Abstract
Medical education has evolved over many years with a shift in focus to include patient-centered clinical skills. Societal pressures and institutions in the House of Medicine gave more power to the voice of the patient. Pioneers such as Drs. Barrow and Stillman were among those visionaries who dreamed, experimented, and published findings about the use of standardized patients in simulated clinical encounters to teach and assess learners by means of a much more objective format. The adoption of SP methodology by licensure in North America broadened the methodology and soon all medical schools included SPs in curricula planning and implementation.
With the injection of simulation, a paradigm shift from lectured-based to practice-based teaching and assessment revolutionized medical education. Human simulation allowed learners to practice with individuals in a safe environment, to apply knowledge and skills in real time, have faculty observe how learners interact with a “patient,” and get direct individualized feedback on the performance of clinical skills.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Revolution
- SP methodology
- Paradigm shift
- Human simulation
- Pioneers
- Visionaries
- Simulated patient history
- Association of standardized patient educators
- History
- Timeline
Introduction
The introduction of simulation, the paradigm that shifted medical education from lecture-based to practice-based teaching and assessment of clinical skills, revolutionized the way in which medicine is taught. Human simulation allowed learners to practice on live individuals in a safe environment, to apply knowledge and skills in real time, have the faculty directly observe interactions with “patients,” and get direct individualized feedback on the performance of clinical skills. As a byproduct, simulation methodology allowed faculty to effectively develop gold standards for practice for each year of training and establish performance criteria for graduation. Many clinical teaching faculty look back 20 years and say, “how could that have NOT been a part of medical education?”
… Very much more time must be hereafter given to those practical portions of the examinations which afford the only true test of man’s fitness to enter the profession …
The day of the theoretical examinations is over. (Sir William Osler, MD 1885) [1]
Fundamental Change to American Medical Schools During the 20th Century
A question arises; should a music student only be allowed to touch a bow or put their hands on the keys of their instrument after they finish conservatory? Should music learners study theory yet not have their instructor observe and coach them on their performance? It seems counter-intuitive. So too does not putting one’s hands on a patient until you have almost completed medical school, or rarely if ever being observed working with patients and receiving constructive feedback.
Traditionally, medicine was taught in large lecture halls and heavily promoted the foundational sciences; students had little or no patient experience. There was little clinical instruction in undergraduate medical education. Rote memorization of copious amounts of information was regurgitated during non-standardized oral examinations; analogous to the music student who doesn’t touch an instrument until after they finish conservatory. However, unlike hitting a wrong note, physician error from lack of practice can have deadly consequences. Medicine like music, requires keen observation as well as continuous practice and constructive feedback for mastery of skills and the nuances of the “art”.
Movers and shakers in history are often not afraid to try something new which challenges the status quo, and true visionaries have the ability to imagine a different future. Abraham Flexner, a former schoolteacher and expert on educational practices and Sir William Osler, a notable physician and dean of the Johns Hopkins Medical School, are frequently cited as such visionaries [2].
Medical practice in the early 1900s had little oversight. “Physicians were primarily “learned gentlemen” in command of few effective practical skills” Medical education was informal, based on apprenticeships with no perscribed assessment of competencies or certifications. In most medical schools, there was a lack of uniformity to patient exposure and students could graduate without any hospital experience [3]. Standards in teaching were inconsistent, mainly due to the variability and lack of thoroughness of the faculty’s own training and teaching style. The Flexner report of 1910 dramatically transformed medical education across the United States. In collaboration with the American Medical Association (AMA) with support from the Carnegie Foundation whose objective was to restructure American medical education, Abraham Flexner a non medical educator, visited hundreds of medical institutions accross the US, Canada and Europe. His seminal report was influential in ending for – profit medical schools, the closure of a 3rd of the schools throughout the US and in setting standards and scholastic rigor in the establishment of a science-based curricular model. This however was almost to the exclusion of the patient as an active entity. This science-based model preticated on the German medical model, promoted “excellence in science but was not balanced by a comparable excellence in clinical caring.” [4] Flexner’s science and rigor in medicine overshadowed the art of medicine: patient-centered care using humanistic approaches.
One of Flexner’s greatest supporters in making this seminal change in medical education was also one of his staunchest critics. Sir William Osler understood the need to develop scientific knowledge, but his concern for the welfare of patients also influenced his teaching. His focus on a more humanistic approach in education included the need for direct observation of students and clinical practice with patients. At the end of the nineteenth century, Osler introduced the concept of grand rounds and restructured the curriculum at Johns Hopkins to include clinical observations in the amphitheater and patient experiences.
These two visionaries helped to overhaul medical education; Flexner by focusing on scientific rigor and setting standards, and Osler with and emphasis on student observation and clinical practice. Thomas P. Duffy a prominant Yale physician and humanist, reflecting back on 100 years after the Flexner report, observed, “We have learned that scientific medicine must travel linked to a professional ethos of caring that has been in place in our oaths and aspirations” [4].
Modern Influences on North American Medical Education
It takes about 30 years for a major change in medical education to occur. (Howard Barrows, 1975)
Fast forward to the early 1980s: the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) promoted the improvement of public health and medical education. These institutions assisted medical schools to adopt curricula to support earlier exposure to patient care and developing students’ clinical and communication skills. However, in the 1980’s and 90’s communication skills were considered part of the “art of medicine” or “soft skills,” something that was rarely taught in a formal way, and almost never assessed.
During the last decade, there was increasing evidence that effective doctor–patient communication produced “better health outcomes, better compliance and higher satisfaction of both doctor and patient” [5]. Much more attention was given to consensus efforts and reports such as one from the Toronto Consensus meeting in the early 1990s which stated, “sufficient data have now accumulated to prove that problems in doctor-patient communication are extremely common and adversely affect patient management” [6]. They concluded there was a “clear and urgent need for teaching of these clinical skills to be incorporated into medical school curriculums and continued into postgraduate training and courses in continuing medical education.” (p 1387) In 1995, the American Academy on Communication in Healthcare, whose mission is to improve communication and relationships between physicians and patients through educational initiatives, published its authoritative reference text, which covered clinical care, education, and research as an exposition of communication training for internal and family medicine. Due to these efforts, and more, communication training became part of the core principles when developing new medical curricula.
As medical education continued evolving, several other important societal initiatives occurred in North America. The American Hospital Association (AHA) revised the 1973 Patient Bill of Rights in 1992, outlining 12 provisions patients and their families should be provided in order to receive effective care in medical centers. These provisions focused on the interactions between health care professionals and patients ensuring respect, autonomy in decision-making, non-discrimination and sensitivity to gender, race, and religion [7]. Communication and interpersonal skills were at the core of these stipulations.
Another influence was the introduction of Direct to Consumer Patient Advertising (DTPCA) , started in the US in the 1980’s. By 2004, the Federal Drug Administration (FDA) relaxed regulations even more, allowing the sales pitch for pharmaceutical products direct to consumers with only major risks disclosed. Whether one agrees or not with DTCPA, some health care providers believed it fostered doctor-patient dialogue and adherence [8].
Technology, the internet, and television began to influence patient expectations and improve the ability to acquire medical knowledge impacting ones own healthcare. Patients were able to come to the physician’s office armed with information. No longer were they content to be a silent partner, but rather demanded a say in decision-making. The need to improve the communication and interpersonal skills to address the growing demand for information by patients became more evident.
In 1999, the Institute of Medicine released the report To Err Is Human: Building a Safer Health System, which exposed the state of medical errors, resulting in 44,000–98,000 unnecessary deaths in the US. The report outlined an agenda of actionable steps hospitals should implement mostly related to systems and market-based restrictions in need of reform. The report opened the public’s eyes to the need for improved or alternative ways of educating healthcare providers [9].
The Introduction of Human Simulation to Medical Education
Two names are prominent when talking about the development of SP methodology in North America; Howard Barrows MD, a neurologist, the “father of Simulated Patients” and Paula Stillman, MD, a pediatrician, who is credited for expanding the role of the SP.
It is a common misconception that SPs started as an instructional format and progressed to assessment. In fact, it was just the opposite. Barrows stated: “the impetus for this technique was produced by our need for better evaluation of the neurological performance of our clinical clerks who spent three weeks on the neurological services in recurring groups of six or seven students during their junior year” [9]. He wanted a fair, rigorous and reliable tool to observe and assess his neurology learners. He wanted a patient case in which he knew all the details that could be consistently reproduced for all his learners. Additionally, he needed an objective way to observe and record the learner’s performance.
Barrows attributes the creation of the SP-based technique to three factors coming together. The first was the impact of his mentor, Dr. David Seegal, and his dedication as a teacher. Seegal spent unheard of amounts of time observing and assessing medical students performing basic clinical skills with a patient. Seegal noted it was absurd that a medical student could graduate without basic skills being formally evaluated. The second factor was Sam, who contributed as a neurological patient who was recruited for the neurology board examination for several years. Over the course of those years, he became extremely knowledgeable about his physical findings. After one full day of examinations, Sam reported one candidate specifically had been rough, but he assured the examiners that “I got even with him: I changed my sensory loss and put my Babinski on the other side.” [10]. The final factor in Barrows’ conception of standardized patients was a woman who modeled for art students, Rose McWilliams. Barrows was filming clips of the neurological examination for his students when he met Rose, who enthusiastically posed as the model for the filming. She became very knowledgeable about the examination techniques and comfortable with the exam. Remembering Sam, Barrows trained Rose in the first simulated neurological case, multiple sclerosis.
During his time at the University of Southern California (USC), Barrows worked with another pioneer in medical education, Stephen Abrahamson, PhD, ScD. Abrahamson was developing one of the first medical education departments in the nation while Barrows was on faculty in the Department of Neurology. Both Abrahamson and Barrows had an innate interest in innovative teaching methods. While Barrows promoted the use of simulating a patient with a human being, Abrahamson saw the potential to use computer generated manikins to help medical school educators improve education and outcomes. His team helped develop Sim One, the first healthcare manikin. His idea that an anesthesia student could safely practise and learn from a computer programed manikin rather than a live patient was yet another milestone in the engaged practise of skill aquisition without the potential of causing irrevocable harm [11].
With the support of Abrahamson, Barrows nurtured the concept of “programmed patients.” However, at USC, Barrows met with such resistance from neurologists and medical educators, he left USC to a more supportive academic climate in Hamilton, Ontario, Canada. In 1969, he became a founding faculty member of a new medical school at McMaster University Faculty of Health Sciences. As a new medical school, McMaster University was the ideal setting for Barrows and his innovative and revolutionary ideas. Barrows pioneered a student-centered pedagogy called problem-based learning. Barrows saw the “simulated patient” teaching and research as integral to this new educational strategy and for life-long learning through the process of inquiry and constructivist learning.
Influenced by Barrows, Dr. Robert Kretzschmar, an Obstetrics and Gynecologist at the University of Iowa, developed the first gynecological teaching associate in 1968. He recruited women to teach the pelvic examination using their own bodies to instruct students on breast and pelvic examinations [12].
In the early 1970’s, Paula Stillman, M.D., was a pediatric clerkship director at the University of Arizona. She wanted a method that would allow her to teach and assess behaviors and techniques in both the content and the process of student medical interviews and one that would be conducive to providing feedback to the learners. Stillman recruited mothers to simulate stories for her learners. Using a checklist, her “simulated mothers” recorded learners’ interviewing skills and provided feedback on communication skills. Stillman was also tasked with finding a method for teaching accurate physical examination skills in the physical diagnosis course for her second year learners. Similar to Kretzschmar, she developed a comprehensive physical exam checklist and trained her first “patient instructors” to teach and assess a systematic physical exam using their own bodies [13].
Kretzschmar and Stillman’s ideas were indeed a huge revolutionary step: the use of lay people to help teach medical education. Not only were they using their bodies and voices to teach but they were now tasked with completing evaluation forms and providing immediate verbal feedback on clinical and communication skills. Most medical educators and physicians were skeptical this would prove to be beneficial, effective method for teaching and assessment. Little did they know the methodology would become a staple of medical education around the world.
Barrows and Stillman viewed medical education from two different perspectives. Barrows wanted to reform the traditional medical curriculum and looked for alternatives. He had an interest in abstract ideas about education and topics such as the clinical reasoning process, integrated cognitive learning, and practice-based experiences. He originally trained SPs from real patient stories and supported a patient-centered and holistic feedback structure. Stillman, on the other hand, wanted to improve traditional educational methods. She focused on teaching and assessment based on concrete processes, observable behaviors related to basic clinical skills, and learner competency. Stillman’s cases were composed of a collection of real patient stories, sometimes including some details from the simulated mothers’ own lives. She designed the first behaviorally anchored communication checklist as a basis for feedback training, known as the Arizona Clinical Interview Rating scale (ACIR) [14].
While Barrows and Stillman were introducing the SP in the United States, in 1975 Ronald Harden, M.D., a Scottish physician and educator, pioneered the Objective Structured Clinical Examination (OSCE) . Harden designed the OSCE as a timed multiple short-station assessment (between 5–10 minutes) that tested a learner’s ability to perform a single skill on a real patient (e.g. examine a shoulder), observed and scored by a faculty member using a checklist. Harden’s colleague, Ian Hart, M.D., was responsible for integrating SPs and the OSCE into specialty examinations at the Royal College of Canada [15].
In 1981, Barrows left McMaster and became the associate dean for education at Southern Illinois University School of Medicine (SIU). Continuing his interest in curriculum reform, in June 1984, Barrows and SIU faculty, in collaboration with Tom Meikle at the Josiah Macy Jr. Foundation, held a conference “How to Begin Reforming the Medical Curriculum”. This invitational conference allowed Barrows to showcase the value and flexibility of SP methodology with demonstrations of the SPs he had trained. At the end of the conference, recommendations were developed including the requirement of a performance-based examination for graduation. Reframing Harden’s OSCE format, Barrows expanded the complexity and scope of the assessment to the learner’s ability to demonstrate the complete range of clinical skills, depending on the presenting problem. Designed to assess the clinical performance of a learner in an actual patient encounter, a multi-station assessment with longer (15–20 minutes) stations was designed to assess taking a history, conducting a physical examination, and communication with the patient (providing patient education, discussing a management plan etc.). Post encounter exercises were paired with each encounter to further assess clinical reasoning and communication with members of the health care team. To distinguish this approach from the OSCE, he named it the Clinical Practice Examination (CPX) [16].
The Josiah Macy Jr. Foundation continued to support a number of demonstration projects, providing opportunities for Barrows to convince deans and associate deans of the benefits of working with SPs. One demonstration took place in the Professional Development Laboratory at SIU, a simulated clinic dedicated to teaching and assessment. His fully equipped simulated clinic became the model for other schools as SP programs grew and the need for clinic space dedicated to teaching and assessment became a reality. SIU introduced its first comprehensive multi-station examination using standardized patients to assess clinical skills in 1986.
Continuing its commitment to curriculum reform and SP methodology, the Josiah Macy Jr. Foundation in 1990 (based in New York City) awarded The Morchand Center for Clinical Competence housed at Mount Sinai School of Medicine a $250,000, 3 year grant for the establishment of a CPX exam. This successful collaboration, coupled with Dr. Meikle's enthusiastic endorsement contributed to the Foundation enbarking on the support of six more consortia accross the United States with each of them subsequently developing thier own CPX. These consortia, one in each region, allowed schools to create and share materials such as cases, assessment rubrics, collaborate on research and establish one simulation center for multiple institutions.
By 1996 The Josiah Macy Jr. Foundation, under the continued enthusiastic leadership of Tom Meikle, awarded $4.6 million in grants to develop and implement a SP-based Clinical Practice Examination (CPX) [17]. The Macy Foundation consortia had grown to include twenty-three medical schools and, in parallel, two independent consortia were formed: Stillman had started the New England Consortium and Reed Williams, PhD, a psychometrician and medical educator who had worked with Barrows at SIU, started the Chicago Clinical skills Consortium. The schools involved in these consortia represented almost one-third of the US medical schools focusing on developing a performance-based clinical assessment of their learners [16].
At SIU, Richard Reznick M.D. was working on his master’s in education when he met Barrows. Reznick’s research interests focused on assessment and technical skill acquisition. He became interested in SPs and OSCEs for national certification. Returning to Canada in 1993, he was instrumental in developing a performance-based examination for the Medical Council of Canada (MCC) . The MCC became the first organization to implement a national standardized patient-based examination as a required part of licensure [11].
Internationally, in the early 1980s, the introduction to and curriculum integration of SP methodology is credited to JJ Rethans M.D and Cees van der Vleuten PhD (Netherlands), David Newbie PhD (Australia) and Ron Harden and Ian Hart (UK) and documented in the medical education literature. This growth has continued globally in the expodential number of publications written over the years and discussed in detail in chapters 14 and 15 [18].
The AAMC and AMA demonstrated their interest in establishing the use of SP methodology in medical education through several events; the recommendations from the General Professional Education of the Physician and College Preparation for Medicine (GPEP) report, a directive to “develop a system of assessment which assures that learners have acquired and can demonstrate on direct observation the core clinical skills and behaviors needed in subsequent medical training” [19]. The AAMC sponsored the 1992 Consensus Conference on the Use of SPs in the Teaching and Evaluation of Clinical Skills. A total of five major reports focusing on the quality of undergraduate medical education, which were issued in the 1980s and the early 1990s – three by the AAMC, one by the AMA, and one by the Macy Foundation – commented on the need to improve the clinical skills education of medical students.
In 1989 and repeated in 1993, AAMC sent a survey on the “use of SPs” to 142 curriculum deans in the US and Canada. Deans from 138 schools reported an increase in the application of the SP methodology with SPs for teaching and evaluation from 94 schools in 1989 to 111 schools in 1993 with 39 working with SPs in a comprehensive examination to assess clinical skills before graduation [20].
Over the years, Barrows and Stillman’s approaches begin to intersect. Stillman was recruited by the ECFMG to set up four pilot sites to develop stations and assessment criteria. Two of these successful pilot sites were directed by several of Barrows’ colleagues; Drs. John Shatzer at Johns Hopkins and Jerry Colliver with Reed Williams at SIU. In 1994 under the leadership of Alton Sutnick, M.D., the Education Commission of Foreign Medical Graduates (ECFMG) authorized the Clinical Skills Assessment as part of its certification of international medical graduates with the help of Miriam ben Friedman, PhD, whose research advanced the field. Barrows’ influence extended to Daniel Klass, MD, whose work at the National Board of Medical Examiners (NBME) with the support of L. Thompson Bowles, MD, the president of the NBME, laid the groundwork for the use of SP-based assessments for the United States Medical Licensing Examination (USMLE) [11].
Several influential institutions were responsible for fueling the use of SP methodology at schools of medicine. In Canada and the US, the MCC, the NBME and the ECFMG identified the need to develop an assessment of competence other than multiple-choice question-based examinations to protect the health of the public through state-of-the-art evaluation methods. This assessment would focus on the demonstration of core abilities: the clinical skills of history-taking and physical examination, medical knowledge, and communication skills. While centered on assessment of physicians, the need for better methods of teaching and assessment impacted the spectrum of health professionals along the continuum of education, training and practice and included research in evaluation as well as development of assessment instruments. The introduction of SP-based clinical skills assessment for licensure found medical schools pressured by the students to prepare them for the examination; licensure has a profound impact on learning and curricula. Coupled with student pressure was schools own desire to have their classes excel and match at their medical institutions of choice. As a result, more dedicated simulation centers were built at schools of medicine across North America [20].
We would be remiss to omit the early contributions of psychometricians during the development of SP methodology: Geoffrey Norman, PhD, David B. Swanson, PhD, Jerry Colliver, PhD, Viet Vu, Phd, Jack Boulet, PhD, and Reed Williams, PhD. to name just a few. There has become a long list of medical eduation researchers who have redefined the methods of evaluation when it comes to the reliable and valid evaluation of the practice of medicine.
Through extensive research, these psychometricians reported on numerous aspects and applications of SP methodology. Their causiously optimistic conclusions on the evidence of the large and systematic knowledge base on SPs fueled more funding for large scale reliability and validity studies which assisted in the acceptance by medical educators and the licensing bodies. The overall body of work suggested, “medical educators should realize the benefits of the high-fidelity standardized approach provided by standardized-patient examination,” and noted “far less is known about the measurement properties of conventional procedures for clinical assessment in medical school courses and clerkships” [21].
In Barrows’ second book, Simulated (Standardized) Patients and Other Simulations, he noted SP methodology was found to be valuable for teaching and assessment in many fields and stated, “Therefore a more generic term ‘human simulations’ may be more appropriate”. He also credited Norman with the name change from Simulated Patient to Standardized Patient. Norman suggested the name change to promote the advantages of working with a patient case that was controlled and standardized versus the variability of working with actual patients in teaching and assessment [22].
The field of human simulation continues to mature, with the creation of standards of best practice by the International Nursing Association for Clinical Simulation and Learning (INACSL) and Association of Standardized Patient Educators (ASPE) [23] as well as certification processes focusing on ensuring pedagogical skills in the design, development and delivery of human simulation activities (Society for Simulation in Healthcare (SSH) – Certified Healthcare Simulation Educator) (CHSE).
ASPE – A Brief History of SP Educators
Throughout the 1990’s, a small group of Standardized Patient Educators (SPE) met at educational meetings such as the American Association of Medical Colleges (AAMC), the Canadian Association of Medical Education (CAME), Ottawa Conference, Association of Medical Education Europe (AMEE).
During 1991–1993, there were several developmental and sentinel meetings of SP Trainers for the purpose of establishing a professional network. The first was an invitational working group of SPEs who met in Niagara-on-the-Lake in Ontario, Canada to discuss ways of encouraging collaboration, sharing resources, and professional development for SPEs. The second meeting of the SP Trainers Group was again an invitational conference: “Standardized Patient Trainers Standard Setting Conference”, in Philadelphia, PA. The third meeting, in 1993, formalized SPEs’ interest in attending conferences specific SP methodology at the Calgary Conference: “Set the Standard.”
These early invitational meetings and conferences were successful in assessing the needs of the SPEs and interest in professional development. The successful attendance of SPEs to these pre-ASPE conferences was encouraging and supported the need for a formal organization. In 2001, a legal process to formalize the Association of Standardized Patient Educators (ASPE) was completed, and the first board of directors established, and initial meeting held in Little Rock, Arkansas. The foundational work since 1991 contributed to the successful introduction of ASPE in 2002. In 2003, ASPE’s 2nd Annual Conference was held in Virginia Beach, VA. The theme was, “Keys to Quality.” This was the first stand-alone, 3-day conference. All of the past ASPE conferences are listed on the ASPE website (aspeducators.org) [11].
Revolution
A paradigm shift is a fundamental change in the basic concepts and experimental practices of a scientific discipline. (Thomas Kuhn)
The introduction of human simulation into medical education was a paradigm shift. Simulation was a departure from the traditional, known, and comfortable. Kuhn, an American philosopher of science introduced in 1962 the term “paradigm shift.” His depiction of a paradigm shift takes place when an anomaly destabilizes traditional scientific practices causing a shift in shared beliefs and assumptions. At the beginning, simulation could be viewed as this anomaly in medical education. Kuhn noted how paradigm shifts and revolutions changed scientific beliefs and conceptions and ultimately world views. Kuhn stated, “during scientific revolutions, scientists see new and different things when looking with familiar instruments in places they have looked before” [24]. Kuhn identifies several steps in the evolutionary process for change to be considered a revolution (Table 3.1). These align with the process that took place in medical education with the introduction of human and computer-based simulation.
The reexamination of fundamental concepts and prior facts are demonstrated in the following “shifts” in medical education through the introduction of simulation:
Shift #1 – Mistakes are tolerated and can provide teachable moments
In a profession where the guiding principle is, “First do no harm,” it is not surprising that the norm is intolerance of error, mainly because of the devastating consequences of medical error. Yet “intolerance” is an austere environment in which to learn. Mistakes can provide great opportunity for growth, if the opportunity is used to extract a “teachable moment.” Simulation allows for planned teachable moments in a safe environment, where learners can make mistakes, but cannot harm “the patient” [25, 26].
Shift #2 – Constructive feedback is consistently and reliably provided to learners
Human simulation allows for the immediate delivery of written or verbal feedback to an individual learner or in a small group setting. Trained SPs and experienced faculty have demonstrated the ability to provide constructive, reliable and valid feedback and is one of the most effective means of solidifying skill acquisition [27]. Peers are expected to practice constructive feedback as well. This is now the norm throughout healthcare curricula throughout the US, Canada, Eurpope and a growing number of other countries. It can be difficult for learners to watch themselves and classmates during video reviews of their SP interactions. However, a process of facilitated reflection and skilled facilitated feedback with small groups allows for learners to grasp “best practices” from each other, observing comparable ways to improve performance [28]. Instead of faculty demonstrating how to do it “right,” they observe peer performance, learning from others’ errors as well as from examples of effectiveness, recognizing one does not always need years of practice to execute effective compassionate care.
Shift #3 – Self-reflection is a meaningful practice
Another benefit of simulation has been emphasis on self-reflection as part of acquiring life-long learning skills. Taking the time to self-reflect can lead to more effective skills and outcomes by evaluating one’s own thinking, process, and behaviors towards others. Asking important questions about personal experiences, motivations, beliefs, and intentions gives insight to understanding emotional responses, biases, and areas of strengths. Reflection has been found to have a positive impact on empathy, learning in complex situations, and participation in the learning process [29]. Reflection builds self-awareness, one of the key elements of Emotional Intelligence. Developing these skills early in training benefits learners when working with patients, in teams on the wards or in the Operating Room [30]. In simulation, self-reflection is an important component of the debriefing, main element of skill aquisition. There is an increasing interest and large body of work examining the role and effectiveness of debriefing in the learning process [31].
Shift #4 – Communication and interpersonal skills can be taught and evaluated
Human simulation and research have supported the teaching and evaluation of communication and interpersonal skills. Just like teaching someone how to take a blood pressure, one can also similarly break down active listening, and empathy into observable behaviors then effective feedback for improvement can be provided. Motivation for asking questions of patients is also tied directly to the ease and “genuineness” of the interaction. Having learners identify the appropriate “intention” by attributing it to the desired need for information from the patient such as when taking a sexual history, takes the focus off oneself and directs it onto their patient [30].
Shift #5 – Medical Education can be taught in an interactive, dynamic format
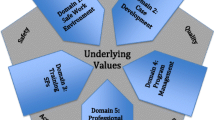
Reexamination of traditional, passive approaches to teaching has encouraged medical education to move towards participatory and experiential learning [31, 32]. Illustrated by the Learning Pyramid in Fig. 3.1, different styles of teaching or ways of obtaining information produce varying results. The learning pyramid shows the least and most optimal methods of retaining information using passive teaching methods (lectures, reading, audiovisual, demonstration) versus participatory teaching methods (discussion, practice, teaching). Although these exact percentages have been refuted, it is the bigger picture which is important - when we are engaged with our mind and body in a meaningful, challenging process via an interaction, that learning experience will be more readily retained [33].
Human simulation incorporates elements from theater, video technology, psychology, sociology, anthropology and virtual reality; and by doing so has created the opportunity for tremendous innovation in experiential teaching [34].
Shift #6 – Graduation from medical school and obtaining licensure in the US and Canadian require multiple methods of assessment
For decades, medical schools used oral or multiple choice question-based assessments (MCQs) to evaluate clinical competencies including knowledge and critical thinking despite research questioning face validity (MCQs), poor content validity and inconsistency, subjectiveness, and the potential for bias with variations in examiner differences (oral examinations) [35].
Since a single method of assessment cannot capture the multiple layers and aspects of clinical competency, multiple assessment methods are required. The NBME, for example, expanded the format of single question MCQs to include sequential MCQs, the use of vignettes to assess critical thinking skills, computer case-based assessment to assess patient management, and introduced standardized patients in their licensure assessments [36, 37]. The introduction of SP-based assessments for licensure in North American, unlike oral examinations, allowed for the control of case content, case portrayal and immediate, standardized direct observed assessment. Because the details of the case are known, evaluation rubrics can be controlled , monitored, and adjusted as needed [38].
Furthermore, the Liaison Committee on Medical Education (LCME) is the U.S. Department of Education recognized accrediting body for programs leading to the MD degree in the United States also promotes the use of a variety of assessment methods. It also accredits MD programs in Canada, in cooperation with the Committee on Accreditation of Canadian Medical Schools (CACMS). The LCME is jointly sponsored by the AAMC and the AMA and publishes the standards MD programs must follow in order to attain accreditation, The standards state MD programs must demonstrate, “The systematic use of a variety of methods to collect, analyze, and use information to determine whether a medical student has acquired the competencies (e.g., knowledge, skills, behaviors, and attitudes) that the profession and the public expect of a physician. (Element 1.4)” [39].
Conclusion
The word revolution is derived from the Latin word revolutio which means “a turn-around.” Modern use of the word equates to violent change such as a revolt or overthrow. Human simulation certainly did not overthrow any institutional leadership or produce demonstrations or armed revolts on medical school campuses. However, through ingenuity, steady practice, incremental changes, and copious research, SP methodology managed to greatly shift the clinical skills curricula of every medical school in North America and numerous others around the globe. It has been a continuous movement over the last three decades, leading to changes in the way we teach, evaluate, and ultimately practice the art of medicine.
In the end, as Thomas Kuhn said “The answers you get depend upon the questions you ask.”
Those of us in the simulation field understand the “right” question at an opportune moment, can make all the difference and lead to positive change. The next enterprise in this journey of human simulation in medicine will depend upon the ingenuity, creativity, boldness, timeliness and applicability to the communities in which we serve [40].
See Appendix 3.1 for a timeline of milestones in the history of the SP methodology and standardized patient educator.
Abbreviations
- AAMC:
-
Association of American Medical Colleges
- ACIR:
-
Arizona Clinical Interview Rating scale
- AHA:
-
American Hospital Association
- AMA:
-
American Medical Association
- AMEE:
-
Association of Medical Education Europe
- ASPE:
-
Association of Standardized Patient Educators
- CACMS:
-
Committee on Accreditation of Canadian Medical Schools
- CAME:
-
Canadian Association of Medical Education
- CHSE:
-
Certified Healthcare Simulation Educator
- CPX:
-
Clinical Practice Examination
- DTCA:
-
Direct to Consumer Advertising
- ECFMG:
-
Education Commission of Foreign Medical Graduates
- FDA:
-
Federal Drug Administration
- GPEP:
-
General Professional Education of the Physician and College Preparation for Medicine
- INACSL:
-
International Nursing Association for Clinical Simulation and Learning
- LCME:
-
Liaison Committee on Medical Education
- MCC:
-
Medical Council of Canada
- MCQ:
-
multiple choice question
- NBME:
-
National Board of Medical Examiners
- OSCE:
-
Objective Structured Clinical Examination
- SIU:
-
Southern Illinois University School of Medicine
- SPE:
-
Standardized Patient Educators
- SSH:
-
Society for Simulation in Healthcare
- USC:
-
University of Southern California
- USMLE:
-
United States Medical Licensing Examination
References
Weitz HH. Sir William Osler: Would He Have Made His Relative Value Units (RVUs)?. Ann Intern Med. 2019;171:208–209. [Epub ahead of print 2 July 2019]. https://doi.org/10.7326/M19-0665.
Dornan T. Osler, flexner, apprenticeship and ‘the new medical education’ Journal of the Royal Society of Med. Vol. 98 March 2005.
Custers Eugène JFM, ten Cate O. The History of Medical Education in Europe and the United States, With Respect to Time and Proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49–S54. https://doi.org/10.1097/ACM.0000000000002079.
Duffy TP. The Flexner Report — 100 Years Later. Yale J Biol Med. 2011;84(3):269–76. Published online 2011 Sep. PMCID: PMC3178858 PMID: 21966046.
Deveugele M, Derese A, De Maesschalck S, Willems S, Van Driel M, De Maeseneer J. Teaching communication skills to medical students, a challenge in the curriculum? Patient Educ Couns. 2005;58:265–70.
Simpson M, Buckman R, Stewart M, Maguire P, Lipkin M, Novack D, et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303(6814):1385–7.
AHA Patient’s Bill of Rights. American Patient Rights Association. https://www.americanpatient.org/aha-patients-bill-of-rights/.
Ventola CL. Direct-to-consumer pharmaceutical advertising: therapeutic or toxic? P T. 2011;36(10):669–84. PubMed PMID: 22346300; PubMed Central PMCID: PMC3278148.
Institute of Medicine (US) Committee on Quality of Health Care in America, Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US); 2000.
Barrows HS. Introduction, simulated patients (programmed patients). Springfield: Charles C Thomas; 1971.
Wallace P. Following the threads of an innovation; the history of standardized patient in medical education. Caduceus. 1997;13(2):5–28.
Kretzschmar RM. Evolution of the Gynecology Teaching Associate: An education specialist. American Journal of Obstetrics and Gynecology 1978;131(4):367–73.
Stillman PL, Sabers DL, Redfield DL. The use of paraprofessionals to teach interviewing skills. Prediatrics 1975;57:769–74.
Stillman P, Brown DR. Redfield DL, Sabers DL. Construct validation of the Arizona clinical interview rating scale. Educ Psych Measure. 1997;37:1031–8.
Harden RM, Lilly P, Patricio M. The definitive guide to the OSCE: the objective structured clinical examination as a performance assessment. Elsevier, 2016;13–23.
Barrows HS. Session One, An Overview of the Uses of Standardized Patients for the Teaching and Evaluation of Clinical Skills, Academic Medicine 1993;68(6).
Tudico C, Thibault GE. The History of the Josiah Macy Jr. Foundation; New York: Josiah Macy Jr. Foundation; 2012.
Bokken, L et al. Strengths and weaknesses of simulated and real patients in the Teaching of Skills to Medical Students: A Review (Sim Healthcare 2008;3:161–9.).
Corbett EC, Jr. Whitcomb M. The AAMC project on the clinical education of medical students clinical skills education. Association of American Medical Colleges Copyright 2004.AAMC 2450 N Street, NW Washington, DC 20037–1127; 2004. https://www.aamc.org/download/68526/data/clinicalskillscorbett.pdf.
Colliver J, Williams RG. Technical issues: test application AAMC. Acad Med. 1993;68(6):454–60. discussion 61–3.
Barrows HS. Simulated (standardized) patients and other simulations. Chapel Hill: Health Sciences Consortium; 1987.
Committee IS. INACSL standards of best practice: simulation SM simulation design. Clin Simul Nurs. 2016; 12S5–S12.
Kuhn T. The structure of scientific revolutions 3rdEdition. 3rd ed. Chicago, London: University of Chicago Press; 1996.
Al-Elq AH. Simulation-based medical teaching and learning. J Family Community Med. 2010;17(1):35–40. https://doi.org/10.4103/1319-1683.68787.
Higham H, Baxendale B. To err is human: use of simulation to enhance training and patient safety in anesthesia, British Journal of Anesthesia, 2017;119(S1):i106–i114.
Howley LD, Martindale J. The efficacy of standardized patient feedback in clinical teaching. Med.Educ Online 2004;9:18. A mixed method analysis Available form http://www.med-ed-online.org.
Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc. 2007;2(2):115-25.
Winkel AF, Yingling S, Jones AA, Nicholson J. Reflection as a learning tool in graduate medical education: a systematic review. J Grad Med Educ. 2017;9:430–9.
Johnson DR. Emotional intelligence as a crucial component to medical education. Int J Med Educ. 2015;6:179–83. ISSN:2042–6372. https://doi.org/10.5116/ijme.5654.3044.
Bejjani J. Emotional intelligence; use in medical education and practice. McGill J Med. 2009;12(2):4.
King A, Hoppe R. “Best practice” for patient-centered communication: a narrative review. J Grad Med Educ. 2013;5(3):385–93. https://doi.org/10.4300/JGME-D-13-00072.1.
Hoppe RB, King AM, Mazor Furman GE, Wick-Garcia P, Corcoran-Ponisciak H, Katsufrakis PJ. Enhancement of the assessment of physician–patient communication skills in the United States Medical Licensing Examination. Acad Med. 2013;88:1670–5.
Masters K, Dale E. Pyramid of Learning in medical education: A literature review, Medical Teacher, 2013;35:11, e1584–e1593.
Alda A. If I understood you, would I have this look on my face? my adventures in the art and science of relating and communicating. New York: Random House; 2017.
Tabish SA. Assessment methods in medical education. Int J Health Sci (Qassim). 2008;2(2):3–7. PMCID: PMC3068728.
Hoffman K. II: The USLME, the NBME, subject examinations, and assessment of individual academic achievement. Acad. Med. 68:10. 1993.
Edelstein RA, Reid HM, Usatine R, Wilkes MS. A comparative study of measures to evaluate medical students’ performances. Acad Med. 2000;75;8:825–33.
Motola I, Devine LA, Chung HS, Sullivan JE, Issenberg B. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Med Teach. 2013;35(10):e1511–30. https://doi.org/10.3109/0142159X.2013.818632.
Functions and structure of a medical school. Standards for accreditation of medical education programs leading to the MD Degree. Published March 2020 For surveys in the 2021–22 academic year standards and elements effective July 1, 2021. LCME Secretariat Association of American Medical Colleges Washington, DC.
Satava R. The revolution in medical education-the role of simulation. J Grad Med Educ. 2009;1(2):172–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix 3.1 Timeline and Intersections
Appendix 3.1 Timeline and Intersections
Milestones in the History of the SP Methodology and the Standardized Patient Educator
1960s
- 1963:
-
First trained patient – called Programmed Patient at USC (H.S. Barrows)
- 1964:
-
First publication in the Journal of Medical Education: “The Programmed Patient: A technique for Appraising Student Performance in Clinical Neurology” (H.S. Barrows)
1970s
- 1971:
-
First book on SPs published: Simulated Patients (Programmed Patients by H.S. Barrows
Name change from “Programmed Patient” to “Simulated Patient”
- 1972:
-
Expansion of the GTA role to include teaching communication skills related to the pelvic examination. (Kretzschmar)
- 1973:
-
“Patient Instructors” introduced. Teaching Physical Examination Techniques by P. Stillman published
- 1975:
-
First article on OSCEs published: “Assessment of clinical competence using objective structured examination.” by R. Harden
1980s
Exact date unknown: Name change from “Simulated Patient” to “Standardized Patient” (G. Norman)
- 1984:
-
Macy Foundation Invitational conference on curriculum reform. SPs were introduced to medical schools throughout the country as a valuable tool for individual student assessment and a means for curricular change in medical education. (H.S. Barrows, Josiah Macy Jr. Foundation)
First multi-station demonstration with SP-based stations (H.S. Barrows)
- 1987:
-
Second Book on SPs published: Simulated (Standardized) Patients and Other Human Simulations” by H.S. Barrows
- 1989:
-
AAMC Survey of 142 curriculum deans in the US and Canada was conducted. 94 of the 136 deans responded indicated that working with SPs were integrated in various ways including teaching the breast, pelvic and male GU and teaching and assessing history taking and the physical examination, patient education and counseling and interviewing skills. Nearly a third of the schools (39) had a central office that coordinates the school’s SP Program
ECFMG vice president Alton Sutnick established a working group to develop a SP-based performance assessment: Howard Barrows, Paula Stillman, Ian Hart
SPEs met randomly at educational meetings such as the American Association of Medical Colleges (AAMC), the Canadian Association of Medical Education (CAME), Ottawa Conference, Association of Medical Education Europe (AMEE)
1990s
- 1991:
-
A survey was sent out to medical schools and SPEs in Canada and the United States exploring interest in a professional development forum. The response rate was overwhelmingly positive.
Invitational meeting held in Toronto Ontario Canada for SP Trainers. A working group of SP trainers met to discuss ways of encouraging resource and professional development for SP trainers. Five international trainers attended.
At the annual American Association of Medical Colleges (AAMC) conference, an informal SP Trainers Caucus was held. Fourteen SPEs attended.
AAMC tasked Dr. Paula Stillman to assess interest in a Special Interest Group (SIG) on Standardized Patients. Twenty-one individuals were invited to present their work on SPs.
Invitational Symposium held at Niagara-on-the-Lake, Ontario Canada: “SP Trainers – A First meeting.” Fourteen participants from diverse backgrounds had much to offer from their respective fields: visual and performing arts, social work and nursing, education and research. (NBME & MCC)
- 1992:
-
The Medical Council of Canada (MCC) developed a licensing examination using with SP-based stations as part of the Medical Council of Canada Qualifying Examination (MCCQE) to assess knowledge, skills and attitudes essential for medical licensure in Canada prior to entry into independent clinical practice.
NBME starts Research on SP-based methods of assessing clinical skills needed for entry into supervised practice.
AAMC SIG on SPs: Call-out to Deans of all AAMC medical schools to introduce the SP SIG and identify those interested in working with SPs. Call for Abstracts started.
SP Educators:
-
Workshop at the Canadian Association for Medical Education (CAEM) - invited presenters with a business meeting at the end of the workshop to query about a professional society.
-
Innovation in Medical Education (IME) Poster exhibit at AAMC and Booth: “Standardized Patient Trainers: Directions for the Future.” Reception/Open House held at the IME meeting to promote SP Trainer Association
-
One Day SP Trainer Lagniappe Caucus, New Orleans LA held prior to AAMC. First meeting to require a registration fee ($20.00)
AAMC consensus conference on the Use of Standardized Patients in Teaching and Evaluation of Clinical Skills. (163 Attendees)
AAMC repeats the 1989 SP Survey. The use of SPs reported by 111 medical schools. Thirty nine of the 111 required learners to take an examination before graduation which involved SPs
- 1993:
-
AAMC Consensus Meeting held in Washington DC
AAMC Group on Educational Affairs assigned Paula Stillman to formally establish a Standardized Patient - Special Interest Group. Target audience: people with an interest in advancing the SP methodology where members communicate, collaborate and meet to promote research, and identify solutions within their particular area. The membership is responsible for ensuring the ongoing activities of the group. Approximately 30–40 attended
Sentinel publication: “Special Issue of the Proceedings of the AAMC’s Consensus Conference on the Use of Standardized Patient in the Teaching and Evaluation of Clinical Skills”. Academic Medicine and Teaching & Learning in Medicine. Gave the community a basis for future work.
SP Trainers Calgary Conference: “Set the Standard,” 44 attendees
- 1994:
-
Second meeting of the SP Trainers Group; Invitational Conference – “Standardized Patient Trainers Standard Setting Conference”, Philadelphia PA. Overall objectives: develop a consensus document on the standards for SP training. Specific issues addressed included the knowledge, attitudes, and skills required to train a SP to simulate a history, a physical and/or a patient education encounter. Invitees explored the requirements for each of these types of encounters for both teaching and assessment for different levels of medical learners. 17 attendees.
- 1995:
-
AAMC SIG on SPs
-
Call for Abstracts continued
-
Steering Committee established for the National Special Interest Group on Standardized Patients
-
First SP Trainer Directory published and distributed by NBME
- 1996:
-
AAMC SIG on SPs
-
Call for Abstracts
-
The SP Trainer Listserv was established by Jennie Struijk, University of Washington. This listserv was instrumental in promoting communication between SPEs and helped to accomplish the goals of networking.
-
Second SP Trainer Directory published and distributed by NBME
- 1997:
-
September: Standardized Patient Educators Conference: “Thinking Outside the Box,” Little Rock, Arkansas with 49 Attendees. The keynote speaker was M. Joycelyn Elders, MD, Former U.S. Surgeon General. First use of “Standardized Patient Educators” in conference title
- 1997–99:
-
AAMC SP SIG continues to grow
-
Call for Abstracts see growth in submissions
-
Presentations with end of meeting Professional development discussions
-
Attendance continues to grow
- 1998:
-
AAMC created the first SP Educator of the year award – “Award for Excellence in the Field of Standardized Patient Education”
The Educational Commission for Foreign Medical Graduates (ECFMG) introduces a SP assessment for all foreign medical graduates. Helped many institutions get started to pilot SP-based assessments.
- 1999:
-
AAMC SP SIG Theme: “Collaborating in the Use of SPs: Models from Business, Research, Inter-Institutional and Inter-Departmental”
-
Call for Abstracts
-
Approx. 100 people attended (standing room only)
Regional Groups on Educational Affairs created SP-Special Interest Groups (CGEA).
2000s
- 2000:
-
AAMC gives notification to disband all SIGs, including the SP SIG. Final SP SIG Theme: “Demonstrating the Value of your SP Program.” The goal of the SP SIG was to develop and nurture a community with common interests in advancing the use of SP methodology, promote research and integrate presentations within the AAMC conference. Our goals were accomplished.
Standardized Patient Educators Conference held in Galveston, Texas, “New Horizons for SP Educators.” The 3-day conference had 150 SPE attend.
-
The first SP online casebook was presented, later folded into the ASPE website and through many iterations, is now part of the Virtual Resource Library
- 2001:
-
ASPE: Final Legal/Formal Process for an SPE Association
First board of directors meeting held in Little Rock, Arkansas.
- 2002:
-
ASPE:
-
The first ASPE website domain (http://www.aspeducators.org) was established
-
ASPE website went “live”
-
ASPE Inaugural Conference was held in conjunction with the Ottawa Conference in Ottawa, Ontario. The theme was, “Advancing the Practice.” The one day conference had 71 attendees.
-
First ASPE logo created
-
ASPE Quarterly newsletter established
- 2003:
-
The Association Council of Graduate Medical Education (ACGME) supports SP methodology for several of the six required competencies.
ASPE 2nd Annual Conference was held in Virginia Beach, Virginia. The theme was, “Keys to Quality.” The first stand-alone, 3-day conference had 163 attendees.
- 2004:
-
The United States Medical Licensing Examination (USMLE) sponsored by the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners (NBME) began using SP methodology in the Step 2 Clinical Skills Examination to assess history-taking, physical examination, communication skills and spoken English proficiency.
- 2017:
-
ASPE Standards of Best Practices was published. ASPE logo updated.
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cohen-Tigor, D., Gliva-McConvey, G. (2020). How a Revolution Took Hold – The Standardized Patient Methodology. In: Gliva-McConvey, G., Nicholas, C.F., Clark, L. (eds) Comprehensive Healthcare Simulation: Implementing Best Practices in Standardized Patient Methodology. Comprehensive Healthcare Simulation. Springer, Cham. https://doi.org/10.1007/978-3-030-43826-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-43826-5_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43825-8
Online ISBN: 978-3-030-43826-5
eBook Packages: MedicineMedicine (R0)