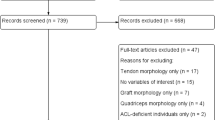
Abstract
A hamstring strain injury has long been considered as a skeletal muscle injury, and the connective tissue associated with the muscle, i.e., the tendon/aponeurosis, has not been addressed sufficiently. A hamstring strain is a traumatic injury which very often occurs at the myotendinous junction (MTJ), which is the interface between the muscle and the tendon. The MTJ is formed during development and animal research clearly shows the interdependence and interaction between the muscle-derived and the connective tissue-derived cells during developmental processes. Additionally, several key molecules are indispensable for the MTJ formation. Although the MTJ is the most affected site after a strain injury, the research in adaptations to loading, unloading, and regeneration of the human MTJ is scarce. Skeletal muscle has a pronounced healing capacity, but the connective tissue in contrast is associated with a long repair period and incomplete repair. The differences in tissue healing and regeneration may complicate MTJ repair after hamstring strain injuries and might be the underlying factor why these sports injuries have a high recurrence rate. Re-injuries might occur as the repaired tissues have inferior mechanical properties as it is often described when scar tissue forms following tissue damage. Prolonged inflammation has been tightly associated with scar formation in several tissues, and recent data on human strain injuries support the idea that inflammation is present for an extended time after strain injuries.
This review provides some of the background on molecular and cellular processes during MTJ formation and during skeletal muscle and connective tissue repair. It summarizes the findings around fibrosis and the link between inflammation and fibrosis/scar formation. Finally, this review elaborates on the proximal hamstring tendinopathy and in which way a loading regime might contribute to healing.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
2.1 Overview of Structural and Cellular Components Affected by Strain Injuries
2.1.1 Insights into the Basics of Muscle Strain Injuries
Human skeletal muscle can be injured by strain, contusion, or direct laceration. The majority of sports-related skeletal muscle injuries are caused either by strain or contusion [1], as lacerations are almost nonexistent in sports. Hamstring strain injuries (HSIs) are a result of excessive intrinsic tensile forces and inflict substantial damage across myofibres, the myofibres’ basement membrane, as well as mysial sheaths and the connected tendon/aponeurosis. Additionally, strain injuries cause blood vessels in the endo- or perimysium to rupture during the trauma [4]. The injury is most commonly located at or adjacent to the myotendinous junction (MTJ) [2,3,4]. Both the proximal and the distal MTJs of the hamstring muscle group cover an extensive part of the muscles rather than a limited area at either end of the hamstring muscles. As an example, the proximal MTJ of the biceps femoris long head (BFLH) spans approximately a third of the total muscle length [5, 6], whereby the myofibres attach to the aponeurosis to transmit force from the BFLH muscle to the tendon. The proximal and distal aponeurosis is often also called the “central tendon” or “intramuscular tendon,” and it is noteworthy that the most severe hamstring muscle injuries involve the central intramuscular tendon, emphasising the role of the connective tissue in relation to HSIs [7].
A large number of different experimental animal models have been introduced over the years to enable the study of tissue repair following muscle injuries. In general, the biggest challenge lies in the development of a model which mimics the injury-causing mechanisms. With regard to muscle strains, the injury provoking impulse is excessive tensile strain. Pioneering work by Tidball and colleagues involved application of passive strain to isolated frog muscles and their attached tendons. This model demonstrated that the location of the tear is at the MTJ [3]. Similar observations were made by Garrett and colleagues reporting the injury site to lie within ~0.5 mm of the MTJ [4]. One of the most important findings relates to the failure site, which is located external to the myofibre cell membrane. This means that the basement membrane of the myofibres is torn off and leaves the myofibres separated from the normally attached connective tissue [3, 4].
The experimental model was later applied to whole frog semitendinosus (ST) muscle-tendon preparations while the muscles were stimulated [2]. In this setup, the failure site was also located at the MTJ where the collagen fibres from the associated tendon became torn off. The separated collagen fibrils are clearly seen on electron micrographs taken from the ST muscle-tendon unit (MTU) (Fig. 8 in [2]): The fingerlike processes from the muscular side of the MTJ are clearly visible, but after the strain injury, there is a detachment of the myofibres from the tendon. It is noteworthy that the muscle tissue appears organised with no detectable damage to the Z-lines, suggesting that the skeletal muscle tissue in itself is not greatly damaged.
Other animal models have focused on the ability of skeletal muscle tissue to initiate repair following complete transections of the soleus muscle at the muscle mid-belly (“laceration injury model”) [8,9,10], or by subjecting muscles to the forces generated by a spring-loaded hammer [11]. The complete laceration injury models showed how regenerating myofibres can enforce attachment to the extracellular matrix (ECM) on the lateral aspect of the myofibres, thereby increasing stability of the injured tissue during the healing. Findings obtained from the laceration injury models also show how the muscle-specific integrin receptor α7β1 expression as well as its distribution is involved in conferring stability between the myofibres and the ECM during regeneration [12, 13]. In general, integrin receptors enable the linkage of cells to the ECM (Fig. 2.3). More specifically, this cell receptor type couples the intracellular cytoskeleton to the specific binding partners in the matrix on the extracellular side. For the muscle-specific integrin receptor α7β1, the binding partner on the extracellular side is laminin (Fig. 2.1).
Schematic illustration of the muscle-specific integrin α7β1 and the binding sites on the laminin α2 chain. The integrin receptor α7β1 has a short intracellular part (in the cytoplasm) and an extended extracellular part, where integrin α7β1 binds to laminin via the laminin globular domains. (Reproduced with adaptation from Fig. 3 of Gawlik and Durbeej [14])
An increase, concomitant with a redistribution of the integrin receptor during the repair of muscle tissue, suggests the importance between the coupling of the myofibres and the surrounding matrix. Another important aspect of the laceration models in animal skeletal muscle is time: Studies applying these models reported that scars are not rapidly replaced but may persist over a prolonged time span, potentially permanently [15]. It is important to keep in mind that the muscle mid-belly is not a common site of failure in HSIs, and it is also somewhat difficult to compare results from a contusion injury to the repair processes of a strain injury. Further, even the application of excessive strain is applied under controlled conditions, where the MTU is stretched until failure with a steady strain rate [2]. This controlled and constant strain does not fully replicate the explosive hamstring movements, which precede an acute HSI. Another aspect to consider when dealing with animal models is the aspect of time, as animals grow and heal substantially faster than humans. Additionally, animals do rarely show signs of pain, which complicates the examination of functional deficits related to these injury models. Finally, the role of the central tendon in HSIs cannot be studied in models, as the tendinous inscriptions extending into the muscle belly are not described in animals.
2.1.2 Development of the Myotendinous Junction and Its Adaptation to Loading and Unloading
The most common localisation of strain injuries is the MTJ, which is the interface where the myofibres attach to the collagen fibres of the tendon [2, 16, 17]. Research into the adult human MTJ in general, and the regenerative capacity of the junction in particular, has remained scarce despite the fact that the MTJ is susceptible to strain injuries. In the optimal way, repair of the injured MTJ replicates the developmental processes to re-establish tissue integrity. The MTJ is a highly specialised anatomical region in the locomotor system, where force generated by the muscle is transmitted from the intracellular contractile elements of the muscle cells to the ECM proteins in the tendon. This linkage enables movement. On a functional level, the MTJ has to overcome a mechanical mismatch as the muscle is highly compliant, but the tendon, on the contrary, is a stiff tissue [18]. The consequences of connecting mechanically different tissues are strain concentrations, which increase the risk of injury. Local strains at the MTJ in the hamstrings can be modified when either muscular (e.g. change in cross section) or tendinous (e.g. change in stiffness) dimensions are altered [19]. Keeping in mind that the connection between different mechanical tissues is a challenge, it is noteworthy that the MTJ can repeatedly withstand high loads [20, 21]. To be able to do so, the MTJ presents with a highly organised structure connecting proteins and matrix from the subsarcolemmal cytoskeleton to the sarcolemma and the basement membrane of the final sarcomeres at the muscular side and then to the collagen fibres on the tendinous part of the MTJ. Both the organisation of the MTJ components and the involved molecules mediate the unique capacities of the MTJ.
The architecture of the adult MTJ is characterised by extensive folding, which results in a significant increase in the muscle-tendon contact area. Shown in rat MTJ development, the organisation of the junction undergoes substantial changes in the first days after birth. Right after birth, the MTJ has a smooth and even appearance, but already 2 weeks later, the junction is more complex, and folding becomes obvious. Following another 2 weeks, rat MTJ has deep recesses and the folding is extensive [22]. It should be noted here that these processes take considerably longer time in human MTJ development.
For a long time, these folds have been described as fingerlike processes, but new imaging techniques on the ultrastructural level in human adult MTJ revealed that the structures resemble ridgelike protrusions. Three-dimensional reconstructions of electron micrographs further showed that collagen fibres of the tendon condense and the tendinous collagen fibres expand into myofibrillar indentations [23]. Based on 2D images, it was postulated that the extensive folding increases the contact area approximately 10–20 times compared to an interface with smooth transitions from one tissue to the other, but these numbers are most likely significantly higher when taking the three dimensions into account (Fig. 2.2).
Electron micrograph of the human myotendinous junction (2D). Figure illustrates the marked folding and interdigitations at the contact area between muscle and tendon. (Reproduced with adaptation from Fig. 3 of Bayer et al. [24])
Functionally, the enclosure of tendon tissue (i.e. collagen fibres) around the myofibres might enable the “grab and trap effect” as discussed by Knudsen and colleagues [23]. The underlying mechanism is based on the mechanically stiff collagen fibres encasing the myofibres at the junction. When the muscle contracts, the myofibres shorten and become wider and the surrounding collagen fibres might reinforce the muscle-tendon connection, thereby improving force transmission. The tendon tissue covering the muscle, also termed “aponeurosis,” is specialised for force transmission from the muscle to tendon and then bone. Biomechanical analyses demonstrated that the aponeurosis has different mechanical properties compared to the free tendon [25]. Magnusson and colleagues showed that the free tendon had a significantly greater strain compared to the aponeurosis under isometric maximum voluntary contractions. The authors suggest that part of the observation reflects the energy storing and releasing capacity of the free tendon, while the aponeurosis is predominantly designed to effectively transmit contractile force at the MTJ [25].
The interaction between the myofibres and the aponeurosis/tendon during isometric contractions is relatively straightforward compared to dynamic situations such as those that occur during stretch-shortening cycle movements. During such movements the muscles are activated prior to the stretch to stiffen the contractile component so that the elongation during the stretch (braking) phase occurs predominantly at the tendon [26]. This provides elastic energy for the shortening (propulsive) phase. In this situation the contractile component (myofibres) is stiffer than the noncontractile component (tendon). However, the level of muscle activation and the length of the muscle fibres can affect the stiffness of the contractile component. At lower activations or longer muscle lengths, the contractile component may be less stiff than the noncontractile component and MTU elongation may occur at the MTJ as opposed to the tendon. With respect to hamstring injury, interrupted motor control and altered biomechanics during stretch-shortening cycle movements, such as sprinting, can place MTUs at lengths and tensions that can predispose them to injury.
The specialised organisation of the MTJ is mediated by a composite of molecules, which act in an orchestrated way during development and homeostasis. On the muscular side, an important protein complex responsible for force transmission from myofibres to the connective tissue is dependent on binding of intramuscular actin to the dystrophin group. Dystrophin at the intracellular part of myofibres is associated with a large oligomeric complex of sarcolemmal proteins and glycoproteins, also known as the dystrophin-glycoprotein complex. Force transmission is allowed through dystrophin binding to the C-terminal of β-dystroglycan. On the extracellular side, α-dystroglycan, which is anchored to β-dystroglycan, serves as a receptor for ligands such as laminin in the basement membrane surrounding myofibres [27, 28] (Fig. 2.3). At the MTJ, the dystrophin-glycoprotein complex is found at high concentrations to provide mechanical stability [29].
The dystrophin-glycoprotein complex composition in mammalian skeletal muscle. In skeletal muscle, β-dystroglycan is linked to the extracellular α-dystroglycan, which, depending on the tissue, links laminin α2 along the sarcolemma. In addition, β-dystroglycan associates with δ-sarcoglycan by which the sarcoglycan-sarcospan complex is stabilised at the sarcolemma. (Reproduced with adaptation from Fig. 1 of Pilgram et al. [30])
Another fundamental segment of the force transmission at the MTJ involves the binding of actin filaments within the terminal sarcomeres to associated “attachment” proteins. These proteins include α-actinin, talin, vinculin, paxillin, and tensin, and they bind to the intracellular β1-subunit of the receptor integrin α7β1 (Fig. 2.1). The transmembrane integrin receptor α7β1 is enriched at the MTJ and binds to laminin in the basement membrane [31]. It is important to note that laminin becomes incorporated in collagen fibres at the MTJ and thereby constitutes an integral part of the junctional ECM. A lack of integrin α7β1 causes abnormal MTJ morphology seen as a clear reduction of the characteristic folding at the MTJ as well as significant weakening of the muscle [32]. In the context of MTJ development, it is noteworthy that the appearance and accumulation of integrin α7β1 coincides with membrane folding and myofibril insertions during developmental stages and might therefore play a role in the very early steps of MTJ organisation [31].
The morphogenesis of the MTJ during embryonic development reflects the coordinated processes of chemical and mechanical signalling as well as the interdependence between myogenic cells and cells differentiating into the tendinous lineage. During development, tendon cells connect with the developing muscle at the MTJ, and the development is to a significant degree governed by the interaction of integrin receptors and ECM molecules secreted by both the muscle and tendon cells [33, 34]. The collagen type XXII (COLXXII) and its receptor binding serve as a good example of the interaction between muscle and tendon cells at the developing MTU and exemplifies the direct link between muscle and tendon tissue on a cellular and molecular level. COLXXII is a collagen subtype predominantly found at the MTJ; it belongs to the collagen subtype of “fibril-associated collagens with interrupted triple helices” (FACITs) and is expressed during development by undifferentiated muscle cells located next to the basement membrane [35]. At that stage, COLXXII expressing cells are in close contact with tendon cells (also called tendon fibroblasts or tenocytes). On the tendinous side, the cell receptors integrin α2β1 and α11β1 are expressed by tendon fibroblasts. Visualisation by the immunofluorescence technique clearly demonstrates co-localisation of COLXXII and α2β1 integrin as well as COLXXII and α11β1 [36]. This co-localisation means that COLXXII and the integrin receptors form a functional unity, which is a necessity for the development of the MTJ. The connection between COLXXII and its binding partners on the tendinous side is required for mechanical stability at the MTJ as the lack of COLXXII (tested by creating a genetic deletion of COLXXII in zebrafish) is associated with a significant decrease in muscle force. This force reduction did not seem to be a result of a defect of contractile elements within myofibres, and also, the basement membrane of the mutant animals remained firmly attached to the sarcolemma. The study of these mutant animals showed that the linkage between muscle fibres and the junctional collagen fibrils was disrupted, myofibres were detached from the MTJ, and the characteristic MTJ architecture of interdigitations was lost [37]. Importantly, COLXXII is identified not only as a part of the MTJ development but also expressed and localised to the myofibre edge at the adult human MTJs [38].
As COLXXII appears to be a key element in conferring mechanical stability to the MTJ, at least during development, it is natural to ask whether loading or unloading in the adult MTJ would affect COLXXII synthesis. This was tested in untrained men undergoing a training programme with heavy resistance exercises of the hamstring muscles for 4 weeks. The intervention did not induce any change in the synthesis or localisation of this collagen type [38], suggesting that COLXXII in the human adult MTJ is not, or only to a minor degree, load sensitive. It could, however, also be that 4 weeks of training was a too short time span to cause significant changes at the human MTJ. Whether COLXXII is affected by immobilisation in humans has remained unexplored.
Tenascin-C is another ECM protein at the MTJ expressed by fibroblasts on the tendinous side of the MTJ. It is a large elastic ECM glycoprotein, which can be stretched several times its resting length by mechanical loading [39]. Tenascin-C is involved in tissue morphogenesis, including tendon, and is load sensitive in the free tendon, the MTJ, and myofascial junction as well as in muscle connective tissue but not in skeletal muscle tissue [40]. Probably its best-known function relates to modulation of cell (de-)adhesion and mechanosensitivity [41]. The lack of mechanical force (generated by muscle contraction), as observed during cast immobilisation, leads to significant changes of tenascin-C expression: In an animal experiment, rat hind limbs were immobilised for 3 weeks and this intervention resulted in a dramatic decrease of tenascin-C at the MTJ and the free tendon. The downregulation of tenascin-C was, however, reversed when the rats were allowed to use their legs normally again. After 8 weeks of remobilisation, tenascin-C was re-expressed at the MTJ, the myofascial junction, and the free tendon [40].
Thrombospondin-4 is a subtype of the thrombospondins, a group of glycoproteins regulating protein-protein and protein-ECM interactions [42]. It serves as a key scaffolding protein mediating the organisation of the MTJ, which probably relates to its role in regulating the structure of collagen fibrils in connective tissues [43]. Thrombospondin-4 is expressed by both myoblasts and tendon fibroblasts and binds integrins through a specific motif (the “KGD motif”), thereby enabling specific cell-cell as well as cell-matrix interactions. Thrombospondin-4 deficiency causes dysfunctional integrin signalling and a disruption of the laminin network at the MTJ. Additionally, the lack of thrombospondin-4 caused muscle detachment from the tendon tissue, suggesting that this protein is a central element in structural and functional integrity, at least in the embryonic stage [33]. The role of thrombospondin-4 is unknown in the human adult MTJ and it is not known whether this molecule is load sensitive and involved in MTJ regeneration after injury.
Understanding of the complexity and the steps involved in the development of MTJ is essential in order to acknowledge the processes required for successful regeneration of the junction after HSIs. Although there is still much unknown about MTJ development, it is obvious that the communication between muscle and tendon cells is fundamental for the development of both tissues and the organisation of the linkage between the different tissues. A good example illustrating the dependency of the several tissues on each other is an avian animal model, in which muscleless wings were produced. In these animals, tendons formed early during development, but did not mature to form individual tendons and were subsequently degraded [44]. Thus, the proximity of muscle and tendon cells is crucial for correct MTJ formation and function. Although speculative, in the context of tissue repair after a strain injury, the separation of muscle and tendon caused by both granulation and scar tissue might hinder the propagation of signals from both tissues and complicate regeneration. MTJ regeneration therefore depends on the cells residing in skeletal muscle as well as cells within the tendon.
Importantly, the MTJ appears to be a very active region, and at least on the muscle side, adaptations to loading have been shown. A recent study on human MTJ samples reports the presence of multiple muscle fibres with central nuclei and positive immunostaining of CD56 [45]. The number of myofibres at the MTJ with central nuclei was as high as 43–50%, compared to 3% in the resting muscle belly of the vastus lateralis [46]. Both central nuclei and CD56 immunoreactivity (marker expressed by newly formed myofibres [47]) are signs of high cellular activity, and these findings indicate that the human MTJ is characterised by continuous remodelling. The authors further report that the number of fibroblasts at the MTJ was not different from the numbers in the muscle belly, but the activity status of these cells was not investigated. It should be noted that this study did not find any differences between MTJ samples from individuals subjected to 4 weeks of heavy resistance training targeting the hamstring muscles and a control group with no specific training. Thus, the loading per se did not seem to affect any of the characteristics measured in this study [45]. Human hamstring muscles subjected to both an acute bout of heavy resistance training and training for 4 weeks prior to tissue sampling at the MTJ demonstrated a higher expression of tenascin-C and the fibril-associated collagen type XIV in the muscle connective tissue, but no direct changes of these markers or any other factors analysed in the study were detected at the MTJ [38].
The architecture of the MTJ and potential changes to different types of training or immobilisation have not been examined in the aforementioned studies including human subjects. A study on rats showed, however, that training can cause modifications at the structural level of MTJs. These rats were subjected to 6 weeks of uphill running, and the percentages of branched interdigitations afterwards were significantly higher compared to a sedentary control group. The researchers specify that both the number and the length of the interdigitations increased in the trained compared to the non-running rats [48]. On the contrary, limb unloading led to a substantial decrease in the muscle-tendon interface seen as a substantial decline in the membrane folding relative to muscle fibre cross-sectional area at the MTJs of rats subjected to 4 days of space flight [49]. Interestingly, this study found an increase in fibroblast-like cells in the proximity of the MTJ of unloaded animals compared to control rats [49], suggesting there is a rapid cellular response to hypoactivity. The underlying mechanisms and the role of these cells are unexplored.
Besides a reduction in the protrusions, unloading, through either hind limb suspension or spaceflight, had an adverse effect on the organisation of the MTJ. The tendinous side was characterised by a more disorganised collagen fibril structure and the muscular side showed z-band disorganisation in myofibres [50]. Strikingly, the induction of exercise during unloading prevented the loss of membrane folding and even increased the complexity of the interdigitations [51]. Similar findings to rat immobilisation were demonstrated with MTJ samples obtained from patients after prolonged bed rest. The MTJ endings of these samples obtained from the lower leg showed a reduction in the protrusions compared to control samples obtained from healthy individuals [52]. It is important to note that all of these studies used 2D analyses and the response might be even more pronounced when using 3D image analysis.
2.1.3 Regeneration of Skeletal Muscle and the Connective Tissue
The study of regeneration following muscle strain injuries is complicated as these injuries predominantly occur at the MTJ [2,3,4]. It is therefore crucial to keep in mind that repair after HSIs does not exclusively involve the regeneration following myofibre necrosis (i.e. myofibre death); it requires the fusion across myofibres and, importantly, includes the attachment of myofibres to the tendon/aponeurosis to enable force transmission. One major factor driving rehabilitation is the timing of loading. A recent study investigating the effect of early compared to delayed loading after muscle strain injuries showed clearly that a delay in loading of damaged musculoskeletal tissue significantly prolongs return to sport (RTS) [53]. These findings underline the importance of mechanical stimulation of healing tissues and cells across different tissues.
Taking into consideration the animal model of strain injuries, one rather surprising finding is that the skeletal muscle tissue in itself does not appear to suffer from damage [2]. The myofibres adjacent to the rupture site have a regular appearance with an organised Z-line alignment, but the basement membrane is torn off and the connection to the connective tissue (tendon/aponeurosis) is lost [2, 3]. However, it is also important to remember that these findings are based on an animal model, and it is very likely that human hamstring muscle strains, as a result of explosive movements, may cause disruption of the MTJ concomitant with myofibre damage. The adverse impact of strain injuries on the muscle has been clearly demonstrated by studies reporting substantial muscle atrophy as a result of strain injuries [54, 55]. This could be due to poor myofibre regeneration, but also reflect the failed repair at the MTJ, meaning that the tight link between the muscle and the connective tissue/tendon/ aponeurosis may not fully reform after a strain injury. A lack of the firm muscle-tendon attachment will influence the mechanical properties of myofibres and tendon collagen fibrils. Further, the neuromuscular innervation might be negatively affected and thereby involved in the adverse long-term outcome of strain injuries on the involved muscle.
Skeletal muscle tissue has powerful regenerative potential, which relies on the activation of muscle stem cells, also known as satellite cells, due to their sublaminar location and association with the plasma membrane [56,57,58] (Fig. 2.4).
Schematic drawing of a longitudinal myofibre illustrating the sarcolemma (plasma membrane) and the basement membrane along with a satellite cell and several myonuclei. (Reproduced with adaptation from Fig. 15 of Mackey and Kjaer [58])
At steady state, the satellite cells are mitotically quiescent (G0 phase, meaning that these cells have reversibly left the cell cycle and do not divide), and they become activated through signals from a diseased or damaged environment. Activated (proliferating) satellite cells are referred to as myogenic precursor cells [59]. Strikingly, satellite cells can become stimulated even though they are located at the other end of a damaged myofibre [60]. Satellite cells are also motile, with an ability to migrate across basement membrane layers [61]. Within hours, several key myogenic factors (such as MyoD, desmin, myogenin) are expressed, and after a few cycles of cell proliferation, the majority of the myogenic precursor cells enter the myogenic differentiation programme. Following exit from the cell cycle, myogenic cells fuse with damaged myofibres or fuse with each other to develop nascent multinucleated myofibres. To avoid depletion of the satellite cell pool, satellite cells have the ability to self-renew by either asymmetric or symmetric division [59].
It is interesting to note that different types of muscles are associated with inherent differences in the activation and differentiation potential of satellite cell subpopulations [62]. The regenerative potential of satellite cells residing in the human hamstring muscles have been investigated far less extensively compared to the quadriceps muscles; therefore, the myogenic repair potential in human hamstring muscles remains somewhat unexplored. A study including both hamstring and calf strain injuries found no differences between the muscle groups in functional or structural recovery after strain injuries [54]. These findings argue against a poor myogenic potential of hamstring muscles. Additionally, when the number of satellite cells was determined in human tissue samples from the hamstring muscles, the number of 0.12 satellite cells/fibre reported is comparable to ratios calculated in other muscles [45]. Therefore, it is more likely that the nature of the strain injury and the different tissues affected prolong or even impede complete tissue healing.
It is noteworthy that the ECM appears to play a key role in the repair of myofibres after injury. This hypothesis is supported by several studies on focal muscle damage, showing that necrotic (“dying”) myofibres require an existing basement membrane [58, 63]. This means that the matrix encasing the myofibres serves as a scaffold and orientation/ guidance for satellite cells to restore damaged myofibres [58] (Fig. 2.5). Thus, the preservation of the basement membrane is a central element in successfully regulating the regeneration after injury.
Schematic drawing of a regenerating myofibre after experimentally induced muscle damage. (a) shows the regenerating myofibre with the basement membrane as a scaffold/orientation for inflammatory cells and myoblasts during repair. Note that the fibre is devoid of a sarcolemma. (b) Illustrates an intact myofibre for comparison. Both sarcolemma and the basement membrane are present. (Reproduced with adaptation from Fig. 15 of Mackey and Kjaer [58])
Experimental animal data indicate that the basement membrane after a strain injury is not retained [3, 64], which probably hampers or even prevents complete repair of damaged muscle tissue as a result of strain injuries. In animal models in which the muscle, along with the basement membrane, was severely damaged, the injured skeletal muscle forms a nonfunctional scar tissue between the ruptured skeletal muscle fibres and the regenerating myofibres [15, 65]. The newly formed myofibres were poor at expanding within the granulation tissue and it can be hypothesised that the damage to the basement membrane scaffold hindered myofibre expansion. These animal models report a failed repair process in which the ruptured skeletal muscle fibres remain separated by the scar. As the defect was still evident 12 months after the trauma, the observation strongly indicates that the scar is permanent.
It is interesting that the integrin subtype α7β1 (Fig. 2.1) appears to play an important role also in the regeneration of myofibres following the rat model of complete muscle transection [12]. There was both an increase in the expression of integrin α7β1 within the regenerating muscle fibres and a dynamic redistribution during regeneration [12]. However, the presence of an intact basement membrane is also required to establish firm adhesions between the intracellular cytoskeleton and the matrix. Another interesting result was that the redistribution of integrin α7β1 to the lateral sarcolemma during skeletal muscle tissue repair only occurred if the injured muscle was mechanically stimulated [10, 12, 66]. This observation suggests the requirement for injured tissue to be put under loading and could be one part of the explanation why athletes who commence rehabilitation early after injury recover faster compared to those who have a period of rest [53]. Given the crucial role of integrin α7β1 in MTJ development, it seems plausible that this integrin subtype is involved not only in myofibre regeneration but also MTJ repair. It is, however, unknown how integrin α7β1 binding is re-established when the basement membrane is absent as demonstrated in muscle tissue put under excessive strain.
In relation to the regenerative capacities of the human MTJs in hamstring muscles, none of the key factors involved in MTJ development have been investigated following HSIs. This means that following hamstring strains the sequence of expression and the localisation of key molecules, such as integrin α7β1, COLXXII, tenascin-C, and thrombospondin-4, are unknown. Moreover, there is a lack of studies on the multiple cellular components at the MTJs and their interplay after an injury. Finally, it has remained elusive whether the characteristic junctional organisation of complex ridgelike tendon protrusions into the muscle tissue is re-established after disruption near or at the MTJ.
The reconnection of myofibre-connective tissue junction and the reformation of the specialised architecture at the MTJ to withstand the high stress put on the tissue probably pose the greatest challenge in repair after strain injuries. The basement membrane of myofibres emphasises the role of the matrix in repair, and it can further be hypothesised that the tendon matrix on the tendinous side of the MTJ limits regeneration. Recently, the intramuscular tendon of the BFLH has gained increased attention in the clinic as time until successful RTS was substantially prolonged when the intramuscular tendon was injured [7]. Additionally, the risk of recurrence might be increased when this tendinous structure is affected, although there are conflicting findings about the association between the intramuscular tendon and the re-injury risk [7, 67]. These findings support the idea that the connective tissue and its regenerative capacities play a decisive role in the repair of strain injuries and the severity of HSI is greatly aggravated when a larger part of the connective tissue structures is involved.
Unlike skeletal muscle, human tendons do not have great regenerative potential. Human tendon tissue has a very slow turnover [68, 69] and tendons contain a low number of cells [70]. Acute tendon ruptures show ongoing signs of repair up to 1 year after the trauma [71] and chronic overuse injuries of tendons cause symptoms and inferior tendon function for a long time, in some cases several years [72, 73]. Cells residing in tendons are generally described as fibroblasts, which are non-haematopoietic, non-epithelial, non-endothelial cells. These cells are arranged in between collagen fibrils along the direction of strain and have an elongated morphology. Tendon fibroblasts are also found in the interfascicular space [74].
Even though tendon fibroblasts are presumably terminally differentiated cells, they still can adapt to the environment, e.g. when mechanical stimuli are withdrawn: when placed in an unloaded environment, tendon fibroblasts shift towards an inflammatory phenotype [75]. These findings are supported in similar experiments which showed that unloading causes catabolic (i.e. negative) adaptations [76, 77]. These findings may have clinical implications when it comes to regeneration at the MTJ after HSIs. As the tendon/aponeurosis is supposedly being torn off from the muscle in a strain injury [2, 3], the collagen fibrils as the basic element of tendon/aponeurosis will become unloaded and influence cellular processes. Thus, a potential shift towards an inflammatory, catabolic phenotype has potentially a dramatic negative impact on the capacity of the tendon/aponeurosis to activate a repair process following muscle strain injuries [64]. It should be noted that stem cells have been identified in adult tendons and that these cells would also require the proper mechanical stimuli, which are presumably not present after a traumatic strain injury [33]. In general, whether and how tendon stem cells are activated in response to human musculoskeletal injuries remains unknown.
Besides the low number of cells present in the tendon, another factor contributing to the limited connective tissue repair might be the poor vascularisation of tendon tissue [78, 79]. Revascularisation of the injured area is a vital process in tissue regeneration; it is one of the first signs of regeneration and a prerequisite for subsequent morphological and functional recovery of the injured skeletal muscle and connective tissue [80, 81]. As the MTJ is a key area through which blood supply to the tendon is provided [78], the restoration of vasculature after a strain injury in this anatomical area is crucial.
Although there are no studies investigating the impact of hypoxia following hamstring strains, intra- or intermuscular hematoma formation [17, 54, 82, 83] is a sign that there is significantly impaired oxygen and nutrient supply. In addition, recent samples of muscle strain hematoma in athletes showed a substantial release of the pro-angiogenic factor vascular endothelial growth factor-A (VEGF-A) over a prolonged period post injury [84]. The growth factor VEGF-A represents a key element in angiogenesis and is one of the target genes of the major transcription factor induced by hypoxia, hypoxia-inducible factor-1α. New formation of capillaries provides the regenerating area with an adequate supply of oxygen and nutrients, which are necessary for energy metabolism for the regenerating myofibres [80] and cells residing at the tendinous part. Whether the vascular supply is completely restored at the injured MTJ remains unknown, as whether the vascularisation of the tendon through the MTJ occurs following this type of injury has not been explored. A recent examination of tissue perfusion following muscle strain injuries reported that there is an increased tissue perfusion for at least up to 6 months post injury [54]. Interestingly, early mobilisation following a crush injury in rats had a positive effect on sprouting of capillaries [80], which supports the recommendation of early loading after injuries [53]. It should be, however, remembered that the response regarding neovascularisation after a HSI might be very different to capillary growth after mid-belly contusion.
Successful regeneration would mean a replication of developmental stages of MTJ formation and data are scarce on this topic, especially in relation to the human MTJ. It is complicated by ethical and anatomical considerations, as it is questionable whether repeated tissue samples should be obtained from patients after a strain injury. Additionally, the MTJ is a very discrete area in the musculoskeletal system, and it would require elaborate equipment and techniques to obtain representative tissue samples.
Finally, another important aspect of regeneration following HSIs is innervation. Even though there is a lack of data on the human neuromuscular junction (NMJ) in general, and the extent to which innervation and NMJs are affected in HSIs, weakness along hamstring muscle length and reduced muscle activation are reported [85, 86]. These observations suggest that neuromuscular adaptations following hamstring strains could be negatively affected. In an animal model applying complete transection of the rat extensor digitorum muscle, the denervated, severed muscle stumps become reinnervated via penetration of new axon sprouting through the connective tissue scar and the formation of the new NMJs [87]. The presence and distribution of NMJs at the interface between the muscle and the tendon/aponeurosis in the human hamstring complex has remained unexplored, and it is therefore difficult to speculate how neural innervation, in general, and the NMJs, in particular, are affected by strain injuries. It is, however, obvious that the presence of a fully restored basement membrane is a prerequisite for functional NMJs [88].
In summary, a hamstring strain is a complex traumatic injury, which does not only affect skeletal muscle but also, and probably even more, the connective tissue in the muscle and the attached tendon/aponeurosis. In the vast majority of strain injuries, the MTJ is damaged, a tissue junction, which is designed to withstand high loads. During development, the coordinated signalling from both muscle and tendon cells ensures MTJ formation. Loading of the MTJ appears vital for maintaining its unique structure and, most likely, its function. The adult human MTJ is a very active region with significant potential for remodelling. The regeneration of the MTJ in athletes suffering from a hamstring strain has remained largely unknown; from a clinical standpoint it is obvious that the greater involvement of connective tissue (i.e. the central tendon) complicates healing. This emphasises the importance of focusing rehabilitation techniques on both muscle and connective tissue stimulation. As immobilisation of the MTJ has detrimental effects, early loading onset after the hamstring injury probably contributes to improving stability of damaged MTJ components post injury.
2.2 Hamstring Injury Sequelae
2.2.1 Structure and Cellular Components of Scar Tissue
Subsequent episodes of pain and re-injury following hamstring strains are frequent and mainly affect the same region as the index injury [89, 90]. Despite the high prevalence, the underlying causes and mechanisms behind the recurrent injuries have not been extensively studied in sports medicine. As re-injuries mostly happen within the first year, and in more than half of these injuries, within the first 25 days after the index injury [90], it can be hypothesised that (1) the repair after the HSI is not completed when the hamstring muscles are fully loaded, or (2) the repaired tissue does not withstand the high loads placed on the injured tissues, or (3) a combination of incomplete healing and mechanically immature repair tissue. In general, there are very few tissues in adult humans that heal by a complete regenerative response, synthesising a tissue identical in structure and function to what it was pre-injury. Mostly, damaged tissue is replaced by structurally and functionally inferior material.
Strain injuries are associated with the formation of scar tissue [55, 91]. Generally, the development of scars refers to the formation of excess fibrous connective tissue in a tissue or organ as a result of prolonged reparative or reactive processes [92]. In the context of HSIs, the formation of scar tissue might hamper the cross-talk between muscle and tendon cells and hypothetically cause the muscle or, more precisely, the myofibres to be permanently disintegrated from the normally attached tendon/aponeurosis. Whether this separation is transient or permanent is currently not known, but there is accumulating evidence that fibrotic tissue is a long-term pathological outcome following muscle strain injuries. Animal models also suggest that the scar tissue is permanent [15].
The initial response to a traumatic injury such as muscle strains is the formation of granulation tissue. Granulation tissue can also be viewed as a provisional matrix comprised of newly formed loose connective tissue filling any gap caused by tissue disruption. It is an evolutionarily conserved process aimed at the reconstitution of tissue integrity promptly after injury [93]. Granulation tissue is rich in the ECM components, fibronectin, tenascin-C, as well as collagen type III, and is mainly synthesised by (myo-)fibroblasts [94,95,96]. Tenascin-C is deposited early during the healing phase to provide elasticity to the granulation tissue to withstand the strains placed on the transient scaffold [97]. Tenascin-C is furthermore involved in the formation of an adhesive environment, which is favourable to cells and acts as a chemokinetic agent [98]. During optimal repair progression, fibronectin and collagen type III are sequentially replaced by collagen type I [99, 100]. This transition in collagen types improves mechanical stability, to a large extent due to the formation of multiple intrafibrillar cross-links in collagen type I [101]. Regarding very early recurrent hamstring injuries, it can be speculated that the strength of the provisional granulation matrix after the strain injury is not mechanically stable enough to allow for explosive movements when commenced too soon after the injury.
On the cellular level, myofibroblasts are the main cell type in granulation tissue, along with a myriad of other cell types, including inflammatory cells, fibroblasts, endothelial cells, and pericytes. Myofibroblasts belong to a specialised group of fibroblasts and their activation involves multiple factors. The two predominant stimulants are transforming growth factor-β1 (TGF-β1) and high matrix stress/stiffness [102]. Additionally, the presence of a splice variant form of fibronectin, ED-A fibronectin, seems to be required for myofibroblast differentiation [103]. Myofibroblasts express α-smooth muscle actin, and the organisation of α-smooth muscle actin into stress fibre-like bundles provides cytoskeletal characteristics of contractile smooth muscle cells. Thus, myofibroblasts can actively contract and remodel the granulation tissue, a process by which scar tissue is stabilised at least during wound healing after skin lesions [102,103,104]. How granulation tissue develops into scar tissue and how the scar is resolved following hamstring strains remains unknown. At this point, it should be remembered that a stable and organised ECM is pivotal to withstanding the high mechanical loads, for example, when the MTJ is subjected to explosive movements. Therefore, the sequence of ECM remodelling appears to be a major player in determining successful or ineffective repair. In the context of HSIs, failure to fully repair might be reflected in increased recurrence.
In successful repair, the myofibroblast-driven contraction of granulation tissue halts and tissue integrity is re-established. Further, concomitant processes such as angiogenesis, which is an integral part of the healing process, cease and myofibroblasts become apoptotic resulting in a largely avascular tissue [105]. However, the observation of fibrotic tissue following HSIs suggests that complete tissue restoration is not accomplished. So far, fibrotic tissue resulting from hamstring strains has only been demonstrated by magnetic resonance imaging (MRI), and therefore, the structure and composition of scars in human athletes remained unexplored. Recently, some insight into the long-term scar tissue has been gained through biopsies obtained from muscle strain injuries, which occurred at least 6 months prior to sampling. These biopsies clearly show high cellularity among disorganised connective tissue, adipocytes interspersed with myofibres, as well as the presence of large blood vessels (Fig. 2.6). The human samples furthermore clearly reveal the absence of any structured interface between myofibres and tendon/aponeurosis. These findings emphasise that scars are in fact highly active regions instead of inert, avascular structures, at least in musculoskeletal tissue, indicating that scar formation and development are tissue dependent. A similar picture was recently gained from the myocardium after a myocardial infarct where the scar is highly populated with cells a long time after the injury with signs of continuous reorganisation of the injured tissue [106].
Human biopsy material from strain injuries, haematoxylin-eosin staining. (a–c) Samples are taken at least 6 months after a strain injury. (a) Longitudinal myofibres are interspersed with adipocytes. (b) Scar tissue shows disorganised connective tissue, substantial accumulation of adipocytes, and blood vessels [54]
The question that remains is whether the presence of scar tissue is associated with an increased risk of recurrence. Despite the scarcity in observations related to HSIs, it is fair to say that scar tissue always replaces functional tissue with potential dramatic consequences on function. From other tissues and organs such as the heart or lung, it is known that scars significantly alter cardiac muscle extensibility and impair lung expansion as well as gas diffusion [106,107,108].
No association between MRI diagnosed fibrosis and recurrent hamstring injuries was reported during a 1-year follow-up period [91]. Interestingly, a study by Silder and colleagues [109] reported higher tissue strains in previously injured hamstrings during lengthening contractions. Their data suggest that the repaired tissue is more compliant compared to healthy uninjured hamstrings and might infer that force transmission at the MTJ in injured hamstring injuries is substantially altered. The presence of scar tissue following a HSI changes the mechanical properties, but whether this has other functional consequences would depend on the size, the maturation, and the organisation of the scar. Additionally, the connection between the myofibres and the scar is a critical factor to the function of the reformed transition area and ultimately the risk of recurrence.
An additional clinical concern is that scar formation at the injury site may result in adverse neural tension. While there is limited research on the topic, a high prevalence of neural tension was reported in a small sample of athletes with prior hamstring strains [110]. Adverse neural tension may contribute to weakness with the hamstrings in a lengthened position [111], and since athletes with prior hamstring injuries are prone to weakness at longer muscle lengths, it may be important to assess for adverse neural tension to optimise treatments [112].
2.2.2 The Inflammation-Fibrosis Link and Its Potential Role in Scar Formation After Strain Injuries
The development of fibrotic tissue is associated with prolonged inflammation [113,114,115,116,117]. It can therefore be anticipated that there is a relationship between inflammatory processes after a HSI and the pathobiological fibrotic changes described in athletes suffering from a hamstring strain [91, 118]. It is, however, important to note that there are no studies investigating this direct relationship. A recent investigation of human muscle strains included a surrogate marker of inflammation and reported long-term increases in perfusion of the injured tissue indicating that inflammation persists for at least 6 months post injury [54].
After a traumatic injury, the inflammatory response often starts with activated platelets during coagulation following the rupture of blood vessels. Activated platelets change shape and secrete the contents of their granules, which involve, among various other factors, cytokines and chemokines to promote activation of inflammatory processes [119, 120]. Further, a major factor driving the sterile (nonpathogenic) inflammatory response is the presence of necrotic (“dying”) cells and cell debris belonging to the endogenous damage-associated molecular patterns (DAMPs). DAMPs, which can also be damaged ECM proteins; proteoglycans, which were released from the ECM; and stress-induced proteins are recognised by the innate immune system through cell receptors such as the toll-like receptors, RIG-I-like receptors, NOD-like receptors, and C-type lectin receptors [121, 122]. When danger signals are sensed, intracellular signalling cascades are activated, of which the nuclear factor-κB (NFκB) pathway is considered one of the key activators of pro-inflammatory responses in macrophages, neutrophils, and mast cells [123]. The immediate response to NFκB activation involves the induction of pro-inflammatory cytokines such as IL-6, IL-8, TNF-α, and adhesion molecules [124, 125].
Inflammatory cells multitask at the wound site by facilitating wound debridement and producing chemokines/cytokines, metabolites, and growth factors needed for tissue repair. At the same time, inflammatory cells also release matrix metalloproteinases (MMPs), which are enzymes involved in the degradation of matrix proteins and could therefore contribute to further damage of the ECM [126]. While research on mechanisms associated with acute pro-inflammatory processes has been extensive, there is still much unknown about the resolution of inflammation and concomitant tissue remodelling, at least for musculoskeletal injuries. It is, however, obvious that failed resolution of inflammation is linked to tissue hyperplasia and scar formation [127, 128]. Resolution of inflammation is tightly associated with the function of anti-inflammatory macrophages and the factors that these cells synthesise and release. Additionally, the termination of the acute inflammatory response is regulated by active processes synthesising endogenous lipid factors that are both anti-inflammatory and pro-resolving [129, 130]. Resolution is therefore an active rather than a passive transition which affects inflammatory cells but also non-myeloid cells.
Monocytes can adopt very different phenotypes, crudely divided into “pro-inflammatory” and “anti-inflammatory” macrophages. Readers should, however, keep in mind that the separation into “pro”- and “anti”-inflammatory macrophages represent only two phenotypes in a wide and still evolving spectrum of macrophage polarisation. Pro-inflammatory macrophages are induced by cytokines interferon-γ and IL-1β and release high amounts of the pro-inflammatory cytokines TNF-α, IL-1β, IL-6, IL-12, and IL-23, as well as with reactive oxygen species (ROS) and nitric oxide (NO) [125, 131, 132]. The pro-inflammatory macrophages are mainly involved in phagocytosis of necrotic cells, whereas anti-inflammatory macrophages are prominent regulators of tissue repair and regeneration and thereby linked to inflammation resolution, tissue remodelling, and angiogenesis. This set of macrophages is stimulated by IL-4 and IL-13 and produce IL-10 as well as the TGF-β1 [125, 132,133,134].
Inferior tissue healing is associated with the presence of anti-inflammatory macrophages, which continue to synthesise and secrete growth factors [125]. A key growth factor in this context is TGF-β1 which is pivotal in the activation of myofibroblasts, a prominent cell type modulating the formation of fibrotic tissue [102, 135] (see also Sect. 2.2.1, page 45). Further, TGF-β1 stimulates the synthesis of ECM proteins [136, 137] and might thereby contribute to the accumulation of excessive connective tissue. Additionally, macrophages are sources of transglutaminases, which are enzymes involved in collagen cross-linking [116], and macrophages themselves play a major role in activating the fibroblast-to-myofibroblast transition [138].
It might therefore appear beneficial to dampen the inflammatory processes after injuries such as hamstring strains, but it is important to remember that interfering with inflammatory processes at any stage will not necessarily lead to improved tissue healing. The role of inflammation on healing of the MTJ after HSIs is unknown, but in skeletal muscle repair, pro-inflammatory macrophages stimulate the proliferation of myogenic cells besides their role in phagocytosis of damaged myofibres [139]. The next sequence in muscle repair is the skewing of pro-inflammatory to anti-inflammatory macrophages which stimulate the myogenic cells to fuse to become new myofibres [140]. Interfering with either the pro-inflammatory or the anti-inflammatory cascade leads to impaired tissue regeneration, emphasising the importance of an orchestrated inflammatory process [141, 142]. Also, in relation to connective tissue, the interference with the anti-inflammatory pathway has adverse effects. Whereas the deletion of a major anti-inflammatory factor (IL-10) speeded up skin wound healing, the long-term response was the development of a disorganised matrix with excessive collagen deposition [128]. In another study, the deletion of IL-4 receptor α, a major factor involved in anti-inflammatory macrophage activation, led to impaired wound healing as a result of a failure of macrophages to initiate successful repair [143]. Another adverse outcome to the inhibition of inflammation was also described in tendon ruptures, where treatment in the very early phase after the trauma resulted in impaired mechanical properties. Noteworthy, dampening of inflammation at a later time point improved material properties [144].
However, the suppression of inflammation following hamstring injuries might be adjuvant to the recovery and the reduction of scar formation, in particular since tissue resident cells can become activated by persistent inflammation [145] and change their cellular behaviour [146, 147]. But given the fact that inflammation and the resolution thereof are considerably complex, it is difficult to determine a certain time frame, during which it would be beneficial to blunt inflammatory agents.
In conclusion, scar formation following traumatic injuries is a pathobiological consequence in many tissues. Following hamstring strains, scars have been visualised and tissue samples suggest that the fibrotic regions are characterised by high a cell number and disorganised connective tissue. Additionally, adipocytes accumulate at the injured site, a process which might contribute significantly to changes in mechanical properties post injury. Observations reporting altered tissue strain after hamstring injuries in human subjects have been made, but there is little data in this field. Scar formation involves a myriad of cellular processes, and it is tightly coupled to persistent inflammation. Whether this is the case in HSIs remains speculative. An important yet under-researched area in the musculoskeletal field is the effect of mechanical loading on the structure and function of scar tissue. One perspective of early onset of loading followed by appropriate load progression might be to stimulate the granulation tissue and later scar tissue optimally to improve strength and stability of the repair tissue.
2.3 Proximal Hamstring Tendinopathy
2.3.1 Pathological Changes in Tendinopathy
Overuse of hamstring tendons is, in most cases, confined to the origin of the hamstring tendons, i.e. the proximal site. Therefore, this paragraph will only discuss the proximal hamstring tendinopathy (PHT). The reader should note that the literature is very limited, and thus, studies of tendons other than PHT are discussed. Tendinopathy is an umbrella term for non-rupture tendon overuse injuries, which cause symptoms such as soreness, pain, swelling, and dysfunction. In contrast to acute, traumatic injuries such as the hamstring muscle strain, tendinopathy is a chronic condition with a gradual onset. Tendinopathy is very common, but the injury aetiology has remained somewhat elusive. The development of tendinopathies is associated with repetitive exposure to both a magnitude and volume of loading that exceed the physiological capacity of the tendon and can be viewed as a repeated disturbance of tendon homeostasis [73]. In other words, overuse injuries emerge as a result of the inability of tendons to keep up with the synthesis of key components constituting the tendon matrix. A fundamental question that has remained unanswered is what defines “healthy” loading leading to tendon adaptations and “excessive” loading resulting in degeneration, pain, and functional impairment. Similar to tendinopathies in other anatomical sites, the PHT appears to be caused by overuse as hardly any non-athletes suffer from chronic injuries of hamstring tendons [148]. Benazzo and colleagues reported that approximately 50% of injured hamstring tendons affect the biceps femoris tendon, 30% the semimembranosus, while the ST appears to be the least affected [149].
Knowledge of structural features of human tendinopathic tendons at the tissue level is predominantly based on samples obtained from chronically injured patella or Achilles tendons [150,151,152,153]. Characteristics of chronic histopathology include disorganised collagen fibres, an increased amount of blood vessels, and ingrowth of sensory nerves [154,155,156,157]. Other histopathological signs of tendinopathic samples show an increase in collagen type III, areas devoid of cells [158] indicating cell death and/or cell migration towards other parts of the tendon, as well as areas of hypercellularity [159]. Fibroblasts in healthy tendon have long extensions projecting into the matrix and through which these cells can communicate with each other. These cellular extensions are absent in tendinopathic tendons, and further, cells lose their tight contact with the ECM. This means that the tight link between the cell and the matrix is disturbed. Lastly, instead of longitudinally extended nuclei which are aligned along the axis of tension, tendon cells in chronically injured tendons have misshaped, more rounded cell nuclei [151].
Histological analysis of samples obtained during surgery for PHT revealed very similar characteristics compared with the aforementioned findings in the Achilles or patella tendons. Samples were collected from human patients with a gradual onset of symptoms at the proximal hamstring origin [160]. These tendons revealed a disorganised collagen matrix, a rounded shape of cell nuclei, and an increase in blood vessels. Further, an increase in mucin (heavily glycosylated proteins) ground substance was seen along with some adipocytes within the tendon matrix. None of these pathological signs were observed in the healthy hamstring tendon control sample [160].
In an early model presented by Gross [161], repeated cycles of injury, inflammation, and repair are suggested to result in the development of poor-quality tissue with inferior mechanical properties. Whether inflammatory events are involved in the development of tendinopathy is a matter of ongoing discussions, but there is accumulating evidence that inflammation plays a role in the early stages of tendinopathy [162]. It is interesting to note that there seems to be an association between the increased number of inflammatory cells and enhanced fibroblast cellularity in early tendinopathic tendon [162]. This suggests an interplay between several cell types in the early events of tendon overuse injury. It is also important to keep in mind that the tendon resident fibroblasts can adopt an inflammatory phenotype depending on the biomechanical environment [75].
Catabolic events that might be involved in the development of tendinopathy include MMPs which digest and degrade connective tissues. These enzymes are separated into four clusters based on their substrate affinity. One important group of MMPs in tendon disorders is the collagenases, i.e. MMP1, MMP8, and MMP13, which degrade fibrillar collagen and are responsible for the balance of collagen synthesis and degradation. Important to keep in mind is that MMP activity is the complex product of synthesis, activation, inhibition, and degradation; an upregulation does not necessarily translate into higher activity. In tendinopathic tendons, MMP1 and MMP13 were found to be upregulated [163], suggesting that there is an increase in remodelling of the tissue. This is supported by a recent study reporting a higher collagen turnover in tendinopathic tissue compared to healthy control tissue [164]. Whether this shift towards more rapid collagen remodelling is also evident in PHT is unknown, yet very likely.
In the more chronic state, tendinopathy has been described as a degenerative process devoid of inflammation. This long-held theory has recently been challenged as inflammatory cells were found in samples from chronic tendon disorders. These cells revealed a complex inflammation signature, which involves the pro-inflammatory interferon, NF-κB, STAT-6, and the glucocorticoid receptor pathways. At the same time, cells in tendinopathic tendons express markers such as CD206 and CD163, which are linked to the alternative inflammatory pathway, suggesting chronic inflammation and ongoing repair processes [146]. Inflammatory cells were also found in chronic Achilles tendinopathies, but it should be noted that healthy control samples also revealed the presence of inflammatory cells such as CD3-positive T-lymphocytes, CD56-positive natural killer cells, and mast cells [152]. In healthy tendons, the number of the inflammatory cells was, however, lower compared to the chronically injured samples. Another study on chronic tendinopathy showed an increase in members of the IL-6 family, indicating ongoing inflammatory processes, but strikingly, the increase in IL-6 was only detectable in the chronically injured Achilles tendon and not the posterior tibialis tendon [165]. This suggests that there might be differences in cellular responses depending on the tendon. Whether or not inflammatory cells play a role in PHT is unknown due to the lack of data on inflammation in PHT.
2.3.2 Cellular Adaptations to Loading and Unloading in Tendon: How Is Mechanical Loading of Tendons Associated with Healing Processes?
Rehabilitation of chronic tendon injuries involves loading-based interventions, in most cases slow and heavy resistance training. These rehabilitative measures have been shown to alleviate pain and promote tissue healing [150, 166]. In particular, regular eccentric training with high loads has been associated with improvements of tendinopathic tendons [167]. Also for PHT, recommendations include eccentric hamstring strengthening [148]. There is, however, very little research on the effectiveness of loading regimes and PHT. Although the eccentric strength training has been viewed as the treatment of choice, other rehabilitation regimes such as heavy slow resistance training with both the concentric and the eccentric phase result in pain reduction and improved function [166, 168], although not specifically for PHT. Further, static (isometric) training has been suggested to improve chronically injured tendons; with greater acute pain reduction after isometric exercises than that after isotonic exercises [169, 170].
Strength training not only improves symptoms of tendinopathic tendons, but also on a structural level, slow, heavy resistance training led to a normalisation of collagen fibril distribution in human samples obtained from tendinopathic patellar tendons [150]. The cellular mechanisms underlying the positive adaptations to heavy loading have remained elusive, but it is important to note that mechanical loading in general is essential for tendon development, homeostasis, and repair.
Short-term strength training of healthy tendon tissue upregulates mRNA for collagen types I and III as well as tendon regulatory factors such as insulin-like growth factor I, TGF-β, and connective tissue growth factor, as well as cross-link forming enzymes. Interestingly, the response was similar regardless of whether the loading regime was based on isometric, concentric, or eccentric muscle contractions [171, 172]. These findings indicate that tendons respond to loading but do not distinguish between different contraction types, which is also supported by another study reporting nearly identical anabolic responses to any of the contraction modes [173]. Whether the picture is similar in human tendinopathic tendon is somewhat unexplored.
The abovementioned studies were performed on rats, and although human tendons show an upregulation of collagen following loading regimes, the response is far more moderate compared to animals [174]. Further, the anabolic response might differ dramatically in tendinopathic tendons, but despite these considerations, it is important to remember that mechanical loading has clear beneficial effects on chronically injured tendons. In tissues other than tendon, mechanical loading of scars can profoundly modify the structure of scar tissue [106, 107]. It is therefore likely that mechanical stimuli can have an impact on collagen fibril structure in tendinopathic tendons including the proximal hamstring tendons.
In the clinic, the beneficial effect of different loading regimes has been repeatedly demonstrated, which raises the question of how tendon fibroblasts in chronically injured tendons sense and translate the mechanical signals to promote tissue healing. One key factor might be the alignment of collagen fibres, as tendon fibroblasts are tightly bound by specific receptors to the collagen matrix. Any change in the organisation of the collagen fibrils inside the tendon will simultaneously affect the tendon cells. This was clearly demonstrated by a dramatic and rapid shift in receptor binding as a result of unloading of a collagen-rich matrices [75, 175]. This means that the cells within the collagen-rich matrix rapidly react to the change in the mechanical environment (i.e. the unloading) and modify the way by which they bind through cell receptors to the matrix.
The strict parallel alignment and the elongated shape of tendon fibroblasts have clearly been shown to promote the expression of tendon cell markers and the expression of collagen type I [176]. Misaligned collagen fibres, random orientation, and the adaptation of a rounded cell shape are features of tendinopathy and have detrimental effects as tendon fibroblasts switch on matrix degradation pathways [177]. Thus, the application of tensile load to the injured tendon through slow muscle contractions might stretch the collagen fibrils and cells and thereby initiate anabolic responses, such as collagen expression, upregulation of integrin receptors, and induction of growth factor signalling [73, 178]. It is important to note that during heavy and slow muscle contraction, the speed of the movement and the magnitude of loading (strain) that the matrix and the cells are subjected to are fundamentally different compared to injury provoking conditions such as running and jumping.
The positive effects of mechanical strain on the degenerative tendon matrix and the tendon fibroblast might reflect the concept put forward by Arnoczky and colleagues [76, 77]. In contrast to the belief that tendinopathy is an overloading of tendon cells, they suggest that pathological changes in tendinopathy are a result of under-stimulation of tendon fibroblasts [77, 179]. An in vitro study on tendons revealed how tendon cells react to stress deprivation; 48 h of unloading caused tendon cells to upregulate MMP13, an enzyme which degrades fibrillar collagen leading to a weakening of the tendon matrix. Unloading for 48 h caused further detachment of the tendon cells from the collagen matrix, which suggests the loss of cell-matrix adhesions [76]. The underlying mechanisms for this hypo-stimulation could be a focal overloading of the tendon matrix, subsequently leading to micro-damage of collagen fibrils and/or a reduction in their stiffness. This change in mechanical properties of the collagen fibrils translates into a reduction of the mechanical load on the tendon cells. Thereby, the complete linkage from the matrix, through integrin receptors and the cytoskeleton, to the nucleus becomes modified.
It is noteworthy that tendon fibroblasts form a network with neighbouring cells through gap junctions [180, 181], which enable signal propagation from one cell to another. While cell communication is an essential tool for nutrient exchange and signal transduction in homeostatic conditions, the tendon cellular network might enforce local pathobiological cellular changes and thereby affect larger parts of the tendon matrix. During healing, however, this cellular network might be advantageous to propagate positive cellular adaptations in one to other tendon areas.
Another positive effect of load on injured tendons is suggested by the finding that strain protects collagen fibrils from collagen degradation. In an elegant study, a group of researchers showed that mechanical strain preserves collagen fibrils in the presence of MMP8; while unloaded fibrils were readily degraded, the strained fibrils were resistant to degradation for a prolonged time [182]. In tendinopathic tendons, increased amounts of several MMPs were measured and a disorganisation of collagen fibrils was described in several studies, suggesting collagen fibrils that are subjected to reduced strain. This combination might be a vicious circle contributing to enhanced tendon matrix catabolism as the disorganised collagen fibrils are more prone for enzymatic digestion. In the context of tissue repair, the regular application of high tensile load in slow motion might gradually straighten the collagen fibrils and thereby protect the matrix from degradation. Although this idea appears as an attractive mechanism, it should be remembered that it is speculative as there are no data on the strain that collagen fibrils in healthy and injured tendons are subjected to during slow loading.
In the clinical practice, one of the most effective treatment options for tendinopathy is heavy slow loading of the injured tendons, but exactly how the tendon cells and the tendon matrix are stimulated and activate a healing response is unclear. It is, however, obvious that unloading leads to catabolic changes in the tendon, indicating that “rest” periods should be avoided. Although the proximal hamstring tendons have not received much attention in tendon research, it is fair to speculate that loading regimes to treat tendinopathic hamstring tendons are suitable to reduce pain and improve structure of chronically injured hamstring tendons.
References
Ekstrand J. Injury incidence and injury patterns in professional football - the UEFA injury study Injury incidence and injury patterns in professional football – the UEFA Injury Study. Br J Sports Med. 2011;45(7):533–8.
Tidball JG, Salem G, Zernicke R. Site and mechanical conditions for failure of skeletal muscle in experimental strain injuries. J Appl Physiol. 1993;74(3):1280–6.
Tidball JG, Chan M. Adhesive strength of single muscle cells to basement membrane at myotendinous junctions. J Appl Physiol. 1989;67(3):1063–9.
Garrett WE, Nikolaou PK, Ribbeck BM, Glisson RR, Seaber AV. The effect of muscle architecture on the biomechanical failure properties of skeletal muscle under passive extension. Am J Sports Med. 1988;16(1):7–12.
van der Made AD, Wieldraaijer T, Kerkhoffs GM, Kleipool RP, Engebretsen L, van Dijk CN, et al. The hamstring muscle complex. Knee Surg Sport Traumatol Arthrosc. 2015;23(7):2115–22.
Woodley SJ, Mercer SR. Hamstring muscles: architecture and innervation. Cells Tissues Organs. 2005;179(3):125–41.
Brukner P, Connell D. “Serious thigh muscle strains”: beware the intramuscular tendon which plays an important role in difficult hamstring and quadriceps muscle strains. Br J Sports Med. 2015;2015:bjsports-2015-095136.
Vaittinen S, Lukka R, Sahlgren C, Rantanen J, Hurme T, Lendahl U, et al. Specific and innervation-regulated expression of the intermediate filament protein nestin at neuromuscular and myotendinous junctions in skeletal muscle. Am J Pathol. 1999;154(2):591–600.
Äärimaa V, Kääriäinen M, Vaittinen S, Tanner J, Järvinen T, Best T, et al. Restoration of myofiber continuity after transection injury in the rat soleus. Neuromuscul Disord. 2004;14(7):421–8.
Kääriainen M, Liljamo T, Pelto-Huikko M, Heino J, Jarvinen M, Kalimo H. Regulation of alpha7 integrin by mechanical stress during skeletal muscle regeneration. Neuromuscul Disord. 2001;11(4):360–9.
Hurme T, Kalimo H, Lehto M, Järvinen M. Healing of skeletal muscle injury: an ultrastructural and immunohistochemical study. Med Sci Sports Exerc. 1991;23(7):801–10.
Kääriäinen M, Nissinen L, Kaufman S, Sonnenberg A, Järvinen M, Heino J, et al. Expression of alpha7beta1 integrin splicing variants during skeletal muscle regeneration. Am J Pathol. 2002;161(3):1023–31.
Kääriäinen M, Kääriäinen J, Järvinen TLN, Nissinen L, Heino J, Järvinen M, et al. Integrin and dystrophin associated adhesion protein complexes during regeneration of shearing-type muscle injury. Neuromuscul Disord. 2000;10(2):121–32.
Gawlik KI, Durbeej M. Skeletal muscle laminin and MDC1A: pathogenesis and treatment strategies. Skelet Muscle. 2011;1(1):1–13.
Vaittinen S, Hurme T, Rantanen J, Kalimo H. Transected myofibres may remain permanently divided in two parts. Neuromuscul Disord. 2002;12(6):584–7.
Garrett WE. Muscle strain injuries. Am J Sport Med. 1996;24(6 Suppl):S2–8.
Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skelet Radiol. 2003;32(10):582–9.
Paxton JZ, Baar K. Tendon mechanics: the argument heats up. J Appl Physiol. 2007;103(7):423–4.
Fiorentino NM, Blemker SS. Musculotendon variability influences tissue strains experienced by the biceps femoris long head muscle during high-speed running. J Biomech. 2014;47(13):3325–33.
Tidball JG. Force transmission across muscle cell membranes. J Biomech. 1991;24(Suppl. 1):43–52.
Tidball JG, Daniel TL. Myotendinous junctions of tonic muscle cells: structure and loading. Cell Tissue Res. 1986;245(2):315–22.
Curzi D, Ambrogini P, Falcieri E, Burattini S. Morphogenesis of rat myotendinous junction. Muscles Ligaments Tendons J. 2013;3(4):275–80.
Knudsen AB, Larsen M, Mackey AL, Hjort M, Hansen KK, Qvortrup K, et al. The human myotendinous junction: an ultrastructural and 3D analysis study. Scand J Med Sci Sport. 2015;25(1):e116–23.
Bayer ML, Mackey A, Magnusson SP, Krogsgaard MR, Kjær M. Treatment of acute muscle injuries. Ugeskr Laeger. 2019;181(8):pii: V11180753.
Magnusson SP, Hansen P, Aagaard P, Brond J, Dyhre-Poulsen P, Bojsen-Moller J, et al. Differential strain patterns of the human gastrocnemius aponeurosis and free tendon, in vivo. Acta Physiol Scand. 2003;177(2):185–95.
Sousa F, Ishikawa M, Vilas-Boas JP, Komi PV. Intensity- and muscle-specific fascicle behavior during human drop jumps. J Appl Physiol. 2006;102(1):382–9.
Townsend DW. Finding the sweet spot: assembly and glycosylation of the dystrophin-associated glycoprotein complex. Anat Rec. 2014;297(9):1694–705.
Ervasti JM, Campbell KP. Membrane organization of the dystrophin-glycoprotein complex. Cell. 1991;66(6):1121–31.
Samitt CE, Bonilla E. Immunocytochemical study of dystrophin at the myotendinous junction. Muscle Nerve. 1990;13(6):493–500.
Pilgram GSK, Potikanond S, Baines RA, Fradkin LG, Noordermeer JN. The roles of the dystrophin-associated glycoprotein complex at the synapse. Mol Neurobiol. 2010;41:1–21.
Bao ZZ, Lakonishok M, Kaufman S. Horwitz a F. Alpha 7 beta 1 integrin is a component of the myotendinous junction on skeletal muscle. J Cell Sci. 1993;106(Pt 2):579–89.
Welser JV, Rooney JE, Cohen NC, Gurpur PB, Singer CA, Evans RA, et al. Myotendinous junction defects and reduced force transmission in mice that lack alpha7 integrin and utrophin. Am J Pathol. 2009;175(4):1545–54.
Subramanian A, Schilling TF. Tendon development and musculoskeletal assembly: emerging roles for the extracellular matrix. Development. 2015;142(24):4191–204.
Schweitzer R, Zelzer E, Volk T. Connecting muscles to tendons: tendons and musculoskeletal development in flies and vertebrates. Development. 2010;137(19):3347.
Koch M, Schulze J, Hansen U, Ashwodt T, Keene DR, Brunken WJ, et al. A novel marker of tissue junctions, collagen XXII. J Biol Chem. 2004;279(21):22514–21.
Zwolanek D, Veit G, Eble JA, Gullberg D, Ruggiero F, Heino J, et al. Collagen XXII binds to collagen-binding integrins via the novel motifs GLQGER and GFKGER. Biochem J. 2014;227:217–27.
Charvet B, Guiraud A, Malbouyres M, Zwolanek D, Guillon E, Bretaud S, et al. Knockdown of col22a1 gene in zebrafish induces a muscular dystrophy by disruption of the myotendinous junction. Development. 2013;140(22):4602–13.
Jakobsen JR, Mackey AL, Knudsen AB, Koch M, Kjær M, Krogsgaard MR. Composition and adaptation of human myotendinous junction and neighboring muscle fibers to heavy resistance training. Scand J Med Sci Sport. 2017;27(12):1547–59.
Oberhauser AF, Marszalek PE, Erickson HP, Fernandez JM. The molecular elasticity of the extracellular matrix protein tenascin. Nature. 1998;393(6681):181–5.
Järvinen TA, Józsa L, Kannus P, Järvinen TLN, Hurme T, Kvist M, et al. Mechanical loading regulates the expression of tenascin-C in the myotendinous junction and tendon but does not induce de novo synthesis in the skeletal muscle. J Cell Sci. 2003;116(Pt 5):857–66.
Midwood KS, Chiquet M, Tucker RP, Orend G. Tenascin-C at a glance. J Cell Sci. 2016;129(23):4321–7.
Adams JC. Thrombospondins: multifunctional regulators of cell interactions. Annu Rev Cell Dev Biol. 2001;17(1):25–51.
Frolova EG, Drazba J, Krukovets I, Kostenko V, Blech L, Harry C, et al. Control of organization and function of muscle and tendon by thrombospondin-4. Matrix Biol. 2014;37:35–48.
Kardon G. Muscle and tendon morphogenesis in the avian hind limb. Development. 1998;125(20):4019–32.
Jakobsen JR, Jakobsen NR, Mackey AL, Koch M, Kjaer M, Krogsgaard MR. Remodeling of muscle fibers approaching the human myotendinous junction. Scand J Med Sci Sport. 2018;28(8):1859–65.
Dreyer HC, Blanco CE, Sattler FR, Schroeder ET, Wiswell RA. Satellite cell numbers in young and older men 24 hours after eccentric exercise. Muscle Nerve. 2006;33(2):242–53.
Jamali AA, Afshar P, Abrams RA, Lieber RL. Differential expression of neural cell adhesion molecule (NCAM) after tenotomy in rabbit skeletal muscle. J Orthop Res. 2002;20(2):364–9.
Curzi D, Salucci S, Marini M, Esposito F, Agnello L, Veicsteinas A, et al. How physical exercise changes rat myotendinous junctions: an ultrastructural study. Eur J Histochem. 2012;56(2):117–22.
Tidball JG, Quan DM. Reduction in myotendinous junction surface area of rats subjected to 4-day spaceflight. J Appl Physiol. 1992;73(1):59–64.
Zamora AJ, Carnino A, Roffino S, Marini JF. Respective effects of hindlimb suspension, confinement and spaceflight on myotendinous junction ultrastructure. Acta Astronaut. 1995;36(8–12):693–706.
Curzi D, Lattanzi D, Ciuffoli S, Burattini S, Grindeland RE, Edgerton VR, et al. Growth hormone plus resistance exercise attenuate structural changes in rat myotendinous junctions resulting from chronic unloading. Eur J Histochem. 2013;57(4):248–55.
Palma LD, Marinelli M, Pavan M, Bertoni-Freddari C. Involvement of the muscle-tendon junction in skeletal muscle atrophy: an ultrastructural study. Romanian J Morphol Embryol. 2011;52(1):105–9.
Bayer MLML, Magnusson SPP, Kjaer M. Early versus delayed rehabilitation after acute muscle injury. N Engl J Med. 2017;377(13):1300–1.
Bayer ML, Hoegberget-Kalisz M, Jensen MH, Olesen JL, Svensson RB, Couppé C, et al. Role of tissue perfusion, muscle strength recovery and pain in rehabilitation after acute muscle strain injury: a randomized controlled trial comparing early and delayed rehabilitation. Scand J Med Sci Sports. 2018;28(12):2579–91.
Silder A, Heiderscheit BC, Thelen DG, Enright T, Tuite MJ. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skelet Radiol. 2008;37(12):1101–9.
Mauro A. Satellite cell of skeletal muscle fibers. J Biophys Biochem Cytol. 1961;9:493–5.
Lepper C, Partridge TA, Fan C-M. An absolute requirement for Pax7-positive satellite cells in acute injury-induced skeletal muscle regeneration. Development. 2011;138(17):3639–46.
Mackey AL, Kjaer M. The breaking and making of healthy adult human skeletal muscle in vivo. Skelet Muscle. 2017;7(1):1–18.
Yin H, Price F, Rudnicki MA. Satellite cells and the muscle stem cell niche. Physiol Rev. 2013;93(1):23–67.
Schultz E. Satellite cell proliferative compartments in growing skeletal muscles. Dev Biol. 1996;175(1):84–94.
Hughes SM, Blau HM. Migration of myoblasts across basal lamina during skeletal muscle development. Nature. 1990;345(6273):350–3.
Collins CA, Olsen I, Zammit PS, Heslop L, Petrie A, Partridge TA, et al. Stem cell function, self-renewal, and behavioral heterogeneity of cells from the adult muscle satellite cell niche. Cell. 2005;122(2):289–301.
Caldwell CJ, Mattey DL, Weller RO. Role of the basement membrane in the regeneration of skeletal muscle. Neuropathol Appl Neurobiol. 1990;16(3):225–38.
Tidball JG. Myotendinous junction: morphological changes and mechanical failure associated with muscle cell atrophy. Exp Mol Pathol. 1984;40(1):1–12.
Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sport Med. 2005;33(5):745–64.
Kääriainen M, Kääriainen J, Jarvinen TLN, Sievanen H, Kalimo H, Jarvinen M. Correlation between biomechanical and structural changes during the regeneration of skeletal muscle after laceration injury. J Orthop Res. 1998;16(2):197–206.
Van Der Made AD, Almusa E, Reurink G, Whiteley R, Weir A, Hamilton B, et al. Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. Br J Sports Med. 2018;52(19):1261–6.
Heinemeier KM, Schjerling P, Heinemeier J, Magnusson SP, Kjaer M. Lack of tissue renewal in human adult Achilles tendon is revealed by nuclear bomb 14C. FASEB J. 2013;27(5):2074–9.
Magnusson SP, Kjaer M. The impact of loading, unloading, ageing and injury on the human tendon. J Physiol. 2019;597(5):1283–98.
Clegg PD, Strassburg S, Smith RK. Cell phenotypic variation in normal and damaged tendons. Int J Exp Pathol. 2007;84:227–35.
Eliasson P, Couppé C, Lonsdale M, Svensson RB, Neergaard C, Kjær M, et al. Ruptured human Achilles tendon has elevated metabolic activity up to 1-year after repair. Eur J Nucl Med Mol Imaging. 2016;43(10):1868–77.
Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper’s knee in male athletes. A prospective follow-up study. Am J Sport Med. 2002;30(5):689–92.
Magnusson SP, Langberg H, Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Publ Gr. 2010;6(10):262–26843.
Kannus P. Structure of the tendon connective tissue. Scand J Med Sci Sport. 2000;10(6):312–20.
Bayer ML, Schjerling P, Herchenhan A, Zeltz C, Heinemeier KM, Christensen L, et al. Release of tensile strain on engineered human tendon tissue disturbs cell adhesions, changes matrix architecture, and induces an inflammatory phenotype. PLoS One. 2014;9(1):e86078.
Arnoczky SP, Lavagnino M, Egerbacher M, Caballero O, Gardner K, Shender MA. Loss of homeostatic strain alters mechanostat “set point” of tendon cells in vitro. Clin Orthop Relat Res. 2008;466:1583–91.
Arnoczky SP, Lavagnino M, Egerbacher M. The mechanobiological aetiopathogenesis of tendinopathy: is it the over-stimulation or the under-stimulation of tendon cells? Int J Exp Pathol. 2007;88:217–26.
Ahmed IM, Lagopoulos M, McConnell P, Soames RW, Sefton GK. Blood supply of the Achilles tendon. J Orthop Res. 1998;16:591–6.
Schmidt-Rohlfing B, Graf J, Schneider U, Niethard FU. The blood supply of the Achilles tendon. Int Orthop. 1992;16(1):29–31.
Järvinen M. Healing of a crush injury in rat striated muscle: 3. A micro-angiographical study of the effect of early mobilization and immobilization on capillary ingrowth. Acta Pathol Microbiol Scand A Pathol. 1976;84A(1):85–94.
Järvinen M. Healing of a crush injury in rat striated muscle. 2. A histological study of the effect of early mobilization and immobilization on the repair processes. Acta Pathol Microbiol Scand A. 1975;83(3):269–82.
Reurink G, Goudswaard GJ a, Tol JL, Almusa E, Moen MH, Weir A, et al. MRI observations at return to play of clinically recovered hamstring injuries. Br J Sports Med. 2014;48(18):1370–6.
Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. Am J Roentgenol. 2004;183(4):975–84.
Bayer ML, Bang L, Hoegberget-Kalisz M, Svensson RB, Olesen JL, Karlsson MM, et al. Muscle-strain injury exudate favors acute tissue healing and prolonged connective tissue formation in humans. FASEB J. 2019;33(9):10369–82.
Tyler TF, Schmitt BM, Nicholas SJ, McHugh MP. Rehabilitation after hamstring-strain injury emphasizing eccentric strengthening at long muscle lengths: results of long-term follow-up. J Sport Rehabil. 2017;26(2):131–40.
Sole G, Milosavljevic S, Nicholson H, Sullivan SJ. Selective strength loss and decreased muscle activity in hamstring injury. J Orthop Sport Phys Ther. 2011;41(5):354–63.
Rantanen J, Ranne J, Hurme T, Kalimo H. Denervated segments of injured skeletal muscle fibers are reinnervated by newly formed neuromuscular junctions. J Neuropathol Exp Neurol. 1995;54(2):188–94.
Carbonetto S, Lindenbaum M. The basement membrane at the neuromuscular junction: a synaptic mediatrix. Curr Opin Neurobiol. 1995;5(5):596–605.
Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–32.
Wangensteen A, Tol JL, Witvrouw E, Van Linschoten R, Almusa E, Hamilton B, et al. Hamstring reinjuries occur at the same location and early after return to sport: a descriptive study of MRI-confirmed reinjuries. Am J Sports Med. 2016;44(8):2112–21.
Reurink G, Almusa E, Goudswaard GJ, Tol JL, Hamilton B, Moen MH, et al. No association between fibrosis on magnetic resonance imaging at return to play and hamstring reinjury risk. Am J Sports Med. 2015;43(5):1228–34.
Wynn T, Yugandhar VG, Clark M. Cellular and molecular mechanisms of fibrosis. J Pathol. 2013;46(2):26–32.
Martin P, Leibovich SJ. Inflammatory cells during wound repair: the good, the bad and the ugly. Trends Cell Biol. 2005;15(11):599–607.
Kurkinen M, Vaheri A, Roberts PJ, Stenman S. Sequential appearance of fibronectin and collagen in experimental granulation tissue. Lab Investig. 1980;43(1):47–51.
Nagata H, Ueki H, Moriguchi T. Fibronectin: localization in normal human skin, granulation tissue, hypertrophic scar, mature scar, progressive systemic sclerotic skin, and other fibrosing dermatoses. Arch Dermatol. 1985;121(8):995–9.
Lehto M, Duance VC, Restall D. Collagen and fibronectin in a healing skeletal muscle injury. An immunohistological study of the effects of physical activity on the repair of injured gastrocnemius muscle in the rat. J Bone Joint Surg Br. 1985;67(5):820–8.
Hurme T, Kalimo H. Adhesion in skeletal muscle during regeneration. Muscle Nerve. 1992;15(4):482–9.
Yates CC, Bodnar R, Wells A. Matrix control of scarring. Cell Mol Life Sci. 2011;68:1871–81.
Lehto M, Sims TJ, Bailey AJ. Skeletal muscle injury—molecular changes in the collagen during healing. Res Exp Med. 1985;185(2):95–106.
Volk SW, Iqbal SA, Bayat A. Interactions of the extracellular matrix and progenitor cells in cutaneous wound healing. Adv Wound Care. 2013;2(6):261–72.
Bailey AJ, Paul RG, Knott L. Mechanisms of maturation and ageing of collagen. Mech Ageing Dev. 1998;106(1–2):1–56.
Klingberg F, Hinz B, White ES. The myofibroblast matrix: implications for tissue repair and fibrosis. J Pathol. 2013;229(2):298–309.
Hinz B. Formation and function of the myofibroblast during tissue repair. J Invest Dermatol. 2007;127(3):526–37.
Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol. 2002;3(5):349–63.
Desmoulière A, Redard M, Darby I, Gabbiani G. Apoptosis mediates the decrease in cellularity during the transition between granulation tissue and scar. Am J Pathol. 1995;146(1):56–66.
Rog-Zielinska EA, Norris RA, Kohl P, Markwald R. The living scar – cardiac fibroblasts and the injured heart. Trends Mol Med. 2016;22(2):99–114.
Holmes JW, Laksman Z, Gepstein L. Making better scar: emerging approaches for modifying mechanical and electrical properties following infarction and ablation. Prog Biophys Mol Biol. 2016;120(1–3):134–48.
Young IH, Bye PTP. Gas exchange in disease: asthma, chronic obstructive pulmonary disease, cystic fibrosis, and interstitial lung disease. Compr Physiol. 2011;1(2):663–97.
Silder A, Reeder SB, Thelen DG. The influence of prior hamstring injury on lengthening muscle tissue mechanics. J Biomech. 2010;43(12):2254–60.
Turl SE, George KP. Adverse neural tension: a factor in repetitive hamstring strain? J Orthop Sport Phys Ther. 1998;27(1):16–21.
Fox M, Mazza D, Kwiecien S, McHugh M. The effect of adverse neural tension on hamstring strength in rugby players. Med Sci Sport Exerc. 2014;46(5):203.
Kornberg C, Lew P. The effect of stretching neural structures on grade one hamstring injuries. J Orthop Sport Phys Ther. 1989;10(12):481–7.
Mann CJ, Perdiguero E, Kharraz Y, Aguilar S, Pessina P, Serrano AL, et al. Aberrant repair and fibrosis development in skeletal muscle. Skelet Muscle. 2011;1(1):21.
Lech M, Anders HJ. Macrophages and fibrosis: how resident and infiltrating mononuclear phagocytes orchestrate all phases of tissue injury and repair. Biochim Biophys Acta Mol basis Dis. 2013;1832:989–97.
Stramer BM, Mori R, Martin P. The inflammation – fibrosis link? A jekyll and hyde role for blood cells during wound repair. J Invest Dermatol. 2007;127(5):1009–17.
Lupher ML, Gallatin WM. Regulation of fibrosis by the immune system. Adv Immunol. 2006;89:245–88.
Satoh T, Nakagawa K, Sugihara F, Kuwahara R, Ashihara M, Yamane F, et al. Identification of an atypical monocyte and committed progenitor involved in fibrosis. Nature. 2017;541(7635):96–101.
Sanfilippo JL, Silder A, Sherry MA, Tuite MJ, Heiderscheit BC. Hamstring strength and morphology progression after return to sport from injury. Med Sci Sports Exerc. 2013;45(3):448–54.
Szpaderska AM, Egozi EI, Gamelli RL, DiPietro LA. The effect of thrombocytopenia on dermal wound healing. J Invest Dermatol. 2003;120(6):1130–7.
Golebiewska EM, Poole AW. Platelet secretion: from haemostasis to wound healing and beyond. Blood Rev. 2015;29(3):153–62.
Chen CJ, Kono H, Golenbock D, Reed G, Akira S, Rock KL. Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat Med. 2007;13(7):851–6.
Schaefer L. Complexity of danger: the diverse nature of damage-associated molecular patterns. J Biol Chem. 2014;289(51):35237–45.
Hayden MS, Ghosh S. NF-κB in immunobiology. Cell Res. 2011;21(2):223–44.
Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, et al. Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nat Med. 2005;11(11):1173–9.
Galli SJ, Borregaard N, Wynn TA. Phenotypic and functional plasticity of cells of innate immunity: macrophages, mast cells and neutrophils. Nat Immunol. 2011;12:1035–44.
Tao Z-Y, Cavasin MA, Yang F, Liu Y-H, Yang X-P. Temporal changes in matrix metalloproteinase expression and inflammatory response associated with cardiac rupture after myocardial infarction in mice. Life Sci. 2004;74:1561–72.
Akbar AN, Salmon M. Cellular environments and apoptosis: tissue microenvironments control activated T-cell death. Immunol Today. 1997;18:72–6.
Eming SA, Werner S, Bugnon P, Wickenhauser C, Siewe L, Utermöhlen O, et al. Accelerated wound closure in mice deficient for interleukin-10. Am J Pathol. 2007;170(1):188–202.
Serhan CN, Clish CB, Brannon J, Colgan SP, Chiang N, Gronert K. Novel functional sets of lipid-derived mediators with antiinflammatory actions generated from omega-3 fatty acids via cyclooxygenase 2-nonsteroidal antiinflammatory drugs and transcellular processing. J Exp Med. 2000;192(8):1197–204.
Serhan CN, Hong S, Gronert K, Colgan SP, Devchand PR, Mirick G, et al. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med. 2002;196(8):1025–37.
Ploeger DTA, Hosper NA, Schipper M, Koerts JA, De Rond S, Bank RA. Cell plasticity in wound healing: paracrine factors of M1/M2 polarized macrophages influence the phenotypical state of dermal fibroblasts. Cell Commun Signal. 2013;11:29.
Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25(12):677–86.
Wynn T. a. Mechanism of fibrosis: therapeutic transplation for fibrotic disease. Nat Med. 2013;18(7):1028–40.
Van Dyken SJ, Locksley RM. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu Rev Immunol. 2013;31:317–43.
Hinz B, Phan SH, Thannickal VJ, Galli A, Bochaton-Piallat ML, Gabbiani G. The myofibroblast: one function, multiple origins. Am J Pathol. 2007;170(6):1807–16.
Ignotz R, Massagué J. Transforming growth factor-beta stimulates the expression of fibronectin and collagen and their incorporation into the extracellular matrix. J Biol Chem. 1986;261:4337–45.
Mishra R, Zhu L, Eckert RL, Simonson MS. TGF-beta-regulated collagen type I accumulation: role of Src-based signals. Am J Physiol Cell Physiol. 2007;292(4):C1361–9.
Pakshir P, Hinz B. The big five in fibrosis: macrophages, myofibroblasts, matrix, mechanics, and miscommunication. Matrix Biol. 2018;68–69:81–93.
McLennan IS. Degenerating and regenerating skeletal muscles contain several subpopulations of macrophages with distinct spatial and temporal distributions. J Anat. 1996;188(Pt 1):17–28.
Saclier M, Yacoub-Youssef H, Mackey a L, Arnold L, Ardjoune H, Magnan M, et al. Differentially activated macrophages orchestrate myogenic precursor cell fate during human skeletal muscle regeneration. Stem Cells. 2013;31(2):384–96.
Perdiguero E, Sousa-victor P, Ruiz-bonilla V, Caelles C, Serrano AL. p38/MKP-1-regulated AKT coordinates macrophage transitions and resolution of inflammation during tissue repair. J Cell Biol. 2011;195(2):307–22.
Cheng M, Nguyen M-H, Fantuzzi G, Koh TJ. Endogenous interferon- is required for efficient skeletal muscle regeneration. AJP Cell Physiol. 2008;294(5):C1183–91.
Knipper JA, Willenborg S, Brinckmann J, Bloch W, Rothenberg ME, Niehoff A, et al. Interleukin-4 receptor α signaling in myeloid cells controls collagen fibril assembly in skin repair. Immunity. 2016;43(4):803–16.
Virchenko O, Skoglund B, Aspenberg P. Parecoxib impairs early tendon repair but improves later remodeling. Am J Sports Med. 2004;32(7):1743–7.
Van Linthout S, Miteva K, Tschöpe C. Crosstalk between fibroblasts and inflammatory cells. Cardiovasc Res. 2014;102:258–69.
Dakin SG, Newton J, Martinez FO, Hedley R, Gwilym S, Jones N, et al. Chronic inflammation is a feature of Achilles tendinopathy and rupture. Br J Sports Med. 2018;52(6):359–67.
Pap T, Müller-Ladner U, Gay RE, Gay S. Fibroblast biology. Role of synovial fibroblasts in the pathogenesis of rheumatoid arthritis. Arthritis Res. 2000;2:361–7.
Lempainen L, Johansson K, Banke IJ, Ranne J, Makela K, Sarimo J, et al. Expert opinion: diagnosis and treatment of proximal hamstring tendinopathy. Muscles Ligaments Tendons J. 2015;5(1):23–8.
Benazzo F, Marullo M, Zanon G, Indino C, Pelillo F. Surgical management of chronic proximal hamstring tendinopathy in athletes: a 2 to 11 years of follow-up. J Orthop Traumatol. 2013;14(2):83–9.
Kongsgaard M, Qvortrup K, Larsen J, Aagaard P, Doessing S, Hansen P, et al. Fibril morphology and tendon mechanical properties in patellar tendinopathy: effects of heavy slow resistance training. Am J Sports Med. 2010;38(4):749–56.
Pingel J, Lu Y, Starborg T, Fredberg U, Langberg H, Nedergaard A, et al. 3-D ultrastructure and collagen composition of healthy and overloaded human tendon: evidence of tenocyte and matrix buckling. J Anat. 2014;224(5):548–55.
Kragsnaes MS, Fredberg U, Stribolt K, Kjaer SG, Bendix K, Ellingsen T. Stereological quantification of immune-competent cells in baseline biopsy specimens from achilles tendons: results from patients with chronic tendinopathy followed for more than 4 years. Am J Sports Med. 2014;42(10):2435–45.
Lian Ø, Scott A, Engebretsen L, Bahr R, Duronio V, Khan K. Excessive apoptosis in patellar tendinopathy in athletes. Am J Sports Med. 2007;35(4):605–11.
Schubert TEO, Weidler C, Lerch K, Hofstädter F, Straub RH. Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis. 2005;64(7):1083–6.
Andersson G, Danielson P, Alfredson H, Forsgren S. Nerve-related characteristics of ventral paratendinous tissue in chronic Achilles tendinosis. Knee Surg Sport Traumatol Arthrosc. 2007;15(10):1272–9.
Glazebrook MA, Wright JR, Langman M, Stanish WD, Lee JM. Histological analysis of Achilles tendons in an overuse rat model. J Orthop Res. 2008;26(6):840–6.
Pingel J, Wienecke J, Kongsgaard M, Behzad H, Abraham T, Langberg H, et al. Increased mast cell numbers in a calcaneal tendon overuse model. Scand J Med Sci Sport. 2013;23(6):353–60.
Matthews TJW. Pathology of the torn rotator cuff tendon: reduction in potential for repair as tear size increases. J Bone Joint Surg. 2006;88-B(4):489–95.
Kvist MH, Lehto MU k, Jozsa L, Järvinen M, Kvist HT. Chronic Achilles paratenonitis: an immunohistologic study of fibronectin and fibrinogen. Am J Sports Med. 1988;16(6):616–23.
Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009;37(4):727–34.
Gross MT. Chronic tendinitis: pathomechanics of injury, factors affecting the healing response, and treatment. J Orthop Sport Phys Ther. 1992;16(6):248–61.
Millar NL, Hueber AJ, Reilly JH, Yinghua X, Fazzi UG, Murrell GAC, et al. Inflammation is present in early human tendinopathy. Am J Sports Med. 2010;38(10):2085–91.
Jones GC, Corps AN, Pennington CJ, Clark IM, Edwards DR, Bradley MM, et al. Expression profiling of metalloproteinases and tissue inhibitors of metalloproteinases in normal and degenerate human Achilles tendon. Arthritis Rheum. 2006;54(3):832–42.
Heinemeier KM, Schjerling P, Øhlenschlæger TF, Eismark C, Olsen J, Kjær M. Carbon-14 bomb pulse dating shows that tendinopathy is preceded by years of abnormally high collagen turnover. FASEB J. 2018;32(9):4763–75.
Legerlotz K, Jones ER, Screen HRC, Riley GP. Increased expression of IL-6 family members in tendon pathology. Rheumatol (UK). 2012;51(7):1161–5.
Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy slow resistance versus eccentric training as treatment for achilles tendinopathy: a randomized controlled trial. Am J Sports Med. 2015;43(7):1704–11.
Alfredson H, Pietilä T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26(3):360–6.
Kongsgaard M, Kovanen V, Aagaard P, Doessing S, Hansen P, Laursen AH, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sport. 2009;19(6):790–802.
Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015;49(19):1277–83.
Rio E, Van Ark M, Docking S, Moseley GL, Kidgell D, Gaida JE, et al. Isometric contractions are more analgesic than isotonic contractions for patellar tendon pain: an in-season randomized clinical trial. Clin J Sport Med. 2017;27(3):253–9.
Heinemeier KM, Olesen JL, Haddad F, Langberg H, Kjaer M, Baldwin KM, et al. Expression of collagen and related growth factors in rat tendon and skeletal muscle in response to specific contraction types. J Physiol. 2007;582(3):1303–16.
Heinemeier KM, Olesen JL, Schjerling P, Haddad F, Langberg H, Baldwin KM, et al. Short-term strength training and the expression of myostatin and IGF-I isoforms in rat muscle and tendon: differential effects of specific contraction types. J Appl Physiol. 2006;102(2):573–81.
Garma T, Kobayashi C, Haddad F, Adams GR, Bodell PW, Baldwin KM. Similar acute molecular responses to equivalent volumes of isometric, lengthening, or shortening mode resistance exercise. J Appl Physiol. 2006;102(1):135–43.
Dideriksen K, Sindby AK, Krogsgaard M, Schjerling P, Holm L, Langberg H. Effect of acute exercise on patella tendon protein synthesis and gene expression. Springerplus. 2013;2:109.
Broberg A, Heino J. Integrin α2β1-dependent contraction of floating collagen gels and induction of collagenase are inhibited by tyrosine kinase inhibitors. Exp Cell Res. 1996;228(1):29–35.
Zhu J, Li J, Wang B, Zhang WJ, Zhou G, Cao Y, et al. The regulation of phenotype of cultured tenocytes by microgrooved surface structure. Biomaterials. 2010;31(27):6952–8.
Schoenenberger AD, Foolen J, Moor P, Silvan U, Snedeker JG. Substrate fiber alignment mediates tendon cell response to inflammatory signaling. Acta Biomater. 2018;71:306–17.
Kjær M, Langberg H, Heinemeier K, Bayer ML, Hansen M, Holm L, et al. From mechanical loading to collagen synthesis, structural changes and function in human tendon. Scand J Med Sci Sports. 2009;19:500–10.
Gardner K, Arnoczky SP, Caballero O, Lavagnino M. The effect of stress-deprivation and cyclic loading on the TIMP/MMP ratio in tendon cells: an in vitro experimental study. Disabil Rehabil. 2008;30(20–22):1523–9.
Young NJ, Becker DL, Fleck RA, Goodship AE, Patterson-Kane JC. Maturational alterations in gap junction expression and associated collagen synthesis in response to tendon function. Matrix Biol. 2009;28(6):311–23.
Waggett AD, Benjamin M, Ralphs JR. Connexin 32 and 43 gap junctions differentially modulate tenocyte response to cyclic mechanical load. Eur J Cell Biol. 2006;85(11):1145–54.
Flynn BP, Bhole AP, Saeidi N, Liles M, Dimarzio CA, Ruberti JW. Mechanical strain stabilizes reconstituted collagen fibrils against enzymatic degradation by mammalian collagenase matrix metalloproteinase 8 (MMP-8). PLoS One. 2010;5(8):e12337.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bayer, M.L., Järvinen, T.A.H. (2020). Basic Muscle Physiology in Relation to Hamstring Injury and Repair. In: Thorborg, K., Opar, D., Shield, A. (eds) Prevention and Rehabilitation of Hamstring Injuries. Springer, Cham. https://doi.org/10.1007/978-3-030-31638-9_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-31638-9_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31637-2
Online ISBN: 978-3-030-31638-9
eBook Packages: MedicineMedicine (R0)