Abstract
Olecranon fractures are very common and, in most cases, require surgery, using either tension band or plate fixation. Studies comparing both methods have failed to show any significant clinical difference, and tension band fixation remains a cost-effective treatment option for simple fractures. However, it must be performed according to proper fixation methods, which is more difficult than it appears to be at first glance.
Indeed, each fragment should be fixed in the case of an olecranon fracture to recreate a stable and mobile elbow. Tension band surgical fixation, using K-wires and metallic wires, is a good surgical option in cases of simple transverse fractures, without elbow instability or dislocation. In order to accomplish this technique, the surgeon requires lateral decubitus positioning, safe surgical approach, anatomic reduction of each fragment with independent small threaded wires, and tension band fixation of the tricipital fragment. Complex fractures and fracture dislocations are preferably treated with a designated periarticular locking plate.
This chapter will present a descriptive classification of olecranon fractures, clarify the indication for tension band in olecranon fractures with illustrative cases, and review surgical tips to increase the solidity of olecranon tension bands, based on biomechanical and clinical studies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Tension band fixation is a classic fracture repair method which is most frequently used in olecranon fractures [1]. According to the theory developed by Pauwels in the 1980s [2], a curved tubular structure submitted to a compressive force presents with a tension side and a compressive side [3]; therefore, when a tension band is applied on the tension side, it will concomitantly increase compression on the opposite side. Following this accepted 40-year-old principle, it is mandatory for the bone on the opposite side of the tension band to present a frank fracture line, with no bone loss and no comminution.
However, the olecranon cannot exactly be described as a curved tubular bone submitted to a compression force, and studies have revealed the weak compression created by olecranon tension bands [4]. Brink et al. actually report greater compression in active extension [5]. Indeed, during active motion, multiple force vectors are applied to the first 8 cm of the olecranon in a complex axis. Anatomic causes include the proximal ulna dorsal angulation (PUDA) , which varies from 0 to 14 degrees [6], and a 14-degree varus angulation, and they need to be considered [7] to obtain anatomic reduction. This portion of the ulna includes two joints, but since it is not a diaphysis, it does require precise anatomic reduction. We could also say that it is part of another “joint,” the forearm pro-supination axis – now considered to be an important virtual articulation. These three joints can be negatively impacted during the treatment of proximal ulna fractures. One such example is PUDA malalignment, shown in the lab to cause radial head subluxation [8]. A case-controlled study on olecranon fracture fixation revealed that patients with a non-anatomic reduction of their PUDA of 5 degrees or more presented with worse outcomes in terms of range of motion [9]. Non-anatomic reduction of the sigmoid notch joint surface is also associated to worse outcomes. Finally, the proximal ulna is the insertion site of the elbow’s collateral ligaments, which need to be preserved or repaired in complex olecranon fracture cases.
That being said, all studies comparing plate and tension band (TB) fixation in olecranon fractures have failed to show any significant clinical difference (Table 10.1) [10,11,12,13,14,15]. Some authors found more complications with the tension band method, mainly associated with a higher hardware removal rate [11, 12]. A systematic review published in 2016 reported equivalent results for both methods, but more reoperations in the TB groups [16]. One of the elements favoring tension band fixation is its much lower cost compared to locking plate fixation. Indeed, with the tension band method, total treatment costs are lower by more than 50%, including reoperation, and the implant itself is six times cheaper [10,11,12,13,14,15, 17]. It therefore should still be used in the case of a simple fracture, in accordance with biomechanical principles. However, two recent papers have shown that it is not as easy as it might appear at first glance to perform a “perfect” tension band of the olecranon, with a vast majority of cases not following guidelines [18, 19]. Criteria used by these authors can be found in Table 10.2 [10,11,12,13,14,15]. Contrary to clinical reports, biomechanical studies show better performance with locking plate systems [4, 20], although it is difficult to accurately compare the varying biomechanical setups from the different studies. When compression is measured, the locking plate creates 343 N of compression vs 77 N for the tension band [4], and on cyclic loading, there is less fragment displacement with plate fixation (0.25 mm vs 1.12 mm) [20].
This chapter will present, first, a descriptive classification of olecranon fractures, to help surgeons understand the injury; second, it will clarify the indication for tension band in olecranon fractures with illustrative cases; and third, it will review surgical tips to increase the solidity of olecranon tension band, based on biomechanical and clinical studies.
Descriptive Olecranon Fracture Classification
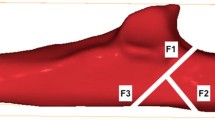
Several olecranon fracture classifications can be used, and in my daily practice, I prefer to make a list of all fractured fragments when planning for surgery. The principal fragments are presented in Fig. 10.1 and listed below:
-
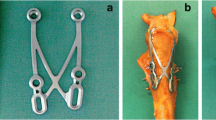
Tricipital fragment (Fig. 10.2)
-
Coronoid fragment
-
Tip of the coronoid
-
Anteromedial facet
-
-
Posterior fragment (Fig. 10.4)
-
Supinator crest (lateral collateral ligament)
-
Sublime tubercle (medial collateral ligament)
Each fragment needs to be fixed in the case of an olecranon fracture to recreate a stable and mobile elbow. Whenever more than the tricipital fragment is involved, a CT scan should be performed, with 3D reconstruction if possible. Failure to identify and treat all fragments can lead to disastrous results (Fig. 10.5).
Complex proximal ulna fracture with initial treatment neglecting the coronoid fragment leading to elbow subluxation. In the presence of concomitant olecranon fracture and coronoid fracture, the coronoid should be fixed first, in flexion. The olecranon is then fixed in extension. Tension band is not recommended in that situation. Fracture fixation revision is showed with coronoid fixation first
Indications for Olecranon Fracture Tension Band
Tension band surgical fixation, using K-wires and metallic wires, is a good surgical fixation option in cases of a simple fracture, without elbow instability or dislocation. For example, a fracture with a tricipital fragment and an intermediate fragment could be fixed by the tension band method in non-osteopenic bone. The intermediate fragment is reduced and fixed, first with a threaded K-wire, followed by a classic tension band. When the coronoid is involved or there is a combined fragmentation of the intermediate fragment and the posterior fragment, plate fixation will create a more stable construct. When there are associated injuries to the radial head and/or ligaments, plate fixation is also more stable (Fig. 10.6).
Surgical Tips and Tricks Based on Biomechanical Studies
A preoperative x-ray of the normal side is useful in complex fractures to achieve patient specific PUDA. It is easier to repair olecranon fractures in lateral decubitus, with the fractured elbow on top. An elbow support is used under the arm and positioned as close as possible to the shoulder, allowing for fluoroscopy visualization. Skin incision is done as a lazy C shape starting on the ridge of the ulna, 7 cm distal to the tip of the olecranon. The incision is directed proximally, 1 cm lateral to the tip of the olecranon. The incision ends in the center of the posterior elbow, 2 cm proximal to the olecranon to expose and protect the triceps. Full-thickness skin flaps are created with a number 15 blade, just enough to see the fracture fragments. Soft tissues are reflected from the fracture edge and the medial and lateral side of the ulnar ridge. Ulnar nerve and collateral ligament insertions should be preserved but not necessarily identified. A sterile Mayo table is also used to support the forearm, with the elbow in extension for the reduction of the posterior and tricipital fragments. Coronoid fragments are reduced with the elbow in flexion [22]. The coronoid is the keystone for elbow stability and usually requires plate fixation [23]. A sterile tourniquet is used and inflated as little as possible, to decrease postoperative edema and pain. Anatomic reduction of all six potential fragments, of both joint surfaces, the PUDA, and the varus angle, need to be as similar as possible to the contralateral side prior to definitive fixation. Small threaded K-wires could be used for interfragmentary fixation of intermediate fragments before “closing” the tricipital fragment [24].
K-Wires
After anatomic reduction with a reduction clamp and temporary K-wires, two 1.6-mm K-wires are drilled in the ulna; this is easier with the elbow in 30 degrees of flexion. The entry points need to be 5 mm anterior to the tip of the olecranon and should be parallel. Views differ on whether or not to enter the anterior cortex:
-
The anterior cortex fixation philosophy is supported by biomechanical studies revealing a stronger pull-out strength [25]. When chosen, it needs to be angled at 25 degrees on the lateral view. This angle represents a compromise, decreasing the probability of intra-articular penetration [26] and neurovascular injuries [27]. Structures at risk are the ulnar artery and anterior interosseous nerve [27]. To prevent synostosis, K-wires should be directly aligned with the ulna and not directed toward the radius [28]. If a surgeon chooses an anterior cortex fixation, it is important to retract the wire by 5 mm, prior to bending and cutting it, making it possible to bend the pin 5 mm away from the cortex. A 5 mm of bent stump is left and the remaining wire is cut. The K-wire is then twisted 180 degrees to grab the metallic wire. The K-wire is finally impacted in the bone for 5 mm. Doing this achieves maximal fixation and minimizes the risk to the anterior structures.
-
The intramedullary fixation philosophy is supported by clinical studies, which report neurovascular complications with the anterior cortex fixation as well as a higher risk of synostosis [29,30,31]. This method is weaker and K-wires are more likely to back out, especially if they are not impacted into the olecranon after having been bent and cut (Fig. 10.7). To create a stronger intramedullary fixation, surgeons can choose longer K-wires or a 6.5-mm cancellous screw [32, 33]. We do not recommend using large screws because of the risk of triceps fragment fragmentation [33].
Wire
A 1-mm wire is inserted through a 2-mm cortical tunnel, distal to the fracture. The two limbs are then crossed. A second wire then goes under the K-wires in the triceps tendon. Precautions should be taken to protect the ulnar nerve on the medial side. K-wires are then retracted 5 mm, one at a time, to prevent fixation failure, before being bent, cut, and re-impacted in the ulnar cortex. Limbs of both wires can now be connected. Compression with the wires is created by a symmetrical rotation and gentle traction of the wires on each side of the fracture. Limbs are then cut and knots are buried in the soft tissue [34]. Alternatively, in an olecranon osteotomy model, Lalliss et al. showed similar strength using a heavy suture (FiberWire, Arthrex, Naples, FL, USA) [35].
Conclusion
Olecranon fractures are very common, requiring surgical interventions in the vast majority of cases. Tension band fixation is a cost-effective procedure favored in simple fractures; however, proper fixation methods need to be followed to prevent failure. These include lateral decubitus positioning, safe surgical approach, anatomic reduction of each fragment with independent small threaded wires, and tension band fixation of the tricipital fragment. Complex fractures and fracture dislocations are preferably treated with designated periarticular locking plates.
References
Wood T, Thomas K, Farrokhyar F, Ristevski B, Bhandari M, Petrisor B. A survey of current practices and preferences for internal fixation of displaced olecranon fractures. Can J Surg. 2015;58(4):250–6.
Pauwels F. Biomechanics of the locomotor apparatus. 1st ed. Berlin/Heidelberg/New York: Springer; 1980.
Hak DJ, Stewart RL. 3.2.3 Tension band principle. In: Rüedi TP, Buckley RE, Moran CG, editors. AO principles of fracture management. 2nd ed. Stuttgart: Thieme; 2007. https://www2.aofoundation.org/wps/portal/!ut/p/a0/04_Sj9CPykssy0xPLMnMz0vMAfGjzOKN_A0M3D2DDbz9_UMMDRyDXQ3dw9wMDAzMjfULsh0VAbWjLW0!/?bone=Radius&segment=Distal&showPage=F&contentUrl=srg/popup/further_reading/PFxM2/323_Tension_bnd.jsp. Accessed 25 Oct 2018.
Wilson J, Bajwa A, Kamath V, Rangan A. Biomechanical comparison of interfragmentary compression in transverse fractures of the olecranon. J Bone Joint Surg Br. 2011;93(2):245–50.
Brink PR, Windolf M, de Boer P, Brianza S, Braunstein V, Schwieger K. Tension band wiring of the olecranon: is it really a dynamic principle of osteosynthesis? Injury. 2013;44(4):518–22.
Rouleau DM, Faber KJ, Athwal GS. The proximal ulna dorsal angulation: a radiographic study. J Shoulder Elb Surg. 2010;19(1):26–30.
Puchwein P, Schildhauer TA, Schöffmann S, Heidari N, Windisch G, Pichler W. Three-dimensional morphometry of the proximal ulna: a comparison to currently used anatomically preshaped ulna plates. J Shoulder Elb Surg. 2012;21(8):1018–23.
Sandman E, Canet F, Petit Y, Laflamme GY, Athwal GS, Rouleau DM. Radial head subluxation after malalignment of the proximal ulna: a biomechanical study. J Orthop Trauma. 2014;28(8):464–9.
Chapleau J, Balg F, Harvey EJ, Ménard J, Vauclair F, Laflamme GY, et al. Impact of olecranon fracture malunion: study on the importance of PUDA (proximal ulna dorsal angulation). Injury. 2016;47(11):2520–4.
Amini MH, Azar FM, Wilson BR, Smith RA, Mauck BM, Throckmorton TW. Comparison of outcomes and costs of tension-band and locking-plate osteosynthesis in transverse olecranon fractures: a matched-cohort study. Am J Orthop (Belle Mead NJ). 2015;44(7):E211–5.
Snoddy MC, Lang MF, An TJ, Mitchell PM, Grantham WJ, Hooe BS, et al. Olecranon fractures: factors influencing re-operation. Int Orthop. 2014;38(8):1711–6.
Tarallo L, Mugnai R, Adani R, Capra F, Zambianchi F, Catani F. Simple and comminuted displaced olecranon fractures: a clinical comparison between tension band wiring and plate fixation techniques. Arch Orthop Trauma Surg. 2014;134(8):1107–14.
DelSole EM, Pean CA, Tejwani NC, Egol KA. Outcome after olecranon fracture repair: does construct type matter? Eur J Orthop Surg Traumatol. 2016;26(2):153–9.
Liñán-Padilla A, Cáceres-Sánchez L. Type II olecranon fractures in patients over 65. Tension band or pre-formed plate? Analysis and results. Rev Esp Cir Ortop Traumatol. 2017;61(5):339–42.
Schliemann B, Raschke MJ, Groene P, Weimann A, Wähnert D, Lenschow S, Kösters C. Comparison of tension band wiring and precontoured locking compression plate fixation in Mayo type IIA olecranon fractures. Acta Orthop Belg. 2014;80(1):106–11.
Ren YM, Qiao HY, Wei ZJ, Lin W, Fan BY, Liu J, et al. Efficacy and safety of tension band wiring versus plate fixation in olecranon fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2016;11(1):137.
Francis T, Washington T, Srivastava K, Moutzouros V, Makhni EC, Hakeos W. Societal costs in displaced transverse olecranon fractures: using decision analysis tools to find the most cost-effective strategy between tension band wiring and locked plating. J Shoulder Elb Surg. 2017;26(11):1995–2003.
Claessen FMAP, van den Bekerom MPJ, van Dijk CN, Goslings JC, Kerkhoffs GMMJ, Doornberg JN. Shoulder elbow platform. Tension band wiring for simple olecranon fractures: evaluation of surgical technique. J Orthop Traumatol. 2017;18(3):275–81. Erratum: J Orthop Traumatol. 2018;19(1):16.
Schneider MM, Nowak TE, Bastian L, Katthagen JC, Isenberg J, Rommens PM, et al. Tension band wiring in olecranon fractures: the myth of technical simplicity and osteosynthetical perfection. Int Orthop. 2014;38(4):847–55.
Gruszka D, Arand C, Nowak T, Dietz SO, Wagner D, Rommens P. Olecranon tension plating or olecranon tension band wiring? A comparative biomechanical study. Int Orthop. 2015;39(5):955–60.
von Rüden C, Woltmann A, Hierholzer C, Trentz O, Bühren V. The pivotal role of the intermediate fragment in initial operative treatment of olecranon fractures. J Orthop Surg Res. 2011;6:9.
Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. J Am Acad Orthop Surg. 2013;21(3):149–60. Review.
Niéto H, Billaud A, Rochet S, Lavoinne N, Loubignac F, Pietu G, et al. Proximal ulnar fractures in adults: a review of 163 cases. Injury. 2015;46(Suppl 1):S18–23.
Suresh SS. Management of comminuted olecranon fractures with precut K-wires and tension band wiring. Tech Hand Up Extrem Surg. 2009;13(2):82–4. Review.
Saeed ZM, Trickett RW, Yewlett AD, Matthews TJ. Factors influencing K-wire migration in tension-band wiring of olecranon fractures. J Shoulder Elb Surg. 2014;23(8):1181–6.
Özsoy MH, Kızılay O, Günenç C, Özsoy A, Demiryürek D, Hayran M, et al. Modified tension band wiring technique for olecranon fractures: where and how should the K-wires be inserted to avoid articular penetration? Acta Orthop Traumatol Turc. 2015;49(2):190–6.
Catalano LW 3rd, Crivello K, Lafer MP, Chia B, Barron OA, Glickel SZ. Potential dangers of tension band wiring of olecranon fractures: an anatomic study. J Hand Surg Am. 2011;36(10):1659–62.
Willinger L, Lucke M, Crönlein M, Sandmann GH, Biberthaler P, Siebenlist S. Malpositioned olecranon fracture tension-band wiring results in proximal radioulnar synostosis. Eur J Med Res. 2015;20:87.
De Carli P, Gallucci GL, Donndorff AG, Boretto JG, Alfie VA. Proximal radio-ulnar synostosis and nonunion after olecranon fracture tension-band wiring: a case report. J Shoulder Elb Surg. 2009;18(3):e40–4.
Lee HJ, Jung JW, Cho DW, Jeon IH. Morphometric analysis of the proximal ulna using three-dimensional computed tomography and computer-aided design: varus, dorsal, and torsion angulation. Surg Radiol Anat. 2014;36(8):763–8.
Rompen JC, Vos GA, Verheyen CC. Acute ischemia of the hand seven months after tension-band wiring of the olecranon. J Shoulder Elb Surg. 2010;19(3):e9–11.
Huang TW, Wu CC, Fan KF, Tseng IC, Lee PC, Chou YC. Tension band wiring for olecranon fractures: relative stability of Kirschner wires in various configurations. J Trauma. 2010;68(1):173–6.
Mauffrey CP, Krikler S. Surgical techniques: how I do it? Open reduction and tension band wiring of olecranon fractures. Injury. 2009;40(4):461–5.
Powell AJ, Farhan-Alanie OM, Bryceland JK, Nunn T. The treatment of olecranon fractures in adults. Musculoskelet Surg. 2017;101(1):1–9.
Lalliss SJ, Branstetter JG. The use of three types of suture and stainless steel wire tension banding for the fixation of simulated olecranon fractures: a comparison study in cadaver elbows. J Bone Joint Surg Br. 2010;92(2):315–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rouleau, D.M. (2020). Olecranon Fractures. In: Crist, B., Borrelli Jr., J., Harvey, E. (eds) Essential Biomechanics for Orthopedic Trauma. Springer, Cham. https://doi.org/10.1007/978-3-030-36990-3_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-36990-3_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-36989-7
Online ISBN: 978-3-030-36990-3
eBook Packages: MedicineMedicine (R0)