Abstract
The success of fat grafting depends on many factors which can affect the viability of the cell. There are so many variables along the procedure that research has tried to establish the best and safest procedure to ensure the best result. The first step is harvesting. Elements such as the diameter of the cannula, the aspirative pressure, the use of local anesthesia, or tumescence have been studied. Even though the variability of the methods used and the difficulty to follow a universal and standardized method, it seems that it would be better to use larger cannulas for harvesting and eliminate local anesthesia from the graft by washing. There is no difference between donor sites, and the results are the same by using handheld syringes or liposuctors, provided the negative pressure exerted is low.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The first known historical reference for the transfer of adipose tissue corresponds to Neuber, which transplants fragments of 1 cm adipose tissue, from the forearm to the face. Lexer in 1910 used fat for facial and malar atrophy and increased malar, and Bruning in 1919 reported the first fat injection through a needle in 1919 [1]. Peer in 1950 refers to a 40–50% retention of transplanted fat per year [2]. The introduction of liposuction increased interest in lipotransfer [3, 4].
In 1987, Bircoll [5] introduced the use of adipose tissue as a breast enhancement material, but it raged with criticism as bad experiences and complications from steatonecrosis accumulated. That is why a panel of experts from the American Society for Plastic and Reconstructive Surgery issues a statement advising against its practice. Coleman is responsible for the standardization of an atraumatic procedure that allows to obtain good and reproducible results with the adipose tissue grafts and denominated Lipoestructura ™ [6]. Basically it consists of an atraumatic fat collection (with 3 mm blunt cannulas and 10 mm syringes), centrifugation at 1286 g (3000 rpm with the Coleman centrifuge) for 3 min to separate the adipose cells from the blood components and cells Broken, and transferred to the tissue by blunt cannulas of about 2–3 mm in multiple passes, using 1 cc in each pass. The importance of micrografting has already been pointed out by Bircoll and Coleman as the most important part of the procedure. In 1993 Carpaneda and Ribeiro compared the viability of various fat cylinders and found that survival is greater in those with less than 3 mm in diameter. The central part of the grafts of more than 3.5 mm was necrosed [7]. This observation has been confirmed more recently by the works of Eto et al. [8] which showed that the adipocytes of a graft begin to die on day one and that only a few adipocytes within 300 μm of the edge of the tissue survive.
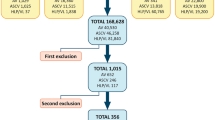
Despite the pioneering effort of Coleman and the enormous advance that his standardization of the method supposed for fat grafting, one of the major criticisms and drawbacks of lipofilling is the variable retention range reported, between 20 and 80% at 1 year [9, 10]. This unpredictability has led to the search of the best method of harvesting which would ensure the best cellular viability and retention. Research has focused on the three phases of preparing the fat: harvesting, processing, and injection. However, there is insufficient scientific evidence to permit the standardization of procedures. Since 2011, there are only five clinical trials and 32 prospective comparative studies [11].
Regarding harvesting, retention could depend on the size of the fat particles. Liposuction disaggregates the fat in particles of different sizes, depending on the cannula diameter. As we have read above, fat diameter is a paramount issue for survival. Eto et al. [8] in their landmark study showed that adipocytes closer to the surface of the particle were more likely to survive. They established that in the outer surviving layer (100–300 μ) all adipocytes and stem cells survive; in the middle layer (600–1200 μ), the adipocytes die but they are replaced by proliferating stem cells; and in the core of the particle, all cells die (Fig. 1).
The aim of this chapter is to review the latest data available regarding harvesting techniques for fat grafting.
Mechanical Damage
The main disadvantage of excising en bloc fat for grafting is the size of the scars. Therefore one of the main goals is to demonstrate that liposuctioned fat conserves the features of the whole fat while being less invasive in its harvesting. Moore et al. [12] showed that cells isolated from intraoperative liposuction and lipectomy samples did not differ functionally, responded similarly to insulin stimulation of glucose transport and epinephrine-stimulated lipolysis, and retained the same growth pattern in culture. Lalikos [13] did not see any difference in architecture comparing liposuctioned and whole fat. In another work, Pu et al. [14] showed no difference in the cellular architecture between the liposuctioned and the en bloc fat, although the liposuctioned cells showed less enzymatic activity of glycerol-3-phosphate dehydrogenase, a marker of cellular metabolism. For the Yoshimura group, however, the aspirated tissue is poorer in ASC and adipocytes, and therefore they defend the need to enrich the aspirate with stem cells (what they call CAL or cell-assisted lipotransfer) [15].
What Is the Best Donor Site?
There is no uniformity of opinions or results regarding the different work performed. For some the abdomen, especially the lower part of it, is the richest in stem cells (it must be borne in mind that it is assumed that the higher the concentration of ASCs, the greater the survival of the graft). For Fraser [16] the best donor site is the hip, and for Rohrich et al. [17] and Li et al. [18], there is no difference between donor sites (level of evidence 1). Another work by Small et al. in breast reconstruction concluded as well that there was no difference in longevity between fat harvested from the abdomen or from the thigh [19].
The main conclusion is that the current literature suggests that there is no significant difference between different donor sources regarding cell viability or volume retention. On the other hand, if we consider the layers of the adipose tissue, there could be a difference. Di Taranto et al. [20] reported that the superficial adipose tissue has a higher stromal compound and higher CD105+ cells comparing to the deep tissue, which would make it a better donor tissue for fat survival.
Effect of Local Anesthesia
Local anesthesia (lidocaine) appears to adversely affect the metabolism of adipocytes, with reduced glucose transport and lipolysis, and viability and differentiation of preadipocytes (ASC) [20]. Articaine/epinephrine and 2% lidocaine are especially harmful. The time between infiltration and aspiration may be relevant in terms of the longer contact between cells and anesthetic [21]. It must be taken into account in any case that these works are done in vitro and does not take into account the actual concentration of the anesthetic in the fluid that infiltrates. They consider in their work as 30 min of exposure, and it is possible that many surgeons wait much less time to obtain the fat once the infiltration is done. Lidocaine potently inhibited glucose transport and lipolysis in adipocytes and their growth in culture [14]. That effect, however, persisted only as long as lidocaine was present; after washing, the cells were able to fully regain their function and growth regardless of whether the exposure was as short as 30 min or as long as 10 days. In fact, it seems that the inhibitory effects of lidocaine disappear when the anesthetic is removed [14].
Epinephrine at different concentrations has not deleterious effect on the number of living cells in a 100× field [22].
Finally, tumescence makes no difference regarding cell viability comparing to the dry technique [23].
Suction Pressure
There is no conclusive data to ensure that syringe harvesting is better than with liposuction. The syringe gets a pressure of 660 mmHG (0.86 at). The percentage of cells in the stromal fraction is greater when using aspiration at 350 mmHg than 700 mmHg and higher in both cases than the syringe. Obtaining a 10 cc syringe and after aspirating 2 cc of air (which is what Coleman recommended) results in a negative pressure of 0.37 at. The 50 cc syringe arrives at a vacuum pressure of 0.76 atm [12]. Ould-Ali shows that with lower vacuum pressure for harvesting, greater adipose tissue survival and less fibrosis [24]. Therefore either the 10 cc syringe is used with the plunger removed 2 cc or a liposuction device at 0.5 at.
Cheriyan et al. [25] compared high pressure (−760 mmHg) versus low pressure (−250 mmHg) for cell viability using trypan blue vital stain technique after digestion with collagenase, and they observed that aspirate collected under low pressure appeared to have a compact, homogenous fat layer without any obvious oil layer, indicative of less rupture of fat cells during low-pressure aspiration. Furthermore, the average number of adipocytes after harvest was 47 percent higher in the low-pressure simple.
Cucchiani and Corrales [26] compared fat aspirated through straight cannulae (15 cm long, 3-holed, 3 mm hole diameter) under low vacuum (220 mm Hg) or high vacuum (720 mm Hg) with a Luer-Lock Terumo™10-mL syringe with plunger set at 2 mL or with a 60-mL Luer-Lock Terumo™ syringe with plunger set at 60 mL, respectively. Vacuum pressures were determined at these plunger positions by means of a vacuometer. The adipocyte viability was studied with a MTT assay. They observed that viability is reduced with higher vacuum pressures, even though the cells are quite resistant to both positive and negative pressures.
Chen et al. [27] compared the results of two different suction pressures on the cell yield of the stromal vascular fraction and the functionality of adipose derived stem cells of the SVF. The adipose tissue was obtained from the abdomen of ten patients at −30 ± 5 or −55 ± 5 kPa (101,32 kPa = 1 at). The cell yield for the lower pressure was twofold higher than with the higher pressure as well as faster cell growth and secretion of basic fibroblast growth factor and vascular endothelial growth factor.
Charles-de-Sá et al. [28], however, comparing samples obtained with different syringes (10 mL, 20 mL, and 60 mL) and different pressures (350 mmHg and 700 mmHg) with 2-hole blunt cannulas measuring 3 mm in diameter, found no significant changes in adipocyte cell count, percentage of endothelial progenitors, viable cells, and rate of late or recent apoptosis. They concluded that the amount of negative pressure used for harvesting adipose tissue by syringes of 10 mL, 20 mL, and 60 mL and by −350 mmHg and − 700 mmHg pressure does not affect the integrity and viability of adipocytes and AMSCs.
The Cannula
Coleman has designed a series of cannulas aimed at obtaining atraumatic fat and its safe infiltration (reducing the possibility of intravascular injection). Özsoy et al. [29] compared 4, 3, and 2 mm cannulas and found higher cell viability in samples harvested with 4 mm cannula. A similar result was reported by Erdim et al. [30] who found a greater viability with large cannulas (6 mm) comparing to 4 and 2 mm liposuction cannulas, and also they did not find any difference in infiltration between cannulas of 14, 16, and 20 G (gauge). Kirkham et al. [31] harvested adipose tissue from the abdomen with 5 mm and 3 mm cannulas with negative pressure (25 mmHG) and grafted the samples in nude mice. The analysis of the graft after 6 weeks showed better results for the group obtained with the 5 mm cannula.
However there are some evidences that harvesting with microcannula (2 mm multiperforated) could be better for tissue regeneration and micrografting. Trivisonno et al. [32] observed higher number of stromal and vascular cells in samples obtained with 2 mm cannula with five round ports along the sides of its distal shaft than with 3 mm and single suction port on the side of its distal end. And Alharbi et al. [33] observed better viability and migration of isolated cells in collagen elastin matrices in the microcannula samples (2 mm multiperforated).
Liposuction techniques have evolved in the last years, and new techniques have been described for removal of unwanted adipose tissue. The physics of these devices rely on their ability to detach the adipocytes from the tissue. Therefore these devices have been tested to know if they are suitable for harvesting fat for grafting. The most popular are ultrasound-assisted liposuction (UAL), power-assisted liposuction (PAL), and water-assisted liposuction (WAL).
Several studies have been done for UAL , showing no difference in cellular damage between conventional (suction-assisted) liposuction and UAL by studying the cellular damage with glycerol-3-phosphate dehydrogenase enzyme assay [12, 34, 35]. Other studies have not shown any difference for fat outcomes comparing handheld syringes, conventional liposuction, and UAL [36,37,38,39].
Using power-assisted liposuction is as well safe for harvesting fat with no difference with manual aspiration [37]. Barzelay et al. [40] studied the difference between samples obtained by resection (en bloc) and power-assisted liposuction (PAL). They did not find any difference between samples regarding the number of nucleated cells and their viability.
Something similar happens with water-assisted liposuction [41]. Meyer et al. [42] reported a good yield of adipose stem cells by using WAL , comparable to other methods of harvesting.
Finally, a recent technology using 1470 nm radial laser that disrupts the collagen seems to avoid cell damage, with a viability of adipocytes of 95.7% [43].
Conclusions
Even though considering the heterogeneity of the published works, the conclusions that can be drawn from the literature are:
-
Donor site is not an important factor.
-
The presence of lidocaine is deleterious for the cell, so the fat should be washed.
-
Aspiration pressure should be around 0.5 at.
-
The diameter of the cannula does not seem an important issue although bigger cannulas are linked to better cell viability.
-
The technology for harvesting has not influence (WAL, PAL, UAL).
References
Butterwick KJ. Autologous fat transfer: evolving concepts and techniques. Surg Skin Proc Dermatol. 2014:464.
Peer LA. Loss of weight and volume in human fat grafts. Plast Reconstr Surg. 1950;5:217–30.
Illouz YG. The fat cell graft: a new technique to fill depressions. Plast Reconstr Surg. 1986;78:122–3.
Fournier PF. Facial recontouring with fat grafting. Dermatol Clin. 1990;8:523–37.
Bircoll M. Cosmetic breast augmentation utilizing autologous fat and liposuction techniques. Plast Reconstr Surg. 1987;79:267–71.
Coleman SR. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001;28:111–9.
Carpaneda CA, Ribeiro MT. Study of the histologic alterations and viability of the adipose graft in humans. Aesth Plast Surg. 1993;17:43–7.
Eto H, Kato H, Suga H, et al. The fate of adipocytes after nonvascularized fat grafting: evidence of early death and replacement of adipocytes. Plast Reconstr Surg. 2012;129:1081–92.
Niechajev I, Sevcuk O. Long term results of fat transplantation: clinical and histologic results. Plast Reconstr Surg. 1994;94:496–506.
Gallego S, Ramirez F, Echeverri A. Magnetic resonance imaging assessment of gluteal fat grafts. Aesth Plast Surg. 2006;30:460–8.
Gir P, et al. Fat grafting: evidence-based review on autologous fat harvesting, processing, reinjection, and storage. Plast Reconstr Surg. 2012;130:249–58.
Moore JH, Kolaczynski JW, Morales LM, et al. Viability of fat obtained by syringe suction lipectomy: effects of local anesthesia with lidocaine. Aesth Plast Surg. 1995;19:335–9.
Lalikos JF, Li YQ, Roth TP, Doyle JW, Matory WE, Lawrence WT. Biochemical assessment of cellular damage after adipocyte harvest. J Surg Res. 1997;70:95–100.
Pu LL, Cui X, Fink BF, Cibull ML, Gao D. The viability of fatty tissues within adipose aspirates after conventional liposuction: a comprehensive study. Ann Plast Surg. 2005;54:288–92.
Eto H, Suga H, Matsumoto D, et al. Characterization of structure and cellular components of aspirated and excised adipose tissue. Plast Reconstr Surg. 2009;124:1087–97.
Fraser JK, Wulur I, Alfonso Z, Zhu M, Wheeler ES. Differences in stem and progenitor cell yield in different subcutaneous adipose tissue depots. Cytotherapy. 2007;9:459–67.
Rohrich RJ, Sorokin ES, Brown SA. In search of improved fat transfer viability: a quantitative analysis of the role of centrifugation and harvest site. Plast Reconstr Surg. 2004;113:391–539.
Li K, et al. Selection of donor site for fat grafting and cell isolation. Aesth Plast Surg. 2013;37:153–8.
Small K, Choi M, Petruolo O, Lee C, Karp N. Is there and ideal donor site of fat for breast reconstruction? Aesth. Surg. J. 2014;34:545–50.
Di Taranto G, Cicione C, Visconti G, et al. Qualitative and quantitative differences of adipose-derived stromal cells from superficial and deep subcutaneous lipoaspirates: a matter of fat. Cytotherapy. 2015;17(8):1076–89.
Maike K, Maximilian Z, Karina G, et al. Local anesthetics have a major impact on viability of preadipocytes and their differentiation into adipocytes. Plast Reconstr Surg. 2010;126:1500–5.
Kim IH, Yang JD, Lee DG, Chung HY, Cho BC. Evaluation of centrifugation technique and effect of epinephrine on fat cell viability in autologous fat injection. Aesth Surg J. 2009;29:35–9.
Agostini T, Lazzeri D, Pini A, et al. Wet and dry techniques for structural fat graft harvesting: histomorphometric and cell viability assessments of lipoaspirated samples. Plast Reconstr Surg. 2012;130:331e–9e.
Ould-Ali D. Mechanical factors influencing fat cell transplants quality. Dallas: IFATS; 2010.
Cheriyan T, Kao HK, Qiao X, Guo L. Low harvest pressure enhances autologous fat graft viability. Plast Reconstr Surg. 2014;133:1365–8.
Cucchiani R, Corrales L. The effects of fat harvesting and preparation, air exposure, obesity, and stem cell enrichment on adipocyte viability prior to graft transplantation. Aesth Surg J. 2016;36:1164–73.
Chen YW, Wang JR, Liao X, et al. Effect of suction pressures on cell yield and functionality of the adipose-derived stromal vascular fraction. J Plast Reconstr Surg. 2017;70(2):257–66.
Charles-de-Sá L, de Amorim NFG, Dantas D, et al. Influence of negative pressure on the viability of adipocytes and mesenchymal stem cell, considering the device method used to harvest fat tissue. Aesth Surg J. 2015;35:334–44.
Özsoy Z, Kul Z, Bilir A. The role of cannula diameter in improved adipocyte viability: a quantitative analysis. Aesth Surg J. 2006;26(3):287–9.
Erdim M, Tezel E, Numanoglu A, Sav A. The effects of the size of liposuction cannula on adipocyte survival and the optimum temperature for fat graft storage: an experimental study. J Plast Reconstr Aesthet Surg. 2009;62:1210–4.
Kirkham JC, Lee JH, Medina MA III, McCormack MC, Randolph MA, Austen WG Jr. The impact of liposuction cannula size on adipocyte viability. Ann Plast Surg. 2012;69:479–81.
Trivisonno A, Di Rocco G, Cannistra C, et al. Harvest of superficial layers of fat with a microcannula and isolation of adipose tissue–derived stromal and vascular cells. Aesth Surg J. 2014;34:601–13.
Alharbi Z, Opländer C, Almakadi S, Fritz A, Vogt M, Pallua N. Conventional vs. micro-fat harvesting: how fat harvesting technique affects tissue-engineering approaches using adipose tissue-derived stem/stromal cells. J Plast Reconstr Aesthet Surg. 2013;66:1271–8.
Rohrich RJ, Morales DE, Krueger JE, et al. Comparative lipoplasty analysis of in vivo-treated adipose tissue. Plast Reconstr Surg. 2000;105:2152–8.
Schafer ME, Hicok KC, Mills DC, Cohen SR, Chao JJ. Acute adipocyte viability after third-generation ultrasound-assisted liposuction. Aesthet Surg J. 2013;33:698–704.
Smith P, Adams WP Jr, Lipschitz AH, et al. Autologous human fat grafting: effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg. 2006;117:1836.
Keck M, Kober J, Riedl O, et al. Power assisted liposuction to obtain adipose-derived stem cells: impact on viability and differentiation to adipocytes in comparison to manual aspiration. J Plast Reconstr Aesthet Surg. 2014;67:e1–8.
Lee JH, Kirkham JC, McCormack MC, Nicholls AM, Randolph MA, Austen WG. The effect of pressure and shear on autologous fat grafting. Plast Reconstr Surg. 2013;131:1125–36.
Fisher C, Grahovac TL, Schafer ME, Shippert RD, Marra KG, Rubin JP. Comparison of harvest and processing techniques for fat grafting and adipose stem cell isolation. Plast Reconstr Surg. 2013;132:351–61.
Barzelay A, Levy R, Kohn E, et al. Power-assisted liposuction versus tissue resection for the isolation of adipose tissue–derived mesenchymal stem cells: phenotype, senescence, and multipotency at advanced passages. Aesth Surg J. 2015;35:NP230–40.
Yin S, Luan J, Fu S, Wang Q, Zhuang Q. Does water-jet force make a difference in fat grafting? In vitro and in vivo evidence of improved lipoaspirate viability and fat graft survival. Plast Reconstr Surg. 2015;135:127–38.
Meyer J, Salamon A, Herzmann N, et al. Isolation and differentiation potential of human mesenchymal stem cells from adipose tissue harvested by water jet-assisted liposuction. Aesth Surg J. 2015;35:1030–9.
Levenberg A, Scheinowitz M, Sharabani-Yosef O. Higher cell viability and enhanced sample quality following laser-assisted liposuction versus mechanical liposuction. JCDSA. 2015;5(03):238.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Benito-Ruiz, J. (2019). Fat Harvesting: The Latest Scientific Evidence on Cell Viability. In: Pinto, H., Fontdevila, J. (eds) Regenerative Medicine Procedures for Aesthetic Physicians. Springer, Cham. https://doi.org/10.1007/978-3-030-15458-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-15458-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15457-8
Online ISBN: 978-3-030-15458-5
eBook Packages: MedicineMedicine (R0)