Abstract
This chapter builds on Chap. 14, describing structured headache services as the healthcare solution to headache.
Where headache services exist at all, their focus is usually, inappropriately, on specialist care, while compartmentalized divisions between primary and secondary care create multiple inefficiencies. The model described here seeks vertical integration while recognizing that headache services not only must but readily can be delivered for the most part in primary care. It is a cost-effective solution and almost certainly cost-saving in all economies.
Political will is needed for change to happen. This is the greatest challenge.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Headache disorders
- Barriers to care
- Public health
- Health policy
- Structured headache services
- Change management
- Needs assessment
- Service organization and delivery
- Primary care
- Specialized centres
- Education
- Economic analysis
- Cost-effectiveness
- Global Campaign against Headache
1 Introduction
Earlier chapters have described the societal impact of headache disorders (Chaps. 4, 8 and 9), and their recognition by the World Health Organization (WHO) from 2000 onwards as a high-priority public-health concern ([1,2,3,4]; also, Chap. 5). Over this period, headache disorders have come to be acknowledged as the second highest cause of disability in the world ([5,6,7]; also, Chap. 9). Three only of the more than 200 headache disorders classified by the International Headache Society [8]—migraine, tension-type headache (TTH) and medication-overuse headache (MOH)—account for almost all headache-attributed burden ([5,6,7]; also, Chaps. 2–4, 8 and 9): These disorders are common and in many cases lifelong conditions (Chap. 2), associated with recognizable and substantial burdens that include personal suffering, disability, impaired quality of life and financial cost ([9]; also, Chaps. 4 and 12). Their impact extends beyond those immediately affected ([9]; also, Chaps. 4 and 8–12).
Not surprisingly, in countries where data are available, large numbers of people with headache are seen by physicians [10, 11]. For example, in a United Kingdom (UK) study based in primary care 20 years ago, 17% of registered patients aged 16–65 years had consulted a general practitioner (GP) because of headache, and a large proportion (9%) were referred to secondary care [12]. Since, in the UK, virtually everyone is registered with a local GP, these are closely indicative of population-based statistics. As a consequence, neurologists, who received by far the most of these referrals, reported that up to a third of all their patients consulted for headache, more than for any other neurological condition [10].
Despite this, everywhere in the world, headache care reaches only a minority of those who might be considered to need it ([4, 13,14,15,16,17,18]; also, Chap. 13). Chapter 14 proposed the solution: structured headache services [4, 19, 20].
Of course, fully developed health services for headache, delivering care equitably and nationwide to large numbers of people, will consume significant healthcare resources. But what this means is not that their priority should be questioned; this is established beyond doubt (see Chap. 14). Rather, it means that their organization calls for efficiency and attention to cost-effectiveness. Here, the service model, adaptable and supported by educational initiatives, is described in detail.
2 The Status Quo: Inefficient and Failing, and Not Only in Low-Income Countries
There is a worldwide context, identified 20 years ago, of low priority accorded to headache disorders in the queue for healthcare resources [21]. Thirteen years later, WHO’s Atlas of Headache Disorders and Resources in the World 2011 described a world of enormous, largely remediable but mostly untreated public ill health attributed to headache ([4]; also, Chap. 5).
Studies in wealthy countries such as the United States of America (USA) and UK found that only two thirds of adults with migraine were correctly diagnosed, only half were consulting healthcare providers, yet over 60% of those not consulting exhibited high migraine-related disability [15]. The Eurolight study in ten countries of the European Union (EU) [22, 23] included indicators of adequacy of medical care [18]. With the focus again on migraine, the findings were depressing. Among 1175 participants in the ten countries reporting frequent migraine—on more than 5 days per month, indicating unambiguous need for preventative medication—fewer than 20% had seen a healthcare professional (GP or specialist). In most countries, fewer than 10% were receiving what might be considered adequate acute treatment, and even smaller proportions had the preventative medication for which they were clearly eligible. In other words, the authors of this report concluded, in wealthy Europe, too few people with migraine consult physicians, and migraine-specific medications are used inadequately even among those who do [18]. Is there hope at all for people with headache in less well-resourced countries?
In Russia, population-based data showed that only 15% of people with headache were consulting, one third of these—far too high a proportion—going directly to neurologists [24, 25]. In Estonia, with better-developed primary care and referral systems, the proportion sent by GPs to neurologists (prior to an educational intervention) was a similar 39.5% [26]. In Nepal, almost three fifths (58%) of participants with headache in a population-based survey had consulted a professional healthcare provider (HCP) in the previous year, and 8% had seen a specialist of some sort [27]. These findings, in a low-income country, suggest better availability of healthcare than in many other, wealthier countries: for example, in Japan [13] and Taiwan [28], in EU countries [15, 18, 29] and in North America [15, 30, 31].
But, of course, all was not as it seemed. The survey in Nepal included a very wide range of HCPs in the count of “medical consultations”, some with no counterparts in many other countries, or who would not be accredited as health professionals [27]. When pharmacist consultations (15%) were excluded, the consultation proportion fell to 43% [27], similar to the 47% in China [32]. When consultations only with physicians were considered, probably the most salient comparison, the proportion (less than 19%: GPs 11%, specialists 8% [27]) was much lower than those elsewhere [13, 15, 18, 29,30,31,32]—except for Russia [24, 25]. Further, Nepal has no headache specialists, and few neurologists or neurosurgeons, so “specialist” consultations were most likely with ophthalmologists, ENT specialists or psychiatrists [27]. In other words, these findings reflected high demand without indicating good care: on the contrary, headache-attributed burden in Nepal remains egregiously high [33].
These Nepalese findings are given emphasis for a reason relevant to what follows in this chapter. The authors took a positive view: over half of survey participants with headache had engaged at some level with professional healthcare [28], a proportion well in line with international recommendations for headache service organization and delivery ([20]; and see estimates below). This indicated that capacity was available within the health services of even this low-income country that could be built upon in a programme aimed at improvement [27].
3 Proposals for Change
So to the solution: nationwide, educationally supported, structured headache services, integrated within a country’s healthcare system, efficiently, effectively and equitably mitigating the personal and societal burdens of headache.
Their focus should be on migraine, TTH and MOH. Other headaches, although generally much less common, are nonetheless important, since they may be symptoms of underlying disorders that threaten health and wellbeing. These secondary headaches [8] require both correct and timely diagnosis and effective treatment, sometimes urgently in order to prevent serious consequences (see Chap. 2). Management of these is, essentially, treatment of the causative disorders and outside the ambit of headache services. On the other hand, their recognition must be the responsibility of the services to which affected patients present—most likely to be headache services when headache is the symptom. So adequate provision is needed for this also.
Proposals for change must build on the health services that exist, in whichever country, wherever it is in the world, accepting that these are differently structured and usually inadequately resourced. In the face of very high levels of need for headache-related healthcare (see below), they must be readily adaptable, as well as efficient, effective and equitable, to match what is achievable in any country while making best use of resources that are available. They should formulate a basic model of healthcare organization rationally spread across primary and secondary healthcare sectors, with due regard for the different skills and levels of expertise in these sectors.
3.1 Headache-Related Healthcare Needs Assessment
Existence of a health disorder does not translate directly into need for professional healthcare. Need is generally defined with regard to potential for benefit (there is no need for something that will not in some way be helpful). The proposal that everyone with headache would gain benefit from professional headache care might be arguable, but the suggestion that they all have a need for care must be constrained in a resource-limited world. Need predicated on anticipated benefit must rise above a threshold of benefit and be judged with due regard to benefits achievable by other means. These stipulations are at the heart of health economics and policy, and dictate constraints to whatever is proposed.
Thresholds are hard to set objectively, although needs assessments are highly sensitive to them. With regard to headache, many people treat themselves, some through necessity, others from choice. Those who do so are not only those who are less severely affected [15]; many choose self-management when they expect the marginal benefit of professional involvement in their care to be small (subthreshold benefit negates need). Here is a problem, because expectations are quite often unrealistic—too high or sometimes too low—so that needs assessments based on what people currently do [10,11,12,13,14,15,16,17,18, 24, 25, 27,28,29,30,31,32] have very questionable validity. This is more so when service improvement is planned: a better service—if “better” means delivering enhanced benefit—should see greater usage than a poor service it replaces (discovered need). While planning must factor this in, it is difficult to estimate.
Aside from these consumer-driven issues, another is also threshold-dependent. Cash-limited health services seek value for money: they will discount assessed needs, however great, whenever utility gain per unit of healthcare resource consumption will be low. In headache medicine, the potential for benefit from professional healthcare is generally greatest among those worst affected, so that health policy might reasonably focus on these. Further, both migraine and MOH, in most cases, can be effectively treated at rather low cost ([34]; and see below).
The approach in this chapter to needs assessment—estimating how much professional care should be provided—is conservative: it will underestimate rather than overestimate need. Any other approach would be unhelpful—as will become apparent.
A first assumption is that only those with disabling headache are in need of professional care. The implication that others can adequately look after themselves is possibly unfair, but the assumption respects a reasonable view of priority. About two thirds (66%) of the world’s population are aged 15–64 years [35], these being the years during which headache disorders tend to be particularly troublesome. About 25% are aged 14 or under [36]. With regional variations, in every million people living in the world, there are 660,000 and 250,000 in these age groups, respectively. Primary headache is less common, and less troublesome, in older people [7].
Best epidemiological evidence ([7]; also, Chaps. 8 and 9) suggests about 15% of adults aged 15–64 have migraine. This number is a global average, still based on incomplete data (see Chap. 9): population-based studies in many countries have found adult prevalences well in excess of 20% ([37]; also, Chap. 8). Some 80% of these (i.e. 12% of adults) are significantly disabled through severe pain and/or debilitating associated symptoms [38]. Perhaps another 25%, although again there are wide variations, have occasional other headaches, mostly episodic TTH (see Chap. 8), which generally is not regarded as significantly disabling ([39]; also, Chaps. 2 and 9). About 1.5% (the proportion varies greatly from country to country) [40] are highly disabled by MOH. In other words, in every million people in the world, there are approximately 80,000 adults disabled at least to some extent by migraine (660,000 adults ∗ 0.15 [prevalence] ∗ 0.8 [proportion disabled]), and therefore in need of headache care, and a minimum of 10,000 with MOH (660,000 adults ∗ 0.015 [prevalence]), all of whom need care because this disorder will not otherwise resolve. Note that the total (90,000 out of 660,000 [13.6%]), which effectively ignores TTH, is of the order only of one third of the estimated prevalence of headache including TTH ([5]; also, Chap. 9), which, arguably, is overconservative.
Needs arise in the child and adolescent populations also but are more difficult to quantify because there are fewer data. Headache is apparently as common in children as in adults, with an estimated 1-year prevalence in excess of 50% (based on rather sparse data) [41]. But it has different characteristics (see Chap. 3). It is clear that migraine prevalence is lower in children [41], dependent upon age and reaching adult levels during the course of adolescence, but undifferentiated headache largely fills its place, albeit with less disabling consequences (Chap. 3). In the absence of better data, a conservative but reasonable working basis is that headache care needs in these age groups are, per head, half those of adults [20]: another 17,000 in each million of the population (250,000 children/adolescents ∗ 0.136/2 [half adult need]).
3.2 Service Provision Requirement
Upon these statistics, with some further assumptions (Table 15.1), it is possible to make estimates of service requirements (Table 15.2).
First, need for care is distinguished from demand. The two overlap, but they are not the same—each can exist without the other. Need for professional headache care, defined as above, becomes demand only in those who seek care (which is not everyone with need (see Chap. 13)). Complex factors, not all well understood, govern healthcare utilization by people with headache [15]. Unavailability of good care is one, and self-perpetuating, since demand is sensitive to this, suppressed regardless of need. Evidence suggests that demand for headache care is expressed by only 50% of those who might be considered in need [12, 13, 15, 42], but the assumption is made here that better and more accessible services will increase this to 75% (still leaving 25% of need unmet).
Second are a range of assumptions about time. Inpatient management is ignored: the need for it in the management of primary headache is very low. Admission is sometimes good practice, because of comorbidities, or for detoxication in MOH, but only in a tiny percentage of all presenting patients. The multiple assumptions relating to time allocations therefore consider only ambulatory care. They are based on expert views of requirement [20], again tempered with conservatism.
Despite this deep conservatism pervading the assumptions, Table 15.2 sets out very challenging estimates of service requirement. While they may be imprecise, two conclusions follow.
3.3 Structured Headache Services
First of these is that headache services must be formally organized and integrated within the structure of local health services. If they merely develop ad hoc, as is now the case in most countries providing any service at all, they can be neither efficient nor equitable. In the context of failing headache services described earlier, systems or practice that lead to large numbers of headache referrals to neurologists [4, 10,11,12, 24,25,26] must be questioned. On the other hand, if headache service provision is envisaged only in the form of headache centres—national or regional—large numbers of referrals are inevitable.
Second, inexorably, is that headache services cannot in any case be provided, in the main, in specialist care. The very limited capacity in specialist care offers no chance of needs being met—or even a substantial part of them.
This is not a bad thing, for two reasons.
First, and of specific relevance to headache, most diagnosis and management of headache disorders requires no more than a basic knowledge of a relatively few very common disorders (see Chap. 2), which ought to be very familiar to primary-care providers. Only standard clinical skills need be applied, and no special investigations or equipment are usually necessary. In other words, there is no clinical objection to locating most headache services in primarycare [20].
Second, wherever healthcare reform is in progress, there is emphasis on strengthening primary care [43,44,45,46,47]. There are good reasons for this, recognized since WHO’s Alma-Ata declaration of 40 years ago [43], which characterized primary healthcare as “the first level of contact of individuals, the family and community with the national health system bringing healthcare as close as possible to where people live and work”. While models of healthcare vary throughout the world, whatever the overarching system of care (assuming there is one), primary care has a recognized and important role nearly everywhere. In highly rural regions, those of sub-Saharan Africa, for example, primary care is the only point of contact for most patients. Among advanced systems, some provide free, subsidized or reimbursed care, supported by insurance-based financial structures operated by the State or in which the State is a controlling intermediary; others levy fees for service, which patients may or may not recover through private or employer-provided insurance. All of these can accommodate primary care as the first port of call [45].
There are other reasons, too, which have to do with efficiency and cost-saving. These are discussed later.
3.4 A Model of Headache-Service Organization
Recognizing these arguments, the fundamental purpose of headache-service organization is to divide service provision rationally between primary and secondary (specialist) care. Within a structured system, management of patients at the lowest level commensurate with good care makes most efficient use of allocated resources and is the means by which effective care can reach more who need it. How this is best done practically depends on the local health-service structure and resources allocated.
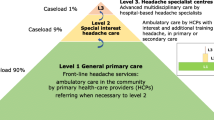
The model described below (Table 15.3; Fig. 15.1) provides a general guide and template, adaptable as necessary. Its essential elements are organization on three interdependent levels, with facilitated but nonetheless controlled pathways between them, and expansion of the contribution from primary care.
3.4.1 Level 1: General Primary Care
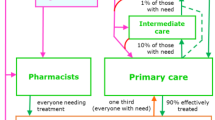
Primary care, with the benefit to patients of being available locally, should be the accessible front line for almost all people needing care for a headache disorder. This is not everyone with headache: an estimated two thirds should, with advice from public education and guidance from pharmacists, be able adequately to manage themselves (see Sect. 15.3.1).
At this level, nonspecialist HCPs—with some training in headache—should meet the needs of the great majority of people consulting for headache [1], controlling flow to higher levels. They may be primary-care physicians (GPs), but this is not essential in a healthcare system that relies more on clinical officers, nurses or pharmacists. Whatever their background, many HCPs at this level will need better knowledge of headache for this purpose, but the model does not require every HCP in primary care to offer headache services if they can share caseload between themselves according to their skills and interests.
Most cases of migraine and TTH should be competently diagnosed and managed at level 1 [48].
Cluster headache, medication-overuse headache (MOH) and some other common secondary headache disorders listed in Table 15.4 should be recognized but not necessarily managed; red-flag warnings of serious secondary headaches (see Chap. 2) should also be recognized and duly acted upon [48]. Referral channels to levels 2 and 3, urgent when necessary, should be in place for these cases and for other patients who are diagnostically complex or difficult to manage [20].
This level should also continue the long-term care of patients discharged with treatment plans from levels 2 or 3 [20].
3.4.2 Level 2: Special-Interest Headache Care
Level 2 may, in some countries, be in primary care, provided by GPs with a special interest and additional training in headache. In others it is more likely to be offered in polyclinics or district hospitals by neurologists, also with additional training in headache [20].
HCPs at this level, usually physicians, should provide more skilled ambulatory care to the small proportion of patients referred upwards from level 1 (Fig. 15.1), who require greater expertise. Their competence should embrace the diagnosis and management of more difficult cases of primary headache and some secondary headache disorders, but not those that are very rare [20]. To fulfil their role, they need access to other services such as neuroimaging, psychology and physiotherapy.
For a minority of their patients—those outside their competence—they require a referral channel to level 3 (Table 15.5) [20].
3.4.3 Level 3: Specialized Headache Centres
Specialized headache centres sit at the apex of structured headache services. In many countries, they remain an unfulfilled aspiration; in others, they exist—disadvantageously—without the lower levels in place. They have four important roles (Table 15.6).
First and foremost, specialized headache centres are tertiary referral centres. They manage the very few patients with primary or secondary headache disorders that are difficult to diagnose or treat, refractory, or for other reasons require specialist intervention [20, 49,50,51,52,53] (Fig. 15.1; Table 15.5). They concentrate experience in the rare primary and secondary headache disorders and cranial neuralgias. For this role, they employ accredited headache specialists and/or neurologists and provide full-time inpatient facilities, multidisciplinary management and access to equipment and specialists in other disciplines (Table 15.7) for the diagnosis and management of the underlying causes of all secondary headache disorders. Specialized headache centres are therefore closely affiliated to a university or other major hospital.
In their second role (Table 15.6), specialized headache centres support nonspecialists at levels 1 and 2 through direct clinical advice, training and development of national management guidelines. This is a symbiotic relationship: demand at level 3 is controllable only when levels 1 and 2 are in place and functioning well. In this role, level 3 not only maintains standards throughout the system but also protects its ability to perform in its first role.
The third role is research (Table 15.6), focused on the other roles. Research may seem a luxury in some countries, but it improves understanding of needs in the local community, what and where they are and how best to meet them. Research thereby helps to control demand while maintaining or improving quality of care.
Finally, specialized centres need to justify their continued existence. Historically, few centres have documented their activities and the outcomes achieved in their intended roles [49,50,51,52, 54,55,56]. In truth this is not easy, but empirical evidence of efficient achievement of desired outcomes justifies investment in the continued existence of specialized centres and appropriate expansion in their number.
3.4.4 Division of Caseload
The model, a broad-based pyramid with a narrow apex, reflects the proportion of presenting patients whose healthcare needs cannot be met at primary care level because of diagnostic or management complexity. Quantitative estimates are necessary. While these are largely based on expert opinion [20], there is some empirical support from a large UK general practice for presuming that about 10% of presenting patients might appropriately be treated at a higher level [12]. Accordingly, level 1 should be able to meet the needs of 90% of people consulting for headache [20] (Fig. 15.1).
On this estimate, and the earlier assumptions about consultation times (Table 15.1), one full-time HCP can provide headache care at level 1 for a population no larger than 30,000 (33 HCPs per million).
Not all of the remaining 10% require the highest (level-3) expertise. In most countries, specialized centres are few and would be overwhelmed even by this proportion. This is the justification for level 2, which should provide care to most patients referred upwards from level 1 (Fig. 15.1). Again on this estimate, and the assumptions about consultation times (Table 15.1), one full-time HCP can provide headache care at level 2 for a population no larger than 200,000 (5 HCPs per million).
At level 3, capacity should match needs at that level: more would simply consume resources that lower levels could use better (i.e. more cost-effectively). When levels 1 and 2 are adequately set up also, demand at level 3 should be limited to no more than 1% of all headache patients (Fig. 15.1). Relieved of the other 99%, specialized headache centres can cover relatively large geographical catchment areas and populations (one full-time specialist per two million people (0.5 per million)). For inpatients, a recommended minimum is two beds per million population [20].
Equitable distribution is a likely challenge, well exemplified by a survey in Brazil. Of 243 “headache specialists” in 2004/2005 (more than twice the number needed in a well-functioning three-level model for Brazil’s 198 million people [57]), the south-east region had 68% for 42.6% of the country’s population, the north-east had only 12.4% for 28.1% of the population, and five of Brazil’s 27 States had none at all [58].
3.4.5 The Gatekeeper Role Within the Model
One of the model’s essential purposes is to shift demand from secondary care services into primary care—a move which is not only appropriate from a clinical viewpoint but also, in general, cost-saving [43,44,45,46,47] (see Sect. 15.5). The gatekeeper role of primary care is a key organizational issue [44, 59].
More needs to be said on this, because it is somewhat controversial [59,60,61]. Patients cannot be blamed for seeking access directly to those whom they perceive to be experts, and gatekeeping is not a norm in many countries’ health systems. Ostensibly, where it is in place, gatekeeping guides patients efficiently and in their best interests through the health system according to their needs, not their demands [59]—a somewhat paternalistic but well-intentioned aim. In reality, it is the principal means of preventing overload in specialist services, which would deny access to some who really need it—a more crucial consideration. Whatever its supposed purpose, gatekeeping contributes—and perhaps is essential—to cost containment, because unrestricted access to specialists induces demand for costly and sometimes unnecessary services.
The effectiveness of this model [60], and the equity of it, rely on efficiency at the interfaces between levels, seams in service continuity where breakdowns can occur readily, and detrimentally to patients [61]. There should not be undue system-created delays or other barriers set against those who do need specialist care—an equally crucial consideration (see Chap. 13). Efficient interfaces between the levels are matters of implementation, best determined in the context of local health services. Importantly, if the model is implemented well, with appropriate provision at each level, demand within the three levels is likely to be self-regulating, effectively governed by waiting lists.
3.4.6 Flexibility of the Model
Much depends on this. How this model might be implemented in a country (or in a regional or district pilot) depends on two principal factors: the resources allocated to headache services (which, as a matter of sensible policy, should match the priority due to them) and the general structure of the health service within which these services are accommodated.
National modifications may therefore be demanded, but the model has considerable flexibility, in a number of ways, that allows adaptation without altering its intrinsic structure (Table 15.8).
3.5 Educational Implications
Education has two major roles in better headache services.
On the one hand, public education needs to improve people’s understanding of headache and of the appropriate use of services. It needs to change their behaviour, not only with regard to seeking healthcare but also, and necessarily, to promote better adherence [63, 64]. On the other hand, professional education must ensure that the expertise necessary at levels 1 and 2 is available. Limited but better knowledge of headache, coupled with the use of evidence-based guidelines in primary care [48], can keep the great majority of patients at level 1, reducing unnecessary demand upon specialist care [26, 65]. A somewhat enhanced but still limited knowledge requirement exists at level 2 [20].
There are, however, major political and logistic implications here. The start is to give more emphasis to headache diagnosis and management in the medical school undergraduate curriculum, ensuring that newly qualified doctors will have at least some understanding of a set of burdensome and very common disorders—which is often not the case now. This is far from easily achieved and will itself involve a battle of priorities in an already overfilled curriculum. But much more is needed, and more quickly. Far-reaching training initiatives, at national level, must be part and parcel of effective headache service reform. The educational challenge is greatest at level 1, because of the weight of numbers of HCPs who need training.
Within the three-level care system proposed, a training role for each higher level to the level below can be envisaged. It is likely that the entire structure will depend upon these roles being developed.
4 Political Will
The expectations of successful implementation embrace improved headache services, achieved in a number of complementary ways: greater community-based availability, reduced delivery costs by pulling inappropriate demand in secondary care back into primary care, freed resources to discover and meet unrecognized headache-related healthcare needs in the community, and mitigated lost productivity and its detriment to gross domestic product ([66,67,68,69,70,71,72,73]; also, Chap. 12). All of these outcomes are politically desirable [4]: there should be political will to achieve them.
Distorted priorities may lie at the heart of the current inadequacies. It is likely to be argued that the creation of a better headache-care structure, and the delivery of more effective care, will stimulate demand—with unaffordable results. There is probable truth in this, but it should be recognized that, if this occurs, it is simply unmasking need that is there already, not creating it. In counter-argument, the humanitarian symptom-based burden (see Chaps. 4 and 8) causing substantial public ill health ([4]; also, Chap. 9) must be seen as unacceptable, as is the financial penalty of inaction.
5 The Cost of Doing Nothing
Chapter 12 lays out the high financial cost of headache as it is—imperfectly treated. Global Campaign studies around the world have estimated massive lost-productivity costs: of up to 2% of gross domestic product [66, 68,69,70,71,72,73]. These, enormous though they may be, are not the sole cost of doing nothing.
While major improvements to services may require substantial up-front investment, there is promise—if even a small part of the lost productivity can be recovered—for even greater savings to offset it [4]. These savings, foregone, are also part of the financial penalty of inaction.
Cost-effectiveness of the structured headache services model was analysed by Lifting The Burden (LTB) in collaboration with WHO [34]. The enquiry, including only migraine (because better data were available), asked what monetary investment would yield what amount of population-level disability reduction. The focus was not on individual drugs, although costs and effects of these must be included, but on the means by and extent to which these would reach and be used by people likely to benefit from them. Effect estimation used clinical trial evidence of drug efficacy (first-line acute and prophylactic) and assumed that structured services, when implemented and supported by educational initiatives, would improve both coverage (the proportion of people needing treatment to whom it was made available) and adherence (the proportion actually taking it as intended) [34]. Estimated costs included those of running the services, those of increased treatment uptake and those of the educational initiatives, aimed at both HCPs and people with headache (the public). Epidemiological data were those supplied by LTB to the Global Burden of Disease Study 2010 (GBD2010) ([74]; also, Chap. 9), from population-based surveys in China [32, 68], India [72, 75, 76], Russia [24, 25, 77] and Zambia [71, 78], the countries included. In the analytical WHO-CHOICE model [79], disability weights were also taken from GBD2010 [39].
The analysis found that self-management with simple analgesics, generating a healthy life year (HLY) for less than USD 100, was a very highly, and by far the most, cost-effective strategy for migraine treatment [34]. Adding a triptan, in a stepped-care treatment paradigm [48], required management within headache services and incurred an incremental cost of over USD 10,000 per extra HLY: still cost-effective and an efficient use of health resources in low- and middle-income countries. Consumer education and provider training were also economically attractive, accelerating progress towards desired levels of coverage and adherence while costing relatively little to implement [34].
However, this analysis was limited in scope: it did not include other headache disorders than migraine, and, crucially, it ignored the indirect costs of lost work productivity (absenteeism because of headache and reduced working effectiveness of those at work despite headache ([66,67,68,69,70,71,72,73]; also, Chap. 12)).
In a further collaboration, between LTB, European Headache Federation (EHF), European Brain Council (EBC) and London School of Economics, wider-ranging analyses are underway (not yet formally published). These similarly estimate cost-effectiveness of structured services delivering appropriate treatments with known efficacy. They compare baseline (current care) with a target scenario in which implemented services, provider training and consumer education improve both coverage and adherence. They include migraine, TTH and MOH. The perspectives are those of provider and society, so analyses include not only direct costs (resources sunk into healthcare provision) per HLY gained but also direct costs invested versus indirect costs saved. Because of the European interests of EHF and EBC, the analyses were of Russia, Spain and Luxembourg, European countries for which LTB had population-based data [22,23,24,25, 27].
The findings, when published, may vary slightly from those in Table 15.9, but the preliminary analyses confirm, as predicted in 2011 by WHO ([4]; also, Chap. 5), that intervention in the form of structured headache services is not only cost-effective but also likely to be cost-saving. The far-right column of Table 15.9 bears witness to the magnitude of the financial penalty of inaction: EUR 6.7 billion per year of unrealized potential savings (in addition to the public-health penalty of 215,000 unrecovered HLYs).
This is a crucial demonstration. The question looms large of how to pay for what the Global Campaign seeks to achieve—beneficial change, in a world of competing demands and scarce resources—but these analyses emphatically provide the answer. While avoidance of wastage is a likely benefit of effective intervention [4], the anticipated benefit of recovered work-productivity losses is greater by far [66,67,68,69,70,71,72,73]. If it is proven that untreated headache costs society more, in total, than treated headache, paying for change should no longer be an issue, at least in more industrialized nations.
On the face of it, governments should urgently want to know this. Perhaps this is the highest priority of all.
But it still has to be empirically demonstrated. The analysis of indirect costs makes assumptions about the relationship between headache-attributed disability and lost productivity. Disability levels of zero and 100% would, presumably, be associated with the same levels of lost productivity, but there is emerging evidence that the relationship between these extremes is far from linear. This is depicted, for migraine, in Fig. 15.2, again showing population-based data from the Global Campaign, from Spain and Luxembourg. At population level, the relationship between disability and lost productivity is clearly complex, with R2 indicating that a linear model explains <12% of the variation.
The relationship between migraine-attributed disability (D) and lost productivity (LP) in population samples from Spain and Luxembourg. D is a proportion on a scale 0–1, calculated as the product of proportion of time in ictal state (attack frequency ∗ attack duration) and disability weight (DW) from GBD2016 ([5]; also, Chap. 9). LP is the proportion of time lost from work (also 0–1), estimated over 3 months from responses to the HALT-90 index [80]
Actually this is not surprising, since many external factors are operating. People have a choice when they wake in the morning with headache, and work beckons. As well as “How ill do I feel?”, personal but non-illness-related questions are brought into play, such as “Is my work important?”, “Do I enjoy it?”, “Can I make up the time later?”, and “Do other people depend on me for their own work?”, along with random factors such as “Is the weather bad?”. All may be influential, but to very different degrees in different people. At individual level, on the other hand, most of these external factors are constant, or at least much less variable, so disability and lost productivity may show the high level of correlation expected. The empirical evidence for this, however, has still to be generated.
In the economic analyses including indirect costs (Table 15.9), structured headache services remain cost-saving if only 4% of lost productivity, proportionately, is recovered by mitigating disability.
6 Concluding Remarks
There are many problems with the current compartmentalized division of headache services between primary and secondary care. The model described seeks vertical integration while recognizing that headache services not only must but readily can be delivered for the most part in primary care. The size of the demand dictates this as the only way forward, but it is a perfectly good way forward in terms of effectiveness of care. The model is capable of adaptation to suit local cultures and healthcare systems. It is cost-effective, and almost certainly cost-saving in all economies.
In all countries, essentially the same need exists, differing only quantitatively. Wherever health-service reform is shifting resources from secondary to primary care, for which momentum is again developing [43, 46, 47], there is opportunity for change. At the same time, in low- and middle-income countries in particular, the growing shift of emphasis in health policy towards chronic non-communicable diseases [81] creates a fair climate for change. Economic (cost-effectiveness) analyses support change.
These arguments must be acknowledged if political will is to be fostered and harnessed and change made to happen. This is the greatest challenge.
References
World Health Organization. Headache disorders and public health. Education and management implications. Geneva: WHO (WHO/MSD/MBD/00.9); 2000.
World Health Organization. Headache disorders. Fact sheet no. 277. Geneva: WHO; 2003.
World Health Organization. Headache disorders. Ch 3.3 in: Neurological disorders: public health challenges. Geneva: WHO; 2007. p. 70–84.
World Health Organization and Lifting The Burden. Atlas of headache disorders and resources in the world 2011. Geneva: WHO; 2011. http://www.who.int/mental_health/management/atlas_headache_disorders/en/2011.
Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V, Abu-Raddad LJ, Ackerman IN, Adamu AA, Adetokunboh O, Afarideh M, Afshin A, Agarwal SK, Aggarwal R, Agrawal A, Agrawal S, Ahmadieh H, Ahmed MB, Aichour MTE, Aichour AN, Aichour I, Aiyar S, Akinyemi RO, Akseer N, Al Lami FH, Alahdab F, Al-Aly Z, Alam K, Alam N, Alam T, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59.
Steiner TJ, Stovner LJ, Vos T, Jensen R, Katsarava Z. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018;19:17.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1–211.
Steiner TJ, Gururaj G, Andrée C, Katsarava Z, Ayzenberg I, Yu SY, Al Jumah M, Tekle-Haimanot R, Birbeck GL, Herekar A, Linde M, Mbewe E, Manandhar K, Risal A, Jensen R, Queiroz LP, Scher AI, Wang SJ, Stovner LJ. Diagnosis, prevalence estimation and burden measurement in population surveys of headache: presenting the HARDSHIP questionnaire. J Headache Pain. 2014;15:3.
Hopkins A, Menken M, De Friese GA. A record of patient encounters in neurological practice in the United Kingdom. J Neurol Neurosurg Psychiatry. 1989;52:436–8.
Wiles CM, Lindsay M. General practice referrals to a department of neurology. J Roy Coll Physicians. 1996;30:426–31.
Laughey WF, Holmes WF, MacGregor AE, Sawyer JPC. Headache consultation and referral patterns in one UK general practice. Cephalalgia. 1999;19:328–9.
Rasmussen BK, Jensen R, Olesen J. Impact of headache on sickness absence and utilisation of medical services: a Danish population study. J Epidemiol Community Health. 1992;46:443–6.
Dowson A, Jagger S. The UK migraine patient survey: quality of life and treatment. Curr Med Res Opin. 1999;15:241–53.
Lipton RB, Scher AI, Steiner TJ, Kolodner K, Liberman J, Stewart WF. Patterns of health care utilization for migraine in England and in the United States. Neurology. 2003;60:441–8.
Takeshima T, Ishizaki K, Fukuhara Y, Ijiri T, Kusumi M, Wakutani Y, Mori M, Kawashima M, Kowa H, Adachi Y, Urakami K, Nakashima K. Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache. 2004;44:8–19.
Radtke A, Neuhauser H. Prevalence and burden of headache and migraine in Germany. Headache. 2009;49:79–89.
Katsarava Z, Mania M, Lampl C, Herberhold J, Steiner TJ. Poor medical care for people with migraine in Europe—evidence from the Eurolight study. J Headache Pain. 2018;19:10.
Antonaci F, Valade D, Lanteri-Minet M, Láinez JM, Jensen J, Steiner TJ. Proposals for the organisation of headache services in Europe. Intern Emerg Med. 2008;3:S25–8.
Steiner TJ, Antonaci F, Jensen R, Lainez MJ, Lanteri-Minet M, Valade D. Recommendations for headache service organisation and delivery in Europe. J Headache Pain. 2011;12:419–26.
American Association for the Study of Headache, International Headache Society. Consensus statement on improving migraine management. Headache. 1998;38:736.
Andrée C, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lair M-L, Lanteri-Minet M, Mick G, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Vriezen P, Lampl C. The Eurolight project: the impact of primary headache disorders in Europe. Description of methods. J Headache Pain. 2011;12:541–9.
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Barré J, Andrée C. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15:31.
Ayzenberg I, Katsarava Z, Sborowski A, Chernysh M, Osipova V, Tabeeva G, Steiner TJ. Headache-attributed burden and its impact on productivity and quality of life in Russia: structured healthcare for headache is urgently needed. Eur J Neurol. 2014;21:758–65.
Ayzenberg I, Katsarava Z, Sborowski A, Obermann M, Chernysh M, Osipova V, Tabeeva G, Steiner TJ. Headache yesterday in Russia: its prevalence and impact, and their application in estimating the national burden attributable to headache disorders. J Headache Pain. 2015;16:7.
Braschinsky M, Haldre S, Kals M, Iofik A, Kivisild A, Korjas J, Koljal S, Katsarava Z, Steiner TJ. Structured education can improve primary-care management of headache: the first empirical evidence, from a controlled interventional study. J Headache Pain. 2016;17:24.
Manandhar K, Risal A, Linde M, Steiner TJ. Health-care utilization for headache disorders in Nepal: a population-based door-to-door survey. J Headache Pain. 2018;19:116.
Wang SJ, Fuh JL, Young YH, Lu SR, Shia BC. Frequency and predictors of physician consultations for headache. Cephalalgia. 2001;21:25–30.
Lampl C, Buzath A, Baumhackl U, Klingler D. One-year prevalence of migraine in Austria: a nation-wide survey. Cephalalgia. 2003;23:280–6.
Lipton RB, Scher AI, Kolodner K, Liberman J, Steiner TJ, Stewart WF. Migraine in the United States: epidemiology and patterns of health care use. Neurology. 2002;58:885–94.
Edmeads J, Findlay H, Tugwell P, Pryse-Phillips W, Nelson RF, Murray TJ. Impact of migraine and tension-type headache on life-style, consulting behaviour, and medication use: a Canadian population survey. Can J Neurol Sci. 1993;20:131–7.
Liu R, Yu S, He M, Zhao G, Yang X, Qiao X, Feng J, Fang Y, Cao X, Steiner TJ. Health-care utilization for primary headache disorders in China: a population-based door-to-door survey. J Headache Pain. 2013;14:47.
Manandhar K, Risal A, Linde M, Steiner TJ. The burden of headache disorders in Nepal: estimates from a population-based survey. J Headache Pain. 2016;17:3.
Linde M, Steiner TJ, Chisholm D. Cost-effectiveness analysis of interventions for migraine in four low- and middle-income countries. J Headache Pain. 2015;16:15.
World Bank. https://data.worldbank.org/indicator/SP.POP.1564.TO.ZS.
World Bank. https://data.worldbank.org/indicator/SP.POP.0014.TO.ZS.
Saylor D, Steiner TJ. The global burden of headache. Semin Neurol. 2018;38:182–90.
Lipton RB, Diamond S, Reed M, Diamond M, Stewart WF. Migraine diagnosis and treatment: results from the American migraine study II. Headache. 2001;41:638–45.
Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, Begum N, Shah R, Karyana M, Kosen S, Farje MR, Moncada G, Dutta A, Sazawal S, Dyer A, Seiler J, Aboyans V, Baker L, Baxter A, Benjamin EJ, Bhalla K, Bin Abdulhak A, Blyth F, Bourne R, Braithwaite T, Brooks P, Brugha TS, Bryan-Hancock C, Buchbinder R, Burney P, Calabria B, Chen H, Chugh SS, Cooley R, Criqui MH, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380:2129–43.
Westergaard ML, Hansen EH, Glumer C, Olesen J, Jensen RH. Definitions of medication-overuse headache in population-based studies and their implications on prevalence estimates: a systematic review. Cephalalgia. 2014;34:409–25.
Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher AI, Steiner TJ, Zwart J-A. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210.
Lyngberg AC, Rasmussen BK, Jørgensen T, Jensen R. Secular changes in health care utilization and work absence for migraine and tension-type headache: a population based study. Eur J Epidemiol. 2005;20:1007–14.
World Health Organization International Conference on Primary Health Care. Declaration of Alma-Ata. Geneva: WHO; 1978.
Tarino E, Webster EG. Primary health care concepts and challenges in a changing world. Alma-Ata revisited. Geneva: WHO; 1995.
Coulter A. Shifting the balance from secondary to primary care. BMJ. 1995;311:1447–8.
Walley J, Lawn JE, Tinker A, de Francisco A, Chopra M, Rudan I, Bhutta ZA, Black RE and the Lancet Alma-Ata Working Group. Primary health care: making Alma-Ata a reality. Lancet. 2008;372:1001–7.
World Health Organization and United Nations Children’s Fund (UNICEF) Global Conference on Primary Health Care. Declaration of Astana. From Alma-Ata towards universal health coverage and the sustainable development goals. Astana, Kazakhstan: WHO/UNICEF; 2018.
Steiner TJ, Jensen R, Katsarava Z, Linde M, MacGregor EA, Osipova V, Paemeleire K, Olesen J, Peters M, Martelletti P on behalf of the European Headache Federation and Lifting The Burden: the Global Campaign against Headache. Aids to management of headache disorders in primary care (2nd edition). J Headache Pain. 2019;20:57.
Harpole LH, Samsa GP, Jurgelski AE, Shipley JL, Bernstein A, Matchar DB. Headache management program improves outcome for chronic headache. Headache. 2003;43:715–24.
Lake AE, Saper JR, Hamel RL. Comprehensive inpatient treatment of refractory chronic daily headache. Headache. 2009;49:555–62.
Göbel H, Heinze A, Heinze-Kuhn K, Henkel K, Roth A, Rüschmann HH. Development and implementation of integrated health care in pain medicine: the nationwide German headache treatment network. Schmerz. 2009;23:653–70.
Jensen R, Zeeberg P, Dehlendorff C, Olesen J. Predictors of outcome of the treatment programme in a multidisciplinary headache center. Cephalalgia. 2010;30:1214–24.
Diener H, Gaul C, Jensen R, Göbel H, Heinze A, Silberstein S. Integrated headache care. Cephalalgia. 2011;31:1039–47.
Saper JR, Lake AE, Madden SF, Kreeger C. Comprehensive tertiary care for headache: a 6-month outcome study. Headache. 1999;39:249–63.
Lemstra M, Stewart B, Olszynski WP. Effectiveness of multidisciplinary intervention in the treatment of migraine: a randomized clinical trial. Headache. 2002;42:845–54.
Rothrock JF, Parada VA, Sims C, Key K, Walters NS, Zweifler RM. The impact of intensive patient education on clinical outcome in a clinic-based migraine population. Headache. 2006;46:726–31.
Populationpyramid.net. https://www.populationpyramid.net/brazil/2010.
Masruha MR, Souza JA, Barreiros H, Piovesan EJ, Kowacs F, Queiroz LP, Ciciarelli MC, Peres MFP. Distribution of “Brazilian headache specialists”. Analyses of Brazilian Headache Society members. Einstein. 2007;5:48–50.
Ferris TG, Chang Y, Blumenthal D, Pearson SD. Leaving gatekeeping behind—effects of opening access to specialists for adults in a health maintenance organization. NEJM. 2001;345:1312–7.
Jones R, Lamont T, Haines A. Setting priorities for research and development in the NHS: a case study on the interface between primary and secondary care. BMJ. 1995;311:1076–80.
Preston C, Cheater F, Baker R, Hearnshaw H. Left in limbo: patients views on care across the primary/secondary interface. Qual Health Care. 1999;8:16–21.
UK Department of Health. Guidelines for the appointment of general practitioners with special interests in the delivery of clinical services: headaches. London: Department of Health; 2003.
Hedenrud T, Jonsson P, Linde M. Beliefs about medicines and adherence among Swedish migraineurs. Ann Pharmacother. 2008;42:39–45.
Mulleners WM, Whitmarsh TE, Steiner TJ. Noncompliance may render migraine prophylaxis useless, but once-daily regimens are better. Cephalalgia. 1998;18:52–6.
Braschinsky M, Haldre S, Kals M, Arge M, Saar B, Niibek M, Katsarava Z, Steiner TJ. Structured education to improve primary-care management of headache: how long do the benefits last? A follow-up observational study. Eur J Neurol. 2018;25:497–502.
Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Andrée C. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19:703–11.
Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med. 1999;159:813–8.
Yu S, Liu R, Zhao G, Yang X, Qiao X, Feng J, Fang Y, Cao X, He M, Steiner T. The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache. 2012;52:582–91.
Selekler MH, Gökmen G, Steiner TJ. Productivity impact of headache on a heavy-manufacturing workforce in Turkey. J Headache Pain. 2013;14:88.
Selekler HM, Gökmen G, Alvur TM, Steiner TJ. Productivity losses attributable to headache, and their attempted recovery, in a heavy-manufacturing workforce in Turkey: implications for employers and politicians. J Headache Pain. 2015;16:96.
Mbewe E, Zairemthiama P, Paul R, Birbeck GL, Steiner TJ. The burden of primary headache disorders in Zambia: national estimates from a population-based door-to-door survey. J Headache Pain. 2015;16:36.
Steiner TJ, Rao GN, Kulkarni GB, Gururaj G, Stovner LJ. Headache yesterday in Karnataka state, India: prevalence, impact and cost. J Headache Pain. 2016;17:74.
Zebenigus M, Tekle-Haimanot R, Worku DK, Thomas H, Steiner TJ. The burden of headache disorders in Ethiopia: national estimates from a population-based door-to-door survey. J Headache Pain. 2017;18:58.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, et al. Years lived with disability (YLD) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–96.
Kulkarni GB, Rao GN, Gururaj G, Stovner LJ, Steiner TJ. Headache disorders and public ill-health in India: prevalence estimates in Karnataka state. J Headache Pain. 2015;16:67.
Rao GN, Kulkarni GB, Gururaj G, Stovner LJ, Steiner TJ. The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka state. J Headache Pain. 2015;16:94.
Ayzenberg I, Katsarava Z, Sborowski A, Chernysh M, Osipova V, Tabeeva G, Yakhno N, Steiner TJ. The prevalence of primary headache disorders in Russia: a countrywide survey. Cephalalgia. 2012;32:373–81.
Mbewe E, Zairemthiama P, Yeh H-H, Paul R, Birbeck GL, Steiner TJ. The epidemiology of primary headache disorders in Zambia: a population-based door-to-door survey. J Headache Pain. 2015;16:30.
World Health Organization. Cost effectiveness and strategic planning (WHO-CHOICE). http://www.who.int/choice/cost-effectiveness/en/.
Steiner TJ, Lipton RB on behalf of Lifting The Burden: The Global Campaign against Headache. The Headache-Attributed Lost Time (HALT) indices: measures of burden for clinical management and population-based research. J Headache Pain. 2018;19:12.
World Health Organization. Noncommunicable diseases. 2018. http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Steiner, T.J. et al. (2019). The Healthcare Solution to Headache. In: Steiner, T., Stovner, L. (eds) Societal Impact of Headache. Headache. Springer, Cham. https://doi.org/10.1007/978-3-030-24728-7_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-24728-7_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-24726-3
Online ISBN: 978-3-030-24728-7
eBook Packages: MedicineMedicine (R0)