Abstract
Purpose of Review
To evaluate the current evidence and literature on treatment options for proximal hamstring injuries.
Recent Findings
Patients with 3-tendon complete tears with greater than 2 cm of retraction have worse outcomes and higher complication rates compared to those with less severe injuries. Endoscopic and open proximal hamstring repair both have favorable patient reported outcomes at 5-year follow up. Proximal hamstring repair in patients who are male, with isolated semimembranosus injury, and have proximal hamstring free tendon rupture are more likely to have earlier return to sports. The Parisian Hamstring Avulsion Score (PHAS) is a validated patient-reported outcome measure to predict return to sports.
Summary
Proximal hamstring injuries may occur in both elite and recreational athletes and may present with varying degrees of chronicity and severity. Injuries occur most commonly during forceful eccentric contraction of the hamstrings and often present with ischial tuberosity tenderness, ecchymosis, and hamstring weakness. Treatment decision-making is dictated by the tendons involved and chronicity. Many proximal hamstring injuries can be successfully treated with non-surgical measures. However, operative treatment of appropriately indicated proximal hamstring tendon injuries can result in significantly better functional outcomes and faster and more reliable return to sports compared to nonoperative treatment. Both endoscopic and open surgical repair techniques show high satisfaction levels and excellent patient-reported outcomes at short- and mid-term follow-up. Postoperative rehabilitation protocols vary across the literature and ongoing study is needed to clarify the optimal program, though emphasis on eccentric hamstring strengthening may be beneficial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal hamstring injuries are a common lower extremity pathology that may present with variable severity and chronicity of presentation. Diagnosis and classification of injury with consideration of patient characteristics is critical in devising an appropriate treatment plan. With increasing awareness of the diagnosis and expanding treatment options, the number of pertinent studies and treatment of proximal hamstring injuries continues to rise [1]. Nonoperative management is successful in many cases; however, the growing literature on operative management has shown excellent results in satisfaction, functional recovery and return to sport. The purpose of this article is to review current evaluation and treatment of proximal hamstring injuries.
Background
Anatomy
The hamstring musculature is composed of the semimembranosus, semitendinosus, and the long and short heads of the biceps femoris (Fig. 1). The semimembranosus has the most lateral origin on the pelvis at the anterosuperolateral aspect of the ischial tuberosity and travels anterior and medial to the semitendinosus and biceps femoris muscles [2, 3]. The proximal tendon has connections to the adductor magnus inferomedially [4]. The semitendinosus originates as part of the conjoined tendon along with the long head of the biceps femoris at the inferomedial aspect of the ischial tuberosity [2, 3]. The long head of the biceps femoris composes the other portion of the conjoined tendon that originates at the inferomedial aspect of the ischial tuberosity [2, 3]. The short head of the biceps femoris does not cross the hip joint and originates on the lateral lip of the femoral linea aspera [3, 5].
Adjacent to the hamstring origin are several critical nerves. The sciatic nerve is approximately 1.1 cm lateral to the proximal hamstring origin and the posterior femoral cutaneous nerve (PFCN) is approximately 0.7 cm lateral to the proximal hamstring origin [6]. Although the latter values for both the PFCN and sciatic nerves are averages, surgeons must always be prepared to encounter either, or both, of these nerves sitting directly on the surface (0.0 cm away) of the proximal hamstring origin. The PFCN is a sensory nerve which is typically derived directly from the sacral plexus roots S1 – S3 [7]. The pudendal nerve originates from the sacral plexus roots S2 – S4 and runs closest to the proximal hamstring origin when it is deep to the sacrotuberous ligament, and it is approximately 2.6 cm superior and 2.3 cm medial to the proximal hamstring origin [6].
Anatomic cadaveric dissection demonstrating the proximity of the sciatic nerve (SC) lateral to the ischial tuberosity (red line) and proximal insertions of the long head of the biceps femoris (Bl), semitendinosus (ST), and semimembranosus (SM). Permission was obtained for re-use of this figure from the publisher [8]
Biomechanics
The hamstring musculature acts primarily to extend the hip and flex the knee. The biceps femoris aids in external rotation of the knee and the semitendinosus and semimembranosus aid in internal rotation of the knee [3]. In the swing phase of the gait cycle, the hamstring muscles activate during hip extension to resist knee extension [4]. During the heel strike of the gait cycle, the hamstring muscles prevent forward translation of the tibia in conjunction with the anterior cruciate ligament (ACL), especially when the knee is partially flexed [3, 9]. At foot strike, the hamstrings aid in hip extension and stabilize the knee [3]. During take-off, the combined contraction of the quadriceps and hamstrings support the weight-bearing leg [3]. It is postulated that the imbalance between hamstring and quadriceps strength during take-off, in addition to the transition from a stabilizing role to contracting role, contributes to hamstring injury [4, 9].
Epidemiology
Injuries to the hamstring are common in both recreational and competitive athletes. Hamstring injuries account for up to 30% of new lower extremity injuries and 10 to 29% of all injuries in athletes [10,11,12,13,14]. Injuries of the hamstring most commonly occur at the musculotendinous junction, and proximal injuries only represent 12% of all hamstring injuries [15]. The biceps femoris is the most commonly injured, followed by the semitendinosus and semimembranosus [16,17,18]. Hamstring injuries are at substantial risk of becoming chronic with reinjury rates ranging from 12 to 34% [10, 16, 19, 20].
Mechanism of Injury
The mechanism of proximal hamstring injury is usually seen with an eccentric load applied to a flexed hip and extended knee causing elevated hamstring tension. The hamstring is under the greatest strain at the end of the swing phase when there is eccentric contraction of the muscle fibers at maximal elongation [21]. Activities with rapid acceleration and deceleration, sprinting, water-skiing, and bull-riding are high-risk activities. Additionally, a common mechanism of injury occurs when the legs separate into a “splits” position with flexion of one hip and extension of the contralateral hip.
Injury Classification
There are many factors that are important to consider in the management of proximal hamstring injuries including location, severity, and acuity. Injury location can be insertional (bony or tendinous avulsion), at the musculotendinous junction, or a midsubstance muscle injury.
Wood et al. classified proximal hamstring injuries into five distinct types [22]:
-
Type 1: Osseous or apophyseal avulsions, seen in skeletally immature patients
-
Type 2: Musculotendinous junction
-
Type 3: Incomplete tendon avulsions from bone
-
Type 4: Complete avulsions, no to minimal tendon retraction
-
Type 5: Complete avulsion with significant tendon retraction
-
Type 5A: no sciatic nerve involvement
-
Type 5B: presence of sciatic nerve tethering
-
Hamstring injuries are also commonly classified by the number of tendons involved as this has been used to guide treatment; they can involve one, two, or all three tendon origins. Acuity of injury presentation is not well defined in the literature with acute injury ranging from 4–12 weeks [23,24,25]. However, it is the authors’ practice that acute injury presentation is less than six weeks from initial injury and chronic is greater than six weeks.
Risks Factors
A variety of risk factors for hamstring injury have been described in the literature including previous hamstring injury, inadequate warm up, muscle fatigue, dehydration, decreased lower extremity flexibility, poor core stability, prior fluoroquinolone antibiotic use, and strength imbalances [26,27,28,29,30,31,32]. Of note, previous injury is the strongest risk factor, increasing risk of reinjury up to six times [31, 32], which is thought to be due to decreased strength of the repair scar tissue, lowering the threshold for reinjury [14].
Clinical Presentation, Physical Examination, and Differential Diagnosis
An acute injury to the proximal hamstring complex typically presents with a palpable pop and pain located in the gluteal or ischial tuberosity region. Injuries often occur during activities with concurrent hip flexion and knee extension. Chronic injury can be a more subtle diagnosis that often presents as gluteal/ischial tuberosity pain that radiates down the posterior thigh. Chronic injuries are commonly seen in populations with repetitive hip flexion with knee extension, such as endurance runners. In this population, PFCN symptoms may frequently predominate, presenting with burning pain while being seated due to direct pressure on one or more of the nerve branches.
Typical physical examination findings include a straight leg gait to avoid hip and knee flexion, posterior thigh swelling and ecchymoses (which can extend to the popliteal fossa and calf due to gravity), palpable mass of muscle distally on posterior thigh, tenderness to palpation of ischial tuberosity, pain with sitting, weakness in knee flexion in comparison to the contralateral extremity, and apprehension with hip flexion. If there is sciatic nerve or PFCN tethering or involvement, patients may have paresthesias down the posterior thigh into the lower leg or even neurologic-origin motor weakness.
A number of diagnoses may have overlapping presentations with proximal hamstring injuries and should be considered in the differential diagnosis. Lumbosacral radiculopathy may present with sciatic nerve-related symptoms and a positive straight leg test. Ischiofemoral impingement (IFI) is caused by compression of tissues between the ischial tuberosity and lesser trochanter. In fact, IFI from the lesser trochanter is likely a frequent causative structural factor in a large number of chronic proximal hamstring tendinopathy cases with or without partial-thickness tears. On physical exam, patients will have pain with concomitant hip extension, adduction, and external rotation. Piriformis or deep gluteal syndrome is extra-pelvic compression of the sciatic nerve. Patients will present with paresthesias or pain in the buttocks with a reproduction or worsening of symptoms with simultaneous hip adduction and internal rotation.
Nonoperative Treatment
Indications for Nonoperative Treatment
While there has been a trend towards surgical management of proximal hamstring injuries, most injuries can be successfully managed nonoperatively depending on patient characteristics, the number of involved tendons, the tear thickness, the presence of and amount of retraction, and the chronicity of injury. Commonly referenced parameters that predict success with nonoperative treatment include low-grade partial tears, tears at the myotendinous junction, tears involving a single tendon, tears involving two tendons with less than two centimeters of retraction, and chronic tendinopathy [22, 33, 34]. Furthermore, patients with significant medical comorbidities or low functional demands may be candidates for nonoperative treatment regardless of tear characteristics (Table 1).
Nonoperative Treatment Modalities
Initial nonoperative treatment includes activity modification, rest, nonsteroidal anti-inflammatories, and targeted physical therapy. The Aspetar eccentric strengthening program is one example of a targeted, staged physical therapy program which progressively incorporates additional movements and activities to guide the transition back to sport [35]. Hamstring-targeted rehabilitation (programs incorporating hamstring specific exercises) has been associated with decreased reinjury rates compared to generalized rehabilitation programs [36]. A randomized trial of Swedish track athletes demonstrated faster return to sport (49 versus 86 days) in athletes undergoing hamstring specific rehabilitation [37].
The Nordic Hamstring Exercise (NHE), an eccentric hamstring strengthening movement, is a cornerstone of most rehabilitative and preventative exercise programs (Fig. 2). In a randomized trial of 942 Danish soccer players, players who underwent eccentric hamstring strengthening had a 59% reduction in odds of new injuries and an 86% reduction in odds of reinjury [38]. One hamstring injury was prevented for every 13 players undergoing NHE preventative programs [38]. A meta-analysis of exercise programs incorporating the NHE demonstrated a reduction in new injury rates by 51% in athletic populations [39]. Based on these results, there is a randomized control trial underway to study the efficacy of NHE at preventing re-injury [40].
Depiction of Nordic Hamstring Exercise (NHE) otherwise known as Nordic Hamstring Curls. Using an assistant to stabilize the feet, the patient starts in a kneeled position (A), eccentrically loads the hamstrings during lowering phase (B), and then contracts the hamstrings to return to the upright kneeling position (C). Clinicians instructing patients to complete this exercise must adequately pad the knee to avoid instigating or worsening anterior knee pain. Alternatively, if anterior knee pain precludes proper form or participation in part of in full, a GHD (glute-hamstring developer) machine is an excellent tool to perform eccentric hamstring strengthening
There has been controversy over the optimal timing of rehabilitation programs following acute injury. However, studies investigating the role for early versus delayed exercises have not shown a significant difference [41].
Role for Biologics
There has been increasing interest in biologic adjuncts to traditional nonoperative treatment such as platelet rich plasma (PRP) injections. Although most studies have reported no difference, one early randomized controlled trial on patients undergoing nonoperative management of acute, partial thickness, single-tendon proximal hamstring injuries suggested intralesional PRP injections may lead to improved recovery [42]. Hamid et al. observed an improvement in return to play (27 vs 43 days) and decreased pain in 14 patients who had been randomized to receive a single autologous PRP injection and rehabilitation compared to 14 patients who underwent rehabilitation alone [42]. In this study, patients received a single 3 mL dose of autologous PRP directly at the injury location using ultrasound guidance, but leukocyte count was not reported [42]. A more recent meta-analysis including 207 proximal hamstring injuries being treated nonoperatively across 10 studies failed to identify a significant difference in return to play timing or reinjury rates among patients who did or did not receive PRP injections as part of their rehabilitation [43].
Importantly, there is also significant heterogeneity in specific PRP administration protocols, including number of injections, leukocyte concentration, and spacing of injections, which could lead to inconsistent results. In ten studies included in a recent meta-analysis, three used leukocyte-rich PRP, two used leukocyte-poor PRP, and five did not report leukocyte concentration [43]. Eight studies administered a single injection and one administered two to three depending on grading [43].
Authors’ Recommendations for Nonoperative Treatment
In the authors’ experience, not all full thickness tears, even with retraction, require surgery to achieve a satisfactory outcome. The authors prefer initial nonoperative treatment for the majority of tears meeting the above-listed criteria (Table 1). The decision to operate should incorporate patient goals and expectations, as well as medical comorbidities and functional demands. While the timing of therapy does not seem to be critically important, a hamstring-targeted therapy program incorporating eccentric exercises should be followed. There is not a consistently proven role for adjunctive PRP injections currently, although PRP use is an area of ongoing research.
Operative Treatment
Indications for Operative Treatment
The decision to perform surgery is guided by injury severity, acuity, patient factors, and surgeon experience. Surveys of American Orthopaedic Society for Sports Medicine (AOSSM) and Arthroscopy Association of Canada (ACC) surgeons showed that the most important considerations for surgical treatment were number of tendons involved, tendon retraction, and patient activity level [44]. Common indications for operative treatment are 3-tendon complete proximal avulsions, 2-tendon avulsions with greater than 2 cm of retraction, and other partial tendon injuries that have failed nonoperative management for minimum three months [45]. A variety of open, endoscopic, and combined repair techniques have been described in the literature. Surgical technique is primarily dictated by surgeon comfort and experience. Endoscopic primary repair, for those trained in the technique, is often used for partial avulsions with minimal retraction (2–5 cm) and a tendon stump that remains under the gluteus maximus [46,47,48]. Although significantly retracted tears (> 5 cm) frequently are approached using an open technique, recent reports suggest an endoscopic approach can successfully treat tears with up to 15 cm of retraction [49]. Open approaches are generally utilized for complete avulsion injuries and in chronic tears with significant tendon retraction. The common recommendations for surgical management are demonstrated in Table 2.
Patient Positioning and Draping for Surgical Treatment
The authors recommend positioning the patient prone with the knees slightly flexed to relieve tension at the proximal hamstring insertion. Additionally, flexion of the table at the hips with slight Trendelenburg can aid in positioning. The entire operative lower extremity is placed within the sterile field. The anal region is draped out of the field to limit incision and surgical field contamination. Additionally, a betadine-soaked sponge may be used to clean for 60 s around the perineum to further reduce the risk of infection. Standard surgical preparation is performed. The ipsilateral foot is placed within a stockinette such that foot/ankle movement can be palpated when dissecting near the sciatic nerve. Fluoroscopy may be helpful for accurate portal placement during endoscopic repair and should be accounted for during patient and table positioning. An arm board or sterile covered Mayo stand may be used to hold the surgical extremity in an abducted position for portal placement and for parts or all of the surgical procedure, as the abducted position will allow the sciatic nerve and PFCN to move laterally away from the proximal hamstring and the ischial bursa.
Endoscopic Repair
In the endoscopic repair of proximal hamstring injuries, the ischial tuberosity and gluteal crease serve as landmarks for portal placement. The first portal (medial portal) is made in or just distal to the gluteal crease in a transverse fashion at a location 2 cm distal to the inferior border of the ischial tuberosity just medial to the lateral border of the tuberosity (Fig. 3), and this position may be confirmed with fluoroscopy. This portal is made first since it is made blindly and is furthest from the sciatic nerve. The arthroscope is then inserted into the ischial bursa using medial portal. The authors prefer use of a 70-degree arthroscope, but a 30-degree arthroscope may also be utilized. Of note, the authors recommend a pump pressure of 30—40 mm Hg or less to limit swelling in the gluteal region. Two additional portals (Figs. 3 and 4) may then be placed lateral to the medial portal. The second portal is usually the central portal, about 2–3 cm lateral to the medial portal and just distal to the gluteal crease, or increasingly distal depending on the amount of torn hamstring tendon retraction. The third portal (lateral portal) is made 2—3 cm lateral to the central portal and usually at the same proximal–distal level as the medial portal. Both the central and lateral portal should be made under direct arthroscopic visualization to prevent PFCN or sciatic nerve injury. A fourth portal is advantageous in instances of multiple double- and triple-loaded suture anchors placed for efficient suture management. This fourth portal is a proximal trans-gluteal portal through the gluteus maximus, below and medial to the inferior gluteal nerve. This portal is helpful for docking sutures proximally while passing and tying sutures distally.
Endoscopic proximal hamstring repair pre-operative markings for portal placement. A Prone position, left proximal hamstring endoscopic repair portals. The first portal is the medial portal in the gluteal crease; the second portal is the central portal, between the medial and lateral (third) portals. The central portal may be placed further distal depending on the degree of tendon retraction. Distal accessory portals further distal in the thigh may be needed to retrieve significantly retracted torn tendons (greater than 5–7 cm). A proximal trans-gluteal portal is an excellent portal for suture management, distal and lateral to the inferior gluteal nerve. B Same photo as A, with the sciatic nerve roughly outlined with the lateral dotted line and the ischial tuberosity roughly outlined with the medial dotted line
A Prone position, oblique view, left proximal hamstring endoscopic repair portals. The arthroscope is in the medial portal; an 8.5 mm diameter cannula is in the central portal (used for suture passage, suture tying, instrumentation); the lateral portal (*) is often used for anchor drilling and suture management; the proximal trans-gluteal portal (#) is a proximal suture management portal. B Same photo as A, direct top-down view
Once in the ischial bursa, the most superficial nerve identified first is the PFCN. PFCN anatomy is variable here at the level of the ischial tuberosity. The constant branch is a vertical proximal to distal branch that is on or just lateral to the tuberosity. Variable branches include a second or third vertical branch, usually increasingly lateral and further distal than the tuberosity. A transverse branch is less commonly encountered. However, when a transverse branch is present, it typically crosses from the lateral aspect of the tuberosity across medially to the perineum over the adductor magnus origin. A transverse branch is cumbersome during both endoscopic or open repair as it crosses directly over the proximal hamstring footprint and must be protected throughout the repair to avoid iatrogenic injury. Deep to the PFCN is the sciatic nerve. A cruciate leash of vessels often connects the PFCN to the sciatic and then proceeds medially to the hamstring / quadratus femoris junction and laterally to the femur. Great care must be taken in surgical dissection here to avoid any inadvertent vessel injury, as this complicates visualization greatly and hemostasis is challenging given the close proximity to both nerves. A clear space lateral to the tuberosity must be obtained with the nerve safely away from the hamstring so that suture passage can be 100% visualized and not contact the sciatic nerve. The sciatic nerve approaches the proximal hamstring more closely in the more proximal aspect of the surgical field, as the nerve crosses superomedially over the obturator internus just proximal to the hamstring origin. An ischial bursectomy is performed with an arthroscopic shaver or radiofrequency device to improve visualization and remove a pain source.
Undersurface partial-thickness tears may be identified via a wave sign or a bubble sign. By palpating the footprint on the ischium, a wave sign can indicate tendon instability characteristic of an undersurface partial-thickness tear. A bubble sign is positive if a needle is placed through the intact tendon into the actual tear at the interface between the tuberosity and the tendon and 5 to 10 mL of air injected with observation of the tendon elevating significantly. Once the partial-thickness tear is confirmed, tendon elevation may be performed depending on the exact tear location. In most high-grade partial-thickness tears, the lateral aspect of the conjoint tendon and the medial aspect of the semimembranosus tear are torn centrally (in the coronal plane, usually the same visualization as the arthroscope affords during repair) in the overall tendon footprint. Thus, a vertical transtendinous split with an arthroscopic knife can open the undersurface tear for complete characterization. Remnant soft tissue can be removed from the tuberosity footprint and the ischial footprint may be decorticated with a burr. While decortication to cancellous bone does afford improved biology, the cancellous bone is softer and the suture anchor(s) used must account for bone mineral density to offer a secure repair. The authors prefer the lateral portal with straight or curved guides to drill and place anchors. Two or three tape or suture double-loaded non-metallic suture anchors are usually used for a routine high-grade partial-thickness tear (Fig. 5). Full-thickness complete retracted tears usually require either three triple-loaded or four double-loaded anchors. A side-to-side (one suture limb lateral, one suture limb medial) repair is typically used for each suture in a partial-thickness repair. A full-thickness complete repair likely necessitates greater suture configuration strength. In this situation, the authors prefer a modified Mason-Allen configuration (Fig. 6). Repair security is tested with a flexion and extension of the hip and knee, in addition to IFI maneuvers from both the lesser (extension, adduction, external rotation) and greater (flexion, abduction, and external rotation) trochanters (Fig. 7).
A Left proximal hamstring endoscopic repair with two tape double-loaded all-suture suture-anchors; viewing from medial gluteal crease portal; sutures exiting from the trans-gluteal suture management portal. B Completed left proximal hamstring endoscopic repair after side-to-side configuration and standard arthroscopic knot-tying techniques
A Right proximal hamstring endoscopic repair with three tape double-loaded all-suture suture-anchors for 5 cm retracted complete full-thickness three tendon tear; viewing from medial gluteal crease portal. B Completed right proximal hamstring endoscopic repair after modified Mason-Allen pulley technique configuration and standard arthroscopic knot-tying techniques
Right proximal hamstring endoscopic repair with fluoroscopic visualization of greater trochanter-ischium ischiofemoral impingement. The endoscope is the inferomedial instrument, while a curved radiofrequency device is used as a radiographic marker indicating the proximal margin of the hamstring origin, where the posterior aspect of the greater trochanter makes contact
Open Repair
For an open repair, a ~ 5 cm horizontal incision is made over the palpable ischial tuberosity within the gluteal fold. In cases of large retraction of the tendon and/or in chronic settings, a longitudinal incision can be made from the ischial tuberosity distally or a T-shaped incision could be created. After subcutaneous dissection, the gluteal fascia is identified and incised in the same direction as the incision. The inferior border of the gluteus maximus is identified and retracted proximally with a blunt retractor to expose the hamstring fascia. In the acute setting, there will often be a hematoma or fascial defect that can help identify the tendons. Once identified, the hamstring tendons are mobilized both bluntly and sharply from adhesions. Care is taken not to injure the PFCN and sciatic nerve during dissection, remembering that these nerves run along the lateral aspect of the tuberosity. Neurolysis of the sciatic nerve may be indicated if adhesions to the nerve are present. The posterior surface of the ischium is identified and prepared with a combination of rongeur, curette, and burr for anchor placement. Anatomic repair with two or three suture anchors is performed placing the anchors at the native origin for the injured tendon(s). In an open approach, the authors will typically use one limb from each suture as a running, locking stitch and the other as a post to dock the tendon down to the tuberosity (Fig. 8).
Combined Endoscopic and Open Repair
Limited literature on combined endoscopic and open repair techniques have been described in the literature for proximal hamstring repair [50,51,52]. This technique is described in the setting of chronic hamstring avulsions, tendon retraction greater than 4 cm, or in proximal hamstring reconstruction [50,51,52]. The described techniques start with endoscopic evaluation of the sciatic nerve and PFCN and preparation of the ischial tuberosity [50,51,52]. Then an open incision is made, either longitudinally over the hamstring stump or along the gluteal crease [50,51,52]. The hamstring stump is then identified and mobilized for anatomic repair with suture anchors [50,51,52]. The benefits of this approach are in its facilitated visualization of the tuberosity and release of adhesions around the nerve with the scope, and a potentially stronger suture construct with an open suture passage technique.
Outcomes and Complications
There have been many studies in recent years evaluating outcomes of proximal hamstring injury treatments, however the majority are small and retrospective with conflicting findings. Over the past two decades years, more systematic reviews have been published that provide valuable insight into the treatment of proximal hamstring injuries [24, 53,54,55,56]. A systematic review by Hillier-Smith and Paton analyzed 35 studies for a total of 1530 proximal hamstring repairs [55]. They report that surgical treatment of proximal hamstring injury, regardless of technique, has high satisfaction rates, improved strength, and enhanced functional clinical outcomes and return to sport times compared to nonoperative treatment [55]. They also reported that surgical treatment of acute compared to chronic injury had significantly faster return to sport times (4.5 vs 6.5 months, p < 0.001), lower re-rupture rates (0.2% vs 1.0%, p = 0.045), and decreased rates of sciatic nerve dysfunction (0.7% vs 5.1%, p < 0.001) [55].
Recent articles from Fenn et al. have provided more insight into the patient outcomes after proximal hamstring repair. In one study, the authors evaluated patient reported outcomes of 75 patients who underwent open or endoscopic proximal hamstring repair at 2-year follow up [57]. They found that patients with 3-tendon complete tears with greater than 2 cm of retraction had significantly lower Patient Acceptable Symptom State (PASS) rates in multiple outcome scores (p ≤ 0.032) and a higher complication rate (45.2%, p = 0.043) compared to less severe injuries [57]. Additionally, they found that in cases with 3-tendon complete tears with less than 2 cm of retraction, endoscopic repair had significantly higher PASS rates across multiple outcome scores compared to open repair [57]. In another study, Fenn et al. evaluated outcomes at mid-term follow-up for proximal hamstring repairs, addressing a current literature gap. They reviewed 35 patients that underwent proximal hamstring repair with greater than 5-year follow up and found that endoscopic and open repair techniques both had favorable patient reported outcomes [58].
In a recent systematic review evaluating complication rates after surgical treatment of proximal hamstring injuries by Lawson et al., the authors evaluated 43 studies that included 2833 proximal hamstring repairs [56]. They found an overall complication rate of 15% which is substantially lower than previously reported rates of 23% [24, 56]. However, these authors acknowledge that they were unable to further compare complications rates between open and endoscopic repair, partial and complete injury, and acute versus chronic injury [56].
Predictive Factors of Return to Sport
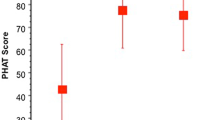
Several studies have sought to identify predictors of return to sport after operative management. A case series of 64 professional athletes undergoing surgical treatment of proximal hamstring injuries found that patients who were male sex (HR 2.91, p = 0.047), had isolated semimembranosus injuries (HR 3.86, p < 0.001), and had proximal hamstring free tendon ruptures (HR 5.18, p < 0.001) were more likely to have earlier return to sports [59]. A recent study by Lefevre et al. validated a new patient-reported outcome measure called the Parisian Hamstring Avulsion Score (PHAS) in 156 patients, serving as another methodology to predict return to sports [60]. In a systematic review from 2019 of sixteen studies, there was a trend toward quicker return to sport with earlier surgical intervention, which is similar to the finding by Hillier-Smith and Paton suggesting that acute injuries had faster return to sport times [55, 61].
Author Recommendations
Based on the current literature and our experience, for acute partial and complete tears with minimal retraction, the authors prefer endoscopic techniques for proximal hamstring repair. For retracted and more chronic tears we prefer an open approach for proximal hamstring repair.
Of note, there are some important distinctions based on our experience between open and endoscopic repair to keep in mind. First, open repair allows for placement of a running, locking stitch technique along the entire length of the tendon, versus the simple or mattress stitch in endoscopic repair. Additionally, endoscopic repair has a steep learning curve and effectiveness may be dependent on surgeon experience. However, morbidity of an open incision is significantly greater than that from endoscopic portal incisions. Furthermore, endoscopic repair allows for more accurate identification and protection of neurologic structures.
Postoperative Rehabilitation
Postoperative rehabilitation protocols after proximal hamstring repair have been shown to be highly variable in the timing of strengthening, stretching, and completion of standardized return to sport criteria before resuming training [62]. While this is in an area for future research and an opportunity to improve patient care, the authors’ recommendation for postoperative proximal hamstring repair is outlined below.
Phase I: 0–6 Weeks Postoperatively
The goal of this phase is wound healing and pain control. Patients typically do not start formal physical therapy until 4–6 weeks postoperatively. Patients are permitted to be touch down weightbearing. A hinge knee brace is worn, locked at 45–50 degrees, until week 4–6. Patients are instructed to avoid hip flexion with knee extension. Of note, allowance of knee extension while upright and passive flexion to 90 degrees while seated has demonstrated good outcomes after proximal hamstring repair [63].
Phase II: 6–12 Weeks Postoperatively
From weeks 4–8, the patient begins gradually progressing active knee flexion in the brace. Weightbearing is progressed as tolerated and the patient is weaned from crutches. The goal of this phase is to normalize gait with full range of motion and initiate basic functional movements such as partial squats without exceeding 60 degrees of knee flexion.
Phase III: 12–16 Weeks
The goal of this phase is to continue progression of hamstring strengthening, including beginning of strengthening of the hamstrings in a lengthened position. Jogging / light running may be initiated in this phase.
Phase IV: 16 + Weeks
Sport-specific movements and impact are initiated. Return to sport criteria includes less than a 10% deficit on functional testing and side-to-side testing compared to the contralateral side.
Additional Author Recommendations
Additional author recommendations from clinical experience are listed below.
-
Both endoscopic and open proximal hamstring repair techniques require careful nerve management of the PFCN and sciatic nerve. Transverse branches of the PFCN can be difficult to manage intraoperatively and likely are a large contributor to post-operative pain.
-
Many chronic high-grade partial thickness tears are attritional, friction-driven injuries derived from IFI between the lesser trochanter and ischium.
-
Full thickness retracted tears can be endoscopically repaired if the tendon is reasonably mobile for anatomic repair, which is usually within a month of initial injury. However, endoscopic repair is still possible in chronic cases with large retraction and may provide a safer technique for nerve protection; endoscopic repair in this setting is technically challenging and may have reduced fixation strength compared to open repair.
-
During the initial learning curve for endoscopic repair, abducting the leg and potentially onto an padded Mayo stand will aid in safe mobilization of the PFCN and sciatic nerve away from the ischial tuberosity.
-
Thorough intraoperative examination under anesthesia for lesser and greater trochanter IFI can help determine the etiology and potential for post-operative pain, despite successful technical repair and ultimate biological healing.
-
Diabetes is a risk factor for repair failure.
-
Patients on weight-loss medication (e.g., ozempic, wegovy) often have poor tuberosity bone quality and anchor pull-out strength may be tested. From our experience, suture anchors have adequate fixation, however solid/metal anchors may be indicated in cases of poor bone stock.
-
Bidets use in the initial postoperative period should be restricted due to risk of surgical site contamination with fecal contents.
Conclusion
Proximal hamstring injuries are common and important to accurately diagnose at presentation. Most hamstring injuries can successfully be managed with nonoperative treatment. However, in the cases of complete rupture, 2-tendon tears with retraction, and injuries refractory to nonoperative treatment, surgical repair is warranted. Open repair techniques have traditionally been employed, however the literature for endoscopic repair is increasing in recent years and is shown to have excellent outcomes. Careful postoperative management and mindful rehabilitation are crucial to limit complications and to improve success after surgical repair.
Competing Interests
The authors declare no competing interests.
Data Availability
No datasets were generated or analysed during the current study.
References
Laszlo S, Jonsson KB. Increasing incidence of surgically treated hamstring injuries: a nationwide registry study in Sweden between 2001 and 2020. Acta Orthop. 2023;94:336–341. Published 2023 Jul 4. https://doi.org/10.2340/17453674.2023.13650.
Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A cadaveric study [published correction appears in J Bone Joint Surg Am. 2007 Mar;89(3):637]. J Bone Joint Surg Am. 2007;89(1):44–8. https://doi.org/10.2106/JBJS.F.00094.
Beltran L, Ghazikhanian V, Padron M, Beltran J. The proximal hamstring muscle-tendon-bone unit: a review of the normal anatomy, biomechanics, and pathophysiology. Eur J Radiol. 2012;81(12):3772–9. https://doi.org/10.1016/j.ejrad.2011.03.099.
Koulouris G, Connell D. Hamstring muscle complex: an imaging review [published correction appears in Radiographics. 2005 Sep-Oct;25(5):1436]. Radiographics. 2005;25(3):571–86. https://doi.org/10.1148/rg.253045711.
Kumazaki T, Ehara Y, Sakai T. Anatomy and physiology of hamstring injury [published correction appears in Int J Sports Med. 2012 Dec;33(12):954]. Int J Sports Med. 2012;33(12):950–4. https://doi.org/10.1055/s-0032-1311593.
Cvetanovich GL, Saltzman BM, Ukwuani G, et al. Anatomy of the pudendal nerve and other neural structures around the proximal hamstring origin in males. Arthroscopy. 2018;34(7):2105–10. https://doi.org/10.1016/j.arthro.2018.02.029.
Jiamjunyasiri A, Tsutsumi M, Muro S, Akita K. Origin, course, and distribution of the posterior femoral cutaneous nerve and the spatial relationship among its branches. Anat Sci Int. 2023;98(4):540–7. https://doi.org/10.1007/s12565-023-00721-x.
Pérez-Carro L, et al. Gross and endoscopic posterior hip anatomy. In: Martin H, Gómez-Hoyos J, editors., et al., Posterior hip disorders. Cham: Springer; 2019. https://doi.org/10.1007/978-3-319-78040-5_1.
Slocum DB, James SL. Biomechanics of running. JAMA. 1968;205(11):721–8.
Croisier JL. Factors associated with recurrent hamstring injuries. Sports Med. 2004;34(10):681–95. https://doi.org/10.2165/00007256-200434100-00005.
Maniar N, Carmichael DS, Hickey JT, et al. Incidence and prevalence of hamstring injuries in field-based team sports: a systematic review and meta-analysis of 5952 injuries from over 7 million exposure hours. Br J Sports Med. 2023;57(2):109–16. https://doi.org/10.1136/bjsports-2021-104936.
Chang JS, Kayani B, Plastow R, Singh S, Magan A, Haddad FS. Management of hamstring injuries: current concepts review. Bone Joint J. 2020;102-B(10):1281–8. https://doi.org/10.1302/0301-620X.102B10.BJJ-2020-1210.R1.
Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–32. https://doi.org/10.1177/0363546510395879.
Ahmad CS, Redler LH, Ciccotti MG, Maffulli N, Longo UG, Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med. 2013;41(12):2933–47. https://doi.org/10.1177/0363546513487063.
Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32(10):582–9. https://doi.org/10.1007/s00256-003-0674-5.
Malliaropoulos N, Isinkaye T, Tsitas K, Maffulli N. Reinjury after acute posterior thigh muscle injuries in elite track and field athletes [published correction appears in Am J Sports Med. 2011 Apr;39(4):NP7]. Am J Sports Med. 2011;39(2):304–10. https://doi.org/10.1177/0363546510382857.
De Smet AA, Blankenbaker DG, Alsheik NH, Lindstrom MJ. MRI appearance of the proximal hamstring tendons in patients with and without symptomatic proximal hamstring tendinopathy. AJR Am J Roentgenol. 2012;198(2):418–22. https://doi.org/10.2214/AJR.11.6590.
Grange S, Reurink G, Nguyen AQ, et al. Location of hamstring injuries based on magnetic resonance imaging: a systematic review. Sports Health. 2023;15(1):111–23. https://doi.org/10.1177/19417381211071010.
Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843–50. https://doi.org/10.1177/0363546510394647.
Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997–2000. Br J Sports Med. 2002;36(1):39–44. https://doi.org/10.1136/bjsm.36.1.39.
Schache AG, Wrigley TV, Baker R, Pandy MG. Biomechanical response to hamstring muscle strain injury. Gait Posture. 2009;29(2):332–8. https://doi.org/10.1016/j.gaitpost.2008.10.054.
Wood DG, Packham I, Trikha SP, Linklater J. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90(11):2365–74. https://doi.org/10.2106/JBJS.G.00685.
Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2130–5. https://doi.org/10.1007/s00167-013-2817-0.
Bodendorfer BM, Curley AJ, Kotler JA, et al. Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2798–808. https://doi.org/10.1177/0363546517732526.
Bowman EN, Marshall NE, Gerhardt MB, Banffy MB. Predictors of clinical outcomes after proximal hamstring repair. Orthop J Sports Med. 2019;7(2):2325967118823712. Published 2019 Feb 15. https://doi.org/10.1177/2325967118823712.
Watsford ML, Murphy AJ, McLachlan KA, et al. A prospective study of the relationship between lower body stiffness and hamstring injury in professional Australian rules footballers. Am J Sports Med. 2010;38(10):2058–64. https://doi.org/10.1177/0363546510370197.
Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25(1):81–5. https://doi.org/10.1177/036354659702500116.
Small K, McNaughton LR, Greig M, Lohkamp M, Lovell R. Soccer fatigue, sprinting and hamstring injury risk [published correction appears in Int J Sports Med. 2009 Aug;30(8):578]. Int J Sports Med. 2009;30(8):573–8. https://doi.org/10.1055/s-0029-1202822.
Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):116–25. https://doi.org/10.2519/jospt.2004.34.3.116.
Worrell TW. Factors associated with hamstring injuries. An approach to treatment and preventative measures. Sports Med. 1994;17(5):338–45. https://doi.org/10.2165/00007256-199417050-00006.
Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for hamstring injuries among male soccer players: a prospective cohort study. Am J Sports Med. 2010;38(6):1147–53. https://doi.org/10.1177/0363546509358381.
Hägglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767–72. https://doi.org/10.1136/bjsm.2006.026609.
Allahabadi S, Salazar LM, Obioha OA, Fenn TW, Chahla J, Nho SJ. Hamstring injuries: a current concepts review: evaluation, nonoperative treatment, and surgical decision making. Am J Sports Med. 2023;24:036354652311649. https://doi.org/10.1177/03635465231164931.
Arner JW, McClincy MP, Bradley JP. Hamstring injuries in athletes: evidence-based treatment. J Am Acad Orthop Surg. 2019;27(23):868–77. https://doi.org/10.5435/JAAOS-D-18-00741.
Aspetar - Aspetar Hamstring Protocol. www.aspetar.com. https://www.aspetar.com/en/professionals/aspetar-clinical-guidelines/aspetar-hamstring-protocol. Accessed 5 Jan 2024
Mendiguchia J, Martinez-Ruiz E, Edouard P, Morin J-B, Martinez-Martinez F, Idoate F, et al. A multifactorial, criteria-based progressive algorithm for hamstring injury treatment. Med Sci Sports Exerc. 2017;49(7):1482–92. https://doi.org/10.1249/MSS.0000000000001241.
Askling CM, Tengvar M, Tarassova O, Thorstensson A. Acute hamstring injuries in Swedish elite sprinters and jumpers: a prospective randomized controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2014;48(7):532–9. https://doi.org/10.1136/bjsports-2013-093214.
Petersen J, Thorborg K, Nielsen MB, Budtz-Jørgensen E, Hölmich P. Preventive effect of eccentric training on acute hamstring injuries in men’s soccer: a cluster-randomized controlled trial. Am J Sports Med. 2011;39(11):2296–303. https://doi.org/10.1177/0363546511419277.
Van Dyk N, Behan FP, Whiteley R. Including the Nordic hamstring exercise in injury prevention programmes halves the rate of hamstring injuries: a systematic review and meta-analysis of 8459 athletes. Br J Sports Med. 2019;53(21):1362–70. https://doi.org/10.1136/bjsports-2018-100045.
Zein MI, Reurink G, Verhagen E, Kerkhoffs GMMJ, Van Der Horst N, Goedhart E, et al. Study on Hamstring Re-injury Prevention (SHARP): protocol for an international multicentre, randomized controlled trial. BMJ Open. 2022;12(11):e065816. https://doi.org/10.1136/bmjopen-2022-065816.
Vermeulen R, Whiteley R, Van Der Made AD, Van Dyk N, Almusa E, Geertsema C, et al. Early versus delayed lengthening exercises for acute hamstring injury in male athletes: a randomized controlled clinical trial. Br J Sports Med. 2022;56(14):792–800. https://doi.org/10.1136/bjsports-2020-103405.
Hamid MSA, Mohamed Ali MR, Yusof A, George J, Lee LPC. Platelet-rich plasma injections for the treatment of hamstring injuries: a randomized controlled trial. Am J Sports Med. 2014;42(10):2410–8. https://doi.org/10.1177/0363546514541540.
Seow D, Shimozono Y, Tengku Yusof TNB, Yasui Y, Massey A, Kennedy JG. Platelet-rich plasma injection for the treatment of hamstring injuries: a systematic review and meta-analysis with best-worst case analysis. Am J Sports Med. 2021;49(2):529–37. https://doi.org/10.1177/0363546520916729.
Pasic N, Giffin JR, Degen RM. Practice patterns for the treatment of acute proximal hamstring ruptures. Phys Sportsmed. 2020;48(1):116–22. https://doi.org/10.1080/00913847.2019.1645576.
Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350–5. https://doi.org/10.5435/00124635-200706000-00004.
Castillo-de-la-Peña J, Wong I. Endoscopic repair of proximal hamstring insertion with sciatic nerve neurolysis. Arthrosc Tech. 2022;11(5):e789-e795. Published 2022 Apr 22. https://doi.org/10.1016/j.eats.2021.12.038.
Domb BG, Linder D, Sharp KG, Sadik A, Gerhardt MB. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013;2(1):e35-e39. Published 2013 Jan 18. https://doi.org/10.1016/j.eats.2012.10.003.
Suppauksorn S, Nwachukwu BU, Beck EC, Okoroha KR, Nho SJ. Endoscopic approach to proximal hamstring avulsion repair. JBJS Essent Surg Tech. 2020;10(4):e19.00037. Published 2020 Dec 24. https://doi.org/10.2106/JBJS.ST.19.00037.
Maier J, Clark E, Laskovski J. Repair of retracted hamstring tears with hamstring pulley technique and inferomedial portal. Arthrosc Tech. 2023;12(12):e2273-e2280. Published 2023 Nov 20. https://doi.org/10.1016/j.eats.2023.07.057.
Atzmon R, Amar E, Maor D, Rath E. A combined endoscopic and open surgical approach for chronic retracted proximal hamstring avulsion. J Hip Preserv Surg. 2019;6(3):284–288. Published 2019 Oct 11. https://doi.org/10.1093/jhps/hnz037.
Factor S, Khoury A, Atzmon R, Vidra M, Amar E, Rath E. Combined endoscopic and mini-open repair of chronic complete proximal hamstring tendon avulsion: a novel approach and short-term outcomes. J Hip Preserv Surg. 2021;7(4):721–727. Published 2021 May 31. https://doi.org/10.1093/jhps/hnab006.
Lakshmanan Sivasundaram, Hevesi M, Rice MW, et al. “Scopen” scope to open hamstring repair. Video J Sports Med. 2022;2(4):263502542210893–263502542210893. https://doi.org/10.1177/26350254221089355.
Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures - a systematic review. Int J Sports Med. 2011;32(7):490–5. https://doi.org/10.1055/s-0031-1273753.
van der Made AD, Reurink G, Gouttebarge V, Tol JL, Kerkhoffs GM. Outcome after surgical repair of proximal hamstring avulsions: a systematic review. Am J Sports Med. 2015;43(11):2841–51. https://doi.org/10.1177/0363546514555327.
Hillier-Smith R, Paton B. Outcomes following surgical management of proximal hamstring tendon avulsions : a systematic review and meta-analysis. Bone Jt Open. 2022;3(5):415–22. https://doi.org/10.1302/2633-1462.35.BJO-2021-0196.R1.
Lawson JJ, Abraham EA, Imbergamo CM, Sequeira SB, Dreese JC, Gould HP. Systematic review of complications associated with proximal hamstring tendon repair. Orthop J Sports Med. 2023;11(9):23259671231199092. Published 2023 Sep 26. https://doi.org/10.1177/23259671231199092.
Fenn TW, Brusalis CM, Allahabadi S, Alvero AB, Ebersole JW, Nho SJ. Association between proximal hamstring tear characteristics and achievement of clinically significant outcomes after endoscopic and open repair at minimum 2-year follow-up. Am J Sports Med. 2024;52(2):390–400. https://doi.org/10.1177/03635465231216118. (Patients with 3-tendon complete tears with greater than 2 cm of retraction had significantly lower outcome scores and a higher complication rate compared to less severe injuries. In patients with 3-tendon complete tears with less than 2 cm of retraction, that endoscopic repair had significantly higher outcomes scores compared to open repair. Current and relevant study with adequate follow up that can help guide clinical decision making).
Fenn TW, Timmermann AP, Brusalis CM, Kaplan DJ, Ebersole JW, Nho SJ. Clinical outcomes after open and endoscopic repair of proximal hamstring tendon tears at a minimum follow-up of 5 years. Orthop J Sports Med. 2023;11(11):23259671231209054. Published 2023 Nov 23. https://doi.org/10.1177/23259671231209054. Endoscopic and open proximal hamstring repair both have favorable patient reported outcomes at 5-year follow up. Fills an important gap in the literature regarding mid-term follow up.
Lefèvre N, Moussa MK, Valentin E, et al. Predictors of early return to sport after surgical repair of proximal hamstring complex injuries in professional athletes: a prospective study. Am J Sports Med. Published online February 14, 2024. https://doi.org/10.1177/03635465231225486. Proximal hamstring repair in patients who are male, with isolated semimembranosus injury, and have proximal hamstring free tendon rupture are more likely to have earlier return to sports. Provides important information regarding return to sport for clinical decision making and patient discussion.
Lefevre N, Kassab Hassan S, Valentin E, et al. Validation of the Parisian hamstring avulsion score (PHAS) in the evaluation and follow-up of patients operated for proximal hamstring avulsion. Am J Sports Med. Published online February 14, 2024. https://doi.org/10.1177/03635465241227434. The Parisian Hamstring Avulsion Score (PHAS) is a validated patient-reported outcome measure to predict return to sports. The PHAS adds another diagnostic tool to aid in clinical decision making and return to sport after proximal hamstring injury.
Belk JW, Kraeutler MJ, Mei-Dan O, Houck DA, McCarty EC, Mulcahey MK. Return to sport after proximal hamstring tendon repair: a systematic review. Orthop J Sports Med. 2019;7(6):2325967119853218. Published 2019 Jun 24. https://doi.org/10.1177/2325967119853218.
Lightsey HM, Kantrowitz DE, Swindell HW, Trofa DP, Ahmad CS, Lynch TS. Variability of United States online rehabilitation protocols for proximal hamstring tendon repair. Orthop J Sports Med. 2018;6(2):2325967118755116. Published 2018 Feb 23. https://doi.org/10.1177/2325967118755116.
Wong SE, Julian KR, Carpio JG, Zhang AL. Proximal hamstring repair with all-suture anchors and an accelerated rehabilitation and bracing protocol demonstrates good outcomes at 1-year follow-up. Arthrosc Sports Med Rehabil. 2024;6(2):100891. Published 2024 Feb 10. https://doi.org/10.1016/j.asmr.2024.100891.
Funding
No funding was received by any authors for this review.
Author information
Authors and Affiliations
Contributions
TY, RH, SA wrote the main manuscript and performed the primary literature review. SW and JH provided expert knowledge on surgical techniques and clinical pearls, provided images for figures, and performed secondary literature review. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
We would like to thank Dr. Alan Zhang for reviewing this manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yetter, T.R., Halvorson, R.T., Wong, S.E. et al. Management of Proximal Hamstring Injuries: Non-operative and Operative Treatment. Curr Rev Musculoskelet Med 17, 373–385 (2024). https://doi.org/10.1007/s12178-024-09911-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-024-09911-0