Abstract
In the accelerated way that Medical Devices (MDs) are developed and revolutionize health care delivery during the last decades, Regulation, Management and Assessment of Health Technology are of paramount importance. This paper provides a short overview of the recent development in this area and discusses some issues related to the new EU regulatory framework on MDs, the need for a more rigorous management and the importance of Health Technology Assessment for MDs. Study is also focusing on the particular characteristics of MDs that impose a different approach, in these three domains, compared to medicinal products, in order to get the expected benefits right to the patients, in a safe and cost-effective way.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The rate of growth of health expenses has consistently exceeded GDP growth in each and every decade. In 2009 EU countries spent, on average, 9.6% of their GDP on health, compared to 8.8% in 2008 and 7.3% in 1998. Between 1980 and 2000, medical technology reduced hospital stays by more than 50% and between 2000 and 2008, by an average of an additional 13%. Still, Medical technology accounts for less than 5% of the total health care expenditure.
Medical technology industry is one of Europe’s most diverse and innovative high-tech sectors, with more than 13,000 patent applications filed by the European Patent Office (EPO) in 2017, more than double compared with the pharmaceuticals. Medical Technology is amongst the largest technical sectors of Europe, with 27,000 medical technology companies, (95% of them SMEs) employing over 675,000 people in Europe [1]. The global medical device market is estimated to more than 400 billion Euros in year 2017, with more than 500,000 medical technologies available. Europe represents 27% of this market, with a 20 million Euros positive MDs trade balance.
The MDs life cycle starts with an idea and hopefully passes a number of stages before it is placed on the market, used and discarded. These phases include the R&D cycle, usually with the development and testing stages, leading to a prototype, that initially undergoes preclinical tests not involving humans. If successful, clinical trials are performed and conformity with the legal framework is certified in order to get approval for placing on the market. Procurement and use are the final phase and if appropriate, Health Technology Assessment is done. The whole MD life cycle is graphically depicted in Fig. 1.
Τhe medical technology sector today is characterized by a high degree of regulation and standardization, aiming to ensure reliability, safety, and performance, under proper conditions of use and maintenance. All medical devices produced and “placed on the market”, are in accordance with the international standards and have the necessary certification in compliance with the Medical Devices Directives and guidelines for the EU, and/or FDA approval for the US. It should also be stressed that, in contrary with the past, life cycle of MDs is quite short today, sometimes down to two years before an improved product becomes available.
2 The Three Pillars for Patient Safety
There are three major ways that patient safety is assured today: Regulations that addresses the issues related to placing safe devices on the market, Management that is related to the safe use of the devices and Assessment that provides evidence-based information for decision making (Fig. 2).
2.1 Regulations
The path to a common European MDs legal framework started in the 80s with the decisions of the ‘New approach and the preparation of the three central European Directives on: the Active Implantable Medical Devices (AIMDs), the In Vitro Diagnostics (IVDs) and the main Medical Devices (MDs) including all other devices not included in the two previous mentioned categories. Three Directives were voted by the European Parliament in the nineties:
These directives were implemented in the form of national laws and therefore harmonization of the European market took place. The Directives are complemented by a number of guidelines (MEDDEVs), like the Risk Classification of MDs or guidelines on Vigilance, and by harmonized standards, that provide technical requirements for conformity assessment. With these European directives, certification became compulsory, in order to prove compliance of the product with the requirements of the Directives, to put the CE marking, otherwise marketing of the product is not allowed [5]. At the same time the application of Information and Communication Technologies were slowly introduced in the regulatory sector although with a lot of reluctance, until the mid 2000s with the launch European Database on Medical Devices (EUDAMED), in spite of the fact that the basic work was ready ten years ago [6] (Fig. 3).
Following some failure cases for the directives to assure patient safety for devices put on the market with the CE mark, in the late 2010s it was decided to change the regulatory framework. As a result, in 2017, the three directives have been replaced by two regulations:
Regulations are stricter in terms of implementation and rules of compliance and monitoring. Their scope is broadened in relation to the three Directives. Some main differences introduced are listed below:
-
The classification of products shows a general trend of upgrading the risk categories.
-
For the certification/licensing of high-risk products, participation of the authorities and/or expert groups is necessary. At the same time the requirements for technical documentation are increasing.
-
The Unique Device Identification (UDI) is introduced to improve the recognition and traceability of products.
-
The central system of safety and vigilance reports is being upgraded and the role of the European Database on Medical Devices (EUDAMED) becomes more critical.
-
A central approach is foreseen for the submission of international clinical investigations and the procedures for the notification of post-clinical valuation.
There is however criticism on the negative impact that this stricter approach will have on innovation. Problems are also faced by the manufacturers with the certification process by the notified bodies that are significantly reduced in number and therefore overcharged and respond to the demand with big delays.
2.2 Management
Health Technology Management, mainly deals with all aspects related to safe and effective use of the devices placed on the market, from the procurement phase up to their withdrawal. Efficient management of technology in the hospital environment starts with good matching between needs and capabilities. To be successful, it must integrate the technology procurement planning and management program at the hospital level, with a final goal to address the needs of proper patient care [9]. Implementing a comprehensive biomedical technology management program is a quite complex and multidimensional process, that depends on the skills and the background of the personnel involved. In principle it contains the tasks briefly outlined below, nowadays performed by the Clinical Engineering Departments:
Medical Equipment Inventorying, consisting of organized records of all medical equipment items belonging to or used in the hospital.
Medical Equipment Procurement Planning, aiming to ensure the availability of appropriate equipment at the right time in the right place.
Medical Equipment Acquisition, including preparation of technical specifications, call for tender, offers evaluation, and contract signing.
Acceptance Testing, to verify that the correct devices have been delivered and properly installed.
Training, to assure proper use of the devices.
Preventive Maintenance, keeping the equipment in good functional condition, through regular inspections and service
Corrective Maintenance, when repairs are necessary for re-establishing the normal operating status.
Quality Assurance, comprising planning and performing quality control and safety tests of medical equipment.
Disposal, when the equipment becomes obsolete.
Management of hospital technology requires creation and continuous update of data files with all interventions performed on each individual equipment, covering its whole life cycle. These data must be easily retrievable and able to be presented to the end users in an appropriate way, i.e. converted into meaningful information. Since the 80s software tools have been created, known as Medical Equipment Management Systems (MEMS) or as Computerized Maintenance Management Systems (CMMS) that assist clinical engineers to performs their tasks, covering all management activities of the CEDs including:
-
management of files for medical devices, manufactures, and suppliers
-
follow up of equipment acquisition procedures, from the request departments to acceptance testing
-
implementation and management of quality and safety protocols and procedures
-
scheduling of all routine procedures, inspections and tests
-
follow up of all corrective maintenance tasks
-
management and monitoring of training activities provided by the CED
-
monitoring of the overall performance of the department, using quality and cost indicators
-
easy access to and exchange of vigilance-related information
-
data analysis and report generation
The ICT evolution has nowadays, provided CMMS operating over networks, interconnected with other hospital information systems and the equipment themselves [10].
2.3 Health Technology Assessment HTA
HTA is multi-disciplinary field of policy analysis that examines the medical, economic, social and ethical implications of the incremental value, diffusion and use of a medical technology in health care. HTA mainly deals and provides information and evidence on:
-
Comparative clinical effectiveness
-
Comparative cost-effectiveness
-
Health delivery organisational aspects
-
Legal framework
-
Ethical, social implications
Balancing access, quality of care and sustainability of a health care system, is a challenging task, especially when deciding on the best use of the limited budgets available. Acceptable levels of safety, cost-effectiveness, may vary in different communities, countries, or circumstances and the overall health benefits for the population should be considered in each case, i.e. what intervention on the adoption of technologies result in the greatest health benefits to a community. Difficult questions like:
-
Are the interventions cost effective?
-
Is the technology affordable?
-
Is context-specific?
should be answered and justified. The problem of «when-to-assess?» is also critical. It should be when enough evidence could be gathered on most parameters to be studied. However, it is a “moving target problem” since there is always the risk that a delay in the time HTA is performed and disseminated, could make its findings soon outdated by technological changes.
Although in the past, the methods applied for medicines were also used for MDs, the need for different approaches in HTA of MDs is now recognized [11]. The new regulatory framework for MDs clearly introduces new incentives for HTA [12].
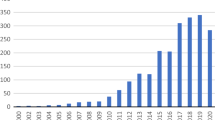
New technologies significantly improve clinical practice, but their rapid growth is making it virtually impossible for care providers to keep in pace with all new advancements. Additionally, reluctance to change long-standing practices, as well as outdated education, restricts the uptake of new and potentially more efficient solutions. Growing concerns about more financial constraints, accountability, transparency, and legitimacy in decision-making processes, imposed more evidence-based approaches. Health Technology Assessment (HTA), emerged exactly from the need to give answers and support decisions on the development, approval, and diffusion of health technologies. Although the scope of HTA is very large and the majority of reports address pharmaceuticals, the medical equipment sector has recently started gaining more attention. Its origin goes back actually in the 1970s, when healthcare institutions were under pressure to apply newly appeared costly medical equipment, especially in the diagnostic imaging area. A kind of precursor was the comparative evaluation trend of MDs that flourished in the 1980s, but was of limited scope and unable to cope with the very rapid changes during the 90s and was therefore abandoned. The growth and development of HTA and especially the hospital-based HTA, during the two last decades, focusing on medical equipment-related technologies, reflects the importance that this field is gaining. CEs being in the center of technology management, with a profound understanding of the technical issues, are well placed to play a pivotal role as members of the interdisciplinary teams working in HTA worldwide.
3 Future Perspectives
Health technology will continue to grow and contribute to improvements in healthcare delivery. At the same time, it will require more often update of regulations in order to face the explosive changes and continue to assure patient safety without compromising innovation.
Apart from the new impressive medical technologies already announced or still at the R&D stage, very important impact comes also from the developments in Information and Communication Technologies, with mobile applications, distance monitoring and data exchange and retrieval. Today’s medical equipment either incorporates embedded computer systems or the equipment is computer-driven. They also started to be interconnected and self-tested or calibrated.
The systematic operation of CMMS will continue to contribute considerably towards the improvement of effective medical technology management in healthcare facilities, with significant benefits relating to cost-effectiveness and safety. However, future CMMS are expected to be directly connected with most of the equipment, with new remote monitoring and diagnostic capabilities.
HTA for medical devices should find its own way and models of conductance, to respond to the large and ever-expanding variety of technologies involved should be crated, in order to continue to play its important role.
4 Conclusions
The future of medical technology will continue to provide impressive solutions and possibilities. However, it is important to keep regulation effective, management efficient and HTA adaptable, taking into account their influence to the financial, social and environmental variables of countries and systems that are directly implemented, but also their indirect impact worldwide.
References
MedTech Europe: https://www.medtecheurope.org
Council Directive 90/385/EEC: Official Journal of the European Commission L-189 (1990)
Council Directive 93/42/EEC: Official Journal of the European Commission L-169 (1993)
Council Directive 98/79/EC: Official Journal of the European Commission L-331 (1998)
Pallikarakis, N., Moore, R.: Health technology in Europe—regulatory framework and industry perspectives of the “new approach”. IEEE Eng. Med. Biol. Mag. 26(3), 14–17 (2007)
Pallikarakis, N., Anselmann, N., Pernice, A. (eds.): Information Exchange for Medical Devices. IOS Press, Amsterdam (1996)
REGULATION (EU) 2017/745: Official Journal of the European Union, L 117/1, 5.5.2017
REGULATION (EU) 2017/746: Official Journal of the European Union, L 117/176, 5.5.2017
Medicines and Healthcare Products Regulatory Agency Annual Report and Accounts 2013/14, Medicines and Healthcare Products Regulatory Agency (MHRA), Williams Lea Group, 117 p., Print ISBN 9781474108119, Web ISBN 9781474108126, https://www.gov.uk/government/publications/medicines-and-healthcare-products-regulatory-agency-annual-report-and-accounts-2013-to-2014
Malataras, P., Bliznakov, Z., Pallikarakis, N.: Re-engineering a medical devices management software system: the web approach. Int. J. Reliable Qual. E-Healthc. 3, 9–18 (2014)
Polisena, J., Castaldo, R., Ciani, et al.: Health technology assessment methods guidelines for medical devices: how can we address the gaps? The international federation of medical and biological engineering perspective. Int. J. Technol. Assess. Health Care 34(3), 276–289 (2018)
Commission Proposal on Health Technology Assessment: European Commission-Fact Sheet. Retrieved from http://europa.eu/rapid/press-release_MEMO-18-487_en.htm (2018)
Acknowledgements
The author wants to acknowledge the precious information, inspiring ideas and fruitful discussions, provided by the IFMBE/Clinical Engineering and Health Technology Assessment Divisions which are exceptionally active and productive during the last period. The unique leading role and guidance of the WHO medical devices sector in the field is equally remarkable and extremely motivating.
Compliance with Ethical Requirements The author declares that there is no Conflict of Interest, or any other no compliance with ethical requirements.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this paper
Cite this paper
Pallikarakis, N. (2020). Medical Devices Regulations, Management and Assessment; New Trends New Needs. In: Tiginyanu, I., Sontea, V., Railean, S. (eds) 4th International Conference on Nanotechnologies and Biomedical Engineering. ICNBME 2019. IFMBE Proceedings, vol 77. Springer, Cham. https://doi.org/10.1007/978-3-030-31866-6_109
Download citation
DOI: https://doi.org/10.1007/978-3-030-31866-6_109
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31865-9
Online ISBN: 978-3-030-31866-6
eBook Packages: EngineeringEngineering (R0)