome. It is possible that neuroinflammation may be related to peripheral inflammation, systemic comorbidities, such as cardiovascular disease and insulin insensitivity, and impaired sleep (Surendranathan et al. 2018; Bohnen et al. 2014; Bohnen and Hu 2019). Finally, availability of new ligands that are specific for α-synuclein protein aggregates will be important to allow longitudinal prodromal studies that may shed light on this sequence of critical pathophysiological events across the spectrum of Parkinsonian dementias.
Abbreviations
- AD:
-
Alzheimer disease
- DLB:
-
Dementia with Lewy bodies
- DTBZ:
-
Dihydrotetrabenazine
- FDG:
-
Fluorodeoxyglucose
- FDOPA:
-
6-Fluorodopa
- MP4A:
-
Methyl-4-piperidyl acetate
- PD:
-
Parkinson disease
- PDD:
-
Parkinson disease with dementia
- PET:
-
Positron Emission Tomography
- PMP:
-
Methyl-4-piperidinyl propionate
References
Aarsland D, Zaccai J, Brayne C (2005) A systematic review of prevalence studies of dementia in Parkinson’s disease. Mov Disord 20:1255–1263
Albin RL, Minoshima S, D’Amato CJ, Frey KA, Kuhl DE, Sima AAF (1996) Fluoro-deoxyglucose positron emission tomography in diffuse Lewy body disease. Neurology 47:462–466
Alexander GE, DeLong MR, Strick PL (1986) Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci 9:357–381
Alves G, Larsen JP, Emre M, Wentzel-Larsen T, Aarsland D (2006) Changes in motor subtype and risk for incident dementia in Parkinson’s disease. Mov Disord 21:1123–1130
Baba T, Hosokai Y, Nishio Y et al (2017) Longitudinal study of cognitive and cerebral metabolic changes in Parkinson’s disease. J Neurol Sci 372:288–293
Ballard C, Ziabreva I, Perry R et al (2006) Differences in neuropathologic characteristics across the Lewy body dementia spectrum. Neurology 67:1931–1934
Bjorklund A, Lindvall O (1984) Dopamine-containing systems in the CNS. In: Bjorklund A, Hokfelt T (eds) Handbook of chemical neuroanatomy. Elsevier, Amsterdam, pp 55–122
Bohnen NI, Albin RL (2011) White matter lesions in Parkinson disease. Nat Rev Neurol 7:229–236
Bohnen NI, Hu MTM (2019) Sleep disturbance as potential risk and progression factor for Parkinson’s disease. J Parkinsons Dis 9:603–614
Bohnen NI, Minoshima S, Giordani B, Frey KA, Kuhl DE (1999) Motor correlates of occipital glucose hypometabolism in Parkinson’s disease without dementia. Neurology 52:541–546
Bohnen NI, Kaufer DI, Ivanco LS et al (2003) Cortical cholinergic function is more severely affected in parkinsonian dementia than in Alzheimer disease: an in vivo positron emission tomographic study. Arch Neurol 60:1745–1748
Bohnen NI, Kaufer DI, Hendrickson R et al (2006) Cognitive correlates of cortical cholinergic denervation in Parkinson’s disease and parkinsonian dementia. J Neurol 253:242–247
Bohnen NI, Muller ML, Koeppe RA et al (2009) History of falls in Parkinson disease is associated with reduced cholinergic activity. Neurology 73:1670–1676
Bohnen NI, Koeppe RA, Minoshima S et al (2011) Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study. J Nucl Med 52:848–855
Bohnen NI, Muller MLTM, Kotagal V et al (2012) Heterogeneity of cholinergic denervation in Parkinson’s disease without dementia. J Cereb Blood Flow Metab 32:1609–1617
Bohnen NI, Kotagal V, Muller ML et al (2014) Diabetes mellitus is independently associated with more severe cognitive impairment in Parkinson disease. Parkinsonism Relat Disord 20:1394–1398
Bohnen NI, Albin RL, Muller ML et al (2015) Frequency of cholinergic and caudate nucleus dopaminergic deficits across the predemented cognitive spectrum of Parkinson disease and evidence of interaction effects. JAMA Neurol 72:194–200
Bohnen NI, Muller MLTM, Frey KA (2017) Molecular imaging and updated diagnostic criteria in Lewy body dementias. Curr Neurol Neurosci Rep 17:73
Braak H, Braak E (1995) Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol Aging 16:271–284
Burack MA, Hartlein J, Flores HP, Taylor-Reinwald L, Perlmutter JS, Cairns NJ (2010) In vivo amyloid imaging in autopsy-confirmed Parkinson disease with dementia. Neurology 74:77–84
Burke JF, Albin RL, Koeppe RA et al (2011) Assessment of mild dementia with amyloid and dopamine terminal positron emission tomography. Brain 134:1647–1657
Christopher L, Marras C, Duff-Canning S et al (2014) Combined insular and striatal dopamine dysfunction are associated with executive deficits in Parkinson’s disease with mild cognitive impairment. Brain 137:565–575
Churchyard A, Lees A (1997) The relationship between dementia and direct involvement of the hippocampus and amygdala in Parkinson’s disease. Neurology 49:1570–1576
Compta Y, Parkkinen L, O’Sullivan SS et al (2011) Lewy- and Alzheimer-type pathologies in Parkinson’s disease dementia: which is more important? Brain 134:1493–1505
Donaghy P, Thomas AJ, O’Brien JT (2015) Amyloid PET imaging in lewy body disorders. Am J Geriatr Psychiatry 23:23–37
Dugger BN, Serrano GE, Sue LI et al (2012) Presence of striatal amyloid plaques in Parkinson’s disease dementia predicts concomitant Alzheimer’s disease: usefulness for amyloid imaging. J Parkinsons Dis 2:57–65
Edison P, Rowe CC, Rinne JO et al (2008) Amyloid load in Parkinson’s disease dementia and Lewy body dementia measured with [11C]PIB positron emission tomography. J Neurol Neurosurg Psychiatry 79:1331–1338
Edison P, Ahmed I, Fan Z et al (2013) Microglia, amyloid, and glucose metabolism in Parkinson’s disease with and without dementia. Neuropsychopharmacology 38:938–949
Emre M (2003) Dementia associated with Parkinson’s disease. Lancet Neurol 2:229–237
Fan Z, Aman Y, Ahmed I et al (2015) Influence of microglial activation on neuronal function in Alzheimer’s and Parkinson’s disease dementia. Alzheimers Dement 11:608–621.e607
Femminella GD, Ninan S, Atkinson R, Fan Z, Brooks DJ, Edison P (2016) Does microglial activation influence hippocampal volume and neuronal function in Alzheimer’s disease and Parkinson’s disease dementia? J Alzheimers Dis 51:1275–1289
Firbank MJ, Yarnall AJ, Lawson RA et al (2017) Cerebral glucose metabolism and cognition in newly diagnosed Parkinson’s disease: ICICLE-PD study. J Neurol Neurosurg Psychiatry 88:310–316
Foster ER, Campbell MC, Burack MA et al (2010) Amyloid imaging of Lewy body-associated disorders. Mov Disord 25:2516–2523
Frey KA, Petrou M (2015) Imaging amyloidopathy in Parkinson disease and Parkinsonian dementia syndromes. Clin Transl Imaging 3:57–64
Frey KA, Koeppe RA, Kilbourn MR et al (1996) Presynaptic monoaminergic vesicles in Parkinson’s disease and normal aging. Ann Neurol 40:873–884
Frost JJ, Rosier AJ, Reich SG et al (1993) Positron emission tomographic imaging of the dopamine transporter with 11C-WIN 35,428 reveals marked declines in mild Parkinson’s disease. Ann Neurol 34:423–431
Gagnon JF, Postuma RB, Mazza S, Doyon J, Montplaisir J (2006) Rapid-eye-movement sleep behaviour disorder and neurodegenerative diseases. Lancet Neurol 5:424–432
Garnett ES, Firnau G, Chan PKH, Sood S, Belbeck LW (1978) [18F]fluoro-dopa, an analogue of dopa, and its use in direct measurement of storage, degeneration, and turnover of intracerebral dopamine. Proc Natl Acad Sci U S A 75:464–467
Gibb W (1989) Dementia and Parkinson’s disease. Br J Psychiatry 154:596–614
Gilman S, Koeppe RA, Nan B et al (2010) Cerebral cortical and subcortical cholinergic deficits in parkinsonian syndromes. Neurology 74:1416–1423
Goldman-Rakic PS (1998) The cortical dopamine system: role in memory and cognition. Adv Pharmacol 42:707–711
Gomperts SN, Rentz DM, Moran E et al (2008) Imaging amyloid deposition in Lewy body diseases. Neurology 71:903–910
Gomperts SN, Locascio JJ, Rentz D et al (2013) Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia. Neurology 80:85–91
Gomperts SN, Marquie M, Locascio JJ, Bayer S, Johnson KA, Growdon JH (2016a) PET radioligands reveal the basis of dementia in Parkinson’s disease and dementia with lewy bodies. Neurodegener Dis 16:118–124
Gomperts SN, Locascio JJ, Makaretz SJ et al (2016b) Tau positron emission tomographic imaging in the lewy body diseases. JAMA Neurol 73:1334–1341
Hall B, Mak E, Cervenka S, Aigbirhio FI, Rowe JB, O’Brien JT (2017) In vivo tau PET imaging in dementia: pathophysiology, radiotracer quantification, and a systematic review of clinical findings. Ageing Res Rev 36:50–63
Halliday GM, Song YJ, Harding AJ (2011) Striatal beta-amyloid in dementia with Lewy bodies but not Parkinson’s disease. J Neural Transm 118:713–719
Hansen AK, Knudsen K, Lillethorup TP et al (2016) In vivo imaging of neuromelanin in Parkinson’s disease using 18F-AV-1451 PET. Brain 139:2039–2049
Hansen AK, Damholdt MF, Fedorova TD et al (2017) In vivo cortical tau in Parkinson’s disease using 18F-AV-1451 positron emission tomography. Mov Disord 32:922–927
Heckers S, Geula C, Mesulam M (1992) Cholinergic innervation of the human thalamus: dual origin and differential nuclear distribution. J Comp Neurol 325:68–82
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG (2008) The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord 23:837–844
Hilker R, Thomas AV, Klein JC et al (2005) Dementia in Parkinson disease: functional imaging of cholinergic and dopaminergic pathways. Neurology 65:1716–1722
Hirsch EC, Graybiel AM, Duyckaerts C, Javoy-Agid F (1987) Neuronal loss in the pedunculopontine tegmental nucleus in Parkinson disease and in progressive supranuclear palsy. Proc Natl Acad Sci U S A 84:5976–5980
Holthoff VA, Vieregge P, Kessler J et al (1994) Discordant twins with Parkinson’s disease: positron emission tomography and early signs of impaired cognitive circuits. Ann Neurol 36:176–182
Hu XS, Okamura N, Arai H et al (2000) 18F-fluorodopa PET study of striatal dopamine uptake in the diagnosis of dementia with Lewy bodies. Neurology 55:1575–1577
Huang C, Tang C, Feigin A et al (2007) Changes in network activity with the progression of Parkinson’s disease. Brain 130:1834–1846
Iannaccone S, Cerami C, Alessio M et al (2013) In vivo microglia activation in very early dementia with Lewy bodies, comparison with Parkinson’s disease. Parkinsonism Relat Disord 19:47–52
Imabayashi E, Yokoyama K, Tsukamoto T et al (2016) The cingulate island sign within early Alzheimer’s disease-specific hypoperfusion volumes of interest is useful for differentiating Alzheimer’s disease from dementia with Lewy bodies. EJNMMI Res 6:67
Irvine GB, El-Agnaf OM, Shankar GM, Walsh DM (2008) Protein aggregation in the brain: the molecular basis for Alzheimer’s and Parkinson’s diseases. Mol Med 14:451–464
Ito K, Nagano-Saito A, Kato T et al (2002) Striatal and extrastriatal dysfunction in Parkinson’s disease with dementia: a 6-[18F]fluoro-L-dopa PET study. Brain 125:1358–1365
Jellinger KA (2000) Morphological substrates of mental dysfunction in Lewy body disease: an update. J Neural Transm 59(Suppl):185–212
Jellinger KA (2006) The morphological basis of mental dysfunction in Parkinson’s disease. J Neurol Sci 248:167–172
Jellinger KA (2012) Interaction between pathogenic proteins in neurodegenerative disorders. J Cell Mol Med 16:1166–1183
Johansson A, Savitcheva I, Forsberg A et al (2008) [(11)C]-PIB imaging in patients with Parkinson’s disease: preliminary results. Parkinsonism Relat Disord 14:345–347
Kalaitzakis ME, Graeber MB, Gentleman SM, Pearce RK (2008) Striatal beta-amyloid deposition in Parkinson disease with dementia. J Neuropathol Exp Neurol 67:155–161
Kalaitzakis ME, Walls AJ, Pearce RK, Gentleman SM (2011) Striatal Abeta peptide deposition mirrors dementia and differentiates DLB and PDD from other Parkinsonian syndromes. Neurobiol Dis 41:377–384
Kantarci K, Lowe VJ, Boeve BF et al (2017) AV-1451 tau and beta-amyloid positron emission tomography imaging in dementia with Lewy bodies. Ann Neurol 81:58–67
Kehagia AA, Barker RA, Robbins TW (2010) Neuropsychological and clinical heterogeneity of cognitive impairment and dementia in patients with Parkinson’s disease. Lancet Neurol 9:1200–1213
Klein JC, Eggers C, Kalbe E et al (2010) Neurotransmitter changes in dementia with Lewy bodies and Parkinson disease dementia in vivo. Neurology 74:885–892
Ko JH, Katako A, Aljuaid M et al (2017) Distinct brain metabolic patterns separately associated with cognition, motor function, and aging in Parkinson’s disease dementia. Neurobiol Aging 60:81–91
Koeppe RA, Gilman S, Joshi A et al (2005) 11C-DTBZ and 18F-FDG PET measures in differentiating dementias. J Nucl Med 46:936–944
Kotagal V, Albin RL, Muller MLTM et al (2012) Symptoms of rapid eye movement sleep behavior disorder are associated with cholinergic denervation in Parkinson disease. Ann Neurol 71:560–568
Kovari E, Gold G, Herrmann FR et al (2003) Lewy body densities in the entorhinal and anterior cingulate cortex predict cognitive deficits in Parkinson’s disease. Acta Neuropathol (Berl) 106:83–88
Lee MS, Rinne JO, Marsden CD (2000) The pedunculopontine nucleus: its role in the genesis of movement disorders. Yonsei Med J 41:167–184
Lee SH, Cho H, Choi JY et al (2018) Distinct patterns of amyloid-dependent tau accumulation in Lewy body diseases. Mov Disord 33:262–272
Lim SM, Katsifis A, Villemagne VL et al (2009) The 18F-FDG PET cingulate island sign and comparison to 123I-beta-CIT SPECT for diagnosis of dementia with Lewy bodies. J Nucl Med 50:1638–1645
Liu AK, Chang RC, Pearce RK, Gentleman SM (2015) Nucleus basalis of Meynert revisited: anatomy, history and differential involvement in Alzheimer’s and Parkinson’s disease. Acta Neuropathol 129:527–540
Luis CA, Barker WW, Gajaraj K et al (1999) Sensitivity and specificity of three clinical criteria for dementia with Lewy bodies in an autopsy-verified sample. Int J Geriatr Psychiatry 14:526–533
Maetzler W, Reimold M, Liepelt I et al (2008) [(11)C]PIB binding in Parkinson’s disease dementia. NeuroImage 39:1027–1033
Maetzler W, Liepelt I, Reimold M et al (2009) Cortical PIB binding in Lewy body disease is associated with Alzheimer-like characteristics. Neurobiol Dis 34:107–112
Mahler ME, Cummings JL (1990) Alzheimer disease and the dementia of Parkinson disease: comparative investigations. Alzheimer Dis Assoc Disord 4:133–149
Mak E, Surendranathan A, Nicastro N, Aigbirhio F, Rowe J, O’Brien J (2019) Imaging tau, neuroinflammation, and abeta in dementia with lewy bodies: a deep-phenotyping case report. Mov Disord Clin Pract 6:77–80
Marion MH, Qurashi M, Marshall G, Foster O (2008) Is REM sleep behaviour disorder (RBD) a risk factor of dementia in idiopathic Parkinson’s disease? J Neurol 255:192–196
Marquie M, Normandin MD, Vanderburg CR et al (2015) Validating novel tau positron emission tomography tracer [F-18]-AV-1451 (T807) on postmortem brain tissue. Ann Neurol 78:787–800
Mashima K, Ito D, Kameyama M et al (2017) Extremely low prevalence of amyloid positron emission tomography positivity in Parkinson’s disease without dementia. Eur Neurol 77:231–237
Mattis PJ, Niethammer M, Sako W et al (2016) Distinct brain networks underlie cognitive dysfunction in Parkinson and Alzheimer diseases. Neurology 87:1925–1933
McKeith IG, Galasko D, Kosaka K et al (1996) Consensus guideline for the clinical and pathological diagnosis of dementia with Lewy bodies (LBD): report of the Consortium on DLB International Workshop. Neurology 47:1113–1124
McKeith IG, Dickson DW, Lowe J et al (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 65:1863–1872
McKeith IG, Boeve BF, Dickson DW et al (2017) Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium. Neurology 89:88–100
Mesulam M (2004) The cholinergic lesion of Alzheimer’s disease: pivotal factor or side show? Learn Mem 11:43–49
Mesulam MM, Geula C (1988) Nucleus basalis (Ch4) and cortical cholinergic innervation in the human brain: observations based on the distribution of acetylcholinesterase and choline acetyltransferase. J Comp Neurol 275:216–240
Minoshima S, Foster NL, Kuhl DE (1994) Posterior cingulate cortex in Alzheimer’s disease. Lancet 344:895
Minoshima S, Foster NL, Sima AA, Frey KA, Albin RL, Kuhl DE (2001) Alzheimer’s disease versus dementia with Lewy bodies: cerebral metabolic distinction with autopsy confirmation. Ann Neurol 50:358–365
Modreanu R, Cerquera SC, Marti MJ et al (2017) Cross-sectional and longitudinal associations of motor fluctuations and non-motor predominance with cerebrospinal tau and Abeta as well as dementia-risk in Parkinson’s disease. J Neurol Sci 373:223–229
Mrak RE, Griffin WS (2007) Common inflammatory mechanisms in Lewy body disease and Alzheimer disease. J Neuropathol Exp Neurol 66:683–686
Muller ML, Bohnen NI (2013) Cholinergic dysfunction in Parkinson’s disease. Curr Neurol Neurosci Rep 13:377
Muller ML, Albin RL, Kotagal V et al (2013) Thalamic cholinergic innervation and postural sensory integration function in Parkinson’s disease. Brain 136:3282–3289
Nagano-Saito A, Kato T, Arahata Y et al (2004) Cognitive- and motor-related regions in Parkinson’s disease: FDOPA and FDG PET studies. NeuroImage 22:553–561
Nedelska Z, Josephs KA, Graff-Radford J et al (2019) (18) F-AV-1451 uptake differs between dementia with lewy bodies and posterior cortical atrophy. Mov Disord 34:344–352
Nejad-Davarani S, Koeppe RA, Albin RL, Frey KA, Muller M, Bohnen NI (2019) Quantification of brain cholinergic denervation in dementia with Lewy bodies using PET imaging with [(18)F]-FEOBV. Mol Psychiatry 24:322
Perry EK, Curtis M, Dick DJ et al (1985) Cholinergic correlates of cognitive impairment in Parkinson’s disease: comparisons with Alzheimer’s disease. J Neurol Neurosurg Psychiatry 48:413–421
Petrou M, Bohnen NI, Muller ML, Koeppe RA, Albin RL, Frey KA (2012) Abeta-amyloid deposition in patients with Parkinson disease at risk for development of dementia. Neurology 79:1161–1167
Petrou M, Dwamena BA, Foerster BR et al (2015) Amyloid deposition in Parkinson’s disease and cognitive impairment: a systematic review. Mov Disord 30:928
Polito C, Berti V, Ramat S et al (2012) Interaction of caudate dopamine depletion and brain metabolic changes with cognitive dysfunction in early Parkinson’s disease. Neurobiol Aging 33:206.e229–206.e239
Postuma RB, Bertrand JA, Montplaisir J et al (2012) Rapid eye movement sleep behavior disorder and risk of dementia in Parkinson’s disease: a prospective study. Mov Disord 27:720–726
Postuma RB, Berg D, Stern M et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Postuma RB, Poewe W, Litvan I et al (2018) Validation of the MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 33:1601–1608
Rowe CC, Ng S, Ackermann U et al (2007) Imaging beta-amyloid burden in aging and dementia. Neurology 68:1718–1725
Roy R, Niccolini F, Pagano G, Politis M (2016) Cholinergic imaging in dementia spectrum disorders. Eur J Nucl Med Mol Imaging 43:1376–1386
Ruberg M, Rieger F, Villageois A, Bonnet AM, Agid Y (1986) Acetylcholinesterase and butyrylcholinesterase in frontal cortex and cerebrospinal fluid of demented and non-demented patients with Parkinson’s disease. Brain Res 362:83–91
Shah N, Frey KA, Muller MLTM et al (2016) Striatal and cortical beta-amyloidopathy and cognition in Parkinson’s Disease. Mov Disord 31:111–117
Shimada H, Hirano S, Shinotoh H et al (2009) Mapping of brain acetylcholinesterase alterations in Lewy body disease by PET. Neurology 73:273–278
Shinotoh H, Namba H, Yamaguchi M et al (1999) Positron emission tomographic measurement of acetylcholinesterase activity reveals differential loss of ascending cholinergic systems in Parkinson’s disease and progressive supranuclear palsy. Ann Neurol 46:62–69
Siderowf A, Xie SX, Hurtig H et al (2010) CSF amyloid {beta} 1-42 predicts cognitive decline in Parkinson disease. Neurology 75:1055–1061
Smith R, Scholl M, Londos E, Ohlsson T, Hansson O (2018) (18)F-AV-1451 in Parkinson’s disease with and without dementia and in dementia with lewy bodies. Sci Rep 8:4717
Smith R, Wibom M, Pawlik D, Englund E, Hansson O (2019) Correlation of in vivo [18F]Flortaucipir with postmortem Alzheimer disease tau pathology. JAMA Neurol 76:310–317
Song IU, Kim YD, Cho HJ, Chung SW, Chung YA (2013) An FP-CIT PET comparison of the differences in dopaminergic neuronal loss between idiopathic Parkinson disease with dementia and without dementia. Alzheimer Dis Assoc Disord 27:51
Stefaniak J, O’Brien J (2016) Imaging of neuroinflammation in dementia: a review. J Neurol Neurosurg Psychiatry 87:21–28
Surendranathan A, Su L, Mak E et al (2018) Early microglial activation and peripheral inflammation in dementia with Lewy bodies. Brain 141:3415–3427
Tard C, Demailly F, Delval A et al (2015) Hypometabolism in posterior and temporal areas of the brain is associated with cognitive decline in Parkinson’s disease. J Parkinsons Dis 5:569–574
Taylor JP, Rowan EN, Lett D, O’Brien JT, McKeith IG, Burn DJ (2008) Poor attentional function predicts cognitive decline in patients with non-demented Parkinson’s disease independent of motor phenotype. J Neurol Neurosurg Psychiatry 79:1318–1323
Tsigelny IF, Crews L, Desplats P et al (2008) Mechanisms of hybrid oligomer formation in the pathogenesis of combined Alzheimer’s and Parkinson’s diseases. PLoS One 3:e3135
Vander Borght T, Minoshima S, Giordani B et al (1997) Cerebral metabolic differences in Parkinson’s and Alzheimer’s disease matched for dementia severity. J Nucl Med 38:797–802
Villemagne VL, Okamura N, Pejoska S et al (2011) In vivo assessment of vesicular monoamine transporter type 2 in dementia with lewy bodies and Alzheimer disease. Arch Neurol 68:905–912
Villemagne VL, Okamura N, Pejoska S et al (2012) Differential diagnosis in Alzheimer’s disease and dementia with lewy bodies via VMAT2 and amyloid imaging. Neurodegener Dis 10:161
Williams-Gray CH, Hampshire A, Barker RA, Owen AM (2008) Attentional control in Parkinson’s disease is dependent on COMT val 158 met genotype. Brain 131:397–408
Williams-Gray CH, Evans JR, Goris A et al (2009) The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain 132:2958–2969
Williams-Gray CH, Mason SL, Evans JR et al (2013) The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. J Neurol Neurosurg Psychiatry 84:1258–1264
Womack KB, Diaz-Arrastia R, Aizenstein HJ et al (2011) Temporoparietal hypometabolism in frontotemporal lobar degeneration and associated imaging diagnostic errors. Arch Neurol 68:329–337
Zhou Z, Muller M, Kanel P et al (2020) Apathy rating scores and beta-amyloidopathy in Parkinson disease patients at risk for cognitive decline. Neurology 94:e376
Zweig RM, Jankel WR, Hedreen JC, Mayeux R, Price DL (1989) The pedunculopontine nucleus in Parkinson’s disease. Ann Neurol 26:41–46
Acknowledgments
The authors gratefully acknowledge research support from the NIH, the Department of Veterans Affairs and the Michael J. Fox Foundation.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kanel, P., Müller, M.L.T.M., Bohnen, N.I. (2021). Parkinsonian Dementias: PET Findings. In: Dierckx, R.A.J.O., Otte, A., de Vries, E.F.J., van Waarde, A., Leenders, K.L. (eds) PET and SPECT in Neurology. Springer, Cham. https://doi.org/10.1007/978-3-030-53168-3_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-53168-3_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53167-6
Online ISBN: 978-3-030-53168-3
eBook Packages: MedicineMedicine (R0)