Abstract
The diagnosis of male infertility implies an impairment of the male reproductive potential. Unfortunately, there is no gold standard for the assessment of the male reproductive potential. The diagnostic accuracy of semen analysis is compromised by substantial overlap between the distributions of semen parameters in empirically fertile and infertile men. Novel assays, including seminal reactive oxygen species levels, sperm DNA fragmentation, and sperm epigenetic testing, may prove to be of greater clinical utility for identifying men with below-average reproductive potential. Efforts to identify and treat modifiable risk factors should ideally be targeted toward these individuals. Although economic analyses have demonstrated that pathology-directed treatment for male infertility is often more cost-effective than immediate use of assisted reproductive technology, there is a declining trend in surgical treatment of male infertility.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Male infertility
- Incidence and prevalence of infertility
- Infertility in the developing world
- Epidemiology of infertility
- Reactive oxygen species
- Sperm DNA fragmentation
- Novel diagnostic assays
- Semen studies
-
There is a 15% lifetime incidence of infertility among couples in Western countries; only 3%–5% of couples are sterile.
-
If the timing of sexual intercourse relative to ovulation is deliberately controlled, then the monthly probability of pregnancy may approach 40%; however, the human average for monthly fecundity is 20%.
-
The absence of a gold-standard test for male infertility is a fundamental problem, preventing an accurate understanding of its epidemiology and of the predictive value of tests employed for its diagnosis.
-
Sperm concentration correlates with the probability of conception up to a density of 40 million/mL, but there is no additional likelihood of pregnancy at higher sperm densities.
-
Purported declines in semen quality during the twentieth century may be an artifact of bias from geographical differences in sperm counts.
-
Economic analyses suggest that pathology-directed treatment of male infertility is generally more cost-effective than proceeding directly to ART.
1 Introduction
This chapter primarily aims to discuss the epidemiologic relationship between infertility and male reproductive potential. It will focus in detail on the accuracy and diagnostic value of semen studies. Controversial reports of declining sperm counts during the twenty-first century will also be addressed, followed by a review of trends in health-care resource utilization and cost analysis models pertinent to the management of male infertility.
Antioxidant therapy for male infertility has an epidemiologic basis in the understanding that reactive oxygen species (ROS) contribute to sperm damage and are present in higher levels in the semen of infertile men [1,2,3,4]. However, given the increasing availability and use of assisted reproductive technology (ART), it may be surprising to encounter an epidemiologic approach to male infertility in the modern era [5]. The relative ease of surgical sperm retrieval in cases of azoospermia and severe oligozoospermia has seemingly rendered comprehensive evaluation and treatment of infertile men less relevant. Even though such an evaluation may identify one or more modifiable risk factors for infertility (as well as potentially serious underlying or coexisting illnesses and genetic abnormalities), the outcome of pathology-directed treatment may take longer to realize.
However, risk and uncertainty are also attendant to the use of ART. Cost-effectiveness studies have demonstrated that a straight-to-ART approach is less efficient than pathology-directed treatment in many situations involving male infertility. Therefore, renewed emphasis is being placed on the paradigm of intervention to correct modifiable male risk factors [6].
2 Epidemiology of Infertility
It is important to distinguish reproductive potential, or capacity, from actual reproductive performance, or outcomes [7, 8]. Infertility is ultimately defined by a reproductive outcome (i.e., childlessness), but “male infertility” is a diagnosis of relative impairment in male reproductive potential. Before discussing male infertility in more detail, we will review the epidemiology of infertility in general.
2.1 Incidence and Prevalence of Infertility in Developed Countries
Childlessness within long-standing marriage has been observed to occur in roughly 10% of couples in developed countries [9]. This figure represents a measure of reproductive outcomes, but it does not exclude couples who remain voluntarily childless or do not have regular intercourse during the fertile phase of the female’s menstrual cycle.
The World Health Organization (WHO) has defined infertility by “the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse,” which captures the concept of impaired reproductive potential [10]. By this criterion, the lifetime incidence of unwanted infertility is approximately 15% among couples in Western countries [11]. Two-thirds of these cases are primary, that is, in couples who have never previously conceived, while one-third are secondary [9].
It is not uncommon to see infertility defined by other durations of time, such as 2 or 5 years. Also, while the outcome of interest in the WHO’s definition is conception, others prefer to regard infertility as the absence of live birth [7, 8]. This distinction is important, because 10–25% of recognized pregnancies end in miscarriage [12].
The annual prevalence of infertility among married US women aged 15–44 years was 6.7% in 2015, down from 11.2% in 1965, 8.5% in 1982, to 7.4% in 2002 [13, 14]. This trend may reflect improvements in reproductive potential, perhaps through better awareness of ideal timing for intercourse, which may be attributable to at-home ovulation tests. However, other factors could also be involved, such as more couples utilizing infertility treatment prior to reaching the 12-month threshold necessary for inclusion in the rate’s numerator. Declining marriage rates among lower socioeconomic classes may also be disproportionately removing women at greater risk of infertility from the denominator [13].
A popular misconception is that infertility is synonymous with, or virtually approximates, sterility [8]. In fact, only 3%–5% of couples are sterile [9, 15].
2.2 Infertility in the Developing World
In 2002, the WHO estimated that 16%–30% of married women in developing countries were experiencing infertility of at least 5 years duration, with the vast majority being secondary [16]. A more recent study, focused on child-seeking women, lowered these estimates to 9%–20% (Table 2.1) [17]. Interestingly, this study found little difference in the prevalence of infertility between high-income countries and low- or middle-income countries of certain regions. Sexually transmitted infections and postpartum complications have been identified as key factors contributing to secondary infertility in the developing world [18].
The rate of childlessness in developing countries among sexually experienced women who are beyond childbearing age is approximately 3% [16]. This figure is comparable to the estimated prevalence of sterility in Western societies.
High cost represents an important barrier to the accessibility of most infertility treatment, and specifically ART, in the developing world [18]. Therefore, further identification of avoidable gonadotoxins, as well as clarification of the role of less expensive therapies, would be especially welcome there [19].
2.3 Reproduction—a Matter of Chance: The Natural History of Infertility
Reproduction has been described as “a matter of chance depending on the subtle balance between success or failure of complex, mostly poorly understood, sequential processes that may lead to a pregnancy and eventually to the birth of a healthy child” [15]. Failure of a couple to reproduce is a unique medical problem in that it occurs between rather than within individuals [7].
Individuals’ reproductive potential is a continuous, as opposed to dichotomous, variable. It reflects the influence of many factors, including age. Reproductive potential declines in members of both sexes over 30 years old, but female age has the most profound effect on the likelihood of conception [20, 21].
Since a couple’s reproductive capacity is the composite of its individual members’ reproductive potentials, it, too, is a continuous variable. Impairment of a male’s reproductive potential may be compensated for—or compounded—by that of his female partner and vice versa. This concept is illustrated by the fact that artificial insemination with donor semen is more often successful in partners of azoospermic men than in partners of men with oligozoospermia [22].
Couples’ monthly, or cycle-wise, likelihood of conception falls along a spectrum of probability. This is referred to as fecundability or monthly fecundity rate (MFR). The average MFR for human couples having regular, unprotected intercourse is approximately 20%, and the overall distribution of human MFRs is believed to range from 0% to 60% [23, 24]. The variable likelihood of pregnancy at 6, 12, 24, and 60 months has been calculated for couples with different MFRs (Table 2.2). Based on these values, a hypothetical model has been constructed of the proportion of couples with varying degrees of reproductive potential (MFR) among residual nonpregnant couples after specified durations of infertility (Table 2.3) [25].
Table 2.2 demonstrates that couples with average fecundability have a better than 90% chance of conceiving within 12 months. However, 30% of couples who do not conceive within 12 months are still of average reproductive potential (see Table 2.3). Population-based studies have found that couples who are infertile after 12 months retain a roughly 50% likelihood of achieving unassisted pregnancy by 24 months [26]. Thereafter, the odds of conception decline precipitously, as illustrated in Fig. 2.1. The proportion of couples that are sterile increases with the duration of infertility.
Cumulative probability of conception in couples having unprotected intercourse. (Reprinted from the Velde et al. [15]. With permission from Elsevier)
An obvious but nevertheless critically important factor in determining reproductive potential is the timing of sexual intercourse relative to ovulation (Fig. 2.2) [27]. In a cohort of 340 German couples who received natural family planning education intended to improve their timing of intercourse, the monthly probability of achieving pregnancy averaged 38%, markedly higher than the average human MFR of 20% [28].
Probability of clinical pregnancy after intercourse on a particular day relative to ovulation (day 0) for couples at specified percentiles of the population distribution of reproductive potential. (Adapted from Dunson et al. [27]. With permission from Oxford University Press)
3 Diagnostic Accuracy and Utility of Semen Studies
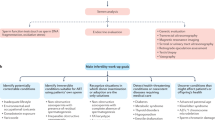
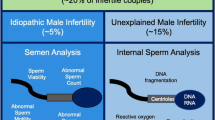
Male infertility is diagnosed in approximately 50% of couples presenting for evaluation of infertility [11]. Basic semen analysis remains the most widely utilized laboratory study for this purpose. However, the limitations of semen analysis should be clearly understood.
The parameters usually assessed by semen analysis include ejaculate volume, sperm concentration (density), sperm motility, and sperm morphology. From the ejaculate volume, concentration, and percentage of motile sperm, the total sperm count and total motile count are calculated. Semen pH, viscosity, white blood cell concentration, and the degree of sperm agglutination may also be reported [29].
More specialized studies that are undertaken on a case-by-case basis include evaluation of sperm viability, antisperm antibodies, and functional assays, such as assessment of sperm–cervical mucus interaction, capacitation, and sperm penetration of a zona-free hamster oocyte [30]. Relatively recent developments have included the introduction of tests for seminal ROS levels and sperm DNA fragmentation [31, 32].
Preliminary studies have also suggested that sperm epigenetics may have a future role in the evaluation of male infertility. Gene H19 is a common target for study and was associated with infertile men by a factor of 9.9 in one meta-analysis [33]. Epigenetic research remains exploratory and is limited by the wide number of possible gene targets for study.
3.1 Relationship Between Semen Parameters and Male Infertility
Semen analysis definitively confirms male factor infertility in men who are found to have semen characteristics at the negative extremes, that is, azoospermia, nonmotile sperm, or the severest cases of teratozoospermia. However, only a small fraction of men who present for evaluation of infertility have such findings [11]. The present section explores the relationship between male infertility and the entire spectrum of semen quality.
Since 1980, the WHO has published reference values for human semen parameters. These values have been changed periodically (Table 2.4) [34]. As of 2010, they represent the fifth percentile in the distribution of semen parameters from a population of men with proven fertility [35]. They provide no information regarding the distribution of semen parameters in men who are infertile.
Although the WHO criteria are commonly used as thresholds for designation of male infertility, the diagnostic picture in a clinical setting is considerably more complex. This scenario is because of substantial overlap between the distributions of semen characteristics in empirically fertile men and those with infertility whose female partners have had a normal fertility evaluation (Fig. 2.3).
Frequency histograms depicting the percentage of men from fertile (shaded bars) and infertile (unshaded bars) couples with sperm concentration (a) sperm motility (b) and sperm morphology (c) within specified ranges. Data were obtained from 696 fertile men and 765 men from infertile couples whose female partners had an unrevealing fertility evaluation. (Reprinted from Guzick et al. [36]. Copyright 2001, with permission from Massachusetts Medical Society. All rights reserved)
Basic performance measures of a test such as semen analysis include calculation of its sensitivity and specificity. These concepts are illustrated in Tables 2.5 and 2.6. If a sperm concentration below 15 million/mL is the criterion for a “positive” result (i.e., diagnosis of male infertility), then men who are actually fertile will be correctly classified 95% of the time. In other words, the threshold of 15 million/mL has a specificity of 95%. However, 85% of infertile men also have sperm concentrations above 15 million/mL; thus, the sensitivity of the test at this threshold is only 15% [36]. Many men with impaired reproductive potential will not be recognized as such.
If we assume that 50% of couples presenting for an evaluation of infertility have a contributing male factor, then the predictive value of a positive result (i.e., its likelihood of being correct) would be 75%. The predictive value of a negative, or normal, result would be only 53% (see Table 2.6).
Of course, diagnostic thresholds can be changed. If they are increased, sensitivity improves, but there is a reciprocal decline in specificity, and vice versa. One way to assess the diagnostic accuracy of a test across all thresholds is by a receiver operating characteristic (ROC) curve [28, 34]. ROC curves are constructed by plotting the probability of detecting true positives (sensitivity) against that of detecting false positives (1 − specificity) at each threshold.
The total area under the ROC curve (AUC) for a particular test represents its overall discriminatory capability. A perfect test has an AUC of 1.0, while a test is useless if the likelihood of a true positive matches that of a false positive at every threshold, resulting in the no-discrimination line from (0, 0) to (1, 1) and an AUC of 0.5. The amount by which a test’s ROC curve diverges from this line—and by extension, to which its AUC exceeds 0.5—is the degree to which it is diagnostically helpful. An AUC that exceeds 0.9 is considered excellent, while an AUC of less than 0.7 is poor.
Figure 2.4 represents an example of an ROC curve generated from MacLeod’s data on sperm concentration in fertile and infertile men [37]. Its AUC is only 0.59, indicating that the overall accuracy of sperm concentration for diagnosis of male infertility just narrowly exceeds that of random chance. In Guzick and colleagues’ series, which was depicted in Fig. 2.3, the AUC for sperm density, motility, and morphology were 0.60, 0.59, and 0.66, respectively [38].
The ROC curve alone does not provide information regarding the likelihood that a specific patient’s positive or negative test result is correct. This probability is dependent both on test performance and the prevalence of disease in the relevant population. As previously illustrated, a diagnosis of male infertility based on sperm concentration below 15 million/mL may be correct 75% of the time in the population of males from infertile couples. False-positive results for infertility are relatively rare in this population. By comparison, if semen analysis were performed on men in the general population (e.g., to assess sperm donors with no prior reproductive history), its positive predictive value would be considerably less, on account of a much lower prevalence of male infertility.
Other studies have reported AUCs for sperm density, motility, and morphology, as described in Table 2.7 [39,40,41,42,43]. In general, motility and morphology demonstrated greater discriminatory capability than sperm concentration. Although the authors of these studies reported “optimal thresholds” for discrimination of fertile and infertile men, some of these thresholds have been criticized for having an unacceptably low positive predictive value in the setting of an infertile population [44].
Guzick and colleagues took a different approach to selecting diagnostic thresholds, using classification and regression tree (CART) analysis to determine two thresholds for each parameter that define the upper and lower boundaries of an indeterminate range lying between the fertile and infertile ranges (see Table 2.7). Unfortunately, a large number of men presenting for infertility evaluation fall into the indeterminate range, leaving unanswered the question of whether they warrant intervention for modifiable risk factors. The odds of male infertility multiply if more than one semen parameter is within the infertile range [36], but only 1% of men fail to meet all five WHO reference criteria for ejaculate volume, total sperm number, sperm concentration, motility, and morphology [45].
3.2 Do Semen Parameters Prospectively Predict Fertility and Assisted Reproductive Technique Outcomes?
Only a handful of studies have attempted to prospectively identify variables associated with male reproductive potential. One such project included 200 couples, some of whom had had prior pregnancies [46]. After discontinuing contraception, the couples were followed for up to 12 months. Around 78% conceived during the study period, and both sperm motility and morphology were significantly associated with fertility. The difference in sperm concentration between fertile and infertile couples remained statistically insignificant.
Bonde and colleagues investigated 430 Danish couples between 20 and 35 years old who had never previously been or tried to become pregnant, following them for up to six menstrual cycles after discontinuation of contraception [47]. Around 60% of couples became pregnant. The probability of conception increased up to a threshold sperm concentration of 40 million/mL, but there was no additional likelihood of pregnancy at higher sperm densities (Fig. 2.5). This finding has led some reproductive specialists to argue that the appropriate threshold of sperm concentration for diagnosis of male infertility should be 40 instead of 15 million/mL [48]. A change of this sort, however, would also increase the number of false-positive diagnoses, prompting unnecessary evaluation and treatment.
Probability of pregnancy per menstrual cycle relative to sperm concentration. (Reprinted from Bonde et al. [47]. with permission of Elsevier)
Leushuis and colleagues have published an incisive review of prediction models in reproductive medicine, including several that use one or more semen characteristics to predict conception by infertile couples [49]. One such model, which has been externally validated in a population excluding men with total motile sperm counts of less than three million, takes account of sperm motility and the characteristics of the female partner and the duration of the couple’s infertility; it is available online at www.freya.nl/probability.php [50]. Another model utilizes inputs of sperm concentration, motility, morphology, and hypoosmotic swelling to assess the likelihood of pregnancy, with a reported accuracy greater than 85% [40]. Of note, however, the AUCs for each variable in this study substantially exceeded those published in the other reports described in Table 2.7, and the predictive model has yet to be validated.
Sperm quality also affects ART outcomes, at least to some degree. Several investigations have demonstrated a positive correlation between semen characteristics, including ROS levels, and in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) success rates; however, there was no apparent association with clinical pregnancy rates [51, 52]. Studies of intrauterine insemination (IUI), by contrast, have shown a correlation between successful outcomes and sperm concentration, motility, and morphology [44, 53,54,55].
3.3 Novel Assays for Diagnosis of Male Infertility
Andrologists often lament the lack of more accurate studies for diagnosis of male infertility. Several tests are currently in various stages of development, including genomic, epigenomic, proteomic, glycomic, lipidomic, and metabolomic analyses [56, 57]. Testing for seminal ROS levels was found to have an AUC of 0.82 in a study of 105 patients [58]. Further evaluation in a larger cohort of patients is necessary.
Sperm DNA fragmentation, or damage, may also have diagnostic value. The etiology of DNA fragmentation appears to be multifactorial, including accumulated defects during spermiogenesis, exposure to oxidative stress, exogenous toxicity (e.g., smoking), and elevated temperature (e.g., secondary to a varicocele) [59].
The degree of DNA fragmentation may have implications for ART success. Evaluation of 1633 IVF and ICSI cycles found the likelihood of a live birth after IVF to be significantly lower at higher levels of fragmentation. Using the sperm chromatin structure assay (SCSA) and DNA fragmentation index (DFI), the odds ratio of live birth after IVF was 0.61 (95% confidence interval 0.38–0.97, p = 0.04) when DFI was >20%. This decrease is believed to be due to impaired fertilization, since DNA fragmentation was not associated with a lower birth rate after ICSI [60].
However, questions remain as to the diagnostic accuracy and predictive value of different DNA fragmentation assays. Cissen and colleagues performed a meta-analysis of various techniques for assessment of DNA fragmentation, finding that only terminal nick-end labeling was able to predict IVF/ICSI outcomes [61].
4 Are Sperm Counts Declining?
One of the most controversial issues in reproductive medicine during the past 30 years has been a purported decline in semen quality during the twentieth century. In 1992, a widely publicized meta-analysis of 61 studies by Carlsen and colleagues appeared to demonstrate a worldwide decrease in average sperm concentration from 113 million/mL in 1940 to 66 million/mL in 1990 [62]. This report was echoed by additional publications, raising the question of whether exposure to environmental toxins, such as estrogenic compounds like diethylstilboestrol (DES), was adversely affecting testicular function [63, 64].
Important methodological shortcomings have since been identified in Carlsen and colleagues’ analysis and in the quality of many studies that were included in their review [65, 66]. Geographical differences were found to be the source of much of the variance in sperm density [67]. All studies included in the review from before 1970 were performed in the USA; however, because US studies generally reported higher sperm concentrations than those conducted elsewhere, the review was biased toward an apparent decline in sperm concentration by inclusion of international studies post-1970.
In subsequent investigations, Fisch and colleagues found no evidence of a decline in sperm density in the USA, although they did identify substantial differences between the average sperm counts of men from different states [68, 69]. Fisch and colleagues also concluded that worldwide studies did not reveal a global decline in semen quality, although more limited, locoregional trends could not be excluded [65].
More recently, Levine and colleagues published a large meta-regression analysis of 185 worldwide studies (including almost 43,000 men) that reported on sperm concentration and total sperm count between 1973 and 2011 [70]. They found a 52% decrease in sperm concentration and a 59% decrease in total sperm count among Western countries (North America, Europe, Australia, and New Zealand) but no significant decline of either parameter in non-Western countries. This decline has not been uniformly reported, though. A key study of nearly 5000 Danish men found a slight increase in sperm concentration, total sperm count, and total normal morphology from 1996–2000 to 2006–2010 [71].
5 Health-Care Resource Utilization for Male Infertility
Medical intervention for male infertility may take the form of outpatient care, surgical procedures, and ART. The Urologic Diseases in America (UDA) Project, which published its first report in 2007, has facilitated a better understanding of the scope of health-care resource utilization for male infertility in the USA.
5.1 Office Visits and Ambulatory Surgery Cases
According to data from the National Ambulatory Medical Care Survey (NAMCS), which are summarized in the UDA Project’s report, the average number of physician office visits for male infertility in the United States exceeded 150,000 annually between 1992 and 2000, with little variability [72]. However, there was a 29% decline in hospital outpatient visits and 23% decline in outpatient visits for male infertility from 2002 to 2006 [73]. The reasons for this trend are unclear but may include preferential use of ART.
Age-wise, the greatest utilization of health-care services for male infertility between 2002 and 2006 was among men 35–39 years old. Varicocele was the most commonly identified diagnostic code, accounting for 53% of office visits and 67% of ambulatory surgeries.
Other data from the NAMCS demonstrate substantial regional variation in resource utilization for male infertility. Men living in the Northeast United States had a rate of ambulatory surgery visits associated with a diagnosis of infertility of 227 per 100,000, while those in the Midwest, South, and West had rates of just 110.9, 128.9, and 119.2 per 100,000, respectively. The decline in outpatient visits was disproportionately experienced in the Northeast and West, decreasing by 36% and 32%, respectively, from 2002 to 2006. Visits in the South and Midwest decreased by 17%. The explanation for this variability is probably multifactorial, reflecting a combination of patient demand and availability of services.
5.2 Assisted Reproductive Technology
About 231,936 ART cycles were performed in the United States in 2015, an increase from 142,435 in 2007 and 81,438 in 1998 [74]. A total of 60,778 live births resulted from these cycles, representing a cumulative success rate of 26.2%. Approximately 33% of ART cycles were associated with a diagnosis of male factor infertility, and 17% were linked to a combination of male and female factors. The overall likelihood of a live birth per ART cycle was 34.4%.
The percentage of ART procedures involving the use of ICSI has steadily increased, from 71% in 2006 to 79% in 2015 [74]. Although ICSI was originally developed specifically to overcome severe oligozoospermia or azoospermia, nearly 70% of ART cycles now utilize ICSI even when no male factor is identified [74].
5.3 Cost of Treatment for Male Infertility
The overall economic burden of health care for male infertility is difficult to estimate precisely. While expenditures for office and ambulatory surgery visits were reported by the NAMCS to be $17 million in 2000, this figure does not account for IVF/ICSI or out-of-pocket expenditures [75]. If the assumed cost per IVF cycle is $15,715, then expenditures on ART alone for male infertility exceeded $1.8B in 2015, given the percentage of ART procedures involving a diagnosis of male factor infertility [74, 76] .
On an individual basis, the average annual expenditures on health care for a privately insured male with infertility was $11,437 from 2003 to 2006, compared with $6942 for men without infertility. The difference in expenditures increases with patient age, from $2249 for men aged 18–34 to $8127 for men aged 55–64, likely due to increased utilization of more costly IVF technology [73].
There are significant disparities between countries in the cost of utilizing ART. In 2009, the average cost of a standard IVF cycle in the United States was $12,513, compared with $8500 in Canada, $6534 in the United Kingdom, and $3956 in Japan [77].
6 Cost Analysis Models for Management of Male Infertility
When a male risk factor for infertility is identified, the couple is often faced with the choice of using ART or having pathology-directed treatment. Evaluating the economic efficiency of these alternatives is the domain of cost analysis.
Cost analysis is only meaningful with respect to treatments that have previously been demonstrated to be effective. Our intention in this chapter is not to review the studies that have established the effectiveness of the interventions discussed here—or, in some cases, the controversies surrounding them. Rather, our focus is limited to a brief introduction to cost analysis studies as they pertain to male infertility.
Two types of cost analysis are utilized in reproductive medicine: cost-minimization analysis and cost-effectiveness analysis. The first, cost-minimization analysis, is also known as cost identification. It involves assessment (and comparison) of the costs associated with particular treatments. Direct and/or indirect costs may be taken into account—direct costs being health-care expenditures and indirect costs being “downstream” burdens such as transportation expenses, lost wages, etc. In well-conducted economic analyses, future costs should be appropriately discounted to present values by a factor of 3%–5% per year.
When the outcomes of alternative interventions are not equivalent, cost-effectiveness analysis is useful to compare them, as it involves not only identifying the costs that accrue but also expressing them relative to the probability of a particular result (e.g., dollars per pregnancy or live birth). Decision analysis, such as Markov modeling, is the most common technique employed for this purpose in the field of male infertility. Details of relevant methodology are covered in Methods for the Economic Evaluation of Health Care Programmes [78].
Comparison of cost-effectiveness has been applied to several management options that may be encountered in male reproductive medicine, including varicocele treatment vs. immediate ART (with or without surgical sperm retrieval), vasectomy reversal vs. ART, and hormonal therapy vs. ART for hypogonadotropic hypogonadism. Pathology-directed intervention has almost invariably been found to be more cost-effective than a straight-to-ART approach [79, 80]. One exception is when a varicocele is present in the setting of nonobstructive azoospermia; in this situation, microsurgical testicular sperm extraction (TESE) for ICSI is more cost-effective than varicocelectomy [81].
Every cost-effectiveness analysis in the arena of male infertility is sensitive to assumptions about treatment costs, success and complication rates, and the subsequent management of couples for whom first-line intervention is unsuccessful [82, 83]. Precise characterization of the clinical scenario(s) is very important and should be considered when determining the generalizability of results. For instance, the age of the female partner has a significant influence on the relative cost-effectiveness of vasectomy reversal and ART [75].
7 Conclusion
This chapter examined a number of issues that are commonly misunderstood and/or misrepresented with respect to the epidemiology of infertility, in general, and male infertility, in particular. First, infertility should not be confused with sterility—or even below-average fecundability. Approximately 10% of couples with average reproductive potential will not conceive within 12 months of unprotected intercourse and are therefore designated as infertile. Such couples may comprise a substantial proportion of those who present for evaluation of infertility (see Table 2.3). Their odds of spontaneous, unassisted conception remain high.
From a clinical standpoint, it would be ideal to accurately identify men with below-average reproductive potential. However, while semen analysis is the most common test employed for this purpose, its utility is limited by substantial overlap between the distributions of semen characteristics in empirically fertile and infertile men. Using relatively low diagnostic thresholds, such as the 2010 WHO reference values, carries the advantage of high specificity and perhaps a relatively decent positive predictive value in the setting of an infertility clinic; unfortunately, the negative predictive value only narrowly exceeds that of a coin flip.
The diagnostic inaccuracy of semen analysis is a fundamental problem for several additional reasons. From an epidemiologic perspective, the absence of a gold-standard test for male infertility means that we have, at best, an uncertain grasp of its actual prevalence, let alone its association with putative risk factors, such as varicocele, cryptorchidism, sexually transmitted infections, etc. Moreover, if the true prevalence of male infertility is unclear then so, too, is the predictive value of tests employed for its diagnosis.
Finally, there is the question of how to counsel infertile men whose semen parameters exceed diagnostic thresholds. Given the poor predictive value of these “negative” results, should we advise consideration of further evaluation and treatment for modifiable risk factors identified in these individuals? An affirmative response to this query carries the risk of unnecessary treatment and costs, while the alternative may deprive some couples of an improvement in reproductive potential that facilitates natural conception, allows the use of IUI instead of IVF, or increases the odds of successful IVF/ICSI [84]. Well-designed studies to address this question are necessary.
8 Review Criteria
An extensive search was performed to identify studies regarding the epidemiology, diagnosis, and treatment of male infertility. Search engines such as MEDLINE (Ovid), PubMed, and Google Scholar were used. For the second edition, emphasis was placed on studies published between 2010 and 2018. Key search terms included male infertility, incidence, epidemiology, sperm count, semen parameters, prediction, cost analysis, DNA fragmentation, IVF, ART, and ICSI. Data were abstracted from publications by the Centers for Disease Control and Prevention (CDC), including the National Ambulatory Medical Care Survey and the CDC’s ART National Summary Report, as well as the Urologic Diseases in America report issued by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Articles published in languages other than English were not considered. Websites and book-chapter citations provide conceptual content only.
References
Agarwal A, Sharma RK, Nallella KP, Thomas AJ Jr, Alvarez JG, Sikka SC. Reactive oxygen species as an independent marker of male factor infertility. Fertil Steril. 2006;86(4):878–85.
Athayde KS, Cocuzza M, Agarwal A, Krajcir N, Lucon AM, Srougi M, et al. Development of normal reference values for seminal reactive oxygen species and their correlation with leukocytes and semen parameters in a fertile population. J Androl. 2007;28(4):613–20.
Sharma RK, Said T, Agarwal A. Sperm DNA damage and its clinical relevance in assessing reproductive outcome. Asian J Androl. 2004;6(2):139–48.
Tremellen K. Oxidative stress and male infertility--a clinical perspective. Hum Reprod Update. 2008;14(3):243–58.
Lumley J. Epidemiological approaches to infertility. Reprod Fertil Dev. 1998;10(1):17–21.
Alukal JP, Lipshultz LI. Why treat the male in the era of assisted reproduction? Semin Reprod Med. 2009;27(2):109–14.
Davies MJ, Delacey SL, Norman RJ. Towards less confusing terminology in reproductive medicine clarifying medical ambiguities to the benefit of all. Hum Reprod. 2005;20(10):2669–71.
Habbema JD, Collins J, Leridon H, Evers JL, Lunenfeld B, te Velde ER. Towards less confusing terminology in reproductive medicine: a proposal. Hum Reprod. 2004;19(7):1497–501.
Greenhall E, Vessey M. The prevalence of subfertility: a review of the current confusion and a report of two new studies. Fertil Steril. 1990;54(6):978–83.
Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology 2009. Fertil Steril. 2009;92(5):1520–4.
Sigman M, Jarow JP. Male infertility. In: Wein AJ, Kavoussi LR, et al., editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders Elsevier; 2007. p. 609–53.
Simpson JL, Jauniaux ERM. Pregnancy loss. In: Gabbe SG, Niebyl JR, Simpson JL, editors. Obstetrics: normal and problem pregnancies. 5th ed. Philadelphia, PA: Churchill Livingstone Elsevier; 2007. p. 628–49.
Stephen EH, Chandra A. Declining estimates of infertility in the United States: 1982-2002. Fertil Steril. 2006;86(3):516–23.
Special calculation by NCHS from NSFG, Martinez, Gladys M, Daniels K, Febo-Vazquez, I. Fertility of men and women aged 15–44 in the United States: National Survey of Family Growth, 2011–2015. National Health Statistics Report. Number 113, 2018.
te Velde ER, Eijkemans R, Habbema HD. Variation in couple fecundity and time to pregnancy, an essential concept in human reproduction. Lancet. 2000;355(9219):1928–9.
Rutstein SO, Shah IH. Infecundity, infertility, and childlessness in developing countries. In: DHS comparative reports no. 9. Calverton: ORC Macro and the World Health Organization; 2004.
Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356.
Lunenfeld B, Van Steirteghem A, Bertarelli F. Infertility in the third millennium: implications for the individual, family and society: condensed meeting report from the Bertarelli Foundation's second global conference. Hum Reprod Update. 2004;10(4):317–26.
Kefer JC, Agarwal A, Sabanegh E. Role of antioxidants in the treatment of male infertility. Int J Urol. 2009;16(5):449–57.
Ford WC, North K, Taylor H, Farrow A, Hull MG, Golding J. Increasing paternal age is associated with delayed conception in a large population of fertile couples: evidence for declining fecundity in older men. The ALSPAC study team (Avon longitudinal study of pregnancy and childhood). Hum Reprod. 2000;15(8):1703–8.
van Noord-Zaadstra BM, Looman CW, Alsbach H, Habbema JD, te Velde ER, Karbaat J. Delaying childbearing: effect of age on fecundity and outcome of pregnancy. BMJ. 1991;302(6789):1361–5.
Evers JL. Female subfertility. Lancet. 2002;360(9327):151–9.
Leridon H, Spira A. Problems in measuring the effectiveness of infertility therapy. Fertil Steril. 1984;41(4):580–6.
Spira A. Epidemiology of human reproduction. Hum Reprod. 1986;1(2):111–5.
Evers JL, te Velde ER. Vruchtbaarheidsstoornissen. In: Heineman MJ, Bleker OP, Evers JL, Heintz AP, editors. Obstetrie en Gynaecologie, de voortplanting van de mens. Maarssen: Elsevier Science; 2001. p. 435–71.
Bongaarts J. A method for the estimation of fecundability. Demography. 1975;12(4):645–60.
Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod. 2002;17(5):1399–403.
Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod. 2003;18(9):1959–66.
Sharlip ID, Jarow JP, Belker AM, Lipshultz LI, Sigman M, Thomas AJ, et al. Best practice policies for male infertility. Fertil Steril. 2002;77(5):873–82.
Muller CH. Rationale, interpretation, validation, and uses of sperm function tests. J Androl. 2000;21(1):10–30.
Barratt CL, Aitken RJ, Bjorndahl L, Carrell DT, de Boer P, Kvist U, et al. Sperm DNA: organization, protection and vulnerability: from basic science to clinical applications--a position report. Hum Reprod. 2010;25(4):824–38.
Kobayashi H, Gil-Guzman E, Mahran AM, Rakesh Nelson DR, Thomas AJ Jr, et al. Quality control of reactive oxygen species measurement by luminol-dependent chemiluminescence assay. J Androl. 2001;22(4):568–74.
Santi D, De Vincentis S, Magnani E, Spaggiari G. Impairment of sperm DNA methylation in male infertility: a meta-analytic study. Andrology. 2017;5(4):695–703.
Menkveld R. Clinical significance of the low normal sperm morphology value as proposed in the fifth edition of the WHO Laboratory manual for the examination and processing of human semen. Asian J Androl. 2010;12(1):47–58.
Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001;345(19):1388–93.
Macleod J. Semen quality in 1000 men of known fertility and in 800 cases of infertile marriage. Fertil Steril. 1951;2(2):115–39.
Niederberger CS. Understanding the epidemiology of fertility treatments. Urol Clin North Am. 2002;29(4):829–40.
Gunalp S, Onculoglu C, Gurgan T, Kruger TF, Lombard CJ. A study of semen parameters with emphasis on sperm morphology in a fertile population: an attempt to develop clinical thresholds. Hum Reprod. 2001;16(1):110–4.
Jedrzejczak P, Taszarek-Hauke G, Hauke J, Pawelczyk L, Duleba AJ. Prediction of spontaneous conception based on semen parameters. Int J Androl. 2008;31(5):499–507.
Menkveld R, Wong WY, Lombard CJ, Wetzels AM, Thomas CM, Merkus HM, et al. Semen parameters, including WHO and strict criteria morphology, in a fertile and subfertile population: an effort towards standardization of in-vivo thresholds. Hum Reprod. 2001;16(6):1165–71.
Ombelet W, Bosmans E, Janssen M, Cox A, Vlasselaer J, Gyselaers W, et al. Semen parameters in a fertile versus subfertile population: a need for change in the interpretation of semen testing. Hum Reprod. 1997;12(5):987–93.
Sripada S, Townend J, Campbell D, Murdoch L, Mathers E, Bhattacharya S. Relationship between semen parameters and spontaneous pregnancy. Fertil Steril. 2010;94(2):624–30.
van der Merwe FH, Kruger TF, Oehninger SC, Lombard CJ. The use of semen parameters to identify the subfertile male in the general population. Gynecol Obstet Invest. 2005;59(2):86–91.
Hart RJ, Doherty DA, McLachlan RI, Walls ML, Keelan JA, Dickinson JE, et al. Testicular function in a birth cohort of young men. Hum Reprod. 2015;30(12):2713–24.
Zinaman MJ, Brown CC, Selevan SG, Clegg ED. Semen quality and human fertility: a prospective study with healthy couples. J Androl. 2000;21(1):145–53.
Bonde JP, Ernst E, Jensen TK, Hjollund NH, Kolstad H, Henriksen TB, et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet. 1998;352(9135):1172–7.
Skakkebaek NE. Normal reference ranges for semen quality and their relations to fecundity. Asian J Androl. 2010;12(1):95–8.
Leushuis E, van der Steeg JW, Steures P, Bossuyt PM, Eijkemans MJ, van der Veen F, et al. Prediction models in reproductive medicine: a critical appraisal. Hum Reprod Update. 2009;15(5):537–52.
van der Steeg JW, Steures P, Eijkemans MJ, Habbema JD, Hompes PG, Broekmans FJ, et al. Pregnancy is predictable: a large-scale prospective external validation of the prediction of spontaneous pregnancy in subfertile couples. Hum Reprod. 2007;22(2):536–42.
Mercan R, Lanzendorf SE, Mayer J Jr, Nassar A, Muasher SJ, Oehninger S. The outcome of clinical pregnancies following intracytoplasmic sperm injection is not affected by semen quality. Andrologia. 1998;30(2):91–5.
Zorn B, Vidmar G, Meden-Vrtovec H. Seminal reactive oxygen species as predictors of fertilization, embryo quality and pregnancy rates after conventional in vitro fertilization and intracytoplasmic sperm injection. Int J Androl. 2003;26(5):279–85.
Allamaneni SS, Bandaranayake I, Agarwal A. Use of semen quality scores to predict pregnancy rates in couples undergoing intrauterine insemination with donor sperm. Fertil Steril. 2004;82(3):606–11.
Ombelet W, Deblaere K, Bosmans E, Cox A, Jacobs P, Janssen M, et al. Semen quality and intrauterine insemination. Reprod Biomed Online. 2003;7(4):485–92.
Shibahara H, Obara H, Ayustawati HY, Suzuki T, Ohno A, et al. Prediction of pregnancy by intrauterine insemination using CASA estimates and strict criteria in patients with male factor infertility. Int J Androl. 2004;27(2):63–8.
Aitken RJ. Whither must spermatozoa wander? The future of laboratory seminology. Asian J Androl. 2010;12(1):99–103.
Deepinder F, Chowdary HT, Agarwal A. Role of metabolomic analysis of biomarkers in the management of male infertility. Expert Rev Mol Diagn. 2007;7(4):351–8.
Desai N, Sharma R, Makker K, Sabanegh E, Agarwal A. Physiologic and pathologic levels of reactive oxygen species in neat semen of infertile men. Fertil Steril. 2009;92(5):1626–31.
Rex AS, Aagaard J, Fedder J. DNA fragmentation in spermatozoa: a historical review. Andrology. 2017;5(4):622–30.
Oleszczuk K, Giwercman A, Bungum M. Sperm chromatin structure assay in prediction of in vitro fertilization outcome. Andrology. 2016;4(2):290–6.
Cissen M, Wely MV, Scholten I, Mansell S, Bruin JP, Mol BW, et al. Measuring sperm DNA fragmentation and clinical outcomes of medically assisted reproduction: a systematic review and meta-analysis. PLoS One. 2016;11(11):e0165125.
Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992;305(6854):609–13.
de Kretser DM. Declining sperm counts. BMJ. 1996;312(7029):457–8.
Sharpe RM, Skakkebaek NE. Are oestrogens involved in falling sperm counts and disorders of the male reproductive tract? Lancet. 1993;341(8857):1392–5.
Fisch H. Declining worldwide sperm counts: disproving a myth. Urol Clin North Am. 2008;35(2):137–46, vii.
Sherins RJ. Are semen quality and male fertility changing? N Engl J Med. 1995;332(5):327–8.
Fisch H, Goluboff ET. Geographic variations in sperm counts: a potential cause of bias in studies of semen quality. Fertil Steril. 1996;65(5):1044–6.
Fisch H, Goluboff ET, Olson JH, Feldshuh J, Broder SJ, Barad DH. Semen analyses in 1,283 men from the United States over a 25-year period: no decline in quality. Fertil Steril. 1996;65(5):1009–14.
Saidi JA, Chang DT, Goluboff ET, Bagiella E, Olsen G, Fisch H. Declining sperm counts in the United States? A critical review. J Urol. 1999;161(2):460–2.
Levine H, Jorgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, et al. Temporal trends in sperm count: a systematic review and meta-regression analysis. Hum Reprod Update. 2017;23(6):646–59.
Jorgensen N, Joensen UN, Jensen TK, Jensen MB, Almstrup K, Olesen IA, et al. Human semen quality in the new millennium: a prospective cross-sectional population-based study of 4867 men. BMJ Open. 2012;2(4).
Niederberger CS, Joyce GF, Wise M, Meacham RB. Male infertility. In: Litwin MS, Saigal CS, editors. Urologic diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: U.S. Government Printing Office; 2007., ; NIH Publication No. 07-5512. p. 461–81.
Saigal CS, Liu H, Hanley JM, Madison RA, Smith AC, Lai JC, Dick AW. Chapter 15: Methods. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office; 2012; NIH Publication No. 12-7865. p. 497–522.
Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. Assisted reproductive technology National Summary Report. Atlanta: US Dept of Health and Human Services; 2015. p. 2017.
Hsieh MH, Meng MV, Turek PJ. Markov modeling of vasectomy reversal and ART for infertility: how do obstructive interval and female partner age influence cost effectiveness? Fertil Steril. 2007;88(4):840–6.
Crawford S, Boulet SL, Mneimneh AS, Perkins KM, Jamieson DJ, Zhang Y, et al. Costs of achieving live birth from assisted reproductive technology: a comparison of sequential single and double embryo transfer approaches. Fertil Steril. 2016;105(2):444–50.
Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril. 2009;91(6):2281–94.
Drummond MF, Schulpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. New York: Oxford University Press; 2005. p. 277–322.
Robb P, Sandlow JI. Cost-effectiveness of vasectomy reversal. Urol Clin North Am. 2009;36(3):391–6.
Shin D, Honig SC. Economics of treatments for male infertility. Urol Clin North Am. 2002;29(4):841–53.
Lee R, Li PS, Goldstein M, Schattman G, Schlegel PN. A decision analysis of treatments for nonobstructive azoospermia associated with varicocele. Fertil Steril. 2009;92(1):188–96.
Meng MV, Greene KL, Turek PJ. Surgery or assisted reproduction? A decision analysis of treatment costs in male infertility. J Urol. 2005;174(5):1926–31; discussion 31.
Penson DF, Paltiel AD, Krumholz HM, Palter S. The cost-effectiveness of treatment for varicocele related infertility. J Urol. 2002;168(6):2490–4.
Esteves SC, Oliveira FV, Bertolla RP. Clinical outcome of intracytoplasmic sperm injection in infertile men with treated and untreated clinical varicocele. J Urol. 2010;184(4):1442–6.
Acknowledgments
The authors thank Kelli M. Mulder and Ranya N. Sweis for critically reviewing an earlier edition of this chapter. Jonathan L. Faasse and Kristin M. Faasse provided valuable assistance with the figures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ohlander, S.J., Halgrimson, W.R., Faasse, M.A. (2020). Epidemiologic Considerations in Male Infertility. In: Parekattil, S., Esteves, S., Agarwal, A. (eds) Male Infertility. Springer, Cham. https://doi.org/10.1007/978-3-030-32300-4_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-32300-4_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32299-1
Online ISBN: 978-3-030-32300-4
eBook Packages: MedicineMedicine (R0)