Abstract
A substantial amount of allogenic blood products is transfused in cardiac surgery. Major perioperative blood loss is therefore related with high additional costs already during initial hospitalization of patients. This chapter describes the relevance of blood loss and transfusion from a resource and patient outcome perspective and describes the economic impact of blood transfusions in cardiac surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Case VignetteA 62-year-old male patient was presented for CABG surgery due to left main stem coronary artery disease. Comorbidities include arterial hypertension, hyperlipidemia, chronic kidney disease grade 2, non-insulin dependent diabetes mellitus, and obesity with a body mass index of 34 kg/m2.
The patient undergoes an uncomplicated procedure and is admitted to the cardiac postoperative care unit. Increased chest tube drainage is observed exceeding 900 mL in 12 h. Even after the transfusion of four units of packed red blood cells (PRBCs), the patient becomes hemodynamically more unstable. Subsequently, a decision to undertake surgical re-exploration is made and the patient is taken back to the operating room.
After surgical control of the bleeding and perioperative transfusion of an additional two units of PRBCs and two units of fresh frozen plasma (FFP), no more bleeding is observed and he is readmitted to the cardiac ICU. On day three the patient can be taken off mechanical ventilation, but due to acute renal failure, continuous veno-venous hemodialysis needs to be started for 5 days and the patient develops a postoperative delirium. He is discharged from the ICU after nine days. His hospital stay is further complicated by a superficial wound infection.
In the end, his length of stay is 15 days longer than the mean time for CABG patients at the hospital. The case cost is more than double the average case due to extra staff and material costs. The reimbursement scheme of the universal public health care provider is insufficient to cover the costs, and the excess must be covered by the hospital.
Why Is It Important?
Major blood loss has been reported as one of the main challenges in cardiac surgery [1]. As a result of the demographic change and a rising number of comorbidities seen in patients presenting for cardiac surgery, there has been a considerable increase in perioperative treatment costs [2]. The true cost of transfusion is hard to estimate as not only the direct acquisition has to be considered, but also indirect costs such as blood collection, testing, distribution, storage, and expenses for staff handling the blood products [3]. Moreover, there is strong evidence that allogenic blood transfusion is associated with longer hospital stay, which significantly increases case costs, with hospital stays accounting for more than half of all transfusion-related costs [4], while evidence shows non-inferiority of restrictive transfusion triggers on patient outcome [5, 6].
In this chapter, we will approach the discussion on blood loss and its economic impact in cardiac surgery from three different dimensions. Firstly, bleeding and costs can be considered from a resource perspective, given that allogenic blood products to manage blood loss are a limited resource. Secondly, it can be seen from a patient outcome centered perspective. Finally, it can be approached in terms of the economic impact resulting from the first two dimensions (Fig. 3.1).
Blood Products as Limited Resource
The proportion of blood products of the total blood supply used in association with cardiovascular surgery has been reported to be 5% in the UK and up to 10–15% in the USA [7, 8]. As a consequence, there is a considerable pressure on health care budgets caused—among others—by allogenic blood products. While there has been an overall decline in the use of allogenic blood products in the USA since 2013, which is mainly attributed to patient blood management strategies and surgical innovations, this has also been followed by a decline in blood collection [9]. Therefore, even if blood supply may currently be relatively stable, allogenic blood continues to be of limited availability from a resource perspective.
The number of PRBC transfusions is reported to vary widely between different hospitals, even to the extent that the institution itself has been identified in one study as an independent risk factor for transfusion [10]. When a liberal rather than a conservative transfusion regimen was followed, the odds ratio for PRBC transfusion in those institutions was 6.5 (95% CI 3.8–10.8). In an observational study that included roughly 100,000 patients from 798 institutions, the rate of PRBC transfusion even ranged from 8% to 93%, showing the need for an evidence-based and more standardized approach to blood transfusion [11].
Patient Outcomes
The second dimension of blood loss considers its relevance in terms of patient outcomes. The lack of a universally agreed definition of blood loss means that different studies have used different criteria when defining major or massive perioperative blood loss. Several studies have found a strong association between major blood loss and increased mortality. Defining massive blood loss as having received at least five units of PRBCs within one day of surgery with cardiopulmonary bypass, Karkouti et al. demonstrated an eightfold increase in mortality in their study of 9215 patients [12]. A study by Ranucci et al. of 16,154 patients showed an increase in relative risk of operative mortality of 12% for every 100 milliliters (mL) blood loss in the first 12 postoperative hours [13]. Major postoperative bleeding in this study was defined as the upper 10th percentile of the overall bleeding distribution, which corresponded to 900 mL within 12 h, or to have needed surgical revision due to postoperative bleeding. Patients in the study that suffered from a major bleeding had a fivefold risk of operative mortality. Additionally, preoperative anemia and PRBC transfusion were identified as independent risk factors multiplying the adverse effect of major bleeding. Christensen et al. have showed similar results in their study that included 1188 patients undergoing surgery requiring cardiopulmonary bypass [14]. Patients with increased chest tube drainage in the first six postoperative hours defined as ≥200 mL/h or ≥2 mL/kg/h for two consecutive hours showed a higher 30-day mortality. Nonetheless, high-risk patients undergoing major surgery under a restrictive transfusion strategy are also at a higher risk for complication including higher mortality [15].
Clinical studies also indicate higher morbidity in patients suffering from major blood loss. Both of the last two mentioned studies showed higher rates of strokes, while others demonstrated higher rates of myocardial infarction in addition to higher rates of acute kidney injury and sepsis [13]. Christensen et al. found higher rates of re-exploration and stay in an ICU >72 h, which was corroborated by Ranucci’s results that also showed a longer stay at the ICU [13, 14]. Recently developed standards for the definition of major blood loss have been positively validated and higher scores shown to be associated with increased mortality [16,17,18]. This hopefully will lead to a better comparability of future research.
The Economic Impact of Blood Loss
The economic impact of blood loss, resulting from the previous two dimensions, constitutes the third dimension needing consideration. Stokes et al. investigated the impact of bleeding-related complications in 103,829 heart surgery patients in the USA [19]. In their study, the mean total adjusted hospital costs for patients with bleeding complications was US$ 39,050 compared to US$ 28,771 for patients without this complication. Bleeding complications in this study were defined as having an international classification of disease code related to either hemorrhages or hematoma complicating a procedure, interventions to control for bleeding or transfusion of blood products. Patients with and without bleeding complications also significantly differed in terms of the length of stay (11 days compared to 6 days, respectively) and number of days in ICU (5 days versus 2 days, respectively) [19].
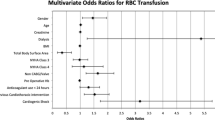
In an analysis that included 463,734 cardiac patients, Zbrozek et al. reported that 51.5% received RBC transfusions, 36.4% fresh frozen plasma (FFP), and 27.7% platelets [20]. Per transfused patient, the mean cost for RBC was $1034, for FFP $323 and for platelets $1281. In a multivariate analysis, the total costs (including expenditures for agents used for bleeding control) increased by 133%. This may be partly explained by a more than fourfold risk of bleeding patients being admitted in an ICU and also to be readmitted for bleeding within 30 days [20].
Christensen et al. conducted a retrospective analysis on the economic impact of postoperative hemorrhage in cardiac surgery [21]. In patients affected by this condition, they found an incremental cost of €6251 on average. Compared to patients without postoperative hemorrhage, univariate analyses demonstrated that bleeding was associated with an increase of €1844 for surgical re-exploration, €639 for blood products, and €3432 for ICU treatment. The authors highlight, however, that additional costs apply to the initial hospitalization with further costs expected for follow-up and rehabilitation care for complications such as stroke and myocardial infarction not considered in this calculation. The overall impact is hence expected to be higher [21].
As evidence on the risks associated with transfusions in cardiac surgery patients has become clearer, structured patient blood management programs have started to be implemented. In order to study the effect of this type of program, Ternström et al. did a prospective study looking at the difference in the year before and after the implementation of one such program in 2010 at the department of cardiothoracic surgery at a Swedish university hospital [22]. The authors found a reduction of transfusion of any blood product by 20.7%, with no evidence of compromised medical safety. This constituted a cost reduction for blood products of 12.4%. To achieve this, the implemented program consisted of three different components, being education, a revision of transfusion guidelines, and a transfusion log.
The probable cost savings from an educational intervention to reduce bleeding-related complications was calculated in a study by Ravyn et al. [23]. The authors developed a model to assess the impact of continuing medical education on the prevention of bleeding-related complications and reoperation for bleeding. Their results suggest that there is a high potential for relevant cost savings by implementing respective educational strategies.
Implications for Daily Practice
In conclusion, there is broad evidence in the literature that transfusion as a consequence of bleeding in cardiac surgery is associated with poor outcomes from a patient and financial perspective. However, the effects of blood loss, transfusion, and the causes leading to transfusion (comorbidities of the patient, hemodynamic instability, acute anemia due to blood loss, etc.) are tightly related and the weight of each component is not yet fully understood. Given the fact that blood transfusions may be life-saving and that studies comparing blood transfusions with placebo in clinical settings are unethical, the estimation of the real clinical impact of transfusion is very difficult. This dilemma also indicates that calculating the real costs of transfusion is complex, as the patient may have died without a transfusion. From an economic point of view, the prolonged length of stay, especially in the ICU, may account for a large portion of case costs. Given that the treatment of bleeding associated complications may be required also after hospital discharge, total costs that result from blood loss are expected to be higher than figures quoted in this chapter. The long-term impact of efficient blood patient management on health resource utilization may thus become considerably more important. Future research may include studies that investigate the impact of a targeted anemia treatment prior to cardiac surgery versus standard of care and the impact of designated treatment algorithms for increased blood loss in the ICU. These studies should include the meticulous prospective sampling of economic data of, e.g., transfusion requirements and ICU treatment to better estimate the costs of blood loss and its required treatment.
References
Petrou A, Tzimas P, Siminelakis S. Massive bleeding in cardiac surgery. Definitions, predictors and challenges. Hippokratia. 2016;20:179–86.
Goldman SM, Sutter FP, Wertan MAC, et al. Outcome improvement and cost reduction in an increasingly morbid cardiac surgery population. Semin Cardiothorac Vasc Anesth. 2006;10:171–5.
Shander A, Hofmann A, Gombotz H, Theusinger OM, Spahn DR. Estimating the cost of blood: past, present, and future directions. Best Pract Res Clin Anaesthesiol. 2007;21:271–89.
Varney SJ, Guest JF. The annual cost of blood transfusions in the UK. Transfus Med. 2003;13:205–18.
Mazer CD, Whitlock RP, Fergusson DA, et al. Restrictive or liberal red-cell transfusion for cardiac surgery. N Engl J Med. 2017;377:2133–44.
Shehata N, Mistry N, da Costa BR, et al. Restrictive compared with liberal red cell transfusion strategies in cardiac surgery: a meta-analysis. Eur Heart J. 2018. https://doi.org/10.1093/eurheartj/ehy435.
Ferraris VA, Brown JR, Despotis GJ, Hammon JW, Reece TB, Saha SP, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. The International Consortium for Evidence Based Perfusion formally endorses these guidelines. Ann Thorac Surg. 2011;91:944–82.
Cobain TJ, Vamvakas EC, Wells A, Titlestad K. A survey of the demographics of blood use. Transfus Med. 2007;17:1–15.
Ellingson KD, Sapiano MRP, Haass KA, et al. Continued decline in blood collection and transfusion in the United States-2015. Transfusion. 2017;57:1588–98.
Stover PE, Siegel LC, Parks R, et al. Variability in transfusion practice for coronary artery bypass surgery persists despite national consensus guidelines: a 24-institution study. Anesthesiology. 1998;88:327–33.
Bennett-Guerrero E, Zhao Y, O’Brien SM, et al. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA. 2010;304:1568–75.
Karkouti K, Wijeysundera DN, Yau TM, et al. The independent association of massive blood loss with mortality in cardiac surgery. Transfusion. 2004;44:1453–62.
Ranucci M, Baryshnikova E, Castelvecchio S, Pelissero G. Major bleeding, transfusions, and anemia: the deadly triad of cardiac surgery. Ann Thorac Surg. 2013;96:478–85.
Christensen MC, Dziewior F, Kempel A, von Heymann C. Increased chest tube drainage is independently associated with adverse outcome after cardiac surgery. J Cardiothorac Vasc Anesth. 2012;26:46–51.
Hovaguimian F, Myles PS. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2016;125:46–61.
Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg. 2014;147:1458–63.
Biancari F, Ruggieri VG, Perrotti A, et al. European multicenter study on coronary artery bypass grafting (E-CABG registry): study protocol for a prospective clinical registry and proposal of classification of postoperative complications. J Cardiothorac Surg. 2015;10:90.
Bartoszko J, Wijeysundera DN, Karkouti K, et al. Comparison of two major perioperative bleeding scores for cardiac surgery trials: universal definition of perioperative bleeding in cardiac surgery and European coronary artery bypass grafting bleeding severity grade. Anesthesiology. 2018;129:1092–100.
Stokes ME, Ye X, Shah M, et al. Impact of bleeding-related complications and/or blood product transfusions on hospital costs in inpatient surgical patients. BMC Health Serv Res. 2011;11:135.
Zbrozek A, Magee G. Cost of bleeding in trauma and complex cardiac surgery. Clin Ther. 2015;37:1966–74.
Christensen MC, Krapf S, Kempel A, von Heymann C. Costs of excessive postoperative hemorrhage in cardiac surgery. J Thorac Cardiovasc Surg. 2009;138:687–93.
Ternström L, Hyllner M, Backlund E, Schersten H, Jeppsson A. A structured blood conservation programme reduces transfusions and costs in cardiac surgery. Interact Cardiovasc Thorac Surg. 2014;19:788–94.
Ravyn D, Ravyn V, Lowney R, Ferraris V. Estimating health care cost savings from an educational intervention to prevent bleeding-related complications: the outcomes impact analysis model. J Contin Educ Heal Prof. 2014;34:S41–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Balzer, F., Uden, H. (2019). Relevance of Blood Loss and Economic Impact. In: von Heymann, C., Boer, C. (eds) Patient Blood Management in Cardiac Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-15342-7_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-15342-7_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15341-0
Online ISBN: 978-3-030-15342-7
eBook Packages: MedicineMedicine (R0)