Abstract
Over the years, there has been progress in the available technology to perform anorectal manometry. For decades, the test had been executed using water-perfusion and sleeve catheter systems. In the past few years, there has been the introduction of both the high-resolution manometry (HRARM) and the 3D high-definition manometry (3DARM or 3DHDM), presenting us the ability to better investigate anorectal dynamics. We are now just beginning to elucidate how these newer systems may be used to expand our understanding, diagnosis, and treatment of patients with defecation disorders, particularly in pediatrics.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others

Keywords
- Anorectal manometry
- Anorectal dysfunction
- Dyssynergic defecation
- Rectal pressures
- Rectoanal inhibitory reflex
Anorectal dysfunction encompasses a variety of disease processes ranging from anatomical to functional abnormalities, which may lead to uncomfortable and distressing symptoms. Anorectal manometry (ARM) is used to obtain an objective assessment of symptoms and often aids in identifying disorders of defecation that cannot always be elucidated clinically. In pediatric patients, the test provides comprehensive information regarding anorectal abnormalities by evaluating the rectoanal muscle coordination , intactness and degree of sphincter tonic contractions, baseline reflexes, and subject perineal and internal rectal sensation. The most commonly evaluated symptoms in pediatrics are constipation and fecal incontinence. Disorders of defecation can be present at birth, while in other patients, it develops over time. Constipation and defecation abnormalities are common and account for approximately 3 % of pediatrician visits [1]. While the incidence of pelvic floor disorders is unknown in the pediatric population, it can affect up to 10–15 % of the adult population [2].
As several of the underlying disease processes including Hirschsprung disease , neuromuscular abnormalities, and dyssynergic defecation can have similar presentations but very different treatments, making the correct diagnosis is important. Anorectal manometry can help differentiate the different etiologies thus helping to guide appropriate therapy. In addition, the ARM can serve as an educational and therapeutic tool by providing information to patients and parents regarding the underlying pathophysiology of their symptoms.
Over the years, there has been progress in the available technology to perform anorectal manometry. For decades, the test had been executed using water-perfusion and sleeve catheter systems. In the past few years, there has been the introduction of both the high-resolution manometry (HRARM) and the 3D high-definition manometry (3DARM or 3DHDM), presenting us the ability to better investigate anorectal dynamics. We are now just beginning to elucidate how these newer systems may be used to expand our understanding, diagnosis, and treatment of patients with defecation disorders, particularly in pediatrics.
Normal Physiology
The pelvic floor is a striated muscular sheet that encloses the anorectum and urinary tract and in conjunction with the anorectal sphincters acts to maintain fecal continence and facilitate defecation [3, 4]. The anorectum is comprised of the union of the internal (IAS) and external (EAS) anal sphincters and the levator ani complex, including the puborectalis muscle, which forms a sling posteriorly, angulating the anal canal at rest [5]. The proximal, medial internal sphincter is formed by thickened circular smooth muscle innervated by the enteric nerves and thus under involuntary, reflexive control, while the distal, lateral external sphincter is comprised of skeletal muscle innervated by sacral nerves, under voluntary control. As the two sphincters are adjoining, they are frequently difficult to differentiate, particularly in younger patients in whom the sphincter size is very small [6, 7].
Continence is maintained at rest by a combination of sphincter pressure with the puborectalis contraction, together greatly exceeding the intrarectal pressure, thus preventing stool passage [8, 9]. The puborectalis muscle (PR ), part of the levator ani muscle complex, is made of skeletal muscle. At rest it forms a sling around the anorectum producing an angle between 85 and 105°. By angulating the rectum, it helps to prevent stool passage and thus assists with continence at rest. Normal physiology has been assessed via ultrasound and MRI, strengthening our understanding of the complex area and the development of the area as a child grows [10].
Defecation requires coordination of multiple muscle systems, involving contraction and relaxation at appropriate times to expel stool. In normal physiology, stool enters the rectum, distending the rectal walls and triggering a reflexive temporary relaxation of the internal sphincter, the rectoanal inhibitory reflex (RAIR) that elicits the urge to defecate. If the subject is not in an appropriate location to pass the stool, voluntary contraction of the external sphincter with persistent contraction of the puborectalis occurs, thus deferring defecation. Once defecation is deemed appropriate by the subject, expulsion of stool can be initiated. In healthy individuals with normal anorectal dynamics, this involves relaxation, contraction, and coordination of muscle systems. Specifically, the abdominal muscles contract to increase intra-abdominal pressure, propelling the stool forward from the rectum through the anal canal. At the same time, there is relaxation of the pelvic floor muscles including the puborectalis muscle, straightening the anal canal and allowing free passage of stool [11, 12]. Finally, both the external and internal sphincters relax, permitting stool to flow out of the canal and thus completing defecation.
Anorectal Manometry
Technical Aspects
There are two main compartments to an anorectal manometry system. These are the catheter or probe with a pressure-sensing apparatus and an inflatable balloon at its tip and the pressure-recording apparatus serving to amplify/record input, display information, and analyze data. Over the past decade, there have been significant advances in technology so that today there are multiple systems available for anorectal assessment, each with their own advantages and disadvantages. For years ARMs have been completed with basic performance systems including sleeve catheters, water-perfusion machines, and air-filled balloon catheters. Their use is now gradually being replaced with high resolution and 3D high definition. For the purpose of this chapter, the most commonly used systems will be reviewed including water perfusion, high resolution, and 3D high definition (Fig. 10.1).
The water-perfusion catheter consists of a flexible thin (diameter between 3.5 and 7.0 mm), plastic tube with four to eight side holes circumferentially or spirally arranged and a central catheter for balloon inflation. The catheter is connected to a perfusion apparatus with a pneumohydraulic pump set to pressures of 10–15 psi with water slowly perfused through the side holes at a rate of 0.1–0.5 mL/min/channel.
In 2007, with advances in technology, a high-resolution, solid-state manometric system was developed that has channels at 0.5–1.0 cm intervals. Each has multiple sensing points which together allow for retrieval of many (usually 36) data points producing a topographical plot of intraluminal pressure. This large amount of data retrieval provides a clearer visualization of the area and prevents loss of potentially important information. The results of the high-resolution catheter correlate well with the water-perfusion studies. Most recently, a 3D high-definition catheter was developed, producing even more accurate and detailed data retrieval. It is 10 cm in length and consists of 256 solid-state microtransducers placed circumferentially 3 mm apart. Due to the placement of these sensors, the results can be interpreted in a multidimensional fashion.
Since the creation of these systems, there has been much interest questioning if the newer modalities of anorectal manometry present added benefit over the older systems. When comparing the various catheter systems, the water-perfusion system has advantages in that it remains a low-cost option with ease of interpretation but can be difficult to calibrate and significant time is needed for maintenance of fluid channels. The newer technology with solid-state catheters has more sensors at closer intervals, thus providing significantly greater anatomic detail than prior systems, including a possible differentiation of the internal and external sphincter, which was not achieved previously [13]. The HRARM and 3DHDM are technically easier to use and, once placed in the appropriate position, do not require significant manipulation with minimal sensor migration, thus improving accuracy. Recently, the 3DARM has allowed for more detailed understanding of the anal canal anatomy. Specifically, it was used to construct a model of the anal canal pressures in pediatric patients noting the longitudinal and radial asymmetry of the anal canal. Thanks to this technology, it is now known that the EAS contributes to distal canal resistance, while PR and IAS contribute to proximal canal [14].
Although these newer probes are exciting, they are much more expensive, require significant time for cleaning, have a shorter life span, and are temperature sensitive. As the HRARM and 3DHDM are relatively new devices, their utility and practicality have not been fully established, particularly in the pediatric population. It is hypothesized that it may be helpful in further understanding the anatomy particularly in those with anatomical anorectal disorders and improved planning for procedures in this area [15]. Several ongoing studies are hoping to investigate if these newer technologies at an increased cost translate into clinical relevance.
Methodological/Practical Aspects
The ARM can be done in children of any age; however only children (usually 5 years and older) are typically able to cooperate with the sensory testing (external and internal) and dynamic components of the test (squeeze and bear-down maneuvers). Thus for younger patients, the ARM is usually limited to the analysis of anal sphincter resting pressure and RAIR. In preparation for an ARM, patients are encouraged to defecate and empty the rectal vault prior to the study. If there is a suspected large stool burden, an enema or suppository is used to prevent stool interference. Typically, as infants have soft stool and enemas may be traumatic at this age, no preparation is necessary [16]. It is suggested that medications that may interfere with function such as opioids or anticholinergics are held during the testing.
To set up for the exam, the patient is placed in the lateral decubitus position, with knees drawn to the chest, thus both hips and knees flexed passed 90°. A digital rectal exam (DRE ) should be completed prior to the exam to evaluate the anatomy for abnormalities and gain a baseline assessment of the function of the area. It also provides a sense of the degree of stool burden and the extent of the patient’s ability to follow commands which is necessary during the study. Adult studies have shown that the digital rectal exam can produce findings that are comparable to the results from the ARM [17]. Prior to the digital insertion, the perianal area should be examined along with assessment of external perineal sensation and anal wink. A finger is then inserted into the rectal canal to evaluate resting tone, squeeze pressure, and defecation dynamics including the presence of a paradoxical puborectalis contraction on bear down.
After completion of the DRE , a lubricated manometry probe is inserted into the rectum. Once placed and in the appropriate location, it is held there for at least 90 s for the anorectal area to acclimate to the insertion prior to obtaining data. It is important to provide clear and detailed explanations during the study as the clinician’s verbal commands and clarifications have been shown to affect accuracy of results [18]. Helping the patient to relax by taking deep breaths or other techniques may be helpful in achieving a better baseline measurement.
Ideally the ARM study is completed in an awake patient without anesthesia or sedation, thus allowing voluntary and sensory testing. However, at times this is not feasible and anesthesia must be given, particularly in the toddler age. As above, one must be aware that this becomes a more limited study as these medications can alter the data. This should be accounted for when interpreting the study. It has been shown that ketamine and midazolam do not affect the sphincter pressure or RAIR response, while propofol decreases the resting sphincter pressure in a dose-dependent manner, although the normal RAIR is maintained [19–21].
Analysis
Baseline, dynamic, and sensory information can be obtained from an anorectal manometry study. Typically a complete study will assess sphincter pressure, bear-down maneuvers, sensation, and reflexes; however in specific situations, the test can be tailored toward particular questions. The following are the common assessments that are completed during the ARM study.
Resting basal pressure : After the patient is relaxed and comfortable with the probe in place, the basal resting sphincter pressure is obtained. This canal pressure measurement is comprised of mostly IAS tone (80 %) with some EAS pressure [22]. A low resting pressure could be indicative of weakness or disruption in the sphincter musculature. With the newer technology, the sphincter pressure can be measured with simple insertion of the catheter and obtaining data from the high-pressure zone. However, with water-perfusion manometry catheters, there are various methods employed. The most common of these is the station pull-through, when sensors are circumferentially arranged on the probe, or continuous withdrawal with spirally arranged sensors.
Squeeze: The squeeze pressure is used to assess sphincter strength/tone. It is produced by the patient voluntarily maximally tightening the anal sphincter and calculated as the highest pressure increase over the baseline resting pressure. This can be calculated as the average of three assessments. It is important to ensure that the intra-abdominal pressure is not increased during this exercise as it would alter the squeeze pressure data. A weak squeeze pressure may indicate myogenic or neurogenic causes (Fig. 10.2b).
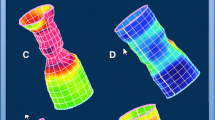
(a) 3D: Resting (Baseline) anal canal during initial recoding. A moderate degree of increased sphincter pressure can be seen. This is often due to patient discomfort/anxiety. It is important to make sure the probe position does not cause discomfort and that the patient is allowed and encouraged to relax as much as possible. (b) 3D squeeze: Significantly increase pressure of sphincter (large white arrow), no pressure increase in abdomen and rectal balloon (rectal pressure, open arrow). (c) 3D bear down: Relaxation of the anal sphincter (black arrow), increase in pressure in the rectum (white arrow). (d) 3D dyssynergic defecation during bear down: Increased sphincter pressure (white arrow) in conjunction with only slightly increased rectal pressure (black arrow). (e) Paradoxical puborectalis: During the bear-down maneuver, a high-pressure area is seen above the sphincter (white arrow) in only the posterior aspect of the anal canal. This is the puborectalis sling which is not relaxing normally. The black arrow points toward the contracted sphincter which is below the puborectalis and is also seen in the anterior aspect of the canal
Anal canal length: The canal length is the measured distance between the anal verge and the location with ≥ 5 mmHg pressure increase over the rectal pressure.
RAIR: The rectoanal inhibitory reflex is obtained to assess the presence of the local enteric reflex. Most importantly, the absence of a RAIR suggests the presence of colonic aganglionosis or Hirschsprung disease. The reflexive relaxation of IAS is naturally caused by stool presence but is simulated during an ARM by rapid balloon inflation and deflation. To date, in pediatrics there is no universally agreed criteria for the presence of a RAIR, which has previously been defined as either a drop in pressure by >5 mmHg or >15 % of the resting pressure. There is typically a dose-related response with greater relaxation and duration of relaxation with larger balloon volumes (Fig. 10.3a). When conducting the test, the clinician must be aware of possible migration of the catheter out of the sphincter, particularly during WPM. Catheter migration may falsely indicate a RAIR response when there is none (Fig. 10.3b). This is the most common cause of a false-positive RAIR (an apparent anal canal relaxation is seen but falsely produced by the catheter migrating in and out of the sphincter region/high-pressure zone with balloon inflation by lack of digitally securing the catheter to the anal margin). The most common cause for a false-negative RAIR test (there is no anal canal relaxation seen, despite balloon insufflation) is a dilated rectum, often due to chronic stool retention. As the rectum is dilated, the balloon does not reach the needed volume to adequately stretch the rectal wall, needed to elicit an anal sphincter relaxation.
(a) Dose-response RAIR 3D ARM. White arrows point to rectal balloon insufflation (which increases rectal sensor pressure). Anal canal relaxation (sphincter relaxation) is seen after each insufflation (black arrows). (b) WP RAIR. The black arrow signals balloon insufflation. The red bar was placed when catheter migration occurred, erroneously making the tracing appear as if anal canal relaxation had resulted from the balloon pressure on the rectum (seen in all four ports). This is a false-negative RAIR
Sensation: Testing the patient’s sensation is an important part of the ARM exam as it provides additional information regarding the patient’s perception of stool which can be indicative of anorectal dysfunction. Sensation is assessed in an awake, active participant (usually aged 5 years and older) by a gradual increase in balloon inflation size. First sensation is defined as the lowest balloon volume that is sensed by the patient. The urge sensation is the lowest balloon volume at which the patient develops the urge to defecate. Finally, the maximum tolerable sensation is the inflation size that is associated with severe urgency and pain. Decreased internal sensation is most often seen with a chronically dilated rectal canal due to persistent constipation.
Bear-down maneuver: The bear-down maneuver , or simulated defecation, is used to assess anorectal and pelvic floor pressure changes during attempted defecation. Similar to above, patients need to have the maturity to understand and cooperate with the testing. This ability is usually acquired around the age of 5 or 6 years. With normal defecation dynamics, there is an expected increase in rectal thrust pressure due to abdominal muscle contraction coordinated with a decrease in anal sphincter pressure. Patients in which these coordinated movements do not occur are thought to have dyssynergic defecation often resulting in outlet obstruction constipation [23]. Additionally, the puborectalis muscle can be visualized with the high-definition manometry, thus allowing for greater understanding of its contribution to defecation dynamics [24] (Fig. 10.2c).
Balloon expulsion: Once these assessments are complete, the probe is removed and a balloon expulsion test is performed. A balloon mounted on a plastic tube is inserted into the rectum and inflated to 50–60 cm3. Some centers use air while others use saline to inflate balloon. The patient is then instructed to sit on a commode and expel the balloon in privacy. The test is considered normal if the patient is able to expel the balloon within a defined time. In adults 1 min is allowed. It is not clear if this time limit is adequate in pediatrics, as well as the right amount of balloon inflation for children, although one series reports that adult volumes and time limit may be applicable [25]. The balloon expulsion test is considered an adjunct evaluation to the ARM to confirm the presence of dyssynergia [25].
Overall, anorectal manometry has been found to be a safe test with rare side effects. With insertion of any foreign object, there is the risk of colonic perforation; therefore care should be taken with placement and removal of probes. Additionally, the study should be delayed or terminated with any abnormal symptom or sign including significant bleeding or acute onset of severe pain.
Reference Values
In general, reliable and reproducible normative values for anorectal manometry are lacking in pediatrics. Although baseline data has been reported in various publications, lack of standardization of the ARM study, a different methodology, and equipment make comparing these values a difficult endeavor [7] (Table 10.1). Therefore, as concrete normative data is lacking in pediatrics, it is always important to correlate the findings with symptom presentation.
The newer modalities of HRARM and 3DHDM have been studied more extensively in the adult literature, showing that the values with high-resolution manometry tend to be higher than those with water perfusion, and there may be differences based on gender, age, and BMI [33–36]. Data is just now being collected in the pediatric population with these modalities [31, 37]. In the future, as these newer systems are used more frequently and studied in more depth, a greater understanding of reference values both in symptomatic and healthy individuals is expected.
Indications
Hirschsprung: Hirschsprung disease is caused by the arrest of migration of the neural crest cells to the colon (see Chap. 25). The length of the aganglionic gut ranges from distal colon (most common) to complete colonic aganglionosis, sometimes even involving varying lengths of small bowel. Any length of colonic aganglionosis leads to an absent RAIR on ARM. Symptoms are frequently present in infancy with delayed passage of meconium (normally in first 24 h) and explosive stool output with digital rectal decompression. Patients may also present with constipation that is refractory to medication, signs of outlet obstruction, and, at times, failure to thrive. Most children are diagnosed within the first year of life, but there is a small subset of patients, particularly those with short-segment Hirschsprung disease that won’t be brought to attention until later in life.
The absence of a RAIR on anorectal manometry has been shown to have a high diagnostic specificity and sensitivity for Hirschsprung disease, particularly in those older than 1 year [38, 39]. The gold standard for diagnosis is a full-thickness biopsy, but the anorectal manometry is a good alternative screening test as it is noninvasive and can often be completed without anesthesia. Patients with an absent RAIR should then proceed to a rectal suction or full-thickness biopsy to confirm the diagnosis.
Anorectal manometry can also be beneficial in postsurgical Hirschsprung patients to characterize the anatomy of the anorectal area, particularly as patients often have one or more surgical interventions and an altered anatomy [40]. Additionally, many patients with Hirschsprung disease continue to have symptoms postsurgically; the anorectal manometry can help to guide further management including additional necessary surgical interventions or medication therapy [41, 42].
Anal achalasia may easily be confused with Hirschsprung disease as the symptoms may be similar including chronic constipation, abdominal distention, and similar findings on ARM: high sphincter tone and non-relaxation of the sphincter with balloon inflation. However, these patients have a normal rectal biopsy [43, 44]. It is likely that anal achalasia is the disease previously known as “ultrashort-segment Hirschsprung disease.” These patients are typically treated similarly to postsurgery Hirschsprung patients, as both the anal achalasia and the post-op Hirschsprung patients have a non-relaxing internal sphincter. Internal anal sphincter botulinum toxin injections have been very successful in improving defecation, although internal sphincter myotomy may be required in a subset of nonresponders [45, 46]. Thus, it is important to categorize these patients in order to provide them with the most appropriate therapy.
Neuromuscular: Patients with neuromuscular disorders such as myopathy or muscular dystrophy can frequently present with symptoms of anorectal dysfunction including constipation and fecal incontinence. Neuromuscular disorders can be evaluated with anorectal manometry to gain a further understanding of sphincter function in addition to the pelvic floor strength. Although there are no specific ARM findings, those with neuromuscular diseases will frequently have hypotonia leading to low resting and squeeze pressures of the sphincter. There will be a RAIR response in these patients as the neurological reflex is intact, but the dose response to increasing inflation sizes may not be present [47]. Decreased muscular strength may also lead to decreased rectal thrust during Valsalva at the time of defecation. Patients with neuromuscular diseases and anorectal dysfunction can be difficult to treat as there are no medical interventions to reverse the disease process. These patients may respond well to conventional constipation therapy including laxative use and scheduled toilet use [48]. Physical therapy may help condition and exercise the striated muscles involved.
Anatomical : Structural abnormalities should be evaluated, particularly in those with postsurgical symptoms. For example, those with imperforate anus repair who remain symptomatic should have an ARM to assess postsurgical sensory and functional capabilities as these may remain abnormal even after the anatomy is repaired [49] (see Chap. 29). Additionally, patients who have undergone colostomy/diverting ileostomy and are preparing for reversal should have anorectal manometry completed to assess functioning of the area and rule out obstructed defecation prior to surgery.
Fecal incontinence: Fecal incontinence which includes both the passage of large bowel movements into the underwear in addition to slow leakage and streaking of the underwear can be further evaluated with an ARM study (see Chap. 43). Although fecal incontinence is frequently due to constipation, the ARM study, particularly the newer modalities, can be used to evaluate for other etiologies. For example, it may be able to show abnormalities in the anal sphincter functioning which can contribute to fecal incontinence. Additionally, spinal cord abnormalities such as meningomyelocele and tethered cord can affect innervation to the sphincter, altering its ability to aid in continence. As the spinal cord lesion may produce upper motor neuron abnormalities, there can be exaggerated contractions or anal spasms of the sphincter with balloon dilation and megacolon. In case of a lower motor neuron syndrome, decreased anal tone may be found. Patients with these suggestive findings on ARM should have an MRI completed to further examine the spinal cord (Fig. 10.4) [28, 50, 51].
Chronic constipation: Anorectal manometry can be used for evaluation in patients with chronic constipation (see Chap. 42). Studies have found that those with chronic constipation have specific anorectal manometry findings including increased frequency and amplitude of the internal anal sphincter contractions [52, 53]. As previously described, in order to appropriately pass stool, subjects need coordination of various pelvic and abdominal muscle systems. Some patients have abnormal movements in some or all of the muscle systems, leading to inappropriate muscle relaxation or contraction, thus complicating defecation [54]. This type of abnormality in defecation dynamics, called dyssynergic defecation, is thought to be the cause of some forms of constipation, particularly related to outlet obstruction [55]. Dyssynergic defecation can be classified according to abnormalities in three areas that can be assessed by anorectal evaluation during bear-down maneuvers including degree of perineal descent during defecation, perineal location at rest, and anal resting pressure [56]. These findings of dyssynergic defecation can be confirmed via an abnormal balloon expulsion test. Newer technology has provided a deeper understanding of anorectal dysfunctions and has helped to identify phenotypes in defecatory disorders and fecal incontinence in addition to providing improved classification of the puborectalis muscle and its role in outlet obstruction [24, 57].
In adult patients, the phenotypic characterization of dyssynergic defecation has been classified into the following four categories related to combinations of rectal thrust in addition to anal canal relaxation [58]:
-
Type 1: paradoxical increase in anal pressure with increase in rectal pressure (>40 mmHg).
-
Type 2: paradoxical increase in anal pressure without increase in rectal pressure (<40 mmHg, poor propulsive force).
-
Type 3: adequate increase in rectal pressure with failed reduction in anal pressure (no anal relaxation) (<20 % baseline pressure).
-
Type 4: inadequate increase in rectal pressure with failed reduction in anal pressure.
Type 4 is the only one that differentiated between healthy volunteers and those with functional constipation [59]. While it is likely that these rectoanal dynamics are similar, it is not currently known whether this classification applies and is useful in children.
Dyssynergic defecation has been treated with biofeedback with varying success in the pediatric population [48, 60]. Using sensors and guidance via animated games, patients are taught to appropriately relax the pelvic floor and sphincters while increasing abdominal pressure. The intention is that with improved muscle coordination, the patient will be able to expel stool more efficiently, decreasing the rectal stool burden.
Anorectal manometry can be used both to diagnose dyssynergic defecation and to guide specific biofeedback treatment, including targeting the puborectalis muscle. Recently, it was found that many healthy adults were found to have dyssynergic patterns of defecation using the 3DHDM. This is hypothesized to be in part related to the larger size and less flexibility of the probe thus possibly stretching the sphincter, leading to decreased accuracy in the results [59]. Therefore, this discrepancy must be taken into account when using the 3DARM system to analyze patients [59], particularly until more data is available in pediatrics.
Conclusion
Anorectal manometry is a safe and well-tolerated procedure that provides valuable information regarding the underlying anatomy and functionality of the anorectal canal. Many pediatric patients have varying symptoms consisting of constipation and/or fecal incontinence which are debilitating and embarrassing. Anorectal manometry can be used to differentiate several of the disease processes that may present with similar symptoms but require different treatments including Hirschsprung disease, spinal cord lesions, neuromuscular disease, and dyssynergic defecation. In recent years, newer technology has been introduced that has allowed us to better describe the anorectal canal and understand anorectal pathology including asymmetric sphincter pressure and types of dyssynergic defecation. However, as these modalities are relatively new, their clinical utility and superiority over prior testing modalities have yet to be determined in pediatrics. In conjunction with correlation to a patient’s symptoms, anorectal manometry is a useful tool to understand the pathophysiology of specific disease entities and for determination of appropriate interventions and treatments. With time, there is anticipation that the clinical usefulness of the newer modalities including 3DHDM and HRARM will be clarified and appropriately implemented.
References
Loening-Baucke V. Constipation in children. Curr Opin Pediatr. 1994;6(5):556–61.
Bharucha AE, Pemberton JH, Locke GR. American gastroenterological association technical review on constipation. Gastroenterology. 2013;144(1):218–38.
Bharucha AE. Pelvic floor: anatomy and function. Neurogastroenterol Motil. 2006;18(7):507–19.
Padda BS, Jung SA, Pretorius D, et al. Effects of pelvic floor muscle contraction on anal canal pressure. Am J Physiol Gastrointest Liver Physiol. 2007;292(2):G565–71.
Jorge JM, Wexner SD. Anatomy and physiology of the rectum and anus. Eur J Surg. 1997;163(10):723–31.
Fritsch H, Brenner E, Lienemann A, et al. Anal sphincter complex: reinterpreted morphology and its clinical relevance. Dis Colon Rectum. 2002;45(2):188–94.
Kumar S, Ramadan S, Gupta V, et al. Manometric tests of anorectal function in 90 healthy children: a clinical study from Kuwait. J Pediatr Surg. 2009;44(9):1786–90.
Bajwa A, Emmanuel A. The physiology of continence and evacuation. Best Pract Res Clin Gastroenterol. 2009;23(4):477–85.
Penninckx F, Lestar B, Kerremans R. The internal anal sphincter: mechanisms of control and its role in maintaining anal continence. Baillieres Clin Gastroenterol. 1992;6(1):193–214.
Benninga MA, Wijers OB, van der Hoeven CW, et al. Manometry, profilometry, and endosonography: normal physiology and anatomy of the anal canal in healthy children. J Pediatr Gastroenterol Nutr. 1994;18(1):68–77.
Liu J, Guaderrama N, Nager CW, et al. Functional correlates of anal canal anatomy: puborectalis muscle and anal canal pressure. Am J Gastroenterol. 2006;101(5):1092–7.
Raizada V, Bhargava V, Karsten A, et al. Functional morphology of anal sphincter complex unveiled by high definition anal manometry and three dimensional ultrasound imaging. Neurogastroenterol Motil. 2011;23(11):1013–9.e460.
Lee YY, Erdogan A. Rao SS High resolution and high definition anorectal manometry and pressure topography: diagnostic advance or a new kid on the block? Curr Gastroenterol Rep. 2013;15(12):360.
Ambartsumyan L, Rodriguez L, Morera C, et al. Longitudinal and radial characteristics of intra-anal pressures in children using 3D high-definition anorectal manometry: new observations. Am J Gastroenterol. 2013;108(12):1918–28.
Lee TH, Bharucha AE. How to perform and interpret a high-resolution anorectal manometry test. J Neurogastroenterol Motil. 2016;22(1):46–59.
Di Lorenzo C, Hillemeier C, Hyman P, et al. Manometry studies in children: minimum standards for procedures. Neurogastroenterol Motil. 2002;14(4):411–20.
Soh JS, Lee HJ, Jung KW, et al. The diagnostic value of a digital rectal examination compared with high-resolution anorectal manometry in patients with chronic constipation and fecal incontinence. Am J Gastroenterol. 2015;110(8):1197–204.
Heinrich H, Fruehauf H, Sauter M, et al. The effect of standard compared to enhanced instruction and verbal feedback on anorectal manometry measurements. Neurogastroenterol Motil. 2013;25(3):230–7.e163.
Pfefferkorn MD, Croffie JM, Corkins MR, et al. Impact of sedation and anesthesia on the rectoanal inhibitory reflex in children. J Pediatr Gastroenterol Nutr. 2004;38(3):324–7.
Tran K, Kuo B, Zibaitis A, et al. Effect of propofol on anal sphincter pressure during anorectal manometry. J Pediatr Gastroenterol Nutr. 2014;58(4):495–7.
Keshtgar AS, Choudhry MS, Kufeji D, et al. Anorectal manometry with and without ketamine for evaluation of defecation disorders in children. J Pediatr Surg. 2015;50(3):438–43.
Scott SM, Gladman MA. Manometric, sensorimotor, and neurophysiologic evaluation of anorectal function. Gastroenterol Clin North Am. 2008;37(3):511–38, vii.
Belkind-Gerson J, Surjanhata B, Kuo B, et al. Bear-down maneuver is a useful adjunct in the evaluation of children with chronic constipation. J Pediatr Gastroenterol Nutr. 2013;57(6):775–9.
Xu C, Zhao R, Conklin JL, et al. Three-dimensional high-resolution anorectal manometry in the diagnosis of paradoxical puborectalis syndrome compared with healthy adults: a retrospective study in 79 cases. Eur J Gastroenterol Hepatol. 2014;26(6):621–9.
Belkind-Gerson J, Goldstein AM, Kuo B. Balloon expulsion test as a screen for outlet obstruction in children with chronic constipation. J Pediatr Gastroenterol Nutr. 2013;56(1):23–6.
Hyman PE, Milla PJ, Benninga MA, et al. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2006;130(5):1519–26.
Li ZH, Dong M. Wang ZF Functional constipation in children: investigation and management of anorectal motility. World J Pediatr. 2008;4(1):45–8.
Sutphen J, Borowitz S, Ling W, et al. Anorectal manometric examination in encopretic-constipated children. Dis Colon Rectum. 1997;40(9):1051–5.
Benninga MA, Omari TI, Haslam RR, et al. Characterization of anorectal pressure and the anorectal inhibitory reflex in healthy preterm and term infants. J Pediatr. 2001;139(2):233–7.
de Lorijn F, Omari TI, Kok JH, et al. Maturation of the rectoanal inhibitory reflex in very premature infants. J Pediatr. 2003;143(5):630–3.
Tang YF, Chen JG, An HJ, et al. High-resolution anorectal manometry in newborns: normative values and diagnostic utility in Hirschsprung disease. Neurogastroenterol Motil. 2014;26(11):1565–72.
Banasiuk M, Banaszkiewicz A, Dziekiewicz M, et al. Values from 3-dimensional high-resolution anorectal manometry analysis of children without lower gastrointestinal symptoms. Clin Gastroenterol Hepatol. 2016;14(7):993–1000.e3. doi:10.1016/j.cgh.2016.01.008.
Carrington EV, Grossi U, Knowles CH, et al. Normal values for high-resolution anorectal manometry: a time for consensus and collaboration. Neurogastroenterol Motil. 2014;26(9):1356–7.
Lee HJ, Jung KW, Han S, et al. Normal values for high-resolution anorectal manometry/topography in a healthy Korean population and the effects of gender and body mass index. Neurogastroenterol Motil. 2014;26(4):529–37.
Li Y, Yang X, Xu C, et al. Normal values and pressure morphology for three-dimensional high-resolution anorectal manometry of asymptomatic adults: a study in 110 subjects. Int J Colorectal Dis. 2013;28(8):1161–8.
Noelting J, Ratuapli SK, Bharucha AE, et al. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol. 2012;107(10):1530–6.
Coss-Adame E, Rao SS, Valestin J, et al. Accuracy and reproducibility of high-definition anorectal manometry and pressure topography analyses in healthy subjects. Clin Gastroenterol Hepatol. 2015;13(6):1143–50.e1.
Noviello C, Cobellis G, Romano M, et al. Diagnosis of Hirschsprung’s disease: an age-related approach in children below or above one year. Colorectal Dis. 2010;12(10):1044–8.
de Lorijn F, Kremer LC, Reitsma JB, et al. Diagnostic tests in Hirschsprung disease: a systematic review. J Pediatr Gastroenterol Nutr. 2006;42(5):496–505.
Banasiuk M, Banaszkiewicz A, Piotrowski D, et al. 3D high-definition manometry in evaluation of children after surgery for Hirschsprung’s disease: a pilot study. Adv Med Sci. 2015;61(1):18–22.
Wildhaber BE, Pakarinen M, Rintala RJ, et al. Posterior myotomy/myectomy for persistent stooling problems in Hirschsprung’s disease. J Pediatr Surg. 2004;39(6):920–6; discussion 20–6.
Koivusalo AI, Pakarinen MP, Rintala RJ. Botox injection treatment for anal outlet obstruction in patients with internal anal sphincter achalasia and Hirschsprung’s disease. Pediatr Surg Int. 2009;25(10):873–6.
Neilson IR, Yazbeck S. Ultrashort Hirschsprung’s disease: myth or reality. J Pediatr Surg. 1990;25(11):1135–8.
Doodnath R, Puri P. Internal anal sphincter achalasia. Semin Pediatr Surg. 2009;18(4):246–8.
Chumpitazi BP, Fishman SJ, Nurko S. Long-term clinical outcome after botulinum toxin injection in children with nonrelaxing internal anal sphincter. Am J Gastroenterol. 2009;104(4):976–83.
Doodnath R, Puri P. Long-term outcome of internal sphincter myectomy in patients with internal anal sphincter achalasia. Pediatr Surg Int. 2009;25(10):869–71.
Lecointe-Besancon I, Leroy F, Devroede G, et al. A comparative study of esophageal and anorectal motility in myotonic dystrophy. Dig Dis Sci. 1999;44(6):1090–9.
Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258–74.
Caldaro T, Romeo E, De Angelis P, et al. Three-dimensional endoanal ultrasound and anorectal manometry in children with anorectal malformations: new discoveries. J Pediatr Surg. 2012;47(5):956–63.
Siddiqui A, Rosen R, Nurko S. Anorectal manometry may identify children with spinal cord lesions. J Pediatr Gastroenterol Nutr. 2011;53(5):507–11.
Raghunath N, Glassman MS, Halata MS, et al. Anorectal motility abnormalities in children with encopresis and chronic constipation. J Pediatr. 2011;158(2):293–6.
Feinberg L, Mahajan L, Steffen R. The constipated child: is there a correlation between symptoms and manometric findings? J Pediatr Gastroenterol Nutr. 2008;47(5):607–11.
Keshtgar AS, Ward HC, Clayden GS. Pathophysiology of chronic childhood constipation: functional and morphological evaluation by anorectal manometry and endosonography and colonic transit study. J Pediatr Surg. 2013;48(4):806–12.
Rao SS, Welcher KD. Leistikow JS Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol. 1998;93(7):1042–50.
Bharucha AE. Difficult defecation: difficult problem assessment and management; what really helps? Gastroenterol Clin North Am. 2011;40(4):837–44.
Bharucha AE, Fletcher JG, Seide B, et al. Phenotypic variation in functional disorders of defecation. Gastroenterology. 2005;128(5):1199–210.
Bharucha AE. Rao SS An update on anorectal disorders for gastroenterologists. Gastroenterology. 2014;146(1):37–45.e2.
Ratuapli SK, Bharucha AE, Noelting J, et al. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology. 2013;144(2):314–22.e2.
Grossi U, Carrington EV, Bharucha AE, et al. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut. 2016;65(3):447–55. doi:10.1136/gutjnl-2014-308835.
Rao SS, Benninga MA, Bharucha AE, et al. ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol Motil. 2015;27(5):594–609.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Zar-Kessler, C., Belkind-Gerson, J. (2017). Anorectal Manometry. In: Faure, C., Thapar, N., Di Lorenzo, C. (eds) Pediatric Neurogastroenterology. Springer, Cham. https://doi.org/10.1007/978-3-319-43268-7_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-43268-7_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43266-3
Online ISBN: 978-3-319-43268-7
eBook Packages: MedicineMedicine (R0)