Abstract
Aneurysmal subarachnoid hemorrhage (aSAH) remains a significant cause of stroke disability despite gradual reductions in physical morbidity and mortality. Heparin is an effective anti-inflammatory agent and may potentially prevent delayed neurological injury in the days to weeks after the hemorrhage. Various human studies have shown the safety of a continuous infusion of low-dose unfractionated heparin in the setting of subarachnoid hemorrhage as well as its efficacy in minimizing delayed neurological deficits including symptomatic cerebral vasospasm, vasospasm-related infarction, and cognitive dysfunction. Studies have also shown mixed results with low-molecular-weight heparin usage in this patient population. Heparin treatment is not associated with significant hemorrhagic complications; however, vigilance is essential for early detection of heparin-induced thrombocytopenia in order to prevent devastating sequelae. Multicenter randomized controlled trials are necessary for objective characterization of the effects of heparin.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Aneurysmal subarachnoid hemorrhage (aSAH) remains a significant cause of stroke fatality and physical disability, despite some reductions in morbidity and mortality over the past few decades. The risk of life-altering complications in the form of debilitating psychosocial and cognitive impairments remains significant in up to 70% of patients who survive the initial bleed [1, 11]. Verbal and visual memory, language, and executive function are the most commonly impaired cognitive domains [9]. These impairments surface in the days to weeks following aneurysmal repair and have been postulated to be due to cerebral vasospasm, neuroinflammation , non-obstructive hydrocephalus, cerebral microthrombi, cortical spreading depolarization, oxidative damage, neuronal cell death, and white matter loss [3, 12,13,14, 19, 20, 25]. A reported 59% of surviving patients never return to their previous occupation, with an even larger majority experiencing deficits in activities of daily living [1, 7]. No treatment strategies have yet proven the ability to prevent neurocognitive impairments after aSAH.
Unfractionated heparin has been shown to be a promising agent in preventing symptomatic cerebral vasospasm and vasospasm-related infarction in the setting of aneurysmal subarachnoid hemorrhage [16, 17]. In addition to its primary clinical usage as an anticoagulant, heparin binding has been shown to interfere with a significant number of other biological pathways [16]. As a negatively charged glycosaminoglycan, heparin has been shown to be involved in the prevention of neuroinflammation, myelin preservation, and inhibition of apoptosis [18, 23]. Such effects can be attributed to heparin’s high negative charge density and strong affinity to bind positively charged molecules such as plasma proteins, proteins released from platelets, cytokines, chemokines, other small biologically active molecules, as well as endothelial cells themselves [18, 23] . In this manuscript, we briefly review the human studies that demonstrate the effect of heparin on aSAH survivors.
Heparin and Subarachnoid Hemorrhage
Initial human studies investigated the role of enoxaparin (low-molecular-weight fractionated heparin) in aneurysmal SAH with mixed results. Citing cerebral vasospasm as the leading cause of fatalities and physical impairment after subarachnoid hemorrhage, Wurm et al. sought to compare exnoaparin’s abilities to reduce risk of vasospasm compared to placebo [22]. One hundred twenty consecutive patients with aSAH (Hunt-Hess I–III) were included after aneurysm repair and were randomly allocated to either one subcutaneous injection of 20 mg enoxaparin or placebo per day for 21 days following SAH [22], Results of the study revealed marked reduction in vasospasm-related infarction (3.5% vs. 28.3%; p < 0.001), shunt-dependent hydrocephalus (1.8% vs. 16.7% placebo; p = 0.019), and delayed ischemic deficits (DID) (8.8% vs. 66.7% placebo; p < 0.001). At 1-year follow-up, patients in the enoxaparin group had significantly better outcomes than the placebo group, supporting the neuroprotective properties of low-molecular-weight heparin [22].
This trial is in stark contrast to a previously conducted double-blind randomized trial showing no effect of enoxaparin on the outcomes of patients following subarachnoid hemorrhage [15]. One hundred seventy patients with aSAH (WFNS grades I–V) were enrolled within 48 h of aneurysm repair. The main endpoint of the trial was neurological outcome at 3 months and did not show any difference between the placebo group and the enoxaparin group [15]. In addition, there was a slight increase in intracranial hemorrhagic complications with no concomitant improvement in neurological outcome [15].
The conflicting data decreased the overall enthusiasm generated by enoxaparin in the treatment of subarachnoid hemorrhage.
Recently, a retrospective cohort study showed significant benefits of unfractionated heparin (UFH) in Fisher grade 3 aneurysmal subarachnoid hemorrhage patients. Eighty-six consecutive patients post aSAH were included in the study evaluating the effects of a continuous infusion of low-dose intravenous unfractionated heparin (LDIVH) on symptomatic cerebral vasospasm and delayed infarct [16]. All patients were treated with craniotomy and surgical clipping of the ruptured aneurysm at least 12 h prior to administration of LDIVH. Forty-seven percent of patients in the control group had symptomatic cerebral vasospasm as compared to 9% in the heparin group (p = 0.0002). Patients in the heparin group had significantly decreased vasospasm-related CT infarctions as compared to the patients in the control group (0% vs. 21%, p = 0.003; Fig. 1). The study demonstrated the safety and potential significant benefit of LDIVH in patients presenting Fisher grade 3 aSAH.
Adapted from Simard et al. [16]. Vasospasm-related outcomes . Incidence of clinical vasospasm and CT infarctions in the control (CTR) and heparin (HEP) groups. *** p = 0.0002; * p = 0.03
In another retrospective review of 118 patients with Fisher grade 2–4 aSAH, nimodipine compliance was evaluated as a predictor of discharge to home. The patients were divided into three groups: full dosing compliance, one or more doses split to prevent nimodipine-induced hypotension, and missed dosing. Full dosing compliance in patients co-treated with low-dose heparin infusion was found to be associated with the highest odds of discharge to home (75% who received all doses, 67% who received ≥1 split doses, and 37% with ≥1 missed doses (p = 0.003)). This study reinforces the importance of full dosing nimodipine compliance and the potential association with improved disposition outcomes [21].
Bruder et al. conducted a retrospective review of 718 patients receiving treatment for aSAH from 1999 to 2014 to evaluate the neuroprotective functions of intravenous unfractionated heparin. One hundred ninety-seven patients in this cohort were treated with a continuous infusion of unfractionated heparin following endovascular coiling of the aneurysm. The rate of cerebral vasospasm was significantly reduced in the heparin group compared with the control group (14.2% vs. 25.4%; p = 0.05) [2]. Duration of treatment was included as an independent variable in heparin treatment. The neuroprotective effect of heparin was enhanced when the treatment was continued for 7 days, but was not significant. About 66.8% of patients who received therapeutic dosage of heparin post aSAH achieved good modified Rankin scores (0–2) at 6 months [2]. In combination with the findings from Simard et al., heparin was proven once again to be safe and potentially efficacious in the treatment of aSAH with a secured aneurysm.
Furthermore, James et al. evaluated a retrospective cohort of 47 aSAH patients for cognitive outcomes based on standard of care therapy versus LDIVH. The Montreal Cognitive Assessment (MoCA) test was used to evaluate the cognitive changes in aSAH patients treated with the LDIVH protocol vs. controls. Patients in the heparin-treated group had a mean MoCA score of 26.4, while those in the control group scored 22.7 (p = 0.013, Fig. 2). Serious cognitive impairment did not occur in the heparin-treated cohort as opposed to the control group (0% vs. 32%; p = 0.008). In their analysis, the authors showed that LDIVH was associated with a positive influence on MoCA score, while fevers and anterior communicating artery aneurysms were associated with negative influences on MoCA scores [8].
Used with permission from the Journal of Neurosurgery [8]. Box and whiskers plot showing the distribution of MoCA scores for each treatment group. Solid horizontal line, median; dashed horizontal line, mean. Note the tight packing and decreased variance of MoCA scores in the LDIVH treatment group. Asterisk denotes significance between the two groups (p = 0.013)
Table 1 is a summary of the main findings in all the human studies of heparin in aSAH.
Complications of Heparin
Hydrocephalus is often considered a delayed neurological deficit associated with aneurysmal subarachnoid hemorrhage. A ventriculostomy drain and a shunt for CSF diversion are the two commonly accepted treatment modalities for hydrocephalus. Ventriculostomy-related hemorrhages have always been a concern in patients placed on IV heparin following aSAH. A retrospective review including 241 patients over a 13-year period was conducted to study the risk of hemorrhage and DVT for ventriculostomy patients on heparin prophylaxis [24]. Hemorrhages were labeled as major or minor depending on the size and mass effect, while DVT incidences were also noted. Among the 53 patients on prophylactic IV heparin, three experienced minor hemorrhages with no incidence of major hemorrhage. This study provided more conclusive evidence that hemorrhages related to IV heparin are rare and minor [24]. This was corroborated by the study by Manoel et al., which showed that DVT chemoprophylaxis does not increase the risk of intracranial hemorrhage in the setting of aSAH [10]. However, the authors cautioned against the usage of IV heparin with dual antiplatelet therapy due to significant concerns of an induced bleeding diathesis [10].
In addition to hemorrhagic complications, heparin-induced thrombocytopenia is a potentially fatal complication associated with a significant decrease in platelet count following multiple day exposure to intravenous heparin [5]. The incidence of heparin-induced thrombocytopenia type II (HIT II) ranges between 0.2 and 3% and has been reported to raise the risk of thrombotic events in patients with this autoimmune disorder [4]. HIT II is characterized by antibodies directed against complexes that form between heparin or other anionic mucopolysaccharides and platelet factor 4, a heparin-binding protein released by activated platelets [6]. Despite a higher incidence of HIT in patients with cerebrovascular neurologic disease, careful daily monitoring of platelet count allows early detection and treatment of HIT with cessation of the heparin infusion [6].
Conclusion
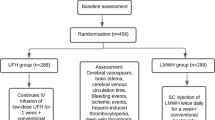
Intravenous unfractionated heparin is a neuroprotective agent in aSAH with proven safety and effectiveness in humans. Multicenter randomized controlled trials are needed to definitively demonstrate the various neuroprotective effects of heparin in patients with aSAH. The Aneurysmal Subarachnoid Hemorrhage Trial Randomizing Heparin (ASTROH) is a phase 2 randomized multicenter trial with blinded adjudication of outcomes and is currently enrolling subjects to evaluate LDIVH in aSAH patients (NCT02501434). Additional evidence supporting the safety and effectiveness of LDIVH in aSAH may help direct future phase 3 studies that could potentially prove heparin is beneficial allowing its acceptance as a standard treatment for aneurysmal subarachnoid hemorrhage survivors.
References
Al-Khindi T, Macdonald RL, Schweizer TA. Cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Stroke. 2010;41:e519–36.
Bruder M, Won S-YY, Kashefiolasl S, Wagner M, Brawanski N, Dinc N, Seifert V, Konczalla J. Effect of heparin on secondary brain injury in patients with subarachnoid hemorrhage: an additional ‘H’ therapy in vasospasm treatment. J Neurointerv Surg. 2017;9:659–63.
Crowley MG, Liska MG, Borlongan CV. Stem cell therapy for sequestering neuroinflammation in traumatic brain injury: an update on exosome-targeting to the spleen. J Neurosurg Sci. 2017;61:291–302.
Girolami B, Prandoni P, Stefani PM, Tanduo C, Sabbion P, Eichler P, Ramon R, Baggio G, Fabris F, Girolami A. The incidence of heparin-induced thrombocytopenia in hospitalized medical patients treated with subcutaneous unfractionated heparin: a prospective cohort study. Blood. 2003;101:2955–9.
Hacker RI, Ritter G, Nelson C, Knobel D, Gupta R, Hopkins K, Marini CP, Barrera R. Subcutaneous heparin does not increase postoperative complications in neurosurgical patients: an institutional experience. J Crit Care. 2012;27:250–4.
Harbrecht U, Bastians B, Kredteck A, Hanfland P, Klockgether T, Pohl C. Heparin-induced thrombocytopenia in neurologic disease treated with unfractionated heparin. Neurology. 2004;62:657–9.
Hellawell DJ, Taylor R, Pentland B. Persisting symptoms and carers’ views of outcome after subarachnoid haemorrhage. Clin Rehabil. 1999;13:333–40.
James RF, Khattar NK, Aljuboori ZS, Page P, Shao EY, Carter LM, Meyer KS, Daniels MJ, Craycroft J, Gaughen JR Jr, Chaudry MI, Rai SN, Everhart DE, Simard JM. Continuous infusion of low-dose unfractionated heparin after aneurysmal subarachnoid hemorrhage: a preliminary study of cognitive outcomes. J Neurosurg. 2018;11:1–8. https://doi.org/10.317.1/2017.11.JNS17894 [Epub ahead of print].
Kreiter KT, Copeland D, Bernardini GL, Bates JE, Peery S, Claassen J, Du YE, Stern Y, Connolly ES, Mayer SA. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke. 2002;33:200–8.
Manoel AL, Turkel-Parrella D, Germans M, Kouzmina E, Almendra Pda S, Marotta T, Spears J, Abrahamson S. Safety of early pharmacological thromboprophylaxis after subarachnoid hemorrhage. Can J Neurol Sci. 2014;41:554–61.
Mavaddat N, Sahakian BJ, Hutchinson PJ, Kirkpatrick PJ. Cognition following subarachnoid hemorrhage from anterior communicating artery aneurysm: relation to timing of surgery. J Neurosurg. 1999;91:402–7.
Parra A, Kreiter KT, Williams S, Sciacca R, Mack WJ, Naidech AM, Commichau CS, Fitzsimmons BF, Janjua N, Mayer SA, Connolly ES Jr. Effect of prior statin use on functional outcome and delayed vasospasm after acute aneurysmal subarachnoid hemorrhage: a matched controlled cohort study. Neurosurgery. 2005;56:476–84; discussion 476–84.
Provencio JJ, Vora N. Subarachnoid hemorrhage and inflammation: bench to bedside and back. Semin Neurol. 2005;25:435–44.
Pyne-Geithman GJ, Caudell DN, Prakash P, Clark JF. Glutathione peroxidase and subarachnoid hemorrhage: implications for the role of oxidative stress in cerebral vasospasm. Neurol Res. 2009;31:195–9.
Siironen J, Juvela S, Varis J, Porras M, Poussa K, Ilveskero S, Hernesniemi J, Lassila R. No effect of enoxaparin on outcome of aneurysmal subarachnoid hemorrhage: a randomized, double-blind, placebo-controlled clinical trial. J Neurosurg. 2003;99:953–9.
Simard JM, Aldrich EF, Schreibman D, James RF, Polifka A, Beaty N. Low-dose intravenous heparin infusion in patients with aneurysmal subarachnoid hemorrhage: a preliminary assessment. J Neurosurg. 2013;119:1611–9.
Simard JM, Schreibman D, Aldrich EF, Stallmeyer B, Le B, James RF, Beaty N. Unfractionated heparin: multitargeted therapy for delayed neurological deficits induced by subarachnoid hemorrhage. Neurocrit Care. 2010;13:439–49.
Simard JM, Tosun C, Ivanova S, Kurland DB, Hong C, Radecki L, Gisriel C, Mehta R, Schreibman D, Gerzanich V. Heparin reduces neuroinflammation and transsynaptic neuronal apoptosis in a model of subarachnoid hemorrhage. Transl Stroke Res. 2012;3:155–65.
Stein SC, Levine JM, Nagpal S, LeRoux PD. Vasospasm as the sole cause of cerebral ischemia: how strong is the evidence? Neurosurg Focus. 2006;21:E2.
Vergouwen MD, Vermeulen M, Coert BA, Stroes ES, Roos YB. Microthrombosis after aneurysmal subarachnoid hemorrhage: an additional explanation for delayed cerebral ischemia. J Cereb Blood Flow Metab. 2008;28:1761–70.
Wessell A, Kole MJ, Badjatia N, Parikh G, Albrecht JS, Schreibman DL, Simard JM. High compliance with scheduled nimodipine is associated with better outcome in aneurysmal subarachnoid hemorrhage patients cotreated with heparin infusion. Front Neurol. 2017;8:268.
Wurm G, Tomancok B, Nussbaumer K, Adelwohrer C, Holl K. Reduction of ischemic sequelae following spontaneous subarachnoid hemorrhage: a double-blind, randomized comparison of enoxaparin versus placebo. Clin Neurol Neurosurg. 2004;106:97–103.
Young E. The anti-inflammatory effects of heparin and related compounds. Thromb Res. 2008;122:743–52.
Zachariah J, Snyder KA, Graffeo CS, Khanal DR, Lanzino G, Wijdicks EF, Rabinstein AA. Risk of ventriculostomy-associated hemorrhage in patients with aneurysmal subarachnoid hemorrhage treated with anticoagulant thromboprophylaxis. Neurocrit Care. 2016;25:224–9.
Zhang ZD, Macdonald RL. Contribution of the remodeling response to cerebral vasospasm. Neurol Res. 2006;28:713–20.
Conflict of Interest
RFJ is the study chair for ASTROH, a phase 2 clinical trial evaluating heparin treatment in aneurysmal subarachnoid hemorrhage. We delare that we have no other conflicts of interest with the contents of this manuscript.
Source of Funding: None.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Khattar, N.K., Bak, E., White, A.C., James, R.F. (2020). Heparin Treatment in Aneurysmal Subarachnoid Hemorrhage: A Review of Human Studies. In: Martin, R., Boling, W., Chen, G., Zhang, J. (eds) Subarachnoid Hemorrhage. Acta Neurochirurgica Supplement, vol 127. Springer, Cham. https://doi.org/10.1007/978-3-030-04615-6_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-04615-6_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04614-9
Online ISBN: 978-3-030-04615-6
eBook Packages: MedicineMedicine (R0)