Abstract
Small colony variants (SCVs) of Staphylococcus aureus (S. aureus), one of the most commonly observed pathogens, have been observed in clinical patients for more than half a century in a variety of infectious diseases (e.g., osteomyelitis, cystic fibrosis, endocarditis, skin infections, and abscess). The presence of S. aureus SCVs in patients has been rising and recent clinical studies have raised concerns about their potential roles in chronic and persistent infections. In this chapter, the emergency and clinical prevalence of S. aureus SCVs are examined; their characteristics and types of samples and techniques studied are discussed; and perspectives and recommendations for their diagnosis, pathogenesis, and treatment are proposed. Clinical cases involving S. aureus infections lasting for weeks or longer, or when pinpoint colonies are noted on routine cultures, should be screened for S. aureus SCVs and, if present, antibiotics that are effective in eliminating S. aureus SCVs must be considered.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Small colony variant
- Staphylococcus aureus
- Chronic infection
- Persistent infection
- Intracellular disease
Introduction
Staphylococcus aureus (S. aureus) is found to be most prevalent in inpatient specimens and second most prevalent in outpatient specimens [1]. Small colony variants (SCVs) of S. aureus have been reported in persistent and chronic infections as well as in secondary infections in genetic and acquired diseases. They have been observed in infections of implants (prosthetic joint, pacemaker), skin (cutaneous abscesses), tissue (muscular abscesses), bone (osteomyelitis), blood (bacterial sepsis), sinuses (sinusitis), and airways (cystic fibrosis or CF) [2,3,4,5,6,7,8,9,10,11,12,13,14].
The clinical presence of S. aureus SCVs has been documented since the 1950s when a dwarf colony was isolated from a skin abscess [15]. This subpopulation of S. aureus produced colonies that were noted to be nonpigmented and nonhemolytic [16]. In 1978, using eight clinical samples, S. aureus SCVs were acquired from blood, osteomyelitis, subcutaneous abscess, and cerebrospinal fluid [17]. These clinical isolates displayed delayed growth and reverted to the parent strain (normal-type or wild-type) when supplemented with certain nutritional needs [16]. Quite a few recent clinical reports have raised concerns about the roles of S. aureus SCVs in the occurrence and persistence of infections. In 2013, Yagci et al. examined 123 CF patients (out of a total of 248 patients) with persistent airway infections and, of these patients, 16% presented with S. aureus SCVs [18]. In 2014, Tande et al. retrospectively examined 35 patients (among a total of 134 infected patients) with periprosthetic joint infections caused by S. aureus; 28.6% of these patients were found to possess S. aureus SCVs [19].
Infections associated with S. aureus SCVs seem to be chronic and usually persist even after long antimicrobial therapies. SCVs, compared to their normal-type, are more resistant to traditional antibiotics and, because of their location within the cells and their reduced uptake of antimicrobial agents, they persist [20, 21]. Certain subtypes are also associated with different treatment types, such as menadione; hemin-dependent subtypes are probably associated with the use of aminoglycoside antibiotics (e.g., kanamycin, tobramycin, gentamicin, streptomycin, and others) [22].
To deal with established infections, delivering an effective and early antimicrobial treatment works the best. In the early stages of infection, localized antimicrobial applications are preferred because they act in the location they are needed, and do not cause as many side effects as the systemic circulation is bypassed. However, the use of antibiotics likely has contributed to the appearance of S. aureus SCVs [4, 23, 24]. Strategies for reducing or eliminating S. aureus SCVs in infections have yet to be developed, but the clinical implications of SCVs are apparent. Understanding the roles and mechanisms of S. aureus SCVs in infection seems to be important to chronic and recurrent infections, and putting an effective therapeutic strategy in place to decrease the chance of chronic and recurrent infections will save patients’ frustration, time, and money.
What Are S. aureus SCVs and Their Characteristics?
S. aureus may be phagocytized by professional phagocytes (e.g., macrophages) and a fraction of the phagocytized bacteria may survive and reside intracellularly. Alarmingly, bacteria like S. aureus have also been found to enter human cells (nonprofessional phagocytes) that do not typically phagocytize foreign materials [25]. Adherence of S. aureus onto such host cell surfaces is a prerequisite for such invasions. S. aureus is known to express an array of adhesins on their surfaces including the microbial surface components recognizing adhesive matrix molecules (MSCRAMMs). S. aureus utilizes these MSCRAMMs to adhere directly and efficiently to host cells or via bridging ligands with host proteins (e.g., fibronectin-binding proteins). Next, the attachment of S. aureus to the host cell surfaces can induce changes in the host cells’ cytoskeleton which leads to the phagocytosis of S. aureus into the host cells [26]. Upon phagocytosis, in general, it requires several characteristics of S. aureus in order for them to survive intracellularly; these characteristics include resistance to the intracellular host defense mechanisms and no killing of the host cells (either by lysis or by inducing apoptosis). Once it has invaded host cells, S. aureus may be destroyed by the intracellular defense mechanisms, maintained as the normal-type in a relatively short time, or, for certain strains of S. aureus, switched to SCVs. For instance, upon infection with S. aureus, epithelial cells were found to contain mainly normal-type S. aureus in the beginning; however, the number of normal-type S. aureus decreased and the number of S. aureus SCVs increased with increasing postinfection time. S. aureus SCVs reached approximately 90% after 28 days [27].
S. aureus SCVs are phenotypically quite different from the normal-type strain and, clinically, their variations are mostly limited to types deficient in electron transport substrates (menadione and hemin) and those deficient in thiamine biosynthesis. As shown in Fig. 1, S. aureus SCVs were observed in at least one of the airway cultures from 24 pediatric patients with CF; 6 of these patients had menadione- and/or hemin-deficient SCVs [24]. The deficiencies of menadione, hemin, and thiamine caused the colonies to grow much more slowly when compared to the normal-type and kept them from being targeted by the host’s intracellular defense mechanisms.
Schematic of culture positivity for S. aureus SCVs among the 24 subjects from whom S. aureus SCV was isolated on one or more occasions. Each horizontal line of circles represents a series of culture results from one SCV-positive subject (each indicated by subject number on the y-axis) by age quarter during the study, with each culture plotted by subject age at the midpoint of each age quarter. Closed circles indicate cultures positive for S. aureus SCVs; open circles are negative. Asterisks indicate subjects who were culture positive for either menadione- or hemin-deficient S. aureus SCVs. (Reprinted with permission from Clinical Infectious Diseases 57:384–391 (2013) [24])
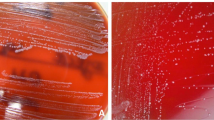
S. aureus SCVs are much smaller (10× difference in size), nonpigmented, and nonhemolytic colonies compared to the parent strain (normal-type or wild-type) (Fig. 2); their small size makes them frequently missed in hospital laboratories. Table 1 lists the characteristics of S. aureus SCVs. Their prominent features include decreased pigmentation and hemolysis, increased resistance to aminoglycosides, and an unstable colony phenotype. Unlike their normal-type, S. aureus SCVs are mostly non-virulent which allows them to be overlooked by host cell defenses. In the normal-type, S. aureus produces alpha-toxin which causes an intracellular signaling cascade that results in the lysis of host cells [28]. In S. aureus SCVs, the synthesis of alpha-toxin is downregulated and the host cells stay intact which provides these facultative bacteria a reservoir in which to persist [26]. Some SCV phenotypes could even survive the bacteriostatic environment of the lysosome; for instance, a menadione auxotroph SCV strain, obtained from an osteomyelitis patient, survived within the lysosome of endothelial cells for 48 h [29]. However, upon supplementing the deficient substrates (e.g., menadione, hemin, and thiamine), S. aureus SCVs may rapidly reverse to the normal-type and lyse the host cells [22]. It is believed that the ability of S. aureus SCVs to persist intracellularly is due in part to the ability of S. aureus to phenotypically switch from the parent strain to the SCVs.
Pictures of S. aureus of same clonal origin on sheep blood agar plates after 48 h incubation. Scale bar = 1 cm. (a) Normal-sized colonies, of 2–3 mm in size, show a typical golden pigmentation. (b) SCVs. (Reprinted with permission from Trends in Microbiology 17:54–58 (2009) [26])
Screening and Identification of S. aureus SCVs from Clinical Patient Samples
S. aureus SCVs have been isolated from a variety of clinical patient samples such as blood, bone, bronchial secretion, bronchoalveolar lavage, cerebrospinal fluid, joint aspiration, tissue aspirate, nares sample, oropharyngeal swab, pus, skin tissue, and sputum (Table 2). They have been characterized mainly by culturing for relatively long time periods and auxotrophy tests (Table 3). S. aureus SCVs are typically cultured, isolated, and identified as pinpoint, nonpigmented, nonhemolytic colonies after 24–72 h incubation on blood agar or Columbia agar. These characteristics set them apart from normal-type S. aureus which is ten times larger and golden. Normal-type S. aureus also grows much faster than SCVs; therefore, SCVs are overgrown by the normal-type and frequently overlooked. S. aureus SCVs can be further classified by testing them for thymidine, hemin, and menadione auxotrophy using agar disk diffusion tests; testing auxotrophy for hemin uses standard disks and testing auxotrophy for thymidine and menadione uses disks with thymidine and menadione, respectively. In addition, the samples must be confirmed as S. aureus by testing for the species specific genes nuc and coa via polymerase chain reaction (PCR) [18], 16S-rRNA-directed in situ hybridization [30], or genotypic analysis “Spa typing” [31].
Emergence and Prevalence of Clinical Cases of S. aureus SCVs
Due to their slow growth rate, atypical colony morphology, unusual biochemical reactions, and reduced coagulase activity, the isolation and identification of S. aureus SCVs have been challenging (especially in the early years). The roles of S. aureus SCVs in infections have been underestimated and likely have contributed to therapeutic failures in clinical settings. The first clinical observations of S. aureus SCVs were reported in the 1950s where pure growth of “dwarf-colony variants” (now known as SCVs) of S. aureus was obtained in cultures from patients with abscesses, septic lesions, and whitlows [15, 32, 33]. Since the mid-1990s, S. aureus SCVs have been increasingly appreciated clinically after they were isolated from a variety of infected patients. S. aureus SCVs have been reported in clinical cases including CF, abscesses, bacteremia, pneumonia, septic arthritis, implant/device-related infection, and skin, soft tissue, and bone infections (Table 4). These clinical cases have shown the versatility of S. aureus SCVs and their presence in diverse clinical scenarios. S. aureus SCVs have been identified as the sole or predominant isolate in some cases [17] and have been increasingly seen in patients with recurrent, persistent infections, especially those that have been treated with antimicrobial therapy such as aminoglycosides and cell-wall-active antibiotics (Table 4).
Osteomyelitis
Osteomyelitis is an infection of the bone that occurs after trauma, surgery, presence of a foreign body such as a prosthesis or after hematogenous seeding. One of the major infecting organisms is S. aureus making S. aureus SCVs a suspect in patients that have persistent or recurrent infections. von Eiff et al. examined bone specimens and deep tissue aspirates from 14 patients with osteomyelitis [4]. Four (29%) out of the 14 patients had S. aureus SCVs. After antimicrobial (gentamicin) treatment for more than 4 weeks, strikingly, infection recurred in the four patients who had S. aureus SCVs whereas those without SCVs did not have recurrence [4]. Along with recurrent infection, patients were more likely to have S. aureus SCVs when they were treated with gentamicin beads; these beads release gentamicin over a period of weeks to months to provide a sustained local level of antibiotics and are commonly used to treat osteomyelitis. All four patients treated with gentamicin beads had S. aureus SCVs while the other patients who were not treated with gentamicin beads did not have S. aureus SCVs [4]. S. aureus SCVs were also recovered in two cases of chronic osteomyelitis where the patients were previously treated with gentamicin beads [34, 35]. These data may suggest that gentamicin beads might have selected for S. aureus SCVs (Table 5), which should alert physicians that gentamicin may select for S. aureus SCVs that could contribute to recurrent and persistent infections.
In 2006, Sendi et al. identified S. aureus SCVs in five periprosthetic joint infection patients [2]. These five patients had a mean age of 62, all experienced treatment failure prior to isolation of S. aureus SCVs despite as many as three surgical revisions and up to 22 months of antibiotics (e.g., intravenous flucloxacillin followed by a combination of rifampin and levofloxacin after a few days for methicillin-susceptible Staphylococcal infections). Even with antimicrobial therapies during early treatment consisting of various combinations of flucloxacillin, vacomycin plus cefepime, ciprofloxacin, and rifampin, all patients had recurrent infections. The spacers were removed after detection of S. aureus SCVs and antimicrobial treatment was chosen based on susceptibility testing. A combination of levofloxacin and rifampin was administered for a course ranging between 5.5 and 7 weeks. Four patients proceeded to receive reimplantations, while one refused in fear of reinfection. Follow-up for these patients ranged between 12 and 48 months; three patients were cured while two were likely cured. Therefore, it seems that, in cases that involve persistent or recurrent infections, S. aureus SCVs should be examined and antibiotics that can eliminate SCVs may need to be considered in order to advance toward proper treatments and possibly avoid surgical revisions. Due to the stubborn nature of SCVs, removal of all implants and extensive debridement are recommended.
Implant/Device-Related Infection
S. aureus is one of the most common causes of infections associated with biomedical implants or devices. S. aureus SCVs have been isolated in cases of pacemaker and ventriculoperitoneal-shunt infections in 2003 and 2005, respectively [2, 36]. In these S. aureus SCV cases, the patients had poor clinical and microbiologic responses to prolonged antimicrobial therapies. Patients were treated unsuccessfully with antibiotics (e.g., cefuroxime) which led to multiple instances of recurrent fever, infection, hospitalization, and surgeries. These cases further emphasize the versatility and infectious nature of S. aureus SCVs. With the increasing use of invasive implants/devices, S. aureus SCVs are expected to become more common; implant/device-related infections that are persistent and resistant should be tested for S. aureus SCVs. Similar to the periprosthetic joint infection cases discussed above, the best way to treat S. aureus SCVs was to completely remove the foreign implant or device and administer appropriate antimicrobial treatment that is effective against S. aureus SCVs.
Cystic Fibrosis (CF)
CF is a progressive, genetic disease that causes persistent lung infections and may also affect the pancreas, liver, kidneys, and intestines. S. aureus SCVs have been frequently isolated in studies involving patients affected by CF [13]. S. aureus is one of the most common bacteria found in the respiratory tracts of children with CF [37] and continues to be one of the major pathogens along with Pseudomonas aeruginosa and Haemophilus influenza [38]. In order to combat these pathogens, long-term prophylactic oral antimicrobial agents such as tetracycline, chloramphenicol, trimethoprim-sulfamethoxazole (SXT), and certain cephalosporins and penicillins [39, 40] are administered. Although normal-type S. aureus can be eliminated from the airways, unfortunately, S. aureus SCVs can form and adapt to the hostile environment leading to chronic and recurrent infections. When looking at 9 studies involving a total of 1266 patients, S. aureus SCVs were identified in 9%, 16%, 17%, 20%, 21%, 24%, 32%, 46%, and 49%, respectively, among patients harboring S. aureus (Table 4) [6, 7, 18, 23, 24, 31, 41,42,43]. Alarmingly, carriers of S. aureus SCVs had been infected with S. aureus longer than those with the normal phenotype [42], showed significantly higher antimicrobial resistance rates than those with the normal phenotype [6], and the presence of SCVs was directly related to poor clinical outcomes [31]. Moreover, patients positive for SCVs were significantly older [6, 18, 42], more commonly co-colonized with Pseudomonas aeruginosa [6], and showed signs of more advanced disease, such as lower forced expiratory volume than patients who had only normal-type S. aureus [6, 42]. Lower weight, advanced age, and prior use of SXT were found to be independent risk factors for S. aureus SCV positivity [6].
Wolter et al. illustrated a unique pattern of culture positivity for S. aureus SCVs in 24 pediatric patients with CF [24]. The patients tended to have “alternating positive and negative culture positivity suggesting repeated selection and enrichment for S. aureus SCVs, incomplete detection, or both” (Fig. 1). Infection with S. aureus SCVs led to a greater drop in lung function and was independently associated with worse CF respiratory outcomes (Table 6). Patients treated with SXT for longer than 18 months or those receiving interventional aminoglycoside treatment were more likely to have SCVs [23, 24]. In fact, it was indicated that SXT was the strongest predictor of S. aureus SCV detection suggesting that SXT strongly selected for S. aureus SCVs. S. aureus SCVs should be a concern for all CF patients especially in those with reduced lung function and those treated with antibiotics for a long period of time. Screening and identification of these SCVs can help guide proper therapeutic treatments.
Abscess
S. aureus SCVs have been isolated from abscesses. One of the first clinical cases of S. aureus SCVs from an abscess patient showed pure tiny colonies (i.e., SCVs) in the cultures of pus samples. The smears of these tiny colonies presented typical Staphylococcal morphology and these tiny colonies reverted to typical large Staphylococcal colonies when cultured in the presence of carbon dioxide [15]. S. aureus SCVs were also identified from a patient with a persistent wound infection (abscess and fistula). A combination treatment of flucloxacillin and rifampicin for 4 weeks led to healing of the chronic wound infection [44].
In another report, methicillin-resistant S. aureus SCVs were identified in a patient with a brain abscess [30]. In this study, computed tomography (Fig. 3) showed a left temporal mass where, 10 years earlier, a neurosurgical intervention had been performed to treat a subarachnoid hemorrhage. The patient was treated with cefamandole for 2 weeks due to a febrile episode and S. aureus was confirmed via 16S rRNA-directed in situ hybridization. S. aureus SCVs were subsequently identified after culturing tissue and pus samples from the abscess for a long time period (i.e., 72 h). This patient was treated with vancomycin, rifampin, and teicoplanin and no infection was observed at the 9-month follow-up. The medical history indicated that this patient had no signs of acute or recurrent infection between the two surgeries. The authors claimed that S. aureus SCVs were the causative microorganisms for the infection; to our understanding, this diagnosis was not conclusive, although it is possible that the surgery performed 10 years prior might be linked to the formation and later proliferation of S. aureus SCVs.
Brain abscess caused by S. aureus SCVs. Left: cerebral computed tomography with contrast medium; (top) intracerebral abscess and (bottom) left temporal intramuscular abscess. Right: Detection of S. aureus cells by in situ hybridization of a tissue section obtained from brain abscess; (top) phase contrast microscopy, (middle) in situ hybridization using a Cy3-labeled S. aureus specific SA-P1 probe, and (bottom) control hybridization with a FLUOS-labeled S. epidermidis probe SEP1. (Reprinted with permission from Journal of Neurology, Neurosurgery, and Psychiatry 74:1000–1002 (2003) [30])
In 1999, the first case of a fatal infection with S. aureus SCVs was reported in an acquired immune deficiency syndrome (AIDS) patient (36-year-old man) who was under long-term treatment with trimethoprim/sulfamethoxazole for prophylaxis of Pneumocystis carinii pneumonia [9]. S. aureus methicillin-resistant SCVs were recovered from a hip abscess in the patient. Vancomycin treatment was administered but the patient’s status deteriorated rapidly; the patient died of refractory septic shock 6 days after admission with fever and progressive pain (of 6 weeks duration) in the right hip [9].
Skin Infection
The first recorded case of a persistent and antimicrobial resistant skin infection due to S. aureus SCVs was reported in 2001 in a 39-year-old patient with Darier’s disease [8]. The patient was hospitalized several times in previous years due to recurrent herpes virus infections and recurrent purulent infections. In 1999, the patient was hospitalized again. Methicillin-resistant S. aureus was isolated from skin and anterior nares leading to a 4-week intravenous course of antimicrobial therapy consisting of vancomycin, rifampicin, and clindamycin. A topical mupirocin ointment was also given for 2 weeks for the nasal mucosa. The skin condition did not significantly improve and topical treatments with steroids and antiseptics (povidone-iodine, chlorhexidine, and chlorquinaldol) were administered. Over a course of 28 months, 119 isolates were derived from 53 clinical specimens obtained from different areas of the affected skin and anterior nares. Hemin-auxotrophic SCVs along with various S. aureus strains were found in the skin infections. With this being said, S. aureus SCVs may be related to skin infections that persist for a long period of time and may be resistant to various therapeutic treatments.
Clinical Significance of S. aureus SCVs
From the clinical cases reported (Table 4), we can see that S. aureus SCVs have significant clinical implications because:
-
S. aureus SCVs are found in a broad range of percentages among S. aureus positive patients such as 6% [45], 9% [31], 15% [46], 16% [18], 17% [6], 20% [42], 21% [41], 24% [24], 29% [4], 32% [43], 46% [23], 49% [7], and 100% [15, 32, 33]. S. aureus SCVs are responsible for [15, 32, 33], most likely responsible for [4, 17], or may contribute to [5,6,7,8,9, 11, 12, 18, 23, 24, 30, 31, 34,35,36, 41,42,43,44,45,46,47,48] the infections observed clinically.
-
A variety of factors including lower weight, advanced age, and prior use of antibiotics may contribute to the development of S. aureus SCVs [6]. For instance, the history of antimicrobial treatments seems to contribute to increased occurrences of S. aureus SCVs, since S. aureus SCVs were more often obtained from patients who were treated with antibiotics (e.g., gentamicin) [4, 6, 9, 12, 33,34,35, 42, 45].
-
S. aureus SCVs have the ability to persist longer within host cells compared to their wild-type strains (Fig. 4) [8], which may explain why S. aureus seems to be eliminated but infection may recur weeks or months later [33]. Because they reside intracellularly and have relatively low virulence, S. aureus SCVs can remain inside other cells and be protected from conventional antibiotic treatments as well as from the intracellular host defense mechanisms.
-
S. aureus SCVs are often more resistant to antibiotics compared to their normal-type strain (Fig. 5) [6] and are difficult to eliminate. However, they can be treated but the optimal treatments still need to be identified and consequences of failure could be unexpected. In 2003, a patient with a brain abscess had S. aureus SCVs and was effectively treated with a combination of vancomycin and rifampin followed by prolonged treatment with teicoplanin; no signs of infection were observed at the subsequent 9-month follow-up [30]. However, various antibiotics have failed to treat S. aureus SCVs and led to recurrent infections [4] and might even have contributed to death [9].
-
The presence of S. aureus SCVs most likely contributed to a poorer clinical outcome, since patients who had S. aureus SCVs were significantly more commonly co-colonized with other bacteria (e.g., Pseudomonas aeruginosa), infected with S. aureus longer, had chronic or persistent infections or infection recurrence, and presented signs of more advanced disease (e.g., lower forced expiratory volume) compared to patients who had only wild-type S. aureus [6, 18, 31, 42]. For instance, it was reported that four patients among 14 infected patients who had S. aureus SCVs all had infection recurrence while the remaining 10 patients with normal-type S. aureus showed no recurrence [4]. S. aureus SCVs were also more often observed among patients with chronic, persistent, or recurrent infections [5, 34, 36, 44, 48].
Electron micrographs of keratinocyte HaCaT cells that were infected with isolates of clinical isogenic normal-type S. aureus and S. aureus SCVs. After incubation of infected HaCaT cells in the presence of lysostaphin for 30 min or 48 h (analogous to an intracellular persistence assay), cells were washed, dehydrated, and embedded in Epon. Ultrathin sections were counterstained and examined by electron microscopy. (a, b), Intracellular persistence of SCVs (SCV1) within viable HaCaT cells after (a) 30 min or (b) 48 h of incubation. Epithelial cells appear viable and show no signs of degeneration (original magnification, ×3400). (c, d) S. aureus of the normal phenotype (NP1) is incorporated (c) after 30 min by intact HaCaT cells; however, (d) after 48 h of incubation, most epithelial cells show severe lytic degeneration and release of bacteria (original magnification, ×3400). (Reprinted with permission from Clinical Infectious Diseases 32:1643–1647 (2001) [8])
Percent antimicrobial resistance of S. aureus isolates. Isolates with the SCV (n = 24) and normal colony variant or NCV (n = 110) phenotypes are compared. (Reprinted with permission from Journal of Clinical Microbiology 45:168–72 (2007) [6])
Summary and Perspectives
S. aureus SCVs have been observed in patients for more than half a century in a variety of infectious diseases including CF, sepsis, bacteremia, endocarditis, skin infections, rhinosinusitis, osteomyelitis, brain abscess, implant/device-related infections, etc. So far, clinical cases of S. aureus SCVs in CF patients have been documented relatively better compared to the other diseases, but this does not necessarily mean that S. aureus SCVs are less commonly found in the other infections. More clinical cases involving S. aureus infections should be examined for presence or absence of S. aureus SCVs. Similarly, SCVs of other bacteria should be carefully examined and treated; SCVs are not limited to S. aureus and have been reported for non-Staphylococcus bacteria that have been recovered from human specimens (Table 7) [28]. More details on diagnosis, pathogenesis, and treatment of S. aureus SCVs are discussed below.
Diagnosis
S. aureus SCVs have been identified from various specimens including bronchial secretion, sputum, bronchoalveolar lavage, oropharyngeal swab, bone, tissue/joint aspirate, skin tissue, anterior nare sample, pus, cerebrospinal fluid, and blood. Currently, most hospital laboratories have the ability to isolate, characterize, and identify normal-type S. aureus, via targeting genes such as nuc, clfA, eap, and coa. In contrast to the normal-type, S. aureus SCVs are much smaller, nonhemolytic, and nonpigmented; these characteristics have made them difficult to recover and classify. Because of their slow growth and atypical morphology, S. aureus SCVs are often missed, misidentified, or misinterpreted by the automated systems routinely used in many clinical laboratories. For instance, S. aureus SCVs were misidentified as coagulase-negative Staphylococcus [9, 44, 48]. Therefore, special efforts should be taken to identify S. aureus SCVs when an infection is particularly resistant to treatment, persists for a long period, or fails to respond to adequate antimicrobial therapy. We recommend that S. aureus SCVs should be suspected whenever pinpoint colonies are noted on routine cultures (even with a small number), and such samples should be run for S. aureus SCVs using appropriate selective media and growth conditions.
Pathogenesis
The development of S. aureus SCVs is likely when the presence of normal-type S. aureus lasts for hours, weeks, or longer; we have confirmed the formation of S. aureus SCVs in osteoblasts and macrophages [49], and that they may contribute to bone infections in vivo [50]. The presence and contribution of S. aureus SCVs in clinical infections most likely have been underestimated and underreported. It is likely that S. aureus SCVs have played an important role in infection persistence; however, complete pathogenesis for S. aureus SCVs has yet to be discovered. The ability of S. aureus SCVs to phenotypically switch back and forth between the normal and variant forms help the organism to evade both host defense and antimicrobial treatments thereby contributing to the persistence of their associated infections. Moreover, the menadione deficient strain of S. aureus SCVs can form more diverse and highly structured biofilms compared to the normal-type [51] and may contribute to their persistence as well.
Treatment
S. aureus SCVs persist intracellularly within their host cells and they are often more resistant to antibiotics than the normal-type S. aureus. Their ability to “hide” intracellularly may protect them from intracellular host defense mechanisms and decrease their exposure to antibiotics. As a result, S. aureus SCVs are difficult to treat. Two approaches may be applied. One is to prevent the development of S. aureus SCVs by striking early in the acute infection stage before SCVs can develop by using effective local and systemic antimicrobial treatments; screening for S. aureus SCVs must be done if such treatments fail since certain antimicrobial treatments may be selective (Table 5) for the development of S. aureus SCVs. The other approach is to identify effective antimicrobial approaches to treat S. aureus SCV-associated infections. Currently, the optimal treatments for infections caused by S. aureus SCVs have not been identified. However, some treatments seem to be promising. A combination of levofloxacin and rifampin cured three patients with S. aureus SCVs [45], a combination of vancomycin and rifampin followed by prolonged treatment with teicoplanin presented no sign of infection at 9-month follow-up in a patient with an S. aureus SCV-associated brain abscess [30]. A combination of flucloxacillin and rifampicin led to healing of a persistent wound infection associated with S. aureus SCVs [44]. In preclinical studies, we have shown that antimicrobial peptides may be effective in eliminating S. aureus that are “hiding” in other cells [52], and tuning immune responses may be promising as well [53,54,55]. Nanomedicine, due to the unique characteristics of nanomaterials, is also emerging as improved or alternative therapies for intracellular pathogens like S. aureus SCVs [56]. Therefore, there are promising treatments and we recommend that antimicrobial agents (e.g., rifampin) which have potent intracellular activity should be used in treating infections caused by S. aureus SCVs.
Overall, S. aureus SCVs should be aggressively and accurately identified whenever infections induced by S. aureus fail apparently “adequate” antimicrobial therapy. The identification will help physicians end ineffective antimicrobial therapeutic treatments, which may inadvertently induce the development of S. aureus SCVs, and promptly initiate proper antimicrobial treatments. Failure to identity and treat S. aureus SCVs may lead to chronic, persistent, and recurrent infections, wound complications, and even death.
References
Styers D, Sheehan DJ, Hogan P, Sahm DF (2006) Laboratory-based surveillance of current antimicrobial resistance patterns and trends among Staphylococcus aureus: 2005 status in the United States. Ann Clin Microbiol Antimicrob 5:2. Epub 2006/02/14. PubMed PMID: 16469106; PMCID: Pmc1397857. https://doi.org/10.1186/1476-0711-5-2
Sendi P, Rohrbach M, Graber P, Frei R, Ochsner PE, Zimmerli W (2006) Staphylococcus aureus small colony variants in prosthetic joint infection. Clin Infect Dis 43(8):961–967. PubMed PMID: 16983605. https://doi.org/10.1086/507633
von Eiff C, Vaudaux P, Kahl BC, Lew D, Emler S, Schmidt A, Peters G, Proctor RA (1999) Bloodstream infections caused by small-colony variants of coagulase-negative staphylococci following pacemaker implantation. Clin Infect Dis 29(4):932–934. PubMed PMID: 10589914. https://doi.org/10.1086/520462
von Eiff C, Bettin D, Proctor RA, Rolauffs B, Lindner N, Winkelmann W, Peters G (1997) Recovery of small colony variants of Streptococcus aureus following gentamicin bead placement for osteomyelitis. Clin Infect Dis 25(5):1250–1251
Proctor RA, van Langevelde P, Kristjansson M, Maslow JN, Arbeit RD (1995) Persistent and relapsing infections associated with small-colony variants of Staphylococcus aureus. Clin Infect Dis 20(1):95–102. PubMed PMID: 7727677
Besier S, Smaczny C, von Mallinckrodt C, Krahl A, Ackermann H, Brade V, Wichelhaus TA (2007) Prevalence and clinical significance of Staphylococcus aureus small-colony variants in cystic fibrosis lung disease. J Clin Microbiol 45(1):168–172. PubMed PMID: 17108072; PMCID: PMC1828983. https://doi.org/10.1128/JCM.01510-06
Kahl B, Herrmann M, Everding AS, Koch HG, Becker K, Harms E, Proctor RA, Peters G (1998) Persistent infection with small colony variant strains of Staphylococcus aureus in patients with cystic fibrosis. J Infect Dis 177(4):1023–1029. PubMed PMID: 9534977
von Eiff C, Becker K, Metze D, Lubritz G, Hockmann J, Schwarz T, Peters G (2001) Intracellular persistence of Staphylococcus aureus small-colony variants within keratinocytes: a cause for antibiotic treatment failure in a patient with Darier’s disease. Clin Infect Dis 32(11):1643–1647. PubMed PMID: WOS:000168588500020. https://doi.org/10.1086/320519
Seifert H, von Eiff C, Fatkenheuer G (1999) Fatal case due to methicillin-resistant Staphylococcus aureus small colony variants in an AIDS patient. Emerg Infect Dis 5(3):450–453. PubMed PMID: WOS:000080827600019
Wise RI (1956) Small colonies (G variants) of staphylococci: isolation from cultures and infections. Ann N Y Acad Sci 65(3):169–174. PubMed PMID: 13363212
Spagna VA, Fass RJ, Prior RB, Slama TG (1978) Report of a case of bacterial sepsis caused by a naturally occurring variant form of Staphylococcus aureus. J Infect Dis 138(2):277–278. Epub 1978/08/01. PubMed PMID: 681802
Quie PG (1969) Microcolonies (G-variants) of Staphylococcus aureus. Yale J Biol Med 41(5):394–403. PubMed PMID: 5780692; PMCID: PMC2591491
Suwantarat N, Rubin M, Bryan L, Tekle T, Boyle MP, Carroll KC, Jennings MT (2018) Frequency of small-colony variants and antimicrobial susceptibility of methicillin-resistant Staphylococcus aureus in cystic fibrosis patients. Diagn Microbiol Infect Dis 90(4):296–299. Epub 2018/01/19. PubMed PMID: 29343421. https://doi.org/10.1016/j.diagmicrobio.2017.11.012
Chen H, Wang Q, Yin Y, Li S, Niu DK, Wang H (2018) Genotypic variations between wild-type and small colony variant of Staphylococcus aureus in prosthetic valve infectious endocarditis: a comparative genomic and transcriptomic analysis. Int J Antimicrob Agents 51(4):655–658. Epub 2017/12/17. PubMed PMID: 29247687. https://doi.org/10.1016/j.ijantimicag.2017.12.006
Hale JH (1951) Studies on staphylococcus mutation: a naturally occurring “G” gonidial variant and its carbon dioxide requirements. Br J Exp Pathol 32(4):307–313. Epub 1951/08/01. PubMed PMID: 14886490; PMCID: Pmc2073169
Wise RI, Spink WW (1954) The influence of antibiotics on the origin of small colonies (G variants) of Micrococcus pyogenes var. aureus. J Clin Invest 33(12):1611–1622. PubMed PMID: 13211817; PMCID: PMC1072592. https://doi.org/10.1172/JCI103041
Acar JF, Goldstein FW, Lagrange P (1978) Human infections caused by thiamine- or menadione-requiring Staphylococcus aureus. J Clin Microbiol 8(2):142–147. PubMed PMID: 701460; PMCID: PMC275172
Yagci S, Hascelik G, Dogru D, Ozcelik U, Sener B (2013) Prevalence and genetic diversity of Staphylococcus aureus small-colony variants in cystic fibrosis patients. Clin Microbiol Infect 19(1):77–84. PubMed PMID: 22284387. https://doi.org/10.1111/j.1469-0691.2011.03742.x.
Tande AJ, Osmon DR, Greenwood-Quaintance KE, Mabry TM, Hanssen AD, Patel R (2014) Clinical characteristics and outcomes of prosthetic joint infection caused by small colony variant staphylococci. MBio 5(5):e01910–e01914. PubMed PMID: 25271290; PMCID: PMC4196237. https://doi.org/10.1128/mBio.01910-14
McNamara PJ, Proctor RA (2000) Staphylococcus aureus small colony variants, electron transport and persistent infections. Int J Antimicrob Agents 14(2):117–122. PubMed PMID: 10720801
Rollin G, Tan X, Tros F, Dupuis M, Nassif X, Charbit A, Coureuil M (2017) Intracellular survival of Staphylococcus aureus in endothelial cells: a matter of growth or persistence. Front Microbiol 8:1354. Epub 2017/08/05. PubMed PMID: 28769913; PMCID: Pmc5515828. https://doi.org/10.3389/fmicb.2017.01354
Balwit JM, van Langevelde P, Vann JM, Proctor RA (1994) Gentamicin-resistant menadione and hemin auxotrophic Staphylococcus aureus persist within cultured endothelial cells. J Infect Dis 170(4):1033–1037
Kahl BC, Duebbers A, Lubritz G, Haeberle J, Koch HG, Ritzerfeld B, Reilly M, Harms E, Proctor RA, Herrmann M, Peters G (2003) Population dynamics of persistent Staphylococcus aureus isolated from the airways of cystic fibrosis patients during a 6-year prospective study. J Clin Microbiol 41(9):4424–4427. PubMed PMID: WOS:000185246800066. https://doi.org/10.1128/Jcm.41.9.4424-4427.2003
Wolter DJ, Emerson JC, McNamara S, Buccat AM, Qin X, Cochrane E, Houston LS, Rogers GB, Marsh P, Prehar K, Pope CE, Blackledge M, Deziel E, Bruce KD, Ramsey BW, Gibson RL, Burns JL, Hoffman LR (2013) Staphylococcus aureus small-colony variants are independently associated with worse lung disease in children with cystic fibrosis. Clin Infect Dis 57(3):384–391. PubMed PMID: 23625938; PMCID: PMC3888146. https://doi.org/10.1093/cid/cit270
Garzoni C, Kelley WL (2009) Staphylococcus aureus: new evidence for intracellular persistence. Trends Microbiol 17(2):59–65. PubMed PMID: WOS:000264279200003. https://doi.org/10.1016/j.tim.2008.11.005
Sendi P, Proctor RA (2009) Staphylococcus aureus as an intracellular pathogen: the role of small colony variants. Trends Microbiol 17(2):54–58. PubMed PMID: WOS:000264279200002. https://doi.org/10.1016/j.tim.2008.11.004
Tuchscherr L, Medina E, Hussain M, Volker W, Heitmann V, Niemann S, Holzinger D, Roth J, Proctor RA, Becker K, Peters G, Loffler B (2011) Staphylococcus aureus phenotype switching: an effective bacterial strategy to escape host immune response and establish a chronic infection. EMBO Mol Med 3(3):129–141. PubMed PMID: WOS:000288727200003. https://doi.org/10.1002/emmm.201000115
Proctor RA, von Eiff C, Kahl BC, Becker K, McNamara P, Herrmann M, Peters G (2006) Small colony variants: a pathogenic form of bacteria that facilitates persistent and recurrent infections. Nat Rev Microbiol 4(4):295–305. PubMed PMID: WOS:000236040200015. https://doi.org/10.1038/nrmicro1384
Schroder A, Kland R, Peschel A, von Eiff C, Aepfelbacher M (2006) Live cell imaging of phagosome maturation in Staphylococcus aureus infected human endothelial cells: small colony variants are able to survive in lysosomes. Med Microbiol Immunol 195(4):185–194. PubMed PMID: WOS:000241356100002. https://doi.org/10.1007/s00430-006-0015-0
Kipp F, Ziebuhr W, Becker K, Krimmer V, Hobeta N, Peters G, Von Eiff C (2003) Detection of Staphylococcus aureus by 16S rRNA directed in situ hybridisation in a patient with a brain abscess caused by small colony variants. J Neurol Neurosurg Psychiatry 74(7):1000–1002. PubMed PMID: 12810807; PMCID: 1738524
Masoud-Landgraf L, Zarfel G, Kaschnigg T, Friedl S, Feierl G, Wagner-Eibel U, Eber E, Grisold AJ, Kittinger C (2016) Analysis and characterization of Staphylococcus aureus small colony variants isolated from cystic fibrosis patients in Austria. Curr Microbiol 72(5):606–611. PubMed PMID: 26821237; PMCID: PMC4828482. https://doi.org/10.1007/s00284-016-0994-z
Sherris JC (1952) Two small colony variants of Staph. aureus isolated in pure culture from closed infected lesions and their carbon dioxide requirements. J Clin Pathol 5(4):354–355. Epub 1952/11/01. PubMed PMID: 13011225; PMCID: Pmc1023676
Goudie JG, Goudie RB (1955) Recurrent infections by a stable dwarf-colony variant of Staphylococcus aureus. J Clin Pathol 8(4):284–287. Epub 1955/11/01. PubMed PMID: 13271575; PMCID: Pmc1023871
von Eiff C, Lindner N, Proctor RA, Winkelmann W, Peters G (1998) Development of gentamicin-resistant small colony variants of S. aureus after implantation of gentamicin chains in osteomyelitis as a possible cause of recurrence. Zeitschrift fur Orthopadie und ihre Grenzgebiete 136(3):268–271. Epub 1998/09/16. PubMed PMID: 9736990
Rolauffs B, Bernhardt TM, von Eiff C, Hart ML, Bettin D (2002) Osteopetrosis, femoral fracture, and chronic osteomyelitis caused by Staphylococcus aureus small colony variants (SCV) treated by girdlestone resection--6-year follow-up. Arch Orthop Trauma Surg 122(9-10):547–550. PubMed PMID: 12483342. https://doi.org/10.1007/s00402-002-0435-2
Spanu T, Romano L, D’Inzeo T, Masucci L, Albanese A, Papacci F, Marchese E, Sanguinetti M, Fadda G (2005) Recurrent ventriculoperitoneal shunt infection caused by small-colony variants of Staphylococcus aureus. Clin Infect Dis 41(5):e48–e52. PubMed PMID: 16080075. https://doi.org/10.1086/432577
Cystic Fibrosis Foundation (2015) Cystic fibrosis foundation patient registry report. https://www.cff.org/Our-Research/CF-Patient-Registry/2015-Patient-Registry-Annual-Data-Report.pdf. Accessed 27 Apr 2017
Lyczak JB, Cannon CL, Pier GB (2002) Lung infections associated with cystic fibrosis. Clin Microbiol Rev 15(2):194–222. PubMed PMID: 11932230; PMCID: PMC118069
Kelly HW (1984) Antibiotic use in cystic-fibrosis. Drug Intell Clin Pharm 18(10):772–783. PubMed PMID: WOS:A1984TL05900001
Marks MI (1981) The pathogenesis and treatment of pulmonary infections in patients with cystic fibrosis. J Pediatr 98(2):173–179
Gilligan PH, Gage PA, Welch DF, Muszynski MJ, Wait KR (1987) Prevalence of thymidine-dependent Staphylococcus aureus in patients with cystic fibrosis. J Clin Microbiol 25(7):1258–1261. PubMed PMID: 3497170; PMCID: PMC269188
Schneider M, Muhlemann K, Droz S, Couzinet S, Casaulta C, Zimmerli S (2008) Clinical characteristics associated with isolation of small-colony variants of Staphylococcus aureus and Pseudomonas aeruginosa from respiratory secretions of patients with cystic fibrosis. J Clin Microbiol 46(5):1832–1834. PubMed PMID: 18322058; PMCID: PMC2395072. https://doi.org/10.1128/JCM.00361-08
Sadowska B, Bonar A, von Eiff C, Proctor RA, Chmiela M, Rudnicka W, Rozalska B (2002) Characteristics of Staphylococcus aureus, isolated from airways of cystic fibrosis patients, and their small colony variants. FEMS Immunol Med Microbiol 32(3):191–197. PubMed PMID: 11934563
Abele-Horn M, Schupfner B, Emmerling P, Waldner H, Goring H (2000) Persistent wound infection after herniotomy associated with small-colony variants of Staphylococcus aureus. Infection 28(1):53–54. PubMed PMID: WOS:000085370400014. https://doi.org/10.1007/s150100050014
Sendi P, Rohrbach M, Graber P, Frei R, Ochsner PE, Zimmerli W (2006) Staphylococcus aureus small colony variants in prosthetic joint infection. Clin Infect Dis 43(8):961–967. PubMed PMID: WOS:000240666200002. https://doi.org/10.1086/507633
Ansari S, Nepal HP, Gautam R, Shrestha S, Chhetri MR, Chapagain ML (2015) Staphylococcus aureus: methicillin resistance and small colony variants from pyogenic infections of skin, soft tissue and bone. J Nepal Health Res Counc 13(30):126–132. PubMed PMID: 26744197
Spearman P, Lakey D, Jotte S, Chernowitz A, Claycomb S, Stratton C (1996) Sternoclavicular joint septic arthritis with small-colony variant Staphylococcus aureus. Diagn Microbiol Infect Dis 26(1):13–15. PubMed PMID: 8950523
Seifert H, Wisplinghoff H, Schnabel P, von Eiff C (2003) Small colony variants of Staphylococcus aureus and pacemaker-related infection. Emerg Infect Dis 9(10):1316–1318. PubMed PMID: WOS:000185836000021
Hamza T, Li B (2014) Differential responses of osteoblasts and macrophages upon Staphylococcus aureus infection. BMC Microbiol 14:207
Hamza T, Dietz M, Pham D, Clovis N, Danley S, Li B (2013) Intra-cellular Staphylococcus aureus alone causes infection in vivo. Eur Cell Mater 25:341–350. discussion 50. Epub 2013/07/09. PubMed PMID: 23832687; PMCID: PMC3830899
Singh R, Ray P, Das A, Sharma M (2010) Enhanced production of exopolysaccharide matrix and biofilm by a menadione-auxotrophic Staphylococcus aureus small-colony variant. J Med Microbiol 59(Pt 5):521–527. PubMed PMID: 20110391. https://doi.org/10.1099/jmm.0.017046-0.
Noore J, Noore A, Li B (2013) Cationic antimicrobial peptide LL-37 is effective against both extra- and intracellular Staphylococcus aureus. Antimicrob Agents Chemother 57(3):1283–1290. Epub 2013/01/01; PubMed PMID: 23274662; PMCID: PMC3591932. https://doi.org/10.1128/aac.01650-12
Li B, Jiang B, Boyce BM, Lindsey BA (2009) Multilayer polypeptide nanoscale coatings incorporating IL-12 for the prevention of biomedical device-associated infections. Biomaterials 30(13):2552–2558. Epub 2009/02/14; PubMed PMID: 19215980; PMCID: PMC3699876. https://doi.org/10.1016/j.biomaterials.2009.01.042
Boyce BM, Lindsey BA, Clovis NB, Smith ES, Hobbs GR, Hubbard DF, Emery SE, Barnett JB, Li B (2012) Additive effects of exogenous IL-12 supplementation and antibiotic treatment in infection prophylaxis. J Orthop Res 30(2):196–202. Epub 2011/08/05. PubMed PMID: 21815205; PMCID: PMC3699881. https://doi.org/10.1002/jor.21520
Hamza T, Barnett JB, Li B (2010) Interleukin 12 a key immunoregulatory cytokine in infection applications. Int J Mol Sci 11(3):789–806. Epub 2010/05/19; PubMed PMID: 20479986; PMCID: 2869233. https://doi.org/10.3390/ijms11030789
Armstead AL, Li B (2011) Nanomedicine as an emerging approach against intracellular pathogens. Int J Nanomedicine 6:3281–3293. Epub 2012/01/10; PubMed PMID: 22228996; PMCID: PMC3252676. https://doi.org/10.2147/ijn.s27285
Acknowledgments
We acknowledge financial support from the Office of the Assistant Secretary of Defense for Health Affairs, through the Peer Reviewed Medical Research Program, Discovery Award under Award No. W81XWH-17-1-0603. We also acknowledge financial support from AO Foundation, Osteosynthesis and Trauma Care Foundation, and the West Virginia National Aeronautics and Space Administration Experimental Program to Stimulate Competitive Research (WV NASA EPSCoR). Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the funding agencies. We thank Suzanne Danley for proofreading.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Andreini, D.E., Bell, C.D., Xing, M., Li, B. (2020). Insights into the Emergence, Clinical Prevalence, and Significance of Staphylococcus aureus Small Colony Variants. In: Li, B., Moriarty, T., Webster, T., Xing, M. (eds) Racing for the Surface. Springer, Cham. https://doi.org/10.1007/978-3-030-34475-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-34475-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34474-0
Online ISBN: 978-3-030-34475-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)