Abstract
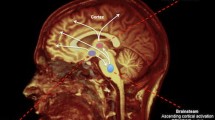
The concept of consciousness has fascinated philosophers, psychologists and neurophysiologists for a long time; however, it remains difficult to give its univocal and universally accepted definition. Consciousness is defined as “the state of full awareness of the self and one’s relationship to the environment”; consequently, a distinction must be made between consciousness (or awareness) and vigilance/alertness (wakefulness). In fact, it is possible for a patient to be conscious, but unresponsive to the examiner, for lack of sensory inputs or for psychiatric reasons. Conversely, a subject can be alert and awake with open eyes, but not conscious and not aware (in part or at all) of itself and of the environment. From a neurophysiological point of view, it has been demonstrated that the brainstem Reticular Activating System (RAS) is responsible for the state of alertness, through its projections to the thalamus and cortex. The integrity of the upper cortical centres, which are closely related to each other and receive the reticular activating stimuli, is also essential for the maintenance of consciousness level. Therefore, Disorders Of Consciousness (DOC) and vigilance may depend on damage to one or both of these neurofunctional systems, acute or chronic, reversible or irreversible. Serious damage to the reticular system, with or without concomitant widespread cortical damage, can produce a state of coma. Coma is then a pathological condition in which the subject lies with eyes closed and he is neither conscious nor alert, with altered - or completely absent - responsiveness to stimuli. In case of widespread damage to the cerebral cortex without involvement of the RAS, a particular condition - named Vegetative State (VS) - may occur: the consciousness of self and of the environment is impaired, but a certain level of vigilance is still preserved. Moreover, there also exist several neurological conditions that can be defined as “borderline”, such as the Minimally Conscious State. Finally, brain death is the irreversible definitive impairment of both the cortical and brainstem functions. Electroencephalography is an important diagnostic and prognostic tool, useful to better characterise the evolution of a coma state, to recognise any kind of epileptiform activity - that could be clinically hidden - and to monitor the effects of antiepileptic drugs, level of sedation, and treatment of intracranial hypertension.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Coma
- Minimally conscious state
- Vegetative state
- Locked-in syndrome
- Brain death
- Status epilepticus
- Alpha coma
- Spindle coma
- Burst-suppression
- Somatosensory-evoked potentials
1 Anatomo-Pathophysiology of Disorders of Consciousness
Disorders Of Consciousness (DOC) result from failure of the arousal system. The current knowledge regarding the anatomo-physiology of vigilance dates back to the 1930s and 1940s, owing to the elegant experiments performed by Bremer [1] and Moruzzi and Magoun [2]. Observing cats with their brainstem sectioned between the pons and midbrain and in the lower part of the bulb, Bremer discovered that rostral section caused a clinical state and an EEG similar to that of sleep (with characteristic synchronised EEG sleep rhythms), while animals with caudal section remained awake but with desynchronised EEG rhythms. Many years later, Dempsey and Morrison [3] demonstrated the presence of a system of non-specific projections (independent from specific sensory nuclei) from the thalami to all the cortical regions. This concept was further demonstrated by Moruzzi and Magoun [2], who observed that the electrical stimulation of the medial mesencephalic tegmentum and of the adjacent areas caused the awakening of slightly anesthetised animals, with corresponding EEG desynchronisation as in normal awakening, in response to sensory stimuli. The sites that induced awakening upon stimulation consisted of a series of neuronal stations extending from the non-specific nuclei of the medial thalamus to the caudal midbrain. These areas corresponded to the complex system of the ascending reticular formation, a system that is widely innervated by axon collaterals of the ascending sensory systems and is, therefore, in a state of tonic activation. Moreover, since this region, in particular the medial thalamus, projected widely to the cerebral hemispheres, the concept of a Reticular Activating System (RAS) that maintained the waking state originated, which inactivation led to a state of unconsciousness. Despite several experimental disagreements [4], the paramedian upper mesencephalic tegmentum and the lower diencephalon began to be considered as the brain system responsible for arousal. The anatomical boundaries of RAS in the upper midbrain are indistinct, since it is scattered throughout the paramedian regions of the rostral part of the pons and of the mesencephalic tegmentum. In the thalamus, RAS includes the posterior, paramedian, parafascicular and medial portions of the centromedian and intralaminar nuclei. In the brainstem, RAS includes the nuclei of the reticular formation, which receive collaterals from the spinal and trigeminal-thalamic pathways and project widely to the entire cortex, and other key structures for arousal, including the raphe nuclei, locus coeruleus, substantia nigra pars compacta, ventral tegmental area and the mesopontine tegmentum, the latter including the pedunculopontine and laterodorsal tegmental nuclei. These nuclei extend throughout the brainstem, sending ascending and descending signals to influence arousal. Furthermore, their dendrites are positioned in the brainstem such as to detect signals that pass to and from the periphery. The dendrites of these neurons form web-like “reticula” around the passing axons and they can detect a wide variety of external sensory or internal thalamic stimuli passing through the surrounding structures. Therefore, these reticular neurons are positioned strategically to respond to both external and internal signals in the control of arousal [5, 6] (Table 46.1).
The sensory stimulation has therefore a double effect; conveying information from somatic structures to the cortex and activating the regions of the central nervous system on which consciousness depends. Moreover, the cortex does not limit to receiving stimuli from the RAS, but also modulates these input information through corticofugal projections towards the reticular formation.
Other anatomical structures more recently considered as fundamental in maintaining the state of consciousness, especially in the transition across the DOC continuum, are the basal forebrain and the hypothalamic systems, that participate in the constitution of the “mesocircuit model”.
The mesocircuit model postulates that the anterior forebrain function is markedly downregulated in all severe brain injuries, as a result of widespread disconnection or neuronal death. A crucial role is proposed for neurons within the central thalamus that are known to show progressive deafferentation in proportion to the severity of structural brain injuries [7]. At the mesocircuit level, a broad reduction in corticostriatal, thalamo-cortical and thalamostriatal outflow is expected to produce sufficient loss of afferent inputs to the Medium Spiny Neurons (MSNs) of the striatum, to prevent these neurons from reaching their firing threshold [8]. The direct deafferentation of central thalamic neurons and the active inhibition of some of these cells by the internal globus pallidus, due to loss of their active inhibition by the MSNs in the striatum, cause a large reduction in the synaptic activity of the entire brain, as reflected by the very low cerebral metabolic rates typical in patients with DOC [9]. As evidence of the important role of the anterior forebrain mesocircuit, the expressed behaviour and level of conscious content increase with restoration of its normal patterns of activity [10]. This model can also explain some of the effects of different activating drugs used in DOC [11] and novel strategies, such as Deep Brain Stimulation (DBS), all of which have the effect of restoring activity of cortical frontal, striatal and central thalamic neurons [12]. It also draws a direct connection across similar shifts in frontal cortical and striatal activation during the sleep–wake cycle and the paradoxical behavioural activation observed during the early stages of anaesthesia [13].
Large reductions of arousal level in normal individuals involve broad hyperpolarisation of these neurons via withdrawal of excitatory neuromodulatory influences from orexinergic, cholinergic, noradrenergic, and other brainstem, basal forebrain and hypothalamic systems [14, 15]. Such hyperpolarisation of cortical and thalamic neurons, as progressively occurs across the deeper stages of sleep or with the broad inhibitory effects of anaesthesia, markedly changes the firing patterns of these neuronal populations, influencing the overall pattern of cortico-thalamic dynamics towards more synchronous and dynamically stereotyped waves of activity as compared with the more spatio-temporally differentiated patterns associated with wakeful conscious state [11].
EEG is important for the assessment of waking state, since the electrical activity of cerebral cortex depends on the characteristics of the thalamo-cortical discharge system, an indispensable component for the maintenance of wakefulness. As already described in Chap. 2, the electrical activity recorded at the surface of the skull depends on the summation of the synaptic potentials arising in the dendrites of cortical neurons; therefore, EEG rhythms depend on the synchronisation of the waves derived from the summation of the synaptic potentials generated by the activity of thalamo-cortical neurons. In turn, the rhythms of thalamic activity depend on the important properties of thalamic retransmission neurons, which can be found in two different physiological states: the transmission mode and the burst mode. In the former case, the membrane potential of a retransmission neuron is close to the discharge threshold and the excitatory synaptic potentials generated by the afferent signals produce a discharge, the characteristics of which are related to those of the sensory stimulus. In the latter case, thalamic neurons are hyperpolarised by inhibitory afferent signals. Thalamic retransmission neurons possess a special voltage-dependent calcium channel that is inactive when the membrane potential is close to the threshold. Conversely, when the retransmission neuron is hyperpolarised, the excitatory synaptic potentials generated by the afferent signals determine the transient opening of these calcium channels and the appearance of a calcium current that carries the neuron membrane potential beyond the threshold necessary for the genesis of the action potential. As a consequence, the neuron generates a burst of action potentials causing a further opening of the calcium channels, until the amount of calcium entering the cell is no longer sufficient to trigger a potassium current that hyperpolarises the cell, returning its potential to the initial level at which a new burst-mode cycle is generated. The thalamic retransmission neurons are initially hyperpolarised, due to their mutual interactions with GABAergic inhibitory interneurons of the reticular nucleus of the thalamus, whose dendrites receive collaterals from the axons of the thalamo-cortical and cortico-thalamic neurons that pass through the nucleus. Neurons of the reticular nucleus hyperpolarise the thalamic retransmission neurons; thus, their ability to reach the threshold of discharge in response to afferent sensory signals depends on the activity of the neurons of the reticular nucleus; when they are hyperpolarised, both retransmission and reticular neurons enter the burst mode.
In retransmission neurons, afferents from the reticular nucleus generate inhibitory synaptic potentials that remove the inactivation of calcium channels; subsequently, modification of the membrane potential generates a burst of action potentials. In turn, thalamic retransmission neurons send excitatory signals to the reticular neurons, which trigger another burst of activity in the reticular neurons. The consequent rhythmic and synchronous discharge of the thalamic retransmission neurons produces waves of excitatory synaptic potentials at the level of the dendrites of the cortical neurons. Depolarisation cycles are recorded as slow and rhythmic EEG waves, and this pattern indicates that the thalamus is unable to retransmit sensory information to the cortex. This type of EEG pattern is observed during deep sleep, but also in pathological conditions characterised by the blockage of the thalamo-cortical transmission, as in coma state. On the contrary, when the thalamus is in transmission mode, as during wakefulness, the desynchronised EEG trace indicates that information regarding sensory stimuli is being relayed. During the normal waking state, the thalamus is maintained in the transmission mode by cholinergic afferents from the rostral pons and from the basal forebrain. The main cholinergic afferents to the thalamic retransmission nuclei originate from the peduncle-pontine nucleus and from the laterodorsal tegmental nuclei of the brainstem. These nuclei, together with the cholinergic neurons of the basal forebrain, innervate the reticular nucleus of the thalamus, reducing its activity, and thus preventing the hyperpolarisation of the thalamic retransmission neurons during the waking state [16].
Knowledge of these anatomo-physiological mechanisms is of fundamental importance in understanding the neuropathological bases of the different types of brain lesions that can cause coma and in making a correct diagnosis of the lesion site. It is known that structural abornalities in different brain regions may have different clinical and electrophysiological aspects. Brainstem sections under the rostral pons have no influence on the state of consciousness; however, acute sections above the inferior colliculus, as well as those of the paramedian reticular formation of the midbrain, always cause coma, even if circumscribed. Posterolateral hypothalamic lesions interrupt the branch passing through the hypothalamus and cause a marked EEG slowing and the induction of coma, even if the branch passing through the thalamus remains intact. In contrast, injuries to the thalamus or its afferents from the reticular nucleus prevent the brain from maintaining a desynchronised or waking state. If the lesions are sufficiently extensive, the EEG rhythm may completely disappear.
2 Coma, Vegetative State, and Minimally Conscious State
Coma is defined as a state of deep, unarousable unconsciousness; the patient lies with eyes closed and, as coma deepens, responsiveness to acoustic and/or painful stimuli diminishes or completely disappears [17]. Coma should be considered a self-limiting or transitory condition that usually resolves within 2–4 weeks, evolving into: partial or complete recovery; Vegetative State (VS) or Minimally Conscious State (MCS); death [13].
The causes of coma can be classified in two principal groups: structural brain diseases and diffuse neuronal dysfunction [18]. Structural brain lesions include Space-Occupying Lesions (SOL) and all conditions of increased intracranial pressure (tumours, abscesses, cerebral oedema, hydrocephalus), anoxic-hypoxic brain disease, epidural or subdural haematoma, cerebral haemorrhages, and acute ischaemic stroke. SOL are also characterised by their location above or below the cerebellar tentorium and are classified as supratentorial or infratentorial brain lesions. Structural brain diseases can also be induced by sepsis, CNS infections, or status epilepticus. A condition of diffuse neuronal dysfunction responsible for coma can be caused by different metabolic syndromes (hypo- or hyperglycaemia, hyponatraemia, hypercalcemia, hepatic and renal failure, thyroid diseases) or toxic agents (sedatives, opioids, toxic alcohols, carbon monoxide).
Vegetative state is a condition characterised by the absence of responsiveness and awareness due to a massive dysfunction of the cerebral cortex of both hemispheres, with sufficient integrity of the diencephalon and brainstem to preserve autonomic and motor reflexes and sleep−wake cycles. VS patients have spontaneous eye-opening movements (because the reticular activating system is intact ) and completely or partially preserved hypothalamic and brainstem functions. The eyes are open during wake and closed during sleep, and ocular movements, such as blinking, roving and nystagmus, are present; breathing is spontaneous.
However, these patients show no evidence of sustained, reproducible, purposeful, or voluntary behavioural response to various stimuli, and there is no evidence of language comprehension or expression. Cranial nerve functions and spinal reflexes are variably preserved, as is the sleep-wave cycle, but there is no control of the sphincters, leading to bowel and bladder incontinence. It is recommended not to use the term “persistent” for VS; aetiology of the brain injury (traumatic or non-traumatic) and the duration of the VS should instead be specified. The clinical course and outcome of VS depend on its cause: acute traumatic and non-traumatic brain injuries, degenerative and metabolic brain disorders, or severe congenital malformations of the CNS. Recovery from a post-traumatic VS is unlikely after 12 months (and more unlikely in adults than in children), while recovery from a non-traumatic VS after 3 months is rare in both adults and children. Finally, patients with metabolic diseases or congenital malformations who remain in a VS for several months are unlikely to recover consciousness [13, 19, 20].
Minimally conscious state must be distinguished from VS. It is a chronic condition consequent to a severe diffuse brain damage, characterised by an altered state of consciousness and a diminished - but demonstrated - self and environmental awareness. This condition may represent a transitional state reflecting clinical improvement following coma or a VS or, conversely, a progressive deterioration of consciousness as in neurodegenerative disease [13, 21].
In comparison with VS, thalamic lesions are less prevalent in MCS, and the relative sparing of cortico-thalamic connections could explain the minimal preservation of cognitive processes. Behavioural features of MCS patients are: response to simple commands and questions (gestural or “yes-no” responses); intelligible verbalisation in response to the linguistic content of questions; reaching for and grabbing objects, recognising their position; recognising the shape and size of objects; pursuit eye movement or fixation on moving objects; appropriate smiling or crying. However, the behavioural responses to stimuli are inconsistent and sometimes even ambiguous.
MCS was recently subcategorised according to the complexity of patients’ behaviour: MCS plus describes high-level behavioural responses (i.e. command execution, intelligible verbalisation, or non-functional communication); MCS minus describes low-level behavioural responses (i.e. visual pursuit, localisation of nociceptive stimulation, or contingent behaviour such as appropriate smiling or crying in response to emotional stimuli) [22].
3 Differential Diagnosis Among Consciousness Disorders
VS and MCS should be placed in differential diagnosis with Akinetic Mutism (AM) and Locked-In Syndrome (LIS).
AM was first described in 1941 by Cairns and colleagues [23] as a mental state in which patients lose the ability to move or to speak. This condition could be explained by damage to the frontal lobe or by the interruption of the complex frontal-subcortical circuits by stroke or degenerative disease [24]. In AM, differently from MCS, speech and movements may be facilitated by exposure to high-intensity sensory or personally salient stimuli.
LIS is a rare and severe condition caused by damage to cortico-spinal and cortico-bulbar pathways due to brainstem lesions. Patients are conscious but cannot respond or move; all voluntary muscles are paralysed, except those used for vertical eye movements and blinking. LIS can be misdiagnosed if the loss of speech and movements is attributed to consciousness impairment. Furthermore, in some cases, LIS may appear to be a VS or MCS at the acute stage, and may only subsequently evolve into the classic LIS features [12]. Most patients in a LIS show an EEG wake pattern similar to that of normal individuals, with preserved consciousness. Thus, the EEG pattern observed in LIS must not be interpreted as an alpha coma pattern and EEG findings may be helpful in differentiating LIS from coma (Table 46.2).
4 Clinical Examination of Comatose Patients
Although the clinical definition of coma is universally accepted, the set of causes that underlie this complex condition and the lesion sites are wide, which justifies the great corollary of possible clinical manifestations. Moreover, a careful clinical examination can often be very useful in individuating, with sufficient precision, the level of the lesion.
It is easy to understand that the first clinical approach to a comatose patient depends strictly on the most probable cause of coma (traumatic, metabolic, anoxic, etc.) and the length of time since the condition has been established, which should not be deduced from only a general physical examination. Alterations in body temperature (fever or hypothermia), cardiac activity and blood pressure, skin appearance, and the breath odor are important to the physician when addressing the possible causes of coma. For instance, the presence of multiple contusions and cerebrospinal fluid otorhinorrhaea are suggestive of traumatic injury; cyanosis indicates hypoxia; petechiae are characteristic of systemic infections or haematological diseases; blood pressure and heart rate may be altered in the case of endocranial hypertension; certain breath odors may be suggestive of renal or hepatic dysfunction or alcohol intoxication. Furthermore, the presence of rigor nucalis should always be investigated, in addition to all other signs of meningeal irritation. Neurological examination should, therefore, test the functionality of the main systems involved in the maintenance of consciousness and, at the same time, identify any other localising signs. In comatose patients, the hemispheres can only be examined by assessment of responses to sound, touch and nociceptive stimuli [25]. The state of consciousness is assessed by the responsiveness to environmental stimuli. Two important aspects of the state of consciousness must be evaluated: the level of consciousness, depending on the patient’s ability to awake and the content of consciousness, depending on the relevance of the patient’s responses. In assessing the level of consciousness, it is necessary to determine the intensity of the stimulation required to arouse the patient: the grading system, from verbal responsiveness to localising responses, non-localising responses and no response, is all needed for the initial assessment of the depth of unresponsiveness, used also to monitor the progress of the clinical status. In case of no response to voice or vigorous shaking, a painful stimulus should be applied to obtain information regarding the laterality of the motor response. It should begin with a modest, lateralised stimulus (compression of the nail beds, the supraorbital ridge, the temporomandibular joint) performed bilaterally and, in the case of no response, a more vigorous midline stimulus may be given in the form of a sternal rub [17]. Patient responses are noted and graded in the specific sections of the Glasgow Coma Scale (GCS). An essential part of neurological examination, especially for its high value in localising brainstem lesions, is the evaluation of cranial nerves and breathing patterns. The most important aspects are: pupillary shape, reaction, and diameter; ocular movements; oculovestibular reflexes. Pupil dilation is mediated by the orthosympathetic innervation of the iris from the superior cervical ganglion. The preganglionic neurons are located in the cervical part of the spinal cord and are under the control of tonic excitatory signals from the hypothalamus. In case of diffuse alterations of the forebrain, the pupils are myotic but reactive to light. Pons lesions can result in a marked myosis with preserved pupillary reactions, due to interruption of the pathways that mediate their dilation; opioids can cause myosis with reactive pupils. The loss of pupillary responses to light is almost always caused by structural changes. Pupils are intermediate (diameter slightly larger than normal) and fixed (unreactive to light) in lesions of the pretectal area of the midbrain, while lesions of the third cranial nerve in the midbrain cause the complete loss of pupillary responses, due to interference with both the descending orthosympathetic system - crossing the midbrain laterally to the nuclei of the third nerve - as well as the parasympathetic system. Unilateral mydriasis can occur from oculomotor nerve injury in the midbrain, since the pupil that loses parasympathetic with preserved orthosympathetic control has a larger diameter than the contralateral. The most common causes of unilateral compression of the oculomotor nerve in comatose patients are attributable to aneurysms of the posterior communicating artery or to the compression of the third cranial nerve by temporal lobe herniation through the tentorium (uncal herniation) [16]. Finally, diencephalic injuries typically result in small and reactive pupils; since this shape is also seen in most types of metabolic encephalopathy, it has limited value in identifying structural causes of coma [15]. The pathways that mediate eye movements run parallel to the RAS at the level of the paramedian tegmentum of the upper part of the brainstem. In comatose patients, the study of oculomotor responses has great value for localisation. Spontaneous and evoked eye movements should be observed. Slow roving eye movements are typical of metabolic encephalopathy and, if conjugate, are expression of an intact ocular motor system. Conjugate lateral deviation of the eyes is typically observed with destructive or irritative lesions: in the former case, the lesion generally involves the frontal eye fields and causes an homolateral deviation of the eyes; in the latter case, the same cortical injury may cause deviation of the eyes away from the side with the lesion, as the result of epileptic activity [15]. The interruption of descending cortico-bulbar pathways for gaze control, passing through the thalamic internal medullary lamina, rather than the internal capsule, may produce “wrong-way eyes”, which deviate away from the side with the lesion [26]. Conjugate vertical deviation of the eyes may be due to lesions of the tectal nuclei. Nonconjugate eye deviation, generally with concomitant strabismus, can be a result of monolateral lesions of oculomotor cranial nerves of the medial longitudinal fasciculus (near the midline tegmentum) on that side, between the abducens and oculomotor nuclei. Bilateral lesions of the medial longitudinal fasciculus impair adduction of both eyes, as well as vertical oculocephalic and vestibulo-ocular eye movements, a condition different from bilateral oculomotor nucleus or nerve injuries, with the preservedpupillary light responses [15]. In light of the above considerations, eye movements in a comatose patient can be summarised as follows: spontaneous roving eye movements, indicating the integrity of the brainstem; skewed deviation, suggesting a brainstem lesion; forced deviation of the eyes to one side, generally indicating an ipsilateral hemispheric or contralateral pons lesion; eye deviation away from the side of the lesion, due to seizures [18].
The oculocephalic reflex is tested in comatose - or severely lethargic - patients by keeping their eyes open and briskly rotating the head side-to-side and up–down. The nerves involved in this reflex, known as the “doll’s eyes reflex”, are the oculomotor nerves and the eighth pair of cranial nerves. If the brainstem is intact, such as in comatose patients due to metabolic encefalopathy, the eyes rotate conjugately in the opposite direction to the head movement. If brainstem gaze centres are damaged, this reflex is reduced or absent [17, 27]. Therefore, “doll’s eye reflex” observation in comatose patients indicates brainstem integrity.
Oculovestibular testing with cold/warm (than body temperature) water infusion is a simple test to check integration of ocular and vestibular pathways. After trauma to the external ear canal and tympanum have been excluded, the patient’s head should be placed at 30° up from horizontal, and cold/warm water infused into the external auditory canal. In a comatose patient with an intact lower midbrain and pons, eyes will tonically and conjugately deviate towards the side of the cold irrigation and away from the side of the warm irrigation [18, 28]. Normally, evoked conjugate eye movements while testing the reflex indicate that the centres of horizontal gaze and median longitudinal fasciculi are intact. A brainstem lesion interrupting the medial longitudinal fasciculus will instead result in the disconjugated abduction of the eye ipsilateral to the cold irrigated ear, but in failure to the adduction of the opposite eye. Conplete absence of oculovestibular responses, not related to drugs intoxication, is a sign of poor prognosis in coma [14, 29, 30].
Breathing patterns should be carefully evaluated, to identify the coma depth. Gradual deterioration from the periodic breathing (cluster or Cheyne-Stokes) to tachypnea and to irregular breathing and gasping with long, irregular apneic periods [14] may occur in the case of widespread supratentorial lesions, deep bilateral brain lesions and metabolic diseases. The Cheyne-Stokes periodic pattern has been attributed to the isolation of the breathing centres of the brainstem, which renders them more sensitive to CO2. As the result of hyperventilation, blood CO2 levels fall below the concentration required to stimulate the regular breathing centres, and breathing gradually stops; CO2 is then increased during the apnea exceeding the respiratory threshold, and the cycle starts over again. When this pattern is present, it is usually not considered a sign of poor outcome, unless other types of pathological breathing, indicating the presence of structural damage to the brainstem, appear. Lesions of the inferior part of the midbrain or of the pontine tegmentum can cause a central neurogenic hyperventilation, characterised by an increase in the respiratory frequency (>40 acts per minute) and in the depth of the breathing, resulting in alkalosis. This pattern suggests the release of the reflex mechanisms responsible for respiratory control in the lower part of the midbrain. Lower pontine lesions may cause an apneustic breath (a pause of 2–3 s following a full inspiration). In the case of injuries to the dorso-medial part of the bulb, the respiratory rhythm becomes chaotic, irregularly interrupted and each breath varies according to frequency and depth (Biot’s breathing pattern) [26], considered a sign of poor prognosis.
Motor responses to pain stimulation is a fundamental indicator of the anatomical site of the brain lesion. An asymmetrical motor response may be suggestive of damage to one cerebral hemisphere. This reflects the importance of performing a bilateral stimulation, since the paralysed limb, often lying extrarotated on the bed, may not respond to the nociceptive stimulus (e.g. in hemiplegia); in this case, stimulation of the sole of the foot can evoke the Babinski sign.
Lesions of the upper part of the midbrain are often clinically characterised by a decorticated posture, both at rest as well as after nocicpetive stimulus, with the upper limbs flexed and the lower limbs extended with toes flexed downwards.
On the other hand, lesions in the lower part of the midbrain or in the upper part of the pons are characterized by a decerebrated posture, with extension of both the upper and lower limbs. The anatomical dividing line between these two postures, decorticated and decerebrated, is the red nucleus in the ventromedial part of the midbrain, responsible for the control of muscle tone in flexor muscle groups of the upper limbs: in a patient with a decorticated posture the red nucleus is intact. Clinical evolution from a decorticated to a decerebrated posture is generally associated with a poor prognosis, since it suggests a rostro-caudal degeneration of the brainstem [16].
Despite the several types of brain injuries that can be responsible for coma, the mechanisms causing consciousness alteration are essentally two: a) the direct damage extension to the diencephalon and midbrain and b) more frequent, the lateral and downward displacement of the subthalamic structures and upper part of the brainstem, with or without herniation of the medial part of the temporal lobe through the tentorium. The term herniation refers to the dislocation of a part of the cerebral or of the cerebellar hemispheres from their normal position to an adjacent compartment, at transfalcial or transtentorial level. Transtentorial herniations are classified in: a) central herniation, with downward dislocation and bilateral compression of the upper portion of the brainstem; b) unilateral dislocation of the medial temporal lobe, including the uncal gyrus, through the tentorial opening. The unilateral herniation causes the “uncal syndrome”, characterised in the early stages by somnolence with unilateral pupillary dilation, usually homolateral to the mass provoking the dislocation of other structures and consequent to the compression of the oculomotor nerve by the uncal gyrus or by its stretching or deviation over the clivus or against the posterior cerebral artery. The time of dislocation development has important clinical and prognostic value; in case of acutely developed masses (tumours with important cerebral oedema, intraparenchymal haematomas), a 3–5 mm horizontal dislocation is associated with a soporous state, a 5–8 mm displacement with stupor, and a displacement greater than 8–9 mm with a coma state [15, 16]. Other types of herniations are represented by: dislocation of cerebellar hemispheres (tonsillar herniation) through the foramen magnum, with the typical clinical manifestations of diseases of the posterior cranial fossa (neck pain, rigor nucalis, head inclination, dysphagia, alterations in heart rhythm and breathing); subfalcial herniation characterised by displacement of the brain (typically the cingulate gyrus) below the free edge of the falx cerebri, due to raised intracranial pressure; ascending transtentorial herniation, in which SOLs in the posterior cranial fossa cause an upper displacement of the superior parts of the cerebellum through the tentorial notch [31].
Acute Intracranial Hypertension Syndrome (AIHS) deserves a separate mention for its clinical and prognostic relevance, being a medical emergency that requires prompt diagnosis and management. AIHS is defined as the persistent increase of Intra Cranial Pressure (ICP) above 20 mm/Hg, for longer than 5 min and in a patient who is not being stimulated. AIHS commonly occurs in acute brain injury related to trauma, ischaemia or haemorrhage and it is associated with a poor outcome, regardless its etiology [32, 33]. Intra Crania Hypertension (ICH) has been sistematically categorised in four categories, according to the aetiology and pathogenic mechanisms: parenchymatous ICH with an intrinsic cerebral cause; vascular ICH caused by altered cerebral blood circulation; ICH caused by altered cerebrospinal fluid dynamics; and idiopathic [34]. A coma preceded by headache, recurrent vomiting, marked hypertension, papillary oedema, and retinal haemorrhages is expression of ICH, often due to cerebral haemorrhage or to rapidly evolving SOLs, such as glioblastoma and cerebral lymphoma. The early diagnosis of these presenting signs and symptoms is important to allow a sudden medical and/or surgical intervention and to avoid the evolution of a deep coma.
5 Neurobehavioural Rating Scales
The Glasgow Coma Scale (GCS), created by Teasdale and Jennett in 1974 [35] in an attempt to bring uniformity to the clinical evaluation of disorders of consciousness, is the most widely used scale to assess the three aspects of a patient’s responsiveness (eye, verbal, and motor ) to external stimuli. The global numerical score obtained from this scale ranges from a maximum of 15 points (full consciousness) to a minimum of 3 points (deep coma). GCS is a very important tool for assessing coma severity, even though it loses its discriminative value in intubated and sedated patients. Furthermore, a criticism to GCS is the poor scoring of the brainstem functionality. Recently, to provide more information regarding the coma severity and prognosis in patients with traumatic brain injury, the arithmetic combination of GCS scores with pupillary response to light has been proposed (GCS-P) [36]. The Pupil Reactive Score (PRS) has a value of 2 points if both pupils are unreactive, 1 if only 1 pupil is unreactive and 0 if both pupils normally react to light. Since the total GCS score can range from 3 to 15, after PRS score subtraction from the GCS, the GCS-P has a possible range of values from 1 to 15. Another coma scale for the assessment of patients with consciousness disorders is the Full Outline of Unresponsiveness (FOUR) score. This coma scale has four testable components (eye response, motor response, brainstem reflexes and respiration) that can be rated even when in intubated patients. The resulting FOUR score is a good predictor of a poor outcome in a critically ill patient and can detect the occurrence of brain death [25, 37].
The Glasgow Outcome Scale (GOS) is the most widely used and accepted measure of outcome following head injury. In the first version of the GOS, patients with a brain injury can be divided into five categories on the basis of the objective degree of recovery: 1, death; 2, vegetative state; 3, severe disability; 4, moderate disability; 5, good recovery [38].
An extended version of the GOS (GOS-E) has been proposed, consisting of eight categories: 1, death; 2, vegetative state; 3, lower severe disability; 4, upper severe disability; 5, lower moderate disability; 6, upper moderate disability; 7, lower good recovery; and 8, upper good recovery [39]. The clinical scales for the evaluation of consciousness disorders are shown in Table 46.3.
6 EEG Patterns in Coma
To accurately describe the EEG of a comatose patient, several critical points, such as the characteristics of background activity (frequency, continuity and reactivity) and the presence of peculiar EEG patterns need to be taken into account, some of which have a specific prognostic value. With the purpose of uniforming and standardising the EEG description in critically ill patients, the American Clinical Neurophysiology Society recently published a reference paper for the EEG terminology in critical care [40].
6.1 Background Activity
Background EEG activity in comatose patients shows a diffuse or localised slowing, which progressively increases in relation to the degree of the encephalopathy responsible for consciousness impairment (Fig. 46.1). As coma state deteriorates, the background activity progressively decreases in amplitude until attenuation (period of activity >10 μV but <50% of the background voltage) or suppression (background activity <10 μV) of the cortical bioelectrical activity occurs (Fig. 46.2). These background changes in EEG are similar to those recorded when the depth of anaesthesia or sedation is increased; thus, the first characteristic to describe background activity is its predominant frequency (delta, theta, alpha, or beta) and distribution, with particular regards to its symmetry/asymmetry. A coma EEG tracing can be symmetrical or asymmetrical; asymmetry is defined as mild (<50% amplitude or 0.5–1 Hz frequency asymmetry) or marked (>50% amplitude or >1 Hz frequency asymmetry), and it must be present for most of the recording time (Fig. 46.3). Other important characteristics of the background activity are the voltage - classifiable as normal (>20 μV), low (10–20 μV), or suppressed (<10 μV) - and the continuity. The background continuity has a significant favourable prognostic value and, accordingly, a prolonged EEG recorded in ICU can be classified into five main categories (Fig. 46.4):
-
Continuous—background activity uninterrupted by periods of attenuation or suppression.
-
Near continuous—periods of attenuation/suppression <10% of the recording.
-
Discontinuous—periods of attenuation/suppression from 11 to 49% of the recording.
-
Burst-attenuation/burst-suppression—>50% of the recording is attenuated/suppressed.
-
Suppression—the entire recording period contains suppression of background activity.
Changes of background activity during various levels of coma. (a–c) continuous theta-delta diffuse activity progressively decreases in frequency, synchronisation and amplitude. As coma deepens, burst-suppression pattern appears (d) and then the background activity is attenuated (e) or completely suppressed (f)
6.2 EEG Reactivity
EEG reactivity to visual, auditory and nociceptive stimuli should always be tested; it consists of changes in amplitude or frequency of the background activity, or in its attenuation. The EEG response to stimuli can be present, absent, or unclear (Figs. 46.5 and 46.6). The appearance of a muscle response or blinking after stimuli should not be considered a form of EEG reactivity. The absence of any reactivity is a sign of a poor prognosis, with the exception of toxic and iatrogenic coma; conversely, EEG reactivity preservation is considered a neurophysiological marker of a more favourable outcome.
Samples of EEG reactivity to nociceptive stimuli. In (a and b), the nociceptive stimulus induces the appearance of delta slowings predominant anteriorly, while in (c) pain induces a marked diffuse attenuation of tracing (a, LFF = 0.53 Hz, HFF = 70 Hz, 70 μV/cm; b, LFF = 0.53 Hz, HFF = 70 Hz, 100 μV/cm; c, LFF = 0.53 Hz, HFF = 50 Hz, 70 μV/cm)
The evaluation of EEG reactivity in critically ill patients is not always easy. Technicians should note and transmit all the information regarding the applied stimuli (e.g. modalities, time intervals) to the reporting physicians and monitor any reaction, such as muscle contractions, automatic eye movements, changes in cardiac and respiratory rhythm, and any other reflex and/or autonomic response directly or indirectly related to cortical activity. Pain stimuli are routinely included in the neurological examination of comatose patients (nasal tickling, trapezius squeeze, skin pinches, pressure to fingernail, nipple pinching), with nociceptive stimuli appearing to best highlight EEG reactivity. Tsetsou et al. investigated the effects of standardised nociceptive stimuli in comatose patients unreactive to auditory stimuli, using three different painful stimuli: bilateral nipple pinching, nasal pinprick and bilateral fingernail compression. In this prospective study, it was demonstrated that bilateral synchronous nipple pinching appears to be the most nociceptive method to test EEG reactivity [41]. Admiraal et al. recently performed a systematic review aimed at identifying definitions of EEG reactivity and testing methods and found that many different protocols exist; however, the definition of EEG reactivity is neither uniform nor replicable. Therefore, standardisation of the stimulation protocol (stimuli used, duration and intensity of each stimulus) and a more precise definition of EEG reactivity are required [42]. Automated quantitative EEG approaches based on probabilistic description of spectral temporal symmetry potentially improve the objective evaluation of the EEG reactivity and thus assisting in the prediction of the clinical outcome [43].
6.3 Peculiar Coma EEG Patterns
6.3.1 Periodic and Rhythmic Patterns: Epileptiform Activity
The difference between periodic and rhythmic patterns is based on the presence or absence of an interval between two consecutive waveforms. Periodic activity is generally characterised by discharges, which are defined as waves with no more than three phases or any wave lasting 0.5 s or less (discharges are the opposite of bursts, which are defined as waveforms with at least four phases that last more than 0.5 s). Periodic discharges are therefore characterised by the repetition of a relatively uniform waveform at near regular intervals. Rhythmic EEG patterns are represented by the repetition of delta waves with relatively uniform morphology and duration, without an interval between the consecutive waveforms (Fig. 46.7).
It should be noted that, according to ACNS-standardised critical care EEG terminology [40], an EEG pattern can be qualified as periodic or rhythmic as long as the pattern continues for at least six cycles (1/s for 6 s or 3/s for 2 s).
Based on their localisation, periodic or rhythmic EEG patterns can be:
-
Generalised (G: Bilateral, bisynchronous and symmetrical).
-
Lateralised (L: Unilateral and bisynchronous, but asymmetrical, focal, regional, or hemispheric patterns).
-
Bilateral Independent (BI: two asynchronous lateralised patterns, one in each hemisphere).
-
Multifocal (Mf: at least three independent lateralised patterns in both hemispheres).
For generalised patterns, it is also necessary to include additional information regarding the predominant site of appearance (frontal, central, or occipital) while, for lateralised patterns, it is important to specify the symmetry vs. asymmetry and the most involved lobes (Figs. 46.8 and 46.9).
Epileptic activity in the EEG of comatose patients may also be recorded as polyspikes, spikes, or sharp waves followed by a slow wave in a regularly repeating and alternating pattern, without any interval between one complex and the next. Periodic and rhythmic EEG patterns and epileptic abnormalities have already been described in detail in Chap. 13.
A detailed EEG interpretation using standardised terminology is extremely important, especially in comatose patients. A large, multicentre study evaluating the effects of periodic and rhythmic patterns on seizure risk in critically ill patients highlighted that Lateralised Periodic Discharges (LPDs), Lateralised Rhythmic Delta Activity (LRDA), and Generalised Periodic Discharges (GPDs) are associated with seizures, unlike Generalised Rhythmic Delta Activity (GRDA) [44]. Punia et al. demonstrated that patients with LPDs on continuous EEG during coma are at least seven times more likely to develop epilepsy following an acute brain insult [45].
The definition and classification of Status Epilepticus (SE) by the International League Against Epilepsy (ILAE) Task Force considers “EEG correlates” as one of four axes (1, semiology; 2, aetiology; 3, EEG correlates; and 4, age) and emphasises that EEG should be performed as early as possible [46].
The ILAE recommends using EEG in an emergency setting with repeated recordings, to highlight the eventual evolution of SE from one form to another. Currently, no evidence-based EEG criteria for SE exist, and none of the ictal EEG patterns of any type of SE are specific; however, EEG is considered indispensable in the diagnosis of Non-Convulsive SE (NCSE).
For the description of EEG patterns in SE, the ILAE Task Force [46] has proposed the following main parameters:
-
Location (generalised, lateralised, bilateral independent, or multifocal).
-
Type (periodic discharges, rhythmic delta activity, or epileptic activity).
-
Morphology (sharpness, number of phases, amplitude, and polarity).
-
Time-related features (prevalence, frequency, duration, onset, and dynamics).
-
Modulation (spontaneous or stimulus-induced).
-
Effects of drugs on the EEG.
Various EEG criteria have been used to identify comatose patients with NCSE, the true incidence of which still remains unknown. The original “Salzburg Consensus Criteria” were modified in accordance with the standardised critical care terminology of the ACNS [40, 47,48,49].
First, the EEG changes that fulfil the modified Salzburg criteria for NCSE should be continuously present for >10 s; these changes can be represented by Epileptiform Discharges (EDs: spikes, polyspikes, sharp waves, sharp-and-slow wave complexes; the frequency of EDs may be >2.5 or <2.5 Hz) or by Rhythmic Delta Activity (RDA: rhythmic activity <4 Hz; the duration of one cycle should vary by <50% from the duration of the subsequent cycle for the majority of cycle pairs to qualify as rhythmic) [40].
Other parameters defining EEG patterns of NCSE are:
Evolution: at least two unequivocal, sequential changes in frequency (at least two consecutive changes of at least 0.5/s, e.g. from 2 to 2.5/s or from 3 to 2/s), morphology (at least two consecutive changes to a novel morphology), or location (sequentially spreading into or out of at least two different IS 10–20 electrode locations). The criteria for evolution must be reached without the pattern remaining unchanged in frequency, morphology, or location for 5 min or longer [40].
Typical ictal spatio-temporal evolution, which consists of incrementing onset (increase in voltage and change in frequency), evolution of the pattern (change in frequency and location), or decrementing termination (voltage and frequency).
Fluctuation: >3 changes, not more than 1 min apart, in frequency (by at least 0.5/s); >3 changes in morphology; or >3 changes in location, which do not qualify as evolving.
Response to intravenous antiepileptic drugs (IV AEDs): the response to IV AEDs should be tested clinically and by EEG (Figs. 46.10 and 46.11). Clinical improvement is defined as the best performance in one of the following three domains: “say your surname”, “repeat 1, 2, 3”, and “raise your arms”; if the patient does not respond, the procedure must be repeated following strong tactile stimuli. EEG improvement is defined as a reduction in the pathological pattern to occasional, i.e. 1-9% of epochs.
In comatose patients without any known epileptic encephalopathy, at least one of the following criteria should be fulfilled for the diagnosis of NCSE:
-
1.
EDs >2.5 Hz (i.e. >25 EDs in a 10-s epoch).
-
2.
Typical ictal spatio-temporal evolution of EDs or RDA (>0.5 Hz).
-
3.
Subtle ictal clinical symptoms (minor twitching of the mouth, periorbital region, or extremities) in close temporal relation to EDs or RDA >0.5 Hz.
If the EDs have a frequency <2.5 Hz or there is only RDA with or without fluctuations, the clinical situation should be carefully evaluated and the clinical and EEG response to IV AEDs should be documented. There are four possible responses: no clinical or EEG improvement, only EEG improvement, only clinical improvement, or EEG and clinical improvement. According to the modified Salzburg Consensus Criteria, for clinical practice, all four constellations qualify for NCSE, while for research projects, patients qualify for NCSE only if EEG and/or clinical improvement is documented (Fig. 46.12) [47, 48].
6.3.2 Spindle Coma and Beta Coma
The presence of normal sleep transients (i.e. vertex sharp waves, K-complexes, and spindles) in the slow EEGs of comatose patients with acute encephalopathy may be considered a prognostic biomarker for both survival and functional recovery. Chatrian et al. (1963) [50] first described an EEG pattern in patients with acute traumatic encephalopathy characterised by vertex wave, K-complex, and sleep spindle sequences (11–14 Hz), which was named “spindle coma”. In patients with head injury, it has been hypothesised that the spindle coma may occur due to a pontomesencephalic junction lesion, with functional preservation of the cortex. This pattern was also later described in patients with non-traumatic coma [51] and it is recognised as having a good prognostic value. If the spindle coma pattern is reactive to external stimuli, the outcome is obviously better, although in most cases it remains uncertain; nevertheless, the prognostic value of this pattern is sometimes often uncertain, since the prognosis depends above all on the underlying aetiology of the coma [52]. A recent retrospective study investigating the early presence of sleep spindles in the cEEGs of 34 children in the first 24 h after resuscitation from cardiac arrest reported that spindles were recorded in approximately 30% of children and were associated with a favourable neurological outcome at 6 months [53].
The “beta coma” pattern is characterised by the presence of diffuse, frontally dominant, beta activity ranging from 12 to 16 Hz. This pattern is most commonly induced by intoxication or withdrawal from benzodiazepines or barbiturates [54], but it may also be the consequence of an acute brainstem lesion (Fig. 46.13).
6.3.3 Alpha, Alpha-Theta, and Theta Coma Patterns
The term Alpha Coma (AC) refers to an EEG coma pattern characterised by the presence of diffuse alpha frequency activity; when alpha activity is mixed with theta frequencies, the pattern is named Alpha-Theta Coma (ATC), whereas when the rhythmic diffuse activity falls within the theta band range, the pattern is named Theta Coma (TC) (Fig. 46.14).
The most well-known and studied pattern is AC, which was first described in 1953 by Loeb and Poggio in patients with pontomesencephalic haemorrhage [55] and, subsequently, in patients with other acute encephalopathies (anoxic, traumatic, toxic, and dysmetabolic) [56, 57]. An AC pattern following cardiac arrest or traumatic brain injury is characterised by a monomorphic and unreactive alpha activity with a frequency of 8–13 Hz and an amplitude of 10–50 μV, diffuse but predominantly in the frontal regions. If the activity is slower (4–7 Hz), the pattern is defined as ATC or TC. When the AC is due to toxic encephalopathies (overdoses of barbiturates, benzodiazepines, anaesthetics, or antidepressant drugs), beta frequencies may be superimposed on the alpha activity, which may sometimes be predominant in the posterior regions. Given the variety of causes, the AC pattern likely arises from different pathophysiological interactions. In the case of brainstem lesions, there is a deafferentation of thalamo-cortical pathways releasing autonomous cortical alpha rhythm generated from the ascending RAS. A study comparing the alpha pattern between healthy subjects and comatose patients showed a lack of interhemispheric coherence in AC, supporting the hypothesis that when a significant thalamo-cortical disruption is determined, the cortical pacemakers operate independently in each hemisphere [58]. It has also been shown that alpha frequencies can be produced by different generators and networks in normal subjects and patients with AC [59]. Following diffuse cerebral hypoxia or diffuse post-traumatic brain lesions, the cortex is destroyed with preservation of thalamic and brainstem structures; in this case, the alpha activity recorded on the scalp originates from subcortical structures. Finally, drugs or sedatives at toxic doses may produce an AC pattern by a direct effect on cortical alpha generators, with or without impairment of ascending modulating inputs [56].
AC is generally considered a biomarker for poor prognosis; however, outcome also depends on the underlying aetiology of the coma (i.e. a poor prognosis for anoxia or trauma, but a better one for toxic or metabolic encephalopathies). Berkhoff et al. [57] performed a prospective study regarding clinical, EEG, and Somato Sensory-Evoked Potential (SSEP) findings in a series of patients with postanoxic ATC and also reviewed 283 cases of postanoxic ATC reported in the literature. These authors described two types of ATC: incomplete and complete. The incomplete ATC is characterised by occipital or diffuse, non-monotonous, hypo-reactive alpha activity; SSEP are usually normal and coma with usually normal brainstem reflexes. Conversely, the complete ATC is characterised by diffuse, frontally predominant, monotonous, reactive alpha activity; SSEP usually altered or absent and deep coma, with usually absent brainstem reflexes.
According to Berkhoff et al. [57], the combination of EEG, SSEP, and clinical findings improves the prognostic evaluation of postanoxic ATC; a full recovery is possible in patients with incomplete ATC, whereas complete ATC is invariably associated with a poor outcome. The prognostic significance of complete and incomplete variants of ATC has been shown in many recent studies, almost always conducted in patients with postanoxic coma [60, 61].
6.3.4 Burst-Attenuation and Burst-Suppression Patterns
The classic definition of a burst-suppression pattern is: “an EEG pattern in which there are generalised and synchronous bursts of high-voltage and mixed-frequency activity alternating with periods of suppression of this activity” [54].
This pattern is observed in comatose patients with diffuse cerebral anoxia (following cardiac arrest), during hypothermia, or as a result of excessive dosage of anaesthetic agents or sedative drugs.
The standardised terminology for EEG in critical care proposed by ACNS [40] specifies the characteristics of the pattern: bursts must average more than 0.5 s, have at least four phases, which can last up to 30 s; the interval between two bursts may be with attenuation (periods of lower voltage >10 μV but <50% of the background voltage) or with suppression (periods of lower voltage are <10 μV); to define a pattern of burst-attenuation or burst-suppression, it is necessary that more than 50% of the recording consists of attenuation or suppression, with alternating bursts. Furthermore, it is necessary to report the typical duration of the bursts and interburst intervals, morphology (sharpness) of a typical burst, and the presence or absence of highly epileptiform bursts.
Highly epileptiform bursts are considered present if multiple epileptiform discharges or rhythmic patterns (potentially ictal) occur within the majority (>50%) of bursts, at an average of 1/s or faster (Fig. 46.15).
In addition to ACNS classification, the EEG patterns with bursts may be subdivided into those with identical bursts and those without. Bursts are “identical” if they have the same amplitude, duration and shape in defined EEG epochs; interburst intervals must also be identical. Burst-suppression with identical bursts is a distinct pathological EEG pattern; it is exclusively observed in comatose patients following cardiac arrest and is invariably associated with a poor outcome (Fig. 46.16) [62, 63].
6.3.5 Electrocerebral Inactivity
The patterns with attenuation and suppression defined above must be distinguished from Electro Cerebral Inactivity (ECI) (the use of terms such as “electrocerebral silence, flat, or isoelectric EEG” to define this condition is discouraged). ECI is characterised by the absence an identifiable electrical activity of cerebral origin over 2 μV (peak to peak), spontaneous or stimulated, in all regions. The ECI is observed in brain death and, for its correct identification, the sensitivity must be increased to a maximum of 2 μV/mm (Fig. 46.17) [64].
7 EEG Patterns in Vegetative State and Minimally Conscious State
The EEGs in many patients with VS may show a continuous generalised polymorphic theta-delta activity, occasionally reactive (with attenuation) only to nociceptive stimuli. In some patients, the background activity is of very low voltage or suppressed. In <10% of patients with VS, a background rhythm of alpha-theta frequency has been described, without demonstration of reactivity at eyes closing. The recording of ictal or interictal epileptiform abnormalities is unusual. In rare cases, patterns with GPDs, LPDs, triphasic waves, and alpha coma have been described [65].
In patients with MCS, the background activity is more frequently preserved and reactive and the sleep architecture is more recognisable (Fig. 46.18).
Forgacs et al. [66] studied the preservation of the EEG organisation during wake and sleep in a large series of patients with VS or MCS (plus and minus). The EEGs were recorded using a video-EEG system and visually reviewed by clinical neurophysiologists. Wake EEG background was classified into four categories based on the degree of abnormalities observed:
Normal (posterior dominant alpha rhythm at 8–12 Hz, amplitude asymmetry not higher than 50% between hemispheres, normal anteroposterior gradient, no focal or hemispheric slowing).
Mildly abnormal (posterior dominant rhythm asymmetrical or mildly slowed, anteropeterior gradient not well organised, mild focal or hemispheric theta slowing).
Moderately abnormal (posterior rhythms of theta frequency at 4–7 and/or presence of focal or hemispheric theta-delta slowing).
Severely abnormal (diffuse background activity <4 Hz).
During sleep, the presence or absence of characteristic elements of sleep architecture was assessed (vertex waves, spindles, patterns of slow waves, and REM sleep). The results were heterogeneous and related to each individual clinical condition and aetiology of DOC; however, overall, the percentage of moderately or severely abnormal wake EEG decreased from the VS to the MCS minus and MCS plus. Sleep architecture abnormalities were present in all subjects; vertex waves and spindles were the most preserved sleep pattern, while REM appeared in only 39% of subjects. This study also attempted to elucidate a correlation between the EEG pattern and the results of an fMRI examination during a cognitive task. All patients with fMRI evidence of following covert commands consistently demonstrated well-organised EEG background during wakefulness and spindling activity during sleep [66].
Using high-density EEG, Landsness et al. [67] studied the sleep of 11 patients with VS or MCS with the aim of correlating the EEG changes during sleep to the behavioural changes in vigilance. All patients with MCS showed clear EEG changes associated with behavioural sleep periods. In contrast, patients with VS preserved behavioural sleep (eyes closed) but the EEG patterns remained unchanged during periods with closed eyes, as compared with periods of behavioural wakefulness.
A recent study by Estraneo et al. [68] proposed a modified classification of the EEG patterns of VS and MCS patients into five categories: normal, mildly abnormal, moderately abnormal, diffuse slowing, and low voltage (defined as a predominant slow EEG activity <20 μV over most brain regions). The authors also analysed EEG reactivity following eye opening and closing and following tactile, acoustic, and nociceptive stimulation. The results of this study demonstrated that EEG abnormalities were more severe in VS than in MCS plus or MCS minus and are prevalent in anoxic aetiology. Reactivity to visual and acoustic stimulation was significantly more frequent in MCS plus and MCS minus than in VS patients. The patients with normal or mildly abnormal background activity showed higher scores in the Coma Recovery Scale-Revised.
In conclusion, EEG - a time-resolved, low-cost, widespread, and easily reproducible diagnostic technique - may be a valid tool for the classification of patients with persistent DOC and may support neuroimaging in defining the prognosis. However, in addition to the inspective analysis of conventional EEG, high-density EEG recordings should be implemented, as well as the correlation between EEG and other neurophysiological techniques and the quantitative analysis of recorded signals. Spectral power analysis revealed that alpha and theta power are significantly lower in VS than in MCS patients, whereas delta power shows the opposite behaviour. Sitt et al. [69] identified a series of measures that, when combined, allow the classification of the state of consciousness. The authors showed that low-frequency power, EEG complexity, and information exchange constitute the most reliable signatures of consciousness, concluding that a reduced set of EEG measures could ultimately serve as a reliable bedside tool to probe consciousness in patients with DOC.
8 EEG in Coma Prognosis
In patients with Acquired Brain Injury (ABI), it is relevant to focus on the prediction of early neurological improvement; however, when patients are still sedated, clinical examination is obviously unreliable, and only instrumental tests are available. Among these, neurophysiological tests (EEG and SSEPs) are important, since they are an extension of clinical examination and integrate with neuroimaging. With respect to the prognostic use of EEG, at least two factors should be considered: the grading system and potential confounding factors (Table 46.4).
It is well-known that the interpretation of EEGs requires more training than the evaluation of other prognostic indicators such as clinical examination and SSEPs, and non-expert interpretation of EEGs introduces the risk of lowering its overall prognostic value. Most grading systems developed decades ago [70,71,72] evaluated a limited number of EEG features, and standardised terminology had not been adopted; therefore, it is reasonable to assume that the EEG reporters could have been biased by these factors. In particular, grading systems and definitions of malignant and benign EEG patterns varied among studies. Together, these factors hinder accurate recommendations and meta-analysis. For instance, in the first guidelines concerning prognosis of comatose survivors following Cardiac Arrest (CA) [73], EEG was not included among the prognostic indicators, since its prognostic accuracy was considered insufficient based on evidence; thus, standardised terminology evaluating all important features would be preferable to assess which individual features of the EEG are the most predictive. A classification scheme based on clear, strict and standardised definitions of patterns should be used to facilitate comparison among different studies. The variability in classification and rating of the EEG findings has been partly addressed by the introduction of standardised critical care EEG terminology by the ACNS, which has shown high inter-rater agreement, especially for periodic or rhythmic activity [40]. According to this classification, we can identify, for prognostic purposes, the following main EEG patterns: continuous, near continuous, discontinuous, epileptiform discharges, burst-attenuation/burst-suppression, attenuation/suppression, and electrocerebral inactivity. Concerning potential confounding factors, temperature and sedation must be taken into account. Over the last decade, Therapeutic Hypothermia (TH) with a target temperature of 32–34 °C has become the standard of care in the management of patients following CA and has also been proposed in Traumatic Brain Injury (TBI). Moderate TH to the level of 32 °C does not significantly affect the continuity or voltage of EEGs. Only under a temperature of 29 °C do we observe the progressive appearance of periodic complexes, burst-suppression (around 24 °C), and E3 (around 22 °C) [74]. Artifacts from muscle shivering, mechanical ventilation, or electrical equipment that frequently accompany TH may affect the reliability of EEG interpretation; nonetheless, it is apparent that many EEG patterns seen during moderate TH have similar prognostic implications as when seen during normothermia [75]. More relevant than the effect of body temperature per se are its metabolic effects. A decreased body temperature decreases the activity of hepatic enzymes by 7–22% per degree below 37 °C, which can result in significantly higher levels of anaesthetic and a prolonged effect of neuromuscular blockade, and it may be difficult to know whether residual sedation affects the clinical and EEG reactivity, even when recordings are performed 24 h after normothermia is restored.
Concerning sedation, based on their pharmacological effects, we expected propofol and midazolam to decrease the continuity of the EEG, leading to a false prediction of a poor outcome. Firstly, a distinction should be made between patients surviving CA and the other acquired brain injuries. Comatose patients affected by TBI) are treated at an early stage with high doses of propofol or midazolam to control the intracranial pressure, and this treatment induces burst-suppression patterns on EEG. Instead, the typical dosages of propofol (1–2 mg/kg/h) or midazolam (0.03–0.1 mg/kg/h) used in CA patients did not affect the continuity of the EEG; in these patients, the severity of postanoxic injury influenced the EEG much more than sedative drugs [76]. During rewarming, even if we consider the prolonged duration of sedative drugs, the dose will be even lower. In any case, in this condition, the absence of reactivity and the Episodic Low-Amplitude Events (ELAEs) [77] should not be considered as reliable for the prognosis of a poor outcome.
The main role of the EEG in TBI is the detection of acute seizures immediately following brain injury. The EEG can also be helpful in determining the prognosis but with the limitation of timing, since all these comatose patients are treated at an early stage with high doses of propofol or midazolam to control the intracranial pressure, creating unreliable EEG findings. As a consequence, the presence of malignant patterns (e.g. burst-suppression) should be interpreted with caution, since it may be related to ongoing sedation rather than cerebral injury; however, knowing the effects of sedation on EEG activity, a comparison between the dosage of the sedatives and the expected EEG pattern should be considered. Approximately 1 week after the onset of the post-traumatic coma, the EEG has predictive value for a good outcome in the case of the presence of reactivity [78]. Logi et al. [79], using the Synek classification in the post-acute phase, showed that in the presence of a benign EEG pattern (which included dominant theta and alpha activity, delta activity with sleep spindles, and high-amplitude frontally predominant rhythmic delta activity in a background of alpha and theta activity), patients regained consciousness. The absence of EEG reactivity marks a poor prognosis in TBI patients when associated with severe SSEP alterations [80].
Another important indication to perform EEG with a prognostic aim is the case of a coma state following CA. Recent European guidelines [81, 82] have recognised EEG as a prognostic indicator in Hypoxic–Ischaemic Encephalopathy (HIE) but with caveats owing to the lack of strong statistical evidence from the pooled data of available studies and the newly emerging influence of confounding factors such as sedation, paralysis, and TH. In light of the data published in recent years, the EEG can be useful for both a poor and a good outcome and neurological prognosis. To this end, the classification of different EEG patterns into three categories has been proposed. Highly malignant EEG patterns include suppressed background without discharges, suppressed background with continuous periodic discharges, and burst-suppression background with or without discharges. Malignant EEG patterns include malignant periodic or rhythmic patterns (abundant periodic discharges, abundant rhythmic polyspike−/spike−/sharp-and-waves, unequivocal electrographic seizure), malignant background (discontinuous background, low-voltage background, reversed anterior-posterior gradient), and unreactive EEG (absence of background reactivity or only stimulus-induced discharges). Benign EEG is characterised by the absence of all the malignant features stated above. For proper prognostic use of the EEG, the natural evolution and pathophysiological basis of EEG changes following CA and return to spontaneous circulation should be carefully taken into account. The electrophysiological changes following CA have been studied in several animal models, showing the clear evolution of changes over time including an initial period of complete EEG suppression, a subsequent burst-suppression pattern, and later transition into continuous cortical activity. The duration of EEG suppression and the latency of emergence of a continuous background correlate with neurological outcome and neuropathological injury [83]. Changes in humans may follow a similar pattern, for instance, studies describe similar natural evolution of the EEG signal along with neurological recovery following cardiac and/or respiratory arrest [84].
Thus, different from SSEPs, EEG is a time-dependent indicator because the prognostic value of a single pattern changes over time, at least until 72 h following CA. This factor strongly influences the “optimal” timing of EEG recording and the distinct EEG patterns, assisting with prognostication in post-CA patients. In each time frame, if standardised definitions of EEG patterns are applied, there is at least one EEG pattern that is specific to good and poor outcomes. From a practical point of view, we can distinguish three temporal frames: 12, 24, and 72 h. During the early phase following CA (12 h, Fig. 46.19), continuous and near continuous EEG indicate a good prognosis (false-positive rate, FPR = 0) [75, 85,86,87]. The value of these EEG patterns for a good prognosis at a very early stage following CA is strengthened when the EEG is used in combination with SSEPs. In fact, both EEG (continuous and quasi-continuous) and SSEP (bilaterally absent) patterns have an FPR = 0, but with opposite prognostic significance (indeed each of these findings is mutually exclusive of the other). The EEG and SSEPs recordings in the same patient increase the number of correctly classified cases (65.2%) in comparison with the number of patients classified by each test individually (EEG predicted a good prognosis in 30.5%; SSEPs predicted a poor prognosis in 34.7%). Moreover, continuous and near continuous EEG are always associated with the presence of cortical SSEPs, whereas bilaterally absent cortical SSEPs are always associated with malignant EEG patterns. This consistency of findings increases the reliability of prediction in a single patient. In literature, there have been reports, albeit rarely, of patients with bilaterally absent cortical SSEPs who have recovered consciousness [88], but no indication of the EEG pattern in these patients was reported. The finding of a continuous or near continuous EEG within 12 h following CA in patients with bilaterally absent cortical SEPs requires caution in the interpretation and a repeat SSEPs recording to avoid a false pessimistic prediction. From a pathophysiological point of view, at least during the early stage following CA, the lack of correlation between SSEPs and EEG could be explained by a selective resistance to hypoxia/ischaemia of their generator systems: somatosensory neurons have both “receiving” and “sending” properties, and then the preservation of N20 reflects an intact “receiving mode”; instead, EEG generation mainly reflects multiple cortical synaptic functions, with greater involvement of “sending mode” [89]. Within the first 12 h, continuous and nearly continuous EEG was always associated with the presence of cortical SSEPs, indicating a low degree of severity of hypoxic–ischaemic encephalopathy. At the same time, the bilaterally absent cortical SSEPs were always associated with malignant EEG as an expression of severe hypoxic–ischaemic encephalopathy. Moreover, when malignant EEG was associated with preserved cortical SSEPs, this indicates an intermediate degree of hypoxic–ischaemic encephalopathy and may explain why some of these patients did not have an unfavourable outcome.
At approximately 24 h (Fig. 46.20), the EEG shows less prognostic utility. Continuous quasi-continuous patterns begin to lose the specificity of 100% for good prognosis. Suppression/burst-suppression patterns show a specificity of 100% for poor prediction at 24 h; however, since these EEG patterns occur in a small percentage (4%) of patients with preserved cortical SSEPs [90], the EEG can slightly increase the prediction of a poor outcome as compared with SSEPs. Moreover, at this time point, the suppressed pattern has not yet reached 100% specificity for a poor outcome.
At 72 h, both malignant EEG patterns and bilaterally absent cortical SSEPs indicate a poor prognosis, with an FPR = 0 (Fig. 46.21). This finding suggests two possible scenarios. On one hand, if unfavourable EEG and SSEP patterns are both present, this confirms and strengthens their prognostic value. On the other hand, since malignant EEG occurs in some patients with present SSEPs, this allows the prediction of an unfavourable prognosis in a greater number of patients. Continuous or near continuous patterns in the later time frames usually predict good outcomes; nevertheless, some patients showing continuous and near continuous EEGs in these time frames can have a poor outcome. These errors in prediction can be explained by the occurrence of alpha-theta coma patterns; the pathogenesis of ATC is thought to involve alternative generators and subcortical pathways including the caudate nucleus, amygdala, hypothalamus, brainstem, and basal forebrain [91]. It is conceivable that the organisation of these subcortical circuits, which are responsible for the appearance of a de novo alpha rhythm, does not occur immediately following CA but takes more time to establish, so that a continuous pattern invariably predicts a good outcome only if observed within the first 12 h following CA. There are two possible ways to avoid a false optimistic prediction. Firstly, the SSEP pattern should be taken into account; if cortical responses are absent in both hemispheres, then the prognosis will be poor. If cortical SSEP responses are present, it would be useful to repeat the EEG after a few days. In the case of a true ATC pattern, an evolution towards the malignant patterns (suppressed or low voltage) is to be expected.
Two more features of EEG, reactivity and epileptiform discharges, are time-dependent.
The presence of reactive EEG has a high positive predictive value for a good outcome, with a false positive rate = 0 during early TH (within 12 h of CA), when it is evident despite sedation; however, only a small subgroup of patients with continuous or near continuous EEG shows a reactive EEG in this time frame, likely due to sedation. The absence of reactivity was reported to be indicative of a poor outcome in a prospective study by Oddo and Rossetti (2014) [92], in which all patients with an unreactive EEG during TH went on to have a poor outcome, except for one; however, different findings have also been reported. [63, 87] The absence of reactivity as a negative prognostic indicator should be applied with great caution in the early post-CA period due to the presence of sedation and/or TH. After 48–72 h, when there is less interference from sedation effects, the absence of reactivity becomes more predictive of a poor outcome. One limitation is that all studies exploring the value of EEG reactivity for prognostication evaluated this feature as an “isolated characteristic”. No study included additional analysis of the background EEG patterns. Indeed, a reactive EEG may be associated with a continuous background pattern with physiological rhythms, whereas a nonreactive EEG may represent a low-voltage background pattern. Thus, since the EEG pattern may already contain sufficient information for reliable prognostication, the additional predictive value of reactivity per se is unclear.
Epileptiform activity is usually observed after 24 h [63, 87], but the presence of epileptiform discharges is not invariably predictive of a poor outcome, for instance, in TH-treated patients in any time frame [93,94,95]. This is why many studies do not include epileptiform activity in the prognostic categories of EEG patterns in HIE coma. Evidence that this pattern is less severe than other malignant patterns is demonstrated by the different percentages of absence of cortical SSEPs in epileptiform (around 20%) and noncontinuous patterns (>65% for burst-suppression, suppression, and isoelectric) [87]; thus, it is conceivable that the former reflects a different grade of encephalopathy severity.
It remains an open issue whether continuous EEG (cEEG) should be preferred to standard EEG (30 min) for prognostication in postanoxic coma. cEEG studies [75, 94, 95] have been useful in identifying the times at which various EEG patterns acquire significant prognostic value and in demonstrating that it is possible to predict good as well as poor outcomes at a very early stage. However, cEEG is not as widely available as standard EEG, and it is also more expensive. Crepeau et al. [75] failed to demonstrate that cEEG was a more effective prognostic tool than standard EEG in clinical practice. Standard EEG can be as informative as cEEG as a predictor of outcome, provided that the timing of the recording is considered.
Background amplitude and continuity are the most relevant features in the postanoxic EEG; however, they remain hard to quantitate by a human observer, with far from perfect inter-rater agreement. Quantitative measures for EEG (qEEG) background continuity and amplitude can improve the prediction of outcome in postanoxic coma. EEG background continuity and the amplitude ratio between bursts and suppressions reliably predict the good and poor outcomes of postanoxic coma [76].
In conclusion, in HIE, the EEG has a high prognostic value for both poor and good outcomes. In fact, when specific EEG patterns are found at a certain time from coma onset, it is possible to predict a neurological outcome with 100% specificity. The continuous and near continuous EEG patterns found within the first 12 h following CA are always associated with a good outcome (recovery of consciousness), whereas an isoelectric pattern (amplitude <2 μV) after 12 h, a burst-suppression pattern after 24 h, and a suppression pattern after 48 h from CA are always associated with a poor outcome. Considering the recent recommendation regarding a multimodal approach [81], an association with SSEP recording is suggested for two reasons: to confirm a poor prognosis (increase certainty) and to increase the number of patients correctly classified (increase sensitivity).
References
Bremer F. L’activitè cerebralè au cours du sommeil et de la narcose. Bull Acad R Soc Belg. 1937;IV:68–86.
Moruzzi G, Magoun H. Brainstem reticular formation and activation of EEG. Electroencephalogr Clin Neurophysiol. 1949;1:455–73.
Dempsey EW, Morison RS. The production of rhythmically recurrent cortical potentials after localized thalamic stimulation. Am J Physiol. 1942;135:293–300.
Steriade M. Arousal: revisiting the reticular activating system. Science. 1996;12:225–6.
Jones BE. Arousal systems. Front Biosci. 2003;8:s438–51.
McClenathan BM, Thakor NV, Hoesch RE. Pathophysiology of acute coma and disorders of consciousness: considerations for diagnosis and management. Semin Neurol. 2013;33:91–109.
Maxwell WL, MacKinnon MA, Smith DH, McIntosh TK, Graham DI. Thalamic nuclei after human blunt head injury. J Neuropathol Exp Neurol. 2006;65:478–88.
Grillner S, Hellgren J, Ménard A, et al. Mechanisms for selection of basic motor programs—roles for the striatum and pallidum. Trends Neurosci. 2005;28:364–70.
Laureys S, Schiff ND. Coma and consciousness: paradigms (re)framed by neuroimaging. Neuroimage. 2012;61:478–91.
Schiff ND. Recovery of consciousness after brain injury: a mesocircuit hypothesis. Trends Neurosci. 2010;33:1–9.
Williams ST, Conte MM, Goldfine AM, et al. Common resting brain dynamics indicate a possible mechanism underlying zolpidem response in severe brain injury. Elife. 2013;19:e01157.
Schiff ND, Giacino JT, Kalmar K, et al. Behavioural improvements with thalamic stimulation after severe traumatic brain injury. Nature. 2007;448:600–3.
Giacino JT, Fins JJ, Laureys S, Schiff ND. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol. 2014;10:99–114.
Saper CB, Scammell TE, Lu J. Hypothalamic regulation of sleep and circadian rhythms. Nature. 2005;437:1257–63.
Llinas RR, Steriade M. Bursting of thalamic neurons and states of vigilance. J Neurophysiol. 2006;95:3297–308.
Saper CB, Lumsden AGS. The sensory, motor, and reflex functions of the brainstem. In: Kandel E, Schwartz J, Jessell TM, Siegelbaum SA, Hudspeth AJ, editors. Principles of neural science. 5th ed. New York: McGraw-Hill; 2012. p. 1019–37.
Posner JB, Saper CB, Schiff ND, Plum F. Plum and Posner’s diagnosis of stupor and coma, vol. 401. 4th ed. New York: Oxford University Press; 2007.
Edlow JA, Rabinstein A, Traub SJ, Wijdicks EFM. Diagnosis of reversible causes of coma. Lancet. 2014;384:2064–76.
The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state (1). N Engl J Med. 1994;330:1499–508.
The Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state (2). N Engl J Med. 1994;330:1572–9.
Giacino JT, Kalmar K. Diagnostic and prognostic guidelines for the vegetative and minimally conscious states. Neuropsychol Rehabil. 2005;15:166–74.
Bruno MA, Vanhaudenhuyse A, Thibaut A, Moonen G, Laureys S. From unresponsive wakefulness to minimally conscious PLUS and functional locked-in syndrome: recent advances in our understanding of disorders of consciousness. J Neurol. 2011;258:1373–84.
Cairns H, Olfield HC, Pennybaker JB, Whineridge D. Akinetic mutism with an epidermoid cyst of the third ventricle. Brain. 1941;34:273–90.
Nagaratnam N, Nagaratnam K, Ng K, Diu P. Akinetic mutism following stroke. J Clin Neurosci. 2004;11:25–30.
Wijdicks EF. Neurologic examination of the comatose patient and localization principles. In: Wijdicks EFM, editor. The comatose patient. 2nd ed. New York: Oxford University Press; 2008. p. 64–83.
Chung CS, Caplan LR, Yamamoto Y, et al. Striatocapsular haemorrhage. Brain. 2000;123:1850–62.
Ropper AH, Brown RH. Adams and Victor’s principles of neurology. 8th ed. New York: McGraw-Hill; 2005. p. 1333.
Huff JS, Stevens RD, Weingart SD, Smith WS. Emergency neurological life support: approach to the patient with coma. Neurocrit Care. 2012;17:S54–9.
Jennett B, Adams JH, Murray LS, Grahm DI. Neuropathology in vegetative and severely disabled patients after head injury. Neurology. 2001;56:486–90.
Zheng W, Lui G, Wu R. Prediction of recovery from a post-traumatic coma state by diffusion-weighted imaging (DWI) in patients with diffuse axonal injury. Neuroradiology. 2007;49:271–9.
Young GB. Impaired consciousness and herniation syndromes. Neurol Clin. 2011;29:765–72.
Cremer OL, van Dijk GW, van Wensen E, et al. Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med. 2005;33:2207–13.
Latorre JG, Greer DM. Management of acute intracranial hypertension: a review. Neurologist. 2009;15:193–207.
Iencean SM, Ciurea AV. Intracranial hypertension: classification and patterns of evolution. J Med Life. 2008;1:101–7.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2:81–4.
Brennan PM, Murray GD, Teasdale GM. Simplifying the use of prognostic information in traumatic brain injury. Part 1: the GCS-pupils score: an extended index of clinical severity. J Neurosurg. 2018;128:1612–20.
Wijdicks EFM, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: the FOUR score. Ann Neurol. 2005;58:585–93.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4.
Jennett B, Snoek J, Bond M, Brooks N. Disability after severe head injury: observation on the use of the Glasgow outcome scale. J Neurol Neurosurg Psychiatry. 1981;44:285–93.
Hirsch LJ, LaRoche SM, Gaspard N, et al. American clinical neurophysiology Society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30:1–27.
Tsetsou S, Novy J, Oddo M, Rossetti AO. EEG reactivity to pain in comatose patients: importance of the stimulus type. Resuscitation. 2015;97:34–7.
Admiraal MM, van Rootselaar AF, Horn J. Electroencephalographic reactivity testing in unconscious patients: a systematic review of methods and definitions. Eur J Neurol. 2017;24:245–54.
Hermans MC, Westover MB, van Putten MJAM, Hirsch LJ. Quantification of EEG reactivity in comatose patients. Clin Neurophysiol. 2016;127:571–80.
Rodriguez Ruiz A, Vlachy J, Lee JW, et al. Association of periodic and rhythmic electroencephalographic patterns with seizures in critically ill patients. JAMA Neurol. 2017;74:181–8.
Punia V, Bena J, Krishnan B, Newey C, Hantus S. New onset epilepsy among patients with periodic discharges on continuous electroencephalographic monitoring. Epilepsia. 2018;59:1612.
Trinka E, Cock H, Hesdorffer D, et al. A definition and classification of status epilepticus—report of the ILAE task force on classification of status epilepticus. Epilepsia. 2015;56:1515–23.
Leitinger M, Beniczky S, Rohracher A, et al. Salzburg consensus criteria for non-convulsive status epilepticus—approach to clinical application. Epilepsy Behav. 2015;49:158–63.
Trinka E, Leitinger M. Which EEG patterns in coma are non-convulsive status epilepticus? Epilepsy Behav. 2015;49:203–22.
Leitinger M, Trinka E, Gardella E, et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15:1054–62.
Chatrian GE, White LE Jr, Daly D. Electroencephalographic patterns resembling those of sleep in certain comatose states after injuries to the head. Electroencephalogr Clin Neurophysiol. 1963;15:272–80.
Britt CW Jr. Nontraumatic “spindle coma”: clinical, EEG, and prognostic features. Neurology. 1981;31:393–7.
Kaplan PW, Genoud D, Ho TW, Jallon P. Clinical correlates and prognosis in early spindle coma. Clin Neurophysiol. 2000;111:584–90.
Ducharme-Crevier L, Press CA, Kurz JE, et al. Early presence of sleep spindles on electroencephalography is associated with good outcome after pediatric cardiac arrest. Pediatr Crit Care Med. 2017;18:452–60.
Husain AM. Electroencephalographic assessment of coma. J Clin Neurophysiol. 2006;23:208–20.
Loeb C, Poggio GF. Electroencephalograms in a case with ponto-mesencephalic haemorrhage. Electroencephalogr Clin Neurophysiol. 1953;5:295–6.
Kaplan PW, Genoud D, Ho TW, Jaollon P. Etiology, neurologic correlations, and prognosis in alpha coma. Clin Neurophysiol. 1999;110:205–13.
Berkhoff M, Donati F, Bassetti C. Postanoxic alpha(theta) coma: a reappraisal of its prognostic significance. Clin Neurophysiol. 2000;111:297–304.
McKeown MJ, Young GB. Comparison between the alpha pattern in normal subjects and in alpha pattern coma. J Clin Neurophysiol. 1997;14:414–8.
Abusleme IE, Chen JWY. Alternative cerebral generators and circuitry pathways in alpha coma revealed by independent component analysis. Clin Neurophysiol. 2009;120:686–94.
Fossi S, Amantini A, Grippo A, Cossu C, Boni N, Pinto F. Anoxic-ischemic alpha coma: prognostic significance of the incomplete variant. Neurol Sci. 2003;24:397–400.
Fernandez-Torre JL, Lopez-Delgado A, Hernandez-Hernandez MA, et al. Postanoxic alpha, theta or alpha-theta coma: clinical setting and neurological outcome. Resuscitation. 2018;124:118–25.
Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. Burst-suppression with identical bursts: a distinct EEG pattern with poor outcome in post-anoxic coma. Clin Neurophysiol. 2014;125:947–54.
Spalletti M, Carrai R, Scarpino M, et al. Single electroencephalographic patterns as specific and time-dependent indicators of good and poor outcome after cardiac arrest. Clin Neurophysiol. 2016;127:2610–7.
Kane N, Acharya J, Benickzy S, et al. A revised glossary of terms most commonly used by clinical electroencephalographers and updated proposal for the report format of the EEG findings. Revision 2017. Clin Neurophysiol Pract. 2017;2:170–85.
Kulkarni VP, Lin K, Benbadis SR. EEG findings in the persistent vegetative state. J Clin Neurophysiol. 2007;24:433–7.
Forgacs PB, Conte MM, Fridman EA, et al. Preservation of EEG organization in patients with impaired consciousness and imaging-based evidence of command-following. Ann Neurol. 2014;76:869–79.
Landsness E, Bruno MA, Noirhomme Q, et al. Electrophysiological correlates of behavioural changes in vigilance in vegetative state and minimally conscious state. Brain. 2011;134:2222–32.
Estraneo A, Loreto V, Guarino I, et al. Standard EEG in diagnostic process of prolonged disorders of consciousness. Clin Neurophysiol. 2016;127:2379–85.
Sitt JD, King J-R, El Karoui I, et al. Large scale screening of neural signatures of consciousness in patients in a vegetative or minimally conscious state. Brain. 2014;137:2258–70.
Prior PF, Scott DF. Outcome after severe brain damage. Lancet. 1973;1:770.
Synek VM. Prognostically important EEG coma patterns in diffuse anoxic and traumatic encephalopathies in adults. J Clin Neurophysiol. 1988;5:161–74.
Young GB, McLachlan RS, Kreeft JH, Demelo JD. An electroencephalographic classification for coma. Can J Neurol Sci. 1997;24:320–5.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the quality standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203–10.
Stecker MM, Cheung AT, Pochettino A, et al. Deep hypothermic circulatory arrest: II. Changes in electroencephalogram and evoked potentials during rewarming. Ann Thorac Surg. 2001;71:22–8.
Crepeau AZ, Fugate JE, Mandrekar J, et al. Value analysis of continuous EEG in patients during therapeutic hypothermia after cardiac arrest. Resuscitation. 2014;85:785–9.
Ruijter BJ, Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJAM. The prognostic value of discontinuous EEG patterns in postanoxic coma. J Clin Neurophysiol. 2018;129:1534–43.
Rae-Grant AD, Strapple C, Barbour PJ. Episodic low-amplitude events: an under-recognized phenomenon in clinical electroencephalography. J Clin Neurophysiol. 1991;8:203–11.
Fischer C, Mutschler V. Traumatic brain injuries in adults: from coma to wakefulness. Neurophysiological data. Ann Readapt Med Phys. 2002;45:448–55.
Logi F, Pasqualetti P, Tomaiuolo F. Predict recovery of consciousness in post-acute severe brain injury: the role of EEG reactivity. Brain Inj. 2011;25:972–9.
Amantini A, Grippo A, Fossi S, et al. Prediction of “awakening” and outcome in prolonged acute coma from severe traumatic brain injury: evidence for validity of short latency SEPs. Clin Neurophysiol. 2005;116:229–35.
Taccone FS, Baar I, De Deyne C, et al. Neuroprognostication after adult cardiac arrest treated with targeted temperature management: task force for Belgian recommendations. Acta Neurol Belg. 2017;117:3–15.
Sandroni C, Cariou A, Cavallaro F, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European resuscitation council and the European Society of Intensive Care Medicine. Resuscitation. 2014;85:1779–89.
Koenig MA, Kaplan PW, Thakor NV. Clinical neurophysiologic monitoring and brain injury from cardiac arrest. Neurol Clin. 2006;24:89–106.
Jørgensen EO, Malchow-Møller A. Natural history of global and critical brain ischaemia. Part II: EEG and neurological signs in patients remaining unconscious after cardiopulmonary resuscitation. Resuscitation. 1981;9:155–74.
Tjepkema-Cloostermans MC, Hofmeijer J, Trof RJ, et al. Electroencephalogram predicts outcome in patients with postanoxic coma during mild therapeutic hypothermia. Crit Care Med. 2015;43:159–67.
Carrai R, Grippo A, Scarpino M, et al. Time-dependent and independent neurophysiological indicators of prognosis in post-anoxic coma subjects treated by therapeutic hypothermia. Minerva Anestesiol. 2016;82:940–9.
Grippo A, Carrai R, Scarpino M, et al. Neurophysiological prediction of neurological good and poor outcome in post-anoxic coma. Acta Neurol Scand. 2017;135:641–8.
Pfeiffer G, Pfeiffer R, Isenmann S. Cerebral hypoxia, missing cortical somatosensory evoked potentials and recovery of consciousness. BMC Neurol. 2014;14:82–7.
van Putten MJ. The N20 in post-anoxic coma: are you listening? Clin Neurophysiol. 2012;123:1460–4.
Scarpino M, Lanzo G, Lolli F, et al. Neurophysiological and neuroradiological multimodal approach for early poor outcome prediction after cardiac arrest. Resuscitation. 2018;129:114–20.
Fossi S, Amantini A, Grippo A, et al. Anoxic-ischemic alpha coma: prognostic significance of the incomplete variant. Neurol Sci. 2004;24:397–400.
Oddo M, Rossetti AO. Early multimodal outcome prediction after cardiac arrest in patients treated with hypothermia. Crit Care Med. 2014;42:1340–7.
Amorim E, Rittenberger JC, Baldwin ME, et al. Malignant EEG patterns in cardiac arrest patients treated with targeted temperature management who survive to hospital discharge. Resuscitation. 2015;90:127–32.
Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. Burst-suppression with identical bursts: a distinct EEG pattern with poor outcome in postanoxic coma. Clin Neurophysiol. 2014;125:947–54.
Sivaraju A, Gilmore EJ, Wira CR, et al. Prognostication of post-cardiac arrest coma: early clinical and electroencephalographic predictors of outcome. Intensive Care Med. 2015;41:1264–72.
Acknowledgements
We are very grateful to Dr. Patrizia Pulitano for her help in selecting and editing the EEG figures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mecarelli, O., Brienza, M., Grippo, A., Amantini, A. (2019). Disorders of Consciousness. In: Mecarelli, O. (eds) Clinical Electroencephalography. Springer, Cham. https://doi.org/10.1007/978-3-030-04573-9_46
Download citation
DOI: https://doi.org/10.1007/978-3-030-04573-9_46
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04572-2
Online ISBN: 978-3-030-04573-9
eBook Packages: MedicineMedicine (R0)