Abstract
The cryopyrin-associated periodic syndrome (CAPS) comprises of three clinical phenotypes, the familial cold-induced autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS) and the ‘chronic infantile neurological cutaneous and articular’ syndrome (CINCA; in the USA known as ‘neonatal onset multisystem inflammatory disease’, NOMID). CAPS is a rare hereditary systemic illness which is caused by mutations of single genes encoding for proteins that are involved in innate immunity regulating inflammation, apoptosis and the production of cytokines. Such diseases can be thought of as ‘inborn errors of inflammation’. In case of CAPS, NLRP3, which is located on chromosome 1q44, has been identified as the responsible gene. NLRP3 encodes for the protein cryopyrin which is mutated in CAPS. In nearly 50 % of the CAPS patients, however, no NLRP3 mutations can be detected, so that the presence of additional genetic factors that initiate and modulate the cryopyrinopathies has been discussed. In some cases with typical clinical features of CAPS but without identifiable NLRP3, germ line mutations and somatic mutations have been discovered.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Core Messages-
The cryopyrin-associated periodic syndromes (CAPS) represent a rare group of autosomal dominant inherited autoinflammatory, systemic diseases.
-
CAPS comprises of three entities, the familial cold-induced autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS) and the ‘chronic infantile neurological cutaneous and articular’ syndrome (CINCA; in the USA known as ‘neonatal onset multisystem inflammatory disease’, NOMID).
-
Overlap syndromes are known.
-
In MWS and CINCA/NOMID, uveitis can be observed.
1 Definition
The cryopyrin-associated periodic syndrome (CAPS) comprises of three clinical phenotypes, the familial cold-induced autoinflammatory syndrome (FCAS), Muckle-Wells syndrome (MWS) and the ‘chronic infantile neurological cutaneous and articular’ syndrome (CINCA; in the USA known as ‘neonatal onset multisystem inflammatory disease’, NOMID). CAPS is a rare hereditary systemic illness which is caused by mutations of single genes encoding for proteins that are involved in innate immunity regulating inflammation, apoptosis and the production of cytokines. Such diseases can be thought of as ‘inborn errors of inflammation’ [12]. In case of CAPS, NLRP3, which is located on chromosome 1q44, has been identified as the responsible gene. NLRP3 encodes for the protein cryopyrin which is mutated in CAPS. In nearly 50 % of the CAPS patients, however, no NLRP3 mutations can be detected, so that the presence of additional genetic factors that initiate and modulate the cryopyrinopathies has been discussed [1]. In some cases with typical features of CAPS but without identifiable NLRP3 germ line mutations somatic mutations have been discovered [20, 23].
2 Clinical Manifestations
2.1 General Disease
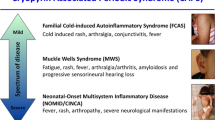
FCAS, MWS and CINCA have been classified as distinct entities of a continuous clinical spectrum, FCAS being the mildest and CINCA being the most severe disease, whereas MWS represents an intermediate form [10]. An overlap between FCAS, MWS and CINCA may occur.
Clinically, FCAS is characterised by 12–72 h lasting episodes of fever (93 %), urticarial rash (100 % cold induced), arthralgias (96 %) and conjunctivitis (84 %) (Table 78.1) [12]. The episodes are precipitated by general cold exposure. In 95 % of the cases, FCAS manifests before the age of 6 months.
MWS is characterised by the triad urticarial rash, progressive sensorineural hearing loss and amyloid A (AA) amyloidosis (Table 78.1). Additional features are arthralgias/arthritis (knee, ankle), fever (12–48 h), lymphadenopathy and oral and/or genital aphthosis [12].
CINCA/NOMID syndrome is characterised by the nearly continuous appearance of inflammatory clinical symptoms and signs beginning as early as at the neonatal period or at early infancy, with a migratory and nonpruritic urticaria-like rash and fever (Table 78.1) [8, 22]. Later, patients develop symptoms of central nervous system (CNS) inflammation, including chronic aseptic meningitis, increased intracranial pressure, cerebral atrophy, seizures and sometimes mental retardation. Approximately 80 % of patients develop progressive sensorineural hearing loss. Characteristic is the huge overgrowth of the patella. Nearly 20 % of the patients die before reaching adulthood [22].
2.2 Ocular Disease
Ocular involvement is common in autoinflammatory disorders. Depending on the clinical phenotype, various ocular structures can be affected. Conjunctivitis, keratitis, episcleritis, anterior or posterior uveitis, optic disc edema and even optic nerve atrophy can be observed in CAPS patients.
Conjunctivitis has been described in more than 80 % of patients during acute episodes of FCAS [11].
Conjunctivitis also represents the most common ocular symptom of MWS (Fig. 78.1). In a family with 16 members suffering from MWS, described by Haas et al., 13 showed conjunctivitis [9]. Conjunctivitis in MWS has been described as a relapsing, spontaneously occurring redness of the conjunctiva that persists for a few days before it spontaneously disappears without any change or increase of therapy or additional use of eye drops. In contrast, other ocular manifestations including keratitis, episcleritis and anterior or posterior uveitis have been described as rare manifestations of MWS. In 2011, however, Zierhut et al. presented a study on 37 family members of which 29 presented an overlapping clinical phenotype of FCAS and MWS. Fifteen (52 %) of the symptomatic family members carried the A439V mutation of the NLRP3 gene. Of the mutation-positive patients, 73 % suffered from conjunctivitis and 67 % from bilateral anterior uveitis. In the mutation-negative cohort, 43 % presented with conjunctivitis and only 7 % with anterior uveitis [25]. Another report presented a 70-year-old female who suffered from an acute unilateral vision loss with photopsias during a relapse of MWS. Clinically, a pale and swollen optic disc could be seen. Functional diagnostic revealed extinct visual evoked potentials and a concentric visual field constriction. Diagnosis of anterior ischemic optic neuropathy (AION) was suspected. Whereas treatment with high-dose corticosteroids and plasmapheresis did not show any effect, some restitution of vision could be seen within 10 days following a single application of 100 mg anakinra [2].
CINCA represents the most severe disease within CAPS which is also true for ocular involvement. Eye disease normally occurs at an average age of 4.5 years, may affect all eye segments and is vision threatening. Symptoms of the anterior eye segment can include dry eye as well as a chronic conjunctivitis or perilimbal redness, respectively. In approximately 40 % of patients, corneal affection can be observed, impressing as interstitial keratitis with stromal opacification, band keratopathy or corneal neovascularisations (Fig. 78.2). Approximately 50 % of CINCA patients develop a mild to moderate, non-granulomatous anterior uveitis that, in contrast to JIA-associated uveitis, does not show complications like posterior synechiae, cataract or secondary glaucoma. Inflammatory involvement of the posterior eye segment, presenting as vitritis, retinal vasculitis or focal chorioretinitis, is a rare event. However, changes of the optic disc affect more than 80 % of patients and thus represent the most common eye manifestation in CINCA. They are bilateral and mostly associated with chronic meningitis [8]. Optic disc edema as well as a moderate to severe atrophy of the optic nerve can occur. Moderate to severe visual impairment has been described in approximately 25 % of CINCA patients, especially in case of corneal or optic disc changes [5].
3 Etiology and Pathophysiology
As of February 2015, 175 disease-associated mutations of the NLRP3 gene have been identified (http://fmf.igh.cnrs.fr/ISSAID/infevers/search.php?n=4). The NLRP3 gene is mainly expressed in polymorphonuclear leucocytes and chondrocytes. The gene product cryopyrin is part of the caspase 1 inflammasome, a cytosolic multiprotein complex that activates caspase 1 to process the proinflammatory cytokines interleukin 1ß (IL-1ß) and IL-18. IL-1ß and IL-18 are important for the regulation of intracellular host defense in response to so-called PAMPs (Pathogen-associated molecular pattern) like bacterial toxins, RNA or small antiviral compounds like R837 and R848 and to DAMPs (Danger-associated molecular pattern) like ATP, cholesterol, amyloid beta or uric acid crystals [1, 4, 6, 7, 19] (see also Chap. 2). Mutational changes of the cryopyrin structure can lead to an auto-activation of the inflammasome even in the absence of stimuli such as bacterial toxins, thus causing an excessive production of IL-1ß and subsequently leading to a massive increase of such acute phase reactants as CRP and serum amyloid A [1]. The severity of the phenotype of individual patients with CAPS seems to be influenced by additional other genetic as well as environmental modifiers [1].
4 Diagnosis
The diagnosis of CAPS is based on the history and symptoms of the patients as well as on the clinical features (Table 78.1) together with the molecular genetic finding of a mutation of the NLRP3 gene. However, in nearly 50 % of cases, such a mutation is lacking. Then the diagnosis can be established by the characteristic clinical features together with a prompt response to treatment with an IL-1ß blocking agent.
5 Differential Diagnosis
From an ophthalmological point of view, differential diagnoses of MWS include other entities of anterior uveitis in childhood. In particular, JIA-associated uveitis, TINU syndrome, sarcoidosis-associated uveitis but also infectious forms like uveitis due to Lyme disease have to be considered. Among the autoinflammatory disorders, Blau syndrome is an important differential diagnosis for anterior uveitis.
6 Therapy
As a consequence of the pathophysiology of CAPS with excessive increases of IL-1ß, blockade of this pro-inflammatory cytokine is the treatment of choice. Until recently, only the IL-1 receptor antagonist anakinra (Kineret®) had been very successfully used in FCAS, MWS and CINCA [3, 8, 10, 15, 17, 18, 21]. If this treatment is stopped, the clinical symptoms immediately recur, but reinstitution of anakinra is again followed by a prompt positive therapeutic response [8]. Under treatment with anakinra, vision of CINCA patients remained stable during the 6-month observation period.
Since 2009, canakinumab (Ilaris®), a fully human anti-IL-1ß monoclonal antibody, has been officially approved for the treatment of CAPS in adults and children from the age of 4 years. In a phase II open-label study, canakinumab at a dose of 2 mg/kg or 150 mg subcutaneously induced rapid and sustained clinical and biochemical responses in seven paediatric patients with CAPS [14]. In an open-label, multicentre, phase III study, 166 adult and paediatric CAPS patients (canakinumab-naïve and pretreated patients from previous studies) have been treated with canakinumab subcutaneously 150 mg or 2 mg/kg (≤40 kg) every 8 weeks for up to 2 years. Complete response was achieved in 78 % of canakinumab-naïve patients within 8–21 days. In 90 % of patients, no relapses occurred and CRP/serum amyloid A levels normalised. Treatment with canakinumab was well tolerated. Predominant adverse events were mild to moderate infections in 66 % of patients [13]. Moreover, canakinumab led to a sustained control of disease activity in MWS even after secondary failure of therapy with anakinra [16]. The results of a recent retrospective analysis demonstrate that canakinumab is a very effective treatment also for conjunctivitis and anterior uveitis associated with MWS [26]. In the U.S.A. with rilonacept (IL-1 trap) an additional treatment option is available (approved for CAPS in February 2008). It is given by weekly subcutaneous injections. In two double-blind, placebo-controlled trials of 6 and 18 weeks duration (41 patients with FCAS, 3 patients with MWS) the patients experienced significant reduction in symptom scores compared with placebo [27, 28].
7 Prognosis
As well as in FCAS and MWS, inflammatory eye manifestations in CINCA show response to IL-1 blockade. However, visual loss caused by optic nerve atrophy, resulting from chronic optic disc swelling, remains irreversible despite IL-1 blockade.
Take-Home Pearls
-
CAPS should not be mistaken for rheumatic diseases, even if patients may exhibit such ‘rheumatic’ features as arthritis, uveitis and AA amyloidosis.
-
Additional clinical features are urticarial rash, fever, progressive sensorineural hearing loss and in case of CINCA CNS involvement.
-
The diagnosis of CAPS is based on the clinical features together with the molecular genetic finding of a NLRP3 mutation.
-
The diagnosis should be made as early as possible, since the life-threatening AA amyloidosis may be prevented by treatment.
-
In nearly 50 % of the cases a NLRP3, mutation is lacking. Then the diagnosis can be made by the characteristic clinical features together with a convincing, prompt and persisting response to the treatment with an IL-1ß-blocking agent after the exclusion of other disorders like juvenile idiopathic arthritis.
References
Aksentijevich I, Putnam D, Remmers EF et al (2007) The clinical continuum of cryopyrinopathies: novel CIAS1 mutations in North American patients and a new cryopyrin model. Arthritis Rheum 56:1273–1285
Alexander T, Klotz O, Feist E et al (2005) Successful treatment of acute visual loss in Muckle-Wells syndrome with interleukin 1 receptor antagonist. Ann Rheum Dis 64:1245–1246
Dalgic B, Egritas O, Sari S, Cuisset L (2007) A variant Muckle-Wells syndrome with a novel mutation in CIAS1 gene responding to anakinra. Pediatr Nephrol 22:1391–1394
Dinarello CA (2007) Mutations in cryopyrin: bypassing roadblocks in the caspase 1 inflammasome for interleukin-1beta secretion and disease activity. Arthritis Rheum 56:2817–2822
Dollfus H, Hafner R, Hofmann HM et al (2000) Chronic infantile neurological cutaneous and articular/neonatal onset multisystem inflammatory disease syndrome: ocular manifestations in a recently recognized chronic inflammatory disease of childhood. Arch Ophthalmol 118:1386–1392
Drenth JP, van der Meer JW (2006) The inflammasome–a linebacker of innate defense. N Engl J Med 355:730–732
Gattorno M, Tassi S, Carta S et al (2007) Pattern of interleukin-1beta secretion in response to lipopolysaccharide and ATP before and after interleukin-1 blockade in patients with CIAS1 mutations. Arthritis Rheum 56:3138–3148
Goldbach-Mansky R, Dailey NJ, Canna SW et al (2006) Neonatal-onset multisystem inflammatory disease responsive to interleukin-1beta inhibition. N Engl J Med 355:581–592
Haas N, Kuster W, Zuberbier T, Henz BM (2004) Muckle-Wells syndrome: clinical and histological skin findings compatible with cold air urticaria in a large kindred. Br J Dermatol 151:99–104
Hawkins PN, Lachmann HJ, Aganna E, McDermott MF (2004) Spectrum of clinical features in Muckle-Wells syndrome and response to anakinra. Arthritis Rheum 50:607–612
Hoffmann HM, Wanderer AA, Broide DH (2001) Familial cold autoinflammatory syndrome: phenotype and genotype of an autosomal dominant periodic fever. J Allergy Clin Immunol 108:615–620
Kastner DL (2003) The hereditary periodic fevers. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH (eds) Rheumatology. Mosby, Edinburgh, pp 1717–1734
Kümmerle-Deschner JB, Hachulla E, Cartwright R et al (2011) Two-year results from an open-label, multicenter, phase III study evaluating the safety and efficacy of canakinumab in patients with cryopyrin-associated periodic syndrome across different severity phenotypes. Ann Rheum Dis 70:2095–2102
Kümmerle-Deschner JB, Ramos E, Blank N et al (2011) Canakinumab (ACZ885, a fully human IgG1 anti-IL-1ß mAb) induces sustained remission in pediatric patients with cryopyrin-associated periodic syndrome (CAPS). Arthritis Res Ther 13:R34
Kümmerle-Deschner JB, Tyrrell PN, Kötter I et al (2011) Efficacy and safety of anakinra therapy in pediatric and adult patients with the autoinflammatory Muckle-Wells syndrome. Arthritis Rheum 63:840–849
Kümmerle-Deschner JB, Wittkowski H, Tyrrell PN et al (2013) Treatment of Muckle-Wells syndrome: analysis of two IL-1-blocking regimens. Arthritis Res Ther 15:R64
Lequerré T, Vittecoq O, Saugier-Veber P et al (2007) A cryopyrin-associated periodic syndrome with joint destruction. Rheumatology (Oxford) 46:709–714
Lovell DJ, Bowyer SL, Solinger AM (2005) Interleukin-1 blockade by anakinra improves clinical symptoms in patients with neonatal-onset multisystem inflammatory disease. Arthritis Rheum 52:1283–1286
Mariathasan S, Weiss DS, Newton K et al (2006) Cryopyrin activates the inflammasome in response to toxins and ATP. Nature 440:228–232
Michels H, Häfner R, Kettner HO et al (2006) Inefficacy of etanercept but successful treatment with anakinra in a 19-year-old TRAPS patient with a TNFRSF1A R92Q germ line defect and a somatic CIAS1 A352S mutation. Arthritis Rheum 54:S638, Abstract 1579
O’Connell SM, O’Regan GM, Bolger T et al (2007) Response to IL-1-receptor antagonist in a child with familial cold autoinflammatory syndrome. Pediatr Dermatol 24:85–89
Prieur AM, Griscelli C, Lampert F et al (1987) A chronic, infantile, neurological, cutaneous and articular (CINCA) syndrome. A specific entity analysed in 30 patients. Scand J Rheumatol 66:57–68
Saito M, Fujisawa A, Nishikomori R et al (2005) Somatic mosaicism of CIAS1 in a patient with chronic infantile neurologic, cutaneous, articular syndrome. Arthritis Rheum 52:3579–3585
Shakeel A, Gouws P (2007) Muckle-Wells syndrome: another cause of acute anterior uveitis. Eye 21:849–850
Zierhut M, Kümmerle-Deschner JB, Lohse P, et al (2011) CAP-syndrome: genetic and clinical investigation in a family of five generations considering particularly uveitis. ARVO abstract no. 6562
Zierhut M, Sobolewska B, Deuter C, Doycheva D, Kümmerle-Deschner J (2013) CAP-syndrome. Response to treatment with canakinumab. ARVO abstract no. 359
Goldbach-Mansky R, Shroff SD, Wilson M et al (2008) A pilot study to evaluate the safety and efficacy of the long-acting interleukin-1 inhibitor rilonacept (interleukin-1 Trap) in patients with familial cold autoinflammatory syndrome. Arthritis Rheum 58:2432–2442
Hoffman HM, Throne ML, Amar NJ et al (2008) Efficacy and safety of rilonacept (interleukin-1 Trap) in patients with cryopyrin-associated periodic syndromes: results from two sequential placebo-controlled studies. Arthritis Rheum 58:2443–52
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Michels, H., Deuter, C., Kümmerle-Deschner, J. (2016). The Cryopyrin-Associated Periodic Syndrome (CAPS). In: Zierhut, M., Pavesio, C., Ohno, S., Orefice, F., Rao, N. (eds) Intraocular Inflammation. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-75387-2_78
Download citation
DOI: https://doi.org/10.1007/978-3-540-75387-2_78
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-75385-8
Online ISBN: 978-3-540-75387-2
eBook Packages: MedicineMedicine (R0)