Abstract
Anorectal manometry (ARM) represents the most commonly performed motility test in pediatric populations. It is a valuable tool to assess anorectal muscle function and coordination, the presence of recto-anal inhibitory reflex, the sphincter tonic contractions and relaxations upon different provocative maneuvers, and the thresholds for rectal and anal sensations. In children, although chronic refractory constipation represents the most important indication for ARM, the latter is also useful for the evaluation of fecal incontinence.
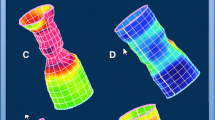
The recent advent of novel technology advances, e.g., high-resolution (HRAM) and 3D high-definition (3DHDAM), has led to increased diagnostic accuracy, making ARM easier to perform and interpret. Nevertheless, the absence of universally agreed normal values in pediatric populations still represents one of the major limitations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Anorectal Physiology
Fecal continence and defecation are highly regulated processes ensured by the synergic and coordinated function of the rectum, pelvic floor muscles, and anal canal. The rectum functions as a reservoir for fecal material and its stretch-sensitive fibers, activated by the intraluminal distension, are essential in signaling the awareness of defecation to the central nervous system and activating spinal reflexes. The anal canal consists of the internal (IAS) and external (EAS) anal sphincters. The former, which is composed of smooth muscle cells, is innervated by the enteric nervous system and therefore not under voluntary control. It is primarily responsible for anal continence as it generates approximately 70–85% of the anal canal pressure. Conversely, the EAS, composed by skeletal muscle cells, is under the voluntary control of the sacral nerves. The two sphincters are closely adjoined and, in young children, a clear physical separation between is difficult to detect [1, 2].
The anal sphincters, the pelvic floor muscles, and the levator ani complex, which includes the puborectalis muscle, are responsible for ensuring the fecal continence at rest. Synergistically, through tonic contractions, the aforementioned structures maintain the anorectum angulated between 85° and 105° [3] and generate a pressure at the level of anal canal that exceeds the rectal pressure, hence preventing the involuntary loss of fecal material [3, 4].
The evacuatory process is a highly regulated and voluntary function. The distension of the rectal wall above an appropriate sensory threshold provokes a temporary reflex relaxation of the IAS, named recto-anal inhibitory reflex (RAIR), which enables the luminal contents to enter the anal canal. The expulsive step, under voluntary control, is characterized by the coordinated relaxation of the EAS and pelvic floor muscles alongside with the abdominal wall contraction, which ultimately enables the passage of the stools through the anal canal [4]. If the subject is not in a socially appropriate setting to defecate, the voluntary contraction of the EAS and the puborectalis muscle prevent the defecation and the stools are returned to the colon by reverse peristalsis.
8.2 Equipment
ARM is by nature a highly technical evaluation and when knowledgeably used, provides an accurate description of anorectal neuromuscular function. However, the manometric data are reliable only if the methodology used to acquire them is accurate.
A manometric apparatus setup consists of a pressure sensor/transducer combination, which detects the pressures in the anal canal and rectum and transduces them into an electrical signal, and a recording device, which amplifies, records, and stores that electrical signal. The pressure sensor/transducer components of the manometric assembly function as a matched pair and are available in two general designs: either water-perfused catheters, connected to a pneumohydraulic perfusion pump and to volume displacement transducers, or strain gauge transducers with solid state circuitry [5].
In the last decade considerable advancements in ARM technology have been witnessed and conventional low-resolution systems have gradually been replaced by high-resolution (HRARM) and 3D high-definition manometry (HDARM). This has been achieved by a combination of new manometric assemblies allowing intraluminal pressure to be recorded from up to 256 pressure sensors spaced <0.3 mm. At the same time, advances in computer processing allow pressure data to be presented in real-time as a compact, either as two-dimensional visually intuitive “spatiotemporal plot” or more sophisticated 3D. In adults, by correlating with anatomic structures defined by MRI or 3D ultrasound, HDARM measurements allow a better definition of the contribution of different components of the anal canal and a better description of the anal canal radial asymmetry [6]. However, the role of our enhanced knowledge of the pathophysiological mechanisms of the different defecation disorders in children is still unclear.
Currently, the catheter used for 3DHRAM has an outer diameter of almost 11 mm [7]. Although the test could in theory be performed at any age, in infants the anal resting pressure could be overestimated and anal canal dynamics upon balloon distension could be misinterpreted [8]. To date, 3DHRAM has been used in children aged above 2 years.
8.3 Methodological Aspects
8.3.1 Preparation of Pediatric Patients and Caregivers
In preparation for the procedure, in children above the age of 1 year, an enema is recommended on the day or the evening prior to the day of tests. Alternatively, in those with significant fecal loading a degree of bowel preparation could be required prior to the procedure. In infants, no bowel preparation is required as they generally have soft stools [9]. Medications that can interfere with the anorectal function should be stopped before the procedure.
Older children are instructed to defecate if required before the test. The child should be placed in the lateral decubitus position, with knees drawn up to the chest, maintaining the hips and knees flexed at 90°. Before the probe insertion, the perianal area should be inspected and a digital rectal examination should be carried out, in order to evaluate the general anatomy, the perianal sensation, skin excoriation, and the presence of rectal impaction. Then, the lubricated manometry probe can be gently inserted into the rectum. Before starting the recording, the operator should wait for few minutes in order to allow the acclimation of anorectal area.
Pediatric gastroenterologists have often to face non-cooperative children and, especially in children under the age of 5, a study under anesthesia may be required. When that happens, only the analysis of anal sphincter resting pressures and RAIR can be performed. Moreover, the results need to be carefully evaluated as different anesthetic agents may interfere with the physiological outcomes [10,11,12,13].
Nevertheless, in some circumstances and indications undoubtedly requiring patients’ cooperation a proper psychological preparation for both children and parents is certainly required. Anorectal manometry has been shown to induce significant preprocedural distress in children and adequate psychological preparation intervention has been shown to reduce anticipatory distress, to improve measurements reliability, and ultimately to better pave future treatments based on the manometric patterns [12, 14,15,16,17].
8.3.2 Study Protocol, Analysis, and Interpretation
Ideally, the full manometric protocol should aim at assessing sphincter pressures at rest and during voluntary contractions, bear-down maneuvers, rectal sensation, and reflexes. Nonetheless, the test should be tailored and the relevant parameters to assess should depend on the clinical indication.
The common parameters assessed during the ARM study are the following:
-
Resting pressure:
The resting pressure should be recorded only after the child is relaxed and comfortable. The basal resting sphincter pressure measurement with new technology of HRAM is simply obtained by inserting the catheter and evaluating in real-time the high-pressure zone over a period of 30 s [10]. Conversely, resting pressure evaluation with low-resolution probes is usually performed through either stationary pull-through or continuous withdrawal [18]. The identification of high-pressure zone allows also the measurement of the anal canal length.
-
RAIR (recto-anal inhibitory reflex) (Fig. 8.1):
The RAIR consists in the relaxation of IAS upon a rectal distention. In pediatrics, there are no universally agreed criteria for its definition. It is currently defined as either a dropping in pressure by >5 mmHg or >15% of the resting pressure [18]. The drop in anal pressure may be difficult to be detected especially in uncooperative children and in patients with baseline low resting pressures (e.g., under anesthesia). The RAIR has a volume-dependent response: the larger the balloon volume, the greater the degree and duration of the relaxation. Its measurement is performed by rapidly inflating the rectal balloon with incremental volumes of 5 mL in infants and newborns (up to 20 mL) and increments of 10 mL in older children [10]. If complete relaxation is not obtained, volumes up to 250–300 mL can be reached in older children to elicit the RAIR. The absence of RAIR is suggestive of colonic aganglionosis or Hirschsprung disease (Fig. 8.2). The most common reason for a false-positive RAIR is represented by the migration of the probe during the procedure, which can be prevented by securing the catheter to the anal verge. Conversely, the most frequent cause for a false-negative RAIR test is rectal dilatation (i.e., megarectum), which does not allow the balloon to stretch the rectal walls (and therefore to generate the trigger pressure for the RAIR) because of the enlarged rectal volume [18].
-
Squeeze pressure (Fig. 8.3):
It is elicited by asking the child to voluntarily contract the anal canal and it is calculated as the greatest pressure increase referred to the baseline resting pressure. In some centers, the average of three measurements is calculated [10, 18]. An increased or decreased value may be due to myogenic or neurogenic causes.
-
Endurance squeeze (Fig. 8.4):
The child is asked to contract the anal canal as strongly as possible for at least 15- to 20-s period.
-
Rectal sensation:
The rectal sensation can be assessed in a cooperative child (usually aged 4–5 years and over) by steadily increasing the balloon size through the inflation of progressively greater volumes of water or air. It can be performed with or without deflation intervals in between the subsequent incremental volumes (intermittent rectal distension method or through ramp inflation method, respectively) [10]. It provides further information on the child’s stool perception, which can be indicative of either anorectal dysfunction or dilated rectum. Three different sensation volumes are usually recorded: (i) the first sensation, which represents the lowest balloon volume at which the patient feels the balloon; (ii) the urge sensation, defined as the lowest volume required to elicit the defecation urge; (iii) the maximum tolerable sensation, reached when severe urgency and pain is experienced. This may be hard to be evaluated in children younger than 7 years of age and children with developmental impairment. Sensations are usually decreased in children with dilated rectum, often due to long-lasting outlet-obstruction constipation.
-
The bear-down maneuver or push (simulated defecation) (Fig. 8.5):
It is carried out to evaluate anorectal and pelvic floor pressure changes during a simulated defecation. Usually, this provocative test is possible to perform in children above 5–6 years of age and it requires significant cooperation. Normally, the defecation attempt should induce a simultaneous and coordinate increase in the rectal pressure and relaxation of anal sphincters. This maneuver allows clinicians to diagnose dyssynergic defecation, which is a common cause of fecal outlet obstruction.
-
Balloon expulsion test:
It is carried out asking the child to sit on a commode or in lateral position and expel the intrarectal inflated balloon, trying to guarantee as much privacy as possible. The test is defined normal if the balloon is expelled. In pediatrics, there is no a consensus on the time cut-off needed to expel the balloon and the ideal balloon volume. Studies have demonstrated that adult normal values can be used. Patients with dyssynergia usually fail to expel the balloon [19]. It has been demonstrated that this test in pediatric patients with outlet-obstruction type of constipation may help in tailoring therapeutic management [19].
Absent RAIR. White and black arrows point rectal balloon insufflation and deflation, respectively. The balloon inflation induces an increase in the rectal pressure, shown in the figure as purple bar. The anal sphincter pressure does not decrease upon rectal balloon insufflation. RAIR is absent in several conditions including colonic aganglionosis or Hirschsprung disease
Endurance squeeze. It is the length of time the child is able to maintain the anal canal pressure during a voluntary contraction. It is elicited by asking the child to voluntarily contract the anal sphincter as strongly as possible for a period of at least 15–20 s. The white arrows point the start and the end of the squeeze
Bear-down maneuver or push in dyssynergic defecation. It is carried out to evaluate anorectal and pelvic floor pressure changes during a simulated defecation. Normal defecation attempt induces a simultaneous and coordinate increase in the rectal pressure and relaxation of anal sphincters. In the figure, there is an increase in rectal pressure (white square) but paradoxical increase in anal pressure, consistent with the diagnose dyssynergic defecation, which is a common cause of fecal outlet obstruction in children
8.3.3 Reference Values
In pediatric age, there is a lack of uniformity in terms of protocols and equipment, and hence lack of normal reference values. Moreover, normal HRAM and 3D HRAM values have been published only for adult populations [20,21,22,23], while only few studies have been performed in children with similar methodologies. Hence, the interpretation still relies on expertise of the pediatric gastroenterologists in the field. Moreover, conventional water-perfused ARM measures are routinely used in manometry reporting despite in adult literature has shown that the values with high-resolution manometry are higher than those with water perfusion [24]. Moreover, significant variability in values might depend on gender, BMI, age, use of different protocols, and the interaction between the patient and the clinician [21, 22, 25, 26].
To date only two studies in pediatric age have been performed using HARM and 3DHARM in order to establish normative values. One study using HARM reported normal values of anorectal sphincter metrics (including resting pressure, anal canal length, and RAIR) in 180 healthy and asymptomatic newborns based on age, and segregated by preterm vs term [27]. Recently, Banasiuk et al. have published a study aimed at evaluating normal 3DHRAM values in 61 children without symptoms from the lower gastrointestinal tract [8]. Normal values in pediatric age using either low- or high-resolution manometry are summarized in Tables 8.1 and 8.2.
Further studies are needed in pediatric populations in order to reach universally agreed normal values.
8.4 Indications
The indications of ARM are the following:
-
To rule out Hirschsprung disease (HD)
HD is characterized by the absence of ganglion cells in the myenteric and submucosal nerve plexuses in the colon and rectum secondary to an aberrant ontogenetic development of the gastrointestinal tract. Hence, due to the lack of innervation in the rectum, ARM shows a typical absence of IAS relaxation upon rectal distention. The absence of RAIR on ARM should prompt rectal suction biopsy (RSB), which is the gold standard for the diagnosis of HD. The absence of RAIR and the presence of ganglion cells at rectal suction biopsies define the condition named anal achalasia, which responds well to the treatment with botulin toxin [18].
Recently, a new measure, the anal sphincter relaxation integral (ASRI), has been developed to objectively quantify the RAIR and discriminate patients with and without HD [32]. However, its role in the clinical management of patients with HD is still to be elucidated.
-
To evaluate the anorectal functions of HD children after surgical repair
ARM plays an essential role in the post-surgical evaluation of these patients. For instance, it has been shown that the measurement of the length of the anal canal in HD children with fecal incontinence after surgical repair enables to pave further effective therapeutic management [33].
-
To evaluate the sphincter function in children with organic causes of constipation (e.g., anorectal malformation, spinal cord lesions)
Children with anorectal malformations need an accurate functional evaluation after anorectal surgery in order to evaluate the residual anorectal function. Additionally, in the pre-surgery workup before reverting colostomy or ileostomy, ARM may be indicated in order to exclude the presence of outlet-obstruction defecation.
Spinal cord abnormalities may increase the tone of the anal sphincters as a consequence of the damage of upper motoneurons and an exaggerated contraction and anal spasms upon balloon dilation or sphincter relaxation with smaller balloon inflating volumes [34]. Conversely, in some neurological conditions the anal tone may be decreased due to abnormalities involving the lower motoneuron [35].
-
To evaluate persisting symptoms of constipation with or without fecal incontinence unresponsive to standard medical therapy
-
To evaluate the anorectal function before and after therapeutic interventions such as botulinum toxin injection and biofeedback
-
To assess the defecation dynamics
The incoordination between the relaxation of the anal sphincters and pelvic floor muscles during defecation, called dyssynergic defecation, may be an underlying cause of constipation. This can be evaluated in real-time with ARM during the bear-down maneuver and, in adult population, ARM allows clinicians to differentiate dyssynergic defecation into different phenotypes according to the presence of adequate/inadequate increase in rectal pressure and failed reduction/paradoxical increase in anal pressure (type 1–4) [36]. Regardless of the type of ARM phenotype, dyssynergic defecation leads to outlet-obstruction constipation. This diagnosis can be confirmed by the inability of expelling the balloon. In children, both the bear-down maneuver and the balloon expulsion test may be falsely labelled as negative, because of the lateral position adopted during the test and the anxiety due to defecate in the presence of the clinicians [19].
8.5 Future Perspectives and Conclusions
Over the last decade, remarkable technical advances, in terms of probe miniaturization and pressure recording systems, have led to a more detailed understanding of the anorectal function. High-resolution (HRAM) and 3D high-definition (3DHDAM) systems will gradually replace conventional low-resolution anorectal manometry. However, in children, although HRAM provides a greater characterization of defecatory disorders phenotypes, fecal incontinence, and anorectal dysmotility in adult population as well as in pediatric patients, it is still limited by the lack of standardization, interpretation, and normal data. The increasing application of new system in clinical will certainly lead to a substantial improvement of appropriate management driven by specific manometric patterns and underlying pathophysiological abnormalities.
References
Fritsch H, Brenner E, Lienemann A, Ludwikowski B. Anal sphincter complex: reinterpreted morphology and its clinical relevance. Dis Colon Rectum. 2002;45(2):188–94.
Kumar S, Ramadan S, Gupta V, Helmy S, Atta I, Alkholy A. Manometric tests of anorectal function in 90 healthy children: a clinical study from Kuwait. J Pediatr Surg. 2009;44(9):1786–90.
Benninga MA, Wijers OB, van der Hoeven CW, Taminiau JA, Klopper PJ, Tytgat GN, et al. Manometry, profilometry, and endosonography: normal physiology and anatomy of the anal canal in healthy children. J Pediatr Gastroenterol Nutr. 1994;18(1):68–77.
Bajwa A, Emmanuel A. The physiology of continence and evacuation. Best Pract Res Clin Gastroenterol. 2009;23(4):477–85.
Rasijeff AMP, Withers M, Burke JM, Jackson W, Scott SM. High-resolution anorectal manometry: a comparison of solid-state and water-perfused catheters. Neurogastroenterol Motil. 2017;29(11):13124. https://doi.org/10.1111/nmo.13124.
Lee TH, Bharucha AE. How to perform and interpret a high-resolution anorectal manometry test. J Neurogastroenterol Motil. 2016;22(1):46–59.
Ambartsumyan L, Rodriguez L, Morera C, Nurko S. Longitudinal and radial characteristics of intra-anal pressures in children using 3D high-definition anorectal manometry: new observations. Am J Gastroenterol. 2013;108(12):1918–28.
Banasiuk M, Banaszkiewicz A, Dziekiewicz M, Załęski A, Albrecht P. Values from three-dimensional high-resolution anorectal manometry analysis of children without lower gastrointestinal symptoms. Clin Gastroenterol Hepatol. 2016;14(7):993–1000.e3.
Di Lorenzo C, Hillemeier C, Hyman P, Loening-Baucke V, Nurko S, Rosenberg A, et al. Manometry studies in children: minimum standards for procedures. Neurogastroenterol Motil. 2002;14(4):411–20.
Rodriguez L, Sood M, Di Lorenzo C, Saps M. An ANMS-NASPGHAN consensus document on anorectal and colonic manometry in children. Neurogastroenterol Motil. 2017;29(1):12944. https://doi.org/10.1111/nmo.12944.
Tran K, Kuo B, Zibaitis A, Bhattacharya S, Cote C, Belkind-Gerson J. Effect of propofol on anal sphincter pressure during anorectal manometry. J Pediatr Gastroenterol Nutr. 2014;58(4):495–7.
Keshtgar AS, Choudhry MS, Kufeji D, Ward HC, Clayden GS. Anorectal manometry with and without ketamine for evaluation of defecation disorders in children. J Pediatr Surg. 2015;50(3):438–43.
Pfefferkorn MD, Croffie JM, Corkins MR, Gupta SK, Fitzgerald JF. Impact of sedation and anesthesia on the rectoanal inhibitory reflex in children. J Pediatr Gastroenterol Nutr. 2004;38(3):324–7.
Lamparyk K, Mahajan L, Debeljak A, Steffen R. Anxiety associated with high-resolution anorectal manometry in pediatric patients and parents. J Pediatr Gastroenterol Nutr. 2017;65(5):e98–e100.
Fortier MA, Kain ZN. Treating perioperative anxiety and pain in children: a tailored and innovative approach. Paediatr Anaesth. 2015;25(1):27–35.
Dias R, Baliarsing L, Barnwal NK, Mogal S, Gujjar P. Role of pre-operative multimedia video information in allaying anxiety related to spinal anaesthesia: a randomised controlled trial. Indian J Anaesth. 2016;60(11):843–7.
Lewis Claar R, Walker LS, Barnard JA. Children’s knowledge, anticipatory anxiety, procedural distress, and recall of esophagogastroduodenoscopy. J Pediatr Gastroenterol Nutr. 2002;34(1):68–72.
Zar-Kessler C, Belkind-Gerson J. Anorectal manometry. In: NT CF, Di Lorenzo C, editors. Pediatric neurogastroenterology. Cham: Springer; 2017. p. 117–28.
Belkind-Gerson J, Goldstein AM, Kuo B. Balloon expulsion test as a screen for outlet obstruction in children with chronic constipation. J Pediatr Gastroenterol Nutr. 2013;56(1):23–6.
Carrington EV, Brokjaer A, Craven H, Zarate N, Horrocks EJ, Palit S, et al. Traditional measures of normal anal sphincter function using high-resolution anorectal manometry (HRAM) in 115 healthy volunteers. Neurogastroenterol Motil. 2014;26(5):625–35.
Noelting J, Ratuapli SK, Bharucha AE, Harvey DM, Ravi K, Zinsmeister AR. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol. 2012;107(10):1530–6.
Li Y, Yang X, Xu C, Zhang Y, Zhang X. Normal values and pressure morphology for three-dimensional high-resolution anorectal manometry of asymptomatic adults: a study in 110 subjects. Int J Color Dis. 2013;28(8):1161–8.
Coss-Adame E, Rao SS, Valestin J, Ali-Azamar A, Remes-Troche JM. Accuracy and Reproducibility of High-definition Anorectal Manometry and Pressure Topography Analyses in Healthy Subjects. Clin Gastroenterol Hepatol. 2015;13(6):1143–50.e1.
Vitton V, Ben Hadj Amor W, Baumstarck K, Grimaud JC, Bouvier M. Water-perfused manometry vs three-dimensional high-resolution manometry: a comparative study on a large patient population with anorectal disorders. Color Dis. 2013;15(12):e726–31.
Carrington EV, Grossi U, Knowles CH, Scott SM. Normal values for high-resolution anorectal manometry: a time for consensus and collaboration. Neurogastroenterol Motil. 2014;26(9):1356–7.
Lee HJ, Jung KW, Han S, Kim JW, Park SK, Yoon IJ, et al. Normal values for high-resolution anorectal manometry/topography in a healthy Korean population and the effects of gender and body mass index. Neurogastroenterol Motil. 2014;26(4):529–37.
Tang YF, Chen JG, An HJ, Jin P, Yang L, Dai ZF, et al. High-resolution anorectal manometry in newborns: normative values and diagnostic utility in Hirschsprung disease. Neurogastroenterol Motil. 2014;26(11):1565–72.
Benninga MA, Omari TI, Haslam RR, Barnett CP, Dent J, Davidson GP. Characterization of anorectal pressure and the anorectal inhibitory reflex in healthy preterm and term infants. J Pediatr. 2001;139(2):233–7.
de Lorijn F, Omari TI, Kok JH, Taminiau JA, Benninga MA. Maturation of the rectoanal inhibitory reflex in very premature infants. J Pediatr. 2003;143(5):630–3.
Li ZH, Dong M, Wang ZF. Functional constipation in children: investigation and management of anorectal motility. World J Pediatr. 2008;4(1):45–8.
Sutphen J, Borowitz S, Ling W, Cox DJ, Kovatchev B. Anorectal manometric examination in encopretic-constipated children. Dis Colon Rectum. 1997;40(9):1051–5.
Wu JF, Lu CH, Yang CH, Tsai IJ. Diagnostic role of anal sphincter relaxation integral in high-resolution anorectal manometry for Hirschsprung disease in infants. J Pediatr. 2018;194:136–41.e2.
Langer JC, Rollins MD, Levitt M, Gosain A, Torre L, Kapur RP, et al. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr Surg Int. 2017;33(5):523–6.
Siddiqui A, Rosen R, Nurko S. Anorectal manometry may identify children with spinal cord lesions. J Pediatr Gastroenterol Nutr. 2011;53(5):507–11.
Huang YH. Neurogenic bowel: dysfunction and rehabilitation. In: Cifu DX, Lew HL, editors. Braddom’s clinical handbook of physical medicine and rehabilitation. Amsterdam: Elsevier; 2018. p. 143–149.e7.
Ratuapli SK, Bharucha AE, Noelting J, Harvey DM, Zinsmeister AR. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology. 2013;144(2):314–22.e2.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Di Chio, T., Pesce, M., Peroni, D., Borrelli, O. (2020). High-Resolution Anorectal Manometry and 3D High-Definition Anorectal Manometry in Pediatric Settings. In: Bellini, M. (eds) High Resolution and High Definition Anorectal Manometry. Springer, Cham. https://doi.org/10.1007/978-3-030-32419-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-32419-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32418-6
Online ISBN: 978-3-030-32419-3
eBook Packages: MedicineMedicine (R0)