Abstract
Contrast-enhanced mammography (CEM) is an imaging tool that is increasingly being used to evaluate for breast cancer. It is important for breast groups to understand how this system works and its impact on clinical workflow prior to implementation to ensure a smooth transition. In this chapter, we will review the equipment, physical space, and data storage requirements; the most common indications for use and the patient selection process; how CEM images are acquired and the steps involved in planning and performing the exam; the necessary staff training; and lastly strategies for marketing your new CEM system.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Contrast-enhanced mammography
- CEM implementation
- CEM equipment requirements
- Technologist training
- Radiologist training
- Radiology workflow
- Image storage
- Patient selection
- Screening
- Protocoling
3.1 CEM Overview
A CEM is a four-view bilateral mammogram acquired using a dual-energy technique in standard craniocaudal and medial lateral oblique projections performed entirely after intravenous injection of nonionic low-osmolar iodinated contrast. During each compression, low-energy images are acquired that provide morphologic and density information similar to a conventional mammogram [1], and high-energy images are acquired that provide vascular information similar to breast MRI. Recombined images are generated from subtracting and post-processing the low- and high-energy images, highlighting areas of contrast uptake. A combination of any findings seen on low-energy and/or recombined images is included in exam interpretation (Fig. 3.1). The added information on enhancement allows CEM to identify cancers that would otherwise be obscured on conventional mammography due to tissue density. As a result, CEM in the diagnostic setting has shown improved performance relative to full-field digital mammography (FFDM) and similar performance to breast MRI [2,3,4,5,6,7]. The Food and Drug Administration (FDA) approved its use as an adjunct to mammography and ultrasound to localize a known or suspected lesion in 2011 [8]. Since that time, there has been increased interest in CEM primarily as a less costly and more accessible alternative to breast MRI.
3.2 Equipment Requirements
One of the perceived strengths of CEM is the relatively few equipment requirements necessary to perform the imaging exam. The minimum requirement includes a mammography unit capable of performing dual-energy imaging. Some older mammography units can be upgraded to allow for the acquisition of dual-energy images. This upgrade includes the addition of software and firmware that includes new dose tables to allow for the correct display of dose for the low- and high-energy images. In addition, a copper filter is added to the mammography unit’s filter wheel (Fig. 3.2). This copper filter selects high-energy X-rays to be used for the high-energy image acquisition. Once the mammography unit has been upgraded, the physicists must test it to ensure it is functioning appropriately. The process of upgrading the mammography unit and undergoing physicist testing takes approximately 2 days. Practices will need to account for the time this unit will be out of use when planning the clinical schedule.
CEM can be viewed on many vendors’ digital workstations with varying functionality. It is worthwhile to contact the vendor managing your imaging display to determine whether CEM can be viewed and what is required to allow viewing. A common method of viewing the CEM study is with the low-energy and recombined images stacked on top of one another. This allows the radiologist to flip between the two images for direct correlation of findings seen on low-energy and recombined images. Vendors distributing CEM mammography equipment typically have viewing workstations with added functionality, such as fading of the low-energy image into the recombined image or the ability to co-register the contrast mammography images with tomosynthesis images, but this added functionality is not required for implementation. Setting up a workstation to be able to view CEM images may take up to a few hours, and this should be accounted for during the implementation schedule.
Lastly, a power injector is a worthwhile consideration for injection of the contrast agent. Although not required, the power injector allows the contrast to be injected more easily than using a manual technique. If using an injector, it must be able to inject the contrast material at a rate of 3 mL/s.
3.3 Physical Space Requirements
The CEM study takes place within the mammography room using CEM-capable mammography equipment. There are a few items that should be close at hand when preparing for the study. These items include a power injector and emergency supplies should the patient develop a contrast reaction. Although it is possible to inject the intravenous line (IV line) outside the mammography unit, it is recommended to perform the injection in the room. This allows for appropriate timing of the CEM study while minimizing the possibility for interruption. It is also preferable to have the patient seated while injecting. This is not only more comfortable for the patient but also safer should the patient have a vasovagal or contrast reaction during, or immediately following, the injection.
To prepare for a possible contrast reaction, it is vital to have emergency supplies readily available. In our department, we keep a small emergency supply box within the contrast mammography room that contains medications used for treating contrast reactions. We also have a crash cart that includes an automated external defibrillator (AED) device and pacer pads close by on the floor. In addition, practices should have policies for how to manage a contrast reaction and who will manage it, should one occur. For hospital-based practices, this can include utilizing the hospital medicine resources. For outpatient sites, an arrangement can be made with local medicine practices, otherwise emergency services will need to be called. The recommended contrast training for technologists and radiologists will be discussed in more depth later in the chapter.
The final component for the CEM room that is worth considering is a scale. At the time of this writing, it is common practice to administer the contrast agent at a dose of 1.5 mL/kg. To determine the correct amount of contrast to administer, practices can choose to ask the patient to provide her weight or can directly weigh the patient. It is worthwhile to first discuss these options with radiology colleagues in the institution’s CT department to see if there are departmental standards for contrast administration.
In addition to preparing the CEM room, it is important to set up a space for placing the IV line. Ideally, this will be a separate room from where the CEM will be performed. It is also helpful to have someone place the IV who has experience performing this task, such as an experienced technologist or nurse. Doing so unlinks IV placement from the performance of the CEM which, in turn, will decrease technologist and mammography room utilization times [9]. A few items are needed to adequately prepare the IV placement room. This includes a chair for the patient to sit in while the IV is placed, IV placement supplies, a sharps container for the needles after they are used, and a point-of-care (POC) test kit for rapid bedside evaluation of renal function (further discussion in contrast safety section). It is worthwhile to consider a reclining chair for IV placement. This may be helpful should the patient have a vasovagal response during IV placement and needs to be laid down.
3.4 Storage Considerations
As reviewed earlier, the standard images for a CEM include standard craniocaudal and mediolateral oblique projections for each breast. Low-energy and high-energy images are acquired during each compression for a total of eight images. The mammography unit automatically processes the low- and high-energy images into a recombined image. The processed recombined images and the processed low-energy images are sent to the imaging workstation for radiologist interpretation and long-term storage. At our institution, the low- and high-energy raw images, of which there are eight, are also sent for storage; however they are not used for interpretation.
The size of each low-energy, high-energy, and recombined image that is acquired and stored is roughly equivalent to a conventional mammographic 2D image. Therefore, the average storage size for a CEM is just a multiple of the average storage size of a conventional 2D mammogram. The storage size will vary depending on whether your institution chooses to store the high-energy images in addition to low-energy and recombined images.
The necessary storage space will increase if additional images are acquired. Additional imaging, such as 90° lateral views, magnification, or spot compression views, can be performed as requested by the interpreting radiologist. These additional images can be acquired using a dual-energy technique highlighting contrast uptake or using only FFDM or tomosynthesis. Should these images be performed using dual-energy, they must be obtained within the 10-min window after contrast administration as contrast is still visible during this time.
It is important to recognize these storage considerations when implementing CEM into your practice as the ability to store the images will depend on the capacity for your PACS.
3.5 Patient Selection
3.5.1 Study Indication
Since receiving FDA approval, CEM has been utilized and studied in many different clinical settings. In non-cancer patients, it has been used to evaluate abnormalities detected on screening mammography or ultrasound, as a follow-up to inconclusive imaging findings, to assess patients with clinical symptoms, and to better detect breast cancer in high-risk women and/or women in whom mammography is of limited value (e.g., dense breast tissue) [2, 3, 10,11,12,13,14,15]. In patients with suspected or known cancer, CEM has been used to evaluate extent of disease, better define mammographically occult cancers, and monitor response to neoadjuvant chemotherapy [16,17,18].
When incorporating CEM into practice, a group must first decide for which cases they will be using the modality, i.e., screening callbacks or palpable lumps or to allow each radiologist to choose when they think CEM would be useful. A good population to learn from could be patients with known cancers. For the imager, the recombined images parallel findings seen on breast MRI, as both are technologies assessing vascularity and tumor angiogenesis. In fact, prior MRI can be used for comparison if there are no prior CEM examinations.
Moving forward, practices may opt to use CEM as an alternative to breast MRI given that it is a lower-cost, faster, more accessible option to breast MRI [9, 19]. Using CEM in this setting may also be more palatable to practitioners and patients given that an IV line is placed and contrast injected with both exams, and therefore no added discomfort or risk is being introduced with the CEM. CEM is particularly useful for patients with relative or absolute contraindications to MRI, including pacemakers, metal devices such as aneurysm clips and cochlear implants, increased body habitus limiting MRI scanner capacity, inability to lay prone, or claustrophobia.
As we gain experience with CEM in our practice, we are transitioning to using CEM as the first-line imaging tool for disease extent in women with newly diagnosed breast cancer who would otherwise be getting contrast-enhanced imaging with breast MRI. The most frequently imaged are those who are young (less than 50 years old), have invasive lobular carcinoma, or have mammographically occult malignancy. Should the CEM be difficult to interpret, such as when there is moderate to marked background enhancement or the malignancy is near the chest wall, we will then recommend breast MRI. Using CEM in this way not only minimizes the wait time for the advanced imaging information but also allows greater interaction between the radiologists throughout the staging process. Often with breast MRI, the exam is interpreted after the patient leaves the department, and in some practices the referring clinician rather than the breast imager may transmit the results to the patient. In our practice, the CEM is performed similarly to a diagnostic mammogram, where the patient waits in the department until all necessary imaging is completed. The results are then immediately transmitted to the patient by the radiologist who also can show the images and answer any questions.
Once the imagers and the rest of the breast care team have gained some familiarity with CEM as a new technology, the practice can consider expanding indications for which CEM is performed.
3.5.2 Contrast Safety
In addition to choosing the indications for use, the practice must establish guidelines for determining who can safely receive the contrast agent. In general, the main concerns relate to allergic-like and physiologic reactions as well as other nonallergic reactions, such as contrast-induced nephropathy (CIN), that may develop after contrast administration. Per the American College of Radiology (ACR) Contrast Manual, acute contrast reactions are rare, occurring in less than 1% of patients, and when occur they tend to be mild and self-limiting. Severe reactions to low-osmolar nonionic contrast agents are extremely rare, reported at 0.04%. Fatalities are also extremely rare with a conservative estimate of 1 fatality per 170,000 contrast-enhanced exams. Delayed allergic-like reactions occur in 0.5–14% of patients and are often cutaneous and self-limited [20].
Contrast-induced nephropathy (CIN) is defined as an acute deterioration of renal function caused by intravascular iodinated contrast administration. Unfortunately, there is very little data on the true incidence of CIN as few studies were designed to allow for differentiation of CIN from other causes of post-contrast acute kidney injury. Despite this, the ACR still supports this diagnosis but states that it is a rare entity.
When determining a patient’s risk for a contrast-related event, it is often necessary to review the patient’s medical history. The ACR Contrast Manual indicates that patients with a history of prior reaction to iodinated contrast media have a fivefold increased risk for developing a subsequent reaction [20]. This is the greatest predictor for subsequent contrast reaction. Beyond that, the manual identifies other medical conditions that may increase the likelihood of an acute reaction; however, the degree of this added risk is not clear. These conditions include asthma, multiple severe allergies, significant cardiovascular disease including aortic stenosis or severe congestive heart failure, anxiety, and renal insufficiency. Acute thyroid storm, recent radioactive iodine therapy or imaging, or use of beta-blockers may also impact a patient’s response to the contrast. Given that the risks for acute contrast reactions are not well-defined, there may be some variability in how practices identify patients at risk for a contrast-related event and who they deem appropriate to receive contrast.
Consensus among all studies evaluating CIN is that underlying severe renal insufficiency is the main risk for development of CIN. However, there is no agreed upon cutoff for serum creatinine of estimated GFR measures to determine when the risk of CIN significantly increases. As a result, practices vary significantly in their guidelines for contrast administration in patients with underlying renal disease. Groups that use renal function measures to determine risk for CIN most commonly use serum creatinine. Increasingly, however, the calculated estimated glomerular filtration rate (eGFR) is being used due to limitations of using the serum creatinine alone. Both measures are limited in patients with acute renal insufficiency [20]. Renal function can be tested in a lab or at the bedside using a point-of-care (POC) test kit (Fig. 3.3). It is important to note that these POC tools may overestimate renal function [21, 22]. Therefore, while they may be an attractive option, it is worthwhile considering formal lab testing, if available.
If your breast imaging group is part of a hospital system or large radiology practice, guidelines for safe contrast administration are often predetermined by the CT section. Otherwise, the ACR Contrast Manual is a valuable resource for understanding the risks of contrast agents, determining screening guidelines, as well as reviewing treatment strategies should a reaction occur [20].
Ultimately, the benefit of imaging must always be weighed with the risk of any contrast-related event. Often CEM is not critical to a patient’s care, and therefore our practice has opted to only offer CEM to those patients without any risk factors for a contrast-related event. Otherwise, conversations are had with the referring staff regarding the medical need for the study.
Once you determine that a patient is safe to receive contrast, there is still the small possibility for a contrast reaction. Therefore, it is vital that staff, primarily the technologists and radiologists, be prepared to address a reaction should it occur. Staff training will be discussed in more depth later in the chapter. There is also the small chance (0.1–1.2%) that the contrast agent will extravasate into the surrounding tissue while being administered [20]. The patient may experience swelling, tightness, or burning at the IV site. When treated appropriately, extravasations often resolve without significant injury. Rarely, however, serious complications may occur. Your practice should have a formal system in place for managing extravasation when it happens.
Overall, determining that a patient is safe to receive contrast is a critical component of the implementation process. Although contrast reactions can happen, significant reactions are uncommon, and this should not deter a practice from implementing CEM.
3.6 Workflow Considerations
There are many aspects to consider when incorporating CEM into clinical workflow. To sufficiently address key components of implementation, we have chosen to divide the clinical experience into three stages: before the patient arrives in the department, while the patient is in the department, and after the patient has left the department (Table 3.1).
3.6.1 Prior to Patient Arrival in the Department
3.6.1.1 Appointment Times
A practice should decide the time that will be allotted for a CEM appointment. The image acquisition time for CEM is similar to that of a diagnostic mammogram; however, the preparation for the study including IV placement requires additional time [9]. Ideally, IV line placement will be performed outside the mammography room and therefore will not impact the appointment time slot, which is often based on mammography room and technologist utilization. In this scenario, the CEM can be scheduled in a routine diagnostic mammogram appointment slot. Should the practice decide to use the mammography room or the mammography technologist for IV placement, it may be worth lengthening the appointment slot to account for this added use of mammography resources. Given that each practice has different available resources, individual groups will have to determine how much time to allocate to the appointment to complete these tasks.
3.6.1.2 Ordering
Once a practice routinely performs CEM, orders may originate from several parties. Many requests for CEM will originate from within the radiology department, such as in the setting of callbacks for abnormal screening studies or to further evaluate inconclusive findings on FFDM, tomosynthesis, and/or ultrasound. Other requests will originate from primary care providers or the breast care team of referrers (surgeons, breast nurse practitioners, medical oncologists, radiation oncologists). A practice must decide whether they will require radiologist approval prior to the clinician placing an order for the study, to ensure the CEM is ordered for the correct indication and is safe to perform, or whether they will allow referrers to place the order without radiologist input. In the latter scenario, it is vital that the breast practice employs a clinical decision support tool or creates an alternate protocoling system, whereby the practice can ensure that the CEM has been appropriately ordered. As with any diagnostic study, if a general practitioner is given the option to order a specific exam, it is important he/she have some knowledge of the indications.
3.6.1.3 Scheduling
Our academic center offers various breast imaging and intervention services at numerous sites throughout our network. Some sites are screening only, others offer diagnostic mammography and ultrasound services with ultrasound interventions only, and our main academic site offers all diagnostic imaging and interventions, including breast MRI and MRI-guided biopsies. Therefore, if a patient at one of these satellite sites needs an MRI biopsy, she would be instructed to go to the main campus for the procedure. Similarly, CEM is only offered at our main campus due to equipment availability. As a result, patients must be appropriately scheduled at the main campus and clearly instructed to arrive at the main site for the imaging exam. For multisite practices like ours, it is important to create a system for how patients from one site will be scheduled at another site. Education of the administrative staff at the different sites is critical.
3.6.1.4 Validating Appropriateness and Protocoling
It is important to make sure that patients who are scheduled for CEM are appropriate candidates for the study before their visit. This is especially true when having patients travel to a satellite office to have the CEM. It is suboptimal for a patient to travel to a distant site only to later discover she cannot have the CEM. As mentioned above, practices with sophisticated ordering programs and IT support can use a decision support platform and incorporate a series of contrast screening questions into the order entry process. Screening can also take place after the CEM has been scheduled by a radiologist or radiologist-in-training.
Once a patient is deemed an appropriate candidate for CEM, a protocol should be provided that indicates three aspects: confirmation that it is safe for the patient to receive a CEM, whether any additional testing is necessary to prove it is safe for the patient to receive contrast (i.e., renal function testing), and what images should be performed at the time of the imaging exam.
There is no agreed upon ordering of images for a CEM. Jochelson and colleagues showed that the order of image acquisition did not impact a radiologist’s ability to identify breast cancer [5]. Some practices begin with one view of the affected side and alternate with the non-affected side, while others do both projections for the affected breast first. Still others will begin with the same projection for both breasts. For example, they will perform craniocaudal views for each breast first followed by the mediolateral oblique views. Lastly, some practices simply have their mammography technologists perform the CEM similarly to how they would perform the diagnostic mammogram in order to keep the mammography technologists comfortable. Each practice should decide how they will acquire the images, and this will be part of their standing protocol for CEM.
Practices may also create protocols for CEM performed for specific indications. For example, a practice offering conventional FFDM may have a “lump protocol” for their technologist that includes routine CC and MLO views with additional images such as a lateral or spot compression or tangential view. If this patient could have CEM, the “lump protocol” may differ, with fewer or no additional images given the benefit of dual-energy imaging offering higher diagnostic capabilities.
3.6.2 During Patient Visit in the Department
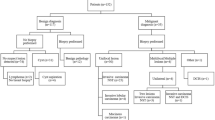
When the patient arrives for a CEM, she interfaces with many different members of the breast imaging team. Figure 3.4 outlines the parallel steps involved by the patient, technologist, radiologist, and other staff during the CEM study. This is discussed in detail below.
3.6.2.1 Screening for Contrast Contraindications
Patients receiving IV contrast for CT are commonly given a questionnaire to evaluate for contrast risk at the time of check-in. This questionnaire is reviewed by the technologist before performing the study and allows the technologist to identify any possible contraindications to contrast administration. Given that the contrast agent used for a CEM is the same as what is used for CT scans, patients receiving CEM should similarly complete these forms, per department protocol, in addition to any conventional mammography questionnaires. The screening questions should include identification of any allergies, any prior history of IV contrast administration or reaction, and questions related to renal function or conditions that may cause renal insufficiency. Breast imaging groups can either use the CT questionnaire itself or make their own based on accepted department guidelines. In our practice, this serves as the second safety check to make sure that the patient is an appropriate candidate for the CEM exam. (The first check occurs before the patient arrives in the department.)
After check-in but before the exam, our practice has opted to have a member of the breast imaging team (nurse, nurse practitioner, or physician) briefly speak to the patient about CEM. We discuss how the exam is performed and the added benefits of this imaging technique. We also ask the patients a series of questions related to contrast risk (Table 3.2). This serves as the third safety check for CEM.
Some practices may opt to perform a time-out procedure immediately prior to contrast administration, similar to what is performed for other imaging-guided procedures and surgical cases. This would serve as the final check before the exam is performed.
3.6.2.2 IV Placement
Although this may appear to be a simple task, IV placement may be one of the more challenging components of CEM implementation. Unlike MRI or CT technologists, mammography technologists may not be familiar with IV line placement and therefore may not embrace this new task. As a result, practices may need to identify other members of the breast imaging team who can comfortably and safely place the IV line. Practices can utilize preexisting resources, such as other CT/MRI technologists, who routinely place IV lines. The feasibility of this is related to how accessible the other services are to the breast imaging suite. Another option is to train other members of the team, such as a nurse navigator or nurse practitioner, if either is available. Lastly, a hospital-based practice may opt to use a specialized IV team; however, this may result in suboptimal efficiency depending on the travel distance required.
The person placing the IV line must learn the gauge of the angiocatheter and location for IV placement. Ideally, a 20 G angiocatheter will be used in the antecubital fossa. However, smaller angiocatheters can be used, if needed. Most importantly, the angiocatheter must be able to support the flow rate of 3 cc/s from the power injector. It is worthwhile to reference the power injector for minimal gauge required for use. It is also important to have a system in place for handling technically challenging IV placements or those patients with chest wall ports.
Ideally, the person placing the IV line should also be trained to perform POC renal function testing, if being used. Not all patients will require this testing, and this should be determined ahead of time based on department guidelines for contrast administration. Independent breast practices should consult the ACR Contrast Manual and other local radiology groups to develop a formal practice guideline.
If the practice opts to have members of the breast imaging team perform IV placement and POC testing, it is useful to train at least two people for this task. This ensures that there is a backup person available should the main person be unavailable. If a second person is not available, then it is worthwhile to create a backup plan with the CT/MRI department or the IV team.
In addition to identifying the staff to place the IV line, it is important to also identify a room for IV line placement. Ideally, the IV line should be placed in a separate room from the mammography unit in order to minimize mammography room utilization times.
3.6.2.3 Contrast Administration
While the patient is having her IV line placed, the technologist can be preparing the mammography room and injector for contrast administration. As the CEM study is sensitive to timing of contrast, we suggest the patient receive the contrast in the same room that the mammography images are performed. Standard practice is to administer the nonionic iodinated contrast agent at a dose of 1.5 mL/kg and at a rate of 3 mL/s. Our group weighs each patient for accurate dosing but this is not universal practice. In addition, a power injector is recommended to administer the contrast agent at the abovementioned rate. It is also recommended that the technologists wear gloves when administering contrast to prevent contamination on the breast or detector.
Although the contrast is being administered by the technologist, all members of the breast imaging team (technologists, nurses, nurse practitioners, physicians-in-training, and physicians) should be trained to manage contrast reactions and extravasation. This training should be performed at routine intervals. In addition, it is worthwhile to have a designated location to observe patients who may have a contrast-related event. This location should be separated from the mammography room to have minimal impact on workflow and other patients presenting for imaging evaluation.
3.6.2.4 Performing CEM (and Any Additional Imaging)
Once the patient has received the contrast, the IV line is disconnected, and the patient is ready for imaging. It is imperative that the dual-energy images be obtained within a 10-minute period to maintain the benefits of contrast enhancement [5]. It is conventional to obtain bilateral craniocaudal and mediolateral oblique dual-energy views, even if there is only one affected symptomatic or abnormal side. However, there is no set standard of which order the images should be acquired. In our practice, following a (minimum) 2-min delay, we alternate imaging of each breast, starting with the craniocaudal view of the affected breast (Fig. 3.5).
Depending on the indication for the exam, additional dual-energy or conventional views can be obtained following the initial four dual-energy views to assist in diagnosis. These views are often determined by the practice’s protocols, although may also be requested by the interpreting radiologist based on the individual case. Having established protocols helps streamline workflow so that any additional images can be obtained while the patient is in the mammography room for the CEM study. This is especially important if additional dual-energy images are being obtained as these should be performed within the 10-min window following contrast injection. Alternatively, the radiologist can stay in the mammography room while the CEM is being performed such that a quick decision can made as to whether additional images should be obtained. Often these additional dual-energy images are acquired after the standard four views are obtained.
Like any diagnostic mammogram, once the initial images are completed, the patient is asked to wait in the diagnostic lounge, and the study is reviewed by the radiologist. Any findings identified by the radiologist are then worked up with mammography, tomosynthesis, or ultrasound, while the patient waits in the department.
3.6.2.5 Management of Results
Once the diagnostic workup is complete, the radiologist must provide an appropriate BI-RADS code (to be discussed in depth in a later chapter) and associated management plan. In many scenarios, conventional mammography, tomosynthesis, and ultrasound may be used for any follow-up or interventional procedures that are necessary. It is important to recognize, however, that there may be CEM-only findings for which mammography, tomosynthesis, and/or ultrasound cannot resolve. At present, MRI is commonly used in this scenario with subsequent MRI biopsy if an MRI correlate is found. Practices without immediate access to breast MRI should connect with local groups who do have MRI. Alternatively, CEM follow-up can be pursued, or CEM-guided biopsy can be attempted using conventional mammography equipment as there is currently no formal method for performing a CEM-guided biopsy.
Regardless of the final recommendation, it is critical for the breast imaging practice to have a plan to ensure that any recommended imaging occurs. For example, if an MRI is going to be recommended, it is important that the practice have a plan for how this will be communicated to the patient and referring physician and how the MRI will be ordered and scheduled.
3.6.3 After Patient Leaves the Department
3.6.3.1 Coding and Billing
Although CEM requires additional time of screening and speaking to the patient about contrast administration, placing the IV line, and administering contrast [9, 23], there is no billing code specific to this study yet. Thus, our practice, like others performing CEM, is billing this procedure as a diagnostic mammogram with IV contrast. As CEM becomes more routinely used, we suspect there will be separate CPT (current procedural terminology) codes taking the additional factors associated with CEM into account. The use of CEM in lieu of MRI can result in a significant cost savings [19], and a practice may be able to elicit institutional support for some of the nonreimbursed time and personnel to build a CEM program.
3.7 Staff Training
Staff training largely involves the technologists, who will be performing the CEM, and the radiologists who will be interpreting the exam (Table 3.3). These two groups will be the focus of this chapter; however, there are others involved in the clinical workflow that should be identified and included in the implementation process. This includes the technical support staff helping with CEM workflow, front desk staff checking patients in, nursing staff helping with IV placement and/or monitoring, and the schedulers and coordinators who are booking the exams. These people are all part of the CEM team. By involving them early you can ensure they understand their role and can successfully perform it.
3.8 Technologists
The technologists play a large role in preparing for and performing CEM. In fact, in our institution the technologists are the main interface with patients during this exam. As a result, it is important that they not only understand how to physically perform the exam, but it is also important they understand the value of the study. This begins with someone from the team providing an educational overview of the modality to include the history of the exam, the data supporting its use, and examples of how CEM can benefit patients. At the beginning, it is also worthwhile to identify two to three technologists who will learn to perform the CEM and who can train additional staff as needed. These technologists will be the first members of the CEM team, so it is vital to choose technologists who can embrace innovation and change. Getting the technologists invested in CEM is a top priority and will allow for a smoother implementation process.
Once the CEM technologists are identified and have received basic training on the background of the technology, they must be trained to perform the exam by an application specialist. This training includes how to perform the exam on both a phantom and a patient, as well as all quality control requirements. This training takes approximately 2 days. The clinical workflow should consider the absence of these technologists and the mammography room when planning for the training.
As mentioned above, the technologists’ role is not isolated to simply performing the CEM. They must also be trained as to which patients are acceptable candidates for the study and who might be at risk for a contrast-related event. As with CT and MRI at our institution, our patients complete a safety form before their CEM to make sure they can safely undergo the imaging exam. This form is the same form used for CT studies, as the risks related to a contrast-related event and radiation are the same. The technologists review these forms before performing the study. Given that not all mammography technologists are acquainted with the risks of iodinated contrast or these forms, they must be trained in the institutional guidelines on who can receive iodinated contrast, who cannot receive contrast, and any required testing that must be performed to determine whether the patient can receive contrast agent.
Depending on your clinical workflow, the technologists may also need to be trained on how to place IV lines and perform bedside renal function testing using a POC test kit. Part of this training includes learning the minimal gauge requirements to handle the power injector flow rate of 3 cc/s. Twenty and twenty-two gauge angiocatheters are commonly used. Chest wall ports often have specific rules for access and training should include these. When using a power injector, it is important that the port is power-injectable and can handle the high flow rates. It is also important to make sure that the injection is performed in a way to preserve the port function, such as using heparin before and after injection to ensure port patency. Lastly, it is worthwhile to have a system in place for those patients that are technically challenging for IV placement.
Once the CEM is performed, the technologists must be aware of how to identify and manage the preliminary phases of a contrast-related event should one occur. These include contrast-related reactions and extravasation. Often breast divisions can use policies already in place for managing contrast reactions and extravasation; however, stand-alone breast imaging practices may need to formulate these from scratch. Overall, CEM training should include training on contrast-related events so all staff can act appropriately in this circumstance. This training should occur at routine intervals. At our institution, training includes an annual lecture followed by clinical scenarios. Simulation has also been shown to be useful for contrast reaction training and should be considered [24, 25].
Lastly, technologists should be knowledgeable about the radiation dose of a CEM, like conventional mammography or tomosynthesis. In our experience, it is not uncommon for patients to ask about radiation dose when an exam is being performed. To aid the technologists, it may be worthwhile to create an educational handout for patients discussing the benefits of CEM while addressing questions related to dose and contrast administration.
3.9 Radiologists
Like technologists, radiologists must first understand the role and value of CEM in their clinical practice. This is vital for ultimate acceptance of this new modality. Often this will involve discussions among the clinical group regarding how best to implement the technology so as to incur minimal disruptions to the clinical workflow. Radiologists must then be trained in two primary areas which include management of contrast-related events and CEM interpretation and reporting.
Along with their technologist colleagues, radiologists must learn how to screen patients for risk factors for contrast administration, identify contrast-related events, and learn how to manage them. This is especially important given that contrast is not routinely administered in breast imaging divisions, and therefore some breast radiologists, particularly those without exposure to breast MRI, may be less comfortable managing contrast-related events than their colleagues in general radiology. Training should be a formal process and can include simulation exercises to maximize radiologist comfort. Given that contrast reactions can also occur with breast MRI, although less frequently, this training serves to prepare breast imagers for adverse events with both modalities.
Radiologists must also learn how to interpret and report CEM cases. Overall, it is a relatively straightforward modality to learn to interpret given that image interpretation is similar to other modalities commonly interpreted by breast imagers. This includes the low-energy images which are similar to conventional mammography and the recombined images which are similar to subtraction images on MRI without kinetics. Lalji and colleagues demonstrated that radiologists with no experience interpreting CEM performed nearly as well as those with 2 years of experience [2].That being said, there is training that is involved to teach radiologists how to appropriately view and hang the CEM images, as well as how to interpret CEM findings. This includes the imaging appearance and management of benign and malignant breast disease on CEM. Radiologists must also be taught how to report CEM, highlighting the fact that CEM interpretations and reports include findings seen on both low-energy and recombined images. As of this writing, there is no formal training requirement for CEM interpretation; however, one study suggested that radiologist performance improved from 80% to 92.4% after diagnosing 100 lesions [3]. Therefore, it is recommended that radiologists have an opportunity to view CEM cases before incorporating CEM into clinical practice.
3.10 Marketing
Having your technologists and radiologists excited about CEM is important, but it is also important to have referring providers and patients on board as well. This can be accomplished through educational conferences, letters to providers, pamphlets, and posters. Showing a few relevant cases at tumor boards may also encourage clinicians to order CEM. Practices should also embrace social media as a platform for advertising their new use of CEM. Finally, radiologists should talk to patients directly, informing them of the new service that the group is offering.
References
Lalji UC, Jeukens CR, Houben I, Nelemans PJ, van Engen RE, van Wylick E, et al. Evaluation of low-energy contrast-enhanced spectral mammography images by comparing them to full-field digital mammography using EUREF image quality criteria. Eur Radiol. 2015;25(10):2813–20.
Lalji UC, Houben IP, Prevos R, Gommers S, van Goethem M, Vanwetswinkel S, et al. Contrast-enhanced spectral mammography in recalls from the Dutch breast cancer screening program: validation of results in a large multireader, multicase study. Eur Radiol. 2016;26(12):4371–9.
Cheung YC, Lin YC, Wan YL, Yeow KM, Huang PC, Lo YF, et al. Diagnostic performance of dual-energy contrast-enhanced subtracted mammography in dense breasts compared to mammography alone: interobserver blind-reading analysis. Eur Radiol. 2014;24(10):2394–403.
Fallenberg EM, Schmitzberger FF, Amer H, Ingold-Heppner B, Balleyguier C, Diekmann F, et al. Contrast-enhanced spectral mammography vs. mammography and MRI – clinical performance in a multi-reader evaluation. Eur Radiol. 2017;27(7):2752–64.
Jochelson MS, Dershaw DD, Sung JS, Heerdt AS, Thornton C, Moskowitz CS, et al. Bilateral contrast-enhanced dual-energy digital mammography: feasibility and comparison with conventional digital mammography and MR imaging in women with known breast carcinoma. Radiology. 2013;266(3):743–51.
Tagliafico AS, Bignotti B, Rossi F, Signori A, Sormani MP, Valdora F, et al. Diagnostic performance of contrast-enhanced spectral mammography: systematic review and meta-analysis. Breast. 2016;28:13–9.
Lee-Felker SA, Tekchandani L, Thomas M, Gupta E, Andrews-Tang D, Roth A, et al. Newly diagnosed breast cancer: comparison of contrast-enhanced spectral mammography and breast MR imaging in the evaluation of extent of disease. Radiology. 2017;285(2):389–400.
GE Healthcare 510(k) premarket notification submission. [Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf10/k103485.pdf]. Accessed February 19, 2019.
Phillips J, Steinkeler J, Talati K, Brook A, Dialani V, Fishman M, et al. Workflow considerations for incorporation of contrast-enhanced spectral mammography into a breast imaging practice. J Am Coll Radiol. 2018;15(6):881–5.
Jochelson MS, Pinker K, Dershaw DD, Hughes M, Gibbons GF, Rahbar K, et al. Comparison of screening CEDM and MRI for women at increased risk for breast cancer: a pilot study. Eur J Radiol. 2017;97:37–43.
Lobbes MB, Lalji U, Houwers J, Nijssen EC, Nelemans PJ, van Roozendaal L, et al. Contrast-enhanced spectral mammography in patients referred from the breast cancer screening programme. Eur Radiol. 2014;24(7):1668–76.
Mori M, Akashi-Tanaka S, Suzuki S, Daniels MI, Watanabe C, Hirose M, et al. Diagnostic accuracy of contrast-enhanced spectral mammography in comparison to conventional full-field digital mammography in a population of women with dense breasts. Breast Cancer. 2017;24(1):104–10.
Phillips J, Miller MM, Mehta TS, Fein-Zachary V, Nathanson A, Hori W, et al. Contrast-enhanced spectral mammography (CESM) versus MRI in the high-risk screening setting: patient preferences and attitudes. Clin Imaging. 2017;42:193–7.
Fallenberg EM, Dromain C, Diekmann F, Renz DM, Amer H, Ingold-Heppner B, et al. Contrast-enhanced spectral mammography: does mammography provide additional clinical benefits or can some radiation exposure be avoided? Breast Cancer Res Treat. 2014;146(2):371–81.
Tennant SL, James JJ, Cornford EJ, Chen Y, Burrell HC, Hamilton LJ, et al. Contrast-enhanced spectral mammography improves diagnostic accuracy in the symptomatic setting. Clin Radiol. 2016;71(11):1148–55.
Iotti V, Ravaioli S, Vacondio R, Coriani C, Caffarri S, Sghedoni R, et al. Contrast-enhanced spectral mammography in neoadjuvant chemotherapy monitoring: a comparison with breast magnetic resonance imaging. Breast Cancer Res. 2017;19(1):106.
Fallenberg EM, Dromain C, Diekmann F, Engelken F, Krohn M, Singh JM, et al. Contrast-enhanced spectral mammography versus MRI: initial results in the detection of breast cancer and assessment of tumour size. Eur Radiol. 2014;24(1):256–64.
Lobbes MB, Lalji UC, Nelemans PJ, Houben I, Smidt ML, Heuts E, et al. The quality of tumor size assessment by contrast-enhanced spectral mammography and the benefit of additional breast MRI. J Cancer. 2015;6(2):144–50.
Patel BK, Gray RJ, Pockaj BA. Potential cost savings of contrast-enhanced digital mammography. AJR Am J Roentgenol. 2017;208(6):W231–W7.
American College of Radiology, ACR Committee on Drugs and Contrast Media ACR manual on contrast media, version 10.3. 2018. https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf
Houben IPL, van Berlo CJLY, Bekers O, Nijssen EC, Lobbes MBI, Wildberger JE. Assessing the risk of contrast-induced nephropathy using a finger stick analysis in recalls from breast screening: the CINFIBS explorative study. Contrast Media Mol Imaging. 2017;2017:5670384.
Snaith B, Harris MA, Shinkins B, Jordaan M, Messenger M, Lewington A. Point-of-care creatinine testing for kidney function measurement prior to contrast-enhanced diagnostic imaging: evaluation of the performance of three systems for clinical utility. Clin Chem Lab Med. 2018;56(8):1269–76.
Patel BK, Garza SA, Eversman S, Lopez-Alvarez Y, Kosiorek H, Pockaj BA. Assessing tumor extent on contrast-enhanced spectral mammography versus full-field digital mammography and ultrasound. Clin Imaging. 2017;46:78–84.
Pfeifer K, Staib L, Arango J, Kirsch J, Arici M, Kappus L, et al. High-fidelity contrast reaction simulation training: performance comparison of faculty, fellows, and residents. J Am Coll Radiol. 2016;13(1):81–7.
Wang CL, Chinnugounder S, Hippe DS, Zaidi S, O’Malley RB, Bhargava P, et al. Comparative effectiveness of hands-on versus computer simulation-based training for contrast media reactions and teamwork skills. J Am Coll Radiol. 2017;14(1):103–10.e3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Phillips, J., Mehta, T.S. (2019). Setting Up a CEM Program. In: Lobbes, M., Jochelson, M. (eds) Contrast-Enhanced Mammography . Springer, Cham. https://doi.org/10.1007/978-3-030-11063-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-11063-5_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-11062-8
Online ISBN: 978-3-030-11063-5
eBook Packages: MedicineMedicine (R0)