Abstract
Pterygium is characterized by encroachment of an abnormal fibrovascular tissue from the bulbar conjunctiva onto the cornea (Arch Ophthalmol 115:1235–1240, 1997). Upon reaching the corneal surface, this fibrovascular tissue exerts cicatricial traction that flattens the caruncle and obliterates the semilunar fold (Arch Ophthalmol 130:39–49, 2012). The indications for pterygium surgery include reduced vision due to obscuration of the optical center of cornea, irregular astigmatism, chronic irritation, recurrent inflammation, motility restriction, and cosmetic reasons. Numerous surgical techniques have been described, but the main concern of pterygium surgery is the unpredictable rate and timing of recurrence (Ocul Surf 12:112–119, 2014). After pterygium excision and thorough removal of the abnormal fibrovascular tissue, a gap is created between the recessed edge of the conjunctiva and underlying healthy Tenon (Arch Ophthalmol 130:39–49, 2012; Am J Ophthalmol 160:438–446, 2015). Such gap serves as the main avenue for pterygium recurrence. In this chapter, we summarize a novel surgical technique termed as “sealing the gap” combined with amniotic membrane transplantation to restore the caruncle morphology, create a mechanical barrier against the truncated fibrovascular tissue, and prevent recurrence without the use of mitomycin-C. The same procedure can be used for both primary and recurrent pterygium (Arch Ophthalmol 130:39–49, 2012).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Amniotic membrane
- Anti-inflammation
- Anti-scarring
- Anti-vascularization
- Caruncle
- Cryopreserved
- Fibrovascular tissue
- Gap
- Pterygium
- Recurrence
- Sealing
Indications
Symptomatic pterygium, reduced vision due to encroachment on the visual axis, irregular astigmatism, chronic irritation, recurrent inflammation, motility restriction, and cosmetic preference (Figs. 4.1 and 4.2)
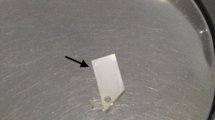
Surgical steps of pterygium by amniotic membrane transplantation. The surgery is performed under topical anesthesia (a), hemostasis, and akinesia achieved by traction sutures (b). For primary pterygium, blunt dissection is used to separate the head of the pterygium from the corneal surface (c). Complete symblepharon lysis by relaxing incisions at the borders to recess the pterygium head to a tension-free state so as to identify the white healthy Tenon’s capsule (asterisk) above (d, an example of recurrent pterygium) the bare sclera. The recessed pterygial head is lifted up by a forceps to illustrate the abnormal fibrovascular tissue (arrow) that is distributed under the overlying conjunctival epithelial tissue and adherent over the bare sclera (e). The abnormal fibrovascular tissue is grabbed and dissected off from the overlying conjunctival epithelial tissue tip of triangle by a sharp scissors (f), whereas the identified healthy Tenon was directly underneath in primary pterygium. Abnormal fibrovascular tissue is stretchable, and vascular (asterisk) adheres to the normal Tenon, which is identified as a non-stretchable and dense white fascia (star) when the conjunctiva is pulled up in primary (g) and recurrent (h) pterygium, respectively. The abnormal fibrovascular tissue (asterisk) is thoroughly removed and truncated (i, j for primary and recurrent, respectively). The residual sticky abnormal fibrovascular tissue is caught by a dry Weck-Cel when applied on the sclera (k, arrow) and subjacent to the conjunctival tissue (l, arrow). The gap is identified as the space between the edge of the healthy Tenon (m, white arrow) and the recessed conjunctival edge (m, red arrow). The gap is sealed with a 10-0 and 9-0 nylon running suture from the superior fornix across the caruncle to the inferior fornix in primary pterygium (n–p) and recurrent pterygium (q, r), respectively. Sealing the gap facilitates the bending and rounding of the recessed conjunctiva due to the natural retraction of the healthy Tenon to restore the normal caruncle configuration for both primary (s, star) and recurrent pterygium (t, star). For multi-recurrent pterygia eyes without sufficient residual conjunctiva in the caruncle, small conjunctival autograft (u) or oral mucosal graft (v) is attached to the sealed gap as the epithelial tissue for healing. Two layers of amniotic membrane are used to cover the exposed muscle (w) and the entire bare sclera (x), respectively, by fibrin glue
Representative surgical outcome. Preoperative (a, c) and postoperative (b, d) of representative patients with sealing the gap in primary (a, b) and recurrent (c, d) pterygium, respectively. For patients with insufficient residual conjunctiva in the caruncle, conjunctival autograft (e), or oral mucosal graft (f), is used to attach to the sealed gap to help provide the epithelial healing source. The caruncle morphology (b, d, f, and h) is restored after surgery, and motility restriction is also corrected (f, h)
Essential Steps
-
1.
Separation of pterygium head from cornea
-
2.
Relaxing incision to identify healthy Tenon
-
3.
Identification and separation of abnormal fibrovascular tissue from the recessed conjunctival epithelial tissue [1]
-
4.
Removal of abnormal fibrovascular tissue and trim off the pterygium head
-
5.
Fornix and caruncle reconstruction by sealing the gap with a 10-0 (primary) or 9-0 (recurrent) nylon running suture [1, 2]
-
6.
Amniotic membrane transplantation covering the rectus muscle (first layer) and the bare sclera (second layer) for ocular surface reconstruction [2]
Complications
-
Pyogenic granuloma
-
Symblepharon
-
Recurrent pterygium
Template Operative Dictation
Preoperative diagnosis
(Primary/Recurrent) pterygium (OD/OS)
(CPT code: 68115, 65870, 68326)
Procedure:
(1) Excision of pterygium, (2) fornix and caruncle reconstruction by sealing the gap, and (3) amniotic membrane transplantation, multiple layers (OD/OS)
Postoperative diagnosis:
Same
Indication:
This ____-year-old (male/female) had developed (decreased vision/ocular redness/severe photophobia/foreign body sensation/motility restriction) caused by progressive growth of the above problem over the past _____ (months/years) despite the conventional maximal medical therapies including ______. After a detailed review of alternatives, risks, and benefits, the patient elected to undergo the procedure.
Description of the procedure:
The patient was identified in the holding area, and the (right/left) eye was marked with a marking pen. The patient was brought into the OR on an eye stretcher in the supine position. A proper time-out was performed verifying correct patient, procedure, site, positioning, and special equipment prior to starting the case. After intravenous sedation, the (right/left) eye was prepped and draped in the usual sterile fashion.
The operating microscope was centered over the (right/left) eye, and an eyelid speculum was placed in the eye. 1:1000 epinephrine was instilled to create vasoconstriction for subsequent hemostasis control. Topical anesthesia was achieved by 2% Xylocaine gel instilled onto the ocular surface. A 7-0 Vicryl suture was placed in the superior and inferior limbal sclera taking episcleral bites as a traction suture by hanging down with a heavy locking needle holder. The eye was reflected temporally. The pterygium head was lifted off from the corneal surface using a blunt dissection technique to allow the tissue to recess. A relaxing incision was made along the pterygium border in both superior and inferior bulbar quadrants toward the fornix to reach the bare sclera so as to recess the pterygial head and body and conjunctival tissue to a tension-free position.
A 0.12 forceps was used to pick up the pterygial head, and the abnormal fibrovascular tissue under the overlying conjunctival epithelial tissue and adherent over the bare sclera was identified. Careful dissection of the abnormal fibrovascular tissue from the pterygium head and body along the overlying conjunctival epithelium was completed using sharp scissors. The abnormal fibrovascular tissue was removed by truncating both the superior and inferior fornix toward the nasal caruncle region. Residual abnormal fibrovascular tissue was detected by contact with a dry Weck-Cel due to its stickiness and was selectively removed from both the episcleral surface and the posterior subjacent healthy Tenon region. The abnormal fibrovascular tissue was further removed from the bare sclera, limbus, and cornea by brushing with a #64 Beaver blade and fine dissection with 0.12 forceps and/or a dental burr. The recessed pterygial head was then trimmed to allow sufficient tissue for the caruncle reconstruction. The gap sandwiched between the recessed conjunctival epithelial tissue and the underlying healthy Tenon’s capsule was identified by two 0.12 forceps; one grabbed the recessed conjunctival edge while the other grabbed the healthy Tenon.
For primary or single-recurrent pterygium with sufficient residual conjunctiva in the caruncle – This gap was sealed by a running (10-0 nylon (for primary) -or- 9-0 nylon (for recurrent)) from one corner of the fornix to the other, across the caruncle where the imaginary semilunar fold was recreated. Due to the posterior location and the natural traction of the normal Tenon’s capsule , the recessed conjunctiva was bent and rounded to restore the caruncle morphology after sealing the gap completely.
For multi-recurrent pterygium where there is no sufficient residual conjunctiva in the caruncle – (A small conjunctival autograft from fellow/operated eye -or- oral mucosal graft when both eyes do not have any healthy conjunctiva) was attached to the sealed gap in the caruncle area with a 8-0 Vicryl suture . They are then anchored to the side of muscle belly with two interrupted 10-0 nylon sutures to provide the healing epithelial source.
A single layer of cryopreserved amniotic membrane was used to cover the medial rectus muscle with the stromal surface facing down using fibrin glue. Another layer of amniotic membrane was used to cover the entire bare sclera with fibrin glue. Excessive fibrin glue and membrane were trimmed off from the borders, and the traction suture was removed.
After topical application of antibiotic (with or without steroid) ointment, the eye was patched, A, B and E, F are over the right eyes, C, D and G, H are over the left eyes, and the patient was transferred to the postanesthesia care unit in stable condition.
Additional Resource
References
Liu J, Fu Y, Xu Y, Tseng SC. New grading system to improve the surgical outcome of multirecurrent pterygia. Arch Ophthalmol. 2012;130(1):39–49.
Zhao D, Yin HY, Cheng A, Chen R, Sheha H, Tseng SC. Sealing of the gap between the conjunctiva and Tenon capsule to improve symblepharon surgery. Am J Ophthalmol. 2015;160(3):438–46.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cheng, A.M.S., Tseng, S.C.G. (2021). Sealing the Gap with Amniotic Membrane Transplantation for Primary and Recurrent Pterygium. In: Rosenberg, E.D., Nattis, A.S., Nattis, R.J. (eds) Operative Dictations in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-030-53058-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-53058-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53057-0
Online ISBN: 978-3-030-53058-7
eBook Packages: MedicineMedicine (R0)