Abstract
Treatment failure is defined as an unsuccessful result of management, and this is observed frequently in acute and long-standing hamstring injuries. The main causes of treatment failure are an incorrect diagnosis or inefficacy of treatment. This chapter will describe the differential diagnoses that can be considered in patients with treatment failure after acute and long-standing hamstring injuries. Reevaluation of the patient and expanding diagnostic workup can be useful to identify other causes of posterior thigh or buttock pain. If the diagnosis remains within the category of acute hamstring injury, hamstring injury sequela, or hamstring tendinopathy, alternative treatments can be considered. Numerous alternative treatment options are available for this patient group. This chapter describes which treatments can be considered and what the current level of evidence for their efficacy is.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Treatment failure
- Incorrect diagnosis
- Inadequate treatment
- Differential diagnosis
- Alternative treatment
- Injection therapy
- Surgery
13.1 Introduction
Treatment failure can be defined as a measure of the quality of health care by assessment of unsuccessful results of management. Incidence rates of acute hamstring injuries are well documented in literature, but similar data are lacking for proximal hamstring tendinopathy (PHT). Patients with PHT experience a more gradual onset with fluctuating symptoms over time [1]. This makes it harder to apply the definition of treatment failure, as there is no acute onset of a reinjury as we recognise in acute hamstring injuries. For assessment of hamstring injuries, this quality of health care can be assessed with reinjury rates, patient-reported outcomes, strength and flexibility measures, or imaging outcomes. Some of the outcome measures, especially reinjury and patient-reported outcomes, are very useful, while other measures are not associated with the clinical signs of treatment failure.
The most common type of treatment failure in acute hamstring injuries is the onset of a reinjury. Other less frequent types are an inadequate rehabilitation with acute onset of pain or a prolonged rehabilitation without full recovery. Treatment failure in long-standing hamstring injuries is most frequently a result of relapse or persistence of symptoms after full rehabilitation.
13.1.1 Epidemiology of Treatment Failure
The different types of treatment failure have diverse incident rates. High recurrence rates following acute hamstring injuries have been reported in the literature. Hamstring reinjury rate is 14–63% within 2 years after the initial injury [2, 3]. It is known that 50% of these reinjuries occur within the first 50 days of return to play (RTP) [4]. This emphasises the close relationship between time to RTP and occurrence of reinjuries. Inadequate rehabilitation and insufficient criteria for return to sport (RTS) participation might be reasons for the large variation in hamstring reinjury incidence.
The other types of treatment failure are less well-described in terms of epidemiology. The onset of acute hamstring pain during conservative treatment (in most cases, this implies rehabilitation) is sometimes reported as reinjury in literature. This should, however, not be interpreted as reinjury but as inadequate rehabilitation. Consequently, part of the definition of a reinjury is that it occurs after a RTP decision has been made as a result of a rehabilitation programme. It is also less common that athletes experience prolonged symptom duration after an acute hamstring injury. This is known as a distinct clinical entity and has also been found in a recent high-quality trial in this field [5]. Epidemiological data of persisting or relapsing symptoms due to PHT are lacking. It is known that tendinopathy at other locations is treatment resistant in 60% of the cases at 5-year follow-up [6].
13.1.2 Impact of Treatment Failure
Hamstring injuries impair athlete performance, as they result in absence from sports for several weeks or months. The financial burden as a result of hamstring injuries is considerable in elite team sports. For example, in the English Premier League, the salary burden as a result of hamstring injuries reaches over € 20 million per season [7].
The impact is also evident at the individual level. Acute hamstring reinjuries and hamstring injury sequelae frequently lead to insecurity of the athletes. This might lead to kinesiophobia or decreased psychological readiness to RTP. This is even more pronounced in case of proximal tendon avulsion injuries which can be career threatening [8]. The impact of PHT is also evident but results more specifically in decreased participation in sports activities or a decreased performance with fluctuating episodes [9].
13.1.3 Causes of Treatment Failure
Treatment failure is a result of either an incorrect diagnosis or an inadequate rehabilitation. In the sections below, we will outline the potential pitfalls in diagnosing and treating hamstring injuries. This can aid the healthcare provider in managing patients with treatment failure of acute hamstring injuries, hamstring injury sequelae, and hamstring tendinopathy.
13.2 Causes of Treatment Failure in Patients with Acute Hamstring Injuries
13.2.1 Incorrect Diagnosis
In case of treatment failure after an initially diagnosed acute hamstring muscle injury, other possible causes of acute posterior thigh pain should be considered. Table 13.1 provides an overview of these. These causes are divided into hamstring muscle-tendon-bone complex injuries and causes from other anatomical structures. In patients with the clinical picture of acute hamstring injuries that fail to respond to rehabilitation, other hamstring muscle-tendon-bone complex injuries should be considered as cause. These specific diagnostic considerations are described more in detail in the section below.
13.2.1.1 Tendon Avulsion Injury
A tendon avulsion is a severe type of acute hamstring injury, characterised by complete de-attachment of one or more hamstring tendons from the bone. It usually involves avulsion of the proximal tendon(s) from the ischial tuberosity, but distal tendon avulsion may also occur. Although older people are more prone to avulsions, these injuries are also observed in younger athletes.
Hamstring tendon avulsions are relatively rare, associated with a prolonged recovery, and may lead to persistent functional impairments [8, 10]. Due to the rarity of this injury, it is often missed at initial diagnosis, resulting in a diagnostic delay and insufficient initial management.
The injury mechanism typically includes a sudden forceful hip flexion and knee extension, such as gliding over a slippery surface or water ski accidents. Recently, an alternative injury mechanism that also involves a considerable hip abduction component (hip flexion-abduction injury mechanism) has been described [11].
In case of a missed avulsion injury, patients often report specific symptoms, even after a period of rehabilitation. These symptoms include persistent hamstring muscle weakness, difficulties in coordinating hip and knee movements, and/or sensory perception in the distribution field of the sciatic nerve. In some patients, the main symptom is persistent pain at the ischial tuberosity during sitting, which is a disabling symptom for patients in their daily living. At physical examination, there is often marked hamstring muscle atrophy and loss of hamstring strength. Some patients are even unable to contract their hamstring muscle. On palpation, the hamstring tendons may not be felt by the examiner due to muscle retraction. Sensory symptoms may occur in the sensory distribution area of the sciatic nerve as a result of the hematoma formation or due to adhesions. Imaging can confirm this diagnosis, and magnetic resonance imaging (MRI) is most frequently used in the clinical setting as this modality is able to depict which of the three hamstring origin sites has been ruptured (Fig. 13.1).
Magnetic resonance imaging (MRI) of a tendon avulsion injury from the ischial tuberosity. Coronal STIR images demonstrating left-sided increased signal intensity distal to the ischial tuberosity. There is an avulsion of all three hamstring tendon insertions from the ischial tuberosity. Note the waviness (or “buckling”) of the proximal tendon, which is indicative of a complete tendon rupture
In both short-living and long-standing cases, there may be an indication for surgical fixation of the avulsed hamstring tendon at the original insertion (see Sect. 13.5.2).
13.2.1.2 Ischial Tuberosity Apophysis Avulsion Fracture
Adolescents are prone to avulsion of the ischial apophysis instead of tendinous proximal hamstring avulsion, especially between the ages of 14–18 years. In any adolescent or young adult with severe (proximal) hamstring pain or difficulties in activating the hamstring muscle after acute injury, an ischial apophysis avulsion should be considered. Plain X-ray can identify a displaced avulsion fracture. In case of a high clinical suspicion and a negative X-ray, a computed tomography (CT) scan or MRI should be considered, as in our experience non- or minimally-displaced apophysis avulsions can be missed.
The literature on treatment of these injuries is limited, and there are no controlled studies comparing conservative with surgical treatment. Based on case series, it is known that with increasing displacement, consolidation of the bony fragment is less likely to occur with conservative treatment [12]. This has led to the expert opinion that larger displaced fragments may require surgical fixation. However, there is no consensus in the literature on the exact cutoff point: >1 cm [13], >1.5 cm [12], and >2 cm [14] are suggested. Other factors that are not related to the fragment displacement, such as sport-specific demands of the hamstring muscles, should be considered in this decision-making. Conservative management consists of 8–12 weeks relative rest post-injury, followed by a progressive exercise programme. Full rehabilitation takes up to 1 year, and hamstring strength deficit may persist in the longer term (see Chap. 10).
13.2.1.3 Adductor Magnus Muscle Injury
The adductor magnus (AM) can be subdivided into two parts: (1) the pubofemoral part that originates from the ischiopubic ramus and inserts on the lower gluteal line and linea aspera and (2) the ischiocondylar part that originates from the inferior ischial tuberosity and takes an almost vertical course to its insertion on the femoral adductor tubercle [15]. The latter ischiocondylar part shares a common innervation and action (hip extension) with the long hamstrings. Adductor magnus injury can mimic a proximal acute hamstring injury, but the prognosis tends to be better. Identifying the precise location of the injury by careful palpation can help to differentiate between these conditions. The AM ischiocondylar origin can be palpated inferior and medial to the proximal hamstring tendons. Additional diagnostics with ultrasound (US) or MRI may help to confirm the diagnosis. When an AM injury has been established, rehabilitation should focus more on actions of this specific muscle group by using hip extension and adduction strengthening exercises.
13.2.1.4 Gastrocnemius Muscle Injury
Acute injury to the proximal gastrocnemius can mimic a distal acute hamstring injury. Differentiating these injuries is relatively easy by clinical examination. Strength testing of the calf muscle by resisted ankle plantar flexion and stretching the gastrocnemius with ankle dorsiflexion with the knee fully extended will provoke symptoms in case of a gastrocnemius injury. On the other hand, strength testing of the hamstrings by resisted hip extension and stretch testing using the (active or passive) knee extension test will provoke symptoms in hamstring injury and not in gastrocnemius injury. Additional diagnostics with US or MRI may help to confirm the diagnosis, especially for more difficult presentations in the popliteal region. When a gastrocnemius injury has been established, rehabilitation should focus more on actions of this specific muscle group by using knee flexion and ankle plantar flexion strengthening exercises.
13.2.2 Inadequate Rehabilitation
A number of considerations arise within the optimal planning of rehabilitation of acute hamstring injury (see Chaps. 10 and 11). Certainly, the need to individualise the approach according to past history of hamstring injury, severity of current injury, type of sport, and the athlete’s aspirations remains paramount.
13.2.2.1 Planning of Rehabilitation
One of the first decisions is around balancing when to begin early mobilisation. Starting too early may compromise healing and lead to greater scar formation [16], whereas too-late mobilisation may lead to a compromised muscle function. Järvinen et al. [16] recommend mobilising (defined as treadmill running) at or around day 5, although obviously this depends on the grade of injury and complexity of the lesion. It has to be acknowledged that broad opinion continues with respect to how aggressive to be in early management, yet it is probable that too-early mobilisation of higher-grade lesions may well compromise longer-term outcomes. Return to running within 4 days conferred significantly greater risk of recurrence than commencing running at 5 days or longer. Interestingly, this delay did not prolong RTP in the latter subjects [17].
In concert with early mobilisation, the choice and timing of supplementary exercises is paramount. Recent research suggests that an overemphasis of concentric exercises will lead to fascicle shortening [18], which will increase risk of hamstring reinjury at higher eccentric loads. Eccentric loading should be introduced early to maintain/improve fascicle lengths and ultimately functional length [2, 19]. The application of knee flexor-dominant or hip extensor-dominant loading is an important consideration which may well be influenced by the site and severity of the lesion. Eccentric exercise of hamstrings at longer muscle lengths appeared to provide a greater fascicle length change, although modest increases were also seen at shorter lengths [20]. Perhaps most importantly, progression of this stimulus is necessary to meet higher loads and functional demands of the sport.
A well-structured running programme to meet demands of the sport including distance, intensity, and acceleration is a key component. This is integral to athlete load management, modelled to RTS in a robust manner. Recent work by Stares et al. [17] presented compelling data demonstrating a more robust RTP was associated with increased volumes of high-speed running prior to resumption of competition. However, this did necessitate a lengthened RTP. This data better informs the risk-reward debate raised previously by Orchard et al. [21] around the RTP decision. These authors described a lack of agreement around robust criteria and the need to consider an increased risk of reinjury associated with earlier return.
13.2.2.2 Managing Risk Factors
As has been stated by many practitioners, history of hamstring injury now confers non-modifiable risk. Conversely, increasing hamstring strength levels and side-to-side balance [2] in the hamstring group offers perhaps one of the best opportunities (in combination with addressing fascicle length) to reduce the inherited risk of the athlete for recurrence or future injury. Considerable work has been contributed in the provision of sport-specific thresholds [18, 22].
As the first weeks of RTS carry the highest risk [4], this requires the management team to closely monitor the athlete with a preparedness to be flexible in sessional demands of the various challenges of the sport [2]. There is currently no scientific evidence that supports adjusting the length of rehabilitation in patients with risk factors. However, in our experience, modification of rehabilitation duration according to risk factors such as past medical history is recommended [21].
13.3 Causes of Treatment Failure in Patients with Ongoing Posterior Thigh Pain, Including Hamstring Injury Sequelae
13.3.1 Incorrect Diagnosis
Ongoing posterior thigh pain is often hard to manage, and other diagnoses should certainly be considered in these cases. Table 13.1 provides an overview of possible causes of posterior thigh pain. Symptoms of hamstring injury sequelae can have their origin in the hamstring muscle-tendon-bone complex or in structures that are not related to the hamstrings. These diagnostic considerations are described below.
13.3.1.1 Hamstring Muscle-Tendon-Bone Complex-Related Causes
13.3.1.1.1 Traction Apophysitis of the Ischial Tuberosity
Traction apophysitis occurs in teenagers prior to complete fusion of the ischial apophysis and results from repeated traction injuries on the apophysis without discrete displacement. These teenagers present with exercise-related localised pain at the ischial tuberosity which can be provoked on palpation. Scientific evidence for the effect of different treatment options is scarce; only a few randomised clinical trials have been performed in patients with an equivalent injury of the tibial tuberosity (M. Osgood Schlatter). Treatment of these traction apophysitis injuries is mainly symptomatic using load management advice. The long-term prognosis for a traction apophysitis is good, as complete recovery can be expected with closure of the ischial growth plate.
13.3.1.1.2 Myositis Ossificans
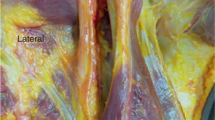
Myositis ossificans is a heterotopic non-neoplastic bone or cartilage formation in or adjacent to a muscle [23]. There are three different types: myositis ossificans progressiva (hereditary and severe generalised form), myositis ossificans without history of trauma (associated with burns, haemophilia, and neurological disorders), and myositis ossificans traumatica (either related to a contusion or repeated minor trauma) [24]. While traumatic myositis ossificans is more common in the anterior thigh muscles [25], it can also occur in the hamstring muscles [26]. Subjects may present with pain, swelling, and a palpable mass. The diagnosis can be confirmed with a plain radiograph (Fig. 13.2) or on US examination. Management of myositis ossificans is mainly conservative, including relative rest to control pain and inflammation, followed by gradual progressive exercise with symptom-based progression.
X-ray depicting myositis ossificans. X-ray of the left femur in anteroposterior direction showing calcifications at the lateral side of the femur in an adolescent basketball player who sustained a direct trauma to the posterolateral side of the left upper leg. When these calcifications are observed in relation to a previous trauma on that location, they are specific for myositis ossificans
13.3.1.2 Non-Hamstring-Related Causes
13.3.1.2.1 Neural Causes
The hamstrings are innervated by the tibial branch (biceps femoris long head (BFLH), semitendinosus (ST), and semimembranosus (SM)) and peroneal branch (biceps femoris short head (BFSH)) of the sciatic nerve. The sciatic nerve is formed from the L4-S3 segments of the sacral plexus. Nerve damage, compression, or irritation can occur at various sites along the way, resulting in posterior thigh pain.
Compression or chemical irritation of the nerve roots in the lower back can occur. Several causes of posterior thigh pain due to nerve root compression are spinal disc herniation, degenerative disc disease, lumbar spinal stenosis, or spondylolisthesis. These causes are usually associated with other neurological symptoms, such as pain and numbness radiating distally, loss of Achilles tendon reflex, or muscle weakness (hamstring muscles, ankle evertors).
Along its pathway, the sciatic nerve can de damaged or compressed by a direct trauma or pelvic trauma [27]. Compression of the sciatic nerve by the hip external rotators has been described (often referred as “piriformis syndrome”), but this clinical entity remains controversial [28]. Other sites of sciatic compression have also been implicated [29,30,31].
Finally, damage or entrapment of peripheral nerves may cause pain. The skin of the posterior thigh is innervated by the posterior femoral cutaneous nerve (PFCN) via its numerous collateral branches. If symptoms of pain and altered sensation are limited to the specific distribution area of the nerve (from the posterior thigh to the popliteal fossa) and pain is exacerbated with sitting or leaning against the buttock, then the PFCN should be considered as the source of the pain [32]. A diagnostic US-guided infiltration with an anaesthetic may help in establishing the diagnosis.
13.3.1.2.2 Vascular Causes
Iliac artery endofibrosis is a rare condition that may result in a reduced blood flow to the lower extremity in otherwise healthy individuals. It is most common in cyclists but has also been reported in other endurance athletes [33]. The hallmark symptomatology of this condition is leg weakness, thigh pain, and resolution of symptoms within 5 min of exercise cessation. Although the pain is usually in the anterior and lateral thigh, it may also be experienced in the posterior thigh. Exercise testing with ankle blood pressure measurements is the most appropriate way to confirm or exclude the diagnosis. Additionally, imaging (US, angiography) may be used for diagnostic purposes [33].
Other rare vascular causes of posterior thigh pain are thrombophlebitis, deep venous thrombosis (DVT) [23, 34], and post-thrombosis syndrome [35]. These venous conditions usually cause symptoms of the lower leg but sometimes may present with posterior thigh pain. Post-thrombosis syndrome is a long-term complication of DVT as a result of valvular incompetence due to damage to the venous valves. Symptoms may include pain, cramping, heaviness, itching, swelling, skin discoloration, and presence of varicose veins [35].
13.3.1.2.3 Bone Pathology
Bone tumours are rare but should not be missed, as delayed diagnosis can be catastrophic, especially in the case of malignant tumours. There are no specific signs that are associated with bone tumours, but night pain and increasing pain that is not associated with activities are signs that increase suspicion of this disease. A plain radiograph is the first step to detect a bone tumour. Subsequently, CT and/or MRI scanning with additional intravenous contrast media may be required.
Stress fractures of the upper thigh (femur, femoral neck) are uncommon but may present as posterior thigh pain. Athletes with high training loads are at increased risk for development of stress fractures of the upper thigh (femur or femoral neck) [36]. Training errors are the most frequent cause of stress fractures, especially a sudden increase in training load. Other risk factors include age, female sex, low bone mass, menstrual cycle disturbance, and bone metabolic disorders. Imaging is often required for confirming this diagnosis. Commonly used imaging modalities to detect stress fractures are plain radiographs, bone scans, MRI, or CT [36].
13.3.1.2.4 Joint Pathology
Referred pain from the sacroiliac, hip, or knee joint may present as posterior thigh pain. A careful history-taking and physical examination of these joints should be part of the differential diagnosis workup of posterior thigh pain in treatment failure after (suspected) hamstring injury sequela.
13.3.1.2.5 Bursitis
Near the hamstring muscle complex, there are two bursae that may provoke posterior thigh pain: the ischiogluteal bursa and the SM bursa. An ischial bursitis presents with inflammatory pain at the hamstring origin, typically when sitting on a hard surface. It can be difficult to distinguish from a PHT. The SM bursa is located posteromedial of the knee at the medial aspect of the SM tendon. Inflammation of this bursa will likewise result in inflammatory symptoms near this posteromedial region of the knee.
Ultrasound or MR imaging can visualise a bursa filled with fluid [37, 38]. The benefit of anti-inflammatory medication is limited. Corticosteroid injection into the enlarged bursa can be performed, but scientific evidence for its efficacy is absent, and these injections can lead to unfavourable complications, such as tendon ruptures and skin atrophy.
13.3.2 Inadequate Rehabilitation and Restoration of Structure, Strength, and Function
Principal considerations in this section centre around whether persisting structural, architectural, strength, control, or fatigue resistance deficits have been identified and addressed within the limited specific evidence relating to this cohort, largely due to the breadth of clinical presentations, which in many cases are multifactorial [39]. This requires a comprehensive and highly individualised approach to each case.
13.3.2.1 Altered Structural Integrity
These may include persisting deficits in the intramuscular aponeuroses and epimyseal or delaminating lesions of the tendon or aponeurosis of origin or insertion. There is conflicting opinion within the literature which variously apportions an increased rehabilitation interval, an increased likelihood of recurrence, or little significance to this aspect [40,41,42]. This may be due in part to the differing demands of the sport cohorts utilised or the distribution of sites. These issues may require specific rehabilitation restrictions or approaches, although this area requires further research to improve our current understanding.
13.3.2.2 Muscle Architecture
Muscle morphology, specifically shorter fascicle lengths in BFLH has been described as a risk factor for hamstring injury in the literature [22]. These authors recommend remedial loading through high-intensity, supramaximal eccentric-dominant exercises such as the Nordic hamstring or loaded eccentric hip extension exercise. Timmins and colleagues provide preliminary data suggesting protective thresholds for fascicle lengths in soccer players [43]. By extension, this approach may also be worthy of further exploration in better ensuring successful hamstring rehabilitation [44, 45], at least in at-risk groups.
13.3.2.3 Muscle Strength
Normalisation of hamstring muscle strength does not occur in the majority of athletes who are clinically recovered after a rehabilitation programme [46]. This isokinetic strength deficit at RTP was also not associated with a higher risk for reinjury. On the other hand, increasing hamstring strength levels and side-to-side strength balance in the hamstring group offers an opportunity to reduce the inherited risk of the athlete for recurrence in the first period after RTP [2]. This implies that hamstring strength deficit may be a more important risk factor to determine in the monitoring phase after RTP.
13.3.2.4 Muscle Fatigue
Fatigue of muscles has long been cited as a risk factor for hamstring injury, yet evidence until recently has been limited to early animal studies [47]. More recent work suggests one of the legacies of a previous hamstring injury within 2 years is the comparative reduction in ability to sustain repeated sprint performance [48]. This was despite a lack of differences between past history and control groups in factors such as maximal speed, leg strength, power, and flexibility. Another study demonstrated that repeated sprint efforts in a previously hamstring-injured group led to specific knee flexor and H:Q ratio peak torque deficits when compared to non-injured controls [49]. This fatigue-induced deficit correctly identified the injured side in all subjects. Additionally, increased investment in higher-speed running prior to return conferred increased protection against hamstring injury recurrence [17].
13.3.2.5 Kinetic Chain Considerations
There appears to be some value in the consideration of contributing factors within the kinetic chain as well as diminishing the risks inherited through previous hamstring injury and other injuries such as knee, anterior cruciate ligament, lumbar spine, and to a lesser extent quadriceps and calf [50]. While intrinsic hamstring issues are an important mainstay of rehabilitation, it is important to also address co-contributors across the kinetic chain including trunk, hip, gluteal, and calf function. Sherry and Best suggest the importance of trunk strength and stability [51]. Others found that older players had ipsilateral hip internal rotation deficits as risk factor [52]. Additionally, contralateral hip flexor tightness [53] and hip extensor strength deficits [54] have been associated with acute hamstring injury. This should be contrasted with a recent publication, describing knee flexor rather than hip extensor deficits persisted following a history of hamstring strain injury (HSI) in a male Australian rules football population [55]. Hip extensor strength however is not routinely tested clinically or in a research setting. It would appear, when faced with management of recurrent hamstring failure, cases should be assessed holistically and managed on an individual basis with a perspective that extends where necessary beyond the hamstring muscle group.
13.3.2.6 Hamstring Muscle Activation
Changes within the hamstring muscle group in terms of activation and coordination after injury have also been postulated but are poorly understood to date. Differential activity of individual hamstrings is described by several researchers [56,57,58], yet the evidence for changes from the “normal” in the hamstring-injured athlete in functional activities such as running and cutting is incomplete. Deeper understanding of activation or coordination changes within the medial or lateral hamstring groups or in synergists in normal, fatigued, and previously injured states are lacking. Bourne et al. [59] found reduced functional MRI changes specific to the BFLH muscle during performance of the Nordic hamstring exercise in athletes with a unilateral history of previous HSI. Silder et al. [60] also demonstrated significant loss of BFLH cross-sectional area assessed on MRI post-injury which appeared to be in part compensated for by hypertrophy of the BFSH. Further insights into differences between previously hamstring-injured and control athletes performing repeated contractions are available [61]. Schuermans et al. report a propensity for the hamstring-injured group towards earlier fatigue in ST, proposing possible overloading of the BF. However, both MRI and electromyogram studies have recognised shortcomings that challenge the validity of inferring individual muscle properties across the hamstring group. Notwithstanding these open findings, it would appear that in individual cases of recurrent BFLH failure, selective hypertrophy, fascicle length, activation, and synergy aspects may need to be specifically addressed.
13.4 Causes of Treatment Failure in Patients with Hamstring Tendinopathy
13.4.1 Incorrect Diagnosis
Proximal hamstring tendinopathy is a potential cause of pain in the buttock region. This condition is characterised by localised pain in the deep ischial tuberosity area, which is often worse during or after activities with hip flexion movements (such as running, lunging, and squatting). Sitting, especially on harder surfaces, often aggravates symptoms. The pain may radiate along the hamstrings to the posterior thigh [62].
Buttock pain may be caused by multiple other conditions, of which most are displayed in Table 13.2 [1]. Comprehensive examination of the lumbar spine, sacroiliac joint, and hip joint is needed to exclude other potential diagnoses. Sciatic nerve entrapment as a result of adhesions between the nerve and proximal hamstring tendon origin or in the buttock interfaces should be considered [63]. Slump testing may aid in identifying sciatic nerve involvement or referred pain, but this test lacks specificity as it might be painful in other conditions as well. Detailed palpation of the ischial and buttock areas can help in the differentiation between tendinopathy and sciatic nerve involvement. Localised pain at the ischial tuberosity is specific for PHT. More diffuse pain running from the buttock to the posterior thigh that cannot be reproduced on palpation is suggestive of neural pathology. While palpation should not be used as the sole diagnostic indicator, it will guide the clinician in the differential diagnosis.
A confirmed PHT that does not respond to therapy could also be caused by metabolic disorders [64]. Internal abnormalities, such as hypercholesterolemia, diabetes, or gout, should be considered as underlying causes. A rheumatic disorder, such as spondyloarthropathy, may have enthesitis as first presentation (Fig. 13.3). Medication is another cause of tendon pain. Use of specific antibiotics (quinolones) and statins is associated with tendon ruptures and tendinopathy.
Magnetic resonance imaging (MRI) of a hamstring tendinopathy and sacroiliitis caused by spondyloarthropathy. Panel (a) is an axial T2-weighted MR image that demonstrates right-sided increased signal intensity of the ischial tuberosity which is indicative of a bony cyst. There is also an increased thickness of the hamstring tendon origin. Panel (b) is a coronal T2-weighted MR image of the pelvis revealing increased signal intensity along the sacroiliac joints in the same patient. Based on the patient’s history and abnormalities on this MRI, this abnormality was interpreted as enthesitis and sacroiliitis caused by a spondyloarthropathy
The abovementioned diagnoses should be considered and corrected or treated in case of treatment failure in a patient with buttock pain. As most PHTs will take weeks to months to recover, there is no specific time point for tendinopathies to consider a treatment as “failing.” When a structured rehabilitation plan combined with load management does not improve symptoms within 8–12 weeks, a reevaluation and consideration of other potential diagnoses is recommended.
13.4.2 Inadequate Rehabilitation
It must be recognised that the evidence base surrounding hamstring tendinopathy rehabilitation is primarily that of case reports, pilot studies, clinical opinion, and narrative reviews. Failure of hamstring tendinopathy rehabilitation may be attributed to a number of factors relating to the overall structure and implementation of an individualised programme.
In the early stage of the rehabilitation, gaining control of symptoms through graduated progression of localised tensile loading and reduction of compression at the lateral ischium in both activities of daily living and in all exercises appears to be important. In patellar tendinopathy, isometric exercises with repeated 45 s holds at 70% of the maximum voluntary contraction have been shown to be promising in pain management and to address motor inhibition [65, 66]. However, these findings were not reproduced in patients with Achilles tendon pain [67]. This research has not been specifically reproduced for hamstring tendinopathy, yet this approach is considered to have some utility in early management, as it aids in early loading within tolerance [1, 9, 68]. Alternatively, eccentric exercise over the knee is proposed by others [69]. Almost all approaches describe commencement of loading with the hip in a neutral position to avoid compression of the common tendon against the inferolateral border of the ischium [70]. Isolation of the symptomatic tendon with application of an effective stimulus and monitoring of the response are the basic principles of this stage. These may require revisiting if the response is below expectation.
In the progression of rehabilitation, utilisation of the principles of heavy slow resistance training or similar strength-based approaches to address associated muscle atrophy appears to be fairly common [71]. Again, no evidence is available specifically for PHT. Initial avoidance of compression at the enthesis is progressed into a graduated reintroduction of the hip flexion component, which is vital to meet functional requirements. Most authors above describe increasing range of hip flexion along with this heavy slow resistance approach. Here, exercise selection is determined through these principles and in accordance with individual responses. As an alternative approach, a case report utilising a specific training programme based on loading the proximal hamstring tendon with slow eccentric exercises on a treadmill is also described [72].
Muscle wasting and strength loss are frequent presentations in this patient group, requiring effective exercise prescription to stimulate muscle hypertrophy. Typically, these sessions are performed three times weekly with an intervening day of lower muscle demand to allow recovery. It is generally been suggested these exercise sets consist of slow repetitions (typically 3 s concentric, 3 s eccentric) with sets of at least 60–70 s duration and maximal weight tolerated. Kongsgaard et al. progressed from 15 repetition maximum sets to six repetition maximum sets [71]. Shortcomings typically encountered are of insufficient isolation of the injured side, not enough resistance, exercises performed or progressed too quickly, or with poor focus on technique. Recent work suggests performing these exercises closely regimented by a metronome may enhance motor pathways [73].
Depending on the sporting requirements of the athlete, progression of rehabilitation to full functional range and elastic load demands on the hamstrings requires further progression of rate of loading of the tendon through graduated higher-speed challenges to the proximal hamstring tendon through activities such as bounding, stairs, and fast pushing/dragging activities, ultimately into RTS. Management errors across these stages include a lack of load quantification and careful progression of these higher-speed demands. While evidence is lacking for ideal programming in progressing later-stage tendinopathy, it does appear that the sensitised tendon is unable to tolerate this form of high loading on consecutive days. Evidence around the duration required for tendon adaptation to higher loading is very limited and relies heavily on early work [74]. Progress from 3-day intervals to 2-day intervals as the athlete returns to sport appears to be a more prudent approach, although monitoring of the response of the affected tendon to this loading in terms of latent symptoms is recommended.
Finally, in returning to sport, the gradual reintroduction of appropriate volumes of sport-specific challenges such as change of direction or volume of running to match the typical demands of training and competition is vital. Avoidance of training load peaks and troughs and gradual building of a protective moderate to high-load foundation are key aspects of a successful RTS [75]. Beyond RTS, there appears to be a requirement with most tendinopathies to continue a routine of strength maintenance and tendon load monitoring over a period of a year or two in order to prevent recurrence [76].
13.5 Management of Treatment Failure in Patients with Acute Hamstring Injuries
13.5.1 Conservative Management
The first step in the management of treatment failure is to reconsider the initial diagnosis and repeat a diagnostic workup to confirm the initial diagnosis. Part of this management includes an exploration of the differential diagnosis (see Table 13.1 for the differential diagnosis of posterior thigh pain). When the initially established diagnosis is correct—but the treatment response is not as expected—a change in conservative management may be considered.
There is a continuous search for treatments to improve and accelerate muscle healing, and a number of medical interventions additional to rehabilitation have been proposed. Especially when initial treatment fails, there is a high demand for additional medical interventions, which may put medical practitioners under pressure. We will discuss the most frequently applied treatment methods.
13.5.1.1 Anti-Inflammatory Medications
Treatment with anti-inflammatory medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids is aimed at reducing the inflammatory response after muscle injury: especially, the use of oral NSAIDs has been widespread. Historically, inflammation was believed to be detrimental for muscle injury healing. However, multiple recent studies have shown that the various phases of the inflammatory process play a critical role in orchestrating muscle regeneration following injury, and there is accumulating evidence that pharmacological inhibition of the inflammatory process actually impairs acute muscle healing [77].
In the field of acute muscle injuries, there is only one clinical randomised controlled trial (RCT) on the efficacy of NSAIDs. This RCT showed that NSAIDs do not exhibit an effect on hamstring pain and muscle strength compared to a placebo intervention [78].
Despite their widespread use, anti-inflammatory medications should not be used following an acute noncontact hamstring injury, as there is growing evidence that it is actually detrimental for muscle healing [79,80,81].
13.5.1.2 Injection Therapies
13.5.1.2.1 Platelet-Rich Plasma (PRP)
Platelet-rich plasma (PRP) is probably the most popular injection therapy for muscle injuries. Since the World Anti-Doping Agency permitted the intramuscular injection of PRP in 2011, this experimental treatment has been increasingly used to treat acute muscle injuries in athletes [82]. PRP is derived from autologous whole blood using centrifuge separation systems to separate the platelets from other blood components. When injected in the injured muscle, platelets release various growth factors like platelet-derived growth factor (PDGF), insulin-like growth factor (IGF-1), basic fibroblast growth factor (bFGF-2), and nerve growth factor (NGF). These growth factors are assumed to provide regenerative benefits to the injured muscle tissue by stimulating myoblast proliferation and accelerating muscle fibre regeneration. There are a multitude of autologous platelet-rich blood products commercially available that differ in their preparation procedure and cellular components. Superiority is often claimed for one PRP product over others, but it remains unproven whether the composition of the PRP is relevant for the efficacy of PRP treatments, and this is subject of an ongoing debate in the literature.
Basic science studies have shown that growth factors can stimulate myoblast proliferation, and in deliberately injured animal muscles, these growth factors increase regeneration [83]. Despite these promising results and apparent widespread clinical use, the positive effects of PRP have not been confirmed in scientific studies on human subjects. A meta-analysis with pooled data of six RCTs showed no superiority of PRP in treating muscle injuries on the time to RTP and the reinjury rate nor were any substantial differences found for pain, muscle strength, flexibility, muscle function, and imaging [84]. There is even evidence that a PRP injection in addition to rehabilitation may be detrimental for muscle healing. A laboratory study in rats demonstrated that rehabilitation alone was more effective for muscle healing than rehabilitation combined with PRP injections [85].
In conclusion, considering the lack of efficacy in high-level RCTs and evidence for a possible adverse effect on rehabilitation, we currently discourage PRP treatment in muscle injuries.
13.5.1.2.2 Actovegin®
Actovegin® is a deproteinised hemodialysate of ultrafiltered calf serum which is suggested to have antioxidant and antiapoptotic properties [86]. To date, there is only one non-randomised clinical pilot study that examined Actovegin® in muscle injury [87]. In this study, athletes with grade I injuries that were treated with Actovegin® injections returned to play significantly earlier (12 days on average, n = 4) than those that only received physiotherapy (20 days on average, n = 4). However, this pilot study is at high risk of bias due to the lack of blinding and randomisation. Future larger randomised studies, including placebo groups and assessment of potential side effects, are necessary to determine whether Actovegin® injections are safe and effective. We do not currently recommend it as a treatment for hamstring injuries.
13.5.1.2.3 Traumeel®
Traumeel® is a homeopathic combination of diluted plant and mineral extracts which is proposed to have an anti-inflammatory effect [88]. This injection therapy is used alone or in combination with Actovegin® in muscle injuries [89], but there is currently no evidence on the effect of intramuscular injection of Traumeel® in muscle injuries.
13.5.1.2.4 Stem Cells
There is increasing interest for the use of stem cell therapy in muscle injuries. Stem cells are undifferentiated cells that can renew themselves or differentiate into cells that are programmed for a certain tissue lineage. These cells may have the ability to contribute to muscle regeneration after injury. Therefore, the concept of transplanting stem cells has been explored for some time; however, the available literature focuses mostly on degenerative muscle disorders, such as muscular dystrophies.
Studies on stem cells in acute injury are currently limited to two murine contusion model studies [90, 91]. These studies found that intramuscular transplantation of muscle-derived stem cells promoted angiogenesis and increased the number and diameter of regenerative muscle fibres. Although these findings are promising, it is not known whether the same results can be found in human muscle tissue. Furthermore, concerns have been raised regarding the potential tumourigenic risk of stem cells.
Despite promising results, we currently do not advocate the use of stem cells in hamstring injuries, as their safety and efficacy in human use are yet to be determined.
In conclusion, the current available evidence does not support any of the available interventions in addition to active rehabilitation in acute muscle injury. For some, there is even (indirect) evidence that they may adversely affect outcome of muscle injury.
13.5.2 Surgical Management
With the exception of complete discontinuity of the bone-tendon-muscle unit (i.e. tendon avulsion injury), surgery is very rarely considered as the primary treatment for hamstring injury. One might even say that, in the setting of managing non-acute hamstring injuries, it can be regarded as a last resort or sometimes even a salvage procedure.
However, part of the challenge of managing muscle injuries that predominantly occur in athletes is to prevent a scenario of treatment failure. Surgical intervention in the acute setting might be warranted in order to avoid such a scenario.
In this paragraph, we will briefly go over the indications for surgery in acute hamstring injuries, as well as surgical treatment for acute hamstring injuries in which conservative management has yielded insufficient improvement.
13.5.2.1 Tendon Avulsion Injury
To date, evidence-based indications for surgical intervention are lacking for hamstring tendon avulsion injury. This may be attributed to a scarcity of controlled studies and the striking underrepresentation of conservatively treated cases in published literature that impede a proper comparison of treatment outcomes [8, 92, 93]. Cohen and Bradley [94, 95] have suggested that surgical repair of the ruptured tendons is indicated in two-tendon avulsions with more than 2 cm of retraction and three-tendon avulsions regardless of the extent of retraction. Without a scientific basis for these criteria and the very limited knowledge of the natural course of this injury, this should be regarded as expert opinion.
Surgical repair of proximal hamstring tendon avulsions comprises protection of the sciatic nerve, mobilisation of ruptured tendons, and fixation of the mobilised tendons to the ischial tuberosity with suture anchors [8].
Based on the most recent and comprehensive systematic review [92], surgical repair resulted in significantly higher patient satisfaction, better hamstring strength recovery, and higher scores on single-leg hop tests and functional testing scales compared to conservative treatment. Strikingly, surgical repair did not significantly improve the chance of returning to sports or pre-injury activity level.
Early (i.e. within 8 weeks after injury) surgical intervention leads to significantly higher patient satisfaction, less residual pain, and higher scores on functional scales compared to delayed intervention [92]. Conversely, there is no difference in rate of RTS or pre-injury activity level, hamstring strength, hamstring endurance, and Tegner scores. Moreover, it is often mentioned that delayed intervention is technically more demanding due to development of adhesions requiring a more extensive neurolysis of the sciatic nerve [8], as well as increased retraction of the ruptured tendons [96]. In the latter case, re-approximation can be more difficult, and sometimes, an allograft or autograft reconstruction is needed to bridge a remaining gap or augment the repair [8]. Interestingly, no significant difference in complications between acute and delayed intervention was found [92].
Distal tendon avulsions make up about 2% of all hamstring injuries and are therefore less common than proximal tendon avulsions [97]. As one would expect, the literature is also more limited.
Lempainen et al. [98] retrospectively analysed 18 operatively treated patients with distal hamstring tears, five of whom had full-thickness tears involving either the distal tendon or musculotendinous junction. In case of a free tendon avulsion, refixation was achieved by means of suture anchors. In case of a tear through the musculotendinous junction, sutures were used following excision of any scar tissue. All five patients were able to RTS at pre-injury level without residual complaints after 2–6 months.
The current literature does not allow for a comparison between conservative and surgical treatment. Moreover, it may not be appropriate to pool distal tears of the three different hamstring muscles as they have different functions with respect to dynamic stabilisation of the knee joint.
13.5.2.2 Intramuscular Tendon Injury
In recent years, hamstring muscle injury with intramuscular (or “central”) tendon involvement (Fig. 13.4) has become notorious because of initial observations that it might lead to disastrous outcome [99]. To be more specific, these injuries were noted to take three to four times as long to recover [41, 100] and were found to have significantly higher recurrence rates [100]. However, when athletes were treated by a physiotherapist blinded to imaging findings, using a criteria-based rehabilitation programme, differences were notably smaller [101]. The difference in time to RTP between injuries without tendon involvement (mean 22 days) and those with full-thickness intramuscular tendon disruption (mean 32 days) was approximately a week and a half. Moreover, reinjury rates within 12 months after RTP for injuries with and without tendon disruption (both 20%) were not significantly different [40].
Magnetic resonance imaging (MRI) of an intramuscular tendon injury. Coronal STIR images demonstrating right-sided increased signal intensity in a feather-shaped pattern located in the proximal BF (long head). Panel (a) depicts a musculotendinous injury without intramuscular tendon injury. Panel (b) depicts an injury with partial-thickness intramuscular tendon injury, as evidenced by increased intratendinous signal intensity, intramuscular tendon disruption, and tendon waviness
Based on this relatively small difference in time to RTP between “regular” hamstring injury and “severe” intramuscular tendon injury, we argue that these intramuscular tendon injuries should not primarily be treated surgically. However, as is the case for persistent or recurrent musculotendinous injuries, there might be a role for surgery in cases that are refractory to conservative strategies.
Lempainen et al. [102] published a case series of eight athletes with intramuscular tendon injuries that were surgically treated. The indication for surgery in acute cases was a full-thickness disruption with a clear gap between tendon ends. For chronic cases, surgical indications included recurrent disabling injury and inability to participate in competitive sports at pre-injury level. The surgical technique depended on the location of the injury and whether it was acute or recurrent. In acute injuries, tendon ends were approximated and sutured. In recurrent injuries, the tendon was repaired using a gliding Z-plasty (i.e. a surgical technique to increase tendon length). When the injury was in proximity to the ischial tuberosity, a suture anchor was placed for additional support of the repair.
All athletes returned to sports at pre-injury level between 2.5 and 4.5 months postoperatively. It should be emphasised that controlled clinical studies on the efficacy of surgical treatment for this condition are lacking.
13.5.2.3 Musculotendinous Injury
The bulk of hamstring injuries do not demonstrate signs of proximal or distal tendon involvement [97, 103], and they are predominantly located at or near the proximal musculotendinous junction. While it is a common injury in sports that usually heals well with conservative treatment [16], it is an injury that should be taken seriously. One of the major problems is a high tendency to recur [3]. For whatever reason, every clinician will have at least one case of an athlete who has sustained injury after injury, usually in the same location [104].
On rare occasions, these recurrent (or persistent) injuries have been managed surgically. One study described a series of 18 distal hamstring tears [98], of which 12 were partial-thickness tears of the musculotendinous junction. Surgical treatment was carried out when athletes were unable to participate in sports at the pre-injury level after at least 6 weeks post-injury. The intervention comprised excision of scar tissue and mobilisation of the injured muscle to ensure there was no restriction due to adhesions, followed by suturing. Eight athletes (67%) returned to sports at pre-injury level after 2–5 months postoperatively, seven of which without any residual symptoms.
Surgery for hamstring injuries is rarely indicated in the acute setting. With the exception of tendinous or bony avulsion, surgical consultation should be postponed until the point at which conservative treatment strategies have insufficiently improved function or symptoms. Based on the limited evidence that is currently at our disposal, surgery appears to be beneficial in these cases and leads to a good chance of returning to sports at pre-injury level. Yet, due to lack of controlled studies, it is unknown whether this approach should be preferred over continuing conservative approaches.
13.6 Management of Treatment Failure in Patients with Ongoing Posterior Thigh Pain, Including Hamstring Injury Sequelae
13.6.1 Conservative Management
Hamstring injury sequelae are challenging to manage and scientific knowledge is limited. We advise to optimise deficits in hamstring strength and flexibility, and to perform a progressive rehabilitation. Although this is the current mainstay of treatment for these patients, there is a subgroup of patients that will remain symptomatic, regardless of treatment.
13.6.2 Surgical Management
Surgery for hamstring injuries is rarely indicated in the acute setting, as described above (Sect. 13.5.1). This also accounts for hamstring injury sequelae. One underlying cause of hamstring injury sequela might be a myositis ossificans.
Myositis ossificans that results in persisting complaints of pain and impaired function with restricted sports activities despite conventionally accepted treatment may benefit from surgery. While this approach is often employed in clinical practice, it is unclear at what point exactly one should regard the conservative treatment as failed and when surgery might be indicated. There are no evidence-based guidelines or controlled studies that can serve as the basis for recommendations with regard to if and when surgery should be performed.
Considering that symptoms and dysfunction tend to regress as the lesion matures over the course of months, sufficient time should be allowed for conservative strategies to elicit an effect. In addition, surgical excision before the lesion has fully matured is traditionally believed to result in local recurrence. Therefore, surgical intervention is generally discouraged before at least 6–12 months after the injury [25].
In a recent study, clinical outcome was reported for high-level athletes undergoing isolated excision of a heterotopic ossification [25]. In most cases (84%), the lesion was located in one of the muscle groups in the thigh region. Following the intervention, indomethacin was administered for 3 weeks, and RTS was allowed 4–6 weeks postoperatively. Overall, surgery resulted in clinical improvement, and the vast majority (97%) was able to return to their pre-injury activity level. Most athletes (81%) were able to return to this level with no or mild residual complaints of pain during activity. With the exception of hypoesthesia at the periphery of the skin incision, there were no complications.
In summary, traumatic myositis ossificans is a self-limiting condition that rarely requires surgery. There are currently no evidence-based surgical indications. In athletes with persisting complaints of pain and dysfunction despite adequate and prolonged conservative treatment, surgical excision of a heterotopic bone appears to result in clinical improvement with a good chance of returning to pre-injury activity.
13.7 Management of Treatment Failure in Patients with Hamstring Tendinopathy
13.7.1 Conservative Management
Management of treatment-resistant PHT starts with reconsidering the initial diagnosis (Table 13.2), reevaluating the treatment strategy, repeating diagnostic workup for buttock pain, and performing additional diagnostics if needed.
It is worth mentioning that exercise-based rehabilitation normally takes weeks to months before a treatment effect can be expected [1]. It is therefore important to set realistic time frames before the start of conservative treatment. This will prevent unnecessary requests for additional diagnostics resulting in increased healthcare costs.
When the initial diagnosis is confirmed, medical therapies may be considered for long-standing PHT that is resistant to exercise-based rehabilitation.
13.7.1.1 Medical Treatment Modalities
Proximal hamstring tendinopathy appears to be something of an “ugly duckling” in the literature on tendinopathy. While the current body of evidence on treatment of Achilles and patellar tendinopathy is rapidly expanding, evidence for treatment of PHT is lagging behind. For distal hamstring tendinopathy, this is even more striking.
13.7.1.2 Nonsteroidal Anti-Inflammatories (NSAIDs)
There is limited evidence that NSAIDs can provide a reduction in symptoms in patients with reactive tendinopathy [76]. The mechanism behind NSAID treatment in this phase may be decreased tendon cell proliferation and simultaneous decreased proteoglycan production. Rest and NSAIDs are less favourable in cases of chronic tendinopathy. Rest can have an initial positive effect on symptoms, but it has also been shown to induce a reduction in the amount of collagen. NSAIDs have fallen out of favour for long-standing tendinopathy, as there is no evidence for their efficacy [105].
13.7.1.3 Extracorporeal Shock Wave Therapy (ESWT)
Another frequently applied treatment in tendinopathy is extracorporeal shock wave therapy (ESWT), which delivers an energy flux through the tendon collagen tissue. ESWT is thought to initiate biological responses and tissue regeneration, but this effect is mainly based on laboratory studies. There is one randomised study on the efficacy of ESWT in athletes with PHT [106]. This study showed that ESWT is safe and more effective than exercise alone, although there were some study limitations (small sample size, a lack of disease-specific measurements, and absence of placebo ESWT and blinding of participants). A recent systematic review demonstrated conflicting evidence for the efficacy of ESWT in lower limb tendinopathies [107, 108]. More evidence is needed to define the efficacy of ESWT treatment in PHT. There might be a subgroup of patients that responds well to this treatment, but to date, it is unknown which patients are good responders.
13.7.1.4 Injection Therapies
Effectiveness of local corticosteroid injections for tendinopathy has mainly been described in case reports or case series [109], but no large randomised studies with long-term follow-up have been performed in patients with lower extremity tendinopathy. Effects of corticosteroid injections are not known for PHT. A systematic review showed that corticosteroids in tendinopathy are effective in the short term but detrimental in the longer term [110]. There is also an association between these injections and occurrence of a total tendon rupture [111]. While the efficacy and safety of corticosteroids is described for tendinopathies in general in these studies [110, 111], it is unknown whether these results can be extrapolated to patients with PHT. A total tendon rupture of the proximal hamstring tendons is a severe complication with dramatic consequences for an athlete. Therefore, clinicians should be cautious with applying intratendinous hamstring injections.
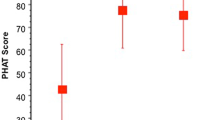
There are numerous other injection treatments that are proposed for tendinopathies. Injection agents that have been used include polidocanol (sclerosing therapy), dextrose (prolotherapy), and autologous blood and PRP. In PHT, no studies have been performed on the effect of sclerosing therapy or prolotherapy. The fact that the sciatic nerve is running next to the hamstring tendon makes it less attractive to inject a sclerosing agent. Prolotherapy results in temporary irritation of this nerve, which can be annoying for patients. There is also no strong evidence for these injection therapies in other tendinopathy locations [112]. Autologous blood injections and PRP injections are used with the aim to deliver growth factors with regenerative effects on the tendon tissue. The use of autologous whole blood and PRP treatment has been evaluated in one randomised study in patients with PHT [113]. Both treatments resulted in an improvement over time, but it is unknown whether these injections are better than other conservative treatments or a “wait-and-see” approach.
In conclusion, there is currently no strong evidence for the effectiveness of second-line treatment options when exercise therapy and load management advice failed for patients with long-standing PHT. Some of the abovementioned options may be considered if the potential benefits and harms are discussed on beforehand with the patient.
13.7.2 Surgical Management
While the histopathological characteristics seen in hamstring tendinopathy correspond with findings in other tendinopathies [1], distinct anatomical features may play a role in the decision-making progress. Therefore, in this section, we will focus specifically on surgical treatment of PHT.
As is the case with almost all musculoskeletal injuries in the athletic population, the primary treatment is conservative [63]. Owing to its heterogeneous presentation and response to treatment, the challenge lies in determining the optimal treatment and the point at which conservative treatment has “failed” and when a surgical approach may be beneficial.
According to a recent review, about one in every five patients experiences persisting symptoms after 6 months of conservative treatment [63]. This point in time has been suggested as the moment at which surgery should at least be considered.
Moreover, the decision for surgical intervention should not only include the duration of symptoms and response to conservative treatments but also the suspected cause of the persisting symptoms. Tendinopathic pain is thought to be related to a combination of neurovascular ingrowth and production of biomechanical substances (e.g. catecholamines, acetylcholine, glutamate) [62]. Yet, it has been postulated that complaints of pain may also arise from compression of the sciatic nerve [114], which runs in close proximity to the proximal hamstring tendons [115]. Compression resulting from adhesions between the nerve and proximal tendons or direct compression caused by thickening of the proximal tendons, previously also referred to as “hamstring syndrome” [1], may need to be addressed as well in order to improve or resolve pain.
Outcome following surgical intervention has only been investigated using retrospective study designs [1, 63, 116]. In the study by Lempainen et al. [63], 103 cases of PHT in 90 athletes were reported. Surgery was indicated when patients experienced chronic and disturbing symptoms despite conservative treatment. Conservative treatments included modification or suspension of sports activities, hamstring stretching, NSAIDs, corticosteroid injections, and physiotherapy. In almost all cases (97%), surgery was performed after symptoms persisted for at least 6 months.
The authors noted that the proximal SM tendon was commonly thickened. Hence, their surgical technique involved a transverse tenotomy of the (thickened) lateral proximal SM tendon several centimetres distal to the ischial tuberosity. Additionally, any adhesions around the sciatic nerve were carefully removed. The distal part was then sutured to the proximal tendon of the long head of the BF in order to prevent retraction of the muscle. Postoperatively, weight-bearing was gradually progressed in the first 2 weeks, and in the first 3–4 weeks, care was taken to avoid excessive stretching of the hamstrings. Isometric exercises and cycling were started at 4 weeks, and weight training and running were started at 8 weeks. Return to full sporting activities was allowed at 2–4 months postoperatively [63].
Surgery resulted in a high rate of RTS at the pre-injury level (89%) after a mean 5 months with no (60%) or minor symptoms (29%) during activity. The complication rate was 10%. Minor complications included DVT (1%), wound fistula (1%), and transient hyperesthesia of the incisional area (2%). Six cases required a reoperation, four due to early symptoms resulting from scar tissue around the hamstring origin and sciatic nerve and two due to late recurring complaints resulting from a regenerated SM tendon.
Benazzo et al. [115] reported the outcomes of 17 athletes who underwent surgery for persisting complaints of PHT that caused limitations or interfered with sport participation. Conservative treatments prior to surgery included physiotherapy, NSAIDs, and corticosteroid injection. All patients had persisting complaints despite a course of conservative treatment of at least 3 months.
The surgical technique involved identification of the involved (i.e. hypertrophic and fibrotic) tendon, followed by a partial transverse tenotomy or repeated puncturing of the tendon and a release of the sciatic nerve. Directly postoperatively, continuous passive motion of the hip and knee was started. Active motion was encouraged from the first day after surgery, and weight-bearing was progressed during the first 10 days. Progressive strengthening was started in the second week and progressed from open to closed kinetic chain after 4 weeks. Running was allowed after 8 weeks.
All patients were able to RTS at pre-injury level after a mean 4 months, either with no residual symptoms (88%) or pain during intense efforts (12%). The complication rate was 12%, including postoperative hematoma and transient hyperesthesia of the incisional area.
Both surgical techniques are similar in the sense that they involve lysis of adhesions in addition to a (partial) tenotomy. These perineural or peritendinous adhesions, which are also observed during surgery for chronic Achilles tendinopathy [116], might play an interesting role with respect to failure of conservative treatment and outcome of surgical treatment.
It should be noted that no prospective controlled studies have been conducted. It is therefore not known whether surgery is superior to conservative treatments in patients with chronic symptoms. Based on the current available evidence, the sole conclusion that can be drawn is that surgical treatment for refractory PHT appears a viable secondary option.
13.8 Conclusion
Treatment failure, defined as an unsuccessful result of management, is observed on a frequent basis in both acute and long-standing hamstring injuries, and it is due to either an incorrect diagnosis or inadequate response to treatment. There is a large range of differential diagnoses that can be considered in patients with treatment failure after acute and long-standing hamstring injuries. Reevaluation of the patient and expanding diagnostic workup are potential options to explain treatment failure. Numerous alternative treatment options for patients with acute hamstring injuries, hamstring injury sequelae, and hamstring tendinopathy are available. In general, there is no strong evidence for the efficacy of these alternative treatment options. Almost all second-line treatment effects are based on level 4 evidence. When considering these treatments, potential adverse events, healthcare costs, and likelihood of efficacy should be taken into account.
References
Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal hamstring tendinopathy: clinical aspects of assessment and management. J Orthop Sports Phys Ther. 2016;46(6):483–93.
de Vos RJ, Reurink G, Goudswaard GJ, Moen MH, Weir A, Tol JL. Clinical findings just after return to play predict hamstring re-injury, but baseline MRI findings do not. Br J Sports Med. 2014;48(18):1377–84.
de Visser HM, Reijman M, Heijboer MP, Bos PK. Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med. 2012;46(2):124–30.
Wangensteen A, Almusa E, Boukarroum S, Farooq A, Hamilton B, Whiteley R, et al. MRI does not add value over and above patient history and clinical examination in predicting time to return to sport after acute hamstring injuries: a prospective cohort of 180 male athletes. Br J Sports Med. 2015;49(24):1579–87.
Reurink G, Goudswaard GJ, Moen MH, Weir A, Verhaar JA, Bierma-Zeinstra SM, et al. Platelet-rich plasma injections in acute muscle injury. N Engl J Med. 2014;370(26):2546–7.
van der Plas A, de Jonge S, de Vos RJ, van der Heide HJ, Verhaar JA, Weir A, et al. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. Br J Sports Med. 2012;46(3):214–8.
Reurink G, Goudswaard GJ, Moen MH, Weir A, Verhaar JA, Bierma-Zeinstra SM, et al. Rationale, secondary outcome scores and 1-year follow-up of a randomised trial of platelet-rich plasma injections in acute hamstring muscle injury: the Dutch Hamstring Injection Therapy study. Br J Sports Med. 2015;49(18):1206–12.
van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43(11):2841–51.
Beatty NR, Felix I, Hettler J, Moley PJ, Wyss JF. Rehabilitation and prevention of proximal hamstring tendinopathy. Curr Sports Med Rep. 2017;16(3):162–71.
Hofmann KJ, Paggi A, Connors D, Miller SL. Complete avulsion of the proximal hamstring insertion: functional outcomes after nonsurgical treatment. J Bone Joint Surg Am. 2014;96(12):1022–5.
van der Made AD, Peters RW, Verheul C, Maas M, Kerkhoffs GM. Abduction in proximal hamstring tendon avulsion injury mechanism—a report on 3 athletes. Clin J Sport Med. 2017.
Ferlic PW, Sadoghi P, Singer G, Kraus T, Eberl R. Treatment for ischial tuberosity avulsion fractures in adolescent athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):893–7.
Gidwani S, Bircher MD. Avulsion injuries of the hamstring origin – a series of 12 patients and management algorithm. Ann R Coll Surg Engl. 2007;89(4):394–9.
Schuett DJ, Bomar JD, Pennock AT. Pelvic apophyseal avulsion fractures: a retrospective review of 228 cases. J Pediatr Orthop. 2015;35(6):617–23.
Obey MR, Broski SM, Spinner RJ, Collins MS, Krych AJ. Anatomy of the adductor Magnus origin: implications for proximal hamstring injuries. Orthop J Sports Med. 2016;4(1):2325967115625055.
Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745–64.
Stares J, Dawson B, Peeling P, Drew M, Heasman J, Rogalski B, et al. How much is enough in rehabilitation? High running workloads following lower limb muscle injury delay return to play but protect against subsequent injury. J Sci Med Sport. 2018;21(10):1019–24.
Timmins RG, Shield AJ, Williams MD, Lorenzen C, Opar DA. Architectural adaptations of muscle to training and injury: a narrative review outlining the contributions by fascicle length, pennation angle and muscle thickness. Br J Sports Med. 2016;50(23):1467–72
Askling CM, Nilsson J. Thorstensson A. a new hamstring test to complement the common clinical examination before return to sport after injury. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1798–803.
Guex K, Degache F, Morisod C, Sailly M, Millet GP. Hamstring architectural and functional adaptations following long vs short muscle length eccentric training. Front Physiol. 2016;7:340.
Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15(6):436–41.
Timmins RG, Bourne MN, Shield AJ, Williams MD, Lorenzen C, Opar DA. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med. 2016;50(24):1524–35.
Alessandrino F, Balconi G. Complications of muscle injuries. J Ultrasound. 2013;16(4):215–22.
Marques JP, Pinheiro JP, Santos Costa J, Moura D. Myositis ossificans of the quadriceps femoris in a soccer player. BMJ Case Rep. 2015;2015.
Orava S, Sinikumpu JJ, Sarimo J, Lempainen L, Mann G, Hetsroni I. Surgical excision of symptomatic mature posttraumatic myositis ossificans: characteristics and outcomes in 32 athletes. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3961–8.
Walczak BE, Johnson CN, Howe BM. Myositis ossificans. J Am Acad Orthop Surg. 2015;23(10):612–22.
Hernando MF, Cerezal L, Perez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skelet Radiol. 2015;44(7):919–34.
Campbell WW, Landau ME. Controversial entrapment neuropathies. Neurosurg Clin N Am. 2008;19(4):597–608.
Martin R, Martin HD, Kivlan BR. Nerve entrapment in the hip region: current concepts review. Int J Sports Phys Ther. 2017;12(7):1163–73.
Meknas K, Christensen A, Johansen O. The internal obturator muscle may cause sciatic pain. Pain. 2003;104(1–2):375–80.
Carro LP, Hernando MF, Cerezal L, Navarro IS, Fernandez AA, Castillo AO. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles Ligaments Tendons J. 2016;6(3):384–96.
Mobbs RJ, Szkandera B, Blum P. Posterior femoral cutaneous nerve entrapment neuropathy: operative exposure and technique. Br J Neurosurg. 2002;16(3):309–11.
Collaborators I. Diagnosis and management of iliac artery endofibrosis: results of a Delphi consensus study. Eur J Vasc Endovasc Surg. 2016;52(1):90–8.
Lutterbach-Penna RA, Kalume-Brigido M, Robertson BL, Jacobson JA, Girish G, Fessell DP. Deep vein thrombosis simulating hamstring injury on sonography. J Ultrasound Med. 2012;31(4):660–2.
Kahn SR, et al. Correction. The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2015;131(8):e359.
DeFranco MJ, Recht M, Schils J, Parker RD. Stress fractures of the femur in athletes. Clin Sports Med. 2006;25(1):89–103.
Davis KW. Imaging of the hamstrings. Semin Musculoskelet Radiol. 2008;12(1):28–41.
Van Mieghem IM, Boets A, Sciot R, Van Breuseghem I. Ischiogluteal bursitis: an uncommon type of bursitis. Skelet Radiol. 2004;33(7):413–6.
Mendiguchia J, Alentorn-Geli E, Brughelli M. Hamstring strain injuries: are we heading in the right direction? Br J Sports Med. 2012;46(2):81–5.
van der Made AD, Almusa E, Reurink G, Whiteley R, Weir A, Hamilton B, et al. Intramuscular tendon injury is not associated with an increased hamstring reinjury rate within 12 months after return to play. In: Br J Sports Med; 2018;52(19):1261–66
Comin J, Malliaras P, Baquie P, Barbour T, Connell D. Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med. 2013;41(1):111–5.
Entwisle T, Ling Y, Splatt A, Brukner P, Connell D, Distal Musculotendinous T. Junction injuries of the biceps femoris: an MRI case review. Orthop J Sports Med. 2017;5(7):2325967117714998.
Opar DA, Drezner J, Shield A, Williams M, Webner D, Sennett B, et al. Acute hamstring strain injury in track-and-field athletes: a 3-year observational study at the Penn Relay Carnival. Scand J Med Sci Sports. 2014;24(4):e254–9.
Timmins RG, Ruddy JD, Presland J, Maniar N, Shield AJ, Williams MD, Opar DA. Architectural changes of the biceps femoris long head after concentric or eccentric training. Med Sci Sports Exerc. 2016;48(3):499–508.
Alonso-Fernandez D, Docampo-Blanco P, Martinez-Fernandez J. Changes in muscle architecture of biceps femoris induced by eccentric strength training with nordic hamstring exercise. Scand J Med Sci Sports. 2018;28(1):88–94.
Tol JL, Hamilton B, Eirale C, Muxart P, Jacobsen P, Whiteley R. At return to play following hamstring injury the majority of professional football players have residual isokinetic deficits. Br J Sports Med. 2014;48(18):1364–9.
Mair SD, Seaber AV, Glisson RR, Garrett WE Jr. The role of fatigue in susceptibility to acute muscle strain injury. Am J Sports Med. 1996;24(2):137–43.
Roksund OD, Kristoffersen M, Bogen BE, Wisnes A, Engeseth MS, Nilsen AK, et al. Higher drop in speed during a repeated sprint test in soccer players reporting former hamstring strain injury. Front Physiol. 2017;8:25.
Lord C, Ma’ayah F, Blazevich AJ. Change in knee flexor torque after fatiguing exercise identifies previous hamstring injury in football players. Scand J Med Sci Sports. 2018;28(3):1235–43.
Toohey LA, Drew MK, Cook JL, Finch CF, Gaida JE. Is subsequent lower limb injury associated with previous injury? A systematic review and meta-analysis. Br J Sports Med. 2017;51(23):1670–8.
Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):116–25.
Gabbe BJ, Bennell KL, Finch CF. Why are older Australian football players at greater risk of hamstring injury? J Sci Med Sport. 2006;9(4):327–33.
Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40(16):3555–62.
Higashihara A, Nagano Y, Takahashi K, Fukubayashi T. Effects of forward trunk lean on hamstring muscle kinematics during sprinting. J Sports Sci. 2015;33(13):1366–75.
Charlton PC, Raysmith B, Wollin M, Rice S, Purdam C, Clark RA, et al. Knee flexion not hip extension strength is persistently reduced following hamstring strain injury in Australian Football athletes: implications for periodic health examinations. J Sci Med Sport. 2018.
Besier TF, Sturnieks DL, Alderson JA, Lloyd DG. Repeatability of gait data using a functional hip joint centre and a mean helical knee axis. J Biomech. 2003;36(8):1159–68.
Bourne MN, Williams MD, Opar DA, Al Najjar A, Kerr GK, Shield AJ. Impact of exercise selection on hamstring muscle activation. Br J Sports Med. 2017;51(13):1021–8.
Mendiguchia J, Garrues MA, Cronin JB, Contreras B, Los Arcos A, Malliaropoulos N, et al. Nonuniform changes in MRI measurements of the thigh muscles after two hamstring strengthening exercises. J Strength Cond Res. 2013;27(3):574–81.
Bourne MN, Opar DA, Williams MD, Al Najjar A, Shield AJ. Muscle activation patterns in the Nordic hamstring exercise: impact of prior strain injury. Scand J Med Sci Sports. 2016;26(6):666–74.
Silder A, Heiderscheit BC, Thelen DG, Enright T, Tuite MJ. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skelet Radiol. 2008;37(12):1101–9.
Schuermans J, Van Tiggelen D, Danneels L, Witvrouw E. Susceptibility to hamstring injuries in soccer: a prospective study using muscle functional magnetic resonance imaging. Am J Sports Med. 2016;44(5):1276–85.
Lempainen L, Johansson K, Banke IJ, Ranne J, Makela K, Sarimo J, et al. Expert opinion: diagnosis and treatment of proximal hamstring tendinopathy. Muscles Ligaments Tendons J. 2015;5(1):23–8.
Lempainen L, Sarimo J, Mattila K, Vaittinen S, Orava S. Proximal hamstring tendinopathy: results of surgical management and histopathologic findings. Am J Sports Med. 2009;37(4):727–34.
Ackermann PW, Hart DA. General overview and summary of concepts regarding tendon disease topics addressed related to metabolic disorders. Adv Exp Med Biol. 2016;920:293–8.
Rio E, Kidgell D, Moseley GL, Cook J. Elevated corticospinal excitability in patellar tendinopathy compared with other anterior knee pain or no pain. Scand J Med Sci Sports. 2016;26(9):1072–9.
Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015;49(19):1277–83.
O’Neill S, Radia J, Bird K, Rathleff MS, Bandholm T, Jorgensen M, et al. Acute sensory and motor response to 45-s heavy isometric holds for the plantar flexors in patients with Achilles tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2765–73.
Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. Phys Sportsmed. 2005;33(5):32–43.
Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. J Orthop Sports Phys Ther. 2014;44(3):198–205.
Cook JL, Purdam C. Is compressive load a factor in the development of tendinopathy? Br J Sports Med. 2012;46(3):163–8.
Kongsgaard M, Kovanen V, Aagaard P, Doessing S, Hansen P, Laursen AH, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sports. 2009;19(6):790–802.
Cushman D, Rho ME. Conservative treatment of subacute proximal hamstring tendinopathy using eccentric exercises performed with a treadmill: a case report. J Orthop Sports Phys Ther. 2015;45(7):557–62.
Rio E, Moseley L, Purdam C, Samiric T, Kidgell D, Pearce AJ, et al. The pain of tendinopathy: physiological or pathophysiological? Sports Med. 2014;44(1):9–23.
Kjaer M, Langberg H, Heinemeier K, Bayer ML, Hansen M, Holm L, et al. From mechanical loading to collagen synthesis, structural changes and function in human tendon. Scand J Med Sci Sports. 2009;19(4):500–10.
Drew MK, Purdam C. Time to bin the term ‘overuse’ injury: is ‘training load error’ a more accurate term? Br J Sports Med. 2016;50(22):1423–4.
Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43(6):409–16.
Duchesne E, Dufresne SS, Dumont NA. Impact of inflammation and anti-inflammatory modalities on skeletal muscle healing: from fundamental research to the clinic. Phys Ther. 2017;97(8):807–17.
Reynolds JF, Noakes TD, Schwellnus MP, Windt A, Bowerbank P. Non-steroidal anti-inflammatory drugs fail to enhance healing of acute hamstring injuries treated with physiotherapy. S Afr Med J. 1995;85(6):517–22.
Mishra DK, Friden J, Schmitz MC, Lieber RL. Anti-inflammatory medication after muscle injury. A treatment resulting in short-term improvement but subsequent loss of muscle function. J Bone Joint Surg Am. 1995;77(10):1510–9.
Warren P, Gabbe BJ, Schneider-Kolsky M, Bennell KL. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br J Sports Med. 2010;44(6):415–9.
Jarvinen TA, Jarvinen M, Kalimo H. Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J. 2013;3(4):337–45.
Hamilton B, Knez W, Eirale C, Chalabi H. Platelet enriched plasma for acute muscle injury. Acta Orthop Belg. 2010;76(4):443–8.
Hamilton BH, Best TM. Platelet-enriched plasma and muscle strain injuries: challenges imposed by the burden of proof. Clin J Sport Med. 2011;21(1):31–6.
Grassi A, Napoli F, Romandini I, Samuelsson K, Zaffagnini S, Candrian C, et al. Is platelet-rich plasma (PRP) effective in the treatment of acute muscle injuries? A systematic review and meta-analysis. Sports Med. 2018;48(4):971–89.
Contreras-Munoz P, Torrella JR, Serres X, Rizo-Roca D, De la Varga M, Viscor G, et al. Postinjury exercise and platelet-rich plasma therapies improve skeletal muscle healing in rats but are not synergistic when combined. Am J Sports Med. 2017;45(9):2131–41.
Brock J, Golding D, Smith PM, Nokes L, Kwan A, Lee PYF. Update on the role of Actovegin in musculoskeletal medicine: a review of the past 10 years. Clin J Sport Med. 2018.
Lee P, Rattenberry A, Connelly S, Nokes L. Our experience on Actovegin, is it cutting edge? Int J Sports Med. 2011;32(4):237–41.
Schneider C. Traumeel – an emerging option to nonsteroidal anti-inflammatory drugs in the management of acute musculoskeletal injuries. Int J Gen Med. 2011;4:225–34.
Wright-Carpenter T, Klein P, Schaferhoff P, Appell HJ, Mir LM, Wehling P. Treatment of muscle injuries by local administration of autologous conditioned serum: a pilot study on sportsmen with muscle strains. Int J Sports Med. 2004;25(8):588–93.
Kobayashi M, Ota S, Terada S, Kawakami Y, Otsuka T, Fu FH, et al. The combined use of losartan and muscle-derived stem cells significantly improves the functional recovery of muscle in a young mouse model of contusion injuries. Am J Sports Med. 2016;44(12):3252–61.
Ota S, Uehara K, Nozaki M, Kobayashi T, Terada S, Tobita K, et al. Intramuscular transplantation of muscle-derived stem cells accelerates skeletal muscle healing after contusion injury via enhancement of angiogenesis. Am J Sports Med. 2011;39(9):1912–22.
Bodendorfer BM, Curley AJ, Kotler JA, Ryan JM, Jejurikar NS, Kumar A, et al. Outcomes after operative and nonoperative treatment of proximal Hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2798–808.
Buckwalter J, Westermann R, Amendola A. Complete proximal hamstring avulsions: is there a role for conservative management? A systematic review of acute repairs and non-operative management journal of ISAKOS: Joint Disorders & Orthopaedic. Sports Med. 2017;2:31–5.
Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40(9):2092–8.
Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350–5.
Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90(11):2365–74.
Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skelet Radiol. 2003;32(10):582–9.
Lempainen L, Sarimo J, Mattila K, Heikkila J, Orava S, Puddu G. Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment. Br J Sports Med. 2007;41(2):80–3.
Brukner P, Connell D. Serious thigh muscle strains’: beware the intramuscular tendon which plays an important role in difficult hamstring and quadriceps muscle strains. Br J Sports Med. 2016;50(4):205–8.
Pollock N, Patel A, Chakraverty J, Suokas A, James SL, Chakraverty R. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med. 2016;50(5):305–10.
van der Made AD, Almusa E, Whiteley R, Hamilton B, Eirale C, van Hellemondt F, et al. Intramuscular tendon involvement on MRI has limited value for predicting time to return to play following acute hamstring injury. Br J Sports Med. 2018;52(2):83–8.
Lempainen L, Kosola J, Pruna R, Puigdellivol J, Sarimo J, Niemi P, et al. Central tendon injuries of hamstring muscles: case series of operative treatment. Orthop J Sports Med. 2018;6(2):2325967118755992.
Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–32.
Wangensteen A, Tol JL, Witvrouw E, Van Linschoten R, Almusa E, Hamilton B, et al. Hamstring reinjuries occur at the same location and early after return to sport: a descriptive study of MRI-confirmed reinjuries. Am J Sports Med. 2016;44(8):2112–21.
Scott A, Huisman E, Khan K. Conservative treatment of chronic Achilles tendinopathy. CMAJ. 2011;183(10):1159–65.
Cacchio A, Rompe JD, Furia JP, Susi P, Santilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med. 2011;39(1):146–53.
Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. Am J Sports Med. 2015;43(3):752–61.
Korakakis V, Whiteley R. The effectiveness of ESWT in lower limb tendinopathy: letter to the editor. Am J Sports Med. 2015;43(10):NP43–4.
Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010;195(4):993–8.
Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376(9754):1751–67.
Seeger JD, West WA, Fife D, Noel GJ, Johnson LN, Walker AM. Achilles tendon rupture and its association with fluoroquinolone antibiotics and other potential risk factors in a managed care population. Pharmacoepidemiol Drug Saf. 2006;15(11):784–92.
Kearney RS, Parsons N, Metcalfe D, Costa ML. Injection therapies for Achilles tendinopathy. Cochrane Database Syst Rev. 2015;5:CD010960.
Davenport KL, Campos JS, Nguyen J, Saboeiro G, Adler RS, Moley PJ. Ultrasound-guided intratendinous injections with platelet-rich plasma or autologous whole blood for treatment of proximal hamstring tendinopathy: a double-blind randomized controlled trial. J Ultrasound Med. 2015;34(8):1455–63.
van der Made AD, Wieldraaijer T, Kerkhoffs GM, Kleipool RP, Engebretsen L, van Dijk CN, et al. The hamstring muscle complex. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2115–22.
Benazzo F, Marullo M, Zanon G, Indino C, Pelillo F. Surgical management of chronic proximal hamstring tendinopathy in athletes: a 2 to 11 years of follow-up. J Orthop Traumatol. 2013;14(2):83–9.
Paavola M, Kannus P, Orava S, Pasanen M, Jarvinen M. Surgical treatment for chronic Achilles tendinopathy: a prospective seven month follow up study. Br J Sports Med. 2002;36(3):178–82.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
de Vos, RJ., Reurink, G., van der Made, A.D., Kerkhoffs, G.M., Purdam, C., Thorborg, K. (2020). When Hamstring Injury Rehabilitation Fails. In: Thorborg, K., Opar, D., Shield, A. (eds) Prevention and Rehabilitation of Hamstring Injuries. Springer, Cham. https://doi.org/10.1007/978-3-030-31638-9_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-31638-9_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31637-2
Online ISBN: 978-3-030-31638-9
eBook Packages: MedicineMedicine (R0)