Abstract
Prostate cancer (PCa) is a disease in which understandings of what it means to be a man and structural inequalities affecting men from different groups intersect and interact in important and complex ways at every stage of the disease “journey” from first noticing a problem, to seeking help and obtaining a diagnosis through treatment to survivorship. PCa needs to be understood with reference to prevailing norms and enactments of masculinity and to the ethnicity and social class of the man with cancer. This chapter will provide basic information about the nature, symptoms and treatment of prostate cancer. It will discuss these in terms of their psychological and psychosocial impact on men and their families, with a particular focus on how concepts of masculinity as well as ethnicity, sexual orientation and gender identity shape these effects.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Prostate Cancer: The Disease, Gender and Inequality
The prostate is a small gland situated immediately under the bladder, in front of the rectum, and surrounding the urethra (see Fig. 1). It’s function is to produce some of the fluid that nourishes and supports sperm following ejaculation. It grows throughout the lifespan post-puberty due to testosterone, and most men as they age will experience lower urinary tract symptoms (LUTS) due to this benign enlargement of the prostate, known as benign prostatic hyperplasia (BPH). These symptoms include frequency, urgency and, in extreme circumstances, acute retention of urine (Gannon et al. 2005). However, the enlargement may also be the result of a cancerous tumour.
Prostate cancer is the most common cancer in men in the UK. A quarter of all new cases of cancer diagnosed in men are prostate cancers. In 2014, around 46,690 men were diagnosed with prostate cancer in the UK. Incidence increases with age. It is uncommon in men before the age of 50 but rapidly increases in successive years. For men aged 55–59 the incidence rate per 100,000 is 181.4; for the range 65–69 it is 585.7/100,000 and for 85–89 the rate is 786.6/100,000 (CRUK 2017).
In 2014, there were 11,287 deaths in the UK from prostate cancer. Prostate cancer accounts for around 12% of male deaths from cancer in the UK and is the second most common cause of cancer death in men, after lung cancer. Approximately 92,300 men in Europe (EU-27) died from prostate cancer in 2012 and worldwide around 307,000 men died from the disease in 2012. Black, Asian and Minority Ethnic status (BAME) is related to mortality rates, which are generally high in predominantly black populations (Caribbean and sub-Saharan Africa), and very low in Asia. For example, African American men have an age adjusted incidence rate 1.6 times that of white American men and a UK study found that black men were three times more likely to be diagnosed with prostate cancer than white men. Subgroup analyses revealed that while the age-adjusted incidence rate for white men was 56.4/100,000 it was 173/100,000 for Afro-Caribbean men and 139/100,000 for black African men (Chinegwundoh et al. 2006). Like many cancers, the rates of PCa increase with age and more than 80% of prostate cancer deaths occur in men of 70 and over.
Diagnosis Symptoms of prostate cancer, including poor urine stream, hesitancy, terminal dribbling, retention and uraemia, usually start to develop once the tumour is large enough to press on the urethra and are very similar to those of BPH. The non-specificity of symptoms and their absence in some cases of cancer makes it difficult to identify the disease in its early stages, which is crucial for effective treatment. The situation is particularly challenging because at present there are no effective screening tests. Detection of PCa is usually on a case-finding basis whereby men that consider themselves at risk, because of family history, ethnicity or both, seek testing. Initial testing is generally by means of blood tests for Prostate Specific Antigen (PSA) accompanied by Digital Rectal Examination (DRE) of the prostate. If these tests indicate possible malignancy then the next stage is biopsy of the prostate. Unfortunately the PSA lacks specificity and sensitivitywhile the DRE can also fail to detect abnormalities in the prostate. Hence, there are no national screening programmes for PCa in either the UK or the US, although there are disagreements as to whether these should be introduced (Barry 2009).
An additional complicating factor is that men are frequently poorly informed about the nature and symptoms of PCa and their risk of developing the disease, with some evidence of ethnic variations (Prostate Cancer UK 2014). Studies of African-American and African men have found that both groups were unaware of the symptoms of the disease and of issues related to testing, early detection and treatment (Allen et al. 2007). Factors associated with low levels of knowledge included level of income and educational level, with some authors suggesting that when income levels are controlled the effect of ethnicity disappears (Winterich et al. 2009). For African-American men lack of knowledge was also associated with lack of medical insurance, indicating that issues of social disadvantage are important in addition to increased biological vulnerability (Allen et al. 2007). All of these may contribute to the poorer outcomes that have been reported for black men treated for prostate cancer (Allen et al. 2007). There have been several attempts to address these issues among African-American men, for example by educational and intervention programmes targeted specifically at this population. These interventions have been shown to improve knowledge of prostate cancer and uptake of screening programmes (Allen et al. 2007).
The fact that the symptoms involve potentially embarrassing urological problems may act as an additional cause of delay in addition to men’s unwillingness to consult doctors. Such barriers to consultation may be greater in some cultural/ethnic groups because of culturally mediated understandings of masculinity that increase resistance to help-seeking in general and investigations such as DREs in particular (Seymour-Smith et al. 2016).
The fact that the PSA test is widely recognised to be unreliable gives rise to challenges for GPs and Primary Care Physicians, in terms of providing guidance to men and enabling informed decision-making, and for men themselves in terms of deciding how they might wish to proceed in the face of uncertainty. There are concerns that testing can result in heightened anxiety in men even when the tests are negative (Macefield et al. 2010) and an elevated PSA can trigger additional more invasive investigations. From the few studies that have been carried out with GPs in relation to this issue there is evidence of considerable ambivalence concerning the PSA test and how best to raise the issue with men that may be at elevated risk and how to advise them about proceeding thereafter (Hale et al. 2010).
Treatment
Treatment depends on the stage of the disease. Castration (surgical or chemical) is often the treatment of choice for advanced cancer because it virtually eliminates testosterone, thereby slowing or stopping the growth of the tumour. Surgical removal of the prostate (radical prostatectomy or RP), external beam radiation therapy, brachytherapy (the implantation of radioactive beads in the prostate) and, in the case of slow-growing tumours, active surveillance may be selected for a localised tumour. All forms of treatment, apart from active surveillance, have been reported to cause temporary or permanent erectile dysfunction (Lavery and Cooperberg 2017). Other side effects include:
-
Urinary incontinence
-
Reduction in the length of the penis
-
Retrograde ejaculation
-
Faecal incontinence (following radiotherapy).
All have been found to have a substantial impact on men’s sense of masculine identity, which for some men results in social withdrawal and isolation (Gannon et al. 2010). The side effects impinge on and compromise characteristics that are associated with the concept of hegemonic masculinity, such as sexual potency, physical strength and emotional resilience.
Treating localised disease Although there are many treatments available for localised PCa surgical removal of the prostate followed by chemotherapy and/or radiation therapy remains the most common intervention and one that is the treatment of choice of many men (Lavery and Cooperberg 2017). Because of the proximity of nerves that controlerection and ejaculation to the prostate and effects on the urinary sphincter RP can result in long-lasting or permanent erectile dysfunction and some degree of urinary incontinence, which can also be long-lasting or permanent (Frey et al. 2014). The severity and duration of these side-effects of treatment have been reduced through the development of nerve-sparing surgical techniques and robotic surgery but they are nonetheless experienced to some degree by most men that undergo RP. The psychological and psychosocial impact depend to some extent on their severity, the age of the man concerned and cultural factors, but studies over the years have demonstrated that it is considerable (e.g. Chapple and Ziebland 2002; Eton and Lepore 2002; Fergus et al. 2002).
Although both ED and urinary incontinence can be distressing the evidence indicates that it is ED that has the most significant impact on men (Stanford et al. 2000). Studies have documented the way in which men’s sense of masculine identity can be challenged and compromised by a complete inability to achieve an erection or by an inability to achieve an erection sufficiently firm to permit intercourse (Grey et al. 2002). Men have described feeling less of a man and, particularly in the case of single men, avoiding social contexts in which the possibility of a sexual relationship might arise. For example, men in a study by Gannon et al. (2010) made comments such as
I am not the same I used to be. I can’t perform so I don’t go to places where I may meet people…
… but as a sexual partner I have no function now.
Even when there is no possibility of a sexual encounter men report distress due to the lack of a physical response to the sight of an attractive woman
let’s say if I see a pretty woman or a pretty girl on TV or something, it is nice but… I just think that is nice. Before probably could feel it was nice. At the moment it is purely in the mind.
Although aids to achieving an erection, such as vacuum pumps, viagra and injections, are available many men prefer not to use them. For some it is because the planning required to use the aids removes the spontaneity that is an important part of a sexual relationship and for others it relates to beliefs that erections should be “natural” and spontaneous. Men that are willing to consider using aids have reported a lack of information from GPs and healthcare professionals (Gannon et al. 2010).
Men adopt a range of strategies to adapt to and manage the distress related to ED. Some simply withdraw from sexual activity, some attempt to normalise this by framing it as something that is inappropriate for people of their age or as something that becomes less possible in a busy life. Others adapt their sexual behaviour to focus less on penetrative sex and more on providing sexual gratification to their partner by other means (Gannon et al. 2010).
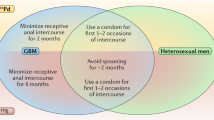
Some groups of men may be particularly affected by ED. Black men often develop the disease at a much younger age than white men, which means that they may have a greater desire to continue to be sexually active. In fact there is evidence that some Black men may be put off being investigated and treated for PCa because of a fear of ED (Weinrich et al. 1998). Gaymen and men that have sex with men (MSM) can also suffer a particular impact because of the fact that greater rigidity is required for anal than vaginal intercourse. In addition, the retrograde ejaculation that is a consequence of RP means a loss of what for many gay and MSM is an important element of the sexual act (Filiault et al. 2008).
In general, the physical side effects of treatment can have a marked psycho-social impact on men although they tend not to report these kind of worries to other people, even to their partners and physicians.
Given the severity of the side effects and the absence of a “gold standard” of treatment men are faced with a difficult choice between a range of options, each of which has serious and unpleasant side effects. There has been little systematic investigation of how such decisions are made, but there is evidence that up to 53% of men subsequently regret them (Steer et al. 2013).
Treating advanced and metastatic disease Tumour growth and development in prostate cancer, like some other cancers including types of breast cancer, is hormone-dependent. Androgens, principally testosterone, are closely implicated in the development, growth and maintenance of the disease and removal of androgens by means of surgical castration has been shown to result in dramatic regression of disease (Huggins and Hodges 1941).
Although surgical castration is still sometimes employed in the treatment of metastatic prostate cancer a range of hormonally-based treatments (sometimes referred to as “chemical castration”) have been developed over the past 30–40 years. These AndrogenDeprivation Therapies (ADT) are widely used in the treatment of locally spread (close to the prostate) and metastatic disease, although studies have found that significant numbers of men with non-metastatic disease receive hormonal intervention at some point (e.g. Cetin et al. 2013). Studies in the 1990s showed benefits of ADT in treating disease that recurred following local treatment (e.g. Messing et al. 1999). Almost half of all men treated for prostate cancer will be offered ADT if men with localised disease are included (Casey et al. 2012).
ADT is a collective term for hormone therapy, which can take a number of forms. Luteinizing hormone-releasing hormone (LHRH) agonists (also called LHRH analogs or GnRH agonists) act by reducing testosterone production in the testicles, though additional drugs are required to stop production at other sites in the body (including the prostate itself). Anti-androgens act by preferentially binding to the sites at which androgens act and thereby blocking them. GnRH antagonists (gonadotrophin-releasing hormone antagonists) are generally used when cancer has spread to the bones of the pelvis and spine.
ADT is widely considered as an effective treatment for prostate cancer (Bolla et al. 2008). It has been demonstrated to increase survival times for men with clinically localised or locally advanced disease and to provide improved symptom control, particularly pain relief, for men with advanced disease (Connolly et al. 2012). However it is associated with significant side effects, including hot flashes, osteoporosis, loss of muscle mass, breast enlargement, anaemia, fatigue, erectile dysfunction, loss of libido, risk of diabetes, risk of cardiovascular disease and, potentially fatal, cardiac events (Holzbeierlein et al. 2004). In addition to these physical effects, many of which parallel those of the menopause in women, there are growing concerns about the cognitive impact of ADT. Of particular concern is evidence implicating it in the development of dementia, including Alzheimer’s disease. A recent US study (Nead et al. 2017) collected data on 9272 men with prostate cancer and the analysis indicated a statistically significant (P < 0.001) association between use of ADT and risk of dementia. The increased risk of developing dementia was 4.4% for men who had received ADT compared with a group that had not.
There is also evidence that ADT can be associated with more subtle cognitive impairments, particularly in relation to executive functioning, which is involved in planning, initiating and sequencing complex goal-directed behaviours. The evidence for a relationship is not clear and studies are not all in agreement. Green et al. (2002) concluded that ADT may be associated with impairments to executive function as well as to memory and attention while other authors such as Joly et al. (2006) and Salminen et al. (2003) found no such association. However, subsequent studies by Salminen et al. (2004, 2005) indicated an association between falling levels of testosterone and a decline in cognitive performance. More recent work by Alibhai et al. (2010) and Wiechno et al. (2013) concluded that ADT had no or a negligible effect on cognitive function. One explanation for the differences in findings is that some tests are insufficiently sensitive to detect impairments and small sample sizes may also be an issue.
While the evidence at present is inconclusive there are reports from men receiving ADT of cognitive difficulties, which they attribute to ADT (Cherrier et al. 2009). This is clearly an area in which further research and the development of sufficiently sensitive neuropsychological measures of executive function are required. Given the substantial number of men receiving some form of ADT it is undoubtedly of considerable clinical and social significance.
The feminising effects of ADT, such as breast enlargement, genital shrinkage, hot flushes, loss of muscle and weight gain can also have a significant impact on men‘s sense of masculinity (Oliffe 2006). Another contributor to this sense of diminished masculinity is increased emotional lability and mood swings (Cary et al. 2014), particularly a greater proneness to tearfulness (Ng et al. 2012). There is also evidence that ADT is associated with depression, probably as a consequence of the reduction in testosterone levels (Lee et al. 2015). It is important to bear in mind that the experience of prostate cancer and the impact of the side-effects of treatment may well contribute to depression and there is evidence that a significant minority of patients not undergoing ADT also experience symptoms (Bennett and Badger 2005).
Prostate Cancer and the Heterosexual Couple
The partners of men with prostate cancer are a crucial source of support throughout the trajectory of the disease from diagnosis, through treatment-related decision-making, treatment and beyond to the transition to survivorship. Indeed, prostate cancer has been described as a couple’s disease because of the way in which both partners are so intimately involved at all stages and each is affected by the experiences they encounter (Harden et al. 2013; Williams et al. 2014). Men clearly benefit from having a supportive partner, for example in terms of improved quality of Life (Gore et al. 2005; Soloway et al. 2005) and better physical and mental health (Krongrad et al. 1996) compared with patients without a partner. The duration of survivorship is greater for married men (Banthia et al. 2003) and partner involvement in care is associated with improved adjustment and emotional health for the patients (Riechers 2004).
It has been recognised for some time now that men often require encouragement from their partner to seek medical advice in relation to symptoms of illness (Norcross et al. 1996) and this is also the case in prostate cancer (Seymour-Smith et al. 2002). Their partner will frequently accompany men to these initial and subsequent appointments and are closely involved in making decisions concerning treatment (Jacobs et al. 2002; Malcarne et al. 2002; Davison et al. 2002). While, as noted above, men are sometimes concerned about the potential impact of side effects erectile dysfunction, women are generally more concerned about survival (Badr and Carmack Taylor 2009). Nevertheless, the side-effects associated with treatment, including both the physical and emotional aspects, do have an emotional impact on the partner. In addition, women frequently express frustration and distress about the unwillingness of their partner to openly share their feelings and they can feel emotionally cut-off from them (Badr and Carmack Taylor 2009). As a result of this range of challenging and distressing experiences female partners of men with prostate cancer report levels of psychological distress that are in general higher than those of their partners (Herr 1997).
Prostate Cancer and GayMen/Men That Have Sex with Men
There are good reasons for thinking that sexual orientation is an important factor in people’s experiences of the healthcare system. Studies have documented accounts from lesbian, gay, bisexual and trans (LGBT) people of experiences of both heteronormativity and homophobia in the healthcare system (e.g. Dean et al. 2000) while others have found that LGBT individuals were reluctant to disclose their sexual orientation to healthcare professionals for fear of homophobia (e.g. Klitzman and Greenberg 2002) or because of concerns about confidentiality (e.g. Cant and Taket 2006). Even in the absence of homophobia LGBT people report experiencing a system in which heterosexuality is assumed to be the norm (e.g. Heaphy et al. 2003) and in which questions about partners or sexual practices are grounded in this assumption (e.g. Neville and Henrickson 2006). Such research suggests that gaymen and men that have sex with men (MSM) may well experience challenges and difficulties in the course of receiving a diagnosis of and undergoing treatment for prostate cancer.
Men in general know very little about the location and function of their prostate and of their risk of developing prostate cancer (e.g. Baker et al. 2007). There is almost no research that has specifically addressed this issue in relation to gaymen/MSM, but a focus group study (Asencio et al. 2009) found that a group of self-identified gaymen had little or no knowledge of the prostate and the potential consequences of the treatment of prostate cancer for sexual activity and performance. Additionally, a study of the relationship between sexual orientation and screening for prostate cancer conducted in California (Heslin et al. 2008) found that gaymen/MSM were less likely to have been screened than exclusively heterosexual men.
We know that female partners of heterosexual men appear to play a significant role in caring for their health and prompting them to seek medical advice but almost nothing about the role played by the partner or friends of gaymen/MSM in their healthcare. Similarly, while female partners play a very significant role in treatment-related decision-making (e.g. Sinfield et al. 2009; Boehmer and Clark 2001) information about the experiences of gaymen/MSM in this regard is lacking.
As described above, it is well established that all forms of treatment for prostate cancer result in a range of unpleasant and distressing side-effects and that such side-effects have a significant impact on quality of life (e.g. Sanda et al. 2008) and on the man’s sense of masculinity (e.g. Stansbury et al. 2005). Experiences of the side effects of treatment for prostate cancer in gay/MSM are likely to be shaped both by prevalent norms within the gay/MSM community and the forms of sexual activity engaged in by individual men. The common side effects, such as erectile dysfunction, urinary incontinence and retrograde ejaculation, are likely to have somewhat different significance for gay compared to straight men (Blank 2005). For example, the degree of rigidity required for anal penetration is greater than that required for vaginal penetration; semen can have non-reproductive significance in the context of gay/MSM sexual activity and the prostate itself is the site of erotic stimulation (Blank 2005; Filiault et al. 2008).
Unlike the situation of female partners of heterosexual men we know nothing about the psychological effects on the partners of gaymen and very little about how gaymen/MSM with prostate cancer and their partners access and make use of support.
Some helpful light can be shed on possible issues facing gaymen living as survivors of prostate cancer by considering the findings of a study of chronic illness in non-heterosexuals (Jowett and Peel 2009). These authors employed an online survey aimed at the LGBT community in the UK and internationally and received responses from 190 self-identified LGBT individuals who were living with a chronic illness. They identified a number of themes in the responses that are relevant to gaymen surviving prostate cancer. One issue was that respondents often experienced the LGBT community as being unsupportive of people with chronic illnesses other than HIV/AIDS. A related point was that a perceived culture that emphasises bodily perfection within the gay community could present the chronically ill with difficulties. This might be particularly relevant to gaymen who have scars and reduced penile length due to radical prostatectomy or who are experiencing bodily changes as a consequence of hormone therapy. A second theme was one of feeling isolated from the LGBT community and the difficulties of identifying others within the LGBT community with the same difficulties, describing themselves as a “minority within a minority”. They also identified themes relating to issues identified above, such as fear of homophobia in the healthcare system and lack of information and support tailored to their particular needs.
Overall, the experiences and needs of gaymen/MSM and the LGBT community more generally have largely been overlooked in research into cancers of all kinds. There is undoubtedly a need for more research to focus on the relationship between sexual orientation and cancer detection, treatment and survivorship generally as well as for prostate cancer in particular (Boehmer et al. 2012).
Surviving Prostate Cancer
In the period 2010–2011, in England and Wales the one-year survival rate for prostate cancer was 94% and the five-year rate was 85%. These survival rates were the highest among the 21 most common cancers in the UK (CRUK 2018). Prostate cancer patients can be characterised as long-term survivors with a high probability of being alive 5 years after the initial diagnosis. While this is excellent news it raises issues about how to support men in living with the side effects described above and dealing with the ongoing uncertainty concerning recurrence that all cancer survivors must contend with. In the case of men this is likely to be exacerbated by their demonstrated difficulties in accessing and making use of social and medical support compared with women in general and womencancer survivors in particular. The participation of patients in treatment-related decision-making and acknowledgement of side effects has been shown to influence their adjustment to their post-treatment life and treatment side effects are also important. The majority of studies have not found significant differences in general health-related quality of life (HRQoL) scores but they have identified differences in disease-specific HRQoL scores. Bacon and his colleagues (2001) examined PCa patients who had received radiotherapy and brachytherapy (the implantation of radioactive beads directly into the prostate) and they reported more bowel dysfunction than those with prostatectomy. Patients treated with radiotherapy and hormones had better or the same sexual and urinary function but lower QoL scores in many domains compared to the prostatectomy patients. Patients who underwent brachytherapy and those who had prostatectomy had similar QoL scores. Patients that had radical prostatectomy had higher HRQoL scores compared to those who did not have treatment and those who had a radiotherapy. Patients who chose therapy with hormoneshad the lowest HRQoL scores among the other treatment groups.
Typically, once men have been successfully treated for prostate cancer they are discharged back to primary care. There is very little research on transfer from hospital-based care to primary care for disease monitoring after primary treatment has been delivered, and most of this has focused on discharge from intensive and acute care. There are a small number of studies that have addressed the ongoing needs of cancer survivors in relation to primary care. Harrison et al. (2012) studied cancer survivors’ experiences of discharge from hospital follow-up. Survivors of breast, colorectal and prostate cancer (n = 1275), 5–16 years post diagnosis were recruited for a questionnaire survey. Approximately one-third of respondents were not discharged from follow-up 5–16 years post diagnosis. Of those who were discharged, a substantial minority reported insufficient time (27.9%), information (24.5–45.0%) or adverse emotions (30.9%) at the time of discharge. However, 90.6% of respondents reported satisfaction with how discharge from hospital follow-up was managed. As part of the same study the researchers (Harrison et al. 2012) also examined the primary health and supportive care needs of the survivors. The most frequently endorsed unmet need was for help to manage concerns about cancer recurrence. Trait anxiety, non-discharged status, dissatisfaction with discharge and receipt of hormonal therapy were predictive of unmet supportive care needs. The most frequently reported unmet needs were “help to manage my concerns about the cancer coming back” and “I need to know that all my doctors talk to each other to coordinate my care”.
Hudson et al. (2012) reported the findings of a US-based study. They conducted in-depth interviews with a purposive sample of early-stage breast and prostate cancer survivors (N = 42) aged from 47 to 80 years, stratified by age, race, and length of time from and location of cancer treatment all of whom had completed treatment at least two years previously. Survivors were at least 2 years beyond completion of their active cancer treatment. Most participants expressed strong preferences to receive follow-up care from their cancer specialists (52%). They described the following barriers to the primary care physician’s engagement in follow-up care: (1) lack of cancer expertise, (2) limited or no involvement with original cancer care, and (3) lack of care continuity. Only one-third of participants (38%) believed there was a role for primary care in cancer follow-up care. While it is important to acknowledge the differences in the way healthcare is delivered in the UK and the US the findings of this study are broadly consistent with the findings of Harrison et al.
These studies raise important questions and some concerns about the way in which the transition to primary care is managed. The focus of survivorship research has been on the patients but the fact that men’s partners are very important in providing support and contributing to decision-making but also experience emotional distress means that it is also important to consider their needs for information and support. Again, very little research or intervention work has been done in this area.
The fact that African-Caribbean and African-American men are at greater risk of developing prostate cancer and also tend to develop it at a younger age than white men means that their experiences and needs as survivors of the disease are likely to be different. This is an area that requires more research attention than it has so far received, but issues relating to sexual performance, fertility and communication of risk to close male relatives are likely to be salient. There are reports that at least some GPs are lacking in awareness of the elevated risk of African-Caribbean men (Thompson 2014) and this may have consequences once these men are discharged back to primary care following treatment in terms of trust in the relationship.
Conclusions and Recommendations
Prostate cancer is virtually a paradigmatic exemplar of the need to adopt a gendered approach to understanding men’s health-related behaviours. Each stage of the journey through prostate cancer, from noticing and acting on symptoms via treatment-related decision-making to being a survivor raises issues and challenges that are grounded in personally and socially constructed understandings of what it is to be a man. The concept of hegemonic masculinity is one way of framing these issues and has been much used in terms of directing and interpreting the findings of research, but it ignores structural inequalities grounded in race and social status that are demonstrably important in the case of prostate cancer in particular, and of men‘s health more generally. A gendered understanding of men’s health that is also cognizant of the importance of such structural inequalities is a key underpinning for research, practice and social policy in the arena of men’s health.
Implications for Practice and Research
Men’s management of their health and their responses to illness and to treatment are influenced by prevailing conceptions and constructions of masculinity. Structural inequalities also play a significant part. Each type of health problem will raise specific issues, but it is possible to identify some broad guiding principles and make suggestions informed by theory and research:
Healthcare professionals of all types need to take gender into account in working with men in both physical and mental health contexts.
Social constructionist, narrative and systemic approaches may be helpful to men in terms of examining and challenging dominant constructions.
Men in minority groups, such as ethnic and sexual minorities, and lower income groups are likely to suffer particular disadvantages, which intersect with issues related to gender.
In terms of research we need to develop a better understanding of how these gendered and structural issues interact and determine outcomes and processes in relation to particular health conditions. In the case of prostate cancer there is a particular need to understand treatment-related decision-making, survivorship and the experiences of men from ethnic and sexual minorities.
References
Alibhai, S. M. H., Breunis, H., Timilshina, N., Marzouk, S., Stewart, D., Tannock, I., et al. (2010). Impact of androgen-deprivation therapy on cognitive function in men with nonmetastatic prostate cancer. Journal of Clinical Onclology,28, 5038–5045.
Allen, J. D., Kennedy, M., Wilson-Glover, A., & Gilligan, T. D. (2007). African-American men’s perceptions about prostate cancer: Implications for designing educational interventions. Social Science and Medicine,64, 2189–2200.
Asencio, M., Blank, T., Descartes, L., & Crawford, A. (2009). The prospect of prostate cancer: A challenge for gay men’s sexualities as they age. Sexuality Research & Social Policy,6(4), 38–51.
Bacon, C. G., Giovannucci, E., Testa, M., & Kawachi, I. (2001). The impact of cancer treatment on quality of life outcomes for patients with localized prostate cancer. Journal of Urology,166, 1804–1810.
Badr, H., & Carmack Taylor, C. L. (2009). Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psycho-Oncology,18, 735–746.
Baker, R., Sinfield, P., Agarwal, S., Tarrant, C., Steward, W., Mellon, J. K., et al. (2007). Prostate cancer care: Improving measures of the patient experience. Report for the NHS Service Delivery and Organisation R&D (NCCSDO). London: SDO. www.sdo.nihr.ac.uk.
Banthia, R., Malcarne, V. L., Varni, J. W., Ko, C. M., Sadler, G. R., & Greenbergs, H. L. (2003). The effects of dyadic strength and coping styles on psychological distress in couples faced with prostate cancer. Journal of Behavioral Medicine,26(1), 31–52.
Barry, M. J. (2009). Screening for prostate cancer—The controversy that refuses to die. New England Journal of Medicine,360(13), 1351–1354.
Bennett, G., & Badger, T. A. (2005). Depression in men with prostate cancer. Oncology Nursing Forum,32, 545–556.
Blank, T. (2005). Gay men and prostate cancer: Invisible diversity. Journal of Clinical Oncology,12, 2593–2596.
Boehmer, U., & Clark, J. A. (2001). Married couples’ perspectives on prostate cancer diagnosis and treatment decision-making. Psycho-Oncology,10, 147–155.
Boehmer, U., Cooley, T. P., & Clark, M. A. (2012). Cancer and men who have sex with men: A systematic review. Lancet Oncology,13(12), e545–e553.
Bolla, M., Collette, L., Van Tienhoven, G., WArde, P., Dubois, J. B., Mirimanoff, R. O. M., et al. (2008). Ten year results of long-term androgen deprivation therapy with goserelin in patients with locally-advanced prostate cancer treated with radiotherapy: A phase III EORTC study. Radiation Oncology,72(Suppl. 1), S30–S31.
Cant, B., & Taket, A. (2006). Lesbian and gay experiences of primary care in one borough in North London, UK. Diversity in Health and Social Care,3(4), 271–279.
Cary, K. C., Singla, N., Cowan, J. E., Carroll, P. R., & Cooperberg, M. R. (2014). Impact of androgen deprivation therapy on mental and emotional well being in men with prostate cancer: Analysis from the CaPSURE registry. Journal of Urology,191, 964–970.
Casey, R. G., Corcoran, N. M., & Goldenberg, S. L. (2012). Quality of life issues in men undergoing androgen deprivation therapy a review. Asian Journal of Andrology,14(2), 226–231.
Cetin, K., Li, S., Blaes, A. H., Stryker, S., Liede, A., & Arneson, T. J. (2013). Prevalence of patients with nonmetastatic prostate cancer on androgen deprivation therapy in the United States. Urology,81(6), 1184–1189.
Chapple, A., & Ziebland, S. (2002). Prostate cancer: Embodied experience and perceptions of masculinity. Sociology of Health & Illness,24(6), 820–841.
Cherrier, M. M., Aubin, S., & Higano, C. S. (2009). Cognitive and mood changes in men undergoing intermittent combined androgen blockade for non-metastatic prostate cancer. Psycho-Oncology,18, 237–247.
Chinegwundoh, F., Enver, M., Lee, A., Nargund, V., Oliver, T., & Ben-Shlomo, Y. (2006). Risk and presenting features of prostate cancer amongst African-Caribbean, South Asian and European men in north-east London. British Journal of Urology International,98, 1216–1220.
Connolly, R. M., Carducci, M. A., & Antonarakis, E. S. (2012). Use of androgen deprivation therapy in prostate cancer: Indications and prevalence. Asian Journal of Andrology,14(2), 177–186.
CRUK Website. Retrieved December 2, 2017, from http://www.cancerresearchuk.org.
CRUK. (2018). Prostate cancer survival statistics. Retrieved December 9, 2018, from https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/survival#ref-0.
Davison, J. B., Gleave, M. E., Goldenberg, L. S., Degner, L. F., Hoffart, D., & Berkowitz, J. (2002). Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nursing,25(1), 42–49.
Dean, L., Meyer, I., Robinson, K., Sell, R., Sember, R., Silenzio, V., et al. (2000). Lesbian, gay, bisexual, and transgender health: Findings and concerns. Journal of the Gay and Lesbian Medical Association,4, 102–151.
Eton, D. T., & Lepore, S. J. (2002). Prostate cancer and health-related quality of life: A review of the literature. Psycho-Oncology,11, 307–326.
Fergus, K., Gray, R., & Fitch, M. (2002). Sexual dysfunction and the preservation of manhood: Experiences of men with prostate cancer. Journal of Health Psychology,7(3), 303–316.
Filiault, S. M., Drummond, M. J. N., & Smith, J. A. (2008). Gay men and prostate cancer: Voicing the concerns of a hidden population. Journal of Men’s Health,5(4), 327–332.
Frey, A. U., Sonksen, J., & Fode, M. (2014). Neglected side effects after radical prostatectomy: A systematic review. Journal of Sexual Medicine,11(2), 374–385.
Gannon, K., Glover, L., O’Neill, M., & Emberton, M. (2005). Lower urinary tract symptoms in men: Self-perceptions and the concept of bother. BJU International,96, 823–827.
Gannon, K., Guerro-Blanco, M., & Abel, P. D. (2010). Reconstructing masculinity following radical prostatectomy for prostate cancer. The Aging Male,13(4), 258–264.
Gore, J. L., Krupski, T., Kwan, L., Maliski, S., & Litwin, M. S. (2005). Partnership status influences quality of life in low-income, uninsured men with prostate cancer. Cancer,104(1), 191–198.
Green, H. J., Pakenham, K. I., Headley, B. C., Yaxley, J., Nicol, D. L., Mactaggart, P. N., et al. (2002). Altered cognitive function in men treated for prostate cancer with luteinizing hormone-releasing hormone analogues and cyproterone acetate: A randomized controlled trial. BJU International,90, 427–432.
Grey, R. E., et al. (2002). Prostate cancer and erectile dysfunction: Men’s experiences. International Journal of Men’s Health,1(1), 15–29.
Hale, S., Groga, S., & Willott, S. (2010). Male GPs’ views on men seeking medical help: A qualitative study. British Journal of Health Psychology,15, 697–713.
Harden, J., Sanda, M. G., Wei, J. T., Yarandi, H. N., Hembroff, L., & Hardy, J. (2013). Survivorship after prostate cancer treatment: Spouses’ quality of life at 36 months. Oncology Nursing Forum,40(6), 567–573.
Harrison, S. E., Watson, E. K., Ward, A. M., Khan, N. F., Turner, D., Adams, E., et al. (2012). Cancer survivors’ experiences of discharge from hospital follow-up. European Journal of Cancer Care,21(3), 390–397.
Heaphy, B., Yip, A., & Thompson, D. (2003). Lesbian, gay and bisexual lives over 50. Nottingham: York House.
Herr, H. W. (1997). Quality of life in prostate cancer patients. CA: A Cancer Journal for Clinicians,47(4), 207–217.
Heslin, K. C., Gore, J. L., King, W. D., & Fox, S. A. (2008). Sexual orientation and testing for prostate and colorectal cancers among men in California. Medical Care,46(12), 1240–1248.
Holzbeierlein, J. M., Castle, E., & Thrasher, J. B. (2004). Complications of androgen deprivation therapy: Prevention and treatment. Oncology,18, 303–309.
Hudson, S. V., Miller, S. M., Hemler, J., Ferrante, J. M., Lyle, J., Oeffinger, K. C., et al. (2012). Adult cancer survivors discuss follow-up in primary care: ‘Not what I want, but maybe what I need’. Annals of Family Medicine,10(5), 418–427.
Huggins, C., & Hodges, C. V. (1941). Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Cancer Research,1(4), 293–297.
Jacobs, J. R., Banthia, R., Robins Sadler, G., Varni, J. W., et al. (2002). Problems associated with prostate cancer: Differences of opinion among health care providers, patients, and spouses. Journal of Cancer Education,17, 33–36.
Joly, F., Alibhai, S. M., Galica, J., Park, A., Yi, Q. L., Wagner, L., et al. (2006). Impact of androgen deprivation therapy on physical and cognitive function, as well as quality of life of patients with nonmetastatic prostate cancer. Journal of Urology,176(6 pt 1), 2443–2447.
Jowett, A., & Peel, E. (2009). Chronic illness in non-heterosexual contexts: An online survey of experiences. Feminism and Psychology,19(4), 454–474.
Klitzman, R., & Greenberg, J. (2002). Patterns of communication between gay and lesbian patients and their health care providers. Journal of Homosexuality,42, 65–75.
Krongrad, A., Lai, H., Burke, M. A., Goodkin, K., & Lai, S. (1996). Marriage and mortality in prostate cancer. The Journal of Urology,156(5), 1696–1700.
Lavery, H. J., & Cooperberg, M. R. (2017). Clinically localized prostate cancer in 2017: A review of comparative effectiveness. Urologic Oncology,35(2), 40–41.
Lee, M., Jim, H. S., Fishman, M., et al. (2015). Depressive symptomatology in men receiving androgen deprivation therapy for prostate cancer: A controlled comparison. Psycho-Oncology,24, 472–477.
Macefield, R. C., Metcalfe, C., Lane, J. A., Donovan, J. L., Avery, K. N. L., Blazeby, J. M., et al. (2010). Impact of prostate cancer testing: an evaluation of the emotional consequences of a negative biopsy result. British Journal of Cancer,102, 1335–1340.
Malcarne, V. L., Banthia, R., Varni, J. W., Robins Sadler, G., Greenbergs, H. L., & Ko, C. M. (2002). Problem-solving skills and emotional distress in spouses of men with prostate cancer. Journal of Cancer Education,17, 150–154.
Messing, E. M., Manola, J., Sarosdy, M., Wilding, G., Crawford, E. D., & Trump, D. (1999). Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. New England Journal of Medicine,341, 1781–1788.
Nead, K. T., Gaskin, G., Chester, C., Swisher-McClure, S., Leeper, N. J., & Shah, N. H. (2017). Association between androgen deprivation therapy and risk of dementia. JAMA Oncology,3(1), 49–55.
Neville, S., & Henrickson, M. (2006). Perceptions of lesbian, gay and bisexual people of primary healthcare services. Journal of Advanced Nursing,55(4), 407–415.
Ng, E., Woo, H. H., Turner, S., Leong, E., Jackson, M., & Spry, N. (2012). The influence of testosterone suppression and recovery on sexual function in men with prostate cancer: Observations from a prospective study in men undergoing intermittent androgen suppression. Journal of Urology,187, 2162–2166.
Norcross, W., Ramirez, C., & Palinkas, L. A. (1996). The influence of women on the health-care seeking behaviour of men. Journal of Family Practice,43(5), 475–480.
Oliffe, J. (2006). Embodied masculinity and androgen deprivation therapy. Sociology of Health & Illness,28, 410–432.
Prostate Cancer UK. (2014). Retrieved May 30, 2018, from https://prostatecanceruk.org/for-health-professionals/our-projects/public-awareness-study.
Riechers, E. A. (2004). Including partners into the diagnosis of prostate cancer: A review of the literature to provide a model of care. Urologic Nursing,24(1), 22–38.
Salminen, E. K., Portin, R. I., Koskinen, A., Helenius, H., & Nurmi, M. (2003). Androgen deprivation and cognition in prostate cancer. British Journal of Cancer,89, 971–976.
Salminen, E. K., Portin, R. I., Koskinen, A., Helenius, H., & Nurmi, M. (2004). Associations between serum testosterone fall and cognitive function in prostate cancer patients. Clinical Cancer Research,10, 7575–7582.
Salminen, E. K., Portin, R. I., Koskinen, A., Helenius, H., & Nurmi, M. (2005). Estradiol and cognition during androgen deprivation in men with prostate carcinoma. Cancer,103, 1381–1387.
Sanda, M. G., Dunn, R. L., Michalski, J., et al. (2008). Quality of life and satisfaction with outcome among prostate cancer survivors. New England Journal of Medicine, 358, 1250–1261.
Seymour-Smith, S., Brown, D., Cosma, G., Shopland, N., Battersby, S., & Burton, A. (2016). “Our people has got to come to terms with that”: Changing perceptions of the digital rectal examination as a barrier to prostate cancer diagnosis in African-Caribbean men. Psycho-Oncology,25, 1183–1190.
Seymour-Smith, S., Wetherell, M., & Phoenix, A. (2002). My wife ordered me to come: A discursive analysis of doctors’ and nurses’ accounts of men’s use of general practitioners. Journal of Health Psychology, 7(3), 253–276.
Sinfield, P., et al. (2009). Men’s and carers’ experiences of care for prostate cancer: A narrative literature review. Health Expectations,12, 301–312.
Soloway, C. T., Soloway, M. S., Kim, S. S., & Kava, B. R. (2005). Sexual, psychological and dyadic qualities of the prostate cancer ‘couple’. BJU International,95(6), 780–785.
Stanford, J. L., Feng, Z., Hamilton, A. S., Gilliland, F. D., Stephenson, R. A., Eley, J. W., et al. (2000). Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: The prostate cancer outcomes study. Journal of the American Medical Association,283, 354–360.
Stansbury, J. P., Mathewson-Chapman, M., & Grant, K. E. (2005). Gender schema and prostate cancer: Veterans’ cultural model of masculinity. Medical Anthropology,22, 175–204.
Steer, A. N., Aherne, N. J., Gorzynska, K., Hoffman, M., Last, A., Hill, J., et al. (2013). Decision regret in men undergoing dose-escalated radiation therapy for prostate cancer. International Journal of Radiation Oncology, 86(4), 716–720.
Thompson, R. (2014). Hear me now one year on. BME Cancer Communities. Retrieved May 31, 2018, from https://bmecancer.co.uk/reports/hmn_year.pdf.
Weinrich, S. P., Boyd, M. D., Bradford, D., et al. (1998). Recruitment of African Americans into prostate cancer screening. Cancer Practice,6(1), 23–30.
Wiechno, P. J., Sadowska, M., Kalinowksi, T., Michalski, W., & Demkow, T. (2013). Does pharmacological castration as adjuvant therapy for prostate cancer after radiotherapy affect anxiety and depression levels, cognitive functions and quality of life? Psycho-Oncology,22, 346–351.
Williams, K. C., Hicks, E. M., Chang, N., Connor, S. E., & Maliski, S. L. (2014). Purposeful normalization when caring for husbands recovering from prostate cancer. Qualitative Health Research,24(3), 306–316.
Winterich, J. A., Grzywacz, J. G., Quandt, S. A., Clark, P. E., Miller, D. P., Acuña, J., et al. (2009). Men’s knowledge and beliefs about prostate cancer: Education, race, and screening status. Ethnicity and Disease,19(2), 199–203.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Gannon, K. (2019). Men’s Health and Cancer—The Case of Prostate Cancer. In: Barry, J.A., Kingerlee, R., Seager, M., Sullivan, L. (eds) The Palgrave Handbook of Male Psychology and Mental Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-04384-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-04384-1_8
Published:
Publisher Name: Palgrave Macmillan, Cham
Print ISBN: 978-3-030-04383-4
Online ISBN: 978-3-030-04384-1
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)