Abstract
Purpose
Pterygium is a non-cancerous, fibrovascular growth of the bulbar conjunctiva that can cause visual disturbance, ocular pain, and cosmetic concerns. Surgical management is required in certain cases, which consists of excising the pterygium and associated Tenon’s, then overlaying the bare sclera with an autograft or amniotic membrane using glue or sutures. The purpose of this study is to assess outcomes of pterygium repair using a newly developed self-adhesive amniotic membrane that does not require glue or sutures for fixation.
Methods
Chart review of pterygium excision using a new self-adhesive amniotic membrane from a single surgical practice from 2012-2018. Descriptive statistics from 51 primary cases of pterygium excision were included.
Results
Pterygium recurrence occurred in 3 of the 51 self-adhesive amniotic membrane cases studied, resulting in a recurrence rate of 5.9%. Pterygium excision with the self-adhesive amniotic membrane had high rate of pyogenic granuloma formation of 27%. Self-adhesive amniotic membranes were found to perform comparably to more widely used techniques for pterygium excision, namely amniotic membranes and conjunctival autographs with glue or sutures. However, the self-adhesive grafts are associated with substantially more pyogenic granuloma formation.
Conclusion
Self-adhesive amniotic membranes offer comparable efficacy for preventing pterygium recurrence in comparison to other amniotic membranes and the conjunctival autograft. The incidence of pyogenic granuloma formation is higher in self-adhesive grafts compared to other widely used options.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pterygium is a non-cancerous, fibrovascular growth of the bulbar conjunctiva [1]. Pterygia are more common in individuals who spend significant time exposed to the sun [2, 3]. While small pterygia are essentially harmless, larger pterygia can grow towards the cornea, causing visual disturbances, discomfort, and cosmetic concerns [4]. In cases where treatment is needed, such as when the pterygium causes restriction of ocular mobility, irregular astigmatism, and/or obstruction of the visual axis, surgical excision of the pterygium may be performed [5]. This consists of removal of the pterygium and associated tenons, leaving behind bare sclera.
Conjunctival autograft and amniotic membrane transplantation have become more common in pterygium excision as the previous bare scleral technique was found to have a high recurrence rate of 88% [2, 6, 7] Both conjunctival autograft and amniotic membrane transplantation have been shown to significantly reduce the recurrence rate of pterygia after excision; however, it is still unclear whether one is definitively more effective than the other [8]. The advantages to using amniotic membranes over conjunctival autografts are less scarring, simplified surgery, and preservation of the conjunctiva for potential operations in the future [2, 9].
Amniotic membrane fixation involves the use of sutures or fibrin glue. Fibrin glue has increased in popularity due to its ease of use, resulting in shorter operating times, and less post-operative inflammation and discomfort for the patient as compared to sutures [10]. The downsides of using fibrin glue are the high cost and potential for infections [11]. Most of the literature on pterygium excision focuses on the use of amniotic membranes with either glue or sutures; however, there is little to no research on the efficacy of glue-less, suture-less amniotic membranes. A self-adhesive amniotic membrane should, in theory, provide all the benefits of an amniotic membrane without the “burden” of fibrin glue or sutures. The self-adhesive amniotic membrane would further simplify pterygium excision for the surgeon and make the procedure less invasive for the patient. This retrospective study aims to report outcomes of primary pterygium excision using a newly developed self-adhesive amniotic membrane and compare those to outcomes reported in the literature for glue or sutures, namely pterygia recurrence rates and post-operative complications.
Methods
The authors reviewed charts of patients who underwent pterygium excision using a self-adhesive membrane from 2012 to 2018. The self-adhesive membrane is manufactured by Biodlogics (Biodlogics LLC., Cordova, TN, USA). It is an amniotic extracellular matrix derived from placental amnionic membrane following delivery of a newborn. The operations were conducted by a single surgeon at a single operative centre. Descriptive statistics were used to analyse outcomes. Demographic information such as patient and surgical characteristics were presented. The primary outcome of the study was pterygium recurrence. Patients included in the study had a minimum of three months follow-up post-surgery. Complications such conjunctival inflammation, dry eye, dislodgement of membrane, diplopia, ocular hypertension, and pyogenic granuloma formation were analysed. GraphPad Prism 8 was used for creation of tables in this report.
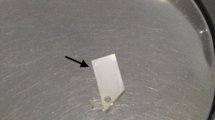
The technique for pterygium repair is as follows: 6–0 silk traction suture is used to immobilize and retract the eye. Lidocaine 1% is injected into the sub-conjunctival area surrounding the pterygium. Using Westcott scissors, a radial incision is made on each side of the body of the pterygium and then scleral dissection is carried from one incision to the other beneath the pterygium and immediately superficial to the sclera. The conjunctiva is then cut concentrically with the plica semilunaris approximately two millimetres lateral to the plica. The Tenon’s and pterygium tissue underlying the medial conjunctiva is excised along with the body of the pterygium. The head of the pterygium is avulsed, and the corneal surface is smoothed using a coarse diamond burr. Bleeding points are controlled with wet-field cautery. A 2 mm subconjunctival pocket is dissected along all incised conjunctival edges. The amniotic graft is then properly oriented and trimmed to match the excision site. The donor site is dried with a weck cell sponge. The graft is then positioned on the excision site stromal side down. The graft is then positioned and squeegeed with a curved round spatula to remove all underlying surface fluid. The edges of the graft are tucked under the free conjunctival edges. A 3-min waiting period ensues to assure adherence. The traction suture is removed. Ophthalmic combination antibiotic/steroid drops are applied.
Results
Fifty-one patients who underwent pterygiectomy using the self-adhesive amniotic membrane from 2012 to 2018 were included in the study. The median age of patients at repair was 56.1 years [IQR 17.2 years]. The median follow-up after surgical repair was 14.3 months [IQR 10.0 months]. Twenty-eight (56%) patients had a past ocular history prior to surgery. There were three patients (6.0%) with prior cataracts, twenty-two patients (44.0%) with dry eye, two patients (4.0%) with glaucoma, and one patient (2.0%) with a combination of ocular maladies. Thirteen patients (26.0%) received peri-operative treatment with artificial tears (n = 7), Combigan topical ointment (n = 2), Visine (n = 2) or combination of therapies (n = 2). Patient demographics and characteristics of pterygia are illustrated in Table 1.
There were no intra-operative or peri-operative complications. Pterygium recurrence occurred in 3 of the 51 self-adhesive amniotic membrane cases studied, resulting in a recurrence rate of 5.9%. One patient with pterygium recurrence required reoperation. Pterygium excision with the self-adhesive amniotic membrane was found to have a high rate of pyogenic granuloma formation with 14 patients (27.4%) developing pyogenic granulomas. These were treated with topical steroids and if recalcitrant they were excised. Median onset of pyogenic granuloma formation was 1.4 months [IQR 0.47 months].
Other post-operative complications include persistent inflammation and scar tissue found in two (3.9%) and one (2.0%) patient, respectively. All three patients with persistent inflammation and scar tissue were treated with topical steroids with complete resolution.
Discussion
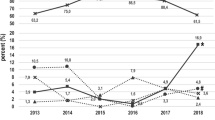
The literature on self-adhesive amniotic membranes for pterygium excision is sparse. To our knowledge, this is the first study assessing clinical outcomes using these membranes. Self-adhesive amniotic membranes were found to perform comparably, with respect to pterygium recurrence, to more widely used techniques for pterygium excision, namely amniotic membranes with glue or sutures and conjunctival autografts. The rates of recurrence reported in the literature for over 1000 cases of pterygium excision procedures performed with amniotic membranes using glue/sutures and conjunctival autografts are 8.9% and 7.7%, respectively [4].
Sekiyama et al. proposed and demonstrated the utility of an adhesive amniotic membrane for ocular surface reconstruction [12]. The membrane they described was a fibrin glue-coated, freeze-dried amniotic membrane (FCFD-AM). Although similar in concept to the self-adhesive membrane used in this study, the method of preparation and mechanism of adhesion are different.
The FCFD-AM as described by Sekiyama et al. was prepared via the following steps: the membrane was washed with a sterile phosphate buffered saline solution containing amphotericin, streptomycin, and penicillin, denuded of its epithelial layer by immersion in ethylene diamine tetraacetic acid (EDTA), coated with a small amount of fibrin glue, and then freeze-dried and gamma irradiated [12]. In contrast, the dehydrated, self-adhesive membrane utilized in this study is prepared in a markedly different process. The membrane is washed multiple times with a sterile saline solution. It is then sterilized, preserved, and dehydrated chemically by being placed in a high concentration (90–100%) ethanol solution. Lastly, it is further sterilized with electron beam (E-beam) irradiation.
Unlike the FCDF-AM, which uses fibrin glue for adhesion to the ocular surface, the mechanism of adhesion for the membrane used in this study is not well characterized as it is a proprietary mechanism not published in the literature. We hypothesize that the self-adhesive nature of the membrane is the result of both intrinsic molecular characteristics of amniotic tissue and the physical properties of the membrane itself, namely its very thin form after processing. The membrane is roughly 30–50 µm in thickness before dehydration and decreases to 10–20 µm once dehydrated. This extremely thin membrane is observed to naturally adhere to the ocular surface, theoretically through frictional and Vanderwaals forces, similar to how thin, plastic kitchen film adheres to surfaces or how certain insects can vertically climb smooth surfaces.
Despite their efficacy in preventing pterygium recurrence, the self-adhesive grafts are associated with substantially more pyogenic granuloma formation compared to the alternatives. Studies using conjunctival autografts and amniotic membranes with sutures have reported pyogenic granuloma rates of 1.4% and 1.25%, respectively, which is significantly lower compared to the 27.4% rate reported in this study [13, 14]. The exact reason for this high incidence of pyogenic granulomas is not known. We believe it is possibly due to having gaps in between the amniotic membrane and the patient’s conjunctiva. Since there is no suture or glue to create a strong closure, dehiscence and gap formation is likely later on, which can contribute to formation of pyogenic granuloma. It is also possible that the methods used to prepare and preserve the grafts could play a role in granuloma formation.
Currently, most amniotic membranes used for pterygium excision are cryopreserved [15]. By contrast, the self-adhesive amniotic membrane used in this study is a dehydrated membrane. Preservation methods have a significant effect on the structural and biochemical characteristics of amniotic membranes [16,17,18].
There are multiple methods to dehydrate membranes including freeze-drying, chemical dehydrating, and heating. Each type of dehydrating method appears to affect the characteristics of the membrane differently. For example, it was found that freeze-dried membranes were structurally and biochemically more similar to fresh amniotic membranes than cryopreserved ones [16]. However, the opposite was found when comparing cryopreserved membranes to membranes dehydrated with heat [18]. Chemically dehydrated membranes, such as the self-adhesive membrane, are not well studied, and their characteristics in comparison with fresh, cryopreserved, and other dehydrated membranes are not known.
The healing, anti-inflammatory, and regenerative properties of amniotic membranes come from their biological activity, which can be largely attributed to the heavy chain hyaluronic acid pentraxin (HC-HA/PTX3) complex [19]. The heavy chain component, HC-HA, was found to have many anti-inflammatory characteristics including antiangiogenic properties, making it crucial for the therapeutic efficacy of amniotic membranes [17]. Membranes dehydrated with heat were found to lack the HC-HA component potentially due to compaction of stromal and chorion layers [18]. Alteration of the biochemical and structural integrity of the amniotic membrane from its method of processing may explain why the incidence of pyogenic granulomas is higher for self-adhesive membranes. The self-adhesive membrane may have reduced levels of factors such as the HC-HA component, which would decrease antiangiogenic and anti-inflammatory properties, creating an environment conducive to pyogenic granuloma formation. Further testing is required to precisely characterize the biochemical activity of the self-adhesive membrane.
Alternatively, a contributing factor to the high incidence of pyogenic granulomas may be the composition of the patient population used in this study as 96.1% of patients analysed were Fitzpatrick 3 or greater. Despite the convenience and efficacy of the self-adhesive graft in preventing pterygium recurrence, the incidence of pyogenic granulomas is unacceptably high compared to other methods.
A limitation of this study is that it does not directly compare outcomes of the self-adhesive membrane with those of other grafts in patients from the same practice and instead uses the abundance of statistics for the other techniques in the literature for comparison. Future studies regarding the self-adhesive membrane should be conducted to analyse outcomes using a larger sample size with a more diverse population as well as directly comparing outcomes with the more commonly used grafts.
Additional studies should also be performed to see if the formation of pyogenic granulomas can be reduced in these self-adhesive grafts with the use of intra-operative adjuvant chemotherapeutics such as mitomycin C. Mitomycin C is an alkylating agent that acts non-specifically on the G1 and S phases of the cell cycle. Its inhibitory effects on inflammatory cell proliferation such as fibroblasts may be beneficial in preventing adverse outcomes following pterygium excision and graft placement [20]. Studies have shown that the use of mitomycin C significantly reduced the incidence of hyperemia and overall complication rate, including recurrence, following pterygium excision [21].
Conclusion
Self-adhesive amniotic membranes offer comparable efficacy for preventing pterygium recurrence in comparison with other amniotic membranes and the conjunctival autograft. The incidence of pyogenic granuloma formation is higher in self-adhesive grafts compared to other options.
References
Bondalapati S, Ambati B (2016) Minimally invasive pterygium surgery: sutureless excision with amniotic membrane and hydrogel sealant. Case Rep Ophthalmol 7(1):79–84. https://doi.org/10.1159/000444076
Kucukerdonmez C, Akova YA, Altinors DD (2007) Comparison of conjunctival autograft with amniotic membrane transplantation for pterygium surgery: surgical and cosmetic outcome. Cornea 26(4):407–413. https://doi.org/10.1097/ICO.0b013e318033b3d4
Prajna NV, Devi L, Seeniraj SK, Keenan JD (2016) Conjunctival autograft versus amniotic membrane transplantation after double pterygium excision: a randomized trial. Cornea 35(6):823–826. https://doi.org/10.1097/ico.0000000000000812
Clearfield E, Muthappan V, Wang X, Kuo IC (2016) Conjunctival autograft for pterygium. Cochrane Database Syst Rev 2:CD011349. https://doi.org/10.1002/14651858.CD011349.pub2
Noureddin GS, Yeung SN (2016) The use of dry amniotic membrane in pterygium surgery. Clin Ophthalmol 10:705–712. https://doi.org/10.2147/OPTH.S80102
Malla T, Jiang J, Hu K (2018) Clinical outcome of combined conjunctival autograft transplantation and amniotic membrane transplantation in pterygium surgery. Int J Ophthalmol 11(3):395–400. https://doi.org/10.18240/ijo.2018.03.08
Rosen R (2018) Amniotic membrane grafts to reduce pterygium recurrence. Cornea 37(2):189–193. https://doi.org/10.1097/ico.0000000000001407
Marsit N, Gafud N, Kafou I et al (2016) Safety and efficacy of human amniotic membrane in primary pterygium surgery. Cell Tissue Bank 17(3):407–412. https://doi.org/10.1007/s10561-016-9554-9
Tanaka TS, Demirci H (2016) Cryopreserved ultra-thick human amniotic membrane for conjunctival surface reconstruction after excision of conjunctival tumors. Cornea 35(4):445–450. https://doi.org/10.1097/ico.0000000000000737
Kheirkhah A, Casas V, Sheha H, Raju VK, Tseng SC (2008) Role of conjunctival inflammation in surgical outcome after amniotic membrane transplantation with or without fibrin glue for pterygium. Cornea 27(1):56–63. https://doi.org/10.1097/ICO.0b013e31815873da
Sharma A, Raj H, Gupta A, Raina AV (2015) sutureless and glue-free versus sutures for limbal conjunctival autografting in primary pterygium surgery: a prospective comparative study. J Clin Diagn Res 9(11):NC06-09. https://doi.org/10.7860/JCDR/2015/15689.6789
Sekiyama E, Nakamura T, Kurihara E et al (2007) Novel sutureless transplantation of bioadhesive-coated, freeze-dried amniotic membrane for ocular surface reconstruction. Invest Ophthalmol Vis Sci 48(4):1528–1534. https://doi.org/10.1167/iovs.06-1104
Zhang Z, Yang Z, Pan Q, Chen P, Guo L (2018) Clinicopathologic characteristics and the surgical outcome of conjunctival granulomas after pterygium surgery. Cornea 37(8):1008–1012. https://doi.org/10.1097/ico.0000000000001647
Ma DH, See LC, Liau SB, Tsai RJ (2000) Amniotic membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C treatment. Br J Ophthalmol 84(9):973–978. https://doi.org/10.1136/bjo.84.9.973
Toker E, Eraslan M (2016) Recurrence after primary pterygium excision: amniotic membrane transplantation with fibrin glue versus conjunctival autograft with fibrin glue. Curr Eye Res 41(1):1–8. https://doi.org/10.3109/02713683.2014.999947
Allen CL, Clare G, Stewart EA et al (2013) Augmented dried versus cryopreserved amniotic membrane as an ocular surface dressing. PLoS ONE 8(10):e78441. https://doi.org/10.1371/journal.pone.0078441
Tighe S, Mead OG, Lee A, Tseng SCG (2020) Basic science review of birth tissue uses in ophthalmology. Taiwan J Ophthalmol 10(1):3–12. https://doi.org/10.4103/tjo.tjo_4_20
Cooke M, Tan EK, Mandrycky C, He H, O'Connell J, Tseng SC 2014 Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/chorion tissue. J Wound Care 23(10):465–474, 476. https://doi.org/10.12968/jowc.2014.23.10.465.
Tseng SC (2016) HC-HA/PTX3 Purified From Amniotic Membrane as Novel Regenerative Matrix: Insight Into Relationship Between Inflammation and Regeneration. Invest Ophthalmol Vis Sci 57(5):ORSFh1-8. https://doi.org/10.1167/iovs.15-17637
Wolters JEJ, van Mechelen RJS, Al Majidi R et al (2021) History, presence, and future of mitomycin C in glaucoma filtration surgery. Curr Opin Ophthalmol 32(2):148–159. https://doi.org/10.1097/icu.0000000000000729
da Costa PC, Julio G, Campos P, Pujol P, Asaad M (2017) Effects of mitomycin C in early conjunctival inflammation after pterygium surgery. Curr Eye Res 42(5):696–700. https://doi.org/10.1080/02713683.2016.1236965
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kothari, E.A., Tenewitz, J.E., Jayman, J.R. et al. Pilot study of a glue-less, suture-less amniotic membrane for pterygium excision. Int Ophthalmol 42, 2933–2938 (2022). https://doi.org/10.1007/s10792-022-02281-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02281-x