Abstract
Since the introduction of noninvasive transcranial brain stimulation techniques decades ago, these tools have been applied in both basic and clinical research, with the aims to enhance knowledge about the pathophysiology as well as to develop new treatment options for neurological and psychiatric diseases. In this chapter, we describe the implementation of these techniques to monitor and modulate neurophysiological processes in the human brain, which enables a better understanding of disease-related pathophysiology, and the development of therapeutic interventions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- NIBS
- TMS
- tDCS
- tACS
- Cortical excitability
- Network connectivity
- Neuroplasticity
- Neurological disease
- Psychiatric disease
1 Introduction
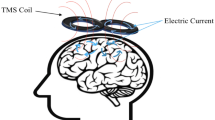
To understand the foundation of central nervous system diseases in humans, the exploration of human brain physiology is of utmost importance. In the last 40 years, numerous tools that allow the exploration of respective mechanisms in health and disease have been developed. Two main groups of tools are neuroimaging and noninvasive brain stimulation (NIBS) approaches. Neuroimaging allows to identify areas activated during psychological and behavioral processes, including not only regional but also network activations, as well as process-related alterations of transmitter and neuromodulator systems. Noninvasive brain stimulation has been developed based on the findings that sufficiently strong electrical stimulation over the scalp is able to activate cortical neurons [1]. Based on these initial findings, numerous tools have been developed, which enable not only global activation of specific target areas but also monitoring the central nervous system conduction time, activation of cortical subsystems defined by neurotransmitters and modulators, and network activation. Because of these specific functions and the high spatial and temporal specificity of some protocols, NIBS allows revealing aspects of human brain physiology, which we cannot obtain by functional imaging alone. Furthermore, brain stimulation approaches are able to modulate task-related cerebral activity. This allows for deriving causal relations about the involvement of specific physiological activity during psychological and behavioral processes, based on intervention-dependent performance alterations. In addition, based on respective alterations, therapeutic interventions have been developed, which aim to counteract pathologically altered cortical activity, neuroplasticity, and oscillatory activity. Some of these interventions, e.g., repetitive transcranial magnetic stimulation (rTMS), have already been approved for routine clinical treatment of psychiatric disorders, while others may also soon reach approval. In this chapter, we provide an overview of the main NIBS tools available at present, which are transcranial magnetic stimulation (TMS) and transcranial electrical stimulation (tES), and discuss their application as a research tool for understanding cognition and behavior, and their potential for treating diseases of the brain. This includes exploration of disease-relevant pathological alterations of brain physiology. Improving the knowledge in this field not only enhances our mechanistic understanding but may also lead to the identification of biomarkers for a specific disease, or therapeutic progress, and thereby guide individualization of therapeutic approaches in the future. Moreover, with both TMS and tES approaches, it is possible to generate plasticity in the human brain. As such, these tools allow us not only to identify plasticity-related pathological alterations in central nervous system diseases, but also to counteract pathological alterations in respective diseases. In the last part of this chapter, we will give examples of how these tools can be used to improve comprehension of disease-specific pathophysiology, and based on this, to develop therapeutic approaches. Finally, we will give a short overview of future developments in the field, which might help to further improve the utility of NIBS.
2 Using NIBS to Monitor Brain Physiology
For the exploration of human brain physiology, NIBS is used to study cortical excitability, cerebral connectivity, and neuroplasticity. These methods help to clarify the physiological foundation of cognitive processes and behavior and are also relevant to identify pathological alterations in clinical syndromes, and mechanistic effects of interventions dedicated to reducing clinical symptoms. In the following, we refer primarily to protocols relevant to psychological and behavioral processes. For determination of central conduction time, mapping procedures, and related protocols, which are relevant for clinical diagnostics of neurological diseases, refer to the respective literature [2].
2.1 Monitoring Cortical Excitability by NIBS
For the exploration of cerebral excitability, TMS is the main stimulation paradigm used for application in humans. Numerous TMS protocols have been developed, including single- and double-pulse stimulation of cerebral target regions, as well as peripheral–central stimulus combinations, to explore the functional state of cortical, corticocortical, and corticospinal pathways. These protocols also allow for a more detailed understanding of the specific functionality of pharmacologically defined subsystems. TMS alone can probe the reactivity of the motor and visual cortex, and when coupled with other neuroimaging techniques such as electroencephalography (EEG), can be used to assess the response of other cortical targets as well. Respective measures are valuable for the identification of neurophysiological and pathophysiological aspects of CNS diseases, and for the exploration of disease dynamics, including the impact of interventions. Thus, TMS-based monitoring approaches, which we describe below, may be powerful co-adjuvants for the early diagnosis and grading of diseases.
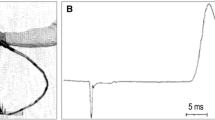
Motor Threshold (MT), Motor Evoked Potential (MEP) amplitude and latency, and the recruitment curve are the main protocols to investigate corticospinal excitability by TMS. MT is a summated index of neuronal membrane excitability of corticospinal neurons, the interneurons projecting onto these neurons along the corticospinal tract, as well as the excitability of motor neurons in the spinal cord, neuromuscular junctions, and muscles [3]. MT is increased by drugs that block voltage-gated sodium channels in the motor cortex but is not altered by the block of glutamatergic or enhancement of GABAergic activity [4]. Thus, MT reflects mainly neuronal membrane, but not synaptic, excitability. The electromyographic amplitude of MEP responses elicited by suprathreshold single-pulse TMS reflects the excitability of motor cortex neurons, the integrity of the corticospinal tract, and conduction along the peripheral motor pathway to the muscles. Here, the recruitment curve describes the sigmoidal input–output properties of the corticospinal system. MEPs elicited by low TMS intensities—similar to MT—reflect primarily neuronal membrane excitability, whereas larger MEPs generated by higher TMS intensities are also partially controlled by glutamatergic synaptic effects [5].
Additional protocols have also been developed for detecting more specific alterations of cortical excitability. The Cortical Silent Period (CSP), Short-Latency Afferent Inhibition (SAI), Short-Latency Intracortical Inhibition (SICI), Long-Interval Intracortical Inhibition (LICI), and I-wave facilitation are neurophysiological measures, which assess intracortical inhibitory processes. CSP refers to a temporary suppression of ongoing electromyographic activity in an active muscle caused by a TMS pulse. It mainly originates from inhibitory mechanisms at the level of the motor cortex and is mediated by GABAA and GABAB receptors in low- and high-stimulus intensities, respectively [4]. SAI is obtained by combination of a peripheral electrical stimulus of a mixed nerve with a subsequent TMS pulse over the motor cortex. Within specific interstimulus intervals, the peripheral nerve stimulus has an inhibitory effect on the TMS-elicited MEP, which is controlled by GABAA receptors and central cholinergic transmission [6]. SICI reflects the inhibitory effect of a subthreshold TMS pulse on the MEP amplitude generated by a subsequent suprathreshold TMS pulse, which is observed at interstimulus intervals (ISIs) between 1 and 6 ms. It is primarily controlled by GABAA receptors but also affected by glutamatergic and dopaminergic systems [4, 7]. LICI is tested by application of two suprathreshold TMS pulses with ISIs of 20–300 ms and controlled by GABAB receptors [8]. Another suprathreshold/subthreshold paired-pulse TMS paradigm to assess intracortical excitability is I-wave facilitation. I-waves or indirect waves are repetitive discharges of corticospinal fibers elicited by a suprathreshold TMS pulse over the motor cortex. I-wave facilitation is attributed to intracortical interactions between circuits responsible for the production of these waves, and depends on GABAA-related neuronal circuits, with later I-waves being more affected by intracortical inhibition than early ones [9, 10].
At the intracortical level, beyond inhibitory mechanisms, facilitation can also be probed by combination of a subthreshold TMS conditioning pulse with a suprathreshold test pulse. For interstimulus intervals of 7–20 ms, the conditioning pulse enhances MEP amplitudes evoked by the test pulse (intracortical facilitation (ICF)), which is primarily controlled by the glutamatergic system [4].
Beyond monitoring motor cortex excitability through TMS, specific protocols have also been developed for probing excitability of other brain areas. Visual cortex excitability can be probed by the TMS threshold for the generation of phosphenes, which are light flashes perceived, in this case, by application of TMS over the respective target area. Furthermore, integration of TMS with neuroimaging techniques such as EEG extends TMS excitability measures to additional cortical regions. Single- and paired-pulse TMS protocols have been integrated into TMS-EEG paradigms to study excitation/inhibition mechanisms at the cortical level in both motor and nonmotor areas. The combination of TMS with EEG has identified novel and useful measures of evoked activity that index inhibitory (e.g., GABAergic) and excitatory neurotransmission (see [11] for a review). LICI-related inhibition of cortical evoked activity, for instance, has been identified for DLPFC and parietal TMS-EEG protocols and is associated with GABA-B receptor activity in these areas [12, 13]. In contrast, the amplitudes of the P30 and P60 components of TEPs were reduced by SICI and increased by ICF protocols in both M1 and DLPFC stimulation, which suggests a dependency of these TEP components from GABAergic and glutamatergic synaptic mechanisms [14]. Considering the ability of paired-pulse TMS-EEG protocols to obtain neurophysiological readouts for nonmotor regions, they might also be suited to characterize healthy versus pathological brain states of these regions and introduce novel electrophysiological diagnostic and prognostic markers in clinical populations.
One relevant limitation of the abovementioned TMS-derived measures is the appreciable level of the observed variability of most of them, which is caused by various biological and methodological factors. This variability compromises the reliability of TMS-derived neurophysiological markers, especially at the level of the individual, which, in addition to difficulties in defining normative values, challenges their use as standard diagnostic protocols. Further studies are required to enhance the sensitivity and specificity of these metrics to translate them into clinical applications.
2.2 Monitoring Network Connectivity by NIBS
Beyond alterations of cortical activity and excitability of regional areas, the pathophysiology underlying psychiatric and neurological disorders is increasingly attributed to dysfunctional networks, involving abnormal interactions between multiple brain regions. NIBS techniques alone, and in combination with neuroimaging methods, promote our understanding of the network activity underlying both healthy human brain functions as well as connectivity changes associated with dysfunctional states.
Two TMS pulses applied to different regions of the brain can be used to probe both intra- and interhemispheric corticocortical interactions. Double-pulse techniques have been especially explored for motor control and movement disorders. One example is the exploration of transcallosal inhibition, where a conditioning TMS stimulus is applied over one motor cortex, and the inhibitory effect is explored on the contralateral homolog [15]. Similarly, a conditioning TMS stimulus over the cerebellum inhibits subsequent motor cortex excitability through cerebellar-cortical pathways [16].
Application of NIBS over a specific region affects not only neural activity of the respective target area but also the evoked activity that propagates to anatomically and functionally interconnected regions. Integration of brain stimulation and neuroimaging tools enables evaluation of these dynamic network interactions. Depending on the neuroimaging modality, different aspects of NIBS-induced changes in brain activity can be captured. EEG is suited to monitor TMS/tES-evoked/altered cortical activity not just at the stimulation site, but also across remote, but interconnected areas. Tracing the spatiotemporal propagation pattern of NIBS evoked potentials with EEG allows determining corticocortical excitability and functional connectivity. The high temporal resolution of the EEG enables tracking of the temporal sequence of communication between regions and, combined with NIBS, can identify effective (causal) connectivity patterns in the brain. Moreover, NIBS techniques can trigger oscillatory rhythms or perturb/enhance ongoing oscillations. NIBS-EEG approaches thus make it possible to study the functional/causal specificity of brain rhythms for distinct cognitive and motor functions/malfunctions. Altered amplitudes, synchronization, and propagation of TMS-induced natural frequencies in different cortical areas have the potential to act as diagnostic and prognostic electrophysiological markers—for a review, see [17].
Besides EEG, use of fMRI in combination with NIBS may also deliver relevant additional information about brain connectivity. Although its temporal resolution is inferior in comparison with EEG measures, important advantages include its superior spatial resolution as well as the opportunity to monitor activity alterations across larger and deeper brain areas, including subcortical regions [18].
3 Using NIBS to Modulate Neurophysiological Processes
In addition to the value provided as a monitoring technique, NIBS is increasingly being used in diverse research and clinical settings as a means to directly modulate neural processes. Researchers wishing to study the causal nature of cognitive functions or neurological disorders may consider NIBS to complement traditional neurophysiological techniques such as electrophysiological recordings in animals, which are often invasive, or functional neuroimaging techniques such as fMRI, or EEG/MEG, which are typically limited in disentangling associative/epiphenomenal observations of neural activity from direct causal relations. NIBS as a neuromodulatory technique is not limited to causing acute or short-lasting effects but may also be used to induce aftereffects that extend beyond the duration of application for up to several minutes or hours. These effects share features that are consistent with synaptic plasticity mechanisms, such as long-term depression/potentiation (LTD/LTP). Respective protocols can thus be used to explore the relevance of plasticity for psychological processes, including the involvement of pathological plasticity in psychiatric and neurological diseases, or to counteract respective pathological plasticity for therapeutic reasons.
3.1 Transcranial Magnetic Stimulation (TMS)
Direct-effects: Single stimuli or short bursts of TMS can be used to induce a “virtual brain lesion” whereby local neural activity is disrupted within a specific brain region during a task, allowing inference on the functional role of a particular region, and also when it may become involved during a task (chronometry studies) [19]. Extending the duration of the disruption can be achieved by repeating pulses of TMS (rTMS) at 5–10 Hz, lasting for a few seconds [20]. Short-lasting rTMS protocols have also been shown to transiently induce and synchronize neural firing, leading to changes in neuronal oscillations [21]. As practical examples of these approaches, Amassian et al. [22] demonstrated the dependence of timing TMS to successful vs. unsuccessful processing of visual stimuli relative to delivery intervals.
After-effects: Short- and long-term aftereffects of TMS have been observed with longer duration repetitive TMS protocols (more than 50 pulses), which induce changes in cortical excitability beyond the stimulation period [23]. Understanding the mechanistic and physiological bases for these effects remains a topic of ongoing research; however, synaptic plasticity is assumed to be the likely model, since (1) the direction of plasticity (LTP or LTD) appears to be dependent on the induction protocol, (2) the effects appear related to the activity of gene-encoded proteins that are active during early stages of synaptic plasticity [24, 25], and (3) among other molecular activity, aftereffects are dependent on neurotransmitter release and NMDA receptor-dependent activity [26, 27]. Specifically, low-frequency stimulation such as rTMS in the range between 0.9 and 1 Hz leads to a reduction in cortical excitability, while higher frequency rTMS above 5 Hz increases cortical excitability [28]. Patterned rTMS, such as continuous or intermittent theta-burst stimulation (c/iTBS), whereby 3 pulses are delivered at 50 Hz and repeated at 5 Hz [29], or quadripulse stimulation, which delivers 4 pulses repeated at a rate of 0.2 Hz [30], also induce lasting effects on cortical excitability. Finally, paired associative stimulation (PAS), which combines stimulation of a mixed peripheral nerve with motor cortex TMS, induces—dependent on the interval between respective stimuli—LTP—or LTD-like plasticity, which is similar to spike-timing-dependent plasticity developed in animal models [31]. However, the strength and duration of these effects are not, in all cases, homogeneous. They depend on the physiological state of the brain prior to and during the stimulation [32], as well as on stimulation parameters such as intensity, number of pulses, and repetition of stimulation [33, 34]. In healthy adults, rTMS, TBS, and QPS have been used to induce functional alterations offline, such as in working memory, motor reaction time, visual attention, and tactile discrimination, among other cognitive paradigms (see review by [35]).
3.2 Transcranial Direct Current Stimulation (tDCS)
Direct-effects: tDCS does not induce firing of action potentials but results in polarity-dependent shifts in the resting membrane potential of neurons. Similarly to TMS, the characterization of the specific cell compartments polarized by tDCS critically depends on the neuronal morphology relative to the induced electric field, as well as stimulation intensity and duration [36]. The polarity of the stimulation (anodal or cathodal) is conventionally termed by the respective type of electrode (surface positive or surface negative) placed over the target cortical area on the scalp. Current flows from the anode to the cathode and must flow into and out of the cell in order to exert effects [37]. Animal studies demonstrated that application of weak DC fields delivered epidurally induced polarity-dependent changes in excitability and spontaneous activity during and after the course of stimulation [38]. In animal and human studies, anodal tDCS applied over the motor cortex results in simultaneous enhancement of motor cortical excitability while cathodal tDCS diminishes it [39]. The neuronal effects depend on membrane polarization changes since pharmacological blockage of voltage-dependent sodium and calcium ion channels abolished the respective effects [40].
After-effects: Neuroplastic aftereffects of tDCS are also mediated by changes in synaptic efficacy, and thereby share properties of LTP/LTD. In the seminal animal study by Bindman et al. [38], anodal stimulation led to enhanced cortical activity and excitability lasting for hours while cathodal stimulation led to reduced activity. In humans, respective identically directed polarity-dependent effects were also observed [39, 41]. These effects depend on NMDA receptor activity, which involves regulation of neuronal calcium [40, 42, 43]. Similarly to TMS mechanisms of synaptic plasticity, aftereffects induced by tDCS are not linear and depend on intrinsic cortical activity [44, 45], as well as stimulation parameters, such as current intensity, stimulation duration, and repetition [46,47,48]. Moreover, physiological effects of tDCS are not limited to the cortical region directly stimulated by the electrode montage, but may also extend to regional and remote loci, either due to the diffuse spatial focality of the induced electric field (depending on the montage—[49]) or by functional connectivity-driven changes [50,51,52]. Similarly to rTMS effects, tDCS induces long-lasting functional changes in target regions and networks, such as in motor learning (see review by [53]), as well as in neuropsychological processes such as emotion, attention, and working memory [54].
3.3 Transcranial Alternating Current Stimulation (tACS)
Direct-effects: tACS is a variant of tDCS, which differs mainly in that tACS is applied with an alternating waveform at a specific frequency (or multiple superimposed frequencies). Therefore, the main rationale of applying tACS is to rhythmically alter cortical activity, which is accomplished by frequency-pulsed subthreshold changes in membrane polarization leading to entrainment of intrinsic oscillatory activity with the applied waveform. In classic montages consisting of two electrodes, oscillatory synchronization between the two sites will become anti-phasic since the electric field should alternate unidirectionally. However, by including more than two electrodes with multichannel stimulators, researchers can synchronize oscillatory activity between two or more regions in-phase by specifying the precise phase of the oscillatory cycle individually for each electrode, while ensuring that the net electric field is conserved [55]. The online physiological effects of tACS on neuronal oscillations have been demonstrated by animal studies [56], as well as human studies using EEG, where alpha frequency stimulation increased the power of the respective frequency band [57]. Stimulation at a specific frequency may also entrain harmonic multiples of that frequency or interact with other frequencies due to cross-frequency coupling. Recent studies supporting the functional relevance of these effects have demonstrated that working memory processes can be facilitated with either theta [58] or theta-gamma coupled tACS [59]. Therefore, tACS provides a customizable approach to investigate the causal dependence of oscillatory activity with cognitive functions.
After-effects: Beyond the direct effects of oscillatory entrainment, a few studies have also reported neuroplastic aftereffects in cortical excitability [60,61,62]. Available evidence suggests that the induction of plasticity might partially depend on the stimulation parameters (e.g., frequency and intensity/amplitude), since high- but not low-intensity tACS induced aftereffects up to 60 minutes after stimulation [61, 62], and since tACS was more effective when applied at the beta frequency, which is the predominant frequency band in the resting motor cortex [63]. In the same way, aftereffects in occipital alpha have been observed when tACS was applied within the alpha range [57, 64]. Since a direct association between excitability alterations and oscillatory changes was not observed, whether the observed aftereffects in oscillatory rhythms reflect LTP/LTD-like plasticity mechanisms, such as spike-timing-dependent plasticity (STDP), remains unclear [62, 65, 66].
To summarize, NIBS offers various means to directly modulate and induce aftereffects in neurophysiological processes, such as cortical excitability, neuronal oscillations, and hemodynamic activity, among others. However, these effects are not linearly related to stimulation parameters, may be heterogeneous between individuals due to anatomical or physiological profiles, and may be nontrivially affected by cognitive state, due to metaplastic or homeostatic regulatory mechanisms. The goal of ongoing research and development of NIBS is to understand how these factors interact with each other, in order to develop better-suited stimulation protocols that deliver state-of-the-art efficacy in research and clinical settings.
4 Translation of NIBS Techniques from Basic to Clinical Applications
NIBS may also be applied in clinical settings to treat psychiatric and neurological diseases. In one perspective, they may be used to explore the pathophysiology of these diseases, which include the development of diagnostic measures and relevant biomarkers to track the efficacy of therapeutic interventions, as well as evaluation of therapeutic effects, and their foundations. In a second approach, NIBS protocols may be applied for therapeutic purposes in order to counteract pathological alterations in brain physiology. They may also serve as adjuvants to support therapeutic activities in other domains, e.g., re-learning or rehabilitative approaches, which profit from enhanced plasticity. In the following, we will give examples of how respective NIBS tools can be employed for these purposes.
4.1 Application of NIBS for Identification of Disease-Related Pathophysiology
NIBS techniques have contributed relevantly in enhancing our understanding of the pathophysiology of neurological and psychiatric diseases. In numerous psychiatric diseases, pathological alterations of cortical excitability have been identified. For example, decreased GABAergic inhibition, as obtained by SICI, has been shown for major depression (MDD), schizophrenia (SCZ), and obsessive-compulsive disorder (OCD). Additionally, enhanced intracortical facilitation has been shown in OCD by ICF protocols (for a review, see [67]). These results suggest an imbalance of corresponding neurotransmitters in the respective diseases, mainly of the glutamatergic and GABAergic systems. Moreover, these findings show that respective alterations differ between disease entities. In Alzheimer’s disease (AD), reduced SAI has been shown in patients at the initial stage of disease, which is expected according to the cholinergic hypothesis of AD, and makes this parameter a potential adjunctive tool for early diagnosis of the disease. This deficit was abolished by cholinergic medication, which further suggests such an approach being promising to explore mechanisms of action of respective pharmacological treatment approaches [6].
Beyond the evaluation of regional excitability alterations in psychiatric diseases, network connectivity analysis based on TMS–EEG has emerged recently as a new option to explore respective pathophysiological alterations in psychiatric and neurological diseases. Here, abnormal functional and effective connectivity have been shown to be relevant in disease populations, e.g., patients with SCZ having reduced amplitude and synchrony of frontal and prefrontal gamma oscillations, which was associated with disrupted effective connectivity, as assessed by TMS-EEG [68]. Another important physiological measure of disease-related pathological alterations is neuroplasticity, which has been extensively studied in neuropsychiatric disorders. PAS-generated LTP-like plasticity is impaired in Parkinson’s disease in the off state but restored by dopaminergic treatment, which underscores the relevance of dopamine for plasticity, and might help to explain the cognitive deficits in these patients [69]. For SCZ, a decrease in LTP-like plasticity was demonstrated via tDCS [70], possibly due to pathological alterations of dopaminergic and glutamatergic activity [71]. In accordance with the importance of plasticity for cognitive functions, the respective plasticity reduction is correlated with cognitive decline in these patients [72], supporting the concept of employing alterations in NIBS-induced plasticity as a biomarker of disease or symptom manifestation [70].
These exemplary studies show that NIBS is not only an important tool to explore different aspects of disease-related pathophysiological alterations in the human brain but also potentially relevant to enhance diagnostic efficiency or predict clinical prognosis, e.g., of pharmacological treatment responses. So far, only TMS measures, including central motor conduction time and the triple stimulation technique, have been clinically adopted for the diagnosis of diseases of the motor system. In principle, the abovementioned protocols might also be valuable for these purposes, including monitoring of not only regional excitability, but also plasticity and connectivity. One current drawback of these techniques, which limits their use at individual level, is the relatively large intra- and interindividual variability. However, new paradigms are under development, which might help to overcome these limitations.
4.2 Application of NIBS as Therapeutic Intervention
Given their capability to induce neuroplasticity, and taking into account pathological alterations of plasticity, and cortical excitability in psychiatric diseases, as well as the importance of neuroplasticity for psychotherapeutic and rehabilitative treatments, NIBS techniques have been implemented in numerous treatment studies. As one of the first clinically approved NIBS interventions, rTMS was shown to be efficient for the treatment of MDD. Based on findings of pathological hypo-activation of the left and a relative hyper-activation of the right dorsolateral prefrontal cortex in depression, and a systemic reduction of LTP, which goes along with cognitive deficits, excitability-enhancing left prefrontal or excitability-reducing right prefrontal rTMS and tDCS have successfully demonstrated to reduce symptoms (see [73] for an overview). This application can be taken as a paradigmatic example for the therapeutic application of NIBS, which has since then extended to a larger disease spectrum with similar underlying concepts. In stroke rehabilitation, upregulation of the lesioned area and downregulation of the nonlesioned contralateral homolog have been proposed as an important therapeutic aim to rebalance the motor system, thereby improving functions. Similarly, tDCS has been shown to improve poststroke recovery through this concept [74]. In addition, NIBS based on similar principles has been applied in numerous neuropsychiatric disorders such as neuropathic pain and SCZ (for an overview, see [75, 76]).
Beyond the sole application of NIBS as a therapeutic option, its combination with conventional treatment has also been probed. The conceptual background is to enhance plasticity and/or functions via synergistic effects of dual interventions. For instance, tDCS has been adopted as an adjunctive therapeutic option for stroke rehabilitation or MDD, as it allows combination with simultaneous occupational/physical therapy or psychotherapy, respectively, and thereby further facilitates the recovery process [77, 78]. Likewise, conventional pharmaceutical treatment, with NIBS as an add-on treatment, has revealed synergistic effects. It has been demonstrated that co-application of a serotonergic antidepressant with bilateral prefrontal tDCS significantly improved depression symptoms as compared to treatment with medication or stimulation alone [73].
Apart from the pathological plasticity, neuropsychiatric symptoms can also be associated with abnormal oscillatory activities of specific brain areas. Here tACS is a potentially valuable approach. tACS was shown to suppress Parkinsonian tremor via phase cancellation when an antagonizing stimulation phase was applied over the motor cortex [79]. A similar principle might be considered for other clinical symptoms. For example, consciousness states are associated with specific brain oscillations of prefrontal areas. Gamma oscillations are specifically relevant for the so-called secondary consciousness states, which allow the separation of inner and outer reality, including, but probably not restricted to, the perceived sense of reality during dreams. Here, enhancing gamma activity not only improved secondary consciousness during dreams [80] but also improved symptoms in a pilot study in OCD. In this condition, symptoms are at least partially caused by an unsurmountable drive to perform activities, which are known to be intellectually senseless by the patients, but cannot be completely suppressed, which may be partially due to a missing cognitive dissociation to respective impulses [81]. However, apart from these approaches, therapeutic tACS studies remain scarce at present.
In general, the therapeutic application of neuromodulatory NIBS techniques shows potential as a clinical intervention, and implementation of some protocols into routine therapy is already showing promising efficacy. Nevertheless, beyond numerous pilot studies in various diseases, there is still a long way to go for many applications to be transferred to routine clinical treatment, due to a relative lack of systematic studies to identify optimal protocols. Moreover, pivotal studies are still required in many fields, and interindividual differences in efficacy require a nuanced approach in study designs and analyses, which has largely not been tackled systematically so far.
5 Conclusions
Noninvasive brain stimulation relevantly enriches the arsenal of methods available to explore the physiological foundation of neurological and psychiatric diseases, including not only pathological alterations but also dynamic changes relevant for treatment effects. Moreover, specific variants of these methods are suited to induce or modulate prolonged alterations of respective physiological processes, which have therapeutic potential. This especially includes NIBS-generated plasticity and alterations of oscillatory brain activity.
For exploration of physiological processes, it is evident that NIBS helps in obtaining a more enriched understanding of the physiological bases of respective diseases at the group level, and thereby insightful knowledge about the general pathophysiology of respective syndromes, as well as physiological alterations which are associated with therapeutic success (although the latter has been explored less extensively). These kinds of studies, especially when combined with imaging methods, might help to develop innovative physiology-based therapeutic regimens and also to evaluate the potential of new treatment options based on their physiological effects. However, a relatively scarce amount of protocols has been used so far as diagnostic procedure for individual patients. Exceptions are central conductance measures, measures of MEP amplitudes under specific conditions (i.e., the triple stimulation technique), and mapping procedures. One reason for this shortcoming is the relevant trial-to-trial variability of TMS-evoked outcome measures. While it might be possible to reduce certain methodologically caused foundations of this variability by sophisticated stimulation protocols, e.g., neuronavigation or robot-assisted procedures, some aspects of this variability are intrinsic, i.e., the partially asynchronous activation of target neurons, and differences in conduction velocity between respective neurons. Thus, usage of respective tools to extract biomarkers at the individual level, and/or tools for personalized medicine, might be somewhat limited with presently available procedures.
For therapeutic applications, plasticity-inducing and plasticity-modulating tools are available at present. These include mainly rTMS and tDCS, but new techniques are emerging, including oscillatory electrical stimulation (tACS, tRNS), stimulation with static magnets, or ultrasound stimulation. These tools have been investigated as viable treatment options for numerous psychiatric and neurological diseases, and conclusive evidence for therapeutic effects in a couple of syndromes is available, such as for rTMS in major depression, which has FDA approval. However, here also, systematic studies are required at the group level to identify protocols with optimized efficacy, as well as protocols that allow a sophisticated and individualized adaptation. Achieving these objectives is not trivial because the effects of these techniques are neuromodulatory, and therefore nonlinear, and state-dependent. Newly developing approaches might combine specific intervention concepts, e.g., by combinations of stimulation with pharmacotherapy, and psychotherapy, to achieve more targeted effects of therapeutic plasticity alterations.
A common limitation of both diagnostic and therapeutic approaches is the restriction of the direct effects of respective interventions to only superficial cortical targets. This might be partially overcome by network stimulation approaches; however, some emerging techniques offer the promise to also allow subcortical stimulation selectively, which would open completely new avenues for NIBS. These include techniques such as ultrasound stimulation and more specialized forms of oscillatory electric brain stimulation protocols.
Taken together, NIBS has been developed into a valuable tool for exploring the physiological underpinning of brain diseases, monitoring therapeutic effects, and also as an interventional method for modulating neurophysiological activity. The combination of NIBS with other approaches and the development of these tools might help to further enhance the utility of respective techniques.
References
Merton PA, Morton HB. Stimulation of the cerebral cortex in the intact human subject. Nature [Internet]. 1980 May 22 [cited 2016 Nov 26];285(5762):227. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7374773.
Committee IFCN, Rossini PM, Burke D, Chen R, Cohen LG, Daskalakis Z, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application: an updated report from an I.F.C.N. Committee. Clin Neurophysiol [Internet]. 2015;126(6):1071–107. https://doi.org/10.1016/j.clinph.2015.02.001.
Ziemann U, Lönnecker S, Steinhoff BJ, Paulus W. Effects of antiepileptic drugs on motor cortex excitability in humans: a transcranial magnetic stimulation study. Ann Neurol. 1996;40(3):367–78.
Paulus W, Classen J, Cohen LG, Large CH, Di Lazzaro V, Nitsche M, et al. State of the art: pharmacologic effects on cortical excitability measures tested by transcranial magnetic stimulation. Brain Stimul [Internet]. 2008;1(3):151–63. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1935861X08000387.
Prout AJ, Eisen AA. The cortical silent period and amyotrophic lateral sclerosis. Muscle Nerve. 1994;17(2):217–23.
Nardone R, Bergmann J, Kronbichler M, Kunz A, Klein S, Caleri F, et al. Abnormal short latency afferent inhibition in early Alzheimer’s disease: a transcranial magnetic demonstration. J Neural Transm. 2008;115(11):1557–62.
Ziemann U, Tergau F, Bruns D, Baudewig J, Paulus W. Changes in human motor cortex excitability induced by dopaminergic and anti-dopaminergic drugs. Electroencephalogr Clin Neurophysiol. 1997;105(6):430–7.
Siebner HR, Dressnandt J, Auer C, Conrad B. Continuous intrathecal baclofen infusions induced a marked increase of the transcranially evoked silent period in a patient with generalized dystonia. Muscle Nerve. 1998;21(9):1209–12.
Hanajima R, Ugawa Y, Terao Y, Enomoto H, Shiio Y, Mochizuki H, et al. Mechanisms of intracortical I-wave facilitation elicited with paired-pulse magnetic stimulation in humans. J Physiol. 2002;538(1):253–61.
Ziemann U, Tergau F, Wischer S, Hildebrandt J, Paulus W. Pharmacological control of facilitatory I-wave interaction in the human motor cortex. A paired transcranial magnetic stimulation study. Electroencephalogr Clin Neurophysiol. 1998;109(4):321–30.
Farzan F, Vernet M, Shafi M, Rotenberg A, Daskalakis ZJ, Pascual-Leone A. Characterizing and modulating brain circuitry through transcranial magnetic stimulation combined with electroencephalography. Front Neural Circuits. 2016;10:73.
Fitzgerald PB, Daskalakis ZJ, Hoy K, Farzan F, Upton DJ, Cooper NR, et al. Cortical inhibition in motor and non-motor regions: a combined TMS-EEG study. Clin EEG Neurosci. 2008;39(3):112–7.
Fitzgerald PB, Maller JJ, Hoy K, Farzan F, Daskalakis ZJ. GABA and cortical inhibition in motor and non-motor regions using combined TMS–EEG: a time analysis. Clin Neurophysiol. 2009;120(9):1706–10.
Cash RFH, Noda Y, Zomorrodi R, Radhu N, Farzan F, Rajji TK, et al. Characterization of glutamatergic and GABA A-mediated neurotransmission in motor and dorsolateral prefrontal cortex using paired-pulse TMS–EEG. Neuropsychopharmacology. 2017;42(2):502.
Meyer B-U, Röricht S, Von Einsiedel HG, Kruggel F, Weindl A. Inhibitory and excitatory interhemispheric transfers between motor cortical areas in normal humans and patients with abnormalities of the corpus callosum. Brain. 1995;118(2):429–40.
Werhahn KJ, Taylor J, Ridding M, Meyer B-U, Rothwell JC. Effect of transcranial magnetic stimulation over the cerebellum on the excitability of human motor cortex. Electroencephalogr Clin Neurophysiol. 1996;101(1):58–66.
Thut G, Miniussi C. New insights into rhythmic brain activity from TMS–EEG studies. Trends Cogn Sci. 2009;13(4):182–9.
Siebner HR, Bergmann TO, Bestmann S, Massimini M, Johansen-Berg H, Mochizuki H, et al. Consensus paper: combining transcranial stimulation with neuroimaging. Brain Stimul [Internet]. 2009;2(2):58–80. Available from: http://www.sciencedirect.com/science/article/pii/S1935861X08003616.
Pascual-Leone A, Walsh V, Rothwell J. Transcranial magnetic stimulation in cognitive neuroscience what does it do and when does it do it? A causal chronometry of brain function. Curr Opin Neurobiol. 2000;10:232–7.
Hallett M. Transcranial magnetic stimulation: a primer. Neuron. 2007;55(2):187–99.
Veniero D, Vossen A, Gross J, Thut G. Lasting EEG/MEG aftereffects of rhythmic transcranial brain stimulation: level of control over oscillatory network activity. Front Cell Neurosci [Internet]. 2015;9:477. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4678227&tool=pmcentrez&rendertype=abstract.
Amassian VE, Cracco RQ, Maccabee PJ, Cracco JB, Rudell A, Eberle L. Suppression of visual perception by magnetic coil stimulation of human occipital cortex. Electroencephalogr Clin Neurophysiol Potentials Sect [Internet]. 1989;74(6):458–62. Available from: https://linkinghub.elsevier.com/retrieve/pii/0168559789900361.
Ziemann U, Paulus W, Nitsche MA, Pascual-Leone A, Byblow WD, Berardelli A, et al. Consensus: motor cortex plasticity protocols. Brain Stimul [Internet]. 2008;1(3):164–82. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1935861X08000429.
Hoppenrath K, Funke K. Time-course of changes in neuronal activity markers following iTBS-TMS of the rat neocortex. Neurosci Lett [Internet]. 2013 Mar 1 [cited 2019 Jul 1];536:19–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23328445.
Volz LJ, Benali A, Mix A, Neubacher U, Funke K. Dose-dependence of changes in cortical protein expression induced with repeated transcranial magnetic theta-burst stimulation in the rat. Brain Stimul [Internet]. 2013 Jul [cited 2019 Jul 1];6(4):598–606. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23433874.
Cirillo G, Di Pino G, Capone F, Ranieri F, Florio L, Todisco V, et al. Neurobiological after-effects of non-invasive brain stimulation. Brain Stimul [Internet]. 2017;10(1):1–18. https://doi.org/10.1016/j.brs.2016.11.009.
Rajan TS, Ghilardi MFM, Wang HY, Mazzon E, Bramanti P, Restivo D, et al. Mechanism of action for rTMS: a working hypothesis based on animal studies [Internet]. Front Physiol. 2017;8 [cited 2019 Jul 2]. Available from: http://journal.frontiersin.org/article/10.3389/fphys.2017.00457/full.
Lenz M, Müller-Dahlhaus F, Vlachos A. Cellular and molecular mechanisms of rTMS-induced neural plasticity. In: Therapeutic rTMS in neurology [Internet]. Cham: Springer International Publishing; 2016. p. 11–22. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/978-3-319-25721-1_2.
Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45(2):201–6.
Hamada M, Terao Y, Hanajima R, Shirota Y, Nakatani-Enomoto S, Furubayashi T, et al. Bidirectional long-term motor cortical plasticity and metaplasticity induced by quadripulse transcranial magnetic stimulation. J Physiol. 2008;586(16):3927–47.
Stefan K, Kunesch E, Cohen LG, Benecke R, Classen J. Induction of plasticity in the human motor cortex by paired associative stimulation. Brain. 2000;123(Pt 3):572–84.
Karabanov A, Ziemann U, Hamada M, George MS, Quartarone A, Classen J, et al. Consensus paper: probing homeostatic plasticity of human cortex with non-invasive transcranial brain stimulation. Brain Stimul [Internet]. 2015;8(5):993–1006. https://doi.org/10.1016/j.brs.2015.01.404.
Tse NY, Goldsworthy MR, Ridding MC, Coxon JP, Fitzgerald PB, Fornito A, et al. The effect of stimulation interval on plasticity following repeated blocks of intermittent theta burst stimulation. Sci Rep [Internet]. 2018 Jun 4 [cited 2019 Jul 2];8(1):8526. Available from: http://www.nature.com/articles/s41598-018-26791-w.
Bäumer T, Lange R, Liepert J, Weiller C, Siebner HR, Rothwell JC, et al. Repeated premotor rTMS leads to cumulative plastic changes of motor cortex excitability in humans. NeuroImage. 2003;20(1):550–60.
Luber B, Lisanby SH. Enhancement of human cognitive performance using transcranial magnetic stimulation (TMS). Neuroimage [Internet]. 2014;85(2):961–70. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1053811913006447.
Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, et al. Transcranial direct current stimulation: state of the art 2008. Brain Stimul [Internet]. 2008;1(3):206–23. Available from: http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B8JBG-4SWGB96-1&_user=10&_coverDate=07%2F31%2F2008&_rdoc=11&_fmt=high&_orig=browse&_srch=doc-info(%23toc%2343558%232008%23999989996%23696438%23FLA%23display%23Volume)&_cdi=43558&_sort=d&_docanchor=&.
Rahman A, Reato D, Arlotti M, Gasca F, Datta A, Parra LC, et al. Cellular effects of acute direct current stimulation: somatic and synaptic terminal effects. J Physiol [Internet]. 2013;591(Pt 10):2563–78. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3678043&tool=pmcentrez&rendertype=abstract.
Bindman LJ, Lippold OCJ, Redfearn JWT. The action of brief polarizing currents on the cerebral cortex of the rat (1) during current flow and (2) in the production of long-lasting after-effects. J Physiol [Internet]. 1964;172(1):369–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14199369%5Cn, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC136885.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol [Internet]. 2000;527(Pt 3):633–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10990547%5Cn, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2270099&tool=pmcentrez&rendertype=abstract.
Nitsche MA, Fricke K, Henschke U, Schlitterlau A, Liebetanz D, Lang N, et al. Pharmacological modulation of cortical excitability shifts induced by transcranial direct current stimulation in humans. J Physiol [Internet]. 2003;553(1):293–301. Available from: http://www.jphysiol.org/cgi/doi/10.1113/jphysiol.2003.049916.
Nitsche MA, Nitsche MS, Klein CC, Tergau F, Rothwell JC, Paulus W. Level of action of cathodal DC polarisation induced inhibition of the human motor cortex. Clin Neurophysiol [Internet]. 2003;114(4):600–4. Available from: http://ac.els-cdn.com/S1388245702004121/1-s2.0-S1388245702004121-main.pdf?_tid=d330e68c-b706-11e2-b24b-00000aab0f02&acdnat=1367925251_049960c317c14dbb692895176e623ccd.
Malenka RC, Bear MF. LTP and LTD: an embarrassment of riches. Neuron [Internet]. 2004 Sep 30 [cited 2016 Nov 25];44(1):5–21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15450156.
Liebetanz D, Nitsche MA, Tergau F, Paulus W. Pharmacological approach to the mechanisms of transcranial DC-stimulation-induced after-effects of human motor cortex excitability. Brain. 2002;125(10):2238–47.
Antal A, Terney D, Poreisz C, Paulus W. Towards unravelling task-related modulations of neuroplastic changes induced in the human motor cortex. Eur J Neurosci. 2007;26(9):2687–91.
Thirugnanasambandam N, Sparing R, Dafotakis M, Meister IG, Paulus W, Nitsche MA, et al. Isometric contraction interferes with transcranial direct current stimulation (tDCS) induced plasticity: evidence of state-dependent neuromodulation in human motor cortex. Restor Neurol Neurosci [Internet]. 2011 [cited 2019 Jul 2];29(5):311–20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21697590.
Batsikadze G, Moliadze V, Paulus W, Kuo M-F, Nitsche MA. Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. J Physiol [Internet]. 2013;591(7):1987–2000. Available from: http://doi.wiley.com/10.1113/jphysiol.2012.249730.
Monte-Silva K, Kuo M-FF, Hessenthaler S, Fresnoza S, Liebetanz D, Paulus W, et al. Induction of late LTP-like plasticity in the human motor cortex by repeated non-invasive brain stimulation. Brain Stimul [Internet]. 2013 May [cited 2014 Feb 27];6(3):424–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22695026.
Monte-Silva K, Kuo M-F, Liebetanz D, Paulus W, Nitsche MA. Shaping the optimal repetition interval for cathodal transcranial direct current stimulation (tDCS). J Neurophysiol. 2010;103(4):1735–40.
Nitsche MA, Doemkes S, Karakose T, Antal A, Liebetanz D, Lang N, et al. Shaping the effects of transcranial direct current stimulation of the human motor cortex shaping the effects of transcranial direct current stimulation of the human motor cortex. J Neurophysiol [Internet]. 2007;97:3109–17. Available from: http://jn.physiology.org/cgi/doi/10.1152/jn.01312.2006.
Polanía R, Paulus W, Antal A, Nitsche MA. Introducing graph theory to track for neuroplastic alterations in the resting human brain: a transcranial direct current stimulation study. Neuroimage [Internet]. 2011;54(3):2287–96. https://doi.org/10.1016/j.neuroimage.2010.09.085.
Polanía R, Nitsche MA, Paulus W. Modulating functional connectivity patterns and topological functional organization of the human brain with transcranial direct current stimulation. Hum Brain Mapp [Internet]. 2011 Aug [cited 2014 Feb 25];32(8):1236–49. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20607750.
Kunze T, Hunold A, Haueisen J, Jirsa V, Spiegler A. Transcranial direct current stimulation changes resting state functional connectivity: a large-scale brain network modeling study. Neuroimage [Internet]. 2016;140:174–87. Available from: http://www.sciencedirect.com/science/article/pii/S1053811916001221.
Buch ER, Santarnecchi E, Antal A, Born J, Celnik PA, Classen J, et al. Effects of tDCS on motor learning and memory formation: a consensus and critical position paper. Clin Neurophysiol [Internet]. 2017;128(4):589–603. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1388245717300263.
Shin Y-I, Foerster Á, Nitsche MA. Transcranial direct current stimulation (tDCS)—application in neuropsychology. Neuropsychologia [Internet]. 2015;69:154–75. Available from: http://www.sciencedirect.com/science/article/pii/S0028393215000639.
Saturnino GB, Madsen KH, Siebner HR, Thielscher A. How to target inter-regional phase synchronization with dual-site transcranial alternating current stimulation. Neuroimage [Internet]. 2017;163:68–80. https://doi.org/10.1016/j.neuroimage.2017.09.024.
Fröhlich F, McCormick DA. Endogenous electric fields may guide neocortical network activity. Neuron. 2010;67(1):129–43.
Zaehle T, Rach S, Herrmann CS. Transcranial alternating current stimulation enhances individual alpha activity in human EEG. PLoS One. 2010;5(11):1–7.
Polanía R, Nitsche MA, Korman C, Batsikadze G, Paulus W. The importance of timing in segregated theta phase-coupling for cognitive performance. Curr Biol [Internet]. 2012 Jul 5 [cited 2014 Jan 21];22(14):1–5. Available from: http://wwdw.ncbi.nlm.nih.gov/pubmed/22683259.
Alekseichuk I, Turi Z, De Lara GA, Antal A, Alekseichuk I, Turi Z, et al. Spatial working memory in humans depends on theta and high gamma synchronization in the prefrontal cortex article spatial working memory in humans depends on theta and high gamma synchronization in the prefrontal cortex. Curr Biol [Internet]. 2016;26(12):1513–1521. https://doi.org/10.1016/j.cub.2016.04.035.
Moliadze V, Antal A, Paulus W. Boosting brain excitability by transcranial high frequency stimulation in the ripple range. J Physiol. 2010;588(24):4891–904.
Antal A, Boros K, Poreisz C, Chaieb L, Terney D, Paulus W. Comparatively weak after-effects of transcranial alternating current stimulation (tACS) on cortical excitability in humans. Brain Stimul [Internet]. 2008 Apr [cited 2015 Jan 6];1(2):97–105. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20633376.
Wischnewski M, Engelhardt M, Salehinejad MA, Schutter DJLG, Kuo M-F, Nitsche MA. NMDA receptor-mediated motor cortex plasticity after 20 hz transcranial alternating current stimulation. Cereb Cortex [Internet]. 2019;29(7):2924–2931. Available from: https://academic.oup.com/cercor/advance-article/doi/10.1093/cercor/bhy160/5051079.
St. Louis EK, Frey LC, Britton JW, Frey LC, Hopp JL, Korb P, et al. The Normal EEG. 2016 [cited 2019 Jul 2]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK390343/.
Kasten FH, Dowsett J, Herrmann CS. Sustained aftereffect of α -tACS lasts up to 70 min after stimulation. Front Hum Neurosci. 2016;10:245.
Thut G, Miniussi C, Gross J. The functional importance of rhythmic activity in the brain. Curr Biol [Internet]. 2012;22(16):R658–63. https://doi.org/10.1016/j.cub.2012.06.061.
Vossen A, Gross J, Thut G. Alpha power increase after transcranial alternating current stimulation at alpha frequency (α-tACS) reflects plastic changes rather than entrainment. Brain Stimul [Internet]. 2015 May [cited 2019 Jul 2];8(3):499–508. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25648377.
Radhu N, de Jesus DR, Ravindran LN, Zanjani A, Fitzgerald PB, Daskalakis ZJ. A meta-analysis of cortical inhibition and excitability using transcranial magnetic stimulation in psychiatric disorders. Clin Neurophysiol. 2013;124(7):1309–20.
Hui J, Tremblay S, Daskalakis ZJ. The current and future potential of transcranial magnetic stimulation with electroencephalography in psychiatry. Clin Pharmacol Ther. 2019;106(4):734–46. https://doi.org/10.1002/cpt.1541. Epub 2019 Aug 30. PMID: 31179533.
Morgante F, Espay AJ, Gunraj C, Lang AE, Chen R. Motor cortex plasticity in Parkinson’s disease and levodopa-induced dyskinesias. Brain. 2006;129(Pt 4):1059–69.
Hasan A, Falkai P, Wobrock T. Transcranial brain stimulation in schizophrenia: targeting cortical excitability, connectivity and plasticity. Curr Med Chem. 2013;20(3):405–13.
Balu DT, Coyle JT. Neuroplasticity signaling pathways linked to the pathophysiology of schizophrenia. Neurosci Biobehav Rev. 2011;35(3):848–70.
Frantseva MV, Fitzgerald PB, Chen R, Möller B, Daigle M, Daskalakis ZJ. Evidence for impaired long-term potentiation in schizophrenia and its relationship to motor skill learning. Cereb Cortex. 2008;18(5):990–6.
Brunoni AR, Sampaio-Junior B, Moffa AH, Aparício LV, Gordon P, Klein I, et al. Noninvasive brain stimulation in psychiatric disorders: a primer. Braz J Psychiatry. 2019;41(1):70–81.
Fregni F, Boggio PS, Mansur CG, Wagner T, Ferreira MJ, Lima MC, et al. Transcranial direct current stimulation of the unaffected hemisphere in stroke patients. Neuroreport. 2005;16(14):1551–5.
Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150–206.
Lefaucheur JP. Cortical neurostimulation for neuropathic pain: state of the art and perspectives. Pain. 2016;157(Suppl):S81–9.
Jung IY, Lim JY, Kang EK, Sohn HM, Paik NJ. The factors associated with good responses to speech therapy combined with transcranial direct current stimulation in post-stroke aphasic patients. Ann Rehabil Med. 2011;35(4):460–9.
Welch ES, Weigand A, Hooker JE, Philip NS, Tyrka AR, Press DZ, et al. Feasibility of computerized cognitive-behavioral therapy combined with bifrontal transcranial direct current stimulation for treatment of major depression. Neuromodulation. 2019;22(8):898–903.
Brittain JS, Probert-Smith P, Aziz TZ, Brown P. Tremor suppression by rhythmic transcranial current stimulation. Curr Biol. 2013;23(5):436–40.
Voss U, Holzmann R, Hobson A, Paulus W, Koppehele-Gossel J, Klimke A, et al. Induction of self awareness in dreams through frontal low current stimulation of gamma activity. Nat Neurosci. 2014;17(6):810–2.
Klimke A, Nitsche MA, Maurer K, Voss U. Case report: successful treatment of therapy-resistant OCD with application of transcranial alternating current stimulation (tACS). Brain Stimul. 2016;9(3):463–5.
Acknowledgments
This work was supported by the BMBF GCBS project (grant 01EE1403C).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jamil, A., Yavari, F., Kuo, MF., Nitsche, M.A. (2020). NIBS as a Research Tool in Clinical and Translational Neuroscience. In: Dell'Osso, B., Di Lorenzo, G. (eds) Non Invasive Brain Stimulation in Psychiatry and Clinical Neurosciences. Springer, Cham. https://doi.org/10.1007/978-3-030-43356-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-43356-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43355-0
Online ISBN: 978-3-030-43356-7
eBook Packages: MedicineMedicine (R0)