Abstract
Semen analysis is used routinely to evaluate infertile men. A significant overlap in sperm concentration, motility, and morphology between fertile and infertile men has been demonstrated. Abnormalities in the male genome characterized by damaged sperm DNA may be indicative of male subfertility in the setting of normal semen parameters. Standard semen analysis cannot discern subtle sperm defects such as DNA damage. Sperm chromatin structure evaluation is an independent measure of sperm quality that provides clear diagnostic and prognostic capabilities. There are a number of assays available to measure sperm chromatin integrity and sperm DNA fragmentation. Among them, SCSA, TUNEL assay, and sperm chromatin dispersion assay are more common. Sperm DNA integrity has been shown to be an underlying factor in men with varicocele, unexplained infertility, recurrent pregnancy loss, intrauterine insemination failures, and in IVF and ICSI failures. There are multiple factors affecting pregnancy outcome in addition to sperm DNA fragmentation. The lack of established thresholds and conflicting pregnancy outcomes prevent the use of sperm DNA fragmentation as a marker of pregnancy failure. However, it is recommended that sperm DNA fragmentation analysis should be included in the evaluation of the infertile male.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Spermatozoa
- Male infertility
- Oxidative stress
- Sperm chromatin
- DNA fragmentation
- TUNEL assay
- Recurrent pregnancy loss
- ART outcome
-
Assessment of sperm chromatin integrity is important. It provides useful information in cases of male idiopathic infertility, post-chemo/radio therapy, and in couples pursuing assisted reproduction.
-
Pathologically increased sperm DNA fragmentation (SDF) is a paternal-derived cause of repeated ART failures.
-
Assessment of SDF is important for evaluating semen samples prior to their use in assisted reproduction particularly in men with multiple sperm defects.
-
There are multiple assays that can be used to evaluate sperm chromatin and SDF.
-
It is important to evaluate the real cause of DNA damage and provide proper therapeutic strategies.
-
Several studies have correlated sperm DNA fragmentation with pregnancy outcome in IVF.
-
The predictive value of SDF testing in regards to IVF/ICSI outcomes is controversial.
-
There is a strong recommendation that sperm DNA fragmentation be included in the evaluation of infertile men.
1 Introduction
Laboratory-based semen analysis is the cornerstone assessment for male factor infertility [1]. However, impaired semen parameter cannot predict the fertility [2]. As a result, this laboratory test cannot differentiate fertile from infertile men. Earlier studies have shown that male infertility did not only include abnormal conventional semen parameters but also showed a correlation between compromised efficiency of DNA integrity and reduced fertility potential [3]. Human sperm DNA is a complex configuration which is very susceptible to damage resulting in defective chromatin structure and quality leading to infertility. One of the main causes of sperm DNA damage is reactive oxygen species (ROS) [4]. ROS are known to induce lipid peroxidation of the plasma membrane of the sperm which is the primary cause of sperm DNA fragmentation (SDF) . High levels of SDF have been shown to have a negative impact on semen parameters and reproductive potential. This abnormality cannot be detected in routine semen analysis.
Many tests have been developed to measure SDF. The most commonly used SDF tests are the terminal deoxynucleotidyl transferase deoxyuridine triphosphate (dUTP) nick end labeling (TUNEL) assay, sperm chromatin structure assay (SCSA), and sperm chromatin dispersion (SCD) assay [5]. A panel composed of fertility experts worldwide extensively studied the utility of sperm DNA fragmentation test as part of the evaluation of infertile men [6]. Their practice recommendations are based on clinical scenarios, and recommend SDF testing for men with varicocele (high grade varicocele with normal semen parameters or low grade varicocele with abnormal semen parameters), unexplained infertility, recurrent pregnancy loss, recurrent intrauterine insemination (IUI) failures, exposure to environmental pollutants, drugs, radiation, smoking, febrile illness, varicocele, advanced age, and obesity can increase SDF fertilization (IVF) and intracytoplasmic sperm injection (ICSI) failures and men with lifestyle risk factors such as exposure to environmental pollutants, drugs, radiation, smoking, febrile illness, varicocele, advanced age, and obesity can increase SDF smoking [6]. Despite the impact of SDF testing to evaluate infertile men, many reproductive societies such as the American Society for Reproductive Medicine (ASRM), European Association of Urology (EAU), American Urological Association (AUA), and National Institute of Clinical Excellence (NICE) do not recommend its use as part of the routine assessment of male infertility. Good methodological studies should be conducted to determine chromatin packaging defects as well as the clinical utility of SDF testing in the evaluation of infertile men. In this chapter, we describe the sperm chromatin structure, factors associated with abnormal chromatin structure, and discuss the methods available to analyze sperm DNA chromatin and DNA integrity.
2 Limitation of Semen Analysis
Routine semen analysis continues to be the cornerstone of laboratory evaluation of male infertility. However, its ability to diagnose male fertility is limited. Semen analysis provides important information about spermatogenesis, sperm production, formation of spermatozoa, and the individual components of semen and their function; however, there is a significant overlap in the semen parameters such as concentration, motility, and morphology between fertile and infertile [7]. Although sperm motility, concentration, and morphology are parameters that collectively provide important information about the efficiency of spermatogenesis, it is important to look for tests beyond traditional semen analysis [8].
The latest edition of the WHO 2010 laboratory manual provides statistically derived 5th centile lower reference limits. The traditional semen analysis has limited ability to identify the underlying alterations in the molecular and cellular mechanisms that play a critical role in fertilization and fertility. Standard measurements of semen parameters do not provide information about the subtle sperm defects that can affect fertility. The head must contain DNA that has been correctly assembled during spermatogenesis and disassembled during spermiogenesis and finally correctly reassembled to partner with the female DNA to ultimately form the new genome. Similarly, the midpiece must contain mitochondria to provide energy, and the flagellum must be present to transfer the energy to provide the motility. Thus, the outcome can help alleviate the emotional and financial burden to the patient [9, 10]. The introduction of improved automated semen analyzers, smart phone semen testing, microfluidics, and proteomics are all platforms that may potentially provide useful information [11,12,13,14], but the technology is still far away from predicting the correct diagnosis with 100% accuracy.
Therefore, there is a need to combine other diagnostic tools to better discriminate infertile men from fertile men, predict pregnancy outcome in female partners, and calculate the risks associated with adverse reproductive events. Perhaps the candidate test with the greatest potential for inclusion is DNA integrity assessment.
3 Sperm DNA Integrity
Sperm chromatin abnormalities have been extensively studied as a cause of male infertility. With the increasing use of assisted reproductive technologies (ART), especially ICSI, attention has focused on the genomic integrity of the male gamete and concerns about the transmission of damaged DNA. The ability of the oocyte to repair DNA damage is limited, and excessive DNA damage raises concerns about potential chromosomal abnormalities, congenital malformations, and developmental abnormalities in ICSI-born children [15,16,17,18]. Disturbances in the male genomic content are negatively associated with fertility potential of spermatozoa, both in vivo and in vitro [19,20,21,22,23,24,25,26,27]. Sperm DNA damage is indicative of male subfertility regardless of the normal semen parameters [28, 29]. High sperm DNA fragmentation can compromise embryo quality and result in pregnancy loss following ART [23]. With increasing reports in the literature regarding the association of sperm DNA fragmentation with pregnancy outcome, there is a strong recommendation for inclusion of sperm DNA fragmentation in the evaluation of male infertility [30].
Sperm chromatin is different from that of somatic cells in terms of the chromatin packaging [31, 32]. The histones are replaced by protamines, which make the sperm nuclei highly compacted [33]. While in the mice, 95% of nucleoproteins are comprised of protamines which confers 40% less nuclear volume than that of normal somatic nuclei [34], human sperm nuclei retains about 15% of the histones and contains considerably fewer protamines (85%) when compared to the sperm nuclei of other species such as bull, stallion, hamster, and mouse [35, 36]. The distinct mammalian sperm chromatin packaging called toroids is comprised of 50–60 kb that are cross-linked by disulfide bonds [37, 38]. This condensed, insoluble, and highly organized structure confers genetic integrity during transport of the paternal genome through the male and female reproductive tracts, ensuring proper fusion of the male and female genome and correctly expressing the genetic information in the developing embryo [30, 39, 40].
In contrast to other species which contain only one type of protamine (P1), human and mice spermatozoa contain a second protamine called P2 which is deficient in cysteine residues [31]. P2 diminishes the disulphide cross-linking which is responsible for stable packaging and makes the sperm nuclei less compacted and more susceptible to DNA strand breaks [41]. Furthermore, the alterations in P1/P2 ratio and absence of P2 are associated with male fertility problems [42,43,44,45,46]. Distinct differences in P1/P2 ratio are reported between fertile and infertile men and P1/P2 ratio has been shown to correlate with sperm DNA fragmentation [47]. Alterations in P1/P2 ratio have been shown to be a good indicator of disturbances in spermatogenesis and lead to male infertility [48].
4 Indications and Importance of Sperm DNA Integrity in Male Infertility
Evaluation of sperm chromatin integrity can be challenging; it is difficult to link it with the known physiological mechanisms. Furthermore, its role in clinical practice especially ART is still controversial [49,50,51]. Evaluating sperm chromatin structure is complex and different methods are necessary to assess this structure. Several confounding factors such as lack of standardized protocols, validated reference ranges, and the assay principles of various sperm DNA testing assays complicate the interpretation of the results. Not all DNA damage is lethal and the oocyte has the ability to repair sperm DNA damage. Although a sperm with damaged DNA can fertilize an egg, it can result in compromised embryonic growth, miscarriage, or childhood deformities [52,53,54,55,56]. Numerous studies have demonstrated significant differences in sperm DNA damage levels between infertile and fertile men [49, 57,58,59,60,61]. Several etiological factors have been implicated in damaging sperm DNA including environmental and lifestyle factors, varicocele, male accessory gland infections, advanced paternal age, and systemic diseases [5, 52, 62,63,64,65,66].
Varicocele has been shown to have an adverse effect on SDF [67]. Higher SDF has been shown in men with varicocele compared to fertile men [68]. Another study reported higher SDF in infertile men with varicocele compared to infertile men without varicocele [69]. Similarly, the same study reported higher SDF rates in men with varicocele and no history of infertility compared with fertile men without varicocele [69]. In a study by Esteves et al., using SCD, varicocele was identified with 94% accuracy based on the rates of degraded sperm determined by the proportion of degraded sperm in the population of spermatozoa with fragmented DNA which was eight-fold higher in men with varicocele than in donors [62]. SDF is also increased in the presence of oxidative stress in these men [70,71,72]. Varicocelectomy has been shown to be beneficial in select cases [73]. Varicocele repair has been shown to lower SDF and increase the chances of a natural pregnancy [67]. A meta-analysis comprised of six studies that evaluated the effect of varicocelectomy on SDF and found an overall reduction in SDF with a mean difference of −3.37% (95% CI: −4.09 to −2.65; p < 0.00001) [68]. Another study evaluated 92 patients with clinical varicocele and examined semen parameters and SDF before and after subinguinal microsurgical varicocele repair [74]. Significant improvement in SDF was reported from a preoperative mean of 42.6–20.5% post-operative (p < 0.001). Similarly, Smit et al. [75] evaluated 49 men with varicocele, oligozoospermia, and primary infertility. Following varicocele repair, SDF was significantly reduced post-operatively, and higher pregnancy rates through natural conception with ART were reported. Other reasons for testing DNA fragmentation are recurrent pregnancy loss, unexplained infertility, ART, and cancer patients undergoing chemotherapy or radiotherapy [6].
5 Clinical Relevance of DNA Integrity with ART Outcomes
Sperm chromatin integrity is important for effective transmission of genetic information. Abnormal sperm chromatin affects both natural fertility and ART outcomes [70, 73, 76,77,78,79,80]. High SDF as determined by SCSA was shown to result in natural pregnancy failure with high odds ratio of 7.01 (95% CI: 3.68–13.36) [81]. High SDF was also shown to result in increased time to pregnancy in first-time couples without any history of infertility [82, 83]. Both, SCD and TUNEL were able to predict natural pregnancy with over 80% sensitivity and specificity [84, 85]. High levels of SDF have also been associated with poor IUI outcomes [86, 87]. A significant adverse effect of high SDF on clinical pregnancy in both IVF and ICSI was also demonstrated in a meta-analysis comprised of 8068 treatment cycles [86]. Another meta-analysis comprising of 2969 couples demonstrated a 2.2 fold risk of miscarriage when semen specimens with high SDF were used for ICSI (95% CI: 1.54–03.03; p < 0.00001) [88]. Similarly, another meta-analysis study comprising of pooled data from 14 studies, abnormally high SDF was associated with higher miscarriage rates in ICSI cycles (OR: 2.68; 95CVI: 1.40–5.14; p = 0.003) [89]. Furthermore, SDF was higher in couples experiencing recurrent pregnancy loss compared to fertile controls (18.8% ± 7.0% vs 12.8% ±5.3%; p < −0.9001) [90]. All these studies elucidate that higher SDF plays a role in both natural pregnancy and in ART outcomes.
6 Contemporary Sperm Chromatin Integrity Tests
Different methods such as aniline blue staining, acridine orange staining, SCSA, 8-hydroxy-2-deoxyguanosine (8-OHdG) assay, Comet assay, sperm chromatin dispersion (SCD) assay and TUNEL assay are available to evaluate sperm chromatin and DNA integrity. These are described below.
6.1 Aniline Blue Staining
The acidic dye aniline blue has a strong affinity for binding with loose or decondensed proteins due to residual histones. Aniline blue does not measure SDF. It does not even measure DNA features. It is only a measure for chromatin condensation. Aniline blue staining differentiates lysine-rich histones and arginine/cysteine-rich protamine nuclei. Immature sperm nuclei are rich in lysine-rich histones and sperm are stained blue, whereas protamines are rich arginine and cysteine and therefore do not pick up the stain, thus remain unstained. Therefore, this technique is able to differentiate immature and mature sperm in ejaculated spermatozoa [91].
The technique involves air-dried smears of ejaculated or washed spermatozoa fixed in 3% glutaraldehyde in phosphate buffered saline (PBS) for 30 min. The fixed slides are stained in acidic (pH 3.5) 5% aqueous aniline blue solution for 5 min. A total of 200 spermatozoa are counted under bright field microscopy. Percentage sperm stained with aniline blue is counted and should not exceed 25% [92]. Immature, decondensed sperm nuclei are stained light blue (Fig. 8.1a–c). A modified method combines aniline blue counterstained with 0.5% Eosin Y for 1 min [93].
Aniline blue (AB) staining of sperm chromatin in a man with spontaneous recurrent abortion showing (a) normal spermatozoa versus (b) spermatozoa with moderate level of remaining histones and (c) spermatozoa with extensive levels of histones. (Reprinted from Kazerooni et al. [96]. With permission from Springer Nature)
The advantage of this technique is that it is simple and inexpensive and requires only a simple bright field microscope. The disadvantage is that the staining is not homogenous. A high percentage of sperm with nuclear instability is reported with aniline blue staining in patients with varicocele, idiopathic infertility, and unilateral cryptorchidism [94]. While its correlation with other sperm parameters is controversial, aniline blue-stained spermatozoa showed normal sperm count, motility, and morphology [95, 96]. While immature sperm chromatin may or may not correlate with abnormal morphology patterns in asthenozoospermic samples [91, 97], chromatin condensation observed by aniline blue staining was reported to be a good predictor of IVF outcome [93, 94]. The aniline blue test could be considered as one of the complimentary tests of semen analysis for assessment of male infertility [96, 98].
6.2 Toluidine Blue Staining
Toluidine blue is a basic thiazine metachromatic dye that binds selectively with acidic components of the tissue. It has a high affinity to bind with the phosphate residues present in sperm DNA of immature nuclei [6, 99, 100]. Air-dried sperm smears are fixed in ethanol-acetone (1:1) at 4°C for 30 min and hydrolyzed in 0.1 N HCl at 4°C for 5 min, followed by rinsing thrice in distilled water. Smears are stained for 5 min with Toluidine blue (0.05%) prepared in 30% citrate phosphates or McIlvain buffer, pH 3.5. Permanent preparations are prepared after dehydrating in tertiary butanol twice for 3 min each followed by xylene twice for 3 min each. Staining is observed using light microscopy. Normal sperm heads stain light blue, whereas sperm heads with abnormal DNA stain purple–violet due to the metachromatic shift [101, 102]. It is therefore a sensitive probe for DNA structure and packaging. Toluidine blue staining has demonstrated application in assessment of male fertility potential with 95% specificity and a sensitivity of 42% when the threshold is set at 45% [103, 104]. It is a simple and inexpensive stain that has been used for morphological assessment by light microscopy. It has also been shown to correlate with other advanced tests of sperm DNA fragmentation, i.e., SCSA and TUNEL [102, 105].
6.3 CMA 3 Assay
Chromomycin A3 (CMA3) is an indirect assay to measure protamine deficiency in sperm DNA. It is only a measure for chromatin condensation. Poor chromatin packaging is revealed by CMA3 a guanine-cytosine-specific fluorochrome which competes with protamine for binding to the minor grooves of DNA [106]. Spermatozoa exhibiting low protamination show high CMA3 binding [107]. The technique involves air drying of methanol-glacial acetic acid (3:1) fixed sperm at 4°C for 20 min. The slides are treated for 20 min with CMA3 solution prepared in McIvlain’s buffer supplemented with 10 mmol/l MgCl2. Slides are rinsed in buffer and mounted with PBS-glycerol (1:1 vol./vol.) and kept overnight at 4°C.
Staining is observed under fluorescence microscope and 200 spermatozoa are counted on each slide. CMA3-positive spermatozoa indicative of poor protamination stain bright yellow or bright green, whereas CMA3-negative spermatozoa (high protamination) stain faint yellow or dull green [96, 108, 109]. (Figure 8.2a–b). CMA3 staining has demonstrated a sensitivity of 73% and a specificity of 75% and reported to be a good discriminator of IVF success [110, 111]. CMA3 results have shown an inverse correlation with sperm concentration, motility especially morphology. Men with poor sperm morphology exhibited a greater degree of protamine deficiency and DNA damage [112, 113]. Furthermore, significantly higher CMA3 staining has been demonstrated in globozoospermic patients [114]. The sensitivity and specificity of CMA3 staining is strongly correlated with that of aniline blue staining [108]. However, this assay is limited due to inter-observer subjectivity.
Chromomycin A3 (CMA3) staining of sperm chromatin in a man with (a) spontaneous recurrent abortion showing normal spermatozoa versus (b) spermatozoa with protamine deficiency. (Reprinted from Kazerooni et al. [96]. With permission from Springer Nature)
6.4 Acridine Orange
Acridine orange is a flurochrome dye used to measure the susceptibility of the sperm nuclear DNA to acid-induced denaturation. It intercalates into double-stranded DNA as a monomer and binds to a single-stranded DNA as aggregate. Acridine orange fluoresces green when bound to native DNA and green the relaxed acridine orange fluoresces red in denatured DNA [115, 116]. Acridine orange is used both in fluorescence microscopy and in flow cytometry. For fluorescence microscopy, thick semen smears are fixed in Carnoy’s fixative (methanol: acetic acid; 1:3) for 2 hours and stained in acridine orange for 5 min. After rinsing in deionized water, about 200 spermatozoa are examined for the intact (green) and damaged DNA (yellow–orange to red) [96] (Figure 8.3a-c). The DNA fragmentation index is calculated by measuring the ratio of yellow to red/green + yellow to red florescence [115].
Acridine orange (AO) staining of sperm chromatin of a man with spontaneous recurrent abortion showing (a) normal, (b) moderately denaturated, and (c) completely denaturated spermatozoa. (Reprinted from Kazerooni et al. [96]. With permission from Springer Nature)
For flow cytometry, 25–100 μL of sample containing about 1 × 106 spermatozoa are suspended in ice cold PBS at pH 7.4 and centrifuged at 600 × g for 5 min. The pellet is resuspended in ice-cold TNE (0.01 mmol/l of tris-HCl, 0.15 mol/l NaCl, and 1 mmol/l EDTA, pH 7.4) and centrifuged at 600 × g for 5 min. After removing the supernatant, the pellet is again resuspended in TNE containing 10% glycerol and fixed in 70% ethanol for 30 min. The fixed samples are treated with triton-X 100 solution (0.15 mol/l NaCl and 0.08 N HCl; pH 1.2) for 30 seconds. Acridine orange (6 μg/mL, 37 mmol/l citric acid, 126 mmol/l Na2HPO4, 1 mmol/L disodium EDTA and 0.15 mol/l NaCl, pH 6.0) is added. A minimum of 5000 cells are examined by flow cytometery using a light source with excitation at 488 nm light source. The ratio of acridine bound to intact double-stranded DNA fluorescing green at 513–530-nm and acridine orange bound to damaged single-stranded DNA fluorescing red is calculated (630 nm) [117].
Acridine orange positive cells are more likely to have structural abnormalities compared to acridine-orange-negative spermatozoa [118]. In infertile men, acridine orange technique demonstrated significantly higher DNA damage in infertile men compared to controls in men with varicocele. This was significantly reduced after varicocele repair demonstrating the clinical utility of this technique [104, 119]. The acridine orange assay shows low intra-assay variability, and the technique is highly reproducible. A strong positive correlation has been demonstrated between acridine orange assay and other techniques that are used to measure single-stranded DNA, such as TUNEL assay [120]. The cutoff to differentiate between fertile and infertile men varies between 20% and 50% [109, 121, 122]. Single-stranded DNA staining has also shown to negatively correlate with the classical IVF and lower pregnancy rates [116, 122,123,124,125].
6.5 Sperm Chromatin Structure Assay
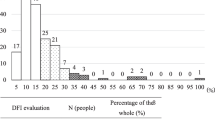
The sperm chromatin structure assay (SCSA) measures in situ DNA susceptibility to the acid-induced conformational helix-coil transition by acridine orange (AO) fluorescence staining. The extent of conformational transition in situ following acid or heat treatment is determined by measuring the metachromatic shift of AO fluorescence from green (native DNA) to red (denatured or relaxed DNA) (Fig. 8.4). The SCSA acid method is much easier to use than the heat treatment. DNA damage that is SCSA-defined is manifested by the DNA Fragmentation Index (DFI) [121].
Schematic of SCSA test showing fluorescence color shift from normal double-stranded (Normal or Native DNA) (green) to fragmented single-stranded DNA (red). (Reprinted from Evenson [221]. With permission from Elsevier)
An aliquot of unprocessed semen (about 13–70 μl) is diluted to a concentration of 1–2 × 106 sperm/ml with TNE buffer (0.01 M Tris-HCl, 0.15 M NaCl, and 1 mM EDTA, pH 7.4). This cell suspension is treated with an acid detergent solution (pH = 1.2) containing 0.1% Triton X-100, 0.15 mol/l NaCl, and 0.08 N HCl for 30 seconds, and then stained with 6 mg/l purified AO in a phosphate-citrate buffer, pH 6.0. The stained sample is placed into the flow cytometer sample chamber [121]. The extent of DNA fragmentation is measured as % of sperm with fragmented DNA termed as DNA fragmentation Index, or DFI. It is the ratio of red fluorescence to total (red + green fluorescence). Native (double-stranded) or intact spermatozoa fluoresce green and fragmented DNA (single-stranded DNA) fluoresce red (Fig. 8.4). Since the SCSA is more constant over prolonged periods of time than routine World Health Organization (WHO) semen parameters, it may be used effectively in epidemiological studies of male infertility [126]. No significant male age-related increase in DFI was demonstrated [127]. SCSA has clearly established clinical thresholds for utility in the human infertility clinic [128]. In clinical applications, the SCSA parameters can distinguish fertile and infertile men. In addition, these parameters are also able to classify men according to the level of in vivo fertility, i.e., high fertility (pregnancy initiated in less than 3 months), moderate fertility (pregnancy initiated within 4–12 months), and no proven fertility (no pregnancy by 12 months). Furthermore, a DFI threshold of <30% can identify samples compatible with in vivo pregnancy (<30%) [25, 86, 129,130,131].
SCSA can predict the various outcomes of ART. However, this is true only for neat semen [132] including the fertilization and implantation rates [22, 86, 133, 134], but this finding was not supported by a study by Lin et al. [135] who reported increased abortion rate in the high DFI (>27%) group. Reports suggest that DFI can be used as an independent predictor of fertility in couples undergoing IUI [22], but an association between SCSA results and IVF and ICSI outcomes are not strong enough [136]. It is also proposed that all infertile men should be tested with SCSA as a supplement to the standard semen analysis [137]. Recent data suggests that ICSI should be the method of choice when DFI exceeds 30% [86].
The SCSA accurately estimates the percentage of DNA-damaged sperm and has a cut-off point (30% DFI) to differentiate between fertile and infertile samples [22, 129]. However, it requires the presence of expensive instrumentation (flow cytometer) and highly skilled technicians. SCSA DFI shows significant association with TUNEL assay results when Spearman’s rank correlation was used, however, regression and concordance correlation results showed that these methods are not comparable. SCSA rather measures DNA damage in terms of susceptibility to DNA denaturation, while TUNEL measures “real” DNA damage [138].
6.6 Measurement of 8-Hydroxy-2-Deoxyguanosine (8-OHdG)
This assay measures levels of 8-hydroxy-2-deoxyguanosine (8-OHdG), which is a byproduct of oxidative DNA damage in spermatozoa. It is the most commonly studied biomarker for oxidative DNA damage. Among various oxidative DNA adducts, 8-OHdG is representative of oxidative DNA damage owning to its high specificity, potent mutagenicity, and relative abundance in DNA [139].
The technique involves three steps: in step 1, DNA extraction is performed with chloroform-isoamyl alcohol (12: 1 v/v) after the sperm cells are washed with sperm wash buffer (10 mmol/l Tris-HCl, 10 mmol/l EDTA, 1 mol/l NaCl, pH 7.0) and lysed at 55 °C for 1 hour with 0.9% SDS, 0.5 mg/ml proteinase K, and 0.04 mol/l dithiothreitol (DTT). After ribonuclease A treatment to remove RNA residue, the extracted DNA is dissolved in 10 mmol/l Tris-HCl (pH 7.0) for DNA digestion. Step II involves the enzymatic DNA digestion that is performed with three enzymes: DNAase I, nuclease P1, and alkaline phosphatase. The final solution is dried under reduced temperature and pressure and is redissolved in distilled and deionized water for HPLC. The third step uses HPLC analysis and consists of a pump, a partisphere 5 C18 column, an electrochemical detector, an ultraviolet detector, an autosampler, and an integrator. The mobile phase consists of 20 mmol/l NH4H2PO4, 1 mmol/l EDTA, and 4% methanol (pH 4.7). The calibration curves for 8-OHdG are established with standard 8-OHdG, and the results are expressed as 8-OHdG/104 dG [97]. 8-oxoG can also be determined using a specific fluorescent probe (8-oxoG) from the OxiDNA assay kit.
8-OHdG provides the most direct evidence suggesting that oxidative sperm DNA damage is involved in male infertility, based on the finding that levels of 8-OHdG in sperm are significantly higher in infertile patients than in fertile controls and have an inverse relationship with sperm concentration [97]. 8-OHdG formation and DNA fragmentation assessed by TUNEL are highly correlated with each other [140]. 8-OHdG levels also are highly correlated with the disruption of chromatin remodeling [141]. Levels of 8-OHdG in sperm DNA have been reported to be increased in smokers, and they inversely correlate with the intake and seminal plasma concentration of vitamin C. It is demonstrated that infertile patients with varicocele have increased 8-OHdG expression in the testis which is associated with deficient spermatogenesis [142]. If not repaired, 8-OHdG modifications in DNA are mutagenic and may cause embryo loss, fetal malformations, or childhood cancer. Moreover, this modification could be a marker of OS in sperm, which may have negative effects on sperm function [143, 144].
6.7 Comet Assay
The comet assay or the single-cell gel electrophoresis is based on the principle of permeabilization and electrophoretic migration of cleaved fragments of DNA. In the neutral comet assay, the migration of the double-stranded DNA loops from a damaged cell comes in the form of a tail unwinding from the relaxed supercoiled nucleus. This unwinding is proportional to the damage that the cell is subjected to. This gives rise to the characteristic appearance of a comet with the tail when seen under fluorescence microscope using DNA stains.
This assay was later modified by Singh et al. [145] using alkaline electrophoresis buffers to expose the alkali-labile sites on the DNA and increase to the sensitivity of the assay to detect both single- and double-stranded DNA. The single- and double-stranded DNA breaks can also be evaluated by the modified two-tailed comet assay [146, 147]. Poor quality chromatin is closely associated with, and highly indicative of, some fertility problems. Many methodologies to assess DNA fragmentation in spermatozoa are available, but they are all unable to differentiate between single-stranded DNA breaks (SSB) and double-stranded DNA breaks (DSB) in the same sperm cell.
The two-tailed Comet assay (2 T-Comet) protocol overcomes this limitation. A modification of the original Comet assay was developed for the simultaneous evaluation of DNA SSB and DSB in human spermatozoa. In this assay, the DNA damage is quantified by measuring the displacement between the genetic material of the nucleus or the comet head and the resulting tail. The tail length is used as an index of the damage. In addition, the “tail moment” is a product of tail length and the intensity or the fraction of the total DNA in the tails. It can also be defined as similar to the torsional moment of the tail [148].
The comet assay is a simple, versatile, sensitive, and rapid assay and has demonstrated some correlation with other assays such as SCSA and TUNEL [149]. The assay requires expertise in result interpretation as it is based on the fluorescence microscopy. The 2 T-Comet assay is a fast, sensitive, and reliable procedure for the quantification and characterization of DNA damage in spermatozoa [150] (Figs. 8.5a–b and 8.6a–c).
Two-tailed (2 T) comet assay protocol detects seven comet types: (1) undamaged; (2) low level of single-stranded DNA breaks (SSB); (3) high level of SSB; (4) low level of double-stranded DNA breaks (DSB); (5) high level of DSB; (6) low level of SSB and low level of DSB; (7) high level of SSB and high level of DSB. Scale bar: 10 μm. (Reprinted from Enciso et al. [150]. With permission from Elsevier)
Characterization of single-stranded DNA (ssDNA) or double-stranded DNA (dsDNA) by fluorescence in-situ hybridization (FISH) and acridine orange staining . (a) ssDNA detection by FISH with a digoxigenin-labeled whole human genome probe and fluorescein isothiocyanate-detected (green) on two-tailed (2 T)-Comets obtained from human spermatozoa, counterstained with propidium iodide (red). (b) 2 T-Comet types found in a normal semen sample first electrophoresed under neutral conditions (from right to left; X-axis) and then 90° electrophoresed under alkaline conditions (from upper to lower; Y-axis), stained with 0.5 × 10–4 mol/l acridine orange. (c) Same images after application of a common electronic filter. (Reprinted from Enciso et al. [150]. With permission from Elsevier)
The comet assay has been used to evaluate the DNA damage after cryopreservation [151]. It has been used to predict embryo development after IVF and ICSI, especially in couples with unexplained infertility [152, 153]. Although the clinical thresholds have been established for diagnosing infertility and predicting IVF outcome [154,155,156,157], not all studies have demonstrated such an association [158].
6.8 Sperm Chromatin Dispersion Test (Halosperm Assay)
The sperm chromatin dispersion (SCD) test produces sperm nucleoids consisting of a central or core and peripheral halo caused by release of DNA loops, signifying the absence of DNA fragmentation. When sperm are treated with an acid solution prior to lysis buffer, a complete absence or a minimal halo is produced in spermatozoa with fragmented DNA. A distinct halo is seen in spermatozoa with intact DNA integrity [159]. When spermatozoa with non-fragmented DNA are immersed in an agarose matrix and directly exposed to lysing solutions, the resulting deproteinized nuclei (nucleoids) show extended halos of DNA dispersion, which can be observed either by bright field microscopy or fluorescent microscopy. The presence of DNA breaks promotes the expansion of the halo of the nucleoid [80, 160,161,162,163,164,165].
In this assay, aliquots of sperm at a concentration of 5–10 million/ml are prepared by diluting in PBS. The samples are mixed with 1% low-melting-point aqueous agarose (to obtain a 0.7% final agarose concentration) at 37 °C. Aliquots of 50 μl of the mixture are pipetted onto a glass slide precoated with 0.65% standard agarose dried at 80 °C, covered with a coverslip, and left to solidify at 4 °C for 4 min. The coverslips are then carefully removed, and the slides are immediately immersed horizontally in a tray of freshly prepared acid denaturation solution (0.08 N HCl) for 7 min at 22 °C in the dark, which generates restricted single-stranded DNA (ssDNA) motifs from DNA breaks. Denaturation is then stopped, and the proteins are removed by transferring the slides to a tray with neutralizing and lysing solution 1 (0.4 mol/l Tris, 0.8 mol/l DTT, 1% SDS, and 50 mmol/l EDTA, pH 7.5) for 10 min at room temperature. The slides are then incubated in neutralizing and lysing solution 2 (0.4 mol/l Tris, 2 mol/l NaCl, and 1% SDS, pH 7.5) for 5 min at room temperature. The slides are thoroughly washed in Tris-borate EDTA buffer (0.09 mol/l Tris-borate and 0.002 mol/l EDTA, pH 7.5) for 2 min, dehydrated in sequential 70%, 90%, and 100% ethanol baths (2 min each), and air-dried. For bright-field microscopy in the improved SCD test (Halosperm® kit), slides were horizontally covered with a mix of Wright’s staining solution (Figs. 8.7a–i and 8.8). Cells can also be stained with DAPI (4′,6-diamidino-2-phenylindole) (2 μg/ml) for fluorescence microscopy [109, 159].
Nucleoids from human sperm cells obtained with the improved SCD procedure . (a–e) DAPI staining for fluorescence microscopy. (a′–e′) Sequential DBD-FISH with a whole genome probe to demonstrate DNA breakage. (a″–e″) Wright staining for bright-field microscopy. (a, a′, a″) Nucleoids with big halo of DNA dispersion. (b, b′, b″) Nucleoids with medium-sized halo. (c, c′, c″) Nucleoids with small halo size. (d, d′, d″) Nucleoids without halo. (e, e′, e″) Nucleoids without halo and degraded. According to the DBD-FISH signal, those nucleoids with small halo, without halo, and without halo and degraded contain fragmented DNA. (f) Microscopic field visualized after Wright staining. Those sperm cells with fragmented DNA are indicated by an asterisk. (g–i) Besides the preservation of the tails, the improved SCD protocol allows for a better chromatin staining, obtaining highly contrasting images for bright-field microscopy (g), where the core and the periphery of the halo are well delimitated (h). (i) The estimation of the halo size was established by comparison of the halo width (2) with the minor diameter of the core (1). (Reprinted from Fernández et al. [222]. With permission from Elsevier)
The SCD test in an individual with varicocele. The frequency of sperm cells without halo and degraded (asterisks) is high, reflective of a very high degree of nuclear damage. (Reprinted from Fernández et al. [222]. With permission from Elsevier)
The SCD test is simple, fast, and reproducible with comparable results to those of the SCSA [162, 164] and TUNEL [166]. The currently available protocol is suitable for bright field microscopy as it significantly reduces equipment cost. The test is successfully used in clinical studies to detect sperm DNA damage [167] and can be simultaneously combined with the FISH (SCD-FISH) assay for detection of aneuploidy in sperm cells [168]. This is the only test allowing sperm DNA fragmentation and chromosomal aneuploidy by FISH in the same cell. Oxidative DNA damage can also be simultaneously determined in the same sperm cell by combining SCD and incubation with an 8-oxoguanine DNA probe [169]. A commercially available Halosperm kit is available to perform this test [170]. Reports suggest that sperm DNA fragmentation as reported by the SCD test is negatively correlated with fertilization rates and embryo quality in IVF/ICSI but not with clinical pregnancy rates or births [162, 171].
6.9 Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling (TUNEL) Assay
This single step staining method labels DNA breaks with FITC-dUTP followed by flow cytometric analysis. TUNEL utilizes a template-independent DNA polymerase called Terminal Deoxynucleotidyl Transferase (TdT), which non-preferentially adds deoxyribonucleotides to 3′ hydroxyl (OH) single- and double-stranded DNA. Deoxyuridine triphosphate (dUTP) is the substrate that is added by the TdT enzyme to the free 3’-OH break-ends of DNA [172,173,174]. DNA fragmentation can be quantified with conventional or the bench top flow cytometry [172] (Fig. 8.9).
TUNEL utilizes a template-independent DNA polymerase called terminal deoxynucleotidyl transferase (TdT) that non-preferentially adds deoxyribonucleotides to 3′ hydroxyl (OH) single and double-stranded DNA. Deoxyuridine triphosphate (dUTP) is the substrate that is added by the TdT enzyme to the free 3’-OH break-ends of DNA. To assess the DNA fragmentation by TUNEL, an APO-DIRECT Kit (BD Pharmingen, CA) is used. It contains the reaction buffer, TdT, FITC-dUTP, and propidium iodide/ RNase stain. The assay kit also contains negative and the positive controls, which are not sperm cells. About 2.5 × 106 sperm are fixed with 3.7% paraformaldehyde for a minimum of 30 min at 4 °C. The sample is centrifuged at 300 × g for 7 min.
Paraformaldehyde is removed by centrifuging the samples at 300 × g for 7 min. Supernatants are discarded and the pellets resuspended with 1 mL of ice-cold ethanol (70% vol./vol.). The tubes are kept at −20 °C for at least 30 min. To create negative sperm controls, the enzyme terminal transferase is omitted from the reaction mixture. To create positive sperm controls, the samples are pretreated with 2% (v/v) hydrogen peroxide and incubation for 1 h at 50 °C. A 50 μL of the stain is added and incubated for 1 h. Following two washes with 1 mL of the “Rinse buffer,” PI /RNase stain is added and incubated for 30 min. For flow cytometry, the laser excitation is provided at 2 wavelengths of 488 nm supplied by a solid blue laser at 20 mW and 640 nm powered by 14.7 mW diode red laser. Green fluorescence (480–530 nm) is measured in the FL-1 channel and red fluorescence (640 nm) in the FL-2 channel. The percentage of positive cells (TUNEL-positive) is calculated on a 1023-channel scale from the flow cytometer software (Fig. 8.10a–e). The analysis is conducted with a similar strategy on both the C6 and the C6 Plus flow cytometer, and dot plots are generated by the BD Accuri software (BD Biosciences, Ann Arbor, MI, United States) [173]. TUNEL results of SDF obtained from a standard (C6) flow cytometer have been compared with a newer version of the same instrument (C6 Plus), and the cutoff, sensitivity, specificity without calibration (adjustment), and after adjustment have been examined. Using identical sperm preparation, matched acquisition settings, the performance of two flow cytometers and two observers has been examined to assess the strength of agreement of the results [175]. After adjustment of the settings, overall concordance was high and the two cytometers showed 100% positive and negative predictive value with 100% area under the curve. The overall correlation coefficient observed between C6 and C6 plus was highly significant (p < 0.0001; r = 0.992; 95% CI 0.982–0.997). After adjustment, the two cytometers showed very high precision of 98% and accuracy of >99%. The inter-observer agreement on C6 flow cytometer for the two observers was 0.801 ± 0.062 and 0.746 ± 0.044 for C6 Plus. A strong agreement was demonstrated between the samples tested on the two flow cytometers after calibration and established the robustness of both instruments [175].
Example of Accuri C6 Workspace and gating strategy used in both laboratories for TUNEL data analysis. (a) FSC/SSC plot showing the gate used for spermatozoa selection (G1). (b) PI/FSC plot with gating for PI positivity (G2). (c) PI/FITC plot of negative control sample (TdT enzyme omitted). (d) PI/FITC plot of standard sample. (e) PI/FITC plot of positive control sample. FSC forward scatter, SSC side scatter, PI propidium iodide fluorescence, FITC fluorescein isothiocyanate fluorescence, Q1-UL upper left quadrant, Q1-UR upper right quadrant, Q1-LL lower left quadrant, Q1-LR lower right quadrant
The standard TUNEL assay can be improved to become more sensitive to DNA fragmentation by incubating sperm cells in 2 mm dithiothreitol (DTT) solution for 45 min prior to fixation with formaldehyde. This modified version of the TUNEL assay was shown to significantly enhance its sensitivity. Mitchell et al. modified the TUNEL methodology by incubating spermatozoa for 30 min at 37 °C with LIVE /DEAD Fixable Dead Cell Stain (far red) (Molecular Probes, Eugene, OR, United States). The cells were then washed three times with culture medium before incubation with DTT allowing both DNA integrity and vitality to be simultaneously assessed [176].
The TUNEL assay has been widely used in male infertility research related to sperm DNA fragmentation. A negative correlation was found between the percentage of DNA-fragmented sperm and motility, morphology, and concentration in the ejaculate [120, 177]. It also appears to be potentially useful as a predictor for IUI pregnancy rates, IVF embryo cleavage rates, and ICSI fertilization rates [19]. In addition, it provides an explanation for recurrent pregnancy loss [149, 177,178,179]. A predictive threshold of 19.2% has been shown significant differentiation between fertile and infertile men with a sensitivity of 64.9% and a specificity of 100% [57, 149]. This is higher than that demonstrated for IUI procedures (12%) [179]. A very high specificity (91.6%) and positive predictive value (90%) was reported at a cutoff point of 16.8% (Fig. 8.11a, b). The high specificity of the TUNEL assay is helpful in correctly identifying infertile patients who do not have sperm DNA fragmentation as a contributory factor [172, 180]. Due to its high positive predictive value, the assay is able to confirm that a man who tests positive is likely to be infertile due to elevated sperm DNA fragmentation. A similar specificity (91%) of TUNEL was reported [181]. The calculated cutoff would be ideal as any value above this threshold will be strongly associated with infertility.
Receiver operator characteristic (ROC) curve showing (a) TUNEL cutoff and the area under the curve. Values within the parentheses represent the 95% confidence interval and (b) Distribution of TUNEL values between controls and infertile men. (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2015–2019. All Rights Reserved)
The TUNEL assay is relatively expensive and time- and labor-consuming. Also, a number of factors can significantly affect assay results including the type and concentration of fixative, fixed sample storage time, the fluorochrome used to label DNA breaks, and the method used to analyze flow cytometric data [182]. The flow cytometric method of assessment is generally more accurate and reliable than fluorescent microscopy, but it is also more sophisticated and expensive and it presents limitations in the accuracy and reproducibility of the measures of sperm DNA fragmentation [182]. Fairly good quality control parameters with minimal inter- and intra-observer variation (<8%) have been demonstrated for the fluorescent TUNEL assay using the bench top flow cytometer [180, 183].
7 Limitations of Current Protocols
One of the criticisms on SDF testing is lack of standardization [184]. While it is true that some of the methods for SDF suffer from high inter-laboratory variation, other tests have been studied extensively to standardize the methods. To achieve this, it is recommended that the testing for SDF should be done in a facility equipped with appropriate instrumentation, qualified technicians, and with both internal and external quality control measures [185]. For example, in a blinded study, two experienced observers carried out inter- and intra-observer variation of TUNEL assay using bench top flow cytometer [183]. The mean TUNEL assay measurement from one observer was confined to the average measurement of the two observers combined with an absolute difference of 1.73% and percent difference of 6.68% in 80% of cases. On the other hand, one TUNEL assay measurement from one observer was likewise limited to the average measurement of the two observers with an absolute difference of 3% in 90% of the cases, while the percentage difference was 9.68% in 80% of the cases. In another study, standardization of the method on SDF testing was assessed in two reference laboratories [183]. No significant differences were detected between the duplicate results. The mean difference between the duplicate readings within each testing centers was 0.5%, while the correlation showed exemplary results (r = 0.75–0.95).
There are three categories in which SDF can be measured directly or indirectly [184]. These include the tests that measure the degree of compaction of the chromatin, tests that measure the DNA breaks before and after DNA denaturation and tests that measure SDF by inserting DNA probes or modified nucleotides at the site of damage. Due to these categories, the results measured from one SDF testing do not imperatively correlate with those obtained by the other tests [186]. In a prospective comparative experimental study on 20 sub-fertile men with unexplained infertility, SCD test measured significantly higher SDF compared to TUNEL assay (20.6 ± 14.0% vs 11.5 ± 7.3%, p < 0.05) [165]. However, these two tests were poorly correlated (r = 0.29) due to the fact that they implemented two distinct methods of SDF detection [165].
As it stands, there are still no clear cutoff values for SDF testing. Sharma et al. [172] provided a detailed protocol and quality control steps on SDF measurement using the TUNEL assay on 95 semen specimens from controls and 261 from infertile men. The positive predictive value was 91.4%, while the negative predictive value was 33.1%. Based on these findings, men with elevated SDF levels are most likely to present a challenge in their reproductive potential. Wewak et al. [84] determined the sperm deoxyribonucleic acid fragmentation index (DFI) of 26.1% as a cutoff point to differentiate infertile men and fertile men using the SCD assay. At this threshold, the prevalence ratio of 2.84 demonstrated the onset of male infertility. In another test using SCD, Lopez et al. [28] reported that the predictive cutoff value of 25.5% DFI could distinguish between successful and unsuccessful IVF or ICSI outcome from 152 infertile couples. SCSA was used to examine the relationship of DNA fragmentation with ART outcomes [59]. The chance of pregnancy in IUI was significantly higher if the value of DFI was 27%. On the other hand, IVF and ICSI outcomes were non-significant in groups with DFI less than 27%. In another study examining the effect of sperm DFI on pregnancy outcome and pregnancy loss in 531 couples after autologous ICSI (n = 416), donor egg procedure (n = 39), and IUI (n = 76), a cutoff of DFI 27% correlated with reproductive outcomes [187].
The current SDF testing methods cannot identify the nature of DNA damage and the location of DNA breaks [188]. Not all SDF tests measure the same damage. Aniline blue and toluidine blue determine the degree of chromatin decondensation while TUNEL, SCD, and SCSA measure DNA breaks [184]. Unlike the semen sample used in ART, SDF measurement is carried out using unprocessed semen [189]. Bungum et al. [132] assessed the effect of SCSA measurement in semen sample from 510 ART cycles prepared by density gradient centrifugation (DGC). No significant difference was seen in clinical pregnancy outcomes between SCSA performed in a neat semen compared to post DGC. In another prospective, observational study comprising of 44 non-azoospermic infertile men and nine fertile men, DFI measured by SCSA increased significantly in infertile men following DGC (25% vs. 15%, p < 0.01) [190]. This may reflect a potential deleterious effect of sperm processing on the integrity of sperm DNA. Similar results were demonstrated in 223 couples undergoing IVF where SDF measurements were analyzed by SCSA after swim-up preparation [191]. Although an abnormal DFI (> 27%) had a lower healthy embryo rate (13.2% vs 27.5%, p < 0.05), there was no noticeable significant differences in fertilization rate, clinical pregnancy rate, and delivery rate. Zini et al. [192] compared the effects of the two sperm processing methods on sperm DNA integrity in 22 semen samples collected from non-azoospermic infertile men. SDF was significantly higher in Percoll-treated spermatozoa compared to samples processed by swim up (10.1% vs 4.8%, p < 0.0001). Mean sperm motility was significantly improved with the two methods (p < 0.005) [192].
8 Controversies of Sperm DNA Fragmentation
Varicocelectomy is recommended in men with a palpable varicocele and abnormal semen parameters [1]. In recent guidelines proposed by Agarwal et al. [193], elevated SDF testing levels may significantly shift the way fertility specialists are discussing varicocelectomy in men with normal semen parameters. Varicocele repair can be considered in infertile men with high grade varicoceles and normal conventional semen parameters or low grade varicoceles with abnormal conventional semen parameters. Multiple studies have determined that elevated SDF can be observed in men with varicoceles even in those with normal conventional semen parameters [63, 194]. Significant reduction in SDF is observed after varicocelectomy [195]. In a prospective study of 60 men with varicocele and abnormal semen parameters, DFI was significantly improved 3–6 months after varicocelectomy (from 29.49% to 18.78%, p < 0.001) [196]. There was a concomitant reduction in ROS (p < 0.001) and significant increase in total non-enzymatic antioxidant capacity (TAC) (p < 0.001) post varicocelectomy. In another prospective study of 72 infertile men with varicocele and oligozoospermia, a significant reduction in DFI was observed after varicocelectomy (from 34.5% to 28.2%, p = 0.024) [197]. Also, other semen parameters such as total sperm count, sperm concentration, percent progressive motility, percent normal morphology were also significantly improved. In recent study of 157 semen samples with varicocele, elevated sperm DFI measured by SCSA of more than 30% was significantly associated with poor motility and viability (p < 0.01). Likewise, abnormal sperm concentration was observed in men with high DFI (24.5% vs. 33.5%, p < 0.05) [198]. SDF testing can help physicians prognosticate infertile men with varicocele. Despite the improvement of SDF after varicocelectomy, there are a number of confounding variables [199]. Further research is warranted to understand fully the exact mechanism(s) of SDF in infertile men with varicocele.
Limited data is available to recommend the benefit of screening for SDF in unexplained infertility, recurrent pregnancy loss, and IUI failure [184]. Couples with unexplained infertility usually demonstrate DNA damage. Vandekerckhove et al. [200] examined the incidence of SDF in couples with previously unexplained infertility who underwent IUI. Using SCD test with a DFI of 20%, the incidence of SDF was 42.9%.
There is still an existing controversy regarding the predictive value of SDF testing the outcomes of IVF and ICSI procedures. SDF alone cannot predict the pregnancy outcomes due to a wide list of factors influencing the ART outcomes [184]. Although the negative impact of elevated SDF on the reproductive outcome in conventional IVF is well studied, its poor association with ICSI is not clearly demonstrated [6]. Lin et al. [135] investigated the relationship of SDF on the outcomes of IVF and ICSI. In 233 couples undergoing ART (IVF = 137; ICSI =86), no significant differences were observed in fertilization rate, good embryo rate and pregnancy rate between the two procedures even in low to high DFI (>27%). On the other hand, total and progressive sperm motility was negatively correlated with high DFI [201, 202]. The quality of post-implantation embryo and spontaneous abortion should be a concern with high DFI affecting the pregnancy outcomes [88, 203]. Cissen et al. [204] performed a systematic review and meta-analysis of 30 extractable data on SDF and clinical outcomes of medically assisted reproduction. TUNEL assay, SCD test, and Comet assay showed no predictive values between IVF and ICSI outcomes. Due to the significant limitations of the evidence available, further research is needed to determine the effect of SDF in reproductive outcome after medically assisted reproduction. In contrast to the recent systematic review and meta-analysis, Simon et al. [205] provided sufficient evidence that SDF has negative impact on reproductive outcome following ART procedures. SDF significantly affects the clinical pregnancy after IVF (OR = 1.65; 95% CI: 1.34–2.04; p < 0.0001) and ICSI (OR = 1.31; 95% CI: 1.08–1.59; p = 0.0068).
Numerous factors can affect the reproductive abilities not only of men but also of women. This is the reason why both partners in an infertile couple should be evaluated at the same time during the assessment of their fertility status. The role of female factors should be addressed in the management of men with SDF [206]. Jin et al. [207] investigated the impact of SDF in 2865 women with different ovarian reserves who underwent ART procedures. Live-birth rate and implantation rate were significantly reduced in women with reduced ovarian reserves when DFI is above 27.3%. In contrast, women with normal ovarian reserves did not demonstrate significance in clinical pregnancy, live-birth rate, and implantation rate with the same values of DFI. Carlini et al. [90] conducted a study on the male factor in 114 Italian infertile men whose wives had recurrent pregnancy loss following natural conception. SDF values were significantly higher in infertile men compared to the controls (18.8% vs 12.8%, p < 0.001).
Based on the results of SDF testing, clinicians may advise the infertile men to take measures to decrease SDF. Yet, there is a lack of evidence to demonstrate that lifestyle changes will improve SDF in men with borderline abnormal or normal conventional semen analysis [184]. Improvement in dietary patterns was able to reduce the DFI (p = 0.05) in 336 men with normal sperm concentration or slight oligozoospermia. In addition, higher sperm concentration and higher level of serum testosterone were observed. The use of antioxidants has also shown a beneficial impact on basic semen parameters, advanced function, outcomes of ART procedures, and live-birth rate [208].
In a placebo-controlled, double-blind, randomized study of 77 infertile men with DFI more than 25%, there was no statistically significant difference observed in those men taking antioxidants for 6 months. Although sperm concentration was significantly improved after the treatment period of 3 months (p = 0.028) and 6 months (p = 0.053) [209]. Intake of antioxidants (vitamins with zinc and selenium) resulted in significant reduction of SDF (−19.1%, p < 0.0004) after 90 days of treatment. In another study, Greco et al. [210] evaluated 38 men with DFI more than 15% and whose wives had one failed ICSI attempt. After 2 months of treatment with antioxidants (vitamin C 1 g/day, vitamin E 1 g/day), significant improvement in clinical pregnancy (48.2% vs 6.9%) and implantation rates (19.6% vs 2.2%) were observed. Despite these findings, further studies with appropriate methodological designs are warranted to determine the benefit of antioxidant therapy to resolve SDF. Despite these findings, antioxidant therapy is a reasonable option for the management of infertile men [211].
9 Common Laboratory Protocols for Measuring DNA Fragmentation by TUNEL and Flow Cytometry (Direct and Indirect Methods)
Sperm DNA integrity is fundamental in sustaining the reproductive potential of a man. This is relevant because of the popularity of ART procedures, which bypass natural selection barriers unlike in the natural process, which only selects sperm with intact DNA to undergo fertilization. The endonucleases which are activated during programmed cell death degrade the sperm chromatin initially into fragments (30 kb) and then into much smaller fragments (50 kb) [180]. DNA fragments being produced during this process can be detected by TUNEL assay. Flow cytometry and fluorescent microscopy can identify the DNA strand breaks using TUNEL assay [28, 212].
The TUNEL assay is one of the most promising methods to measure SDF. This measures both single and double DNA strand breaks. It directly quantifies DNA damage while other tests assess the DNA integrity indirectly by examining its susceptibility to acid or alkaline denaturation. It is detected by flow cytometry making it a robust evaluation for SDF [173, 183, 213]. The modified dUTP can be labeled either directly with fluorescein-dUTP or indirectly through labeled antibodies or streptavidin. Flow cytometry is used in quantification with TUNEL assay which make rapid evaluation of more than 10,000 spermatozoa per sample. This is combined with staining of the nucleus with propidium iodide (PI) to factor out apoptotic bodies in the semen sample which allows additional diagnostic power in two distinct intensities of the spermatozoa. Spermatozoa with normal DNA integrity will only demonstrate background staining. On the other hand, those fragmented DNA with multiple chromatin 3’OH ends will fluoresce brightly [117].
The protocols must be standardized and validated before it can be used in clinical practice. Sharma et al. [180] reported an earlier detailed standardization of the TUNEL assay with less than 10% on both inter- and intra-observer variability and inter assay variability. With a sensitivity of 64.9% and specificity of 100%, a threshold value of 19.25% can differentiate infertile men with SDF from fertile men. In a more recent study on the standardization of TUNEL assay, the cutoff value of 16.8% showed a specificity of 91.6% and sensitivity of 32.6 with a positive predictive value of 91.4% and a negative predictive value of 33.1%. At this threshold, abnormal SDF level are strongly indicative that SDF may be the cause of reproductive incapacity of a man [172].
10 Challenges Using Indirect Assays to Measure DNA Integrity by TUNEL Assay
Ribeiro et al. [214] compared the efficacy between the indirect antibody-based labeling system (BrdUTP/fluorescein-anti-BrdUTP) and the direct labeling system (fluorescein-dUTP). Both labelling systems showed similar staining functions in live spermatozoa. When compared to direct labeling system, the TUNEL indirect labeling system underestimates the SDF with the differences ranging from 19.2% to 85.3% (p < 0.05). These differences were more pronounced in semen samples with total motility less than 40% or weak propidium iodide stained spermatozoa (PI dimmer spermatozoa) higher than 14%. In addition, a major difference was observed when dead spermatozoa were stained (40.1% vs 65.7%, p < 0.05). There was a correlation between the number of immotile spermatozoa and the intensity of difference between the two labeling systems. Indirect TUNEL labeled to lesser extent the PI dimmer population. Compared to direct labeling, indirect labeling only stained a small number from the PI – dimmer population (90.6% vs 17.9%). Overall, only 30–100% of the total number of spermatozoa stained with direct TUNEL labeling system was stained with indirect method. In this study, the most probable reason in the different staining efficiency of both the labeling system was due to the steric hindrance of the antibody during its binding to the BrdUTP. In addition, condensed chromatin architecture in dead spermatozoa contributed to the staining differences.
In earlier studies, measurement of TUNEL assay was highly correlated with sperm vitality [176, 215]. There was a significant difference on the staining efficiency of the dead population of indirect labeling compared to direct labeling (40.1% vs 65.7%, p < 0.05). On the other hand, no significant difference was found on staining the number of live spermatozoa using both TUNEL labeling methods 8.9% vs 8.3%, p > 0.05) [214]. TUNEL assay should be standardized in all laboratory centers performing this specialized test. This will help clinicians to further assess these infertile men whose treatment options may highly depend in the results of SDF testing.
11 Common Direct Methods to Measure DNA Integrity
Apart from the TUNEL assay, the comet assay is likewise a direct method to measure SDF. This quantifies the amount of DNA damage per spermatozoon. The degree of SDF is proportional to the intensity and length of the DNA fragments that stream out of the sperm head. This represents the amount of migrated DNA which looks like a comet with a tail when viewed under the fluorescent microscope and DNA stains. This assay is beneficial for men with severe oligozoospermia as low as 5000 sperm [216]. Comet assay can detect alterations in DNA bases aside from its identification of the usual DNA strand breaks. However, this is not a rapid test, as it demands highly specialized personnel to run the assay.
12 Current Challenges in Sperm Chromatin Integrity Tests
Well-known professional specialty societies do not recommend the routine use of SDF testing in the evaluation of men presenting with problematic reproductive potential [217]. This is due to unavailability of good quality methodological studies in support of the application of this laboratory test in the clinical scenarios. On the other hand, there is a wide list of evidences including systematic reviews and meta-analyses demonstrating the beneficial impact of SDF testing to reproductive outcome. Despite these findings, different professional societies still do not recommend the routine use of SDF testing in the evaluation of infertile men [1, 217, 218]. In a strengths-weaknesses-opportunities-threats (SWOT) analysis by Esteves et al. on the clinical utility of SDF testing, 51 out of 58 fertility expert participants were supportive of the recommendation set by the clinical practice guideline. Thirty participants expressed their concerns regarding the technical weak points of the SDF testing [184].
Cost of the SDF testing is one of the drawbacks of requesting this procedure. It was reported that SDF testing costs roughly $170.4 ± 122.9 (range $0–450). In a survey, 46.9% of clinicians expressed their unwillingness to utilize these test due to cost to the patients [219]. Majzoub et al. [219] developed a questionnaire to survey fertility specialists on major aspects of SDF testing. Forty-nine invited scholars from 19 different countries mostly composed of urologists (44.9%) completed the questionnaires. The majority (79.6%) of the participants commonly requested SDF testing as part of the evaluation of infertile men. TUNEL (30.6%) and SCSA (30.6%) were frequently utilized to analyze SDF. DFI of 30% was used as a threshold value by 61.2% of the participants. The most common indication to request for SDF testing was recurrent conventional IVF failure or pregnancy loss following conventional IVF (91.8%). The least common reason was to assess patients with low grade varicocele and subnormal semen parameters (46.9%). Cost (46.9%) and lack of validation (36.7%) were major factors for not requesting for SDF testing.
13 Future Direction
With support from the Society for Translational Medicine in endorsing the clinical practice guidelines for SDF testing in the evaluation of infertile men, other specialty societies may re-review their recommendations on the potential benefit of this specialized test [193]. There should be an expanded list of indications on who will benefit from this testing and not only be limited to practice recommendations. Good methodological studies should be conducted to determine the positive impact on the clinical utility of SDF testing in the evaluation of infertile men [220]. With more research, a solid evidence-based foundation for future utilization of SDF testing will benefit those men with reduced reproductive potentials as this might be their only hope to father a child.
14 Conclusion
In this chapter, we have emphasized the importance of assessing sperm chromatin integrity. Results of sperm assessment provide useful information in cases of male idiopathic infertility and in couples pursuing assisted reproduction. There are multiple assays that can be used to evaluate sperm chromatin. Each assay has advantages and limitations. Choosing the right assay is important and depends on factors such as equipment cost, availability of an andrology laboratory, and the presence of experienced technicians. It is important to determine the underlying cause of DNA damage and provide proper therapeutic treatment before attempting ART to minimize downstream potential side effects of offspring. It is important to design methods for selecting sperm with undamaged DNA in ART, especially in ICSI. Assessment of sperm DNA damage can be a potential tool for evaluating semen samples prior to their use in assisted reproduction. It allows for the chance to select spermatozoa with intact DNA or with the least amount of DNA damage for use in assisted conception. It provides better diagnostic and prognostic capabilities than standard sperm parameters for assessing male fertility potential. There is a strong data supporting the inclusion of sperm DNA fragmentation in the evaluation of the infertile male.
15 Review Criteria
An extensive search of studies examining the relationship between sperm chromatin and sperm DNA fragmentation and male infertility and ART outcome was performed using search engines such as Google Scholar and PubMed. The start and end dates for these searches were September 1996 and September 2018, respectively. The overall strategy for study identification and data extraction was based on the following key words: “male infertility,” “sperm chromatin,” “reactive oxygen species,” “infertile men,” “DNA fragmentation,” “marks of sperm chromatin assessment,” “direct and indirect markers of sperm DNA fragmentation,” “sperm DNA fragmentation and male infertility,” and “sperm DNA fragmentation and ART failure.” Articles published in languages other than English were excluded. Data published in conference or meeting proceedings, websites, or books was also excluded.
References
Jarow J, Sigman M. The optimal evaluation of the infertile male: AUA best practice statement. American Urological Association, Education and Research, Inc. 2010;1–38.
Patel AS, Leong JY, Ramasamy R. Prediction of male infertility by the World Health Organization laboratory manual for assessment of semen analysis: a systematic review. Arab J Urol. 2018;16(1):96–102.
Leuchtenberger C, Schrader F, Weir DR, Gentile DP. The deoxyribosenucleic acid (DNA) content in spermatozoa of fertile and infertile human males. Chromosoma. 1953;6(1):61–78.
Tremellen K. Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update. 2008;14(3):243–58.
Majzoub A, Esteves SC, Gosálvez J, Agarwal A. Specialized sperm function tests in varicocele and the future of andrology laboratory. Asian J Androl. 2016;18(2):205–12.
Agarwal A, Majzoub A, Esteves SC, Ko E, Ramasamy R, Zini A. Clinical utility of sperm DNA fragmentation testing: practice recommendations based on clinical scenarios. Transl Androl Urol. 2016;5(6):935–50.
Agarwal A, Sharma RK, Nallella KP, Thomas AJ, Alvarez JG, Sikka SC. Reactive oxygen species as an independent marker of male factor infertility. Fertil Steril. 2006;86(4):878–85.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001;345(19):1388–93.
Barratt CL, Mansell S, Beaton C, Tardif S, Oxenham SK. Diagnostic tools in male infertility—the question of sperm dysfunction. Asian J Androl. 2011;13(1):53.
Hwang K, Lipshultz LI, Lamb DJ. Use of diagnostic testing to detect infertility. Curr Urol Rep. 2011;12(1):68–76.
Su T-W, Erlinger A, Tseng D, Ozcan A. Compact and light-weight automated semen analysis platform using lensfree on-chip microscopy. Anal Chem. 2010;82(19):8307–12.
Segerink LI, Sprenkels AJ, ter Braak PM, Vermes I, van den Berg A. On-chip determination of spermatozoa concentration using electrical impedance measurements. Lab Chip. 2010;10(8):1018–24.
Gou H-L, Zhang X-B, Bao N, Xu J-J, Xia X-H, Chen H-Y. Label-free electrical discrimination of cells at normal, apoptotic and necrotic status with a microfluidic device. J Chromatogr A. 2011;1218(33):5725–9.
Huang X-Y, Sha J-H. Proteomics of spermatogenesis: from protein lists to understanding the regulation of male fertility and infertility. Asian J Androl. 2011;13(1):18.
Hansen M, Kurinczuk JJ, Bower C, Webb S. The risk of major birth defects after intracytoplasmic sperm injection and in vitro fertilization. N Engl J Med. 2002;346(10):725–30.
Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med. 2002;346(10):731–7.
Moll AC, Imhof SM, Cruysberg JR, Schouten-van Meeteren AY, Boers M, van Leeuwen FE. Incidence of retinoblastoma in children born after in-vitro fertilisation. Lancet. 2003;361(9354):309–10.
Ørstavik K, Eiklid K, Van Der Hagen C, Spetalen S, Kierulf K, Skjeldal O, et al. Another case of imprinting defect in a girl with Angelman syndrome who was conceived by intracytoplasmic sperm injection. Am J Hum Genet. 2003;72(1):218.
Agarwal A, Said TM. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update. 2003;9(4):331–45.
Agarwal A, Allamaneni SS. Sperm DNA damage assessment: a test whose time has come. Fertil Steril. 2005;84(4):850–3.
Erenpreiss J, Spano M, Erenpreisa J, Bungum M, Giwercman A. Sperm chromatin structure and male fertility: biological and clinical aspects. Asian J Androl. 2006;8(1):11–29.
Evenson D, Wixon R. Meta-analysis of sperm DNA fragmentation using the sperm chromatin structure assay. Reprod Biomed Online. 2006;12(4):466–72.
Borini A, Tarozzi N, Bizzaro D, Bonu M, Fava L, Flamigni C, et al. Sperm DNA fragmentation: paternal effect on early post-implantation embryo development in ART. Hum Reprod. 2006;21(11):2876–81.
Aitken RJ, De Iuliis GN. Origins and consequences of DNA damage in male germ cells. Reprod Biomed Online. 2007;14(6):727–33.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2006;22(1):174–9.
Ozmen B, Koutlaki N, Youssry M, Diedrich K, Al-Hasani S. DNA damage of human spermatozoa in assisted reproduction: origins, diagnosis, impacts and safety. Reprod Biomed Online. 2007;14(3):384–95.
Tarozzi N, Bizzaro D, Flamigni C, Borini A. Clinical relevance of sperm DNA damage in assisted reproduction. Reprod Biomed Online. 2007;14(6):746–57.
Lopes S, Jurisicova A, Sun J-G, Casper RF. Reactive oxygen species: potential cause for DNA fragmentation in human spermatozoa. Hum Reprod. 1998;13(4):896–900.
Sakkas D, Tomlinson M. Assessment of sperm competence. Semin Reprod Med. 2000;18(02):133–40.
De Jonge C. Paternal conributions to embryogenesis. Reprod Med Rev. 2000;8(3):203–14.
Corzett M, Mazrimas J, Balhorn R. Protamine 1: protamine 2 stoichiometry in the sperm of eutherian mammals. Mol Reprod Dev. 2002;61(4):519–27.
Lewis JD, Song Y, de Jong ME, Bagha SM, Ausió J. A walk though vertebrate and invertebrate protamines. Chromosoma. 2003;111(8):473–82.
Bellve AR, McKay DJ, Renaux BS, Dixon GH. Purification and characterization of mouse protamines, P1 and P2. Amino-acid sequence of P. Biochemistry. 1988;27(8):2890–7.
Steven Ward W, Coffey DS. DNA packaging and organization in mammalian spermatozoa: comparison with somatic cell. Biol Reprod. 1991;44(4):569–74.
Gatewood J, Cook G, Balhorn R, Bradbury E, Schmid C. Sequence-specific packaging of DNA in human sperm chromatin. Science. 1987;236(4804):962–4.
Bench GS, Friz AM, Corzett MH, Morse DH, Balhorn R. DNA and total protamine masses in individual sperm from fertile mammalian subjects. Cytometry. 1996;23(4):263–71.
Fuentes-Mascorro G, Serrano H, Rosado A. Sperm chromatin. Arch Androl. 2000;45(3):215–25.
Steven Ward W. Deoxyribonucleic acid loop domain tertiary structure in mammalian spermatozoa1. Biol Reprod. 1993;48(6):1193–201.
Solov’eva L, Svetlova M, Bodinski D, Zalensky AO. Nature of telomere dimers and chromosome looping in human spermatozoa. Chromosom Res. 2004;12(8):817–23.
Ward WS, Zalensky AO. The unique, complex organization of the transcriptionally silent sperm chromatin. Crit Rev Eukaryot Gene Expr. 1996;6:2–3.
Jager S. Sperm nuclear stability and male infertility. Arch Androl. 1990;25(3):253–9.
Balhorn R, Reed S, Tanphaichitr N. Aberrant protamine 1/protamine 2 ratios in sperm of infertile. Experientia. 1988;44(1):52–5.
Bench G, Corzett MH, De Yebra L, Oliva R, Balhorn R. Protein and DNA contents in sperm from an infertile human male possessing protamine defects that vary over tim. Mol Reprod Dev. 1998;50(3):345–53.
de Yebra Ls BJ-L, Vanrell JA, Corzett M, Balhorn R, Oliva R. Detection of P2 precursors in the sperm cells of infertile patients who have reduced protamine P2 levels 55Funded by grants from Dirección General de Investigación Cientifica y Técnica (DGICYT# PB92-0810) and Fondo de Investigaciones Sanitarias (FIS93/0670) to R.O. and by a fellowship from the Generalitat de Catalunya to L. de Y. Fertil Steril. 1998;69(4):755–9.
Nasr-Esfahani MH, Salehi M, Razavi S, Mardani M, Bahramian H, Steger K, et al. Effect of protamine-2 deficiency on ICSI outcome. Reprod Biomed Online. 2004;9(6):652–8.
Aoki VW, Liu L, Carrell DT. Identification and evaluation of a novel sperm protamine abnormality in a population of infertile males. Hum Reprod. 2005;20(5):1298–306.
García-Peiró A, Martínez-Heredia J, Oliver-Bonet M, Abad C, Amengual MJ, Navarro J, et al. Protamine 1 to protamine 2 ratio correlates with dynamic aspects of DNA fragmentation in human sperm. Fertil Steril. 2011;95(1):105–9.
Nanassy L, Liu L, Griffin J, T Carrell D. The clinical utility of the protamine 1/protamine 2 ratio in sperm. Protein Pept Lett. 2011;18(8):772–7.
Payne JF, Raburn DJ, Couchman GM, Price TM, Jamison MG, Walmer DK. Redefining the relationship between sperm deoxyribonucleic acid fragmentation as measured by the sperm chromatin structure assay and outcomes of assisted reproductive techniques. Fertil Steril. 2005;84(2):356–64.
Tomlinson M, Moffatt O, Manicardi GC, Bizzaro D, Afnan M, Sakkas D. Interrelationships between seminal parameters and sperm nuclear DNA damage before and after density gradient centrifugation: implications for assisted conception. Hum Reprod. 2001;16(10):2160–5.
Seli E, Gardner DK, Schoolcraft WB, Moffatt O, Sakkas D. Extent of nuclear DNA damage in ejaculated spermatozoa impacts on blastocyst development after in vitro fertilization. Fertil Steril. 2004;82(2):378–83.
Lewis SEM. Should sperm DNA fragmentation testing be included in the male infertility work-up? Reprod Biomed Online. 2015;31(2):134–7.
Agarwal A, Cho C-L, Esteves SC, Majzoub A. Current limitation and future perspective of sperm DNA fragmentation tests. Transl Androl Urol. 2017;6(Suppl 4):S549–S52.
Cozzubbo T, Neri QV, Rosenwaks Z, Palermo GD. To what extent can oocytes repair sperm DNA fragmentation? Fertil Steril. 2014;102(3):e61.
Meseguer M, Santiso R, Garrido N, García-Herrero S, Remohí J, Fernandez JL. Effect of sperm DNA fragmentation on pregnancy outcome depends on oocyte quality. Fertil Steril. 2011;95(1):124–8.
Ashwood-Smith M, Edwards R. Genetics and human conception: DNA repair by oocytes. MHR: Basic Sci Reprod Med. 1996;2(1):46–51.
Sergerie M, Laforest G, Bujan L, Bissonnette F, Bleau G. Sperm DNA fragmentation: threshold value in male fertility. Hum Reprod. 2005;20(12):3446–51.
Saleh RA, Agarwal A, Nada EA, El-Tonsy MH, Sharma RK, Meyer A, et al. Negative effects of increased sperm DNA damage in relation to seminal oxidative stress in men with idiopathic and male factor infertility. Fertil Steril. 2003;79:1597–605.
Bungum M, Humaidan P, Spano M, Jepson K, Bungum L, Giwercman A. The predictive value of sperm chromatin structure assay (SCSA) parameters for the outcome of intrauterine insemination, IVF and ICSI. Hum Reprod. 2004;19(6):1401–8.
Tomlinson MJ, Moffatt O, Manicardi GC, Bizzaro D, Afnan M, Andrology SD. Interrelationships between seminal parameters and sperm nuclear DNA damage before and after density gradient centrifugation: implications for assisted conceptio. Hum Reprod. 2001;16(10):2160–5.
McKelvey-Martin V, Melia N, Walsh I, Johnston S, Hughes C, Lewis S, et al. Two potential clinical applications of the alkaline single-cell gel electrophoresis assay:(1) human bladder washings and transitional cell carcinoma of the bladder; and (2) human sperm and male infertility. Mutat Res/Fundam Mol Mech Mutagen. 1997;375(2):93–104.
Esteves SC, Gosálvez J, López-Fernández C, Núñez-Calonge R, Caballero P, Agarwal A, et al. Diagnostic accuracy of sperm DNA degradation index (DDSi) as a potential noninvasive biomarker to identify men with varicocele-associated infertility. Int Urol Nephrol. 2015;47(9):1471–7.
Cho C-L, Esteves S, Agarwal A. Novel insights into the pathophysiology of varicocele and its association with reactive oxygen species and sperm DNA fragmentation. Asian J Androl. 2016;18(2):186–93.
Aitken RJ, Krausz C. Oxidative stress, DNA damage and the Y chromosome. Reproduction. 2001;122(4):497–506.
Hamada A, Esteves SC, Nizza M, Agarwal A. Unexplained male infertility: diagnosis and management. Int Braz J Urol. 2012;38(5):576–94.
Ahmad G, Moinard N, Esquerré-Lamare C, Mieusset R, Bujan L. Mild induced testicular and epididymal hyperthermia alters sperm chromatin integrity in men. Fertil Steril. 2012;97(3):546–53.
Tiseo B, Esteves S, Cocuzza M. Summary evidence on the effects of varicocele treatment to improve natural fertility in subfertile men. Asian J Androl. 2016;18(2):239–45.
Wang Y-J, Zhang R-Q, Lin Y-J, Zhang R-G, Zhang W-L. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online. 2012;25(3):307–14.
Zini A, Dohle G. Are varicoceles associated with increased deoxyribonucleic acid fragmentation? Fertil Steril. 2011;96(6):1283–7.
Agarwal A, Hamada A, Esteves SC. Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol. 2012;9:678.
Blumer CG, Restelli AE, Giudice PTD, Soler TB, Fraietta R, Nichi M, et al. Effect of varicocele on sperm function and semen oxidative stress. BJU Int. 2012;109(2):259–65.
Chen S-S, Huang William J, Chang Luke S, Wei Y-H. Attenuation of oxidative stress after varicocelectomy in subfertile patients with varicocele. J Urol. 2008;179(2):639–42.
Esteves S, Roque M, Agarwal A. Outcome of assisted reproductive technology in men with treated and untreated varicocele: systematic review and meta-analysis. Asian J Androl. 2016;18(2):254–8.
Kadioglu TC, Aliyev E, Celtik M. Microscopic varicocelectomy significantly decreases the sperm DNA fragmentation index in patients with infertility. Biomed Res Int. 2014;2014:695713.
Smit M, Romijn Johannes C, Wildhagen Mark F, Veldhoven Joke LM, Weber Robertus FA, Dohle Gert R. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2013;189(1):S146–S50.
Kumar M, Kumar K, Jain S, Hassan T, Dada R. Novel insights into the genetic and epigenetic paternal contribution to the human embryo. Clin (Sao Paulo, Brazil). 2013;68 Suppl 1(Suppl 1):5–14.
Lewis SEM, Aitken RJ. DNA damage to spermatozoa has impacts on fertilization and pregnancy. Cell Tissue Res. 2005;322(1):33–41.
Esteves SC. Novel concepts in male factor infertility: clinical and laboratory perspectives. J Assist Reprod Genet. 2016;33(10):1319–35.
Agarwal A, Cho C-L, Esteves SC. Should we evaluate and treat sperm DNA fragmentation? Curr Opin Obstet Gynecol. 2016;28(3):164–71.
Gosálvez J, Rodríguez-Predreira M, Mosquera A, López-Fernández C, Esteves S, Agarwal A, et al. Characterisation of a subpopulation of sperm with massive nuclear damage, as recognised with the sperm chromatin dispersion test. Andrologia. 2014;46(6):602–9.
Zini A. Are sperm chromatin and DNA defects relevant in the clinic? Syst Biol Reprod Med. 2011;57(1–2):78–85.
Buck Louis GM, Sundaram R, Schisterman EF, Sweeney A, Lynch CD, Kim S, et al. Semen quality and time to pregnancy: the longitudinal investigation of fertility and the environment study. Fertil Steril. 2014;101(2):453–62.
Spanò M, Bonde JP, Hjøllund HI, Kolstad HA, Cordelli E, Leter G. Sperm chromatin damage impairs human fertility‡‡the Danish first pregnancy planner study is a collaborative follow-up study on environmental and biological determinants of fertility. The project is coordinated by the Steno Institute of Public Health, Aarhus University and is undertaken in collaboration with the Department of Growth and Reproduction, National University Hospital, Copenhagen. The team includes Jens Peter E. Bonde, Niels Henrik I. Hjøllund, Tina Kold Jensen, Tine Brink Henriksen, Henrik A. Kolstad, Erik Ernst, Aleksander Giwercman, Niels Erik Skakkebæk, and Jørn Olsen. Fertil Steril. 2000;73(1):43–50.
Wiweko B, Utami P. Predictive value of sperm deoxyribonucleic acid (DNA) fragmentation index in male infertility. Basic Clin Androl. 2017;27(1):1.
Chenlo PH, Curi SM, Pugliese MN, Ariagno JI, Sardi-Segovia M, Furlan MJ, et al. Fragmentación del ADN espermático empleando el método de TUNEL. Actas Urol Esp. 2014;38(9):608–12.
Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, Erenpreiss J, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22(1):174–9.
Duran EH, Morshedi M, Taylor S, Oehninger S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort stud. Hum Reprod. 2002;17(12):3122–8.
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, et al. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012;27(10):2908–17.
Zhao J, Zhang Q, Wang Y, Li Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil Steril. 2014;102(4):998–1005.e8.
Carlini T, Paoli D, Pelloni M, Faja F, Dal Lago A, Lombardo F, et al. Sperm DNA fragmentation in Italian couples with recurrent pregnancy loss. Reprod Biomed Online. 2017;34(1):58–65.
Hammadeh M, Zeginiadov T, Rosenbaum P, Georg T, Schmidt W, Strehler E. Predictive value of sperm chromatin condensation (aniline blue staining) in the assessment of male fertility. Arch Androl. 2001;46(2):99–104.
Baker H, Liu D. Assessment of nuclear maturity. London: CRC Press; 1996.
Wong A, Chuan SS, Patton WC, Jacobson JD, Corselli J, Chan PJ. Addition of eosin to the aniline blue assay to enhance detection of immature sperm histones. Fertil Steril. 2008;90(5):1999–2002.
Foresta C, Zorzi M, Rossato M, Varotto A. Sperm nuclear instability and staining with aniline blue: abnormal persistance of histones in spermatozoa in infertile men. Int J Androl. 1992;15(4):330–7.
Kim H-S, Kang MJ, Kim SA, Oh SK, Kim H, Ku S-Y, et al. The utility of sperm DNA damage assay using toluidine blue and aniline blue staining in routine semen analysis. Clin Exp Reprod Med. 2013;40(1):23–8.
Kazerooni T, Asadi N, Jadid L, Kazerooni M, Ghanadi A, Ghaffarpasand F, et al. Evaluation of sperm’s chromatin quality with acridine orange test, chromomycin A3 and aniline blue staining in couples with unexplained recurrent abortion. J Assist Reprod Genet. 2009;26(11–12):591–6.
Kodama H, Yamaguchi R, Fukuda J, Kasai H, Tanaka T. Increased oxidative deoxyribonucleic acid damage in the spermatozoa of infertile male patients. Fertil Steril. 1997;68(3):519–24.
de Jager C, Aneck-Hahn NH, Bornman MS, Farias P, Leter G, Eleuteri P, et al. Sperm chromatin integrity in DDT-exposed young men living in a malaria area in the Limpopo Province, South Africa. Hum Reprod. 2009;24(10):2429–38.
Agarwal A, Sharma R, Ahmad G. Sperm chromatin assessment. In: Textbook of assisted reproductive techniques. 5th ed. Boca Raton: CRC Press; 2017. p. 65–87.
Marchesi DE, Biederman H, Ferrara S, Hershlag A, Feng HL. The effect of semen processing on sperm DNA integrity: comparison of two techniques using the novel toluidine blue assay. Eur J Obstet Gynecol Reprod Biol. 2010;151(2):176–80.
Erenpreiss J, Bars J, Lipatnikova V, Erenpreisa J, Zalkalns J. Comparative study of cytochemical tests for sperm chromatin integrity. J Androl. 2001;22(1):45–53.
Erenpreiss J, Jepson K, Giwercman A, Tsarev I, Erenpreisa J, Spano M. Toluidine blue cytometry test for sperm DNA conformation: comparison with the flow cytometric sperm chromatin structure and TUNEL assays. Hum Reprod. 2004;19(10):2277–82.
Tsarev I, Bungum M, Giwercman A, Erenpreisa J, Ebessen T, Ernst E, et al. Evaluation of male fertility potential by toluidine blue test for sperm chromatin structure assessment. Hum Reprod. 2009;24(7):1569–74.
Talebi AR, Moein MR, Tabibnejad N, Ghasemzadeh J. Effect of varicocele on chromatin condensation and DNA integrity of ejaculated spermatozoa using cytochemical tests. Andrologia. 2008;40(4):245–51.
Shamsi MB, Imam SN, Dada R. Sperm DNA integrity assays: diagnostic and prognostic challenges and implications in management of infertility. J Assist Reprod Genet. 2011;28(11):1073–85.
Hosseinifar H, Yazdanikhah S, Modarresi T, Totonchi M, Sadighi Gilani MA, Sabbaghian M. Correlation between sperm DNA fragmentation index and CMA3 positive spermatozoa in globozoospermic patients. Andrology. 2015;3(3):526–31.
Erenpreisa J, Erenpreiss J, Freivalds T, Slaidina M, Krampe R, Butikova J, et al. Toluidine blue test for sperm DNA integrity and elaboration of image cytometry algorithm. Cytometry A. 2003;52A(1):19–27.
Manicardi GC, Bianchi P, Pantano S, Azzoni P, Bizzaro D, Bianchi U, et al. Presence of endogenous nicks in DNA of ejaculated human spermatozoa and its relationship to chromomycin A3 accessibility. Biol Reprod. 1995;52(4):864–7.
Zini A, Fischer MA, Sharir S, Shayegan B, Phang D, Jarvi K. Prevalence of abnormal sperm DNA denaturation in fertile and infertile men. Urology. 2002;60(6):1069–72.
Esterhuizen A, Franken D, Lourens J, Prinsloo E, Van Rooyen L. Sperm chromatin packaging as an indicator of in-vitro fertilization rates. Hum Reprod. 2000;15(3):657–61.
Sakkas D, Urner F, Bizzaro D, Manicardi G, Bianchi P, Shoukir Y, et al. Sperm nuclear DNA damage and altered chromatin structure: effect on fertilization and embryo development. Hum Reprod. 1998;13(suppl_4):11–9.
Franco J Jr, Mauri A, Petersen C, Massaro F, Silva L, Felipe V, et al. Large nuclear vacuoles are indicative of abnormal chromatin packaging in human spermatozoa. Int J Androl. 2012;35(1):46–51.
Manochantr S, Chiamchanya C, Sobhon P. Relationship between chromatin condensation, DNA integrity and quality of ejaculated spermatozoa from infertile men. Andrologia. 2012;44(3):187–99.
Hosseinifar H, Yazdanikhah S, Modarresi T, Totonchi M, Sadighi Gilani M, Sabbaghian M. Correlation between sperm DNA fragmentation index and CMA 3 positive spermatozoa in globozoospermic patients. Andrology. 2015;3(3):526–31.
Mohammed E-EM, Mosad E, Zahran AM, Hameed DA, Taha EA, Mohamed MA. Acridine orange and flow cytometry: which is better to measure the effect of varicocele on sperm DNA integrity? Adv Urol. 2015;2015:814150.
Hoshi K, Katayose H, Yanagida K, Kimura Y, Sato A. The relationship between acridine orange fluorescence of sperm nuclei and the fertilizing ability of human sperm. Fertil Steril. 1996;66(4):634–9.
Gorczyca W, Gong J, Darzynkiewicz Z. Detection of DNA strand breaks in individual apoptotic cells by the in situ terminal deoxynucleotidyl transferase and nick translation assays. Cancer Res. 1993;53(8):1945–51.
Skowronek F, Casanova G, Alciaturi J, Capurro A, Cantu L, Montes J, et al. DNA sperm damage correlates with nuclear ultrastructural sperm defects in teratozoospermic men. Andrologia. 2012;44(1):59–65.
Zini A, Blumenfeld A, Libman J, Willis J. Beneficial effect of microsurgical varicocelectomy on human sperm DNA integrity. Hum Reprod. 2005;20(4):1018–21.
Zini A, Bielecki R, Phang D, Zenzes MT. Correlations between two markers of sperm DNA integrity, DNA denaturation and DNA fragmentation, in fertile and infertile men. Fertil Steril. 2001;75(4):674–7.
Evenson DP, Jost LK, Marshall D, Zinaman MJ, Clegg E, Purvis K, et al. Utility of the sperm chromatin structure assay as a diagnostic and prognostic tool in the human fertility clini. Hum Reprod. 1999;14(4):1039–49.
Gopalkrishnan K, Hurkadli K, Padwal V, Balaiah D. Use of acridine orange to evaluate chromatin integrity of human spermatozoa in different groups of infertile me. Andrologia. 1999;31(5):277–82.
Virant-Klun I, Tomazevic T, Meden-Vrtovec H. Sperm single-stranded DNA, detected by acridine orange staining, reduces fertilization and quality of ICSI-derived embryos. J Assist Reprod Genet. 2002;19(7):319–28.
Katayose H, Yanagida K, Hashimoto S, Yamada H, Sato A. Use of diamide–acridine orange fluorescence staining to detect aberrant protamination of human-ejaculated sperm nuclei. Fertil Steril. 2003;79:670–6.
Lazaros LA, Vartholomatos GA, Hatzi EG, Kaponis AI, Makrydimas GV, Kalantaridou SN, et al. Assessment of sperm chromatin condensation and ploidy status using flow cytometry correlates to fertilization, embryo quality and pregnancy following in vitro fertilization. J Assist Reprod Genet. 2011;28(10):885–91.
Spanò M, Kolstad AH, Larsen SB, Cordelli E, Leter G, Giwereman A, et al. The applicability of the flow cytometric sperm chromatin structure assay in epidemiological studie. Hum Reprod. 1998;13(9):2495–505.
Nijs M, De Jonge C, Cox A, Janssen M, Bosmans E, Ombelet W. Correlation between male age, WHO sperm parameters, DNA fragmentation, chromatin packaging and outcome in assisted reproduction technology. Andrologia. 2011;43(3):174–9.
Evenson DP, Kasperson K, Wixon RL. Analysis of sperm DNA fragmentation using flow cytometry and other techniques. Soc Reprod Fertil Suppl. 2007;65:93–113.
Evenson DP, Larson KL, Jost LK. Sperm chromatin structure assay: its clinical use for detecting sperm DNA fragmentation in male infertility and comparisons with other techniques. J Androl. 2002;23(1):25–43.
Castilla J, Zamora S, Gonzalvo M, Del Castillo JL, Roldan-Nofuentes J, Clavero A, et al. Sperm chromatin structure assay and classical semen parameters: systematic review. Reprod Biomed Online. 2010;20(1):114–24.
Giwercman A, Lindstedt L, Larsson M, Bungum M, Spano M, Levine RJ, et al. Sperm chromatin structure assay as an independent predictor of fertility in vivo: a case–control study. Int J Androl. 2010;33(1):e221–e7.
Bungum M, Spanò M, Humaidan P, Eleuteri P, Rescia M, Giwercman A. Sperm chromatin structure assay parameters measured after density gradient centrifugation are not predictive for the outcome of ART. Hum Reprod. 2008;23(1):4–10.
Miciński P, Pawlicki K, Wielgus E, Bochenek M, Tworkowska I. The sperm chromatin structure assay (SCSA) as prognostic factor in IVF/ICSI program. Reprod Biol. 2009;9(1):65–70.
Li Z, Wang L, Cai J, Huang H. Correlation of sperm DNA damage with IVF and ICSI outcomes: a systematic review and meta-analysis. J Assist Reprod Genet. 2006;23(9):367–76.
Lin M-H, Kuo-Kuang Lee R, Li S-H, Lu C-H, Sun F-J, Hwu Y-M. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90(2):352–9.
Collins JA, Barnhart KT, Schlegel PN. Do sperm DNA integrity tests predict pregnancy with in vitro fertilization? Fertil Steril. 2008;89(4):823–31.
Lewis SEM, Agbaje I, Alvarez J. Sperm DNA tests as useful adjuncts to semen analysis. Syst Biol Reprod Med. 2008;54(3):111–25.
Henkel R, Hoogendijk CF, Bouic PJD, Kruger TF. TUNEL assay and SCSA determine different aspects of sperm DNA damage. Andrologia. 2010;42(5):305–13.
Shen H-M, Ong C-N. Detection of oxidative DNA damage in human sperm and its association with sperm function and male infertility. Free Radic Biol Med. 2000;28(4):529–36.
Aitken RJ, De Iuliis GN, Finnie JM, Hedges A, McLachlan RI. Analysis of the relationships between oxidative stress, DNA damage and sperm vitality in a patient population: development of diagnostic criteria. Hum Reprod. 2010;25(10):2415–26.
De Iuliis GN, Thomson LK, Mitchell LA, Finnie JM, Koppers AJ, Hedges A, et al. DNA damage in human spermatozoa is highly correlated with the efficiency of chromatin remodeling and the formation of 8-hydroxy-2′-deoxyguanosine, a marker of oxidative Stress1. Biol Reprod. 2009;81(3):517–24.
Ishikawa T, Fujioka H, Ishimura T, Takenaka A, Fujisawa M. Increased testicular 8-hydroxy-2′-deoxyguanosine in patients with varicocele. BJU Int. 2007;100(4):863–6.
Loft S, Kold-Jensen T, Hjollund NH, Giwercman A, Gyllemborg J, Ernst E, et al. Oxidative DNA damage in human sperm influences time to pregnancy. Hum Reprod. 2003;18(6):1265–72.
Agarwal A, Varghese AC, Sharma RK. Markers of oxidative stress and sperm chromatin integrity. In: Park-Sarge O-K, Curry TE, editors. Molecular endocrinology: methods and protocols. Totowa: Humana Press; 2009. p. 377–402.
Singh NP, McCoy MT, Tice RR, Schneider EL. A simple technique for quantitation of low levels of DNA damage in individual cells. Exp Cell Res. 1988;175(1):184–91.
Singh NP, Danner DB, Tice RR, McCoy MT, Collins GD, Schneider EL. Abundant alkali-sensitive sites in DNA of human and mouse sperm. Exp Cell Res. 1989;184(2):461–70.
Cortés-Gutiérrez EI, Fernández JL, Dávila-Rodríguez MI, López-Fernández C, Gosálvez J. Two-tailed comet assay (2T-comet): simultaneous detection of DNA single and double strand breaks. In: Pellicciari C, Biggiogera M, editors. Histochemistry of single molecules: methods and protocols. New York: Springer; 2017. p. 285–93.
Hellman B, Vaghef H, Boström B. The concepts of tail moment and tail inertia in the single cell gel electrophoresis assay. Mutat Res/DNA Repair. 1995;336(2):123–31.
Benchaib M, Braun V, Lornage J, Hadj S, Salle B, Lejeune H, et al. Sperm DNA fragmentation decreases the pregnancy rate in an assisted reproductive techniqu. Hum Reprod. 2003;18(5):1023–8.
Enciso M, Sarasa J, Agarwal A, Fernández JL, Gosálvez J. A two-tailed comet assay for assessing DNA damage in spermatozoa. Reprod Biomed Online. 2009;18(5):609–16.
Duty SM, Singh NP, Ryan L, Chen Z, Lewis C, Huang T, et al. Andrology. Reliability of the comet assay in cryopreserved human. Hum Reprod. 2002;17(5):1274–80.
Morris ID, Ilott S, Dixon L, Brison DR. Andrology. The spectrum of DNA damage in human sperm assessed by single cell gel electrophoresis (comet assay) and its relationship to fertilization and embryo developmen. Hum Reprod. 2002;17(4):990–8.
Tomsu M, Sharma V, Miller D. Embryo quality and IVF treatment outcomes may correlate with different sperm comet assay parameter. Hum Reprod. 2002;17(7):1856–62.
Lewis SEM, Agbaje IM. Using the alkaline comet assay in prognostic tests for male infertility and assisted reproductive technology outcomes. Mutagenesis. 2008;23(3):163–70.
Shamsi M, Venkatesh S, Tanwar M, Singh G, Mukherjee S, Malhotra N, et al. Comet assay : a prognostic tool for DNA integrity assessment in infertile men opting for assisted reproduction. Indian J Med Res. 2010;131(5):675–81.
Simon L, Lutton D, McManus J, Lewis SEM. Sperm DNA damage measured by the alkaline comet assay as an independent predictor of male infertility and in vitro fertilization success. Fertil Steril. 2011;95(2):652–7.
Lewis SEM, Simon L. Clinical implications of sperm DNA damage. Hum Fertil. 2010;13(4):201–7.
Abu-Hassan D, Koester F, Shoepper B, Schultze-Mosgau A, Asimakopoulos B, Diedrich K, et al. Comet assay of cumulus cells and spermatozoa DNA status, and the relationship to oocyte fertilization and embryo quality following ICSI. Reprod Biomed Online. 2006;12(4):447–52.
Fernández JL, Muriel L, Rivero MT, Goyanes V, Vazquez R, Alvarez JG. The sperm chromatin dispersion test: a simple method for the determination of sperm DNA fragmentation. J Androl. 2003;24(1):59–66.
Ankem MK, Mayer E, Ward WS, Cummings KB, Barone JG. Novel assay for determining DNA organization in human spermatozoa: implications for male factor infertility. Urology. 2002;59(4):575–8.
Muriel L, Meseguer M, Fernández JL, Alvarez J, Remohí J, Pellicer A, et al. Value of the sperm chromatin dispersion test in predicting pregnancy outcome in intrauterine insemination: a blind prospective study∗. Hum Reprod. 2006;21(3):738–44.
Muriel L, Garrido N, Fernández JL, Remohí J, Pellicer A, de los Santos MJ, et al. Value of the sperm deoxyribonucleic acid fragmentation level, as measured by the sperm chromatin dispersion test, in the outcome of in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril. 2006;85(2):371–83.
Muriel L, Goyanes V, Segrelles E, Gosálvez J, Alvarez JG, Fernández JL. Increased aneuploidy rate in sperm with fragmented DNA as determined by the sperm chromatin dispersion (SCD) test and FISH analysis. J Androl. 2007;28(1):38–49.
Fernández JL, Muriel L, Goyanes V, Segrelles E, Gosálvez J, Enciso M, et al. Halosperm® is an easy, available, and cost-effective alternative for determining sperm DNA fragmentation. Fertil Steril. 2005;84(4):860.
Feijó CM, Esteves SC. Diagnostic accuracy of sperm chromatin dispersion test to evaluate sperm deoxyribonucleic acid damage in men with unexplained infertility. Fertil Steril. 2014;101(1):58–63.e3.
Zhang L-h, Qiu Y, Wang K-h, Wang Q, Tao G, L-g W. Measurement of sperm DNA fragmentation using bright-field microscopy: comparison between sperm chromatin dispersion test and terminal uridine nick-end labeling assay. Fertil Steril. 2010;94(3):1027–32.
Meseguer M, Santiso R, Garrido N, Gil-Salom M, Remohí J, Fernandez JL. Sperm DNA fragmentation levels in testicular sperm samples from azoospermic males as assessed by the sperm chromatin dispersion (SCD) test. Fertil Steril. 2009;92(5):1638–45.
Balasuriya A, Speyer B, Serhal P, Doshi A, Harper JC. Sperm chromatin dispersion test in the assessment of DNA fragmentation and aneuploidy in human spermatozoa. Reprod Biomed Online. 2011;22(5):428–36.
Santiso R, Tamayo M, Gosálvez J, Meseguer M, Garrido N, Fernández JL. Simultaneous determination in situ of DNA fragmentation and 8-oxoguanine in human sperm. Fertil Steril. 2010;93(1):314–8.
Fernández JL, Cajigal D, López-Fernández C, Gosálvez J. Assessing sperm DNA fragmentation with the sperm chromatin dispersion test. In: Didenko VV, editor. DNA damage detection in situ, ex vivo, and in vivo: methods and protocols. Totowa: Humana Press; 2011. p. 291–301.
Velez de la Calle JF, Muller A, Walschaerts M, Clavere JL, Jimenez C, Wittemer C, et al. Sperm deoxyribonucleic acid fragmentation as assessed by the sperm chromatin dispersion test in assisted reproductive technology programs: results of a large prospective multicenter study. Fertil Steril. 2008;90(5):1792–9.
Sharma R, Ahmad G, Esteves SC, Agarwal A. Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay using bench top flow cytometer for evaluation of sperm DNA fragmentation in fertility laboratories: protocol, reference values, and quality control. J Assist Reprod Genet. 2016;33(2):291–300.
Gupta S, Sharma R, Agarwal A. Inter-and intra-laboratory standardization of TUNEL assay for assessment of sperm DNA fragmentation. Curr Protoc Toxicol. 2017;74(1):16.1.1-.1.22.
Agarwal A, Gupta S, Sharma R. Measurement of DNA fragmentation in spermatozoa by TUNEL assay using bench top flow cytometer. In: Andrological evaluation of male infertility. New York: Springer; 2016. p. 181–203.
Sharma R, Gupta S, Henkel R, Agarwal A. Critical evaluation of two models of flow cytometers for the assessment of sperm DNA fragmentation: an appeal for performance verification. Asian J Androl. 2019;21(5):438–44.
Mitchell LA, De Iuliis GN, Aitken RJ. The TUNEL assay consistently underestimates DNA damage in human spermatozoa and is influenced by DNA compaction and cell vitality: development of an improved methodology. Int J Androl. 2011;34(1):2–13.
Carrell DT, Liu L, Peterson C, Jones K, Hatasaka H, Erickson L, et al. Sperm DNA fragmentation is increased in couples with unexplained recurrent pregnancy loss. Arch Androl. 2003;49(1):49–55.
Aitken RJ. The amoroso lecture the human spermatozoon–a cell in crisis? J Reprod Fertil. 1999;115(1):1–7.
Sun J-G, Jurisicova A, Casper RF. Detection of deoxyribonucleic acid fragmentation in human sperm: correlation with fertilization in vitro. Biol Reprod. 1997;56(3):602–7.
Sharma RK, Sabanegh E, Mahfouz R, Gupta S, Thiyagarajan A, Agarwal A. TUNEL as a test for sperm DNA damage in the evaluation of male infertility. Urology. 2010;76(6):1380–6.
Cui Z-L, Zheng D-Z, Liu Y-H, Chen L-Y, Lin D-H, Feng-Hua L. Diagnostic accuracies of the TUNEL, SCD, and comet based sperm DNA fragmentation assays for male infertility: a meta-analysis study. Clin Lab. 2015;61(5–6):525–35.
Muratori M, Tamburrino L, Tocci V, Costantino A, Marchiani S, Giachini C, et al. Small variations in crucial steps of TUNEL assay coupled to flow cytometry greatly affect measures of sperm DNA fragmentation. J Androl. 2010;31(4):336–45.
Ribeiro S, Sharma R, Gupta S, Cakar Z, De Geyter C, Agarwal A. Inter- and intra-laboratory standardization of TUNEL assay for assessment of sperm DNA fragmentation. Andrology. 2017;5(3):477–85.
Esteves SC, Agarwal A, Cho C-L, Majzoub A. A strengths-weaknesses-opportunities-threats (SWOT) analysis on the clinical utility of sperm DNA fragmentation testing in specific male infertility scenarios. Transl Androl Urol. 2017;6(Suppl 4):S734–S60.
Esteves SC, Majzoub A, Agarwal A. The importance of quality control and quality assurance in SDF testing. Transl Androl Urol. 2017;6(Suppl 4):S604–S6.
Esteves SC, Sharma RK, Gosálvez J, Agarwal A. A translational medicine appraisal of specialized andrology testing in unexplained male infertility. Int Urol Nephrol. 2014;46(6):1037–52.
Rilcheva VS, Ayvazova NP, Ilieva LO, Ivanova SP, Konova EI. Sperm DNA integrity test and assisted reproductive technology (art) outcome. J Biomed Clin Res. 2016;9(1):21–9.
Esteves SC, Agarwal A, Majzoub A. The complex nature of the sperm DNA damage process. Transl Androl Urol. 2017;6(Suppl 4):S557–S9.
Agarwal A, Cho C-L, Esteves SC, Majzoub A. Implication of sperm processing during assisted reproduction on sperm DNA integrity. Transl Androl Urol. 2017;6(Suppl 4):S583–S5.
Zini A, Nam RK, Mak V, Phang D, Jarvi K. Influence of initial semen quality on the integrity of human sperm DNA following semen processing. Fertil Steril. 2000;74(4):824–7.
Niu Z-H, Shi H-J, Zhang H-Q, Zhang A-J, Sun Y-J, Feng Y. Sperm chromatin structure assay results after swim-up are related only to embryo quality but not to fertilization and pregnancy rates following IVF. Asian J Androl. 2011;13(6):862.
Zini A, Finelli A, Phang D, Jarvi K. Influence of semen processing technique on human sperm DNA integrity. Urology. 2000;56(6):1081–4.
Agarwal A, Cho C-L, Majzoub A, Esteves SC. The Society for Translational Medicine: clinical practice guidelines for sperm DNA fragmentation testing in male infertility. Transl Androl Urol. 2017;6(Suppl 4):S720–S33.
Esteves SC, Majzoub A, Agarwal A. Further evidence supports the clinical utility of sperm DNA fragmentation testing in male infertility workup and assisted reproductive technology. Transl Androl Urol. 2017;6(Suppl 4):S428–S36.
Werthman P, Wixon R, Kasperson K, Evenson DP. Significant decrease in sperm deoxyribonucleic acid fragmentation after varicocelectomy. Fertil Steril. 2008;90(5):1800–4.
Abdelbaki SA, Sabry JH, Al-Adl AM, Sabry HH. The impact of coexisting sperm DNA fragmentation and seminal oxidative stress on the outcome of varicocelectomy in infertile patients: a prospective controlled study. Arab J Urol. 2017;15(2):131–9.
Telli O, Sarici H, Kabar M, Ozgur B, Resorlu B, Bozkurt S. Does varicocelectomy affect DNA fragmentation in infertile patients? Indian J Urol. 2015;31(2):116–9.
Park Y-S, Lee S-H, Choi HW, Lee HS, Lee JS, Seo JT. Abnormal human sperm parameters contribute to sperm DNA fragmentation in men with varicocele. World J Mens Health. 2018;36(3):239–47.
Agarwal A, Cho C-L, Majzoub A, Esteves SC. Frontiers in clinical andrology. Transl Androl Urol. 2017;6(Suppl 4):S343–S5.
Vandekerckhove FWRC, De Croo I, Gerris J, Vanden Abbeel E, De Sutter P. Sperm chromatin dispersion test before sperm preparation is predictive of clinical pregnancy in cases of unexplained infertility treated with intrauterine insemination and induction with clomiphene citrate. Front Med. 2016;3:63.
Das M, Al-Hathal N, San-Gabriel M, Phillips S, Kadoch I-J, Bissonnette F, et al. High prevalence of isolated sperm DNA damage in infertile men with advanced paternal age. J Assist Reprod Genet. 2013;30(6):843–8.
Giwercman A, Richthoff J, Hjøllund H, Bonde JP, Jepson K, Frohm B, et al. Correlation between sperm motility and sperm chromatin structure assay parameters. Fertil Steril. 2003;80(6):1404–12.
Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum Reprod. 2008;23(12):2663–8.
Cissen M, van Wely M, Scholten I, Mansell S, de Bruin JP, Mol BW, et al. Measuring sperm DNA fragmentation and clinical outcomes of medically assisted reproduction: a systematic review and meta-analysis. PLoS One. 2016;11(11):e0165125.
Simon L, Zini A, Dyachenko A, Ciampi A, Carrell D. A systematic review and meta-analysis to determine the effect of sperm DNA damage on <i>in vitro</i> fertilization and intracytoplasmic sperm injection outcome. Asian J Androl. 2017;19(1):80–90.
Agarwal A, Cho C-L, Majzoub A, Esteves SC. The role of female factors in the management of sperm DNA fragmentation. Transl Androl Urol. 2017;6(Suppl 4):S488–S90.
Jin J, Pan C, Fei Q, Ni W, Yang X, Zhang L, et al. Effect of sperm DNA fragmentation on the clinical outcomes for in vitro fertilization and intracytoplasmic sperm injection in women with different ovarian reserves. Fertil Steril. 2015;103(4):910–6.
Majzoub A, Agarwal A. Systematic review of antioxidant types and doses in male infertility: benefits on semen parameters, advanced sperm function, assisted reproduction and live-birth rate. Arab J Urol. 2018;16(1):113–24.
Stenqvist A, Oleszczuk K, Leijonhufvud I, Giwercman A. Impact of antioxidant treatment on DNA fragmentation index: a double-blind placebo-controlled randomized trial. Andrology. 2018;6(6):811–6.
Greco E, Romano S, Iacobelli M, Ferrero S, Baroni E, Minasi MG, et al. ICSI in cases of sperm DNA damage: beneficial effect of oral antioxidant treatment. Hum Reprod. 2005;20(9):2590–4.
Majzoub A, Agarwal A, Esteves SC. Antioxidants for elevated sperm DNA fragmentation: a mini review. Transl Androl Urol. 2017;6(Suppl 4):S649–S53.
Sharma R, Agarwal A. Laboratory evaluation of sperm chromatin: TUNEL assay. In: Sperm chromatin. New York: Springer; 2011. p. 201–15.
Sharma R, Masaki J, Agarwal A. Sperm DNA fragmentation analysis using the TUNEL assay. In: Carrell DT, Aston KI, editors. Spermatogenesis: methods and protocols. Totowa: Humana Press; 2013. p. 121–36.
Ribeiro SC, Muratori M, De Geyter M, De Geyter C. TUNEL labeling with BrdUTP/anti-BrdUTP greatly underestimates the level of sperm DNA fragmentation in semen evaluation. PLoS One. 2017;12(8):e0181802.
Muratori M, Tamburrino L, Marchiani S, Cambi M, Olivito B, Azzari C, et al. Investigation on the origin of sperm DNA fragmentation: role of apoptosis, immaturity and oxidative Stres. Mol Med. 2015;21(1):109–22.
Lewis SEM, John Aitken R, Conner SJ, Iuliis GD, Evenson DP, Henkel R, et al. The impact of sperm DNA damage in assisted conception and beyond: recent advances in diagnosis and treatment. Reprod Biomed Online. 2013;27(4):325–37.
Cho C-L, Agarwal A, Majzoub A, Esteves SC. The debate on sperm DNA fragmentation test goes on. Transl Androl Urol. 2017;6(Suppl 4):S702–S3.
Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile male: a committee opinion. Fertil Steril. 2015;103(3):e18–25.
Majzoub A, Agarwal A, Cho C-L, Esteves SC. Sperm DNA fragmentation testing: a cross sectional survey on current practices of fertility specialists. Transl Androl Urol. 2017;6(Suppl 4):S710–S9.
Cho C-L, Agarwal A, Majzoub A, Esteves SC. Future direction in sperm DNA fragmentation testing. Transl Androl Urol. 2017;6(Suppl 4):S525–S6.
Evenson DP. The Sperm Chromatin Structure Assay (SCSA®) and other sperm DNA fragmentation tests for evaluation of sperm nuclear DNA integrity as related to fertility. Anim Reprod Sci. 2016;169:56–75.
Fernández JL, Muriel L, Goyanes V, et al. Simple determination of human sperm DNA fragmentation with an improved sperm chromatin dispersion test. Fertil Steril. 2005;84(4):833–42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sharma, R., Martinez, M.P., Agarwal, A. (2020). Sperm Chromatin Integrity Tests and Indications. In: Parekattil, S., Esteves, S., Agarwal, A. (eds) Male Infertility. Springer, Cham. https://doi.org/10.1007/978-3-030-32300-4_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-32300-4_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32299-1
Online ISBN: 978-3-030-32300-4
eBook Packages: MedicineMedicine (R0)