Abstract
Unprecedented explosion of research in the field of nanotechnology has gained importance in the treatment, prevention, and eradication of antibiotic-resistant bacterial strains. The emerging multidrug-resistant bacteria (MDRB) pose a major threat to the modern health-care system. The MDRB strains cannot be treated with conventional antibiotics due to their rapid mutations and resistance. Antibiotic-resistant bacteria that produce biofilm are responsible for approximately 700,000 deaths each year. One of the biggest problems faced by research society is to find alternatives to combat the increasing number of resistant variants. Photodynamic therapy (PDT) was established recently and remains a successful treatment modality for infectious diseases caused by microbial strains and biofilms. Light-mediated inactivation through photodynamic therapy provides new dimensions to eradicate antibiotic-resistant microbes. Antimicrobial photodynamic therapy (aPDT) has gained interest in nanotechnology where the effectiveness of photosensitizers (PS) can be enhanced by the use of nanoparticles (NPs). In the last two decades, different techniques have been raised for aPDT in combination with nanoparticles. Nanoparticles are used in aPDT either as photosensitizing agents or as PS delivery agents. Nanoparticles used in aPDT improve the dispersion and selective delivery of PS to the target cells. Over last decades, various nanoparticles are utilized in aPDT as nanocarriers. Polymeric nanovehicles, nanomicelles, and liposome are used to encapsulate PS molecules. The inorganic metallic nanoparticles are extensively studied for the photoinactivation of resistant microorganisms and their biofilms. The four types of combinations between nanoparticles and PS are categorized as nanoparticles embedded with PS, nanoparticles with PS bound to the surface, nanoparticles as the PS, and PS alongside nanoparticles. Nanoparticles have enhanced the activity of aPDT by encapsulating the PS in nanoparticles or binding the PS on the surface of nanoparticles covalently. The photoactive nanoparticles were successful as antimicrobial agents and more effective against antibiotic-resistant microbial strains and their biofilms.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
13.1 Introduction
13.1.1 The Emergence of Multidrug-Resistant Bacteria
Antibiotic resistance in microorganisms and associated infections are serious and growing challenge in health-care system. Antibiotic-resistant bacteria were observed in the patients with weak health condition, regular and repeated exposure to antibiotics, and frequent hospitalization. For instance, methicillin-resistant Staphylococcus aureus (MRSA) is prevalent in hospitalized patients and even exhibits resistance to alternative antimicrobial agents especially vancomycin. The resistance to vancomycin is reported in several bacteria including hospital-acquired pathogenic bacteria Enterococcus sp. Lack of effective therapies for multidrug-resistant bacteria urges the immediate attention in antimicrobial drug discovery process (McAdam et al. 2012).
Even though antibiotics have saved billions of lives, current antimicrobial resistance (AMR) patterns among the bacterial pathogens become a reason for thousands of deaths worldwide. Scientists concluded that optional use of antimicrobial agents, window of treatment period, and choice of antibiotics and dosage of antibiotics are the important factors that can reduce the consequences of AMR (Holmstrup and Klausen 2018). Antibiotic resistance is observed in both hospital settings and primary health-care centers as leading threat to human health (National Collaborating Centre for Infectious Diseases 2010).
The diseases associated with AMR strains in health-care system include gonorrhea, tuberculosis, typhoid fever, and group B Streptococcus infections (Llor and Bjerrum 2014). AMR is known as silent pandemic with profound effect on treatment procedures. Microorganisms are adapted to the available antimicrobial agents through evolution which resulted in the difficulties in disease treatment. Still now, there is no “single silver bullet” to reduce the AMR strains to avoid innumerable future victims of antibiotic-resistant diseases. According to the specific Sustainable Development Goals (SDGs) agenda , it is the peak time to find a permanent solution to this evolving threat caused by antibiotic-resistant bacteria (Jasovský et al. 2016).
13.1.2 Emerging Infectious Diseases and Antibiotic-Resistant Biofilms
Microorganisms thrive in diverse habitats as they are having the ability to adhere to substrates and form communities. These microorganisms living in populations can able to cooperate, compete, and interact to carry out complex processes. Microbial biofilms are represented by single species or multispecies encased in a self-produced exopolysaccharide matrix (EPS) (Bjarnsholt 2013). Biofilms also contribute to the emerging problem of antibiotic resistance in microorganisms. Horizontal gene transfer in bacteria mediates the evolution and genetic diversity among microbial communities. The highly protected structure of biofilms formed by EPS prevents the contact of antimicrobial agents to bacteria by selectively restricting the diffusion (Chadha 2012).
The possible reasons for the antibiotic resistance in biofilms include restricted penetration of drugs, decreased growth rate of cells, and resistance gene expressions. According to the global report made by National Institutes of Health, biofilms are accountable for more than 60% of microbial infections which are difficult to eradicate. There are common bacterial infections caused by biofilms, and frequently relapsing are urinary tract infections caused by E. coli, dental plaques, gingivitis, middle ear infections caused by Haemophilus influenza , catheter-related infections caused by Staphylococcus aureus , and other Gram-positive organism. Complications associated with antibiotic-resistant and biofilm-forming bacteria are life-threatening which causes grave morbidity and mortality (Lewis 2001). Other life-threatening infections by antibiotic-resistant bacteria are diseases in cystic fibrosis patients caused by P. aeruginosa, indwelling-device-associated infections by S. aureus, and endocarditis by S. aureus. The growing incidence of nosocomial infections is the major burden on health-care system which are contributed mainly by antimicrobial-resistant pathogens.
A group of nosocomial pathogens termed as “ESKAPE” with antibiotic resistance are the major reason for increased treatment costs and high morbidity and mortality. The ESKAPE pathogens cover both the Gram-negative and Gram-positive bacteria such as Enterococcus faecium, S. aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species (Santajit and Indrawattana 2016). ESKAPE pathogens causing nosocomial infections exhibit different profiles of antibiotic resistance, infections, and disease transmission. The array of resistance mechanism utilized by pathogens includes enzymatic inactivation, drug target modification, change in the integrity of cell membrane, expression of efflux pump mechanism, and protection by biofilms. In the near future, antimicrobial resistance profiles and biofilms of these pathogens seem to be a major challenge to global health-care systems. This alters the scientific community regarding the scarcity of potential antimicrobial agents in the pipeline and the need for developing new therapeutic methods or novel antimicrobial agents against infections caused by pathogens (Wilson 2014; Li and Nikaido 2009; Wright 2005; Aziz et al. 2014, 2015, 2016).
13.1.3 Survival Mechanisms of Bacterial Biofilms
Biofilms are population or group of microorganisms having complex architecture made of proteins, polysaccharide, and DNA which are self-protected by EPS matrix from adverse conditions. Biofilms that establish on medical devices, living tissues, and water bodies are difficult to eradicate. They are recalcitrant to antibiotics, phagocytosis, and other disinfectants. The structure of biofilms is supported by several interstitial voids such as macro- and microvoids that allow the diffusion of drugs, but the cells modulate the architecture of biofilm communities in response to the external and internal stimuli which pump out the antimicrobial agents. The cells in close proximity exchange their chromosomal plasmids and exhibit bacterial communication pathways called quorum sensing (Singh et al. 2017).
The stable and compact nature of biofilms, reduced rates of cell growth, protection by matrix polymers, and respiration of biofilm bacteria prevent the attack and destruction of biofilms by natural and artificial chemical agents. The enhanced resistance is a profound trait associated with biofilms. Biofilms show 10–1000-fold resistance to several antimicrobial agents than the planktonic bacteria. For instance, S. aureus cells are susceptible to chlorine, an oxidizing biocide, but demand 600-fold increased concentration of antimicrobial agents to kill biofilms of S. aureus (Jing et al. 2014; Costerton et al. 1995; Donlan 2002). The factors contributing to antibiotic resistance include poor penetration of antibiotic, reduced growth of cells, and unique biofilm structure. The antimicrobial agents are unable to penetrate through all areas of biofilms and especially unable to reach the deeper layers of biofilm. The capacity of antibiotic to penetrate the biofilm layers is purely dependent on the concentration and choice of antibiotic used (Vrany et al. 1997). Nondividing cells of biofilms escape from the detrimental effects of antibiotics targeted against their growth specific factors due to the reduced growth in biofilms. Scientists have reported that the unusual resistance of biofilms is contributed by the above mentioned factor (Davies 2003). Other important factor governing the antimicrobial resistance is the heterogeneity of cells within the biofilm. Signaling factors, waste products, and nutrient gradients can determine the formation of heterogeneity within the biofilm. Studies reveal that the location of cells in the biofilm community exhibits varying response to antimicrobial agents. The slow growth rate of some cells may lead to the initiation of general stress response within the biofilm. The stress response faced by biofilm cells protects them from extreme environmental conditions including cold shock, heat shock, chemical agents, and changes in the pH (Mah and O’Toole 2001). Persister and phenotypic variants are responsible for high levels of resistance in biofilms. Most of biofilm cells are sensitive to antibiotics similar to planktonic cells, whereas the persister cells are responsible for the survival of cells. Persister cells survive from the action of antimicrobial agents, while phenotypic variants survive even in elevated levels of antibiotics (Drenkard and Ausubel 2002). Overproduction and expression of multidrug efflux pumps in prokaryotic and eukaryotic cells are the reason for the extrusion of drugs, toxic metabolites, and other compounds from the cell which contributes resistance to the antibiotics (Drenkard 2003). The most important feature of biofilms and planktonic cells toward antimicrobial agents is their high resistance profiles. The infections caused by microbial biofilms are problematic and hard to eradicate. There are several factors contributing to the resistance, and the antibiotic resistance in biofilms is multifactorial (Fig. 13.1).
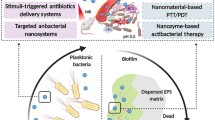
13.1.4 Antimicrobial and Antibiofilm Strategies
Recently health-care system has reached “post antibiotic era” where many of the antimicrobial agents are no longer effective and useful. This is because of the failure in the discovery of antibiotics; so far no new classes of antibiotics were designed from the past 45 years for infections caused by Gram-negative bacteria. According to the reports, only 37 antimicrobial drugs were successful in phase II or phase III clinical trials of 2016. Therefore, the needs to develop alternative therapeutic methods are urged in research to treat infections caused by drug-resistant microbes. Moreover along with antibiotic resistance, antibiotics may show accidental consequences such as stimulating hyper-inflammatory effects or off-target effects by disturbing beneficial microbiota. The disturbances to the normal microbiota can be detrimental to our health resulting in disease. The critical aspect taken into consideration during the design of next-generation antimicrobials is to preserve the normal microbiota (Fernandes and Martens 2017). Next-generation antimicrobials for infectious diseases include nucleic acid-based approaches for selectively targeting microorganisms. CRISPR-Cas system has been developed to selectively target antibiotic-resistant genes in complex microbial consortia and pure cultures. Other than nucleic acid-based systems, peptide-based antimicrobials are also under research with enhanced specificity. Peptide molecules are easily modified to achieve specific functions especially their biophysical properties such as net charge, amphiphilicity, and hydrophobicity to enhance the antimicrobial action. Many synthetic variants are designed based on their structure-activity relationship with observed broad-spectrum antimicrobial action. A synthetic peptide-based antibiotic, e.g., lysins, showed antimicrobial activity against Gram-positive and Gram-negative bacterial pathogens (de la Fuente-Nunez et al. 2017).
The next-generation antimicrobial therapies based on peptides and nucleic acid systems are still in infancy due to the limitations in their clinical applications. These therapeutic methods can be upgraded for better antimicrobial activities by protecting them from host degradation by proteases and nucleases. New drug carrier agents are required for the efficient and enhanced delivery to the target sites. A paradigm shift in the design of new and effective antimicrobials includes selection of effective antibiofilm molecules, better use of existing antimicrobials, development of next-generation antibiotics against biofilms, and regulatory issues for the establishment of new diagnostic assays (Ceri et al. 2010). Novel strategies are required to control the biofilm formation by considering the health-related problems due to biofilms, which include prevention of cell adhesion to the substrates, reduction in the EPS production, and disruption of quorum-sensing phenomenon in bacteria (Majik and Parvatkar 2013). Novel antibiofilm strategies include the use of natural products (plant extracts, honey, essential oil, cumin oil, cinnamon oil), bacteriophage therapy, quorum quenching molecules, new surfaces for prevention of biofilm (new coatings and paint, new surface materials, and surface modifications), nanotechnology (micro- and nanoemulsion) and controlling biofilms with enzymes (deoxyribonuclease 1, lysostaphin, α-amylase, lyase, and lactonase), photodynamic therapy, biosurfactants, bacteriocin, bioelectric approach, and ultrasonic treatment (Sadekuzzaman et al. 2015). The design and development of potential antibiofilm strategies have gained much interest in the field of medicine. Still, biomedical researchers are in urge for development of alternative methods to inhibit biofilm-associated infections.
13.1.5 The Emergence of Antimicrobial Photodynamic Therapy
In the array of promising novel therapeutic methods, light-based therapy known as photodynamic therapy (PDT) is introduced. PDT was discovered by Oskar Raab and Hermann von Tappeiner 100 years ago. Now PDT is known as alternative treatment modality for localized infections other than tumor cells. Antimicrobial photodynamic inactivation (aPDI) is a potential antimicrobial method that works on several factors of multidrug resistance patterns such as virulence traits, biofilms, spores, and efflux pumps (St. Denis et al. 2011). aPDI involves the integration of harmless light of appropriate wavelength with light-sensitive dye or photosensitizer in presence of oxygen present in/around the cells. The photoactivated photosensitizer is excited to an energetic state where it undergoes collision with oxygen and results in the generation of cytotoxic reactive oxygen species. There are many advantages of aPDI over conventional therapies which make it superior. aPDI never leads to the development of resistance in microorganisms, and the effective action is more rapid compared to other methods. This method is effective for the photoinactivation of both native bacterial strains and multidrug-resistant strains (Dai et al. 2010). The photophysical processes behind aPDI are classified into type I and type II mechanisms. Both type I and II can occur together based on the type of photosensitizer (PS) and the microenvironment of PS used. PS excited by light is entered to a long-lived triplet state where it interacts with molecular oxygen in type I (energy transfer) or type II (electron transfer) mechanism. Free radicals such as superoxide anion and hydroxyl radicals are produced by type I, and singlet oxygen is produced by type II process (Huang et al. 2012a).
Several life-threatening pathogens of humans that are resistant to the available antibiotics can be treated by aPDI. There are several categories of PS available for the effective photoinactivation of pathogens. New methylene blue and dimethylmethylene blue from phenothiazinium family of PS were reported for phototoxicity against MRSA, fungi, and some Gram-negative bacteria, revealing their broad spectrum of action (Sperandio et al. 2013). The photodamage caused by PS against microorganisms includes morphological and functional changes (Fig. 13.2). It can be loss of enzyme activity, protein oxidation, lipid peroxidation, DNA damage, formation of protein-protein cross-links, inhibition of metabolic process, change in the mesosome structure, damage to the cell membrane, cytoplasmic leakage, and inactivation of membrane transport system.
13.2 Antimicrobial Photodynamic Therapy and Nanotechnology
Ideal characteristics of PS for optimal photoinactivation include purity of the PS at a stable composition; solubility in aqueous solutions; high quantum yield of ROS for maximum potential; safe, nontoxic nature; and selectivity toward target cells instead of host cells. Still, many photosensitizers such as phthalocyanines, chlorins, and porphyrins that are highly lipophilic tend to aggregate in physiological solutions that results in poor aPDI (Jori et al. 2006). aPDI requires various tools for the optimal delivery of PS molecules to the target cells. The field of nanotechnology enhanced the antimicrobial photodynamic therapy and eliminated the limitations related to PS as the nanoparticles can be employed as PS carrier to the microbial cells. Several suitable PS nanocarriers and conjugates were studied with maximum antimicrobial action. Liposomes, micelles, and nanoparticles are studied widely as carriers with improved PS delivery (Kashef et al. 2017) (Table 13.1).
The unique features of nanoparticles include their nanoscale size, high surface-to-volume ratio, and tunable morphology which allows the application of nanotechnology in aPDI. The physical and chemical properties of nanoparticles (NPs) enable them to cross the biological barriers and gain the access to target site. Manipulation of NPs in their shape, chemical properties, and size facilitates the molecular interaction of the drug or PS by increasing the potential in therapy. Also they are engineered to deliver the therapeutic agents precisely to the target site. Application of nanotechnology gained importance in aPDI as the effectiveness of therapy increases with NPs. The bacterial inactivation kinetics of PS is significantly improved by the use of nanoparticles (St. Denis et al. 2011). The application of nanotechnology in aPDI includes delivery of PS by encapsulating PS in NPs, increased quantum yield of ROS by covalent attachment of PS to NPs, and NPs acting as photosensitizers (fullerenes, titanium oxide, etc.) (Fig. 13.3).
13.2.1 Fullerenes
Fullerenes are allotropic form of carbon with a closed cage shape, and the number of carbon molecules can be of 60, 70, 72, 76, 84, and up to 100. Fullerenes gained much attention in aPDI due to their tunability to impart higher ROS generation for effective photodestruction. Scientists have explored fullerenes for the delivery of PS by attaching to the hydrophilic or amphiphilic groups added. Fullerenes are superior to the conventional PS in many cases. They are more photostable and less photoinactivated compared to the tetrapyrroles. Fullerenes generate ROS through both type I and II pathways. Light-harvesting antenna can be attached to the C60 fullerenes to enhance the quantum yield of ROS. Moreover, self-assembly of fullerenes into vesicles enhances the tissue-targeting property and also allows multivalent drug deliver to cells (Huang et al. 2012b). A novel N,N-dimethyl-2-(4′-N,N,N-trimethylaminophenyl)fulleropyrrolidinium iodide (DTC(60)(2+)) synthesized effectively and photoinactivated E. coli with a 3.5 log decrease in the cells when treated with 1 μM of fullerene derivative for 30 min exposure (Mroz et al. 2007). Buckminster fullerene (C60) photoinactivated the enveloped virus, Semliki Forest virus or vesicular stomatitis virus, when irradiated with visible light for 5 h and resulted in the reduction of virion units to 7 logs (Käsermann and Kempf 1998). Fullerenes have been tested for their in vivo photoinactivation capacity in mice model infected with bacteria. An excision mice wound infection model inoculated with Proteus mirabilis and Pseudomonas aeruginosa was photoinactivated using tris-cationic BF6 fullerenes and irradiated with a white light of 400–700 nm. Mice infected with P. mirabilis showed an 82% survival by fullerene-mediated aPDI, and mice infected with P. aeruginosa showed survival of 60% when tobramycin is combined with aPDI for synergistic therapeutic effect (Sharma et al. 2011).
Zhao et al. (2019) described aPDI of plant pathogenic fungi, Sclerotinia sclerotiorum and Fusarium graminearum, with self-n-doped fullerene ammonium halides. Studies have verified that improved antifungal activity was not dependent on ROS production but because of the reducing property of halide anions (Zhao et al. 2019). Photoactivated C60 fullerenes reduced the infectious titer of iridovirus by 4.5 lg ID 50/ml units by a light exposure for 1 h (Rud et al. 2012). Scientists have reported the importance of charged moieties on fullerenes and their photoinactivation ability. In the study, a series of cationic fullerenes were used as PS against S. aureus, E. coli, and C. albicans. Tetra cationic derivative of fullerene was found to be the most active against S. aureus, whereas C. albicans showed resistance to aPDI, and intermediate activity was noticed against E. coli (Mizuno et al. 2011). Antimicrobial photodynamic activity of fullerenes and their hydroxylated derivatives, fullerenols, showed highest activity against Malassezia furfur, C. albicans, Staphylococcus epidermidis, and Propionibacterium acnes. The antimicrobial activity of fullerenes against fungi was higher than the bacteria due to their greater interaction with the fungal cell wall components (Aoshima et al. 2009).
13.2.2 Carbon Nanotubes and Graphene
Carbon nanotubes (CNT) are carbon allotropes with cylinder structure made of graphene sheets. CNTs are categorized as single-walled and multiwalled carbon nanotubes, where single-walled are made by wrapping a single layer of graphene sheet onto a seamless cylinder and multiwalled with multiple layers of graphene (Wang et al. 2009). Graphene oxide (GO) is made of sp2 and sp3 hybridized carbon atoms and gained much interest in aPDI due to the well-dispersed stability in solution, large surface area, and excellent biocompatibility (Wang et al. 2011). The unique optical properties of CNT and graphene oxide (GO) allow them to absorb light in the range of 700–1100 nm. The NIR irradiation makes them suitable for all biological applications, targeted treatment, and deeper penetration into tissues. These nanomaterials exhibit photoinactivation properties and antibacterial activities (Weissleder 2001). Graphene nanowalls with stainless steel as substrates damaged cell membrane of S. aureus within 1 h of interaction with bacteria (Akhavan and Ghaderi 2010). GO/titanium oxide films exhibited phototoxicity against E. coli after 4 h of solar light exposure (Akhavan and Ghaderi 2009). The ability of carbon nanotubes and GO to inactivate bacteria after few minutes of interaction is well studied. Magnetic reduced GO functionalized with glutaraldehyde effectively killed E. coli and S. aureus under NIR laser irradiation (Wu et al. 2013). It reduced 99% of Gram-negative and Gram-positive bacterial cells upon 10 min of exposure. Graphene quantum dots synthesized with two photon excitation, two photon stability, strong two photon luminescence, and two photon absorption in NIR region showed increased phototoxicity against E. coli and MRSA (Kuo et al. 2016). The toxicity mechanisms of CNTs include disruption of metabolic pathways, oxidative stress, damage to the cell membrane, generation of ROS, and oxidative stress.
Bacteria were damaged when contact with CNTs due to the interaction with the cell membrane. Single-walled CNTs were more toxic in photoinactivation of bacteria than multiwalled due to their size (Kang et al. 2008). Reports are available on the antibacterial and antiviral applications of CNT-drug conjugates. Multiwalled carbon nanotubes conjugated with protoporphyrin IX (PPIX) were inactivated 80% of S. aureus colonies within 1 h of visible light exposure. The photodamage was due to the combined effect, i.e., mechanical strength of CNT and biocidal nature of porphyrins (Spagnul et al. 2015). Banerjee et al. (2012) investigated antiviral photodynamic inactivation of PPIX-conjugated multiwalled carbon nanotubes against influenza virus. It was found that visible-light-mediated photoinactivation reduced the ability of virus particles to infect mammalian cells without any development of resistance (Banerjee et al. 2012).
13.2.3 Metal NPs in aPDT
Among metals, gold (Au) and silver (Ag) are involved in the plasmonic enhancement of aPDT. These metal NPs (AuNPs and AgNPs) potentiate the optical field near to the surface due to the electron conductance by local electric field and finally increase the photoactivity of PS attached to it (Huang et al. 2012b). Methylene blue-conjugated AuNPs reduced the viable count of S. aureus to three percentages on photoinactivation with diode laser of 660 nm. Gold NPs were found to be effective dye carrier (Tawfik et al. 2015). Methylene blue-conjugated AuNPs photoinactivated nosocomially acquired C. albicans biofilms through type I toxicity (Khan et al. 2012). AuNPs with PPIX was employed previously for the photoinactivation of S. aureus using xenon light. Protein damage that occurred after aPDT was one of the bactericidal effect noticed (Fathi et al. 2013). Gold nanorods functionalized with a series of boron dipyrromethene (BODIPY) dyes were proposed as good PS for antimicrobial photodynamic inactivation which results in high quantum yield of singlet oxygen and low fluorescent yields (Kubheka et al. 2016).
Silver is a known antimicrobial agent and has good affinity toward sulfur and phosphorus atoms in biomolecules. AuNPs can cause damage to the cell membrane affecting the cell viability, involved in inhibition of enzyme required for DNA replication, and cause cell death. The antimicrobial activity of AuNPs depends on the size, shape, surface area, and dose of particles employed (Dakal et al. 2016; Durán et al. 2016; Matsumura et al. 2003). Misba et al. (2016) studied antibacterial and antibiofilm efficacy of novel AuNPs-toluidine blue conjugates against S. mutans. The study revealed that the viability of cells was reduced by 4 log 10 reductions. The conjugates exhibited bactericidal effect with different mechanisms of action such as antibiofilm activity, cell membrane damage, and leakage of cellular contents (Misba et al. 2016).
13.2.3.1 Titanium Oxide and Zinc Oxide
Zinc oxide (ZnO) and titanium oxide (TiO2) are effective photocatalysts of aPDI which produces ROS upon light exposure by transferring electrons. The most abundantly produced ROS are hydroxyl radicals. These metal NPs are able to excite with UV light and visible light (Rehman et al. 2009). TiO2 was found to be effective photocatalyst than ZnO for antimicrobial activity in disinfecting the wastewater (Foster et al. 2011). The antimicrobial activities of ZnO and TiO2 have been reported against broad spectrum of organisms along with the combined effects of metal oxide NPs under UV irradiation. Reported photoactivated ZnO and TiO2 nanoparticles significantly inhibited pathogens prevalent in infected wounds such as S. aureus and S. epidermidis (Lipovsky et al. 2011). An orthodontic adhesive containing cationic curcumin conjugated to ZnONPs was successfully used to control biofilms formed by cariogenic bacteria Lactobacillus acidophilus, Streptococcus sobrinus, and Streptococcus mutans and reduced their metabolic activity to 100% (Pourhajibagher et al. 2019).
ZnONPs showed antimicrobial potential against nosocomial pathogens especially imipenem- and colistin-resistant A. baumannii and K. pneumonia. The photodestruction activity of ZnONPs was due to membrane disruption, ROS generation, protein dysfunction, imbalanced metal homeostasis, and DNA damage (Yang et al. 2018; Bhuyan et al. 2015). In another study, combined action of photosensitizer and titanium oxide at very low concentration of nanoparticles was employed for effective antimicrobial activity. TiO-methylene blue conjugate showed good antimicrobial activity against E. coli, S. aureus, and C. albicans when irradiated with light at two wavelengths (405 and 625 nm) (Tuchina and Tuchin 2010). TiO2 nanoparticles photoactivated by UVA light produced reactive oxygen species and exhibited antimicrobial reduction up to 6 logs against broad-spectrum microorganisms such as fungi, Gram-positive bacteria, and Gram-negative bacteria (Huang et al. 2016). Nitrogen doped onto TiO2NPs used in dental resin formulations showed antibacterial activity against E. coli after 1 h of exposure with blue light (Zane et al. 2016).
13.3 Nanocarriers in aPDT
A nanocarrier in antimicrobial photodynamic therapy offers wide applications. Nanocarriers used in aPDT help in the controlled and sustained release of PS, targeted PS delivery, and less toxicity to host cells. Both hydrophilic and hydrophobic drugs can be encapsulated into NPs that results in the successful penetration of drugs. Several PS tend to form aggregates in aqueous solutions and form inactive photosensitizers. Some PSs is unable to cross the biofilms and penetrate into the bacterial cell. The advantages of nanocarriers in aPDT include the enhanced inactivation kinetics of PS, improved quantum ROS yield, and use as photosensitizers. Several metal-based NPs and carbon-based NPs are successful nanocarriers of PSs to bacteria. Carboxyl-functionalized carbon nanotubes were used as carriers of methylene blue for the effective photodestruction of E. coli and S. aureus (Parasuraman et al. 2019). There are other inorganic NPs such as upconversion NPs, magnetic NPs, and calcium phosphate NPs that act as good drug carriers for antimicrobial photodynamic inactivation. Nanocarriers used in aPDT include polymeric NPs, nanomicelles, liposomes, and nanoemulsions for improved delivery of drugs and reduced minimum inhibitory concentration of drugs.
13.3.1 Liposomes
There are several nanocarriers used for the effective and improved delivery of drugs. Liposomes are having micro- or nanostructured vesicles formed by lipid bilayer around the aqueous core with size ranging from 50 to 1000 nm (Derycke 2004). Liposomes are widely used nanocarriers as they are able to carry hydrophilic drugs in aqueous core and hydrophobic drugs in fatty acid chains in the lipid bilayers (Torchilin 2005). Liposomes in conjugation with different PS with targeted delivery are successfully applied against many bacteria in vitro. The enhanced PS delivery to the target bacteria is mediated by combining liposomes with cationic phospholipids such as dimethyldioctadecylammonium bromide or sterilamine. Liposomes imparted with positive charges help in the stronger attachment to the negatively charged bacterial surface. This helps in the selective delivery of drugs to the bacteria over host cells (Paulo et al. 2011).
In a study, liposomes loaded with hematoporphyrin eradicated Gram-positive pathogens such as MSSA and MRSA (Tsai et al. 2009). Modified liposomes carrying novel antimicrobial peptide and potent PS temoporfin were used for the effective delivery of drug to bacteria. The targeted delivery of temoporfin loaded in liposomes eradicated MRSA and reduced P. aeruginosa by 3.3 log 10 when irradiated with 625 nm laser (Yang et al. 2011). Methylene blue- and toluidine blue-encapsulated liposomes exhibited 3 log reductions in the growth of S. aureus and E. coli compared to free liposomes when excited under blue light (Nakonechny et al. 2010).
13.3.2 Polymeric Nanoparticles
Polymeric nanoparticles are well-known drug delivery systems in aPDI. The polymeric nanoparticles are synthesized using different substrates including silica, proteins (collagen, human seroalbumin), poly lactic-co-glycolic acid (PLGA), and polysaccharides (alginate, dextran, and chitosan) (Prasad et al. 2017). Among all the polymeric NPs, PLGA exhibited more photodestruction on bacteria (Pagonis et al. 2010). These NPs are capable of concentrating more PS on bacterial cell wall resulting in the lethal damage to the bacteria. The polymeric NPs are synthesized in such a way that PS binds firmly to the membrane. The different chemical functionalization of polymeric NPs helps in the controlled release of drugs and targeted delivery (Hah et al. 2011). Methylene blue-loaded PLGA NPs when irradiated with a red light of 660 nm inhibited dental plaque pathogen of humans. Methylene blue PLGA NPs eliminated the dental plaque microorganisms in the biofilm stage by 25% more than that of biofilms treated with MB (de Freitas et al. 2016). In another study, PLGA nanoparticles encapsulated with methylene blue showed phototoxicity against planktonic cells and biofilms of dental plaque microorganisms isolated from chronic periodontitis patients (Klepac-Ceraj et al. 2011). Curcumin-encapsulated polymeric NPs (PLGA and dextran sulfate) with enhanced water solubility were employed for antimicrobial photodynamic inactivation of C. albicans and for oral candidiasis (Sakima et al. 2018).
13.3.3 Nanoemulsions
Nanoemulsions (NEs) are made of two immiscible liquids where one liquid is continuous phase and other as noncontinuous droplets. The diameter of these droplets is smaller than 300 nm. Like liposomes, nanoemulsions are also used for improving the properties of hydrophobic PS. These emulsions are employed particularly for topical drug delivery systems. NEs are known as skin permeation inducers. NEs with skin permeation ability are applied in aPDT for superficial skin infections because they can penetrate the stratum corneum to reach the deeper side of the epidermis. The inability of some hydrophilic drugs or PS to reach lower epidermis layer can be incorporated into nanoemulsion (Maisch et al. 2009). NEs exhibit broad-spectrum antimicrobial action with less generation of resistance and are suitable for surface contamination and wound treatment (Hwang et al. 2013). Ribeiro et al. (2015) described photodynamic antibiofilm therapy of MRSA and MSSA using chloroaluminum phthalocyanine encapsulated in NEs on irradiation with LED source (Ribeiro et al. 2015). The cell metabolism of MSSA and MRSA was reduced by 80% and 73%, respectively, with significant reduction in the CFU/ml of bacteria (Ribeiro et al. 2015). Scientists have reported that cationic NEs with zinc 2,9,16,23-tetrakis(phenylthio)-29H,31H-phthalocyanine reduced the biofilms formed by C. albicans and other fungi such as T. mucoides and K. ohmeri. The biofilms of C. albicans were reduced by 0.45 log 10 and other fungi reduced to 0.85 and 0.84 log 10 (Junqueira et al. 2012).
13.3.4 Nanomicelles
Nanomicelles are more appropriate for the delivery of PS than liposomes as they improve the solubility of PS and prevent the aggregation of PS in aqueous solutions. Preparation and scale up of micelles are much easier than that of liposomes and are widely used drug carriers (Tsai et al. 2009). Aluminum chloride phthalocyanine formulated in block copolymers of micelles proved to be potential drug delivery system and antimicrobial photodynamic agent against S. aureus and C. albicans (Vilsinski et al. 2015). Hypericin-encapsulated pluronic P123 micelles were reported as promising PS for the treatment of chronic infections caused by Gram-positive bacteria. The biofilms of E. faecalis and S. aureus were reduced to 2.86 and 2.30 CFU log reductions (Vilsinski et al. 2015). Chitosan micelles encapsulated with thymol were synthesized for the effective aPDT against biofilms. Light controllable micelles are formulated for controlled release of thymol which generated ROS with strong bactericidal effect on biofilms of Listeria monocytogenes and S. aureus (Wang et al. 2019).
13.4 Conclusions
In this chapter, we have summarized the recent advancement and developments occurred in the photoinactivation of microorganisms using nanostructures. Nanostructures alone or in conjugation with conventional photosensitizers are photoactivated under visible light and employed as a promising and alternative therapeutic strategies for the eradication and elimination of antimicrobial resistance bacteria and biofilms. Several nanostructures are applied as dye or drug carriers to the target bacteria for antimicrobial and antibiofilm therapy. The disadvantages of traditional photosensitizers have forced the integration of nanotechnology in aPDT. The solubility and stability of PS are improved through the use of dye delivery agent. These dye delivery agents enhance the antimicrobial photoinactivation of PS by increasing the solubility of dyes and improving the photoinactivation kinetics and quantum yield of ROS.
References
Akhavan O, Ghaderi E (2009) Photocatalytic reduction of graphene oxide nanosheets on TiO2 thin film for photoinactivation of bacteria in solar light irradiation. J Phys Chem C 113:20214–20220. https://doi.org/10.1021/jp906325q
Akhavan O, Ghaderi E (2010) Toxicity of graphene and graphene oxide nanowalls against bacteria. ACS Nano 4:5731–5736. https://doi.org/10.1021/nn101390x
Aoshima H, Kokubo K, Shirakawa S et al (2009) Antimicrobial activity of fullerenes and their hydroxylated derivatives. Biocontrol Sci 14:69–72. https://doi.org/10.4265/bio.14.69
Aziz N, Fatma T, Varma A, Prasad R (2014) Biogenic synthesis of silver nanoparticles using Scenedesmus abundans and evaluation of their antibacterial activity. J Nanopart 2014:689419. https://doi.org/10.1155/2014/689419
Aziz N, Faraz M, Pandey R, Sakir M, Fatma T, Varma A, Barman I, Prasad R (2015) Facile algae-derived route to biogenic silver nanoparticles: Synthesis, antibacterial and photocatalytic properties. Langmuir 31:11605−11612. https://doi.org/10.1021/acs.langmuir.5b03081
Aziz N, Pandey R, Barman I, Prasad R (2016) Leveraging the attributes of Mucor hiemalis-derived silver nanoparticles for a synergistic broad-spectrum antimicrobial platform. Front Microbiol 7:1984. https://doi.org/10.3389/fmicb.2016.01984
Banerjee I, Douaisi MP, Mondal D, Kane RS (2012) Light-activated nanotube–porphyrin conjugates as effective antiviral agents. Nanotechnology 23:105101. https://doi.org/10.1088/0957-4484/23/10/105101
Bhuyan T, Mishra K, Khanuja M, Prasad R, Varma A (2015) Biosynthesis of zinc oxide nanoparticles from Azadirachta indica for antibacterial and photocatalytic applications. Mater Sci Semicond Process 32:55–61
Bjarnsholt T (2013) The role of bacterial biofilms in chronic infections. APMIS 121:1–58. https://doi.org/10.1111/apm.12099
Ceri H, Olson ME, Turner RJ (2010) Needed, new paradigms in antibiotic development. Expert Opin Pharmacother 11:1233–1237. https://doi.org/10.1517/14656561003724747
Chadha T (2012) Antibiotic resistant genes in natural environment. Agrotechnology 01:1–3. https://doi.org/10.4172/2168-9881.1000104
Costerton JW, Lewandowski Z, Caldwell DE et al (1995) Microbial biofilms. Annu Rev Microbiol 49:711–745. https://doi.org/10.1146/annurev.mi.49.100195.003431
Dai T, Tegos GP, Zhiyentayev T et al (2010) Photodynamic therapy for methicillin-resistant Staphylococcus aureus infection in a mouse skin abrasion model. Lasers Surg Med 42:38–44. https://doi.org/10.1002/lsm.20887
Dakal TC, Kumar A, Majumdar RS, Yadav V (2016) Mechanistic basis of antimicrobial actions of silver nanoparticles. Front Microbiol 7:1–17. https://doi.org/10.3389/fmicb.2016.01831
Davies D (2003) Understanding biofilm resistance to antibacterial agents. Nat Rev Drug Discov 2:114–122. https://doi.org/10.1038/nrd1008
De Freitas LM, Calixto GMF, Chorilli M et al (2016) Polymeric nanoparticle-based photodynamic therapy for chronic periodontitis in vivo. Int J Mol Sci 17:769. https://doi.org/10.3390/ijms17050769
De la Fuente-Nunez C, Torres MD, Mojica FJ, Lu TK (2017) Next-generation precision antimicrobials: towards personalized treatment of infectious diseases. Curr Opin Microbiol 37:95–102. https://doi.org/10.1016/j.mib.2017.05.014
Derycke A (2004) Liposomes for photodynamic therapy. Adv Drug Deliv Rev 56:17–30. https://doi.org/10.1016/j.addr.2003.07.014
Donlan RM (2002) Biofilms: microbial life on surfaces. Emerg Infect Dis 8:881–890. https://doi.org/10.3201/eid0809.020063
Drenkard E (2003) Antimicrobial resistance of Pseudomonas aeruginosa biofilms. Microbes Infect 5:1213–1219. https://doi.org/10.1016/j.micinf.2003.08.009
Drenkard E, Ausubel FM (2002) Pseudomonas biofilm formation and antibiotic resistance are linked to phenotypic variation. Nature 416:740–743. https://doi.org/10.1038/416740a
Durán N, Durán M, de Jesus MB et al (2016) Silver nanoparticles: a new view on mechanistic aspects on antimicrobial activity. Nanomed Nanotechnol Biol Med 12:789–799. https://doi.org/10.1016/j.nano.2015.11.016
Fathi A, Rasekaran R et al (2013) Influence of hydrogen peroxide or gold nanoparticles in protoporphyrin IX mediated antimicrobial photodynamic therapy on Staphylococcus aureus. Afr J Microbiol Res 7:4617–4624. https://doi.org/10.5897/2013.5885
Fernandes P, Martens E (2017) Antibiotics in late clinical development. Biochem Pharmacol 133:152–163. https://doi.org/10.1016/j.bcp.2016.09.025
Foster HA, Ditta IB, Varghese S, Steele A (2011) Photocatalytic disinfection using titanium dioxide: spectrum and mechanism of antimicrobial activity. Appl Microbiol Biotechnol 90:1847–1868. https://doi.org/10.1007/s00253-011-3213-7
Hah HJ, Kim G, Lee Y-EK et al (2011) Methylene blue-conjugated hydrogel nanoparticles and tumor-cell targeted photodynamic therapy. Macromol Biosci 11:90–99. https://doi.org/10.1002/mabi.201000231
Holmstrup P, Klausen B (2018) The growing problem of antimicrobial resistance. Oral Dis 24:291–295. https://doi.org/10.1111/odi.12610
Huang L, Xuan Y, Koide Y et al (2012a) Type I and type II mechanisms of antimicrobial photodynamic therapy: an in vitro study on Gram-negative and Gram-positive bacteria. Lasers Surg Med 44:490–499. https://doi.org/10.1002/lsm.22045
Huang Y-Y, Sharma SK, Dai T et al (2012b) Can nanotechnology potentiate photodynamic therapy? Nanotechnol Rev 1:111–146. https://doi.org/10.1515/ntrev-2011-0005
Huang Y-Y, Choi H, Kushida Y et al (2016) Broad-spectrum antimicrobial effects of photocatalysis using titanium dioxide nanoparticles are strongly potentiated by addition of potassium iodide. Antimicrob Agents Chemother 60:5445–5453. https://doi.org/10.1128/AAC.00980-16
Hwang YY, Ramalingam K, Bienek DR et al (2013) Antimicrobial activity of nanoemulsion in combination with cetylpyridinium chloride in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother 57:3568–3575. https://doi.org/10.1128/AAC.02109-12
Jasovský D, Littmann J, Zorzet A, Cars O (2016) Antimicrobial resistance—a threat to the world’s sustainable development. Ups J Med Sci 121:159–164. https://doi.org/10.1080/03009734.2016.1195900
Jing H, Mezgebe B, Aly Hassan A et al (2014) Experimental and modeling studies of sorption of ceria nanoparticle on microbial biofilms. Bioresour Technol 161:109–117. https://doi.org/10.1016/j.biortech.2014.03.015
Jori G, Fabris C, Soncin M et al (2006) Photodynamic therapy in the treatment of microbial infections: basic principles and perspective applications. Lasers Surg Med 38:468–481. https://doi.org/10.1002/lsm.20361
Junqueira JC, Jorge AOC, Barbosa JO et al (2012) Photodynamic inactivation of biofilms formed by Candida spp., Trichosporon mucoides, and Kodamaea ohmeri by cationic nanoemulsion of zinc 2,9,16,23-tetrakis(phenylthio)-29H, 31H-phthalocyanine (ZnPc). Lasers Med Sci 27:1205–1212. https://doi.org/10.1007/s10103-012-1050-2
Kang S, Herzberg M, Rodrigues DF, Elimelech M (2008) Antibacterial effects of carbon nanotubes: size does matter. Langmuir 24:6409–6413. https://doi.org/10.1021/la800951v
Käsermann F, Kempf C (1998) Buckminsterfullerene and photodynamic inactivation of viruses. Rev Med Virol 8:143–151. https://doi.org/10.1002/(SICI)1099-1654(199807/09)8:3<143::AID-RMV214>3.0.CO;2-B
Kashef N, Huang Y-Y, Hamblin MR (2017) Advances in antimicrobial photodynamic inactivation at the nanoscale. Nanophotonics 6:853–879. https://doi.org/10.1515/nanoph-2016-0189
Khan S, Khan AU, Azam A, Alam F (2012) Gold nanoparticles enhance methylene blue-induced photodynamic therapy: a novel therapeutic approach to inhibit Candida albicans biofilm. Int J Nanomedicine 2012:3245–3257. https://doi.org/10.2147/IJN.S31219
Klepac-Ceraj V, Patel N, Song X et al (2011) Photodynamic effects of methylene blue-loaded polymeric nanoparticles on dental plaque bacteria. Lasers Surg Med 43:600–606. https://doi.org/10.1002/lsm.21069
Kubheka G, Uddin I, Amuhaya E et al (2016) Synthesis and photophysicochemical properties of BODIPY dye functionalized gold nanorods for use in antimicrobial photodynamic therapy. J Porphyr Phthalocyanines 20:1016–1024. https://doi.org/10.1142/S108842461650070X
Kuo W-S, Chang C-Y, Chen H-H et al (2016) Two-photon photoexcited photodynamic therapy and contrast agent with antimicrobial graphene quantum dots. ACS Appl Mater Interfaces 8:30467–30474. https://doi.org/10.1021/acsami.6b12014
Lewis K (2001) Riddle of biofilm resistance. Antimicrob Agents Chemother 45:999–1007. https://doi.org/10.1128/AAC.45.4.999-1007.2001
Li X-Z, Nikaido H (2009) Efflux-mediated drug resistance in bacteria. Drugs 69:1555–1623. https://doi.org/10.2165/11317030-000000000-00000
Lipovsky A, Gedanken A, Nitzan Y, Lubart R (2011) Enhanced inactivation of bacteria by metal-oxide nanoparticles combined with visible light irradiation. Lasers Surg Med 43:236–240. https://doi.org/10.1002/lsm.21033
Llor C, Bjerrum L (2014) Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 5:229–241. https://doi.org/10.1177/2042098614554919
Lucky SS, Soo KC, Zhang Y (2015) Nanoparticles in photodynamic therapy. Chem Rev 115:1990–2042. https://doi.org/10.1021/cr5004198
Magadla A, Oluwole DO, Managa M, Nyokong T (2019) Physicochemical and antimicrobial photodynamic chemotherapy (against E. Coli) by indium phthalocyanines in the presence of silver-iron bimetallic nanoparticles. Polyhedron 40:2710–2721. https://doi.org/10.1016/j.poly.2019.01.032
Mah T-FC, O’Toole GA (2001) Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol 9:34–39. https://doi.org/10.1016/S0966-842X(00)01913-2
Maisch T, Santarelli F, Schreml S et al (2009) Fluorescence induction of protoporphyrin IX by a new 5-aminolevulinic acid nanoemulsion used for photodynamic therapy in a full-thickness ex vivo skin model. Exp Dermatol 19:e302–e305. https://doi.org/10.1111/j.1600-0625.2009.01001.x
Majik M, Parvatkar P (2013) Next generation biofilm inhibitors for Pseudomonas aeruginosa: synthesis and rational design approaches. Curr Top Med Chem 14:81–109. https://doi.org/10.2174/1568026613666131113152257
Matsumura Y, Yoshikata K, Kunisaki S, Tsuchido T (2003) Mode of bactericidal action of silver zeolite and its comparison with that of silver nitrate. Appl Environ Microbiol 69:4278–4281. https://doi.org/10.1128/AEM.69.7.4278-4281.2003
McAdam AJ, Hooper DC, DeMaria A et al (2012) Antibiotic resistance: how serious is the problem, and what can be done? Clin Chem 58:1182–1186. https://doi.org/10.1373/clinchem.2011.181636
Misba L, Kulshrestha S, Khan AU (2016) Antibiofilm action of a toluidine blue O-silver nanoparticle conjugate on Streptococcus mutans: a mechanism of type I photodynamic therapy. Biofouling 32:313–328. https://doi.org/10.1080/08927014.2016.1141899
Mizuno K, Zhiyentayev T, Huangv L et al (2011) Antimicrobial photodynamic therapy with functionalized fullerenes: quantitative structure-activity relationships. J Nanomed Nanotechnol 02:1–9. https://doi.org/10.4172/2157-7439.1000109
Mroz P, Tegos GP, Gali H et al (2007) Photodynamic therapy with fullerenes. Photochem Photobiol Sci 6:1139–1149. https://doi.org/10.1039/b711141j
Nakonechny F, Firer MA, Nitzan Y, Nisnevitch M (2010) Intracellular antimicrobial photodynamic therapy: a novel technique for efficient eradication of pathogenic bacteria. Photochem Photobiol 86:1350–1355. https://doi.org/10.1111/j.1751-1097.2010.00804.x
National Collaborating Centre for Infectious Diseases (2010) Proceedings of Community-Acquired Antimicrobial Resistance Consultation Notes, Winnipeg, MB, Canada, 10–11 February 2010 Available at: http://www.nccid.ca/files/caAMR_ConsultationNotes_final.pdf
Nombona N, Antunes E, Chidawanyika W et al (2012) Synthesis, photophysics and photochemistry of phthalocyanine-ɛ-polylysine conjugates in the presence of metal nanoparticles against Staphylococcus aureus. J Photochem Photobiol A Chem 233:24–33. https://doi.org/10.1016/j.jphotochem.2012.02.012
Pagonis TC, Chen J, Fontana CR et al (2010) Nanoparticle-based endodontic antimicrobial photodynamic therapy. J Endod 36:322–328. https://doi.org/10.1016/j.joen.2009.10.011
Paramanantham P, Antony AP, Sruthil Lal SB et al (2018) Antimicrobial photodynamic inactivation of fungal biofilm using amino functionalized mesoporous silica-rose bengal nanoconjugate against Candida albicans. Sci Afr e00007:1. https://doi.org/10.1016/j.sciaf.2018.e00007
Parasuraman P, Anju VT, Sruthil Lal S et al (2019) Synthesis and antimicrobial photodynamic effect of methylene blue conjugated carbon nanotubes on E. coli and S. aureus. Photochem Photobiol Sci 1(8):563–576. https://doi.org/10.1039/C8PP00369F
Paulo J, Longo F, Muehlmann LA, De Azevedo RB (2011) Nanostructured carriers for photodynamic therapy applications in microbiology, pp 189–196
Pissuwan D, Cortie CH, Valenzuela SM, Cortie MB (2010) Functionalised gold nanoparticles for controlling pathogenic bacteria. Trends Biotechnol 28:207–213. https://doi.org/10.1016/j.tibtech.2009.12.004
Pourhajibagher M, Salehi Vaziri A, Takzaree N, Ghorbanzadeh R (2019) Physico-mechanical and antimicrobial properties of an orthodontic adhesive containing cationic curcumin doped zinc oxide nanoparticles subjected to photodynamic therapy. Photodiagn Photodyn Ther 25:239–246. https://doi.org/10.1016/j.pdpdt.2019.01.002
Prasad R, Pandey R, Varma A, Barman I (2017) Polymer based nanoparticles for drug delivery systems and cancer therapeutics. In: Natural Polymers for Drug Delivery (eds. Kharkwal H and Janaswamy S), CAB International, UK. 53–70
Rehman S, Ullah R, Butt AM, Gohar ND (2009) Strategies of making TiO2 and ZnO visible light active. J Hazard Mater 170:560–569. https://doi.org/10.1016/j.jhazmat.2009.05.064
Ribeiro APD, Andrade MC, Bagnato VS et al (2015) Antimicrobial photodynamic therapy against pathogenic bacterial suspensions and biofilms using chloro-aluminum phthalocyanine encapsulated in nanoemulsions. Lasers Med Sci 30:549–559. https://doi.org/10.1007/s10103-013-1354-x
Rud Y, Buchatskyy L, Prylutskyy Y et al (2012) Using C 60 fullerenes for photodynamic inactivation of mosquito iridescent viruses. J Enzyme Inhib Med Chem 27:614–617. https://doi.org/10.3109/14756366.2011.601303
Sadekuzzaman M, Yang S, Mizan MFR, Ha SD (2015) Current and recent advanced strategies for combating biofilms. Compr Rev Food Sci Food Saf 14:491–509. https://doi.org/10.1111/1541-4337.12144
Sakima V, Barbugli P, Cerri P et al (2018) Antimicrobial photodynamic therapy mediated by curcumin-loaded polymeric nanoparticles in a murine model of oral candidiasis. Molecules 23:2075. https://doi.org/10.3390/molecules23082075
Santajit S, Indrawattana N (2016) Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed Res Int 2016:1–8. https://doi.org/10.1155/2016/2475067
Sharma SK, Chiang LY, Hamblin MR (2011) Photodynamic therapy with fullerenes in vivo: reality or a dream? Nanomedicine 6:1813–1825. https://doi.org/10.2217/nnm.11.144
Singh S, Singh SK, Chowdhury I, Singh R (2017) Understanding the mechanism of bacterial biofilms resistance to antimicrobial agents. Open Microbiol J 11:53–62. https://doi.org/10.2174/1874285801711010053
Spagnul C, Turner LC, Boyle RW (2015) Immobilized photosensitizers for antimicrobial applications. J Photochem Photobiol B Biol 150:11–30. https://doi.org/10.1016/j.jphotobiol.2015.04.021
Sperandio F, Huang Y-Y, Hamblin M (2013) Antimicrobial photodynamic therapy to kill Gram-negative bacteria. Recent Pat Antiinfect Drug Discov 8:108–120. https://doi.org/10.2174/1574891X113089990012
St. Denis TG, Dai T, Izikson L et al (2011) All you need is light. Virulence 2:509–520. https://doi.org/10.4161/viru.2.6.17889
Tawfik AA, Alsharnoubi J, Morsy M (2015) Photodynamic antibacterial enhanced effect of methylene blue-gold nanoparticles conjugate on Staphylococcal aureus isolated from impetigo lesions in vitro study. Photodiagn Photodyn Ther 12:215–220. https://doi.org/10.1016/j.pdpdt.2015.03.003
Torchilin V (2005) Fluorescence microscopy to follow the targeting of liposomes and micelles to cells and their intracellular fate. Adv Drug Deliv Rev 57:95–109. https://doi.org/10.1016/j.addr.2004.06.002
Tsai T, Yang Y-T, Wang T-H et al (2009) Improved photodynamic inactivation of Gram-positive bacteria using hematoporphyrin encapsulated in liposomes and micelles. Lasers Surg Med 41:316–322. https://doi.org/10.1002/lsm.20754
Tuchina ES, Tuchin VV (2010) TiO2 nanoparticle enhanced photodynamic inhibition of pathogens. Laser Phys Lett 7:607–612. https://doi.org/10.1002/lapl.201010030
Vilsinski BH, Gerola AP, Enumo JA et al (2015) Formulation of aluminum chloride phthalocyanine in pluronic TM P-123 and F-127 block copolymer micelles: photophysical properties and photodynamic inactivation of microorganisms. Photochem Photobiol 91:518–525. https://doi.org/10.1111/php.12421
Vrany JD, Stewart PS, Suci PA (1997) Comparison of recalcitrance to ciprofloxacin and levofloxacin exhibited by Pseudomonas aeruginosa biofilms displaying rapid-transport characteristics. Antimicrob Agents Chemother 41:1352–1358
Vt A, Paramanantham P, Sb SL et al (2018) Antimicrobial photodynamic activity of rose bengal conjugated multi walled carbon nanotubes against planktonic cells and biofilm of Escherichia coli. Photodiagn Photodyn Ther 24:300–310. https://doi.org/10.1016/j.pdpdt.2018.10.013
Wang X, Li Q, Xie J et al (2009) Fabrication of ultralong and electrically uniform single-walled carbon nanotubes on clean substrates. Nano Lett 9:3137–3141. https://doi.org/10.1021/nl901260b
Wang Y, Li Z, Wang J et al (2011) Graphene and graphene oxide: biofunctionalization and applications in biotechnology. Trends Biotechnol 29:205–212. https://doi.org/10.1016/j.tibtech.2011.01.008
Wang Z, Bai H, Lu C et al (2019) Light controllable chitosan micelles with ROS generation and essential oil release for the treatment of bacterial biofilm. Carbohydr Polym 205:533–539. https://doi.org/10.1016/j.carbpol.2018.10.095
Weissleder R (2001) A clearer vision for in vivo imaging. Nat Biotechnol 19:316–317. https://doi.org/10.1038/86684
Wilson DN (2014) Ribosome-targeting antibiotics and mechanisms of bacterial resistance. Nat Rev Microbiol 12:35–48. https://doi.org/10.1038/nrmicro3155
Wright G (2005) Bacterial resistance to antibiotics: enzymatic degradation and modification. Adv Drug Deliv Rev 57:1451–1470. https://doi.org/10.1016/j.addr.2005.04.002
Wu M-C, Deokar AR, Liao J-H et al (2013) Graphene-based photothermal agent for rapid and effective killing of bacteria. ACS Nano 7:1281–1290. https://doi.org/10.1021/nn304782d
Yang K, Gitter B, Rüger R et al (2011) Antimicrobial peptide-modified liposomes for bacteria targeted delivery of temoporfin in photodynamic antimicrobial chemotherapy. Photochem Photobiol Sci 10:1593. https://doi.org/10.1039/c1pp05100h
Yang M, Chang K, Chen L et al (2018) Blue light irradiation triggers the antimicrobial potential of ZnO nanoparticles on drug-resistant Acinetobacter baumannii. J Photochem Photobiol B Biol 180:235–242. https://doi.org/10.1016/j.jphotobiol.2018.02.003
Yin R, Agrawal T, Khan U et al (2015) Antimicrobial photodynamic inactivation in nanomedicine: small light strides against bad bugs. Nanomedicine 10:2379–2404. https://doi.org/10.2217/nnm.15.67
Zane A, Zuo R, Villamena F et al (2016) Biocompatibility and antibacterial activity of nitrogen-doped titanium dioxide nanoparticles for use in dental resin formulations. Int J Nanomedicine 11:6459–6470. https://doi.org/10.2147/IJN.S117584
Zhao J, Lin Z, Fang S et al (2019) Photoexcitation of self-n-doped fullerene ammonium halides: the role of halide ion and a possible synergistic dual-redox cycle mechanism within their aggregate. J Photochem Photobiol A Chem 373:131–138. https://doi.org/10.1016/j.jphotochem.2019.01.008
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Anju, V.T., Siddhardha, B., Dyavaiah, M. (2020). Nanostructures for Antimicrobial and Antibiofilm Photodynamic Therapy. In: Prasad, R., Siddhardha, B., Dyavaiah, M. (eds) Nanostructures for Antimicrobial and Antibiofilm Applications. Nanotechnology in the Life Sciences. Springer, Cham. https://doi.org/10.1007/978-3-030-40337-9_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-40337-9_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40336-2
Online ISBN: 978-3-030-40337-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)