Abstract
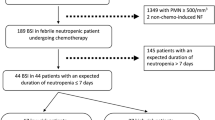
Neutropenic patients are predisposed to polymicrobial infections that may cause substantial morbidity and mortality. Neutropenia is defined as a neutrophil count of <500 cells/mm3, or a count of <1000 cells/mm3 with a predicted decrease to <500 cells/mm3. Many factors play a role in the development of bacteremia such as the use of cytotoxic chemotherapy that leads to neutropenia, and also contributes to the disruption of skin and mucosal barriers. Moreover, exposure to pathogens is possible due to the frequent utilization of foley catheters and venous catheters in patients with cancer (Rolston et al., Clin Infect Dis 45(2):228–233, 2007). Lastly, the use of prophylactic antibiotics can lead to breakthrough MDR bacteria limiting antimicrobial options for therapy (Rolston et al., Clin Infect Dis 45(2):228–233, 2007; Perez et al., Clin Infect Dis 59(Suppl 5):S335–S339, 2014).
Both gram-negative and gram-positive organisms are culpable for infection in these immunocompromised patients. Although gram-negative bacteremia is still a leading cause in most recent years, infections by gram-positive bacteria have increased. This could be secondary to the wide use of long-term vascular catheters (Holland et al., Clin Infect Dis 59(Suppl 5):S331–S334, 2014; Baskaran et al., Int J Infect Dis: IJID: Off Publ Int Soc Infect Dis 11(6):513–517, 2007).
The most common microorganisms that cause bacteremia in neutropenic patients are the Enterobacteracie group, Pseudomonas aeruginosa , Staphylococcus aureus, Coagulase negative Staphylococci, and streptococcus species. In addition, other species will be discussed in this chapter (Rolston et al., Clin Infect Dis 45(2):228–233, 2007; Baskaran et al., Int J Infect Dis: IJID: Off Publ Int Soc Infect Dis 11(6):513–517, 2007; Yadegarynia et al., Caspian J Int Med 4(3):698–701, 2013).
Less common bacteria including nocardia and mycobacterium spp will not be discussed in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Viridans Group Streptococci (VGS)
- Toxic shock-like syndrome
- Stenotrophomona Maltophilia
- VRE colonization
- C. jeikeium
- Rothia mucilaginosa
- Fusobacterium necrophorum
- F. nucleatum
- Carbapenemase-producing Klebsiella pneumoniae (KPC)
- Pseudomonas aeruginosa
- MRSA
- Multidrug resistant (MDR)
Gram Positive Organisms
Gram positive bacteria have been an important cause of bacteremia in neutropenic patients. Many studies have concluded that this rate is only increasing exponentially over the years. One study from the International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer documented that almost 30% of single microorganism isolates recovered during mid 1970’s were Gram positive bacteria, compared with 67% of such organisms isolated during the early 1990’s [1]. Among the most common organisms are Staphylococcus aureus, coagulase negative Staphylococcus and streptococcus species. A very important cause of bacteremia in patients with neutropenia and cancer is Viridans group streptococci (VGS), originating from the normal flora in humans [1].
Viridans Group Streptoccoci (VGS)
In most recent years, the isolation of VGS from the blood of neutropenic patients with cancer has increased. Streptococcus mitis has been the most common pathogen in these cases. VGS are part of the oral cavity flora. They are also found on the skin, female genital tract, upper respiratory tract and the gastrointestinal tract. In normal conditions this organism has low morbidity, but they cause serious infection when the oral mucosa or other sites are compromised along with a deficient host defense such as in a patient with neutropenia and cancer.
In neutropenic patients, this organism can cause very high fevers for several days in spite of proper antibiotics. In addition, it has been associated with toxic shock like syndrome and ARDS as discussed below.
Severe neutropenia is an important factor for VGS bacteremia. Other risk factors include bone marrow transplantation and mucositis [2].
Chemotherapy induced gastric ulcers may allow streptococci to grow in an environment with low acid protection due to the administration of agents such as proton pump inhibitors, histamine 2 blockers and antacids [1].
Chemotherapeutic agents predispose the patients to immunosupression. Cytosine arabinoside, which is an antimetabolic agent used in the treatment of acute myeloid leukemia, acute lymphocytic leukemia and lymphomas, at high doses has been implicated as a risk factor for bacteremia with VGS. Certain antimicrobial agents may predispose to bacteremia with VGS. Oral prophylaxis with either sulfamethoxazole trimethoprin or fluoroquinolones has been highly associated with VGS due to the resistance of this bacteria to these agents [3, 4].
Viridans Streptococci Toxic Shock-like Syndrome and ARDS
In approximately 21–25% of children post- bone marrow transplant, a toxic shock-like syndrome has been reported with VGS bacteremia. The usual organism isolated is S. mitis. This syndrome is very rare in patients without neutropenia and presents with hypotension, palmar desquamation, respiratory distress syndrome, rash, fever, and confusion, which can rapidly progress to coma, multiple organ failure and death. This syndrome usually occurs within 2 or 3 days after presentation. The symptoms may worsen and produce respiratory symptoms within 48 h. This complication is believed to be immunologically mediated [5].
ARDS presents with hypoxia and shortness of breath. Cough and fever are often present. Tachycardia and tachypnea are common features and may be the initial symptoms. Occasionally, patients may experience pleuritic pain followed by hypoxia and respiratory failure [6].
Resistance of VGS against many antibiotics has been increasingly recognized. In early studies, it was concluded that this pathogen was susceptible to penicillin, however, some studies have described intermediate and high-level penicillin resistance. Resistances against second generation cephalosporins, such as Cefuroxime and third generation cephalosporins like Ceftriaxone have also been described [1].
Due to its high efficacy and low resistance, Vancomycin is routinely given in addition to various β-lactam agents (cefepime, ceftriaxone, piperacillin tazobactam or carbapenem) as part of the initial empirical antimicrobial regimens for neutropenic patients with VGS bacteremia [1] (Table 1). Once susceptibilities results are available, vancomycin can be discontinued if indicated.
If hypoxia is present, corticostisteroids should be given to prevent the development of ARDS and respiratory failure [5].
The mortality rate due to VGS bacteremia in spite of appropriate antibiotics can fluctuate from 0 to 20% but can increase up to 60–100%if toxic shock like syndrome develops [1].
Staphylococcus aureus
S. aureus is a major cause of infection in neutropenic patients with cancer. Although S. aureus is most commonly implicated in soft tissue infections and pneumonia, it is responsible for almost 15% of bacteremia cases [7].
The presence of pneumonia and bacteremia results in a mortality rate for up to 50% which is higher than that observed in patients without cancer.
Treatment of S. aureus bacteremia in neutropenic patients does not differ from the non-neutropenic. Early removal of the central venous catheter (CVC) and prolonged intravenous antibiotic therapy for several weeks is recommended especially for complicated endovascular infections and persistent bacteremias [8, 9].
Initial empiric treatment should include vancomycin until methicillin resistant Staphylococcus aureus (MRSA) is excluded. If methicillin sensitive Staphylococcus is isolated, vancomycin can be de-escalated to a beta-lactam agent such as nafcillin, oxacillin, or cefazolin (Table 1).
Echocardiogram is recommended for all the patients with S. aureus bacteremia to rule out endocarditis [10, 11].
Enterococci
Enterococci spp are low virulence organisms; however, they represent a major cause of bacteremia in the cancer population. E. faecalis and E. faecium are the most common species of enterococcus bacteremia in cancer patients. Risk factors for bacteremia include nosocomial infection, prior antibiotic exposure including levofloxacin, prolonged neutropenia, and stem cell transplantation [12, 13].
Enterococci faecium susceptibilities to B-Lactam antibiotics varies, and vancomycin resistance is increasing [14].
The mechanism of resistance of Vancomycin-resistant enterococci (VRE) is due to the change in the bacterial cell wall decreasing the affinity of vancomycin to its site of action. VRE species more commonly encode the VanA and the VanB genotypes followed by the VanD and the VanC genotypes [15].
Colonization of VRE in the stool of neutropenic patients, represent high risk of subsequent VRE bacteremia [13, 16].
The treatment of choice for enterococcus bacteremia includes penicillin type of antibiotics such as ampicillin or piperacillin provided that the organism is sensitive. Vancomycin is also an option for penicillin allergic patients (Table 1). Compared with other streptococcus species, enterococcus are more resistant to killing by monotherapy with the above antibiotics. Combination therapy including aminoglycosides or double beta lactam including ceftriaxone is usually recommended for endocarditis. Data on combination therapy for uncomplicated enterococcus bacteremia are scarce.
Daptomycin and linezolid are the most widely used antibiotics for VRE faecium or VRE fecalis bacteremia [15] (Table 1).
In vitro studies have revealed synergy when using daptomycin in combination with ampicillin or ceftaroline for complicated and persistent VRE bacteremia [17].
Corynebacterium
Corynebacterium are aerobic, gram positive, catalase-positive, nonsporulating, nonmotile rods. There are many subtypes of Corynebacterium, such as C. diptheriae and nondiptherial, like Corynebaterium striatum, Corynebacterium amycolatum, Corynebacterium minutissimum, Corynebacterium xerosis, Corynebacterium freneyi and Corynebacterium jeikeium . They were thought to be contaminants as they are present in the normal flora, but recent studies have shown that they are opportunistic pathogens in immunocompromised hosts with cancer and hematologic malignancies. In this section, we will review the Corynebactrerium species most relevant in neutropenic patients.
Corynebacterium striatum
Corynebacterium striatum colonize the skin and mucous membranes of humans. They are also found in the environment. C. striatum has rarely been reported to be a pathogen, causing pulmonary infections and bacteremia only in immunocompromised patients. Infections are also associated with implanted indwelling devices. Thrombophlebitis associated with central venous catheters has been reported. The majority of C. Striatum infections are nosocomial wound infections and less often, systemic infections.
All strains of C. striatum are resistant to penicillin, but are susceptible to other beta lactam antibiotics and to vancomycin. For serious infections vancomycin is the drug of choice [18, 19] (Table 1).
Corynebacterium jeikeium
C. jeikeium is only pathogenic for humans. It is found in soil and water and is part of normal human skin flora. The colonization rate increases with hospitalization. C. jeikeium is the most common cause of diphtheroid endocarditis of prosthetic valves.
C. jeikeium infections may present with skin and soft tissue lesions in patients who are granulocytopenic. Lesions are usually at local infection sites of previous bone marrow biopsy, intravascular catheter insertion, or perianal fissures. The lesions usually precede septicemia and are designated as the primary source of infection [20, 21].
Corynebacterium jeikeium is highly resistant to beta-lactam agents, aminoglycosides, and quinolones. Vancomycin is the most active antibiotic (Table 1). High level daptomycin resistance is rare with one case report of bacteremia reported [22].
In general, removal of the CVC is recommended in order to clear the bacteremia. Removal of involved prosthetic device is usually required for cure [22].
Rothia mucilaginosa
Rothia mucilaginosa (previously known Stomatococcus mucilaginosus) is an aerobic or facultative anaerobic gram positive cocco bacilli. Rothia spp are part of the oropharynx flora and can be associated with periodontal disease. Risk factors for invasive disease include profound neutropenia, alcoholism, liver disease and HIV infection. Clinical syndromes include bacteremia, endocarditis, meningitis, pneumonia, and infections of the bone and soft tissues [23].
Previous studies have demonstrated that Rothia spp are susceptible to most beta lactam agents, however species with partial resistance to penicillin and methicillin have been recently described. Given concerns for beta lactam resistace, vancomycin is the ideal empiric therapy for Rothia mucilaginosa bacteremia until susceptibilities are available [23] (Table 1).
Lactobacillus
Lactobacilli are gram positive microareophilic organisms that are part of the normal oral, gastrointestinal and genitourinary flora. Bacteremia is rare, but the most common species associated with this entity are Lactobacillus casei and Lactobacillus rhamnosus. Clinical manifestations of Lactobacillus bacteremia can range from asymptomatic to fever, leukocytosis and rigors or severe septicemia and may be combined with pneumonia, deep abdominal abscesses or endocarditis. Some findings also include elevated c – reactive protein values. The infection may be underdiagnosed, because lactobacilli are difficult to culture and to identify and are often confused as contaminants. L. rhamnosus cause more severe infections with a higher inflammatory response.
Risk factors include persistent prolonged neutropenia, use of broad-spectrum antibotics, especially vancomycin (which results in the persistence of vancomycin resitant GI flora), corticosteroids and a history of organ transplantation and other immunosuppressive conditions [24].
The treatment of choice for Lactobacillus bacteremia include penicillin, ampicillin and piperacillin. Clindamycin is also an active agent (Table 1). Susceptibilities to cephalosporins varies. Combination therapy with penicillin and aminoglycosides may be required for complicated infections. Lactobacillus are uniformly resistant to vancomycin [25].
Anaerobic Bacteremia
Information on anaerobic bacteremia in cancer patients is very limited since it only represents about 5–9% of all episodes of bacteremia in hospitalized patients. Anaerobic bacteremia may be undetected due to subtle clinical symptoms. Chemotherapy causes mucosal and visceral damage thus increasing the risk of bacteremia related to endogenous anaerobes.
Gastrointestinal and hematological malignancies are the most common underlying diseases, female genital tract malignancies are also important to note. Most cases of anaerobic bacteremia are caused by Bacteroides fragilis, Clostridium perfringens and Peptostreptococcus spp. Other less common pathogens, but still important in neutropenic patients is Fusobacterium spp. [26, 27].
Empirical antimicrobial therapy should be started as soon as the infection is suspected. Prompt and adequate therapy is associated with increased survival. In general aminopenicilins, with or without B-lactamase inhibitors, Carbapenems, Clindamycin and Metronidazole are active against anaerobic isolates with some spectrum difference depending on the species isolated [28].
Fusobacterium necrophorum
Fusobacterium necrophorum represents less than 1% of bacteremias in humans. Only a few hundred cases have been reported in the literature. F. Necrophorum is associated with severe septicemia also known as necrobacillosis, postanginal sepsis or Lemierre’s syndrome.
Lemierre’s Syndrome
Lemierre’s syndrome is a very serious complication of pharyngeal infection due to F. necrophorum. It usually occurs a few days after the onset of a sore throat.
A more concise definition for Lemierre’s syndrome is the presence of a history of angina illness or similar clinical findings, followed by internal jugular vein thrombophlebitis which propagates from the tonsillar veins to the internal jugular vein causing septicemia. This causes septic emboli including necrotic abscesses the lungs and other sites such as bones, liver and joints. Isolation of F. necrophorum from blood culture or any other sterile site is a good indicator for diagnosis, but it is not found in all cases of this disease. It is not clear whether it is due to external factors such as timing of sampling, prior antibiotic therapy or the association of this disease with other organisms such as Peptostreptococcus.
The diagnosis of Lemierre’s syndrome is clinical. Although this is a very rare disease, its peculiar symptoms should prompt clinical suspicion. The onset of rigors 4–12 days after the resolution of the sore throat is classic. The occurrence of chills indicate that the organisms are present in the circulation. Patients may complain of neck pain and tenderness. Anterior cervical lymphadenopathy is often present. Edema at the angle of the jaw, reflecting the development of internal jugular thrombophlebitis may be mistaken for tender cervical nodes [29, 30].
Fusobacterium nucleatum
This Gram-negative bacilli is commonly found in the gastrointestinal, oropharyngeal and respiratory tracts. It is a common cause of periodontal infection. The most common source of bacteremia associated with F. nucleatum comes from an oropharyngeal source of infection [31].
Certain risk factors overlap amongst patients with F. nucleatum and F. necrophorum . The most common types of malignancy associated with bacteremia include lymphoma and acute leukemia. Treatment with intensive chemotherapy, corticosteroids and bone marrow transplantation also increases the risk for bacteremia. Severe oral mucositis caused by chemotherapy is also an important risk factor as it can serve as a portal of entry for a systemic infection and the propagation of a polymicrobial infection with other pathogens, such as Staphylococcus and E. coli. Prophylactic treatment with macrolides, especially erythromycin is an important risk factor for F. necrophorum infection due to its high resistance [32].
Penicillin, piperacillin-tazobactam, carbapenems, clindamycin and metronidazole are all active against F. nucleatum F. necrophorum . [33] (Table 2)
Gram-Negative Rods
Gram negative bacilli are a very common cause of bacteremia in neutropenic patients. The most common gram-negative rods causing bacteremia are Escherichia coli, Klebsiella spp. and Pseudomona aeruginosa . Before the introduction of the antibiotic era, mortality rates in neutropenic patients with leukemia and Gram-negative infections were as high as 91%. In general, Gram-negative bacteria are reported as MDR if not susceptible to at least 3 of the following antimicrobials: Antipseudomonal penicillins, cephalosporins, carbapenems, aminoglycosides or fluorquinolones [34].
In this chapter, we will discuss the most common gram negative organisms that cause bacteremia in neutropenic patients.
Escherichia coli
Escherichia coli is of great concern in immunocompromised patients. There has been an emergence of a resistant E. coli sequence type ST131. This type of E. coli produces extended-spectrum β-lactamases, and almost all are resistant to fluoroquinolones. Data suggests that this strains of E. coli may be the main explanation for the recent increase in antimicrobial resistance. Serious extra-intestinal infections with this Multi Drug Resistant E. coli ST131 often leave physicians with limited treatment options, higher costs, and increased usage of last resort antimicrobials, such as carbapenems. E. coli is a major pathogen and one of the most common cause of gram negative bacteremia resulting in extended hospital stays. E. coli, like many Gram-negative pathogens can cause septic shock with a fatal outcome.
The most common risk factors for E. coli bacteremia are solid tumors of the gastrointestinal tract, previous chemotherapy, prior surgery within 10 days and vascular catheter insertion [40,41,37].
The treatment of choice for E coli bacteremia include piperacillin tazobactam, cephalosporins, and carbapenems. Combination with aminoglycosides until susceptibilities are available may be required depending on prior cultures, recent use of antibiotics or local susceptibility data (Table 3).
Klebsiella pneumoniae
Some strains of Klebsiella pneumonia are part of the gastrointestinal flora. When the mucosal barrier of the gastrointestinal tract is disrupted, this bacteria can gain access to the blood stream causing serious blood stream infections. Profound neutropenia especially with chemotherapy treatment within 1 month represent a substantial risk for bacteremia [38].
Carbapenemase-producing Klebsiella pneumoniae (KPC) has been identified as an important strain causing nosocomial bacteremia in patients with hematologic malignancies and aplastic anemia [39].
Mortality rates for Klebisella bacteremia is higher when the initial empiric treatment is inadequate [40]. Age plays an important role where newborns and elderly are primarily susceptible.
The treatment of choice for klebsiella bacteremia include piperacillin tazobactam, cephalosporins, and carbapenems. Aminoglycosides in combination with the one of the above also can be used for initial empiric therapy pending susceptibilities (Table 3).
Carbapenems are preferable to piperacillin/tazobactam or cephalosporins when a critically ill patient is in need of empirical therapy especially when there is concern for resistance. Patients who receive a carbapenem as monotherapy or combination therapy during the first days after a blood culture is positive for an extended spectrum beta-lacatamse (ESBL) producing K. pneumoniae, had a significantly lower mortality than those who received non-carbapenem antibiotics [40].
Pseudomonas aeruginosa
Pseudomonas aeruginosa infections in neutropenic cancer patients have decreased after the implementation of antibiotics with-anti-pseudomonal activity; however, they are still one of the most common gram-negative bacterial species associated in neutropenic patients.
Mortality due to this pathogen is reported to be about 20% and this number can increase in patients receiving inappropriate antibacterial treatment. Polymicrobial infection is associated with a worse prognosis.
Patients with Pseudomonas bacteremia treated with combination empirical antimicrobial therapy prior to the result susceptibility testing are available have a better 30-day survival compared to monotherapy. However, combination antimicrobial therapy given as definitive treatment for P. aeruginosa bacteremia does not improve the rate of survival compared to appropriate definitive monotherapy. A potential advantage of initial empiric combination antimicrobial therapy over monotherapy is the higher probability that the infecting pathogen will be covered by at least one of the components of the regimen until susceptibly data is available. Furthermore, different mechanisms of action between two antibiotics may be synergistic, resulting in enhanced bacterial kill activity compared to the additive activities of the antibiotics when assessed separately. Finally, use of combination therapy may suppress emergence of resistant subpopulations of bacteria.
Treatment of pseudomonas bacteremia include piperacillin tazobactam, cefepime, cefazidime, meropenem, imipenem, or doripenem. Aminoglycoside combination therapy may be helpful to broaden the antimicrobial coverage for MDR strains and consequently improve the outcomes of patients with P. aeruginosa bacteremia. Once more information is obtained from the cultures, a targeted antimicrobial agent based on the antibiotic susceptibility results may be pursued [46,47,48,44] (Table 3).
For more resistant strains of pseudomonas, ceftolozane-tazobactam can be an option [45].
Stenotrophomona Maltophilia
Stenotrophomona Maltophilia is rarely responsible for community-acquired serious infections. Rather, it is usually a commensal, a colonizer, or part of the endogenous flora of hospitalized patients. It has been increasingly reported as a cause of life-threatening infections, especially in the immunocompromised, such as those with hematological malignancy and in recipients of hematopoietic stem cell transplantation (HSCT), indwelling venous catheterization, long-term hospitalization, aggressive chemotherapy and use of broad-spectrum antibiotics including carbapenems [46].
S. maltophilia bacteremia in patients with hematologic malignancies is a serious complication of profound, persistent neutropenia and broad-spectrum antibiotic use. This pathogen is highly resistant and its antimicrobial resistance may increase when patients are treated with antibiotics over extended periods. Inappropriate antibiotic use is associated with an elevated morbidity and mortality [47, 48].
Complications of S. maltophilia infections are septic shock, respiratory failure, pulmonary hemorrhage and septic thrombophlebitis. Morbidity and mortality are high; however, the prognosis may be improved by prompt administration of active antibiotics.
S. maltophilia strains are resistant to the majority of agents used for the empirical treatment of febrile neutropenia including most beta-lactams. Sulfamethoxazole-Trimethoprin and minocycline are very active against most stenotrophomona infections [49, 50] (Table 3).
Newer quinolones, particularly in combination with Sulfamethoxazole-Trimethoprin may be an option. Other combination agents can be used depending on the susceptibilities of the organisms [51].
Multidrug Resistant Gram Negative
The widespread use of antibiotics and the emergence of multidrug resistant (MDR) bacteria has shown to increase mortality particularly in immunosuppressed patients. Screening for MDR bacteria may facilitate prompt isolation and directed treatment targeting the MDR bacteria when the patient demonstrates early signs of infection [52].
Carpapenem-Resistant Enterobacteria (CRE)
Neutropenic patients are at risk for enteric gram negative rod bacteremia from gastrointestinal tract translocation. Beta- lactam agents are recommended for empiric therapy of neutropenic fever, however over the last decade, CRE have emerged as a threat particularly to this vulnerable population.
Identification of CRE usually takes up to 3 days using conventional culture methods. This can delay proper treatment significantly increasing mortality [53].
CRE are universally resistant to all beta-lactam agents due to different carbapenemases. Carbapenemase are classified as type A, B, C and D depending on their molecular structure.
The most clinically significant and the most common type in United States is the Class A beta-lactamase known as klebsiella pneumonia carbapenemase (KPC) [54].
Class B beta-lactamase are also known as the metallo-beta-lactamases (MBLs). The New Delhi metallo-beta-lactamase is the most clinically significant of this group [55].
Class D beta-lactamases are also named the OXA type enzymes because of their preference to hydrolyze oxacillin over penicillin. Six subgroups have been identify with different degrees of carbapenem hydrolyzing activity [56].
Treatment recommendations for CRE infections is limited and controversial depending on the subtype and susceptibility results. For KPC, ceftazidime-avibactam or meropenem varbobactam are an option provided that the organism is susceptible [57, 58].
Other alternatives particularly for subtypes resistant to the above antimicrobials i.e. the MBLs include a polymyxin based regimen combined with prolonged carbapenem infusion. For polymyxin resistant strains ceftazidime-avibactam in combination with aztreonam has been used [59].
Other antibiotics with a broader spectrum to treat MDR gram negative rods are under different stages of development including imipenem/cilastin with relebactam, avibactam combined with aztreonam or ceftaroline [60].
Newer antibiotics hopefully will offer a light of cure of MDR gram negative infections in neutropenic patients while receiving aggressive chemotherapy.
References
Tunkel AR, Sepkowitz KA. Infections caused by viridans streptococci in patients with neutropenia. Clin Infect Dis. 2002;34(11):1524–9.
Husain E, Whitehead S, Castell A, Thomas EE, Speert DP. Viridans streptococci bacteremia in children with malignancy: relevance of species identification and penicillin susceptibility. Pediatr Infect Dis J. 2005;24(6):563–6.
Wisplinghoff H, Reinert RR, Cornely O, Seifert H. Molecular relationships and antimicrobial susceptibilities of viridans group streptococci isolated from blood of neutropenic cancer patients. J Clin Microbiol. 1999;37(6):1876–80.
Razonable RR, Litzow MR, Khaliq Y, Piper KE, Rouse MS, Patel R. Bacteremia due to viridans group Streptococci with diminished susceptibility to Levofloxacin among neutropenic patients receiving levofloxacin prophylaxis. Clin Infect Dis. 2002;34(11):1469–74.
Dompeling EC, Donnelly JP, Raemaekers JM, De Pauw BE. Pre-emptive administration of corticosteroids prevents the development of ARDS associated with Streptococcus mitis bacteremia following chemotherapy with high-dose cytarabine. Ann Hematol. 1994;69(2):69–71.
Mokart D, van Craenenbroeck T, Lambert J, Textoris J, Brun JP, Sannini A, et al. Prognosis of acute respiratory distress syndrome in neutropenic cancer patients. Eur Respir J. 2012;40(1):169–76.
Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28(3):603–61.
El Zakhem A, Chaftari AM, Bahu R, El Helou G, Shelburne S, Jiang Y, et al. Central line-associated bloodstream infections caused by Staphylococcus aureus in cancer patients: clinical outcome and management. Ann Med. 2014;46(3):163–8.
Ghanem GA, Boktour M, Warneke C, Pham-Williams T, Kassis C, Bahna P, et al. Catheter-related Staphylococcus aureus bacteremia in cancer patients: high rate of complications with therapeutic implications. Medicine. 2007;86(1):54–60.
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18–55.
Holland TL, Arnold C, Fowler VG Jr. Clinical management of Staphylococcus aureus bacteremia: a review. JAMA. 2014;312(13):1330–41.
Garsin DA, Frank KL, Silanpaa J, Ausubel FM, Hartke A, Shankar N, et al. Pathogenesis and models of enterococcal infection. In: Gilmore MS, Clewell DB, Ike Y, Shankar N, editors. Enterococci: from commensals to leading causes of drug resistant infection. Boston: Massachusetts Eye and Ear Infirmary; 2014.
Sanchez-Diaz AM, Cuartero C, Rodriguez JD, Lozano S, Alonso JM, Rodriguez-Dominguez M, et al. The rise of ampicillin-resistant Enterococcus faecium high-risk clones as a frequent intestinal colonizer in oncohaematological neutropenic patients on levofloxacin prophylaxis: a risk for bacteraemia? Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis. 2016;22(1):59.e1–8.
Cetinkaya Y, Falk P, Mayhall CG. Vancomycin-resistant enterococci. Clin Microbiol Rev. 2000;13(4):686–707.
Levitus M, Perera TB. Vancomycin-Resistant Enterococci (VRE). StatPearls. Treasure Island: StatPearls Publishing StatPearls Publishing LLC.; 2018.
Alevizakos M, Gaitanidis A, Nasioudis D, Tori K, Flokas ME, Mylonakis E. Colonization with vancomycin-resistant enterococci and risk for bloodstream infection among patients with malignancy: a systematic review and meta-analysis. Open Forum Infect Dis. 2017;4(1):ofw246.
Bartash R, Nori P. Beta-lactam combination therapy for the treatment of Staphylococcus aureus and Enterococcus species bacteremia: a summary and appraisal of the evidence. Int J Infect Dis: IJID: Off Publ Int Soc Infect Dis. 2017;63:7–12.
Daisuke U, Oishi T, Yamane K, Terada K. Corynebacterium striatum bacteremia associated with a catheter-related blood stream infection. Case Rep Infect Dis. 2017;2017:2682149.
Watkins DA, Chahine A, Creger RJ, Jacobs MR, Lazarus HM. Corynebacterium striatum: a diphtheroid with pathogenic potential. Clin Infect Dis. 1993;17(1):21–5.
Rozdzinski E, Kern W, Schmeiser T, Kurrle E. Corynebacterium jeikeium bacteremia at a tertiary care center. Infection. 1991;19(4):201–4.
Dan M, Somer I, Knobel B, Gutman R. Cutaneous manifestations of infection with Corynebacterium group JK. Rev Infect Dis. 1988;10(6):1204–7.
Rezaei Bookani K, Marcus R, Cheikh E, Parish M, Salahuddin U. Corynebacterium jeikeium endocarditis: a case report and comprehensive review of an underestimated infection. IDCases. 2018;11:26–30.
Ramanan P, Barreto JN, Osmon DR, Tosh PK. Rothia bacteremia: a 10-year experience at Mayo Clinic, Rochester, Minnesota. J Clin Microbiol. 2014;52(9):3184–9.
Salminen MK, Rautelin H, Tynkkynen S, Poussa T, Saxelin M, Valtonen V, et al. Lactobacillus bacteremia, clinical significance, and patient outcome, with special focus on probiotic L. rhamnosus. GG Clin Infect Dis: Off Publ Infect Dis Soc Am. 2004;38(1):62–9.
Antony SJ. Lactobacillemia: an emerging cause of infection in both the immunocompromised and the immunocompetent host. J Natl Med Assoc. 2000;92(2):83–6.
Lassmann B, Gustafson DR, Wood CM, Rosenblatt JE. Reemergence of anaerobic bacteremia. Clin Infect Dis. 2007;44(7):895–900.
Noriega LM, Van der Auwera P, Phan M, Daneau D, Meunier F, Gerain J, et al. Anaerobic bacteremia in a cancer center. Support Care Cancer: Off J Multinat Assoc Support Care Cancer. 1993;1(5):250–5.
Zahar JR, Farhat H, Chachaty E, Meshaka P, Antoun S, Nitenberg G. Incidence and clinical significance of anaerobic bacteraemia in cancer patients: a 6-year retrospective study. Clin Microbiol Infect. 2005;11(9):724–9.
Riordan T. Human infection with Fusobacterium necrophorum (Necrobacillosis), with a focus on Lemierre’s syndrome. Clin Microbiol Rev. 2007;20(4):622–59.
Centor RM, Atkinson TP, Ratliff AE, Xiao L, Crabb DM, Estrada CA, et al. The clinical presentation of Fusobacterium-positive and streptococcal-positive pharyngitis in a university health clinic: a cross-sectional study. Ann Intern Med. 2015;162(4):241–7.
Candoni A, Fili C, Trevisan R, Silvestri F, Fanin R. Fusobacterium nucleatum: a rare cause of bacteremia in neutropenic patients with leukemia and lymphoma. Clin Microbiol Infect. 2003;9(11):1112–5.
Landsaat PM, van der Lelie H, Bongaerts G, Kuijper EJ. Fusobacterium nucleatum, a new invasive pathogen in neutropenic patients? Scand J Infect Dis. 1995;27(1):83–4.
Jensen A, Hansen TM, Bank S, Kristensen LH, Prag J. Fusobacterium necrophorum tonsillitis: an important cause of tonsillitis in adolescents and young adults. Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis. 2015;21(3):266.e1–3.
Gustinetti G, Mikulska M. Bloodstream infections in neutropenic cancer patients: a practical update. Virulence. 2016;7(3):280–97.
Olson D, Yacoub AT, Gjini AD, Domingo G, Greene JN. Escherichia coli: an important pathogen in patients with hematologic malignancies. Mediterranean J Hematol Infect Dis. 2014;6(1):e2014068.
Carratala J, Fernandez-Sevilla A, Tubau F, Callis M, Gudiol F. Emergence of quinolone-resistant Escherichia coli bacteremia in neutropenic patients with cancer who have received prophylactic norfloxacin. Clin Infect Dis. 1995;20(3):557–60.. discussion 61–3
Krcmery V, Spanik S, Mrazova M, Trupl J, Grausova S, Grey E, et al. Bacteremias caused by Escherichia coli in cancer patients – analysis of 65 episodes. Int J Infect Dis: IJID: Off Publ Int Soc Infect Dis. 2002;6(1):69–73.
Ko WC, Paterson DL, Sagnimeni AJ, Hansen DS, Von Gottberg A, Mohapatra S, et al. Community-acquired Klebsiella pneumoniae bacteremia: global differences in clinical patterns. Emerg Infect Dis. 2002;8(2):160–6.
Tofas P, Skiada A, Angelopoulou M, Sipsas N, Pavlopoulou I, Tsaousi S, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections in neutropenic patients with haematological malignancies or aplastic anaemia: analysis of 50 cases. Int J Antimicrob Agents. 2016;47(4):335–9.
Girometti N, Lewis RE, Giannella M, Ambretti S, Bartoletti M, Tedeschi S, et al. Klebsiella pneumoniae bloodstream infection: epidemiology and impact of inappropriate empirical therapy. Medicine. 2014;93(17):298–309.
Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, Oh MD, et al. Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis. 2003;37(6):745–51.
Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH. Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother. 2005;49(4):1306–11.
Kim HS, Park BK, Kim SK, Han SB, Lee JW, Lee DG, et al. Clinical characteristics and outcomes of Pseudomonas aeruginosa bacteremia in febrile neutropenic children and adolescents with the impact of antibiotic resistance: a retrospective study. BMC Infect Dis. 2017;17(1):500.
Kim YJ, Jun YH, Kim YR, Park KG, Park YJ, Kang JY, et al. Risk factors for mortality in patients with Pseudomonas aeruginosa bacteremia; retrospective study of impact of combination antimicrobial therapy. BMC Infect Dis. 2014;14:161.
Lopez-Calleja AI, Morilla Morales E, Nunez Medina R, Fernandez Esgueva M, Sahagun Pareja J, Garcia-Lechuz Moya JM, et al. Antimicrobial activity of ceftolozane-tazobactam against multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa clinical isolates from a Spanish hospital. Revista espanola de quimioterapia : publicacion oficial de la Sociedad Espanola de Quimioterapia. 2019;32(1):68–72.
Micozzi A, Venditti M, Monaco M, Friedrich A, Taglietti F, Santilli S, et al. Bacteremia due to Stenotrophomonas maltophilia in patients with hematologic malignancies. Clin Infect Dis. 2000;31(3):705–11.
Cho SY, Lee DG, Choi SM, Park C, Chun HS, Park YJ, et al. Stenotrophomonas maltophilia bloodstream infection in patients with hematologic malignancies: a retrospective study and in vitro activities of antimicrobial combinations. BMC Infect Dis. 2015;15:69.
Gokhan Gozel M, Celik C, Elaldi N. Stenotrophomonas maltophilia infections in adults: primary bacteremia and pneumonia. Jundishapur J Microbiol. 2015;8(8):e23569.
Al-Anazi KA, Al-Jasser AM. Infections caused by Stenotrophomonas maltophilia in recipients of hematopoietic stem cell transplantation. Front Oncol. 2014;4:232.
Wei C, Ni W, Cai X, Zhao J, Cui J. Evaluation of trimethoprim/sulfamethoxazole (SXT), minocycline, tigecycline, moxifloxacin, and ceftazidime alone and in combinations for SXT-susceptible and SXT-resistant stenotrophomonas maltophilia by in vitro time-kill experiments. PLoS One. 2016;11(3):e0152132.
Looney WJ, Narita M, Muhlemann K. Stenotrophomonas maltophilia: an emerging opportunist human pathogen. Lancet Infect Dis. 2009;9(5):312–23.
Ballo O, Tarazzit I, Stratmann J, Reinheimer C, Hogardt M, Wichelhaus TA, et al. Colonization with multidrug resistant organisms determines the clinical course of patients with acute myeloid leukemia undergoing intensive induction chemotherapy. PLoS One. 2019;14(1):e0210991.
Satlin MJ, Cohen N, Ma KC, Gedrimaite Z, Soave R, Askin G, et al. Bacteremia due to carbapenem-resistant Enterobacteriaceae in neutropenic patients with hematologic malignancies. J Inf Secur. 2016;73(4):336–45.
Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, et al. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45(4):1151–61.
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, et al. Characterization of a new metallo-beta-lactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53(12):5046–54.
Turton JF, Ward ME, Woodford N, Kaufmann ME, Pike R, Livermore DM, et al. The role of ISAba1 in expression of OXA carbapenemase genes in Acinetobacter baumannii. FEMS Microbiol Lett. 2006;258(1):72–7.
Parruti G, Frattari A, Polilli E, Savini V, Sciacca A, Consorte A, et al. Cure of recurring Klebsiella pneumoniae carbapenemase-producing Klebsiella pneumoniae septic shock episodes due to complicated soft tissue infection using a ceftazidime and avibactam-based regimen: a case report. J Med Case Rep. 2019;13(1):20.
Athans V, Neuner EA, Hassouna H, Richter SS, Keller G, Castanheira M, et al. Meropenem-vaborbactam as salvage therapy for ceftazidime-avibactam-resistant klebsiella pneumoniae bacteremia and abscess in a liver transplant recipient. Antimicrob Agents Chemother. 2019;63(1):1–8.
Marshall S, Hujer AM, Rojas LJ, Papp-Wallace KM, Humphries RM, Spellberg B, et al. Can ceftazidime-avibactam and aztreonam overcome beta-lactam resistance conferred by metallo-beta-lactamases in enterobacteriaceae? Antimicrob Agents Chemother. 2017;61(4):1–9.
Karaiskos I, Galani I, Souli M, Giamarellou H. Novel beta-lactam-beta-lactamase inhibitor combinations: expectations for the treatment of carbapenem-resistant Gram-negative pathogens. Expert Opin Drug Metab Toxicol. 2019;15(2):133–49.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hernandez, S., Velez, A.P., Lamarche, J., Greene, J.N. (2019). Bacteremia in Neutropenic Patients. In: Velez, A., Lamarche, J., Greene, J. (eds) Infections in Neutropenic Cancer Patients. Springer, Cham. https://doi.org/10.1007/978-3-030-21859-1_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-21859-1_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21858-4
Online ISBN: 978-3-030-21859-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)