Abstract
Aneurysmal subarachnoid hemorrhage (SAH) is associated with numerous “delayed neurological deficits” (DNDs) that have been attributed to multiple pathophysiological mechanisms, including ischemia, microthrombosis, free radical damage, inflammation, and vascular remodeling. To date, effective prophylactic therapy for SAH-induced DNDs has been elusive, due perhaps to the multiplicity of mechanisms involved that render typical, single-agent therapy seemingly futile. We hypothesized that heparin, which has multiple underappreciated salutary effects, might be useful as a multitargeted prophylactic agent against SAH-induced DNDs. We performed a comprehensive review of the literature to evaluate the potential utility of heparin in targeting the multiple pathophysiological mechanisms that have been identified as contributing to SAH-induced DNDs. Our literature review revealed that unfractionated heparin can potentially antagonize essentially all of the pathophysiological mechanisms known to be activated following SAH. Heparin binds >100 proteins, including plasma proteins, proteins released from platelets, cytokines, and chemokines. Also, heparin complexes with oxyhemoglobin, blocks the activity of free radicals including reactive oxygen species, antagonizes endothelin-mediated vasoconstriction, smooth muscle depolarization, and inflammatory, growth and fibrogenic responses. Our review suggests that the use of prophylactic heparin following SAH may warrant formal study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aneurysmal subarachnoid hemorrhage (SAH) is associated with numerous adverse sequelae [1, 2]. Patients who survive the initial hemorrhage are at high risk for delayed secondary brain injury, including cerebral infarction, neuronal cell death, white matter abnormalities, and hydrocephalus, resulting in focal neurological deficits, cortical dysfunction and long-term cognitive and psychosocial deficits. Collectively, these abnormalities are referred to as SAH-induced “delayed neurological deficits” (DNDs).
Several distinct pathophysiological mechanisms are known to play important causative roles in SAH-induced DNDs, including ischemia, microthrombosis, free radical damage, inflammation, and vascular remodeling [3–12]. Cerebral infarction is strongly associated with poor outcome after SAH, symptomatic vasospasm is the most important factor predisposing to infarction [13], and dysregulation of endothelin signaling is currently viewed as a critical antecedent to vasospasm [14–16]. However, specific block of endothelin pathways, albeit effective at reducing vasoconstriction, does not necessarily improve patient outcome [3, 17], pointing to crucial roles for pathophysiological processes other than vasoconstriction. Microthrombi may contribute to ischemic damage, but non-ischemic mechanisms also play critical roles. Free radical injury induced by blood products is particularly damaging to white matter, and the inflammatory response provoked by blood products contributes not only to vasospasm, but to edema, cell death and generalized cortical dysfunction. To date, effective prophylactic therapy for SAH-induced DNDs has been elusive [18, 19], due perhaps to the multiplicity of mechanisms involved that render typical, single-agent therapy seemingly futile.
Heparin is a member of a family of polyanionic polysaccharides called glycosaminoglycans, composed of hexuronic acid and d-glucosamine residues joined by glycosidic linkages [20]. Unfractionated heparin (UH) is a heterogeneous mixture of polysaccharide chains of varying lengths resulting in a range of molecular weights from 3 to 30 kDa, whereas low molecular weight heparin (LMWH) ranges from 3 to 6 kDa [21]. Heparin (always used here to refer to UH) has the highest negative charge density of any known biological molecule and as a result, has a high propensity to bind to positively charged proteins and surfaces. More than 100 heparin-binding proteins have been identified [22], with the growing list including numerous plasma proteins, proteins released from platelets, cytokines, chemokines, and other small biologically active molecules, as well as endothelial cells themselves [23–26]. Although clinically utilized almost exclusively for its anticoagulant properties, heparin binding can interrupt numerous other biological pathways [27]. Among its wide-ranging effects, heparin complexes with free hemoglobin itself, including oxyhemoglobin [28], it blocks the activity of free radicals (FR) including reactive oxygen species (ROS) [29], it antagonizes endothelin-mediated vasoconstriction [30–32], it binds to several cytokines and all chemokines, thereby imparting potent anti-inflammatory effects [22, 33, 34], and it binds to several growth factors, thereby imparting anti-mitogenic [35–37] and anti-fibrotic [38] effects. To our knowledge, no other compound exhibits such a broad diversity of biological effects that seem so intimately relevant to mechanisms implicated in SAH-induced DNDs. The very multiplicity of mechanisms targeted by heparin suggests that it may be particularly attractive as multitargeted prophylactic agent to ameliorate the wide-ranging abnormalities induced by SAH.
Several excellent reviews on the molecular and cellular mechanisms that are activated following SAH have been published recently [4, 12, 39–41], but our purpose here is different. The present review focuses specifically on heparin, and links individual cellular and molecular mechanisms activated by SAH directly to known actions of heparin. Here, we demonstrate how heparin might serve as an effective multitargeted prophylactic agent to combat SAH-induced DNDs.
Review
Oxyhemoglobin (OxyHb)
There is considerable evidence implicating a component of erythrocyte lysate (hemolysate), especially oxyhemoglobin (OxyHb) or hemoglobin degradation products, in the etiology of vasospasm [42, 43]. The release of OxyHb from lysing erythrocytes in the subarachnoid space is believed to play a key role in vasospasm. OxyHb is present in high concentrations in CSF during the time of vasospasm. Erythrocytes are the only component of blood required for vasospasm to develop, and the most vasoactive substance within erythrocytes is OxyHb. OxyHb can act by a variety of pathways over a prolonged period of time to produce arterial narrowing and ultrastructural damage to arteries resembling those encountered after SAH. OxyHb has multiple actions, including scavenging nitric oxide (NO), inhibiting endothelium-dependent relaxation, generating ROS, activating the tyrosine kinase–mitogen-activated kinase (MAPK) pathway, releasing vasoactive eicosanoids and endothelin from the arterial wall, producing bilirubin and lipid peroxides, and causing damage to perivascular nerves.
In this context, an intriguing target of heparin binding is hemoglobin itself [28]. Both OxyHb and deoxyhemoglobin are strongly bound by heparin with a stoichiometry of binding (polyanion/tetrameric hemoglobin) that is less than unity. The overall affinity of hemoglobin for different anions is greater as the charge on the anion increases, and is maximal for polyanions such as heparin, which possesses the highest negative charge density of any biological molecule. To our knowledge, the hypothesis that heparin reduces the toxicity of OxyHb (or some other component of hemolysate) in the context of SAH has not been specifically tested. The published experiment that comes closest to addressing this question involved an experimental model of SAH in which intracisternal heparin injection was shown to significantly reduce vascular wall changes [44]. Because OxyHb as well as hemolysate are themselves toxic when injected intracisternally [45], it would be interesting to determine whether their toxicity is neutralized when they are mixed with various amounts of heparin.
Free Radicals (FR) Including Reactive Oxygen Species (ROS)
Considerable evidence suggests that FR-mediated mechanisms contribute to vasospasm after SAH [46, 47]. As noted above, OxyHb is believed to be the, or one of the, principle spasmogen(s) responsible for vasospasm. OxyHb may cause vasospasm by generating oxygen-derived FR in the subarachnoid space. Superoxide radical is formed during the auto-oxidation of OxyHb. If iron is released from the heme moiety, superoxide can generate the highly injurious hydroxyl radical. Lipid peroxides are found in elevated concentrations in CSF during vasospasm in animals and humans. There is a progressive increase in thiobarbituric acid-reactive substances with time after SAH. The prevention of vasospasm by compounds that inhibit lipid peroxidation (21-aminosteroids such as tirilazad), that scavenge FR (nicaraven) or that chelate iron (deferroxamine) supports a role for FR-mediated processes in vasospasm. One or more of several mechanisms may be downstream effectors of FR reactions. ROS have direct vasocontractile effects on cerebral arteries in vitro, but different ROS have different contractile characteristics [48]. Peroxidation of membrane lipids occurs and is proposed to be an important antecedent leading to vasospasm. Alternatively, since FR act on bilirubin, biliverdin, and possibly heme to produce BOXes (Bilirubin OXidized Products), bilirubin oxidation products may act on vascular smooth muscle cells to produce chronic vasoconstriction and vasospasm combined with a vasculopathy due to smooth muscle cell injury [7, 49].
Despite considerable evidence, it has not been fully appreciated that heparin is a potent inhibitor of FR activity [50]. Heparin decreases FR release by activated neutrophils and mitigates FR effects in vivo. It alleviates FR production, and significantly decreases hydrogen ion accumulation. Heparinase pretreatment markedly increases FR release by endothelial cells. Small amounts of heparin enhance the antioxidant activity of superoxide dismutase. Heparin sulfate proteoglycans tether antioxidant superoxide dismutase to cell surfaces and so contribute to the inhibition of FR tissue injury. Certain glycosaminoglycans, including heparin, have features that allow them to act as FR sinks. Heparin markedly reduces FR release in vivo after ischemia/reperfusion and protects endothelial cells from FR injury. Heparin scavenges FR released by the action of myeloperoxidase and it binds and sequesters Fe2+ ions and decreases peroxidation of unsaturated fatty acids in the presence of Fe2+. Metal chelators like heparin have anti-oxidant activity and block activation of nuclear factor κB (NF-κB). Overall, considerable evidence indicates that heparin-like activity is part of the organism’s anti-oxidant defenses, implying that heparin therapy may reduce the harmful actions of FR (see [50] for original citations).
Endothelin (ET)
Several highly potent vasoactive compounds have been identified in the CSF and plasma of patients after SAH. Among these, the endothelins (ETs), especially endothelin-1 (ET-1), are believed to play a critical role in SAH-induced DNDs [15, 16]. ET-1, acting by way of endothelin receptor type A on vascular smooth muscle cells (VSMC), is one of the most potent vasoconstrictors known. Acting in concert with other vasoactive factors, ETs may contribute substantially to the disturbed equilibrium between constriction and relaxation that typifies vascular responses following SAH. Endothelin concentrations in plasma or CSF correlate with delayed cerebral ischemia and vasospasm after SAH, with the highest levels of ET predicting cerebral ischemia and symptomatic vasospasm [51, 52]. The potential involvement of ET in cerebral vasospasm following SAH has triggered considerable interest in designing therapeutic strategies to inhibit biological effects of ET. Major approaches have included: (i) reducing the levels of circulating ET-1 by specific anti-ET-1 antibodies, (ii) antagonizing ET receptors, and (iii) suppressing the biosynthesis of ET-1 using inhibitors of endothelin-converting enzymes (ECEs) [14, 53]. A number of experimental studies demonstrate the preventive or therapeutic potential of ET receptor antagonists in the context of SAH [54, 55]. Importantly, it was recently found that specific block of endothelin pathways, albeit effective at reducing vasoconstriction, may not improve patient outcome post-SAH [3, 17].
ET-1 has a number of effects other than vasoconstriction. It can also cause vasodilation via release of nitric oxide (NO) and prostacyclin. More importantly, ET-1 plays a role in fibrosis, endothelial and smooth muscle proliferation, and inflammation. It increases the contractile potency of other vasoconstrictors such as norepinephrine, serotonin, and angiotensin I. It contributes to vascular inflammation by stimulating neutrophil adhesion, platelet aggregation, and smooth muscle proliferation [15, 16].
Heparin interferes with ET-1 and its downstream effects at multiple levels. Heparin downregulates transcription of the ET-1 gene in endothelial cells, with ET-1 mRNA expression significantly suppressed by heparin in a dose-dependent manner [31, 32, 56, 57].
ET-1-induced vasoconstriction, which involves a complex signaling pathway, is inhibited by heparin. Activation of the endothelin type A receptor by ET-1 results in transactivation of the epidermal growth factor receptor (EGFR), which is required for a full constrictive response to ET-1. Importantly, the specific ligand involved in EGFR transactivation has been identified as heparin-binding epidermal growth factor (HB-EGF) [30]. Thus, vasoconstriction induced by ET-1 is antagonized by heparin, which neutralizes activity of HB-EGF. Notably, HB-EGF−/− mice are available [30], but to our knowledge, have not been assessed for their susceptibility to SAH-induced DNDs.
Heparin also antagonizes ET-1 actions other than vasoconstriction. Heparin significantly suppresses ET-1-induced increases in intracellular calcium and inositol 1,4,5-trisphosphate levels in cultured vascular smooth muscle cells in a dose-dependent manner, and it inhibits ET-1 release from cultured endothelial cells [32]. Constitutive ET-1 overexpression (as may occur in an inflammatory environment) promotes VSMC proliferation via an external autocrine mechanism [58]. Heparin inhibits sustained activity of MAPK kinase-1 and prevents DNA synthesis induced by endothelin-1 [59].
Potassium Channels
Apart from ET-1, vasoconstriction associated with vasospasm may be due to altered function of potassium channels [60]. In VSMC, cytoplasmic calcium concentration is a critical determinant of contractile state, and key mediators determining calcium influx (and hence intracellular calcium concentration) are voltage-dependent calcium channels (L-, R-, T-types). As implied by the name, “voltage-dependent” calcium channel, a critical regulator of the activity of these channels is the membrane potential of the cell, which is determined largely by potassium channels.
Several types of K+ channels are expressed in cerebral vascular smooth muscle, including several shown to be downregulated in the context of experimental SAH [60, 61]. Germane to the present discussion, KV channels are inhibited by heparin due to regulation by HB-EGF which, as mentioned above, is a necessary intermediate in ET-1-mediated vasoconstriction. In an elegant series of experiments, Wellman and colleagues [62, 63] showed that OxyHb suppresses KV currents in cerebral vascular smooth muscle cells, probably due to channel endocytosis, and that this effect is mediated by HB-EGF. They showed that OxyHb activates matrix-metalloproteinase, which in turn cleaves pro-HB-EGF, releasing if from the membrane and allowing it to bind to its cognate receptor, EGFR. This complex mechanism of K+ channel down-regulation is believed to be responsible for OxyHb-mediated membrane depolarization, calcium channel activation and vasoconstriction that are the hallmarks of the smooth muscle pathophysiology following SAH.
Growth Factors
Cerebral blood vessels affected by vasospasm exhibit structural changes consistent with the actions of vascular mitogens (growth factors) [64–66]. Smooth muscle and myofibroblast proliferation, as well as cellular necrosis and remodeling, are common features of vasospastic segments. Intimal hyperplasia, as well as collagen deposition and fibrosis, have also been extensively described. These “late” arterial wall changes are not believed to be responsible for vasospasm per se [67, 68]. However, it is possible that early phenotypic changes in VSMC that are induced by growth factors contribute to reduced cell polarization, altered response to vasodilatory agents and decreased vessel compliance after SAH [69].
There is growing appreciation that the MAPK (ERK1, ERK2) cascade may play an important role in cerebral vasospasm [70–73]. MAPK is a family of serine/threonine protein kinases involved in cell growth, transformation, and proliferation through activation of transcription factors and target genes. It also plays an important role in prolonged smooth muscle contraction by phosphorylating caldesmon, which is a thin filament-associated protein that inhibits α-actin. Tyrosine kinase and MAPK cascades play a role in hemolysate-induced contraction of rabbit cerebral arteries, independent of intracellular Ca2+ concentration [70].
The MAPK cascade is upregulated by several mechanisms relevant to SAH, including FR such as superoxide anion, inflammatory cytokines such as TNFα, and by one or more growth factors, including: (i) HB-EGF [74], (ii) platelet-derived growth factors [75], and (iii) thrombin [73], each of which deserves brief review.
HB-EGF, the heparin-binding member of the EGF family implicated in ET-1-mediated vasoconstriction and in KV channel down-regulation (see above), has also been implicated in vascular pathological processes, including cerebral ischemia and VSMC hyperplasia [76–78].
Platelet-derived growth factors have also been implicated in SAH-induced vessel wall changes. As reviewed in Borel et al. [79], coagulation of subarachnoid blood activates platelets, which release potent growth factors, including platelet-derived growth factor-AB (PDGF-AB), transforming growth factor-β1 (TGF-β1), and vascular endothelial growth factor (VEGF). The PDGFs and TGF-β are potent mitogens for smooth muscle cells in the vascular media and fibroblasts in the adventitia, whereas VEGF stimulates proliferation of vascular endothelium. Previous studies have shown that PDGFs are increased in the CSF of patients with SAH (see [79, 80] for additional citations).
Thrombin has also been implicated in SAH-induced vessel wall changes. Subarachnoid clot releases thrombin, which can act as a growth factor. As reviewed in Zhang et al. [81] and in Tsurutani et al. [82], once bleeding into the subarachnoid space occurs, thrombin is activated rapidly and remains at a high level because a firm, persistent fibrin network is produced through activation of the coagulation system in the subarachnoid space. CSF thrombin is only minimally inactivated by the antithrombin-III found in circulating blood and by the thrombomodulin found in vascular endothelial cells. Post-SAH CSF thrombin activity is correlated with the persistence of blood and development of vasospasm. After SAH, levels of thrombin-AT-III complex and prothrombin fragment F1 + 2, both molecular markers of CSF thrombin activation, are elevated and these levels correlate well with both the clinical severity at the onset of SAH and the occurrence of cerebral vasospasm (see [82] for additional citations).
Heparin suppresses phenotypic changes of VSMC associated with proliferation in vitro, prevents intimal hyperplasia after arterial injury in vivo [59, 83], and inhibits growth factors involved in vessel wall changes post-SAH. As implied by its name, heparin is a potent inhibitor of HB-EGF and thus blocks HB-EGF-mediated VSMC hyperplasia [74, 84]. Moreover, heparin blockade of thrombin-induced VSMC migration involves inhibition of EGFR transactivation by HB-EGF-like growth factor [37, 85, 86]. Heparin is a potent modulator of receptor binding of growth factors including fibroblast growth factor (FGF) VEGF and PDGF [87–89], and heparin inhibits thrombin-induced mitogen-activated protein kinase signaling in VSMC [59]. Localized release of perivascular heparin inhibits intimal proliferation after endothelial injury without systemic anticoagulation [86]. Heparin reduces proliferative angiopathy following subarachnoid hemorrhage in cats [90]. The preventive effect of intracisternal heparin regarding proliferative angiopathy after experimental SAH in rats [44] was mentioned above.
Chemokines, Cytokines
As detailed in the excellent reviews by Dhar and Diringer [91] and by Provencio and Vora [5], activation of a systemic immune response after SAH is frequently manifested by elevated levels of circulating cytokines, the major effectors of systemic inflammation. The clinical manifestations of this process have been termed the Systemic Inflammatory Response Syndrome (SIRS), a constellation of findings originally described in association with sepsis. SIRS is characterized by elevated heart rate, respiratory rate, temperature, and leukocyte count. It reflects a systemic process associated with endothelial activation and dysfunction that predisposes to altered tissue perfusion, organ failure, and worse outcome. This host response also includes activation of complement and coagulation cascades, with the potential for thrombosis and impaired microcirculatory flow. High levels of catecholamines are released after SAH and are known to correlate with extra-cerebral organ dysfunction including myocardial stunning, neurogenic pulmonary edema and activation of a systemic immune response. SIRS is seen in most patients with SAH, and is associated with extra-cerebral organ dysfunction and worse outcome. Its components, such as fever and leukocytosis, have long been associated with adverse events after SAH.
SIRS is associated with vasospasm [92]. There is growing recognition that inflammation, both local (neuroinflammation) and systemic, plays an important role in the pathogenesis of vasospasm after SAH [93–98]. Infiltrates of inflammatory cells are seen in the walls of vasospastic arteries. Levels of several important proinflammatory proteins such as ICAM-1, VCAM-1, L-selectin, and E-selectin are elevated after SAH compared with control patients. Levels and time course of E-selectin, a protein involved in leukocyte rolling prior to diapedesis, is associated with moderate to severe vasospasm. In addition, IL-6, IL-β, and TNFα are increased in SAH and are associated with poor outcome. Agents that block these inflammatory cascades, such as corticosteroids and non-steroidal anti-inflammatory agents, may reduce experimental vasospasm. Overall, it is likely that inflammatory activation places patients at higher risk for development of DNDs, both ischemic and otherwise (see [5, 91] for original citations).
Apart from vasospasm, neuroinflammation is also closely linked to deterioration of higher cortical function including memory [99–102]. Cognitive dysfunction and memory deficits are observed following many inflammatory states, including infection, traumatic brain injury, normal aging, and Alzheimer’s disease. Similarly, cognitive dysfunction and memory deficits are very common following SAH, leading to life-altering psychosocial deficits in patients with otherwise “favorable” outcomes [103–105]. Although frequently attributed to ischemia, other mechanisms, especially neuroinflammation, are likely to play an important role, since even SAH patients without vasospasm frequently suffer from these sequelae.
Heparin possesses potent anti-inflammatory and immunomodulatory activities [22, 33, 34]. In various clinical settings involving high-risk patients, heparin can reduce the inflammatory response, lower oxidative stress, and help to ameliorate clinical outcome [106–109]. In patients as well as in experimental models of ischemia, heparin reduces inflammatory responses and is positively associated with early recovery [110, 111].
Anti-inflammatory effects of heparin are mediated through one or more of several mechanisms (Table 1). Heparin may exert its anti-inflammatory effects through the transcription factor, NF-κB [112]. Once bound and/or internalized into the cytoplasm, heparin can bind electrostatically to the positively charged nuclear localization sequence of NF-κB and prevent it from translocating to the nucleus. Inflammation is associated with the coordinated action of a series of cytokine and adhesion molecule genes. Regulation of these genes involves NF-κB, a ubiquitous inducible transcription factor. NF-κB is activated by a vast number of agents including cytokines, growth factors, and FR including ROS generated after SAH. The genes regulated by NF-κB are diverse but include those that transcriptionally promote expression of many inflammatory and immune response genes including ICAM-1, L- and P-selectins, and interleukin-6 and 8. In addition, the pro-inflammatory cytokine best recognized for activating NF-κB, TNFα, induces profound alterations in endothelial cell phenotype, including upregulation of expression of ET-1 [113, 114], which as reviewed above, has been strongly implicated in SAH-induced DNDs.
Anti-inflammatory effects of heparin also result from its ability to compete for binding with numerous pro-inflammatory cytokines and chemokines, and thereby inhibit their function [115–117]. Chemokines are a superfamily of small, heparin-binding cytokines that induce directed migration of various types of leukocytes through interactions with a group of seven-transmembrane G protein-coupled receptors. At present, over 40 members have been identified in humans. Chemokines are potent attractants for leukocytes such as neutrophils and monocytes, and are thus important mediators of acute and chronic inflammatory responses [116, 117]. The continuous expression of chemokines is associated with chronic inflammation [115, 118] of the sort seen after SAH.
The underlying mechanism for the anti-inflammatory effect of heparin involving cytokines and chemokines is that heparin, a soluble glycosaminoglycan (GAG), has a structure and biological activities that are similar to those of cell-surface GAG such as heparan sulfate, integral components of the extracellular matrix, cell and basement membranes. GAGs play an important role in immune and inflammatory responses. During inflammation, the electrostatic interactions of membrane-associated GAG to cytokines and chemokines generally enhance their functions and stability, promoting localization of these molecules onto the extracellular matrix or cell membranes at specific anatomical sites. Binding of cytokine to GAGs is important for augmentation of specific receptor activity and protection from proteolytic inactivation. Additionally, because they immobilize and oligomerize chemokines on endothelial surfaces, GAGs facilitate the formation of concentration gradients and thereby promote leukocyte migration. Binding of cytokine or chemokine to GAG also may cause oligomerization or conformational changes of the ligand, which influence interactions with the specific receptor. Notably, ligands bound to soluble GAG such as heparin may not be accessible for binding to their cognate receptors because of electrostatic repulsion between mutually acidic molecules. These complex interactions between membrane-bound and circulating factors determine the ability of heparin to modulate or inhibit immune responses (see [119] for original citations).
Heparin in Patients with SAH
Having reviewed the various pathophysiological mechanisms induced by SAH that may be susceptible to blockade by heparin, we now examine the few reports available that address the potential value of heparin in managing patients with SAH. Unfortunately, the available data are too sparse and too diverse in nature to permit a proper meta-analysis.
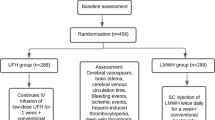
Administration of heparin has been advocated to reduce complications of SAH [120, 121], based on the hypothesis that microemboli are an important cause of ischemic injury following SAH [8, 9]. In support of this hypothesis, an anticoagulating dose of heparin was reported to reduce ischemic events in patients with SAH who were undergoing gradual carotid ligation [122, 123]. In a related finding, the anticoagulation of patients with SAH using low molecular weight heparin (LMWH) (Enoxaparin) was found in one study to significantly reduce vasospasm [124], although this was not confirmed by a second group of investigators [125, 126]. Discrepant findings with LMWH may reflect the possibility that some other mechanism reviewed above that is targeted by unfractionated heparin (and not by LMWH), may be more important that microemboli.
Unfractionated vs. Low Molecular Weight Heparin
There is considerable evidence to support the concept that the biological effects of unfractionated heparin are not reproduced by LMWH. Different molecular weight fractions have different effects on various biological systems. Heparin inhibition of endothelial cell proliferation and organization is dependent on molecular weight in a manner that differs from that required for anticoagulant activity [127]. The binding of unfractionated heparin to thrombin-activated endothelial cells is significantly greater than the binding of LMWH [128], suggesting that unfractionated heparin would be more effective in limiting inflammatory responses involving endothelial surfaces [33]. P- and L-selectin binding is inhibited by unfractionated heparin at concentrations 12–50-fold lower than those recommended for effective anticoagulation in vivo, with LMWHs being much poorer inhibitors [129]. Similarly, the antiproliferative activity of heparin on smooth muscle is maximal in its high molecular weight component [130]. LMWHs have lower affinities than unfractionated heparin for all cell receptors studied and are less likely to exert their effects through cellular interactions [131, 132]. Rats subjected to temporary focal cerebral ischemia and that received unfractionated heparin show significantly better outcomes compared to animals receiving an equivalent dose of LMWH [133]. Such data suggest that the mixed reports of efficacy of LMWH on SAH-induced DNDs [124–126] may be related to the absence of crucial high molecular weight components that are present only in unfractionated heparin.
Manner of Administration of Heparin
The manner of administration of heparin may play an important role in efficacy. Evidence gathered in clinical trials with LMWH or UH given subcutaneously at low or moderate doses to patients with acute stroke is believed to be a poor predictor of potentially beneficial effects of UH administered IV on a weight-adjusted basis [134]. (This opinion is reinforced by the fact that the primary reason that most clinicians use early intravenous anticoagulation is to prevent early stroke recurrence, not to improve outcome after stroke [135]). Animal studies indicate that, when heparin is used to target growth factors (intimal hyperplasia), its effects are actually adverse when it is administered twice daily subcutaneously, whereas greater beneficial effects are observed when it is administered by continuous intravenous infusion [136]. This may be the reason that standard prophylaxis against deep vein thrombosis (heparin, 5000 IU subcutaneously, 2–3 times daily) has not been associated with any salutary effect regarding SAH-induced DNDs.
Is There a Role for Unfractionated Heparin in Patients at Risk for DNDs?
The use of heparin in the context of SAH has not gained popular acceptance among clinicians, due possibly to a lack of widespread appreciation of its pleiotropic properties, and to well justified fears of complications including heparin-induced thrombocytopenia (HIT) [137] and hemorrhage [55]. However, the information compiled here suggests that a non-anticoagulating dose could potentially benefit patients with SAH who are at risk for DNDs. Indeed, the authors have used the following approach for some time with encouraging results: in patients whose aneurysm is confirmed to be excluded from the circulation, unfractionated heparin (8 IU/kg/h by constant IV infusion) is started 12 h after craniotomy, with the dose being increased by 1 IU/kg/h every 12 h to a final dose of 10 IU/kg/h, and is maintained for 10–14 days. Although a review of these patients is in progress and it is too early to draw conclusions, our experience to date suggests that this regimen is safe, results in no elevation of partial thromboplastin times, and confers significant protection from early and late DNDs.
Summary
Experimental and clinical studies have shown numerous beneficial effects of heparin in remarkably divergent conditions, from cancer [138] to a variety of inflammatory conditions, including but not limited to allergic reactions, burns, inflammatory bowel disease, and vascular inflammation [33, 34, 107, 108, 111, 112, 139–142]. As reviewed above, heparin exhibits a broad diversity of biological effects, many of which can be directly tied to pathophysiological mechanisms that have been implicated in SAH-induced DNDs. As a result, heparin may well serve as a long-sought multitargeted prophylactic agent against SAH-induced DNDs. Based on the review presented here, we believe that further study of the safety and efficacy of prophylactic unfractionated heparin in patients with SAH is warranted.
References
Bederson JB, Connolly ES Jr, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009;40:994–1025.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96.
Macdonald RL, Pluta RM, Zhang JH. Cerebral vasospasm after subarachnoid hemorrhage: the emerging revolution. Nat Clin Pract Neurol. 2007;3:256–63.
Rothoerl RD, Ringel F. Molecular mechanisms of cerebral vasospasm following aneurysmal SAH. Neurol Res. 2007;29:636–42.
Provencio JJ, Vora N. Subarachnoid hemorrhage and inflammation: bench to bedside and back. Semin Neurol. 2005;25:435–44.
Kranc KR, Pyne GJ, Tao L, et al. Oxidative degradation of bilirubin produces vasoactive compounds. Eur J Biochem. 2000;267:7094–101.
Pyne-Geithman GJ, Caudell DN, Prakash P, et al. Glutathione peroxidase and subarachnoid hemorrhage: implications for the role of oxidative stress in cerebral vasospasm. Neurol Res. 2009;31:195–9.
Vergouwen MD, Vermeulen M, Coert BA, et al. Microthrombosis after aneurysmal subarachnoid hemorrhage: an additional explanation for delayed cerebral ischemia. J Cereb Blood Flow Metab. 2008;28:1761–70.
Stein SC, Levine JM, Nagpal S, et al. Vasospasm as the sole cause of cerebral ischemia: how strong is the evidence? Neurosurg Focus. 2006;21:E2.
Zhang ZD, Macdonald RL. Contribution of the remodeling response to cerebral vasospasm. Neurol Res. 2006;28:713–20.
Crowley RW, Medel R, Kassell NF, et al. New insights into the causes and therapy of cerebral vasospasm following subarachnoid hemorrhage. Drug Discov Today. 2008;13:254–60.
Hansen-Schwartz J. Cerebral vasospasm: a consideration of the various cellular mechanisms involved in the pathophysiology. Neurocrit Care. 2004;1:235–46.
Fergusen S, Macdonald RL. Predictors of cerebral infarction in patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2007;60:658–67.
Lin CL, Jeng AY, Howng SL, et al. Endothelin and subarachnoid hemorrhage-induced cerebral vasospasm: pathogenesis and treatment. Curr Med Chem. 2004;11:1779–91.
Zimmermann M, Seifert V. Endothelin and subarachnoid hemorrhage: an overview. Neurosurgery. 1998;43:863–75.
Zimmermann M, Seifert V. Endothelin receptor antagonists and cerebral vasospasm. Clin Auton Res. 2004;14:143–5.
Macdonald RL, Kassell NF, Mayer S, et al. Clazosentan to overcome neurological ischemia and infarction occurring after subarachnoid hemorrhage (CONSCIOUS-1): randomized, double-blind, placebo-controlled phase 2 dose-finding trial. Stroke. 2008;39:3015–21.
Deshaies EM, Boulos AS, Popp AJ. Peri-operative medical management of cerebral vasospasm. Neurol Res. 2009;31:644–50.
Otten ML, Mocco J, Connolly ES Jr, et al. A review of medical treatments of cerebral vasospasm. Neurol Res. 2008;30:444–9.
Casu B. Structure of heparin and heparin fragments. Ann N Y Acad Sci. 1989;556:1–17.
Kandrotas RJ. Heparin pharmacokinetics and pharmacodynamics. Clin Pharmacokinet. 1992;22:359–74.
Young E. The anti-inflammatory effects of heparin and related compounds. Thromb Res. 2008;122:743–52.
Hirsh J, Anand SS, Halperin JL, et al. Mechanism of action and pharmacology of unfractionated heparin. Arterioscler Thromb Vasc Biol. 2001;21:1094–6.
Gandhi NS, Mancera RL. The structure of glycosaminoglycans and their interactions with proteins. Chem Biol Drug Des. 2008;72:455–82.
Coombe DR. Biological implications of glycosaminoglycan interactions with haemopoietic cytokines. Immunol Cell Biol. 2008;86:598–607.
Mulloy B. The specificity of interactions between proteins and sulfated polysaccharides. An Acad Bras Cienc. 2005;77:651–64.
Lindahl U, Lidholt K, Spillmann D, et al. More to “heparin” than anticoagulation. Thromb Res. 1994;75:1–32.
Amiconi G, Zolla L, Vecchini P, et al. The effect of macromolecular polyanions on the functional properties of human hemoglobin. Eur J Biochem. 1977;76:339–43.
Engelberg H. Actions of heparin that may affect the malignant process. Cancer. 1999;85:257–72.
Chansel D, Ciroldi M, Vandermeersch S, et al. Heparin binding EGF is necessary for vasospastic response to endothelin. FASEB J. 2006;20:1936–8.
Kuwahara-Watanabe K, Hidai C, Ikeda H, et al. Heparin regulates transcription of endothelin-1 gene in endothelial cells. J Vasc Res. 2005;42:183–9.
Yokokawa K, Mandal AK, Kohno M, et al. Heparin suppresses endothelin-1 action and production in spontaneously hypertensive rats. Am J Physiol. 1992;263:R1035–41.
Elsayed E, Becker RC. The impact of heparin compounds on cellular inflammatory responses: a construct for future investigation and pharmaceutical development. J Thromb Thrombolysis. 2003;15:11–8.
Tyrrell DJ, Horne AP, Holme KR, et al. Heparin in inflammation: potential therapeutic applications beyond anticoagulation. Adv Pharmacol. 1999;46:151–208.
Higashiyama S, Iwabuki H, Morimoto C, et al. Membrane-anchored growth factors, the epidermal growth factor family: beyond receptor ligands. Cancer Sci. 2008;99:214–20.
Higashiyama S, Nanba D. ADAM-mediated ectodomain shedding of HB-EGF in receptor cross-talk. Biochim Biophys Acta. 2005;1751:110–7.
Kalmes A, Daum G, Clowes AW. EGFR transactivation in the regulation of SMC function. Ann N Y Acad Sci. 2001;947:42–54.
Rider CC. Heparin/heparan sulphate binding in the TGF-beta cytokine superfamily. Biochem Soc Trans. 2006;34:458–60.
Kolias AG, Sen J, Belli A. Pathogenesis of cerebral vasospasm following aneurysmal subarachnoid hemorrhage: putative mechanisms and novel approaches. J Neurosci Res. 2009;87:1–11.
Hansen-Schwartz J, Vajkoczy P, Macdonald RL, et al. Cerebral vasospasm: looking beyond vasoconstriction. Trends Pharmacol Sci. 2007;28:252–6.
Sehba FA, Bederson JB. Mechanisms of acute brain injury after subarachnoid hemorrhage. Neurol Res. 2006;28:381–98.
Macdonald RL, Weir BK. A review of hemoglobin and the pathogenesis of cerebral vasospasm. Stroke. 1991;22:971–82.
Asano T. Oxyhemoglobin as the principal cause of cerebral vasospasm: a holistic view of its actions. Crit Rev Neurosurg. 1999;9:303–18.
Tekkok IH, Tekkok S, Ozcan OE, et al. Preventive effect of intracisternal heparin for proliferative angiopathy after experimental subarachnoid haemorrhage in rats. Acta Neurochir (Wien). 1994;127:112–7.
Macdonald RL, Weir B, Zhang J, et al. Adenosine triphosphate and hemoglobin in vasospastic monkeys. Neurosurg Focus. 1997;3:e3.
Macdonald RL, Marton LS, Andrus PK, et al. Time course of production of hydroxyl free radical after subarachnoid hemorrhage in dogs. Life Sci. 2004;75:979–89.
Sakaki S, Ohta S, Nakamura H, et al. Free radical reaction and biological defense mechanism in the pathogenesis of prolonged vasospasm in experimental subarachnoid hemorrhage. J Cereb Blood Flow Metab. 1988;8:1–8.
Tosaka M, Hashiba Y, Saito N, et al. Contractile responses to reactive oxygen species in the canine basilar artery in vitro: selective inhibitory effect of MCI-186, a new hydroxyl radical scavenger. Acta Neurochir (Wien). 2002;144:1305–10.
Clark JF, Sharp FR. Bilirubin oxidation products (BOXes) and their role in cerebral vasospasm after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2006;26:1223–33.
Engelberg H. Actions of heparin in the atherosclerotic process. Pharmacol Rev. 1996;48:327–52.
Juvela S. Plasma endothelin concentrations after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2000;92:390–400.
Kessler IM, Pacheco YG, Lozzi SP, et al. Endothelin-1 levels in plasma and cerebrospinal fluid of patients with cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Surg Neurol. 2005;64(Suppl 1):S1–5.
Ohkuma H, Parney I, Megyesi J, et al. Antisense preproendothelin-oligoDNA therapy for vasospasm in a canine model of subarachnoid hemorrhage. J Neurosurg. 1999;90:1105–14.
Chow M, Dumont AS, Kassell NF. Endothelin receptor antagonists and cerebral vasospasm: an update. Neurosurgery. 2002;51:1333–41.
Weyer GW, Nolan CP, Macdonald RL. Evidence-based cerebral vasospasm management. Neurosurg Focus. 2006;21:E8.
Reantragoon S, Arrigo LM, Dweck HS, et al. Suppression of endothelin-1 production in cultured human umbilical vein endothelial cells by heparin fractions separated by strong anion exchange chromatography. Arch Biochem Biophys. 1996;327:234–8.
Reantragoon S, Arrigo LM, Seoud MM, et al. Specific heparin fractions suppress endothelin-1 production in cultured human umbilical vein endothelial cells. Arch Biochem Biophys. 1994;314:315–22.
Alberts GF, Peifley KA, Johns A, et al. Constitutive endothelin-1 overexpression promotes smooth muscle cell proliferation via an external autocrine loop. J Biol Chem. 1994;269:10112–8.
Hedin U, Daum G, Clowes AW. Heparin inhibits thrombin-induced mitogen-activated protein kinase signaling in arterial smooth muscle cells. J Vasc Surg. 1998;27:512–20.
Aihara Y, Jahromi BS, Yassari R, et al. Molecular profile of vascular ion channels after experimental subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2004;24:75–83.
Weyer GW, Jahromi BS, Aihara Y, et al. Expression and function of inwardly rectifying potassium channels after experimental subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2006;26:382–391.
Ishiguro M, Morielli AD, Zvarova K, et al. Oxyhemoglobin-induced suppression of voltage-dependent K+ channels in cerebral arteries by enhanced tyrosine kinase activity. Circ Res. 2006;99:1252–60.
Koide M, Penar PL, Tranmer BI, et al. Heparin-binding EGF-like growth factor mediates oxyhemoglobin-induced suppression of voltage-dependent potassium channels in rabbit cerebral artery myocytes. Am J Physiol Heart Circ Physiol. 2007;293:H1750–9.
Zubkov AY, Tibbs RE, Clower B, et al. Morphological changes of cerebral arteries in a canine double hemorrhage model. Neurosci Lett. 2002;326:137–41.
Ohkuma H, Tsurutani H, Suzuki S. Changes of beta-actin mRNA expression in canine vasospastic basilar artery after experimental subarachnoid hemorrhage. Neurosci Lett. 2001;311:9–12.
Ohkuma H, Suzuki S, Ogane K. Phenotypic modulation of smooth muscle cells and vascular remodeling in intraparenchymal small cerebral arteries after canine experimental subarachnoid hemorrhage. Neurosci Lett. 2003;344:193–6.
Macdonald RL, Weir BK, Young JD, et al. Cytoskeletal and extracellular matrix proteins in cerebral arteries following subarachnoid hemorrhage in monkeys. J Neurosurg. 1992;76:81–90.
Pluta RM, Zauner A, Morgan JK, et al. Is vasospasm related to proliferative arteriopathy? J Neurosurg. 1992;77:740–8.
Ivanov A, Gerzanich V, Ivanova S, et al. Adenylate cyclase 5 and KCa1.1 channel are required for EGFR up-regulation of PCNA in native contractile rat basilar artery smooth muscle. J Physiol. 2006;570:73–84.
Zubkov AY, Ogihara K, Tumu P, et al. Mitogen-activated protein kinase mediation of hemolysate-induced contraction in rabbit basilar artery. J Neurosurg. 1999;90:1091–7.
Aoki K, Zubkov AY, Tibbs RE, et al. Role of MAPK in chronic cerebral vasospasm. Life Sci. 2002;70:1901–8.
Satoh M, Parent AD, Zhang JH. Inhibitory effect with antisense mitogen-activated protein kinase oligodeoxynucleotide against cerebral vasospasm in rats. Stroke. 2002;33:775–81.
Zhang JH. Role of MAPK in cerebral vasospasm. Drug News Perspect. 2001;14:261–7.
Reynolds CM, Eguchi S, Frank GD, et al. Signaling mechanisms of heparin-binding epidermal growth factor-like growth factor in vascular smooth muscle cells. Hypertension. 2002;39:525–9.
Maeda Y, Hirano K, Hirano M, et al. Enhanced contractile response of the basilar artery to platelet-derived growth factor in subarachnoid hemorrhage. Stroke. 2009;40:591–6.
Raab G, Klagsbrun M. Heparin-binding EGF-like growth factor. Biochim Biophys Acta. 1997;1333:F179–99.
Kawahara N, Mishima K, Higashiyama S, et al. The gene for heparin-binding epidermal growth factor-like growth factor is stress-inducible: its role in cerebral ischemia. J Cereb Blood Flow Metab. 1999;19:307–20.
Jin K, Mao XO, Sun Y, et al. Heparin-binding epidermal growth factor-like growth factor: hypoxia-inducible expression in vitro and stimulation of neurogenesis in vitro and in vivo. J Neurosci. 2002;22:5365–73.
Borel CO, McKee A, Parra A, et al. Possible role for vascular cell proliferation in cerebral vasospasm after subarachnoid hemorrhage. Stroke. 2003;34:427–33.
Gaetani P, Tancioni F, Grignani G, et al. Platelet derived growth factor and subarachnoid haemorrhage: a study on cisternal cerebrospinal fluid. Acta Neurochir (Wien). 1997;139:319–24.
Zhang Z, Nagata I, Kikuchi H, et al. Broad-spectrum and selective serine protease inhibitors prevent expression of platelet-derived growth factor-BB and cerebral vasospasm after subarachnoid hemorrhage: vasospasm caused by cisternal injection of recombinant platelet-derived growth factor-BB. Stroke. 2001;32:1665–72.
Tsurutani H, Ohkuma H, Suzuki S. Effects of thrombin inhibitor on thrombin-related signal transduction and cerebral vasospasm in the rabbit subarachnoid hemorrhage model. Stroke. 2003;34:1497–500.
Mishra-Gorur K, Castellot JJ Jr. Heparin rapidly and selectively regulates protein tyrosine phosphorylation in vascular smooth muscle cells. J Cell Physiol. 1999;178:205–15.
Lee KS, Park JH, Lee S, et al. HB-EGF induces delayed STAT3 activation via NF-kappaB mediated IL-6 secretion in vascular smooth muscle cell. Biochim Biophys Acta. 2007;1773:1637–44.
Kalmes A, Vesti BR, Daum G, et al. Heparin blockade of thrombin-induced smooth muscle cell migration involves inhibition of epidermal growth factor (EGF) receptor transactivation by heparin-binding EGF-like growth factor. Circ Res. 2000;87:92–8.
Okada T, Bark DH, Mayberg MR. Localized release of perivascular heparin inhibits intimal proliferation after endothelial injury without systemic anticoagulation. Neurosurgery. 1989;25:892–8.
Levine A, Kenet G, Bruck R, et al. Effect of heparin on tissue binding activity of fibroblast growth factor and heparin-binding epidermal growth factor in experimental colitis in rats. Pediatr Res. 2002;51:635–40.
Kawanabe Y, Masaki T, Hashimoto N. Involvement of epidermal growth factor receptor-protein tyrosine kinase transactivation in endothelin-1-induced vascular contraction. J Neurosurg. 2004;100:1066–71.
Pukac LA, Carter JE, Ottlinger ME, et al. Mechanisms of inhibition by heparin of PDGF stimulated MAP kinase activation in vascular smooth muscle cells. J Cell Physiol. 1997;172:69–78.
Kapp JP, Clower BR, Azar FM, et al. Heparin reduces proliferative angiopathy following subarachnoid hemorrhage in cats. J Neurosurg. 1985;62:570–5.
Dhar R, Diringer MN. The burden of the systemic inflammatory response predicts vasospasm and outcome after subarachnoid hemorrhage. Neurocrit Care. 2008;8:404–12.
Yoshimoto Y, Tanaka Y, Hoya K. Acute systemic inflammatory response syndrome in subarachnoid hemorrhage. Stroke. 2001;32:1989–93.
Dumont AS, Dumont RJ, Chow MM, et al. Cerebral vasospasm after subarachnoid hemorrhage: putative role of inflammation. Neurosurgery. 2003;53:123–33.
Gallia GL, Tamargo RJ. Leukocyte-endothelial cell interactions in chronic vasospasm after subarachnoid hemorrhage. Neurol Res. 2006;28:750–8.
Rothoerl RD, Axmann C, Pina AL, et al. Possible role of the C-reactive protein and white blood cell count in the pathogenesis of cerebral vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2006;18:68–72.
Clatterbuck RE, Gailloud P, Ogata L, et al. Prevention of cerebral vasospasm by a humanized anti-CD11/CD18 monoclonal antibody administered after experimental subarachnoid hemorrhage in nonhuman primates. J Neurosurg. 2003;99:376–82.
Fassbender K, Hodapp B, Rossol S, et al. Inflammatory cytokines in subarachnoid haemorrhage: association with abnormal blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry. 2001;70:534–7.
Ono S, Date I, Onoda K, et al. Decoy administration of NF-kappaB into the subarachnoid space for cerebral angiopathy. Hum Gene Ther. 1998;9:1003–11.
Hein AM, O’Banion MK. Neuroinflammation and memory: the role of prostaglandins. Mol Neurobiol. 2009;40:15–32.
Skaper SD. The brain as a target for inflammatory processes and neuroprotective strategies. Ann N Y Acad Sci. 2007;1122:23–34.
Rosi S, Ramirez-Amaya V, Vazdarjanova A, et al. Neuroinflammation alters the hippocampal pattern of behaviorally induced Arc expression. J Neurosci. 2005;25:723–31.
Chen J, Buchanan JB, Sparkman NL, et al. Neuroinflammation and disruption in working memory in aged mice after acute stimulation of the peripheral innate immune system. Brain Behav Immun. 2008;22:301–11.
Hutter BO, Gilsbach JM, Kreitschmann I. Quality of life and cognitive deficits after subarachnoid haemorrhage. Br J Neurosurg. 1995;9:465–75.
Ljunggren B, Sonesson B, Saveland H, et al. Cognitive impairment and adjustment in patients without neurological deficits after aneurysmal SAH and early operation. J Neurosurg. 1985;62:673–9.
Ravnik J, Starovasnik B, Sesok S, et al. Long-term cognitive deficits in patients with good outcomes after aneurysmal subarachnoid hemorrhage from anterior communicating artery. Croat Med J. 2006;47:253–63.
Goudeau JJ, Clermont G, Guillery O, et al. In high-risk patients, combination of antiinflammatory procedures during cardiopulmonary bypass can reduce incidences of inflammation and oxidative stress. J Cardiovasc Pharmacol. 2007;49:39–45.
Saliba MJ Jr. Heparin in the treatment of burns: a review. Burns. 2001;27:349–58.
Saliba MJ Jr. The effects and uses of heparin in the care of burns that improves treatment and enhances the quality of life. Acta Chir Plast. 1997;39:13–6.
Papa A, Danese S, Gasbarrini A, et al. Review article: potential therapeutic applications and mechanisms of action of heparin in inflammatory bowel disease. Aliment Pharmacol Ther. 2000;14:1403–9.
Cervera A, Justicia C, Reverter JC, et al. Steady plasma concentration of unfractionated heparin reduces infarct volume and prevents inflammatory damage after transient focal cerebral ischemia in the rat. J Neurosci Res. 2004;77:565–72.
Chamorro A, Obach V, Vila N, et al. Comparison of the acute-phase response in patients with ischemic stroke treated with high-dose heparin or aspirin. J Neurol Sci. 2000;178:17–22.
Hochart H, Jenkins PV, Smith OP, et al. Low-molecular weight and unfractionated heparins induce a downregulation of inflammation: decreased levels of proinflammatory cytokines and nuclear factor-kappaB in LPS-stimulated human monocytes. Br J Haematol. 2006;133:62–7.
Le Brun G, Aubin P, Soliman H, et al. Upregulation of endothelin 1 and its precursor by IL-1beta, TNF-alpha, and TGF-beta in the PC3 human prostate cancer cell line. Cytokine. 1999;11:157–62.
Marsden PA, Brenner BM. Transcriptional regulation of the endothelin-1 gene by TNF-alpha. Am J Physiol. 1992;262:C854–61.
McFadden G, Kelvin D. New strategies for chemokine inhibition and modulation: you take the high road and I’ll take the low road. Biochem Pharmacol. 1997;54:1271–80.
Sheikine Y, Hansson GK. Chemokines and atherosclerosis. Ann Med. 2004;36:98–118.
Yoshie O, Imai T, Nomiyama H. Chemokines in immunity. Adv Immunol. 2001;78:57–110.
Soehnlein O, Zernecke A, Eriksson EE, et al. Neutrophil secretion products pave the way for inflammatory monocytes. Blood. 2008;112:1461–71.
Ranjbaran H, Wang Y, Manes TD, et al. Heparin displaces interferon-gamma-inducible chemokines (IP-10, I-TAC, and Mig) sequestered in the vasculature and inhibits the transendothelial migration and arterial recruitment of T cells. Circulation. 2006;114:1293–300.
Chimowitz MI, Pessin MS. Is there a role for heparin in the management of complications of subarachnoid hemorrhage? Stroke. 1987;18:1169–72.
Wang DZ, Futrell N, Taylon C, et al. Anticoagulation for prevention of cerebral infarcts following subarachnoid hemorrhage. Surg Neurol. 1995;44:270–4.
Kapp J, Neill WR, Salter JE, et al. Systemic heparin in the early management of ruptured intracranial aneurysms: review of 104 consecutive cases and comparison with concurrent controls. Neurosurgery. 1987;20:564–70.
Kapp JP, Neill WR, Neill CL, et al. The three phases of vasospasm. Surg Neurol. 1982;18:40–5.
Wurm G, Tomancok B, Nussbaumer K, et al. Reduction of ischemic sequelae following spontaneous subarachnoid hemorrhage: a double-blind, randomized comparison of enoxaparin versus placebo. Clin Neurol Neurosurg. 2004;106:97–103.
Juvela S, Siironen J, Varis J, et al. Risk factors for ischemic lesions following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2005;102:194–201.
Siironen J, Juvela S, Varis J, et al. No effect of enoxaparin on outcome of aneurysmal subarachnoid hemorrhage: a randomized, double-blind, placebo-controlled clinical trial. J Neurosurg. 2003;99:953–9.
Khorana AA, Sahni A, Altland OD, et al. Heparin inhibition of endothelial cell proliferation and organization is dependent on molecular weight. Arterioscler Thromb Vasc Biol. 2003;23:2110–5.
Young E, Venner T, Ribau J, et al. The binding of unfractionated heparin and low molecular weight heparin to thrombin-activated human endothelial cells. Thromb Res. 1999;96:373–81.
Koenig A, Norgard-Sumnicht K, Linhardt R, et al. Differential interactions of heparin and heparan sulfate glycosaminoglycans with the selectins. Implications for the use of unfractionated and low molecular weight heparins as therapeutic agents. J Clin Invest. 1998;101:877–89.
Chan P, Mill S, Mulloy B, et al. Heparin inhibition of human vascular smooth muscle cell hyperplasia. Int Angiol. 1992;11:261–7.
Dawes J. Interactions of heparins in the vascular environment. Haemostasis. 1993;23(Suppl 1):212–9.
Tiozzo R, Cingi MR, Croce MA. Interaction of heparan sulfate and its fractions with endothelial cells in culture. Int J Tissue React. 1993;15:163–8.
Yanaka K, Spellman SR, McCarthy JB, et al. Reduction of brain injury using heparin to inhibit leukocyte accumulation in a rat model of transient focal cerebral ischemia. I. Protective mechanism. J Neurosurg. 1996;85:1102–7.
Chamorro A. Heparin in acute ischemic stroke revisited. Rev Neurol (Paris). 2008;164:815–8.
Moonis M, Fisher M. Considering the role of heparin and low-molecular-weight heparins in acute ischemic stroke. Stroke. 2002;33:1927–33.
Edelman ER, Karnovsky MJ. Contrasting effects of the intermittent and continuous administration of heparin in experimental restenosis. Circulation. 1994;89:770–6.
Linkins LA, Warkentin TE. The approach to heparin-induced thrombocytopenia. Semin Respir Crit Care Med. 2008;29:66–74.
Bobek V, Kovarik J. Antitumor and antimetastatic effect of warfarin and heparins. Biomed Pharmacother. 2004;58:213–9.
Bowler SD, Smith SM, Lavercombe PS. Heparin inhibits the immediate response to antigen in the skin and lungs of allergic subjects. Am Rev Respir Dis. 1993;147:160–3.
Seeds EA, Page CP. Heparin inhibits allergen-induced eosinophil infiltration into guinea-pig lung via a mechanism unrelated to its anticoagulant activity. Pulm Pharmacol Ther. 2001;14:111–9.
Zak-Nejmark T, Krasnowska M, Jankowska R, et al. Heparin modulates migration of human peripheral blood mononuclear cells and neutrophils. Arch Immunol Ther Exp (Warsz). 1999;47:245–9.
Derhaschnig U, Pernerstorfer T, Knechtelsdorfer M, et al. Evaluation of antiinflammatory and antiadhesive effects of heparins in human endotoxemia. Crit Care Med. 2003;31:1108–12.
Acknowledgments
JMS is supported by grants from the National Institutes of Health (HL082517, NS061808, NS060801), the Department of Veterans Affairs (Baltimore VA), the Department of Defense (PT074766, SC090293), and the Christopher and Dana Reeves Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simard, J.M., Schreibman, D., Aldrich, E.F. et al. Unfractionated Heparin: Multitargeted Therapy for Delayed Neurological Deficits Induced by Subarachnoid Hemorrhage. Neurocrit Care 13, 439–449 (2010). https://doi.org/10.1007/s12028-010-9435-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9435-1