Abstract
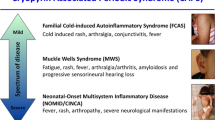
Cryopyrin-associated periodic syndrome (CAPS) is an umbrella term today used for three formerly described conditions in order of increasing severity familial cold autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS), and chronic infantile neurologic cutaneous and articular syndrome (CINCA), also known as neonatal-onset multisystem inflammatory disease (NOMID)
CAPS is an autosomal dominant disease that starts early in life
Mutations in CAPS give rise to a gain-of-function in the NLRP3 inflammasome
Somatic mosaicism should be considered in patients with clinical CAPS and no mutation detected in the NLRP3 with Sanger sequencing
CAPS is characterized by a varying degree of systemic inflammation, urticaria-like rash, musculoskeletal symptoms, and a risk of amyloidosis and neurologic sequelae
Treatment with IL-1 blockade is generally very effective in CAPS
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
A 4-year-old Caucasian girl is referred to your outpatient clinic due to rash and fever episodes, starting as she was 2 weeks old. The fever episodes have been non-regular, lasting 1–5 days and associated with moderately raised inflammatory markers, that is CRP being 6–9 mg/dL and SAA 14–27 mg/dL. Between the episodes, CRP and SAA has been in a range of 1.5–2 mg/dL and 4.5–6 mg/dL, respectively. Her blood count has been normal except for a mild anemia. The rash has been localized on the legs and arms, and on occasions the trunk has been affected.
The girl often complains of headache and has been diagnosed with a moderate bilateral sensorineural hearing impairment. The episodes are more frequent during winter. Her family history is positive as the girl’s mother has similar, but milder symptoms, not having received a proper explanation or a clear diagnosis. Both parents are of Caucasian origin. When you examine the girl on the third day of an episode, your findings include mild bilateral non-purulent conjunctivitis as well as a non-itching urticaria-like rash located on arms, legs and trunk, as described by the parents. Lymph nodes and oral cavity are normal. Heart and lungs are clear. Abdomen is soft without hepatosplenomegaly. There is no arthritis.
-
A.
Systemic-onset JIA (SoJIA)
-
B.
Cryopyrin-associated periodic syndrome (CAPS)
-
C.
TNF-receptor associated periodic syndrome (TRAPS)
-
D.
Mevalonate kinase deficiency (MKD)
-
E.
Familial Mediterranean fever (FMF)
The correct answer is B.
The most likely diagnosis is cryopyrin-associated periodic syndrome CAPS. CAPS is an autoinflammatory syndrome, inherited in an autosomal dominant pattern and usually starts early in life [1]. CAPS is an umbrella term for, the three formerly used names in order of increasing severity, familial cold autoinflammatory syndrome (FCAS) [2], Muckle-Wells syndrome (MWS) [3] and chronic infantile neurologic cutaneous and articular syndrome (CINCA) [4], the latter is also known as neonatal-onset multisystem inflammatory disease (NOMID). Diagnostic criteria for CAPS have recently been published [5]. These include elevated inflammatory markers (CRP or SAA) as a mandatory criteria and at least two of the following six CAPS typical signs/symptoms: urticaria-like rash, cold-triggered episodes, sensorineural hearing loss, musculoskeletal symptoms of arthralgia/arthritis/myalgia, chronic aseptic meningitis, and skeletal abnormalities of epiphyseal overgrowth/frontal bossing. In contrast to allergic urticaria, the skin rash in CAPS is non-pruritic and histopathology examination of biopsy material shows neutrophil infiltration instead of mast cell activation.
SoJIA is not a Mendelian inherited disease except for an ultra-rare variant. SoJIA presents later in life with longer fever episodes as stated in the clinical criteria (>2 weeks). TRAPS is an autosomal dominant disease, but the fever episodes are usually more than 1–2 weeks, longer than 1–5 days in the present case and the disease onset is usually later in life.
There is an overlap between duration of fever episodes in our patient with FMF (<3 days). Yet, the fever episodes in FMF do not exceed 3 days. FMF is not associated with urticaria-like rash, sensorineural hearing impairment, non-purulent conjunctivitis or presentation at the age of two weeks. The parents are of European origin, an ethnicity that is uncommon in FMF, i.e. FMF is most common in Arabs, Jews, Armenians and Turks.
Finally, in MKD, formerly known as HIDS, urticaria-like rash, sensorineural hearing impairment and non-purulent conjunctivitis is uncommon. In addition, the patient lack symptoms that are typical of MKD such as diarrhea and generalized lymphadenitis. The duration of episodes in MKD is usually 3–7 days. The onset of MKD is generally during the first or the second year of life, but not as early as the neonatal period except for the most severe form, mevalonate aciduria.
-
A.
NLR family pyrin domain containing 3 (NLRP3)
-
B.
TNF receptor superfamily member 1A (TNFRSF1A)
-
C.
Mevalonate kinase (MVK)
-
D.
Mediterranean Fever (MEFV)
The correct answer is A.
CAPS is caused by mutations in NLRP3 formerly known as NALP3 or CIAS1. Mutations in NLRP3 were initially described in FCAS and MWS by Hoffman et al. in 2001 [6]. Soon after that, mutations in the same gene were found to cause CINCA/NOMID [7]. For almost half of the patients with clinical features of CINCA/NOMID no mutation in the NLRP3 gene is found when investigated with Sanger sequencing. Many of these patients have somatic mosaicism, that is, they only have the disease causing mutation in a portion of their cells.
Mutations in TNFRSF1A, MVK and MEFV are responsible for TRAPS, MKD and FMF, respectively.
-
A.
TNFα
-
B.
IL-1β
-
C.
IL-6
-
D.
Interferon-γ
The correct answer is B.
The symptoms of CAPS are mainly caused by an overproduction of IL-1β. Mutation in NLRP3 cause a conformation change in cryopyrin leading to a gain-of-function in this protein. Cryopyrin forms the NLRP3 inflammasome together with procaspase 1 and ASC. This complex cleaves pro-caspase 1 to caspase 1 that in turn activates pro-IL-1β to IL-1β. IL-1β acts locally in the tissue and increased levels of IL-1β are rarely found in serum of patients with CAPS.
-
A.
Corticosteroids
-
B.
Colchicine
-
C.
IL-1 blockade
-
D.
IL-6 blockade
The correct answer is C.
As CAPS is an IL-1 driven disease, treatment with IL-1 blockade is usually very effective [8]. Three different drugs blocking IL-1β have been shown to be effective in CAPS. The short-acting IL-1 receptor antagonist anakinra was the first one to be studied and showed a remarkable potential to regress symptoms of CAPS [9]. Long-acting monoclonal IL-1 inhibitors, rilonacept and canakinumab were later found to give an equally good effect. Almost all inflammatory symptoms in CAPS respond to IL-1 blockade, except for skeletal manifestations.
Corticosteroids are effective but high doses are usually needed and side effects justify against their use as long-term treatment option in CAPS. Some patients may benefit from corticosteroids on demand in combination with continuous IL-1 blockade [8]. There is no evidence for efficacy of colchicine or IL-6 blockade.
-
1.
Aseptic meningitis
-
2.
Migraine-like headache
-
3.
Raised intracranial pressure
-
4.
Stroke
-
5.
Sensorineural hearing impairment
-
6.
Peripheral neuropathy
-
A.
1, 2, 3, 6
-
B.
1, 2, 4, 5
-
C.
1, 2, 3, 5
-
D.
2, 4, 5, 6
-
E.
1, 3, 5, 6
-
A.
The correct answer is C.
Neurological manifestations are very common in CAPS [10, 11]. Aseptic meningitis and raised intracranial pressure are usual finding from lumbar puncture and CSF analysis. Both of these findings are reversed using IL-1 blocking agents. Sensorineural hearing impairment is another common complaint. IL-1 blockade can halt progression of sensorineural hearing impairment, but might not reverse the hearing damage. Migraine-like symptoms are often described by patients with CAPS. As migraine headaches are quite common in general population, co-existence of “true” migraine could overshadow CAPS induced migraine-like headaches. Peripheral neuropathy is not associated with CAPS.
-
A.
Life-long treatment is necessary
-
B.
Treatment for at least 2 years and reevaluation for continuation of therapy
-
C.
Treatment should be continued until he is symptom-free for at least 2 years
-
D.
There is no definitive answer to this question and treatment is tailored individually
The correct answer is A.
So far, there is no definitive cure of the disease and patients require a life-long treatment to avoid symptoms and prevent secondary complications, such as amyloidosis and neurological sequelae. This is in contrast to treatment of some multifactorial autoinflammatory diseases like SoJIA, in which treatment might be stopped after stable remission.
-
Cryopyrin-associated periodic syndrome (CAPS) is an umbrella term today used for three formerly described conditions in order of increasing severity familial cold autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS), and chronic infantile neurologic cutaneous and articular syndrome (CINCA), also known as neonatal-onset multisystem inflammatory disease (NOMID)
-
CAPS is an autosomal dominant disease that starts early in life
-
Mutations in CAPS give rise to a gain-of-function in the NLRP3 inflammasome
-
Somatic mosaicism should be considered in patients with clinical CAPS and no mutation detected in the NLRP3 with Sanger sequencing
-
CAPS is characterized by a varying degree of systemic inflammation, urticaria-like rash, musculoskeletal symptoms, and a risk of amyloidosis and neurologic sequelae
-
Treatment with IL-1 blockade is generally very effective in CAPS’
References
Aksentijevich I, Putnam CD, Remmers EF, Mueller JL, Le J, Kolodner RD, Moak Z, Chuang M, Austin F, Goldbach-Mansky R, Hoffman HM, Kastner DL. The clinical continuum of cryopyrinopathies: novel CIAS1 mutations in North American patients and a new cryopyrin model. Arthritis Rheum. 2007;56(4):1273–85.
Kile RLRH. A case of cold urticaria with an unusual family history. JAMA. 1940;114:1067–8.
Muckle TW, Urticaria M. Deafness, and amyloidosis: a new heredo-familial syndrome. Q J Med. 1962;31:235–48.
Prieur AM, Griscelli C, Lampert F, Truckenbrodt H, Guggenheim MA, Lovell DJ, Pelkonnen P, Chevrant-Breton J, Ansell BM. A chronic, infantile, neurological, cutaneous and articular (CINCA) syndrome. A specific entity analysed in 30 patients. Scand J Rheumatol Suppl. 1987;66:57–68.
Kuemmerle-Deschner JB, Ozen S, Tyrrell PN, Kone-Paut I, Goldbach-Mansky R, Lachmann H, Blank N, Hoffman HM, Weissbarth-Riedel E, Hugle B, Kallinich T, Gattorno M, Gul A, Ter Haar N, Oswald M, Dedeoglu F, Cantarini L, Benseler SM. Diagnostic criteria for cryopyrin-associated periodic syndrome (CAPS). Ann Rheum Dis. 2017;76(6):942–7.
Hoffman HM, Mueller JL, Broide DH, Wanderer AA, Kolodner RD. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001;29(3):301–5.
Feldmann J, Prieur AM, Quartier P, Berquin P, Certain S, Cortis E, Teillac-Hamel D, Fischer A, de Saint Basile G. Chronic infantile neurological cutaneous and articular syndrome is caused by mutations in CIAS1, a gene highly expressed in polymorphonuclear cells and chondrocytes. Am J Hum Genet. 2002;71(1):198–203.
Ter Haar N, Lachmann H, Ozen S, Woo P, Uziel Y, Modesto C, Kone-Paut I, Cantarini L, Insalaco A, Neven B, Hofer M, Rigante D, Al-Mayouf S, Touitou I, Gallizzi R, Papadopoulou-Alataki E, Martino S, Kuemmerle-Deschner J, Obici L, Iagaru N, Simon A, Nielsen S, Martini A, Ruperto N, Gattorno M, Frenkel J. Treatment of autoinflammatory diseases: results from the Eurofever registry and a literature review. Ann Rheum Dis. 2013;72(5):678–85.
Hawkins PN, Lachmann HJ, Aganna E, McDermott MF. Spectrum of clinical features in Muckle-Wells syndrome and response to anakinra. Arthritis Rheum. 2004;50(2):607–12.
Parker T, Keddie S, Kidd D, Lane T, Maviki M, Hawkins PN, Lachmann HJ, Ginsberg L. Neurology of the cryopyrin-associated periodic fever syndrome. Eur J Neurol. 2016;23(7):1145–51.
Levy R, Gerard L, Kuemmerle-Deschner J, Lachmann HJ, Kone-Paut I, Cantarini L, Woo P, Naselli A, Bader-Meunier B, Insalaco A, Al-Mayouf SM, Ozen S, Hofer M, Frenkel J, Modesto C, Nikishina I, Schwarz T, Martino S, Meini A, Quartier P, Martini A, Ruperto N, Neven B, Gattorno M. Phenotypic and genotypic characteristics of cryopyrin-associated periodic syndrome: a series of 136 patients from the Eurofever registry. Ann Rheum Dis. 2015;74(11):2043–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Berg, S., Fasth, A., Wekell, P. (2019). Rash and Fever since Two Weeks of Age. In: Rezaei, N. (eds) Pediatric Immunology. Springer, Cham. https://doi.org/10.1007/978-3-030-21262-9_102
Download citation
DOI: https://doi.org/10.1007/978-3-030-21262-9_102
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21261-2
Online ISBN: 978-3-030-21262-9
eBook Packages: MedicineMedicine (R0)