Abstract
Nanomedicine has become a hot field of research, as it has the potential for developing several innovations in healthcare and, in particular, new pharmaceutical formulations. The need of innovative ways for drug transportation and delivery has accelerated the advances in the field of nanomaterials for pharmaceutical applications. The ultimate purpose of designing nanomaterials for drug delivery must be to ensure that the drug to be released exerts its pharmacological effect at the lowest possible dose, with the least number of side effects and equal benefits to a high dose. These so-called “nanopharmaceuticals” may possess distinctive features useful to improve the stability of the drugs, extend their systemic half-lives, enhance efficiency, increase bioavailability, and delay clearance. There is no doubt that nanopharmaceuticals are a promising strategy to overcome traditional pharmacokinetic limitations. Researchers around the world have been making important efforts to design and test novel nanoformulations, especially in in vitro and in vivo model studies. Virtually, all routes of drug administration have been investigated at this level. Compared to the high number of nanoformulations that are currently in the discovery and preclinical stages of the development pipeline, there are still very few nanopharmaceuticals in clinical trials and even less already in the market. This current scenario points to the need to accelerate nanomedicine endeavors in order to spur these formulations through the drug discovery pipeline.
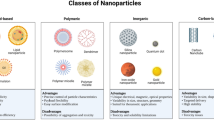
In this chapter, we will present some of the several opportunities for the design and use of nanomaterials (nanoliposomes, micelles, carbon nanostructures, dendrimers, polymeric, and inorganic nanoparticles) for pharmaceutical formulations. The experimental challenges, associated with moving from bench to bedside, will be addressed, as well as concerns about the precise control of drug release, their biodistribution or fate, and their toxicity, especially when they do not biodegrade. The need to validate and standardize protocols for early detection of toxicity, as well as an in depth understanding of the interaction among nanoparticles and tissues, organs, cells, and biomolecules, will be stated. Finally, the importance of developing a close interaction between scientists, regulators, institutions, and industry in order to help accelerate the efforts in the field will be indicated. The application of several innovative approaches to the design of new nanopharmaceuticals may allow achieving innovation and disruptive advances, providing safe, convenient, and cost-effective drug formulations to patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Nanomaterials
- Dendrimers
- Polymeric nanoparticles
- Inorganic nanoparticles
- Micelles
- Nanoliposomes
- Graphene
- Graphene oxide
- Carbon nanotubes
- Drug delivery
- Controlled release
- Theranostics
- Pharmaceutical formulation
- Nanotoxicity
9.1 Introduction
Nanomaterials have dimensional features in the range from 1 to 100 nm (1 nm = 1 × 10−9 m). Their sizes are smaller or comparable to those of common biologically relevant cells, bacteria, or virus or even of their molecular components such as proteins, nucleic acids, antibodies, and other important biomolecules. That characteristic may allow them to cross most physical or biological barriers (Fig. 9.1) or to generate different kinds of specific interactions. For example, once a nanomaterial comes in contact with a biological fluid, a nanoparticle-protein complex is formed (the process is known as “protein corona” formation). This complex will determine the fate of the nanomaterial, its systemic circulation, biodistribution, bioavailability, and even its toxicity. Nanomaterials, on the other hand, can be designed to be able to selectively recognize certain cell types or tissues by chemical modification of their surfaces. By selecting the type of nanomaterial and the specific chemical modification of their surfaces, different applications such as new tools for biomedical diagnosis or treatments, fortified foods, water pollution treatment, or advanced materials for textiles or construction can be achieved. In that way, the chemical and physical interactions of a nanomaterial can be finely tuned, selectively controlling how this affects their unique new properties and uses.
Nanotechnology exploits the physical properties of materials in the nanoscale. At that scale, optical, mechanical, magnetic, electronic, and chemical properties suffer drastic changes, making these properties highly attractive to be exploited in innovative technological applications (Halappanavar et al. 2018; Mostafalou et al. 2013). The great interest risen by use of nanomaterials in biomedical applications has originated a new multidisciplinary field called nanomedicine, where pharmaceutical nanotechnology is a very recent and attractive branch (Juillerat et al. 2015; Khan 2012; Chekman 2010). In terms of economic impact, it is expected that nanomedicine will grow in value by about 9% annually; it is a market with a value of nearly 112 billion dollars, as estimated in 2016, and it is predicted to reach nearly 261 billion dollars by 2023 (Grand View Research 2017). In particular, advanced drug delivery systems account for nearly 12 billion dollars (11% of the total), with half of that market consisting of systems for controlled release, liposomal drug delivery, gene therapy, and polymer-based systems, among others. The development of nanostructured materials for pharmaceutical applications (“nanopharmaceuticals”) such as controlled drug delivery and release carriers, agents for imaging and diagnosis, as well as innovative therapeutic vehicles, both as active pharmaceutical ingredients (API) and components of the pharmaceutical formulation, is currently a very active field of research (Beyer et al. 2016). Nanopharmaceuticals are a relatively recent class of therapeutic agents containing nanomaterials with unique physical and chemical properties because of their small size. They present new opportunities for the transport and stabilization of poorly soluble or unstable APIs (synthetic drugs, phytochemicals, proteins, nucleic acids, genes, etc.), as well as targeting them towards a specific site of the organism. However, the idea of nanopharmaceuticals must be handled carefully, as there is no consensus in the field. For the purposes of this chapter, a nanopharmaceutical will be considered as a complex system where an API is associated with an excipient (usually, the nanomaterial), as previously indicated. Due to their characteristics, these nanopharmaceuticals may be multifunctional, having better biological tissue distribution and becoming useful to mobilize drugs more easily through different biological barriers. They are interesting, versatile, and potent vehicles for the therapeutic treatment of different diseases (Mendez-Rojas et al. 2014; Sasaki and Akiyoshi 2010). Several of the actual challenges that current pharmaceutical formulations present may be overcome by the use of nanomaterials. So far, several advances and studies have been made with respect to the use of nanotechnology for the treatment and improvement of pharmaceutical formulations that may be useful against several diseases, rising very high expectations concerning positive results and benefits for society. Nanomaterials of different composition (organic, inorganic and composites) such as polymer-based, liposomes, quantum dots, iron oxide nanoparticles, or gold nanoparticles have been developed to provide fast and sensitive detection of disease-related molecular indicators.
We can safely consider that, in the near future, nanomaterials will be found more frequently in novel pharmaceutical formulations as they can bring solutions to the current challenges and limitations found in drug delivery and release systems, offering advantages and opportunities that will finally benefit both patients and the pharmaceutical industry. In order to reach a point where nanotechnology and all the applications mentioned above can be effective and applicable, joint efforts are needed between scientists, clinicians, the pharmaceutical industry, and legislative bodies to successfully implement the design and application of nanosystems in the treatment of several diseases that are currently challenging our health systems worldwide (Luque-Michel et al. 2017).
9.2 Current Approaches to Optimize Drug Deliverability
There are several important challenges in drug delivery and release in today’s pharmaceutical industry (Onoue et al. 2014; Chekman 2010). Nanotechnology offers a novel approach for solving these problems, advancing the industry from the model of high sales volume of popular, financially profitable drugs to a more “personalized medicine” model, where attention is given to the individual and not to a general, faceless, complex market. The pharmaceutical industry faces several challenges in order to develop new pharmaceutical formulations. Drug solubility in physiological conditions needs to be improved, while drug release has to be finely controlled. Biocompatibility and safety of the formulation has to be increased by avoiding drug clearance and increasing the plasmatic life of the drug in order to avoid the use of higher therapeutic doses. Drug transport to specific organs, tissues, or systems needs to become specific to avoid secondary effects, optimizing the drug pharmacokinetics and developing the co-delivery of multiple therapeutic drugs against different targets. Finally, real-time monitoring of drug delivery and distribution, as well as effective post-therapy assessment outcomes, to facilitate a faster development of improved APIs with minimal safety concerns has to be considered (Onoue et al. 2014; Chekman 2010).
Nanomaterials may help to solve most of these challenges since efficacy, safety, patient convenience, and compliance are demanding tasks that encourage to seek continuous optimization of drug delivery systems. Today there are very promising and highly complex high-tech APIs (e.g., biotech drugs), for which it would be very disappointing if deficiencies in their formulation and release systems would limit their bioavailability, their arrival at the target site, and their in vivo performance in general. Efficient dosage forms depend on a deep understanding of the pathways of the physiologic disposition of a drug since many physicochemical, biopharmaceutic, and pharmacokinetic factors can result in incomplete bioavailability and in the need of using a high amount of the drug thus incrementing costs and side effects.
A drug delivery system can be defined as a formulation or a device that enables the introduction of a pharmaceutical compound in the body and improves its efficacy and safety by controlling the rate, time, and place of its release (Bruschi 2015). Therefore, the route of administration is intimately related to the concept of drug delivery. Based on drug solubility and toxicity, drug delivery systems aim to prolong residence of a drug in biological fluids, to enhance solubility for improving its bioavailability and to ensure targeted action (Demina and Skatkov 2013).
The solubility of an API is relevant to select the right formulation approach and manufacturability and, as mentioned before, is one of the factors governing bioavailability. Thus, in 1995 the US Food and Drug Administration agency initiated the Biopharmaceutics Classification System (BCS) to support the waiving of bioequivalence studies of certain orally administered generic dosage products. The BCS classifies APIs in four classes according to their solubility in aqueous medium and their intestinal permeability properties (WHO 2016). BCS class I drugs (highly soluble, highly permeable) are readily eligible for biowaivers and class IV (poorly soluble, poorly permeable) are not. Class II drugs (poorly soluble, highly permeable) and class III drugs (highly soluble, poorly permeable) are eligible for biowaivers if they dissolve very rapidly either at pH values typical of the small intestine or under all physiological pH conditions, respectively (Chavda et al. 2010) (See Table 9.1).
The BCS can be usefully applied as a prognostic tool for designing or selecting drug delivery technologies (See Table 9.2). Drug release can be modulated using controlled release technology for class I drugs or increasing dissolution rate for class II drugs. Class III drugs technologies include manipulating the site or rate of exposure or incorporating functional agents into the dosage form to modify the metabolic activity of the enzyme systems. Class IV compounds are generally not suitable for oral drug delivery and are rarely developed to reach the market because of their erratic and poor absorption as well as their inter- and intra-subject variability (Chavda et al. 2010). Certainly, most of the class IV drugs are substrates for P-glycoprotein (resulting in low permeability) and substrates for cytochrome P450 3A4 (prompting to extensive pre-systemic metabolism) which further potentiates the problem of poor therapeutic potential of these drugs (Ghadi and Dand 2017).
The BCS is still evolving since there may be a risk of misclassification of some drugs because it is based on highest dose and on rigid definitions of solubility and permeability (Chavda et al. 2010). Moreover, Daousani and Macheras (2016) correlated the heterogeneous aspects of oral drug absorption with the biopharmaceutic classification of drugs. They found that for class I drugs no time dependency is expected for both absorption and non-absorption processes, while due to the biopharmaceutical properties of class II, III, and IV drugs, these drugs travel throughout the GI tract, and therefore, both absorption and non-absorption processes will exhibit time dependency. Therefore, the BCS is a very useful guiding tool primarily for the development of oral drug delivery formulations and technologies.
Recently, the Biopharmaceutics Drug Disposition Classification System (BDDCS) was proposed (Benet 2013). After classifying the drugs of 500 bioequivalence studies according to BCS and BDDCS, Cristofoletti et al. (2013) found that the final outcome of a bioequivalence study is strongly influenced by the solubility of the drug, but not by its intestinal permeability or extent of metabolism. Thus, solubility outweighs any effect of the extent of drug absorption and determines the need for particular drug delivery and release approaches.
As for therapeutic peptides and proteins, their biophysical stability, low bioavailability, and metabolic liability comprise the main challenges to overcome and succeed in oral formulation development and final bioperformance. Particularly, their oral bioavailability is limited by chemical and enzymatic degradation in the gastrointestinal tract, efflux pumps, first-pass gut, and hepatic metabolism, as well as their inability to cross the epithelial barrier of the gastrointestinal tract (Bak et al. 2015). Therapeutic peptides and proteins are usually classified as class III or class IV drugs by the BCS system (e.g., cyclosporine A, an immunosuppressant peptide, as a class IV compound), which means that low permeability is their main biopharmaceutical challenge together with the aforementioned limitations concerning oral drug product development. Considering that, excipients play a pivotal role in formulation development. Peptide stabilizers, pH modifiers, antioxidants, or metal chelators to minimize degradation, peptidase inhibitors, surfactants to better solubilize peptides, and biocompatible mucoadhesive polymers to promote peptide absorption are carefully chosen together with enteric coating approaches and appropriate packaging to preserve the integrity of the molecules and to overstep the oral delivery barriers (Bak et al. 2015).
In some cases, direct structural modifications of therapeutic peptides and proteins are needed. The example of success is represented by cyclosporine A, for which cyclization and therefore its decreased flexibility may confer to this drug a superior absorption after oral administration (Bruno et al. 2013). In addition, the covalent conjugation of polyethylene glycol to therapeutic peptides and proteins, called “pegylation,” improves drug delivery by increasing water solubility, enhancing stability, and half-life, reducing immunogenicity and limiting antigenic reactions (Milla et al. 2012). Moreover, the introduction on nonnatural amino acids as in the case of the Hybridtide® technology grants therapeutic peptides and proteins of proteolytic stability and dramatically enhanced half-life, facilitating oral delivery and overall improving pharmacokinetics (Horne et al. 2009). Protein lipidization, vitamin B12 conjugation, prodrug synthesis, and locking the conformation of therapeutic peptides and proteins by linking some residues to a synthetic hydrocarbon backbone are other effective strategies to improve stability and oral absorption (Bruno et al. 2013).
Likewise, carrier systems are rapidly evolving in very interesting ways to advance oral deliverability. Some interesting examples are the bilosomes, which are bile salt stabilized delivery nanovesicles that act as very stable penetration enhancers to promote oral bioavailability of large molecular weight proteins and peptides (Ahmad et al. 2017). Orally administered bilosome-based vaccine formulations (e.g., influenza, tetanus, and hepatitis B) represent a major step forward in vaccine technology by preventing antigen degradation and enhancing mucosal penetration (Chilkwar et al. 2015).
IgG antibodies as nanoscale proteins may also act as drug carriers in the so-called antibody-directed enzyme prodrug therapy and antibody-targeted drug conjugates, allowing for targeted drug delivery. Ibritumomab-tiuxetan-90Yttrium, a B-lymphocyte antigen CD20-directed radiotherapeutic IgG1k (mouse monoclonal aldolase C antibody) indicated for relapsed or refractory, low-grade or follicular B-cell non-Hodgkin lymphoma, is a leading example of this kind of systems (Tridente 2014).
Drug delivery has also been evolving to stimuli-responsive systems that improve bioavailability, reduce the cost of production, and increase patient compliance by allowing pH, temperature, light, ultrasound energy, magnetic or electric fields, swelling processes, or specific chemical agents or enzymes to regulate drug release (Halappanavar et al. 2018; Bajpai et al. 2010). Moreover, according to intended therapy, drug delivery and release is also classified in the following scenarios: rapid therapeutic onset (e.g., for drugs for acute pain or insomnia treatment), multiphasic or fixed-dose combination delivery (e.g., for antihistaminics or antimigraine drugs), delayed or chronotherapeutic onset (e.g., for oral antidiabetics, proton pump inhibitors, or antihypertensive drugs), and maintenance of target exposure (e.g., for some antibiotics or Alzheimer’s disease drugs) (Selen et al. 2014). This is known as therapy-driven drug delivery and is also extremely relevant to design and selection of excipients and drug delivery systems. Ultimately, linear, pulsed, or delayed release profiles enabled by the previously mentioned systems and others face always the challenge of being predictable and reproducible as well as allowing for minimum fluctuation in plasma drug levels.
The ultimate purpose of drug delivery strategies must be to ensure that the drug to be released exerts its pharmacological effect and, if possible, that it does so at the lowest possible dose and causing the least amount of adverse effects. Furthermore, patient compliance and treatment cost are also of the utmost importance because if the patient does not adhere to treatment or does not have access to it, all the research behind a medication will be wasted.
9.3 Routes of Administration for Nanopharmaceuticals
Along with the physical-chemical properties of a drug and the dosage form in which that drug is given, the route of administration plays an important role on the rate and extent of systemic drug absorption. Nanoformulations currently available for clinical use are typically administered orally or parenterally by the intravenous, subcutaneous, and intramuscular routes (Table 9.3). Some other administration routes have been meagerly explored by approved nanodrugs, either because of their complexity or because there are few active substances that, based on their pharmacodynamics and indication, require delivery to a very specific site of action. However, among the nanopharmaceuticals that are currently under investigation, many other administration routes are now being examined such as the transdermal, vaginal, pulmonary, and ophthalmic routes.
9.3.1 Oral Administration
The oral route is widely recognized as the most convenient, noninvasive, safe, conventional, cost-effective, and traditional way to administer drugs. However, it offers many disadvantages that nanocarrier-based formulations may help to solve. Targeted drug delivery is a big challenge when drugs are administered orally; this route usually requires formulating high amounts of the active substance increasing the production costs. As revised in the previous section, poor water solubility plays a crucial role when trying to improve the oral bioavailability of an API. The oral route is also challenging for APIs labile to gastrointestinal pH, bacteria, and enzymes.
To date, an important amount of knowledge has been gathered regarding the performance of different types of oral nanosystems for drug delivery. It has been reported that positively charged particles are absorbed more efficiently through the gastrointestinal tract as well as small nanoparticles (50–100 nm) which are absorbed in greater proportion than larger ones (500 nm) and distribute better to the kidneys, liver, spleen, lungs, and even brain. It is also known that particulate carrier systems administered orally could also undergo paracellular uptake from the digestive tract into blood circulation as well as the lymphatic system. On the other hand, it has been described that biodegradable (e.g., poly lactic acid) and lipid-based nanoparticles could suffer a significant degradation in gastric and intestinal fluids due to its surface composition (Hamidi et al. 2013). Much of this data has been applied to optimize oral drug delivery.
For example, by reducing the particle size to less than one micron using wet-milling techniques, the NanoCrystal® technology has overcome the solubility problem and allowed for various oral nanomedicines to be prepared and marketed, e.g., fenofibrate tablets (TRICOR®) and megestrol acetate oral suspension (MEGACE® ES) (Agarwal et al. 2018).
As far as lipid-based nanosystems are concerned, they are known to mimic food, improve gut solubilization and mucosal permeation, inhibit intestinal metabolism and/or P-glycoprotein efflux, and improve lymphatic uptake resulting in oral bioavailability augmentation (Borišev et al. 2018). A great challenge is represented by the hydrophilic low-permeability anticancer drug doxorubicin, which exhibits low oral bioavailability due to active efflux from intestinal P-glycoprotein. Thus, its oral administration remains a problem and no oral formulation for doxorubicin is marketed, till date (Ahmad et al. 2018). Attempts to tackle these obstacles were reported by Daeihamed et al. whose doxorubicin-loaded non-PEGylated, 120-nm-sized positively charged rigid liposomes attained a fourfold increase in oral bioavailability in a preclinical study (Daeihamed et al. 2017). Previously, another study in rats demonstrated a 384% enhancement in oral bioavailability compared to solution of a doxorubicin hydrochloride loaded lipid-based nanocarrier (LIPOMER) (Benival and Devarajan 2012).
9.3.2 Parenteral Administration (Intravenous, Intramuscular Subcutaneous)
Low bioavailability can be completely overcome by administering drugs intravenously and to some extent by using the intramuscular or the subcutaneous routes. Invasiveness, safety, and toxicity issues of injections together with pain and patient compliance concerns reduce as a whole the therapeutic value of parenterally administered drugs for long-term management of certain diseases. Yet, most nanopharmaceuticals already on the market are designed for parenteral administration.
Intravenous administration of nanoparticles allows for intracapillary passage followed by an efficient cellular uptake, also for macrophage endocytosis and for passive drug delivery to inflammatory sites with leaky vasculature (Gelperina et al. 2005). Thus, depending on the desired site of action and the nature of the nanoformulation, this route offers clear advantages.
The antimalarial drug artemisinin, for example, has no intravenous formulation available due to its poor aqueous solubility. Ibrahim et al. reported the preparation of a promising nanoformulation based on biodegradable albumin-bound artemisinin suitable for intravenous injection which enabled direct contact of artemisinin with infected erythrocytes. In in vitro experiments as well as in Plasmodium falciparum-infected “humanized” mice, the nanoparticles proved to be highly effective (Ibrahim et al. 2015).
In the case of solubility problems of drugs such as paclitaxel, an interesting approach to surpass this limiting factor was its binding with albumin, a natural carrier of endogenous and exogenous molecules. The high-solubility 130 nm albumin-bound particle form of paclitaxel contained in Abraxane® increased drug penetration into the tumor cells after intravenous administration. Unfortunately, P-glycoprotein mediated resistance affecting the antitumoral activity of paclitaxel could not be overcome by the nanoparticle formulation (Zhao et al. 2015).
Intramuscular injection offers the advantages of sustained release and long action; and compared to the intravenous route, it allows relative avoidance of the reticuloendothelial system (RES), the natural particle-removal system of the body (Hamidi et al. 2013). Increased bioavailability, bypassing the intestinal metabolism, and reduced toxic effects are some of the benefits of the intramuscular route that make it very popular. Moreover, intramuscular long-acting formulations provide great opportunities for chronic patients who benefit from once monthly administration or even less frequently by improving adherence, variability in drug exposure and treatment costs.
Recently, Zhou et al. improved the delivery, biodistribution, and viral clearance profiles of the antiretroviral drug cabotegravir by creating its myristoylated prodrug and formulating it into nanoparticles of stable size and shape. The particles exhibited enhanced monocyte-macrophage entry, retention, and RES depot behavior demonstrated in vitro as well as in animal models by means of viral restriction evaluations. The nanoformulated prodrug also showed the possibility of extended dosing intervals towards maximizing patient convenience (Zhou et al. 2018).
The subcutaneous route allows good absorption especially for drugs with a low oral bioavailability. Long-acting and targeted drug delivery are favorable outcomes from subcutaneous administration. Depending on size and composition, particles reach the circulation via the lymphatic system. Size plays also an important role when sustained release is the major objective since large nanoparticles persist longer at the injection site (Hamidi et al. 2013). The keratinous subcutaneous layer is the major barrier the nanoparticles encounter upon administration. It is a hydrophobic and rigid structure, which is difficult for particles to cross unless penetration enhancers (e.g., monoolein) are used to promote drug diffusion and solubility within this layer. Besides, the presence of an immunological barrier made of Langerhans and dendritic cells below the subcutaneous layer requires the use of nanocarrier coating (e.g., with polyethylene glycol) in order to prevent macrophage elimination (Bose et al. 2014). When the drug finally reaches the well-irrigated dermis layer of skin, it can diffuse into the systemic circulation.
An illustrative example of this administration route comes from the application of nanocarriers in traditional herbal medicine. Indeed, the nanonization of phytoceuticals seeks to advance phytotherapeutics by improving their pharmacokinetic and pharmacodynamic profile. Curcumin, a very promising natural anticancer agent, has very poor aqueous solubility and a very limited systemic bioavailability. Thus, Ranjan et al. formulated a prolonged subcutaneous delivery nanosystem that showed improved effectiveness on a non-small cell lung cancer xenograft model (Ranjan et al. 2016).
9.3.3 Transdermal Administration
Unlike topical formulations, transdermal medications are intended to exert clinical effects at distant or deeper tissue sites. Transdermal is a route of administration wherein active ingredients are delivered across the skin in order to reach the dermal layer by means of transcellular, intercellular, or hair follicles pathways for becoming available for systemic absorption via the dermal microcirculation.
The transdermal route requires sufficient lipophilicity of the active substance to be administered even when penetration enhancers or fasteners such as limonene may be added to the formulation to ease the permeation of drugs through the skin barrier. Transdermal delivery systems are useful to achieve controlled release of the drug over long periods while avoiding gastrointestinal effects or first-pass metabolism in the liver for certain drugs if they were administered orally. Moreover, they are noninvasive systems that have better patient compliance and can be easily removed by the patient when necessary (Gönüllü and Şaki 2017).
Skin penetration of large and hydrophilic drugs, or even macromolecules, is limited but nanocarriers have been successful crossing this barrier and even more so when the skin is disrupted, e.g., in diseases like psoriasis and atopic dermatitis. Regarding these two skin diseases in particular, in recent years several murine models have been used to develop and optimize transdermal nanocarrier formulations loaded with drugs like tretinoin, methotrexate, tacrolimus, cyclosporin A, and ketoprofen showing very promising results (Palmer and DeLouise 2016). Also, the treatment of psychiatric disorders can use nanosystems for transdermal administration; Iqbal et al. produced a solid lipid nanoparticle-based formulation for delivery of olanzapine whose favorable performance will allow its inclusion in and production of transdermal patches (Iqbal et al. 2017).
9.3.4 Pulmonary Administration
Pulmonary delivery implies a noninvasive route capable of granting a rapid onset of action of which most important advantages are its large absorptive surface area, its large absorptive mucosal membrane, and its high vascularity. To achieve a sustained therapeutic effect from the pulmonary route of administration, a nanodrug needs to avoid the pulmonary clearance processes mediated by the mucociliary apparatus and the alveolar macrophages. Enzyme degradation is also an obstacle, but metabolizing enzyme activities are limited compared to the gastrointestinal tract and liver. In cases of infections, the delivery systems should resist entrapment and inactivation of drugs by bacterial biofilms. Moreover, if the pharmacological action is meant to take place locally, sufficient lung-tissue retention needs to be guaranteed and systemic absorption minimized in order to avoid rapid elimination of the drug and undesirable systemic effects (El-Sherbiny et al. 2015; Lee et al. 2015).
Particle size, shape, and orientation allow for deposition at the targeted site in the respiratory system and influence avoidance of clearance mechanisms. By attaching or coating the drug with a stealth material, e.g., hyaluronic acid or polyethylene glycol, it is also possible to evade the pulmonary clearance features. Regarding the most promising type of nanosystems, the liposomal-based aerosol formulations have shown to prolong the retention half-life as well as solid lipid nanoparticles, polymeric micelles, and cyclodextrins (El-Sherbiny et al. 2015).
Due to their particle size, inhalable pharmaceutical forms using nanocarriers pose the risk of being exhaled during breathing. Thus, several strategies can help to solve this limitation: nebulization of nanocarriers as a colloidal suspension; mixing nanocarriers along with inert carriers, e.g., lactose and mannitol; or embedding the nanosized system into microparticles (Moreno-Sastre et al. 2015). One example is the suspension consisting of amikacin sulfate encapsulated in liposomes for inhalation (Arikayce™) which maximizes delivery to the lungs due to particle size as well as the antimicrobial efficacy, due to the ability to penetrate and diffuse through sputum into the bacterial biofilm. This formulation also decreases the potential for systemic toxicity. Presently it is undergoing clinical trials and FDA scrutiny (ClinicalTrials.gov 2018a). Also, in the final stretch for approval remains the cisplatin-based formulation named SLIT cisplatin. This formulation was planned for inhalation by patients with relapsed/progressive osteosarcoma metastatic to the lung. The acronym SLIT comes from “sustained release lipid inhalation targeting” and consists of aerosolized cisplatin loaded into lipid vesicles. The goal of this delivery system is to achieve drug accumulation in lungs while reducing exposure to other organs and thus the risk of hemotoxicity, nephrotoxicity, ototoxicity, and neurotoxicity (ClinicalTrials.gov 2018b; Lee et al. 2015).
Certainly, one major disadvantage of nanosystems is their potential toxicity. Most of the nanoparticles for drug delivery are usually made with well-tolerated materials, “generally recognized as safe” (GRAS), aimed to avoid toxic effects (Moreno-Sastre et al. 2015). Nevertheless, it has been reported that nanoparticles get absorbed from the olfactory mucosa into the central nervous system through the olfactory nerve, which can be considered a good approach to crossing the blood–brain barrier and delivering nanoparticles to the brain but at the same time this could act as a toxic outcome pathway (Hamidi et al. 2013).
9.3.5 Vaginal Administration
The vaginal route offers a high contact surface and a rich blood supply for drug absorption to obtain local (i.e., intravaginally delivery), uterine, or systemic effects (i.e., transvaginally delivery). The vagina is an effective drug administration route for local delivery of microbicide, contraceptive, and anticancer agents. When it comes to systemic active compounds, it represents a noninvasive route that allows for controlled transmucosal delivery. The vaginal route avoids the gastrointestinal environment and the hepatic first-pass metabolism, but the cervicovaginal mucus, the menstrual cycle, the vaginal pH, and its fluids (Leyva-Gómez et al. 2018) challenge the biodistribution and retention of a formulation. Thus, in order to extend their cervicovaginal residence time, nanosystems aimed to deliver drugs via vaginal mucosa must possess surface properties capable of interacting with O-glycosylated macromolecules, the main component of the mucus responsible for mucoadhesion. Polymer-based nanoparticles have the greatest potential for bioadhesion propensity and increased penetration capacity. For example, solid lipid nanoparticles based on polyoxyethylene (40) stearate containing the antifungal drugs ketoconazole and clotrimazole showed, under pH conditions simulating the pathologic environment, potential utility against vaginal infections caused by Candida albicans (Cassano et al. 2016). More recently, clotrimazole loaded into poly (d,l-lactide-co-glycolide) nanoparticles with chitosan-modified surface showed enhanced antifungal activity and mucoadhesive properties also for treating vaginal candidiasis (Martínez-Pérez et al. 2018).
9.3.6 Ophthalmic Administration
Nanoparticles have also shown great potential for ophthalmic formulations. The eyes have very poor retention of dosage forms and many anatomical and physiological barriers that cannot be penetrated easily. Low bioavailability, limited dose and volume capacity, and the presence of ocular tissue enzymes and efflux proteins are also concerns when designing ophthalmic products. Improving corneal residence time is one of the main objectives of pharmaceutical nanoformulations since tears, blinking and solution drainage result in loss of therapeutic drug levels on the pre-corneal surface. For treating some ocular diseases, intravitreal, subretinal, or subconjunctival injections could deliver adequate amounts of drug to the posterior segments of the eye, but this method causes pain and carries bleeding, toxicity, or infection risks. Thus, topical instillation remains a more convenient alternative (Tahara et al. 2017; Xu et al. 2013).
Liposomes are considered the ideal drug delivery systems because of their biocompatibility and their capacity of enclosing both hydrophilic and hydrophobic drugs. In addition, several studies have proved the efficacy of nanosuspensions for improving the bioavailability of corticosteroids such as dexamethasone and prednisone (Wang et al. 2016). Tahara et al. (2017) developed submicron-sized PLGA nanoparticles loaded with coumarin-6 as a model drug and marker and which surface was modified by chitosan, glycol chitosan, or polysorbate 80. The nanosystem improved the drug delivery efficiency to the retina after administration as topical eye drops to mice. Drug eluting contact lenses are also a good alternative for sustained delivery. A preclinical study with dogs showed that silicone hydrogel vitamin E-loaded contact lenses prolonged the release of the drug timolol and increased its bioavailability with only one-third of the loaded drug compared to eye drops (Xu et al. 2013). Lastly, a research group from the University Eye Hospital Tübingen (Germany) launched a nanocarrier system based on lipid-modified DNA strands that self-assemble into micelles with a hydrophobic core and a hydrophilic corona. The so-called “nano-I-drops” technology can be equipped with different drugs by hybridization with an aptamer. This DNA nanoparticles show excellent adherence to the corneal surface for extended periods reducing the need for frequent application and thereby minimizing side effects (Willem de Vries et al. 2018).
There is no doubt that nanopharmaceuticals are a promising strategy to overcome traditional pharmacokinetic limitations. Researchers around the world have been making countless efforts to design and test novel nanoformulations, especially in in vitro and in animal model studies. Virtually, all routes of drug administration have been investigated at this level. However, compared to the high number of nanoformulations that are currently in the discovery and preclinical stages of the development pipeline, there are still very few nanopharmaceuticals in clinical trials and even less already marketed.
9.4 Nanocarriers: Composition, Structure, and Properties of Selected Recent Systems
Pharmaceutical technology allows us to select among several materials for designing the most appropriate pharmaceutical form to prepare a medicine, according with their physical and chemical characteristics and use. Nanocarriers, nanosuspensions, and nanogels are considered as some of the most common systems for the formulation of potentially useful nanopharmaceuticals. Nanosuspensions and nanogels chemical and physical characteristics have been reviewed and discussed previously in the scientific literature (Dhanapal and Ratna 2012; Asadian-Birjand et al. 2012) and won’t be further discussed here. Nanocarriers, in the other hand, are colloidal systems with sizes in the range in between 10 and 100 nm; they have been widely used for diagnostics, treatment, and tracking of biomarkers. There are several types of nanocarriers, most of them designed to contain APIs encapsulated into their structures. Nanocarriers for controlled delivery are usually designed to avoid unintended exposure of the individual to the API, protecting simultaneously from being detected by the host’s immune and clearance system. Additionally, surface functionalization of nanocarriers is used to achieve delivery of the drug contents with great specificity (Halappanavar et al. 2018). Direct delivery of drugs into the site of action helps to reduce side effects. This approach is limited to skin, ocular, or mucosal pathologies using drops, creams, lotions, or emulsions. However, tissue or organ selectivity can be achieved with surface modified nanopharmaceuticals (Fig. 9.2).
Surface modification of nanocarriers for targeted drug delivery. (a) Traditional pharmaceuticals without surface modification. (b) Nanopharmaceuticals with surface modification. Diana cells can be targeted with the drug nanocarrier using ligand and receptor interactions like antibody-antigen interaction, allowing a specific drug release
During the last 5 years, more than 2000 papers were published containing the keywords “nanocarrier,” “drug delivery,” and “release.” The majority (90%) are devoted to micelles, nanoliposomes, niosomes, polymeric nanoparticles, and dendrimers, while the remaining 10% explore the use of single-walled carbon nanotubes (SWCNTs), multi-walled carbon nanotubes (MWCNTs), lipid-core nanoparticles, and inorganic nanoparticles. Tekade et al. (2016) presented the state-of-the-art on the interface of nanotechnology and combination chemotherapy, which has shown a remarkable promise in the therapy of resistant tumors. Anticancer drugs in combination with small interfering RNAs (siRNAs), such as VEGF, XLAP, PGP, MRP-1, BCL-2, and cMyc, are some examples that are mentioned in their article. The siRNAs have shown an immense promise of eliminating drug resistance genes, as well as recovering the sensitivity of tumors resistant to cancer therapy. Following this same line, Jeetah et al. (2014) mentioned different classes of phytochemicals and some of their members that have been encapsulated in nanovehicle systems for chemotherapeutic or chemopreventive properties. They focused mainly on block copolymer nanomicelles, nanoparticles, polymer-drug conjugates, liposomes, and solid lipid nanocarriers. Nearly 20 different phytochemicals were reviewed and the advantages of trapping in nanocarriers were evaluated. Petrenko et al. (2014), also mention that the nanoencapsulation of anticancer drugs improves their therapeutic indexes by virtue of the improved retention and permeation effect, which achieves passive targeting of nanoparticles in tumors. Derived from the aforementioned, we realize that, indeed, the research and use of nanotechnology for the treatment of cancer is taking a primordial focus at present. The controlled release of drugs is another crucial point in the use of nanotechnology in medicine. A drug carrier should ideally be able to deliver drug molecules to the site of action and to interact specifically with target cells. In 2016, Pastorino’s research group reviewed different studies where different organic and inorganic nanosystems have been proposed and tested. An interesting technique is the layer-by-layer self-assembly of the nanoengineering shells onto sacrificial templates. Attention has been focused on the possibility of synthesizing calcium carbonate nanoparticles in a very controlled manner, which has opened new perspectives for this type of carrier systems. One issue related with drug delivery is the transfollicular drug delivery. Hansen et al. (2014), reported improved needle-free transcutaneous immunization by means of a more efficient drug supply making use of nanotechnology. Nanotechnology can facilitate transfollicular delivery because the nanoparticles penetrate deeper and to a higher extent into hair follicles than solutions. In addition, nanoencapsulation can stabilize antigens and increase their antigenicity. Therefore, the development of more efficient adjuvant-coupled nanocarriers with high antigen payload is a solution to improve the supply of drugs. Naumenko et al. (2014) described the recent advances in the manufacture and utilization of nanoparticle-labeled cells, showing that one of the most promising techniques is the layer-by-layer polyelectrolyte assembly on cells and intracellular and extracellular labelling with magnetic nanoparticles. Among the applications that stand out include the tissue engineering and tumor therapy, showing that nanotechnology not only has application in transport of drugs but also in different medical therapies.
Pescina et al. (2015) reviewed the literature on the most recent advances on blindness and visual impairment treatment using nanopharmaceuticals. They mention that the nanoencapsulation of peptides and proteins presents a series of advantages for their ocular delivery, since it can protect the drug from metabolic activity, control, and maintain the release and increase the bioavailability of the drug after topical or intravitreal administration. The nanoparticulate formulations contribute to improvements in ocular treatments, it is possible to overcome the ocular barriers, the residence time in the eye is improved, and the local level of the drug is increased. In this case, proteins are also used for the preparation of nanovehicles for ophthalmic administration, so that they have a function as therapeutic agents and in turn as carriers.
It is worth highlighting the current interest regarding DNA research. DNA is also emerging as intelligent material to construct nanovehicles for targeted drug delivery. Okholm et al. (2016) mention that although the applications of DNA nanostructures are still in the early stages of research, there are great expectations to offer solutions for targeted therapy. With the use of these DNA nanostructures, the selection and crossing of biological barriers will be facilitated. These nanostructures functionalized with molecules such as polymers, proteins, peptides, small molecules, nucleic acids, or lipids have found applications in the study of subdiffraction resolution fluorescence imaging, membrane channeling, enzyme cascades, molecular walkers, plasmonic chirality, and molecular electronics. In addition, the DNA nano vehicles can be designed to function autonomously in the body. With more specific knowledge of the molecular characteristics of diseases and the behavior of nanoparticles in vivo, it would be expected that nanoparticles could be customized in the future to provide safe and efficient individualized treatment for patients.
Some recent advances on some of the most common nanostructured materials used as nanocarriers for drug transport and release, such as micelles, nanoliposomes, carbon-based nanostructures (nanotubes, graphene, and graphene oxide), dendrimers, polymeric nanoparticles, and inorganic nanoparticles are discussed in the following paragraphs in order to better understand their potential impact on the development of nanopharmaceuticals.
9.4.1 Polymeric Nanoparticles
Polymeric nanoparticles are spherically shaped particles with a large surface to volume ratio; due to their size, they can biodistribute easily in the organism, making them of interest for biomedical applications as imaging, therapeutic, or diagnostics agents. Drug transport and release can be improved when nanoparticles are used as carriers, as they can cross through biological barriers without problems, decreasing the needed dose for pharmacological action and potential toxicity. Oncological applications are among the most promising fields for lipid nanoparticles (Mostafalou et al. 2013). Usually, polymeric nanoparticles are biocompatible, biodegradable, and nontoxic. Synthetic or natural polymers, shaped as nanocapsules (empty core) or nanospheres (porous structures), have been explored. In nanocapsules, the polymeric membrane surrounds a central cavity where the API is confined, while in nanospheres the drug is dispersed in the polymeric matrix (Fig. 9.3). Some common materials used to prepare them are albumin, chitosan, alginate, poly(lactide-co-glycolide), polylactide, and polyethylene glycol, among several others. Their surfaces can be easily modified and functionalized.
Cancer is one of the health problems that have attracted a larger number of research groups to find potential solutions. Luque-Michel et al. (2017) have recently reviewed the use of polymer-based nanocarriers for cancer therapy. Polymer-based nanocarriers have been used to maximize the effectiveness of cancer treatment and minimize the adverse effects of standard therapy. As chemotherapy may induce undesirable side effects, the development of novel therapeutic formulations that are able to reduce or avoid them is desirable. For example, BH3-mimetic ABT-737 is a chemotherapeutic agent for cancer treatment that induces thrombocytopenia. Schmid et al. (2014) found that this side effect could be reduced through the encapsulation of BH3-mimetic ABT-737 in PEGylated poly(lactide-co-glycolide) nanoparticles. Side effects of camptothecin, another anticancer compound that can cause leukopenia and gastrointestinal toxicity, were decreased when encapsulated in the same system, in contrast with the administration of free camptothecin. When both anticancer compounds, BH3-mimetic ABT-737 and camptothecin, were co-encapsulated in a single polymeric nanoparticle, synergistic induction of apoptosis in both in vitro and in vivo colorectal cancer models was found, decreasing substantially the undesired effects in the animal model. This successful strategy to decrease toxicity and secondary effects, enhancing the clinical efficacy of synergistic drug combinations may be explored in future nanopharmaceutical formulations in order to tackle that specific challenge. Another challenge where PNPs may find useful application is as stabilizing agent of sensitive, easily degradable, biomolecules with therapeutic action, such as proteins, genes, and nucleic acids. For example, tenfibgen, the carboxy-terminal fibrinogen globe domain of tenascin-C, nanocapsules with sizes under 50 nm were used as nanocarriers to protect DNA/RNA chimeric oligomers for tumor-directed delivery targeting casein kinase 2 (CK2) α-α′ xenograft tumors in mice. Systemic delivery of s50-TGB-RNAi-CK2 specifically targets malignant cells, including tumor cells in the bone, while low doses reduce size and CK2-related signals in orthopedic primary and metastatic xenograft prostate cancer tumors (Trembley et al. 2014; Ahmed et al. 2016). This approach may be used one day for the design of effective and affordable gene therapy.
Several biocompatible and biodegradable biopolymers such as polysaccharides (chitosan, carboxymethylcellulose, starch), poly(lactide-co-glycolide), polycaprolactone, and others have also been explored as building blocks for the design of polymeric nanoparticles. Some of those biopolymers can be pH- or thermally sensitive, allowing activation of drug releasing under specific chemical or physical environments, improving their performance as controlled transport systems and protecting, at the same time, sensitive molecules with pharmaceutical activity. Bahreini et al. (2014) prepared chitosan-tripolyphosphate nanoparticles loaded with the lyophilized enzyme L-asparaginase II by an ionotropic gelation method; the immobilized enzyme showed an increased in vitro half-life and good thermal and pH stability, in comparison to the free enzyme. Loading efficiency was tuned by changing the chitosan and tripolyphosphate concentrations. In other approach, poly(lactide-co-glycolide) or polycaprolactone nanoparticles loaded with a novel antiplatelet N-substituted-phenylamino-5-methyl-1H-1,2,3-triazole-4-carbohydrazide derivative were prepared as a potential promising therapy for the treatment of thrombotic disorders. As current commercial antiplatelet treatments produce undesirable side effects, the use of biocompatible nanocarriers was considered for the design of better therapeutic agents. Their controlled release profile and their in vitro and in vivo evaluation in a thromboembolism pulmonary animal model was analyzed over 21 days, showing promising activity and low toxicity (Sathler et al. 2014).
Other promising area using polymeric nanoparticles is focused in the treatment of obesity and overweight. Obesity affects, along with overweight, a third of the global population. In recent years, Leptin (Lep), an adipocyte-secreted hormone to control appetite and thermogenesis, has been evaluated combinated with a copolymer Pluronic p85 (Lep@NP85). This conjugate, administered intranasally using the nose-to-brain (INB) route, has shown higher affinity upon binding with the leptin receptor. Many cases of obesity are associated to a leptin resistance. The Lep@Np85 improve not only the accumulation of the leptin as a part of the conjugate in the animal brain, also is observed a significant weight loose. This modified form of leptin show the same activity of the alone hormone after intranasal administration. The LepNP85 with optimized conjugation chemistry is a promising candidate for treatment of obesity (Yuan et al. 2017).
9.4.2 Micelles, Nanoliposomes, and Lipid-Core Nanocapsules
Micelles are spherical structures with sizes usually under 20–50 nm (liposomes are regularly range from 100 nm to 3 μm). They are composed by amphiphilic chains self-assembled in solution as a closed-cage because of polar/nonpolar interactions (Fig. 9.4a, b). Usually, the internal cavity (core) is hydrophobic while the exterior (shell) is hydrophilic (direct micelle), but they can also have a hydrophilic core and a hydrophobic shell (inverse micelle). This duality allows micelles to be applied on the selective solubilization of polar and nonpolar drugs, depending on the administration route. At the internal cavity of direct micelles, small molecules, poorly soluble in water, can be stored, protected, and stabilized by the external layer (Fadeel et al. 2012). These versatile systems can be used for transportation and release of water-insoluble drugs and imaging agents. They are highly stable in physiological conditions, being able to circulate during prolonged times and accumulate in specific target sites when functionalized with appropriate ligands in their surfaces. Nanoliposomes, on the other hand, are nanometric versions of liposomes. Spherical in shape, they can be produced from natural phospholipids, cholesterol, and their derivatives (Fig. 9.4c). Most used systems for encapsulation of APIs and for the design of controlled release systems can be classified, according to the number and size of bilayers as multilamellar and large or small unilamellar vesicles. Size, as well as lipid composition, determines properties such as fluidity, permeability, stability, and structure. There are five types of nanoliposomes, in terms of their composition and intracellular internalization mechanism: conventional, pH-sensitive, cationic, long circulating, and immunoliposomes. When a vesicle is formed from non-ionic surfactants, it is called noisome; although their properties are close to those of a liposome, they have larger chemical stability but higher production costs (Chekman 2010). Nanoliposomes have been successfully tested in Food and Drug Administration clinical tests, and some of them have received authorization for developing cosmetics and therapeutic agents as Daunoxome® and Ambisome® for cancer treatment. Several amphiphilic molecules have been used for the formation of stable micelles and nanoliposomes for nanopharmaceutical formulations: polyethylene glycol lipids, pluronic, poly(amino acid)-b-polyethylene glycol (amino acid = glutamic, aspartic), polycaprolactone-b-methoxy-polyethylene glycol, methoxy poly(ethylene glycol)-b-poly(d, l-lactide), chitosan grafted with palmitoyl, and poly(N-isopropylacrylamide)-poly(vinylpyrrolidone)-poly(acrylic acid), among several others (Fig. 9.5).
The fact that micelles and nanoliposomes improve solubility of poorly soluble molecules, as well as protecting encapsulated substances from degradation and clearance, among other properties, makes them attractive for their use as nanocarriers in drug delivery. They have also been explored as efficient vehicles for improving the drug’s pharmacokinetics, biodistribution, and cellular uptake, decreasing biodegradation, inadequate tissue distribution, and toxicity. Recently, Haratifar et al. (2014) prepared casein micelles to encapsulate epigallocatechin gallate, the major catechin found in green tea. Epigallocatechin gallate has antiproliferative activity on colon cancer cells, and it was shown that epigallocatechin gallate containing micelles decreased the proliferation of HT-29 cancer cells in vitro. These results indicate that protecting epigallocatechin gallate or other sensitive therapeutical molecules in a polymeric matrix may be of utility for the stabilization of sensitive APIs and biomolecules, improving their biodistribution and therapeutic efficiency. For example, the transport and release of antioxidants has an ample market of applications, both for pharmaceutical use as well as for food fortification. Several potent antioxidants, as well as other useful natural molecules with benefic therapeutic effects, have poor solubility or are unstable at physiological conditions, many of them being prone to enzymatic biodegradation. Nanocarriers may become an alternative to improve both their solubility and stability. Resveratrol and curcumin, two polyphenols well known by their antioxidant properties, were encapsulated in poly(lactide-co-glycolide) lipid-core nanocapsules (Fig. 9.3d). The in vitro antioxidant activity against hydroxyl radicals, as well as their antioxidant release profile improved after nanoencapsulation. Co-encapsulation of both antioxidants was also explored, and it is a promising strategy to enhance performance when treating diseases associated with oxidative stress (Coradini et al. 2014, 2015). Docosahexanoic acid, an omega-3 polyunsaturated fatty acid known for its health benefits in the development of infants, has also protective effects against H. pylori gastric infection. Docosahexanoic acid was encapsulated in a lipid-core nanocapsule (average size of 302 nm) produced by hot homogenization and ultrasonication using a mixture of commercial surfactants (Precirol ATO5®, Miglyol-812® and Tween 60) and showed inhibition of H. pylori growth in vitro (Seabra et al. 2017). Rice bran oil, a natural extract obtained from the hard outer brown layer of rice (rice husk) traditionally used to protect skin from UVB radiation damage as well as for deep-frying cooking. UVB radiation may induce skin damage and cancer, so protection against it may help to prevent these problems. The extract was encapsulated in lipid-core nanocapsules (medium size ~200 nm) and its ability to prevent ear edema induced by UVB irradiation showed a 61% efficiency, reducing at the same time oxidative stress and carcinogenesis response (Rigo et al. 2015). In a similar work, Badea et al. (2015) developed an integrative approach against basal cellular carcinoma. They encapsulated two anticancer drugs (5-fluorouracil, a hydrophilic chemotherapeutic drug and ethylhexyl salicylate, a lipophilic UVB sunscreen agent) in nanostructured lipid carriers made of bioactive squalene (50.8% w/w) obtained from amaranth seed oil, as a chemoprotective agent. The co-loaded nanocapsules (100 nm in diameter) were able to block UVB light efficiently, as well as to scavenge free radicals (70%);in vitro drug release showed sustained release of 5-fluorouracil, suggesting this system may become an effective preventive agent against photoaging, skin cancer, and skin damage. Finally, N,O-carboxymethyl chitosan nanoparticles were loaded with 5-fluorouracil and curcumin, and their in vivo pharmacokinetics was evaluated. The loaded nanocarriers were blood compatible, releasing the drug over a period of 4 days in a pH range from 4.5 to 7.4 and showing good anticancer effects against colon cancer cells (HT-29) (Anitha et al. 2014).
9.4.3 Carbon Based Nanomaterials
Carbon-based nanomaterials for drug delivery are a rapidly growing field. There are several types of carbon-based nanomaterials. Figure 9.6 shows some of the most representative systems, such as fullerenes, graphene, carbon sponges, nanocones, single-walled carbon nanotubes, and multi-walled carbon nanotubes, among others. Carbon nanotubes are usually formed by hexagonal open or closed networks of carbon atoms, sometimes presenting different kinds of defects (substitutional or geometrical) and may have diameters from 1 nm (single-walled carbon nanotubes) to several hundreds of nanometers (multi-walled carbon nanotubes) and lengths from 1 nm to several micrometers. Carbon nanotubes have been extensively studied for clinical use, as they are able to penetrate easily the cell membrane, carrying APIs. Due to their high aspect ratio, they have a large capacity for storage inside several small molecules, and their surfaces can be easily modified to improve their specificity, biodistribution, and biocompatibility. Their low solubility in aqueous systems is a problem, being prone to agglomeration. Multi-walled carbon nanotubes are potentially toxic after modifying their solubility, as they become more bioavailable (Hilder and Hill 2007).
The use of graphene-based nanocarriers for drug delivery applications has been recently reviewed and discussed (Liu et al. 2013). The easiness for chemical modification of their surfaces to tune their biocompatibility and toxicity or controlling releasing mechanisms (pH-sensitive, thermal, photo- and magnetic induction) opens numerous possibilities for the development of efficient therapeutic and diagnostic systems. For example, dopamine conjugated graphene oxide nanoparticles were recently prepared and used as nanocarriers for cellular delivery of the anticancer drug methotrexate. The loaded nanocarriers were tested in a human breast adenocarcinoma cell line showing significant antitumor activity and improving drug delivery. The design of novel nanocarrier conjugates is then a promising field of research for the development of useful therapeutical agents (Masoudipour et al. 2017). In other work, a conjugated graphene oxide-gallic acid drug-delivering system was recently developed by Dorniani et al. (2016) and characterized by several analytical techniques (X-ray diffraction, Fourier transform infrared spectroscopy, high-resolution transmission electron microscopy, Raman and Ultraviolet/Visible spectroscopy). The nano-conjugate was able to release gallic acid in phosphate buffer system at pH 7.4 in a sustainable way; in vitro evaluation against normal fibroblast (3 T3) and liver cancer cells (HepG2) showed good inhibitory effect on cancer cells without affecting normal cell growth.
Carbon nanotubes have emerged as an exciting alternative for transporting therapeutical molecules. Functionalization of carbon nanotubes decreases toxicity and immunogenic response, displaying a promising potential to become platforms for drug delivery of peptides, proteins, nucleic acids, and drugs. They can be used as components in multifunctional composites for use as theranostic agents. For example, a composite of multi-walled carbon nanotubes and cobalt ferrite nanoparticles has been designed for use as a MRI contrast agent. Coating the multi-walled carbon nanotube@CoFe2O4 nanocomposite with mesoporous silica resulted in increased biocompatibility and loading efficiency. When loaded with doxorubicin, the nanocomposite showed good pH-responsive drug release within 48 h (Fan et al. 2017). Molecules with low solubility such as curcumin, a potent antioxidant that protects against oxidative stress-related injuries and anticancer activity, have been also loaded in carbon nanocarriers. Multi-walled carbon nanotubes functionalized with polyvinyl alcohol and loaded with curcumin were evaluated in vitro showing good release performance at physiological pH (7.4–5.5); at low pH values, release increased (25–30%) than at higher pH values (Zawawi et al. 2017).
9.4.4 Inorganic Nanoparticles
Numerous nanomaterials with different chemical compositions (magnetite, Fe3O4; silica, SiO2; zinc oxide, ZnO; zerovalent metals such as Ag, Au, Pt; CdS and ZnSe quantum dots), which may present an ample variety of shapes (rods, wires, tubes, particles, sheets) and structures (core-shell, multilayered, organically/inorganically coated, hollow o porous, among others), have been explored as drug delivery systems (Fig. 9.7). Coupling of APIs on the surface of inorganic nanoparticles (surface functionalization) changes the stability of the nanomaterial, as well as its biocompatibility. Inorganic nanomaterials can be easily chemically modified on their surfaces, in order to achieve more stable systems, with increased half-life, to be exploited as drug delivery and controlled release systems (Vargas-Gonzalez et al. 2016). They are easy to modify in their surfaces and have been explored for drug delivery, imaging, diagnosis, etc.
Metallic and metal oxide nanoparticles can act as drug nanocarriers or also as antimicrobial agents themselves. Aside from their microbicide activity, inorganic nanoparticles may possess interesting physical properties such as magnetism, catalytic activity, redox active behavior, and fluorescence, among others. These properties make them useful for the design of multifunctional nanocarriers, with great potential for theranostic applications. The use of metal-based nanomaterials as antimicrobials, as well as the mechanisms of action, has been discussed by Raghunath and Perumal (2017). In particular, the toxicity of silver nanoparticles in biological systems has been explored by several research groups, and it is a very active field; the antimicrobial activity of silver nanoparticles and its potential use for the design of novel nano-antibiotics has been recently reviewed (Vazquez-Muñoz et al. 2017). For example, Marslin et al. (2015) used extracts of Withania somnifera to reduce AgNO3 and prepare a cream formulation containing silver nanoparticles with antimicrobial activity; the cream was reported to be effective against S. aureus, P. aeruginosa, P. vulgaris, E. coli, and C. albicans. This formulation may be an alternative to the use of conventional antibiotics or for the treatment of antibiotic-resistant pathogens (Marslin et al. 2015). Other metal oxides have been used as support for silver nanoparticles immobilization. Recently, hollow TiO2-coated CeO2 nanocarriers were prepared and loaded with silver nanoparticles and their Ag+ ion releasing performance evaluated. These systems showed excellent antibacterial activity against E. coli, although they were also cytotoxic against a model epithelial barrier cell type (A549 cells) (Gagnon et al. 2016). Further research on the use of silver nanoparticles is necessary in order to avoid toxicological effects that may affect their antibacterial performance.
Mesoporous materials, such as hollow nanoparticles, have been explored as alternatives to carry different kind of biologically active molecules in their inner space, becoming great choices for drug transport and delivery. Further modification of the surface of nanomaterials, both to enhance molecular recognition of specific targets or to attach pro-drugs that can be carried until the right conditions (pH, enzymatic activity) break the bond, releasing the active principle, is an active field of research. Recently, the antitumor performance of ZnO hollow nanocarriers containing the anticancer drug PTX, against breast cancer in an animal model was reported (Puvvada et al. 2015). The surface of the hollow ZnO nanoparticles was modified with folate groups, improving their uptake by breast malignant cells; a drug release efficiency of 75% within 6 h in the characteristic low, acidic, pH of the tumor microenvironment was determined. Fluorescence of the nanocarrier increased because of drug release, becoming thus a useful way to evaluate the nanocarrier’s performance. This dual, pH-sensitive, and fluorescent nanocarrier may be useful for improving chemotherapy tolerance and anticancer efficiency and to develop flexible theranostic tools for both diagnostics and anticancer therapy. The development of multifunctional inorganic-organic, hybrid, nanocarriers is a very exciting field. Landarani-Isfahani et al. (2017) reported the development of magnetic nanoparticles conjugated with G2 triazine dendrimers (Fe3O4@SiO2/G2), loaded with methotrexate, that are pH-responsive; the chemotherapeutic hybrid nanocarrier was tested against in vitro using MCF-7, HeLa, and Caov-4 cell lines, showing good cytotoxicity. These nanocomposites were biocompatible and degradable as indicated by blood safety analyses and could be used as effective drug carriers for anticancer applications. In other work where dendrimers and inorganic nanoparticles were mixed, a system consisting of polyamidoamine dendrimers conjugated with magnetic nanoparticles was prepared and characterized; the nanocomposite performance as a stimuli-responsive drug carrier for thermally activated chemotherapy of cancer was evaluated (Nigam and Bahadur 2017). When alternating current magnetic fields were applied to the doxorubicin-loaded formulation, a synergistic effect on the inhibition of cervical cancer cell growth was found. These novel hybrid systems may be of interest for the development of innovative combinatorial therapeutic agents.
Finally, innovative ideas on the design of inorganic nanocarriers conjugated with bioactive molecules, such as enzymes or proteins with antiviral or anticancer activity, have been explored. First, a tyrosine kinase conjugate with gold nanorods was prepared by Liu et al. (2017) and evaluated as potential platforms for targeted drug delivery and photothermal tumor ablation. In the absence of laser irradiation, moderate necrosis of human metastatic renal carcinoma cells in a nude mice model was observed; however, under irradiation, both with or without gold nanorods, tumor necrosis improved, although irradiation in the presence of gold nanorods showed a synergistic complete tumor necrosis. Finally, momodicas anti-HIV protein, a 30 kDa single-stranded, type-I ribosome inactivating protein with antitumor and anti-HIV activities was encapsulated in zirconium egg- and soy-phosphatidylcholines nanoparticles; the nanocarriers were characterized by transmission electron microscopy and X-ray diffraction. The obtained nanoformulation showed positive results in antimicrobial and anti-HIV assays, with low toxicity and good first order releasing kinetics (Caizhen et al. 2015).
9.4.5 Dendrimers
Dendrimers are hyperbranched, tree-like structured polymers, of large size and complexity, but with a well-defined chemical structure (Fig. 9.8). Dendrimers grow branches from a central core. Their usual size does not exceed 15 nm, having a relatively dense surface with an almost empty core, having also very low polydispersity index, high bio-permeability and biocompatibility. These large molecules present numerous internal voids and channels that can be used to trap host molecules (Onoue et al. 2014). They can be used to improve solubility of APIs and have been explored in the formulation of several controlled release systems. Dendrimers can be designed for multiple drug target-specific controlled release, but there are several concerns related to their toxicity profile. According to the nature of their chemical components, there are several types of dendrimers: polyamidoamine, poly(glycerol), melamine, triazine, polyethylene glycol, carbohydrate, or citric acid derivatives, among several others.
Sundry reviews on the use of dendrimers as drug carriers have been published recently (Elkin et al. 2017; Viswanath and Santhakumar 2017; Sheikhpour et al. 2017). Dendrimers containing terminal amine groups are pH-stimuli-responsive, becoming useful for controlled release of drugs. There are several examples of these nanosized highly branched fractal-like macromolecules, both as pure dendrimers or as in combination with other nanomaterials. As dendrimers can be designed to overcome limitations that most common drugs present such as low solubility, stability, biodistribution, or specificity, they can be tuned to be able to reach specific targets, to avoid immune clearance, and to present reduced toxicity. Dendrimers can enter into the cells through phagocytosis or endocytosis, improving the therapeutic efficiency. The use of dendrimers containing biomolecules, such as amino acids, peptides, or antibodies is an active field of research as these derivatives may be highly effective to recognize specific targets. For example, Kim et al. (2017) prepared a four-branched arginine-glycine-aspartic acid tripeptide (RGD) dendrimer, bound to polyethylenimine-grafted chitosan containing a targeted gene for alpha-beta-integrin. The dendrimer was capable to inhibit the growth of a solid tumor in vivo in a mouse xenograft model. When mixed with other nanomaterials, multifunctional dendrimer-containing nanocarriers can be obtained. A multifunctional dendrimer conjugated to gold nanoparticles and loaded with doxorubicin was designed as a novel nano-platform for pH triggered doxorubicin intracellular delivery. Exploiting the luminescent properties of gold nanoparticles, cell internalization, and doxorubicin release was monitored using confocal laser scanning microscopy, and in vitro studies showed increased cytotoxic effect. This development could lead to the design of a promising nanocarrier for imaging the intracellular transport of several anticancer drugs (Khutale and Casey 2017). In other similar work, the utility of multifunctional dendrimers to serve as molecular theranostic agents was explored where an anionic linear globular dendrimer G2 was conjugated with an AS1411 aptamer to target human breast cancer cells (MCF-7) and deliver iohexol. The nanoconjugated toxicity on nucleolin-positive MCF-7 cells and nucleolin-negative HEK-293 cells was assessed by the 2,3-bis-(2-methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5-carboxanilide cell viability and apoptosis/necrosis assays, and in vivo computerized tomography imaging, showing promising effects after reducing the number of cancer cells (Mohammadzadeh et al. 2017).
The good transfection efficiency and low toxicity of dendrimers make them promising for gene therapy and as nuclei acids carriers. Askarian et al. (2017) reported the preparation and characterization of polyamidoamine-pullulan conjugate nanoparticles with sizes in the range from 118 to 194 nm. These systems showed good efficiency as transfection agents in HepG2 (receptor-positive) and N2A (receptor-negative) cell lines, improving delivery of nucleic acids into the liver cells expressing asialoglycoprotein receptor with minimal transfection in nontargeted cells. In another work, Lee et al. (2017) recently reported a similar system, based on a G4-polyamidoamine dendrimer containing the cathepsin B-enzyme-sensitive sequence (glycine-phenylalanine-leucineglycine, GFLG), which presented excellent transfection efficiency and low cytotoxicity in HeLa cells. These dendrimer nanocarriers, with controllable sizes and architectures, low toxicity, and improved targeting properties, may become one day an efficient nanocarrier for gene therapy, among other applications.
Table 9.4 summarizes some of the selected examples of nanocarriers recently reported.
In summary, there are several opportunities on the design and use of nanostructured materials for drug delivery and release. These nanomaterials may help to overcome several of the already identified challenges associated with traditional pharmaceutical formulations such as specificity, controlled release under specific conditions or external stimuli, stabilization of unstable drugs or biomolecules, and theranostic multifunctionality (e.g., imaging + diagnosis + drug transport), among several others. Polymeric nanoparticles rise as some of the most studied systems, but others such as dendrimers, carbon-based, and inorganic nanoparticles are also becoming prominent and their unique physical properties make them very promising.
9.5 Challenges Associated with the Use of Nanomaterials in Pharmaceutical Formulations
As previously discussed, the unique physical characteristics of nanostructured materials make them very attractive for use as components in the development of new pharmaceutical formulations. However, practical and commercial applications should consider that chemical composition, including purity, crystallinity, and physical properties of the components, as well as their reduced dimensions that affect directly the effective surface area, may affect not only their solubility but also their chemical reactivity. Furthermore, the role of the surfactant agents (organic, inorganic, or composite) as well as that of the chemical functions present on the nanomaterial’s surface may play a decisive role not only in their stability in solution but also in the biocompatibility and biodistribution (Fig. 9.9). Chemical or physical interactions among nanostructured carriers and the physiological media components (proteins, sugars, ions) will also affect the stability of the nanopharmaceutical, as well as its drug delivery/release kinetics. In biological systems, these properties have a big impact on pharmacokinetics and toxicity, as they affect directly the nanocarriers’ biodistribution and effective internalization in cells and tissues (Halappanavar et al. 2018; Juillerat et al. 2015; Gracssian 2008).
Chemical modification of the nanocarriers’ surface may be used as a way to increase stability, solubility, or biocompatibility, decreasing the probability of clearing by the reticuloendothelial system. However, physical and chemical degradation of the surfactants may generate reactive oxygen species or yield other toxic derivatives that may negatively affect the organism. Furthermore, the interaction of the nanomaterials with biomolecules present in the physiological medium may result in the formation of a biological corona on its surfaces that may drastically affect their properties; these properties may be completely different to those of the original nanomaterial, changing their bioavailability, toxicity, or reactivity (Halappanavar et al. 2018; Mahmoudi et al. 2011).
Undesirable adverse reactions to some components of nanopharmaceuticals could become a potential problem, limiting their functionality. Moreover, the large reactivity derived from the aspect ratio, may be responsible of some observed adverse responses. However, as nanopharmaceuticals can be administered in low doses, these adverse reactions may also decrease. A new discipline called nano-pharmacovigilance must be aware of these potential hazards in order to be able to assess the risk of nanotechnology applied to drug development and thus to design proper risk minimization plans for nanomedicines to intervene in a timely manner (Salas-Rojas et al. 2017).
Some recent reports on cytotoxicity, DNA damage, inflammatory responses, and generation of reactive oxygen species, among other adverse reactions have been observed (Holden et al. 2013; Fadeel et al. 2012). The toxicity of nanomaterials (also known recently as nanotoxicity) is an active research field that deals with the possible toxic effects on health of nanomaterials, when they are in contact with human or other living organisms (Halappanavar et al. 2018; Oberdörster et al. 2005). Although currently there is no consensus on the safety or toxicity of several commonly used nanomaterials, it is probable that their unique surface properties derived of their small size may result in adverse effects. However, more research in this field is required in order to better understand the risks and impacts of the use of nanomaterials in pharmaceutical formulations (Saiyed et al. 2011).
To date, very few nanopharmaceuticals are reaching the final phases of development of new medicines and approval for commercialization. Researchers agree that in order to move from the bench to the bedside, several experimental challenges need to be addressed. There is still concern about the precise control of drug release of nanoformulations, about their biodistribution or their fate, especially when they do not biodegrade, and, of course, their toxicity. Thus, there is consensus regarding the need of validated and standardized protocols for early detection of toxicity and for nanoparticle characterization using in vitro assays and appropriate animal models of disease (Mendez-Rojas et al. 2016). In vivo studies need to go in depth into the understanding of how nanoparticles interact with target organs, tissues, cells, and intracellular molecules, to what extent they remain stable and what is their potential to accumulate (Hua et al. 2018; Ventola 2017; Min et al. 2015).
A close interaction between regulators, academic institutions, research centers, and the industry can help accelerate the translation of nanomedicine efforts. In addition, through the application of the “quality by design” approach, sound science and quality risk management can merge to achieve innovative and even disruptive breakthroughs in new nanopharmaceuticals development and at the same time to provide of safe, convenient, and cost-effective drugs to patients.
9.6 Conclusions
The promises and impacts of nanotechnology are expected to be bigger than the dimensional scale where it is usually defined. Without any doubt, nanomaterials will allow the development of novel products that overcome the different obstacles and challenges currently found in the pharmaceutical industry for targeted drug delivery such as limited bioavailability, low stability, limited permeability across biological barriers, immune surveillance, and target specificity. The development of intelligent, implantable, and biocompatible devices that can be used for the automatic administration of nanopharmaceuticals directly in the organism is an advance that may be useful for cancer therapy, vaccination, and gene therapy or for the treatment of neurodegenerative diseases. In addition, the exploration of alternative administration routes such as pulmonary drug delivery or transdermal application of drugs will expand the therapeutic choices for the treatment of different diseases. The use of multifunctional materials with unique magnetic, optical, thermal, or mechanical properties widen the possibilities for the design of theranostic systems capable of not only carrying and delivering drugs but also to help with imaging, diagnostics, and even therapeutic uses. However, the large-scale production of safe, biocompatible, and economical nanomaterials suitable for pharmaceutical use is still a limitation that needs to be solved in order to have real applications in human health. A clear understanding of the interactions between nanoformulations and cell components is necessary for the success of such applications. In this sense, combining computational models, bioinformatics tools, and quantitative molecular techniques might allow a deeper understanding of the interaction of nanoformulations with the cell dynamic and the biological systems. This comprehensive understanding is critical, particularly with respect to potential toxicological effects.
There are still several questions and challenges in the field that need to be solved in order to understand not only the toxicological effects of nanoformulations in living organisms but also the environmental effects of them and the opportunities for regulatory approval and commercialization. Nanopharmaceuticals are on the rise, and their impact on the development of a more personalized medicine, with important benefits for patients and physicians, is still beyond our imagination.
References
Agarwal V, Bajpai M, Sharma A (2018) Patented and approval scenario of nanopharmaceuticals with relevancy to biomedical application, manufacturing procedure and safety aspects. Recent Pat Drug Deliv Formul 12(1):40–52
Ahmad J, Singhal M, Amin S, Rizwanullah M, Akhter S, Kamal MA, Haider N, Midoux P, Pichon C (2017) Bile salt stabilized vesicles (bilosomes): a novel nano-pharmaceutical design for oral delivery of proteins and peptides. Curr Pharm Des 23(11):1575–1588
Ahmad N, Ahmad R, Alam MA, Ahmad FJ (2018) Enhancement of oral bioavailability of doxorubicin through surface modified biodegradable polymeric nanoparticles. Chem Cent J 12:65
Ahmed K, Kren BT, Abedin MJ, Vogel RI, Shaughnessy DP, Nacusi L, Korman VL, Li YM, Dehm SM, Zimmerman CL, Niehans GA, Unger GM, Trembley JH (2016) CK2 targeted RNAi therapeutic delivered via malignant cell-directed tenfibgen nanocapsule: dose and molecular mechanisms of response in xenograft prostate tumors. Oncotarget 7(38):61789–61805
Anitha A, Sreeranganathan M, Chennazhi KP, Lakshmanan VK, Jayakumar R (2014) In vitro combinatorial anticancer effects of 5-fluorouracil and curcumin loaded N,O-carboxymethyl chitosan nanoparticles toward colon cancer and in vivo pharmacokinetic studies. Eur J Pharm Biopharm 88:238–251
Asadian-Birjand M, Sousa-Herves A, Steinhilber D, Cuggino JC, Calderon M (2012) Functional nanogels for biomedical applications. Curr Med Chem 19(29):5029–5043
Askarian S, Abnous K, Ayatollahi S, Farzad SA, Oskuee RK, Ramezani M (2017) PAMAM-pullulan conjugates as targeted gene carriers for liver cell. Carbohydr Polym 157:929–937
Badea G, Lacatusu I, Ott C, Badea N, Grafu I, Meghea A (2015) Integrative approach in prevention and therapy of basal cellular carcinoma by association of three actives loaded into lipid nanocarriers. J Photochem Photobiol B 147:1–8
Bahreini E, Aghaiypour K, Abbasalipourkabir R, Mokarram AR, Goodarzi MT, Saidijam M (2014) Preparation and nanoencapsulation of L-asparaginase II in chitosan-tripolyphosphate nanoparticles and in vitro release study. Nanoscale Res Lett 9:340
Bajpai A, Shukla S, Saini R, Tiwari A (2010) Stimuli responsive drug delivery systems: from introduction to application. Rapra-Smithers Press, Shawbury
Bak A, Leung D, Barrett SE, Forster S, Minnihan EC, Leithead AW, Cunningham J, Toussaint N, Crocker LS (2015) Physicochemical and formulation developability assessment for therapeutic peptide delivery – a primer. AAPS J 17(1):144–155
Benet LZ (2013) The role of BCS (biopharmaceutics classification system) and BDDCS (biopharmaceutics drug disposition classification system) in drug development. J Pharm Sci 102(1):34–42
Benival DM, Devarajan PV (2012) Lipomer of doxorubicin hydrochloride for enhanced oral bioavailability. Int J Pharm 423(2):554–561
Beyer S, Xie L, Schmidt M, de Bruin N, Ashtikar M, Ruschenbaum S, Lange CM, Vogel V, Mantele W, Parmham MJ, Wacker MG (2016) Optimizing novel implant formulations for the prolonged release of biopharmaceuticals using in vitro and in vivo imaging techniques. J Control Release 235:352–364
Borišev I, Mrđanovic J, Petrovic D, Seke M, Jović D, Srđenović B, Latinovic N, Djordjevic A (2018) Nanoformulations of doxorubicin: how far have we come and where do we go from here? Nanotechnology 29(33):332002
Bose T, Latawiec D, Mondal PP, Mandal S (2014) Overview of nano-drugs characteristics for clinical application: the journey from the entry to the exit point. J Nanopart Res 16:2527
Bruno BJ, Miller GD, Lim CS (2013) Basics and recent advances in peptide and protein drug delivery. Ther Deliv 4(11):1443–1467
Bruschi ML (ed) (2015) Strategies to modify the drug release from pharmaceutical systems. Woodhead Publishing, Cambridge
Caizhen G, Yan G, Ronron C, Lirong Y, Panpan C, Xuemei H, Yuanbiao Q, Quinqshan L (2015) Zirconium phosphatidylcholine-based nanocapsules as an in vivo degradable drug delivery system of MAP 30, a momordica anti-HIV protein. Int J Pharm 483:188–199
Cassano R, Ferrarelli T, Mauro MV, Cavalcanti P, Picci N, Trombino S (2016) Preparation, characterization and in vitro activities evaluation of solid lipid nanoparticles based on PEG-40 stearate for antifungal drugs vaginal delivery. Drug Deliv 23(3):1047–1056
Chavda HV, Patel CN, Anand IS (2010) Biopharmaceutics classification system. Sys Rev Pharm 1(1):62–69
Chekman IS (2010) Pharmacological and pharmaceutical foundation of nanodrugs. Likars'ka Sprava/Ministerstvo Okhorony Zdorov'ia Ukrainy 1(2):3–10
Chilkwar RN, Nanjwade BK, Nwaji MS, Idris SM, Mohamied AS (2015) Bilosomes based drug delivery system. J Chem Applications 2(1):5
ClinicalTrials.gov (2018a) Search term: Arikace. U.S. National Library of Medicine, Bethesda, MD. Last updated 05 July . Available from: https://clinicaltrials.gov/ct2/results?cond=&term=arikace&cntry=&state=&city=&dist=
ClinicalTrials.gov (2018b) Search term: SLIT cisplatin. U.S. National Library of Medicine, Bethesda, MD. Last updated 05 July 2018. Available from: https://clinicaltrials.gov/ct2/results?cond=&term=slit&cntry=&state=&city=&dist=
Coradini K, Lima FO, Oliveira CM, Chaves PS, Athayde ML, Carvalho LM, Beck RC (2014) Co-encapsulation of resveratrol and curcumin in lipid-core nanocapsules improves their in vitro antioxidant effects. Eur J Pharm Biopharm 88:178–185
Coradini K, Friedric RB, Fonseca FN, Vencatto MS, Andrade DF, Oliveira CM, Battistel AP, Guterres SS, da Rocha MI, Pohlmann AR, Beck RC (2015) A novel approach to arthritis treatment based on resveratrol and curcumin co-encapsulated in lipid-core nanocapsules: in vivo studies. Eur J Pharm Sci 78:163–170
Cristofoletti R, Chiann C, Dressman JB, Storpirtis S (2013) A comparative analysis of biopharmaceutics classification system and biopharmaceutics drug disposition classification system: a cross-sectional survey with 500 bioequivalence studies. J Pharm Sci 102(9):3136–3144
Daeihamed M, Haeri A, Ostad SN, Akhlaghi MF, Dadashzadeh S (2017) Doxorubicin-loaded liposomes: enhancing the oral bioavailability by modulation of physicochemical characteristics. Nanomedicine (Lond) 12(10):1187–1202. https://doi.org/10.2217/nnm-2017-0007
Daousani C, Macheras P (2016) Biopharmaceutic classification of drugs revisited. Eur J Pharm Sci 95:82–87
Demina NB, Skatkov SA (2013) Development strategies and biopharmaceutical aspects of drug delivery systems. Russ J Gen Chem 83:2519
Dhanapal R, Ratna JV (2012) Nanosuspensions technology in drug delivery. Int J of Pharm Rev Res 2(1):46–52
Dorniani D, Saifullah B, Barahuie F, Arulselvan P, Bin Hussein MZ, Fakurazi S, Twyman LJ (2016) Graphene oxide-gallic acid nanodelivery system for cancer therapy. Nanoscale Res Lett 11:491
Elkin I, Banguy X, Barret CJ, Hildgen P (2017) Non-covalent formulation of active principles with dendrimers: current state-of-the-art and prospects for further development. J Control Release 264:288–305
El-Sherbiny IM, El-Baz NM, Yacoub MH (2015) Inhaled nano- and microparticles for drug delivery. Glob Cardiol Sci Pract 2015:2. https://doi.org/10.5339/gcsp.2015.2
Fadeel B, Pietroiusti A, Shvedova A (2012) Adverse effects of engineered nanomaterials. Exposure, toxicology, and impact of human health. Academic Press, Waltham
Fan HT, Xing XJ, Yang YH, Li B, Wang CC, Qiu DF (2017) Triple function nanocomposites of porous silica-CoFe2O4-MWCNTs as a carrier for pH-sensitive anti-cancer drug controlled delivery. Dalton Trans 46(43):14831–13838
Gagnon J, Clift MJD, Vahnecke D, Widnersson IE, Abram SL, Petri-Fink A, Caruso RA, Rothen-Rutishauser B, Fromm KM (2016) Synthesis, characterization, antibacterial activity and cytotoxicity of hollow TiO2-coated CeO2 nanocontainers encapsulating silver nanoparticles for controlled silver release. J Mater Chem B 4(6):1166–1174
Gelperina S, Kisich K, Iseman MD, Heifets L (2005) The potential advantages of nanoparticle drug delivery systems in chemotherapy of tuberculosis. Am J Respir Crit Care Med 172(12):1487–1490. https://doi.org/10.1164/rccm.200504-613PP
Ghadi R, Dand N (2017) BCS class IV drugs: highly notorious candidates for formulation development. J Control Release 248:71–95
Gönüllü U, Şaki D (2017) Formulation and characterization of norethisterone transdermal patch as an alternative route to oral administration. Trop J Pharm Res 16(12):2785–2792
Gracssian V (2008) Nanoscience and nanotechnology, environmental and health impact. Wiley, Hoboken
Grand View Research (2017) Nanomedicine market analysis by products, (therapeutics, regenerative medicine, diagnostics), by application, (clinical oncology, infectious diseases), by nanomolecule (gold, silver, iron oxide, alumina), & segment forecasts, 2013–2025. Last Updated April 2017. Available from: https://www.mordorintelligence.com/industry-reports/healthcare-nanotechnology-nanomedicine-market
Halappanavar S, Vogel U, Wallin H, Yauk C (2018) Promise and peril in nanomedicine: the challenges and needs for integrated systems biology approaches to define health risk. WIREs Nanomed Nanobiotechnol 10(1):e1465. https://doi.org/10.1002/wnan.1465
Hamidi M, Azadi A, Rafiei P, Ashrafi H (2013) A pharmacokinetic overview of nanotechnology-based drug delivery systems: an ADME-oriented approach. Crit Rev Ther Drug Carrier Syst 30(5):435–467
Hansen S, Lehr CM (2014) Transfollicular delivery takes root: the future for vaccine design? Expert Rev Vacciones 13(1):5–7
Haratifar S, Meckling KA, Corredig M (2014) Antiproliferative activity of tea catechins associated with casein micelles, using HT29 colon cancer cells. J Dairy Sci 97:672–678
Hilder TA, Hill JM (2007) Carbon nanotubes as drug delivery nanocapsules. Curr Appl Phys 8:258–261
Holden PA, Nisbet RM, Lenuhan HS, Miller RJ, Cherr GN, Schimel JP, Gardea JL (2013) Ecological nanotoxicology: integrating nanomaterial hazard considerations across the subcellular, population, community, and ecosystems levels. Chem Res 46(3):813–822
Horne WS, Johnson LM, Ketas TJ, Klasse PJ, Lu M, Moore JP, Gellman SH (2009) Structural and biological mimicry of protein surface recognition by alpha/beta-peptide foldamers. Proc Natl Acad Sci U S A 106(35):14751–14756
Hua S, de Matos MBC, Metselaar JM, Storm G (2018) Current trends and challenges in the clinical translation of nanoparticulate nanomedicines: pathways for translational development and commercialization. Front Pharmacol 9:790. https://doi.org/10.3389/fphar.2018.00790
Ibrahim N, Ibrahim H, Sabater AM, Mazier D, Valentin A, Nepveu F (2015) Artemisinin nanoformulation suitable for intravenous injection: preparation, characterization and antimalarial activities. Int J Pharm 495(2):671–679. https://doi.org/10.1016/j.ijpharm.2015.09.020
Iqbal N, Vitorino C, Taylor KM (2017) How can lipid nanocarriers improve transdermal delivery of olanzapine? Pharm Dev Technol 22(4):587–596. https://doi.org/10.1080/10837450.2016.1200615
Jeetah R, Bhaw-Luximon A, Jhurry D (2014) Nanopharmaceutics: phytochemical-based controlled or sustained drug-delivery systems for cancer treatment. J Bbiomed Nanotech 10(9):1810–1840
Juillerat L, Fjellesbo LM, Dusinska M, Collins AR, Handy R, Riediker M (2015) Biological impact assessment of nanomaterial used in nanomedicine. Introduction to the NanoTEST project. Nanotoxicology 9:5–12
Khan AU (2012) Nanodrugs: optimism for emerging trend of multidrug resistance. Int J Nanomedicine 7:4323–4324
Khutale GV, Casey A (2017) Synthesis and characterization of a multifunctional gold-doxorubicin nanoparticle system for pH triggered intracellular anticancer drug release. Eur J Pharm Biopharm 119:372–380
Kim YM, Park SC, Jang MK (2017) Targeted gene delivery of polyethyleneimine-grafted chitosan with RGD dendrimer peptide in alpha(v)beta(3) integrin-overexpressing tumor cells. Carbohydr Polym 174:1059–1068
Landarani-Isfahani A, Moghadam M, Mohammadi S, Royyaran M, Moshtael-Arani N, Rezaei S, Tangestaninejad S, Mirkhani V, Mohammadpoor-Baltork I (2017) Elegant pH-responsive nanovehicle for drug delivery based on triazine dendrimer modified magnetic nanoparticles. Langmuir 33(34):8503–8515
Lee W-H, Loo C-Y, Traini D, Young PM (2015) Inhalation of nanoparticle-based drug for lung cancer treatment: advantages and challenges. Asian J Pharm Sci 10(6):481–489. https://doi.org/10.1016/j.ajps.2015.08.009
Lee S, Son SJ, Song SJ, Ha TH, Choi JS (2017) Polyamidoamine (PAMAM) dendrimers modified with cathepsin-B cleavable oligopeptides for enhanced gene delivering. Polymers 9(6):224
Leyva-Gómez G, Piñón-Segundo E, Mendoza-Muñoz N, Zambrano-Zaragoza ML, Mendoza-Elvira S, Quintanar-Guerrero D (2018) Approaches in polymeric nanoparticles for vaginal drug delivery: a review of the state of the art. Int J Mol Sci 19(6):pii: E1549. https://doi.org/10.3390/ijms19061549
Liu J, Cui L, Losic D (2013) Graphene and graphene oxide as new nanocarriers for drug delivery applications. Acta Biomater 9(12):9243–9257
Liu J, Abshire C, Carry C, Sholl AB, Mandava SH, Datta A, Ranjan M, Callaghan C, Peralta DV, Williams KS, Lai WR, Abdel-Mageed AB, Tarr M, Lee BR (2017) Nanotechnology combined therapy: tyrosine kinase-bound gold nanorod and laser thermal ablation produce a synergistic higher treatment response of renal cell carcinoma in a murine model. BJU Int 119:342–348
Luque-Michel E, Imbuluzqueta E, Sebastian V, Blanco-Prieto MJ (2017) Clinical advances of nanocarrier-based cancer therapy and diagnostics. Expert Opin Drug Deliv 14(1):75–92
Mahmoudi M, Lynch I, Ejtehadi MR, Monopoli MP, Bombelli FB, Laurent S (2011) Protein-nanoparticle interactions: opportunities and challenges. Chem Rev 111:5610–5637
Marslin G, Selvakesavan RK, Franklin G, Sarmento B, Dias ACP (2015) Antimicrobial activity of cream incorporated with silver nanoparticles biosynthesized from Withania somnifera. Int J Nanomedicine 10:5955–5596
Martínez-Pérez B, Quintanar-Guerrero D, Tapia-Tapia M, Cisneros-Tamayo R, Zambrano-Zaragoza ML, Alcalá-Alcalá S, Mendoza-Muñoz N, Piñón-Segundo E (2018) Controlled-release biodegradable nanoparticles: from preparation to vaginal applications. Eur J Pharm Sci 115:185–195. https://doi.org/10.1016/j.ejps.2017.11.029
Masoudipour E, Kashanian S, Maleki N (2017) A targeted drug delivery system based on dopamine functionalized nano graphene oxide. Chem Phys Lett 668:56–63
Méndez-Rojas MA, Sánchez-Salas JL, Angulo-Molina A, Palacios-Hernández TJ (2014) Environmental risks of nanotechnology: evaluating the ecotoxicity of nanomaterials. In: Kharisov BI, Kharissova O, Dias RH (eds) Nanomaterials for environmental protection. Wiley, New York
Mendez-Rojas MA, Sanchez-Salas JL, Santillán-Urquiza E (2016) Nanotoxicology: toxicology of nanomaterials – the dawn of nanotoxicology. In: Kharisov BI, Kharissova OV, Ortiz-Méndez U (eds) CRC concise encyclopedia of nanotechnology. Taylor & Francis Group, Boca Raton
Milla P, Dosio F, Cattel L (2012) PEGylation of proteins and liposomes: a powerful and flexible strategy to improve the drug delivery. Curr Drug Metab 13(1):105–119
Min Y, Caster JM, Eblan MJ, Wang AZ (2015) Clinical translation of nanomedicine. Chem Rev 115(19):11147–11190. https://doi.org/10.1021/acs.chemrev.5b00116
Mohammadzadeh P, Cohan RA, Ghoreishi SM, Bitarafan-Rajabi A, Ardestani MS (2017) AS1411 aptamer-anionic linear globular dendrimer G2-lohexol selective nano-theranostics. Sci Rep 7:11832
Moreno-Sastre M, Pastor M, Salomon CJ, Esquisabel A, Pedraz JL (2015) Pulmonary drug delivery: a review on nanocarriers for antibacterial chemotherapy. J Antimicrob Chemother 70(11):2945–2955
Mostafalou S, Hamidreza M, Ali R, Abdollahi M (2013) Different biokinetics of nanomedicines linking to their toxicity; an overview. DARU J Pharm Sci 21:14–18
Naumenko EA, Dzamukova MR, Fakhrullina GI, Akhatova FS, Fakhrullin RF (2014) Nano-labelled cells – a functional tool in biomedical applications. Curr Opin Pharmacol 18:84–90
Nigam S, Bahadur D (2017) Dendrimer-conjugated iron oxide nanoparticles as stimuli-responsive drug carriers for thermally-activated chemotherapy of cancer. Colloids Surf B Biointerfaces 155:182–192
Oberdörster G, Oberdörster E, Oberdörster J (2005) Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ Health Perspect 113(7):823–839
Okholm AH, Kjems J (2016) DNA nanovehicles and the biological barriers. Adv Drug Deliv Rev 106:183–191
Onoue S, Yamada S, Chan HK (2014) Nanodrugs: pharmacokinetics and safety. Int J Nanomedicine 9:1025–1037
Palmer BC, DeLouise LA (2016) Nanoparticle enabled transdermal drug delivery systems for enhanced dose control and tissue targeting. Molecules 21(12):E1719. https://doi.org/10.3390/molecules21121719
Pastorino L, Dellacasa E, Dabiri MH, Fabiano B, Erokhina S (2016) Towards the fabrication of polyelectrolyte-based nanocapsules for bio-medical applications. Bionanoscience 6(4):496–501
Pescina S, Sonvico F, Santi P, Nicoli S (2015) Therapeutics and carriers: the dual role of proteins in nanoparticles for ocular delivery. Curr Top Med Chem 15(4):369–385
Petrenko VA, Jayanna PK (2014) Phage protein-targeted cancer nanomedicines. FEBS Lett 588(2):341–349
Puvvada N, Rajput S, Kumar BNP, Sarkar S, Konar S, Brunt KR, Rao RR, Mazumdar A, Das SK, Basu R, Fisher PB, Mandal M, Pathak A (2015) Novel ZnO hollow-nanocarriers containing paclitaxel targeting folate-receptors in a malignant pH-microenvironment for effective monitoring and promoting breast tumor regression. Sci Rep 5:11760
Raghunath A, Perumal E (2017) Metal oxide nanoparticles as antimicrobial agents: a promise for the future. Int J Antimicrob Agents 49(2):137–152
Ranjan AP, Mukerjee A, Gdowski A, Helson L, Bouchard A, Majeed M, Vishwanatha JK (2016) Curcumin-ER prolonged subcutaneous delivery for the treatment of non-small cell lung cancer. J Biomed Nanotechnol 12(4):679–688
Rigo LA, da Silva CR, de Oliverira SM, Cabreira TN, de Bona da Silva C, Ferreira J, Beck RC (2015) Nanoencapsulation of rice bran oil increases its protective effects against UVB radiation-induced skin injury in mice. Eur J Pharm Biopharm 93:11–17
Sachan NK, Bhattacharya A, Pushkar S, Mishra A (2009) Biopharmaceutical classification system: a strategic tool for oral drug delivery technology. Asian J Pharm 3(2):76–81
Saiyed MA, Patel RC, Patel SC (2011) Toxicology perspective of nanopharmaceuticals: a critical review. Int J Pharm Sci Nanotech 4(1):1287–1295
Salas-Rojas SG, Angulo-Molina A, Mendez-Rojas MA (2017) Farmacovigilancia de nanomedicamentos. In: Castro-Pastrana LI, Salas Rojas SG (eds) Retos actuales en farmacovigilancia: Una visión integral de los desafíos de la atención sanitaria. Editorial UDLAP, Puebla
Sasaki Y, Akiyoshi K (2010) Nanogel engineering for new nanobiomaterials: from chaperoning engineering to biomedical applications. Chem Rec 10(6):366–376
Sathler PC, Lourenco AL, Rodrigues CR, da Silva LCRP, Cabral LM, Jordao AK, Cunha AC, Vieira MCB, Ferreira VF, Carvalho-Pinto CE, Kang HC, Castro HC (2014) In vitro and in vivo analysis of the antithrombotic and toxicological profile of new antiplatelets N-acylhydrazone derivatives and development of nanosystems determination of novel NAH derivatives antiplatelet and nanotechnological approach. Thromb Res 134:376–383
Schmid D, Jarvis GE, Fay F, Small DM, Greene MK, Majkut J, Spence S, McLaughlin KM, McCloskey KD, Johnston PG, Kissenpfennig A, Longley DB, Scott CJ (2014) Nanoencapsulation of ABT-737 and camptothecin enhances their clinical potential through synergistic antitumor effects and reduction of systemic toxicity. Cell Death Dis 5:e1454
Seabra CL, Nunes C, Gomez-Lazaro M, Correia M, Machado JC, Gonçalves IC, Reis CA, Reis S, Martins MCL (2017) Docosahexaenoic acid loaded lipid nanoparticles with bactericidal activity against helicobacter pylori. Int J Pharm 519:128–137
Selen A, Dickinson PA, Müllertz A, Crison JR, Mistry HB, Cruañes MT, Martinez MN, Lennernäs H, Wigal TL, Swinney DC, Polli JE, Serajuddin ATM, Cook JA, Dressman JB (2014) The biopharmaceutics risk assessment roadmap for optimizing clinical drug product performance. J Pharm Sci 103(11):3377–3397
Sheikhpour M, Barani L, Kasaeian A (2017) Biomimetics in drug delivery systems: a critical review. J Control Release 253:97–109
Tahara K, Karasawa K, Onodera R, Takeuchi H (2017) Feasibility of drug delivery to the eye's posterior segment by topical instillation of PLGA nanoparticles. Asian J Pharm Sci 12(4):394–399
Tekade RK, Tekade M, Kesharwani P, D'Emanuele A (2016) RNAi-combined nano-chemotherapeutics to tackle resistant tumors. Drug Discov Today 21(11):1761–1774
Trembley JH, Unger GM, Korman VL, Abedin MJ, Nacusi LP, Vogel RI, Slaton JW, Kren BT, Ahmed K (2014) Tenfibgen ligand nanoencapsulation delivers bi-functional anti-CK2 RNAi oligomer to key sites for prostate cancer targeting using human xenograft tumors in mice. PLoS One 9:e109970
Tridente G (2014) Adverse events with biomedicines. Prevention through understanding. Springer, Milan
Vargas-Gonzalez BA, Castro Pastrana LI, Mendoza-Alvarez ME, Gonzalez-Rodriguez R, Coffer JL, Mendez-Rojas MA (2016) Hollow magnetic iron oxide nanoparticles as sodium meclofenamate drug delivering systems. J Nanomed Res 3(6):00071
Vazquez-Muñoz R, Borrego B, Juarez-Moreno K, Garcia-Garcia M, Mota Morales JD, Bogdanchikova N, Huerta-Saquero A (2017) Toxicity of silver nanoparticles in biológica systems: does the complexity of biological systems matter? Toxicol Lett 276:11–20
Ventola CL (2017) Progress in nanomedicine: approved and investigational nanodrugs. PT 42(12):742–755
Viswanath V, Santhakumar K (2017) Perspectives on dendritic architectures and their biological applications: from core to cell. J Photochem Photobiol B 173:61–83
Wang X, Wang S, Zhang Y (2016) Advance of the application of nano-controlled release system in ophthalmic drug delivery. Drug Deliv 23(8):2897–2901
WHO Drug Information (2016) A framework for risk-based identification of essential medicine products for local manufacturing in low- and middle-income countries. WHO Drug Inf 30(1):7–12
Willem de Vries J, Schnichels S, Hurst J, Strudel L, Gruszka A, Kwak M, Bartz-Schmidt KU, Spitzer MS, Herrmann A (2018) DNA nanoparticles for ophthalmic drug delivery. Biomaterials 157:98–106. https://doi.org/10.1016/j.biomaterials.2017.11.046
Xu Q, Kambhampati SP, Kannan RM (2013) Nanotechnology approaches for ocular drug delivery. Middle East Afr J Ophthalmol 20(1):26–37. https://doi.org/10.4103/0974-9233.106384
Yuan D, Yi X, Zhao Y et al (2017) Intranasal delivery of N-terminal modified leptin-pluronic conjugate for treatment of obesity. J Control Release 263:172–184
Zawawi NA, Majid ZA, Rashid NAA (2017) Adsorption and desorption of curcumin by poly(vinyl) alcohol-multiwalled carbon nanotubes (PVA-MWCNT). Colloid Polym Sci 295(10):1925–1936
Zhao M, Lei C, Yang Y, Bu X, Ma H, Gong H, Liu J, Fang X, Hu Z, Fang Q (2015) Abraxane, the nanoparticle formulation of paclitaxel can induce drug resistance by up-regulation of P-gp. PLoS One 10(7):e0131429. https://doi.org/10.1371/journal.pone.0131429
Zhou T, Su H, Dash P, Lin Z, Dyavar Shetty BL, Kocher T, Szlachetka A, Lamberty B, Fox HS, Poluektova L, Gorantla S, McMillan J, Gautam N, Mosley RL, Alnouti Y, Edagwa B, Gendelman HE (2018) Creation of a nanoformulated cabotegravir prodrug with improved antiretroviral profiles. Biomaterials 151:53–65. https://doi.org/10.1016/j.biomaterials.2017.10.023
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Castro-Pastrana, L.I., Angulo Molina, A., Flood-Garibay, J.A., Quintana-Romero, D.A., Crespo-Morán, P., Méndez-Rojas, M.Á. (2021). Recent Advances on Nanostructured Materials for Drug Delivery and Release. In: Yata, V., Ranjan, S., Dasgupta, N., Lichtfouse, E. (eds) Nanopharmaceuticals: Principles and Applications Vol. 2. Environmental Chemistry for a Sustainable World, vol 47. Springer, Cham. https://doi.org/10.1007/978-3-030-44921-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-44921-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-44920-9
Online ISBN: 978-3-030-44921-6
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)